Abstract
Excessive alcohol use is a risk factor for most cardiac diseases. The prevalence of unhealthy alcohol use among hospitalized cardiac patients is uncertain as is the frequency with which it is addressed. We performed a single center, patient-level anonymous survey among hospitalized cardiac patients eligible for cardiac rehabilitation. Hazardous drinking was defined as an Alcohol Use Disorders Identification Test (AUDIT) score of 8 or greater. Binge drinking was defined as 5+ drinks for men or 4+ for women on ≥1 occasion within the past 30 days. Unhealthy drinking was defined as either hazardous or binge drinking. Of 300 patients approached, 290 (96.7%) completed the survey. Mean (±SD) age was 69±11 years; 70% were male and 31% were cardiac surgical patients. The proportion (95% CI) of hazardous, binge, and unhealthy drinking was 12% (9–16), 16% (12–20), and 18% (14–23), respectively. Overall, 58% of subjects reported being screened for alcohol use, mostly by nurses (56%). Those with unhealthy drinking reported being counseled more frequently about their alcohol use compared to non-unhealthy drinkers (11% vs 3%, p=0.03), but the large majority (89%) of unhealthy drinkers reported receiving no advice about their alcohol use while admitted. In conclusion, almost one-fifth of hospitalized cardiac patients reported unhealthy drinking, these patients were only screened about half of the time, and were rarely counseled about their alcohol use.
Keywords: Alcohol Use Disorder, Quality of Care, Hospital Screening
INTRODUCTION
A variety of old observational studies suggested that moderate alcohol consumption, defined as one drink per day for women and two drinks per day,1 might be cardioprotective.2–5 As a result, cardiovascular clinicians may be less apt to screen or counsel patients on alcohol use, despite a known 7% prevalence of hazardous drinking in the general public and guidelines that recommend universal screening.6–7 This is particularly problematic as, emerging research now concludes that alcohol confers no health benefits and that the safest level of use is none.8 Moreover, heavy alcohol use, especially binge drinking, has long been associated with increased risk of cardiovascular death from myocardial infarction (MI), heart failure (HF), and stroke, 9–12 but little is known about the prevalence of unhealthy drinking among hospitalized cardiac patients and how often they are screened or counseled. To address this question, we surveyed inpatients with acute cardiac illness regarding their alcohol use, receipt of screening, and reported counseling from healthcare professionals during admission.
METHODS
We performed an anonymous, single-center, patient-level survey among consecutive patients hospitalized with acute cardiac illnesses and referred for cardiac rehabilitation at Baystate Medical Center, a 760-bed tertiary care center, which serves as the only regional percutaneous coronary intervention (PCI) and cardiac surgical capable center in Western Massachusetts and is also affiliated with the University of Massachusetts of Medical School. Between June 2019 and September 2019, we approached adults, aged 18 years or older, admitted to hospital with acute coronary syndromes [MI or unstable angina], atherosclerotic peripheral vascular disease (PVD), and chronic systolic HF, as well as those undergoing coronary artery bypass grafting (CABG), PCI, and/or heart valve repair/replacement. In order to maximize generalizability and survey representativeness, exclusion criteria were minimized and excluded only those who spoke a language other than Spanish or English, were cognitively unable to complete the survey, or were deemed too frail to participate in cardiac rehabilitation, such as those with a planned discharge to hospice or long-term nursing home.
To maximize our response rate and reduce the risk of social desirability bias, several steps were taken to keep the survey anonymous. First, patients were specifically told not to put their name or any identifying information on the survey. Second, no links to the name or medical record number or participants were ever made. Third, at the end of each week, the list used to recruit patients was destroyed. In order to assure patient eligibility, all patient charts were evaluated by phase I cardiac rehabilitation staff members who confirmed their diagnosis and eligibility allowing us verify eligibility while maintaining anonymity. At no point was any protected health information retrieved, recorded, or verified from the electronic medical record by the research team.
A member of the research team approached eligible patients, and verbally verified the reason for admission to the hospital. If a patient was busy or unavailable, the team returned up to three additional times to ask for participation. If a patient declined to participate, they were no longer approached. Consistent with patterns known in inpatient cardiac rehabilitation,13 patients were typically approached towards the end of their hospitalization. No patients were surveyed on the day or admission or while in an intensive care unit. This procedure allowed the hospital team the maximal chance to screen the patient for alcohol use, while still allowing time for the research team to approach patients. The purpose and intent of the survey was then explained in detail including risks and benefits of participation. Patients were allowed to skip any questions which they preferred not to answer. The study protocol was approved by the Institutional Review Board of Baystate Medical Center, who deemed survey completion to be adequate documentation of consent. No compensation was included for study participation. Survey results were collected and managed using REDCap electronic data capture tools hosted at Tufts Medical Center.
The survey itself consisted of three sections. The first section used the Alcohol Use Disorders Identification Test (AUDIT), a 10-question validated screen for alcohol use disorders.14 This section included a both visual and written description of the definition of a standard drink of alcohol. The second section included 16 questions that assessed the patient’s experience of alcohol use screening and counseling while in the hospital, as well as any prior experience patients may have had with alcohol counseling from healthcare providers. These 16 questions were then cognitively tested for content clarity with a convenience sample of 15 eligible patients admitted to inpatient cardiac units. Cognitive testing was used to ensure ease of use, comprehensiveness, appropriate length, and clarity.15 The survey was written at a Flesch-Kincaid Grade Level of 8.2. The final section of the survey included 9 questions that assessed demographic, medical, and social factors. The complete survey tool is found in the supplementary material. Certified medical translators translated the survey into Spanish.
The National Institute of Health definition of a “standard drink,” 14 grams of pure alcohol, was utilized and included in the survey.16 Hazardous alcohol consumption was defined as an AUDIT score of ≥8.14 Binge drinking was defined as 5 or more alcoholic drinks for males or 4 or more alcoholic drinks for females on the same occasion (i.e., at the same time or within a couple of hours of each other) at least once in the past month.17 For the purposes of this study, we defined “unhealthy drinking” as either hazardous alcohol use or binge drinking.
The primary outcome assessed was the rate of unhealthy drinking among patients admitted for acute cardiac illnesses. Secondary outcomes evaluated patients’ experience with alcohol use screening and counseling both in the acute inpatient setting as well as what, if any, prior experience they had with screening or counseling with healthcare professionals.
Although definitions of alcohol use vary, about 9% of US adults meet the criteria for an alcohol use disorder.5 The 2015 US National Survey on Drug Use and Heath, reports the incidence of heavy drinking and binge alcohol use to be around 7% and 25%, respectively, 7 although these proportions vary substantially based on age. To allow us to assess a range of proportions for hazardous, binge, and unhealthy drinking with modest precision, we planned to survey 300 patients, which would allow us to calculate these proportions with a 3% margin of error. Categorical data was summarized with frequencies and proportions. Continuous variables were reported as means, medians and interquartile ranges for continuous variables with 95% confidence intervals. For univariable analyses, t-tests were employed for continuous variables and chi-square or odds ratio for categorical variables, as appropriate with 95% confidence intervals. Finally, to understand patterns in screening and counseling, we used multivariable logistic regression to estimate the cross-sectional associations between patient characteristics and these outcomes. Software used included JMP 12.01 (Cary NC) and MedCalc Version 15.0 Software (Ostend, Belgium). A p-value of <0.05 was considered significant.
RESULTS
Over 4-months, we approached 300 patients of whom 290 (96.7%) completed the survey. Most survey participants were male, white, with and about 69 years old (Table 1). Most common admitting diagnosis was MI with 32% of patients having undergone cardiac surgery. Most patients drank only occasionally and roughly 17% of patients identified themselves as daily drinkers. On days when alcohol was consumed, the mean number of patient-reported standard alcohol drinks consumed was 1.8 ± 2.4. Median and mean AUDIT scores were 1 (0, 4) and 3.0 ± 3.9, respectively. The frequency of self-reported hazardous alcohol use (AUDIT ≥8) was 12% (n=35, 95% CI 9–16). The rate of binge drinking was 15% (n=45, 95% CI 12–20). Binge drinking behavior was more common in men and in older patients, specifically, 91% of binge drinkers were men (41 men vs. 4 women, p = 0.0006) with a 10-year difference between binge drinkers and non-binge patients (60.5 ± 12.3 vs 70.0 ± 11, p < 0.001). Overall, the rate of unhealthy drinking (either hazardous or binge drinking) was 18% (n=53, 95% CI 14–23).
Table 1.
Patient characteristics of those admitted for acute cardiac illnesses and surveyed about alcohol use.
| Patient Characteristics (N = 290) | |
|---|---|
| Age, years | 68 ± 11 |
| Men | 203 (70%) |
| Body mass index (kg/m2) | 29 ± 6 |
| Spanish speaking | 12 (4%) |
| White | 253 (87%) |
| Asian | 3 (1%) |
| Black / African American | 12 (4%) |
| Hispanic / Latino | 20 (7%) |
| Native American | 1 (<1%) |
| Other | 1 (1%) |
| Hypertension | 239 (82%) |
| Hyperlipidemia | 214 (74%) |
| Type II diabetes mellitus | 135 (47%) |
| Stroke | 35 (12%) |
| Heart failure | 76 (26%) |
| Peripheral vascular disease | 26 (9%) |
| Myocardial infarction | 92 (32%) |
| Obstructive sleep apnea | 69 (24%) |
| Atrial fibrillation | 73 (25%) |
| Chronic kidney disease | 56 (19%) |
| Cirrhosis | 4 (1%) |
| Pancreatitis | 11 (4%) |
| Cancer | 40 (14%) |
| Reason for Admission* | |
| Myocardial infarction | 101 (35%) |
| Coronary artery bypass grafting | 52 (18%) |
| Percutaneous coronary intervention | 47(16%) |
| Stable angina | 3 (1%) |
| Peripheral vascular disease | 1 (<1%) |
| Chronic heart failure | 55 (19%) |
| Heart valve repair / replacement | 39 (14%) |
| Education Level (n=287) | |
| Did not graduate high school | 37 (13%) |
| Graduated high school/GED or equivalent | 108 (38%) |
| Some college, no degree | 50 (17%) |
| Associates degree | 35 (12%) |
| Bachelor’s degree | 32 (11%) |
| Advanced degree, masters | 20 (7%) |
| Doctorate | 5 (2%) |
| Income Level (n=225) | |
| <20,000 | 45 (20%) |
| 20,000 – 34,999 | 49 (21%) |
| 35,000 – 49,999 | 51 (23%) |
| 50,000 – 74,999 | 51 (23%) |
| 75,000 – 99,999 | 22 (9%) |
| >100,000 | 7 (3%) |
Data reported as either mean ± standard deviation or frequency (n, %).
More than one response was considered acceptable.
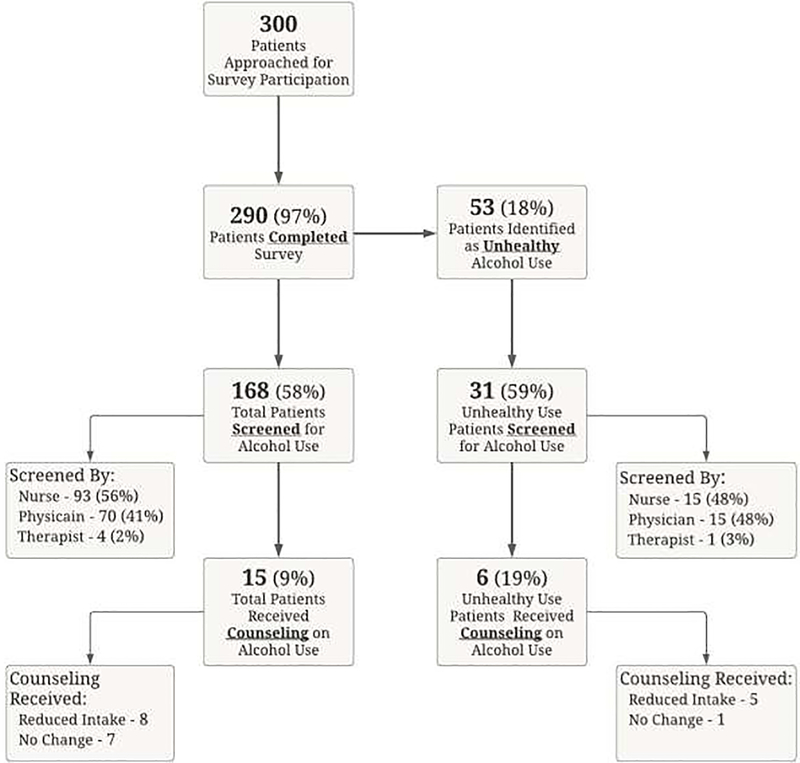
During admission, 58% of subjects reported being screened about alcohol use at any point during the hospitalization. (Figure 1.) Patients reported that nurses were the most likely to ask about alcohol use followed by physicians or therapists. On multivariable analysis, only increasing age was associated with increased alcohol screening (rate increase by 2.9% per 10-year increase, p = 0.007). Notably, there was no association between screening for alcohol use and the presence of unhealthy drinking (58% vs 59%, p = 0.92).
Figure 1.
Flow chart depicting rates of alcohol use screening and counseling of those patients surveyed, including those identified as unhealthy use behavior.
Those who were screened for alcohol use, most (91%) reported having not received any counseling on alcohol use. Of the patients that were counseled, half were counseled to reduce alcohol use. Patients were more likely to report counseling if they were screened by a doctor or nurse practitioner (16 vs 4% p = 0.013) or if they had a higher AUDIT score (χ2 = 5.1, p = 0.02).
In total, 53 patients reported unhealthy drinking, and on average consumed 5 standard alcoholic drinks per day. The average AUDIT score for these patients was 9.5. The rate of alcohol use screening in the unhealthy drinking cohort was similar to the entire group (59%), counseling was more frequent (19%, n = 6), 5 patients were counseled to reduce alcohol use, and 1 patient was told to make no change in their alcohol use. Thus, the vast majority (89%) of unhealthy drinkers reported having received no advice from a healthcare professional regarding their alcohol use while admitted to the hospital.
Finally, of those surveyed, 23 patients (8%) reported having been told by a healthcare professional, at any point in the past, that alcohol use was good for their general health. Only 12% of patients reporting having ever received a recommendation on alcohol use from their cardiologist or cardiac surgeon. Of those patients, 70% reported having received counseling to decrease their alcohol intake and 12% patients reporting counseling to increase their intake, the rest (18%) were unsure if they ever received counseling on alcohol use from their cardiologist or cardiac surgeon.
DISCUSSION
In this survey, of nearly 300 patients admitted to the hospital for a cardiac illness with an excellent response rate, we found that a sizeable fraction of patients were unhealthy drinkers, screening for alcohol use was reported by only half of patients and rates of counseling were overall very low. Nurses did most of the screening, however, most screening appears to have been fairly cursory, as many patients with unhealthy drinking were not identified in this process.
The present understanding of the relationship between alcohol use and cardiovascular disease continues to evolve, mainly with respect to issue of alcohol use in moderation.2,4,18,19 That said, the fact remains heavy alcohol consumption is cardiotoxic, even after adjustment for other risk factors.9 Additionally, the rate of binge and hazardous drinking is increasing within the general population and is associated with an increase in all-cause mortality.8,20–21 Alarmingly, we also identified a small portion of patients who had actually been counseled to increase their alcohol use, despite guidelines that clearly recommend against such advice.22
Our report is consistent with prior studies, showing that, among the general inpatient population, about 16% of patients have unhealthy alcohol consumption, as assessed by the 3-item AUDIT-C.23,24 Given this substantial prevalence, the key necessary first step in addressing unhealthy alcohol use is consistent screening. Multiple validated tools are readily accessible, including the AUDIT-C, CAGE questionnaire and the ‘single-question’ alcohol screen from National Institute on Alcohol Abuse and Alcoholism (NIAAA).5 These tools are essential parts of effective screening strategies within a variety of clinical settings.6,25 Once appropriately identified, inpatient motivational counseling may represent an effective method to address unhealthy drinking behavior, with prior research demonstrating heavy drinkers are 2 times as likely to moderate their use after such interventions.26 Implementing screening/counseling initiatives in the emergency room setting have been explored in a randomized fashion but have fallen short on achieving sustained alcohol use moderation,27 whereas a similar approach in the primary care setting found lower rates of self-reported drinking at 12-months.28 Reports on reducing excessive drinking via brief counseling interventions are plentiful, including multiple meta-analyses. Conversely, experience with integrating an approach aimed solely at screening initiatives, particularly in an inpatient cardiac population, is an area of research that is missing. More effort in needed in the realm of efficacious screening strategies, especially on admission, which should afford the ability to identify those with unhealthy alcohol use, potentially mitigating the dangerous consequences of acute alcohol withdrawal and facilitate more proactive motivational counseling, treatment, and resource referrals.
The reasons for our low screening rates are unclear but likely multifactorial. First, as a general rule screening for substance use disorders in hospitalized patients is generally poor. Second, among cardiac patients, the belief that moderate alcohol use may imparting a cardiovascular benefit may dissuade clinicians from consistently screening for harmful alcohol use. Lastly, alcohol use may be a socially difficult topic to broach, influenced by different age groups, genders, and cultural backgrounds. A simple universal approach to this at-risk group may be difficult to employ broadly and would likely be inadequate to fully address the scope and nuances of the issue.
Our report has several strengths. First, we had extremely high participation rates, with nearly 97% of patients completing the survey. This is likely the result of the anonymity provided, clarity and ease of the survey itself. The use of the AUDIT questionnaire also provided a well validated means of assessing alcohol use consumption. An important limitation of this study is that it does not comprise the totality of cardiac patients, including patients with arrhythmias, hypertension, or those with heart failure from diastolic dysfunction. That said, the eligibility for cardiac rehabilitation implies that each of these patients had a reasonable prognosis and should have been screened and counseled for harmful alcohol use. The nature of being a single-centered study means our results may not uniformly apply to other institutions with significantly different patient populations or clinical settings, although our results are generally consistent with prior studies.29,30 Because all survey answers were self-reported, it is possible that our reported rates of screening and counseling are lower than what actually happened in the hospital because some patients did not recall being screened or counseled. Similarly, it is possible that patients may have been screened for alcohol use after survey completion, however, we know that most cardiac rehabilitation evaluations actually occur in the latter half of the hospitalization, based on national estimates.13 Patients may have also given incorrect answers about their medical history, but due to the cardiac rehab staff evaluation, we know that all patients at least had active cardiac disease. Additionally, alcohol use may have been underreported by participants due to social desirability bias, however, if this bias were present to a significant extent, such a bias would underestimated the true extent of the problem and would only add to the significance of our findings.
In our study of patients hospitalized with a cardiovascular diagnosis, unhealthy alcohol use appears to be quite common. We identified significant gaps in alcohol use screening and counseling of unhealthy alcohol consumption, which is of particular concern give this level of alcohol use has been shown to increase cardiovascular mortality. This study highlights the need for more robust screening and counseling initiatives aimed at proper identification and treatment of those at risk to the deleterious effects of alcohol use when consumed in excess.
Supplementary Material
FUNDING
Dr. Quinn Pack is supported by a grant from the National Heart, Lung and Blood Institute of the National Institutes of Health of Bethesda, MD under award number 1K23HL135440, as well as by the Research Pilot Award Program from Baystate Medical Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS/DISCLOSURES
All authors report no conflicts of interest.
References
- 1.Anon. 2015–2020 Dietary Guidelines for Americans - health.gov. Available at: https://health.gov/dietaryguidelines/2015/. Accessed March 27, 2019.
- 2.Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol Consumption and Cardiovascular Mortality among U.S. Adults, 1987–2002. J Am Coll Cardiol 2010;55. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865979/. Accessed March 30, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai J, Mukamal KJ, Krasnow RE, Swan GE, Reed T. Higher usual alcohol consumption was associated with a lower 41-y mortality risk from coronary artery disease in men independent of genetic and common environmental factors: the prospective NHLBI Twin Study. Am J Clin Nutr 2015;102:31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedmann PD. Alcohol Use in Adults. N Engl J Med 2013;368:365–373. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med 2004;140:554–556. [DOI] [PubMed] [Google Scholar]
- 7.Hedden SL, Kennet J, Lipari R, Medley G, Tice P, Copello EAP, Kroutil LA. Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. 2015:74. [Google Scholar]
- 8.GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Lond Engl 2018;392:1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB. Alcohol consumption, binge drinking, and early coronary calcification: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol 2005;161:423–433. [DOI] [PubMed] [Google Scholar]
- 10.O’Keefe JH, Bybee KA, Lavie CJ. Alcohol and Cardiovascular Health: The Razor-Sharp Double-Edged Sword. J Am Coll Cardiol 2007;50:1009–1014. [DOI] [PubMed] [Google Scholar]
- 11.Malyutina S, Bobak M, Kurilovitch S, Gafarov V, Simonova G, Nikitin Y, Marmot M. Relation between heavy and binge drinking and all-cause and cardiovascular mortality in Novosibirsk, Russia: a prospective cohort study. The Lancet 2002;360:1448–1454. [DOI] [PubMed] [Google Scholar]
- 12.Kanny D, Naimi TS, Liu Y, Brewer RD. Trends in Total Binge Drinks per Adult Who Reported Binge Drinking - United States, 2011–2017. MMWR Morb Mortal Wkly Rep 2020;69:30–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pack QR, Priya A, Lagu TC, Pekow PS, Berry R, Atreya AR, Ades PA, Lindenauer PK. Cardiac Rehabilitation Utilization During an Acute Cardiac Hospitalization: A National Sample. J Cardiopulm Rehabil Prev 2019;39:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol 1995;56:423–432. [DOI] [PubMed] [Google Scholar]
- 15.McColl E. Review of Cognitive Interviewing. A Tool for Improving Questionnaire Design. Qual Life Res 2006;15:571–573. [Google Scholar]
- 16.Anon. What Is A Standard Drink? Natl Inst Alcohol Abuse Alcohol NIAAA 2011. Available at: https://www.niaaa.nih.gov/what-standard-drink. Accessed August 27, 2020.
- 17.Anon. Drinking Levels Defined. Natl Inst Alcohol Abuse Alcohol NIAAA 2011. Available at: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-bingedrinking. Accessed August 27,2020.
- 18.Hvidtfeldt UA, Tolstrup JS, Jakobsen MU, Heitmann BL, Grønbaek M, O’Reilly E, Bälter K, Goldbourt U, Hallmans G, Knekt P, Liu S, Pereira M, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Rimm EB, Ascherio A. Alcohol intake and risk of coronary heart disease in younger, middle-aged, and older adults. Circulation 2010;121:1589–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tolstrup J, Jensen MK, Tjønnel and A, Overvad K, Mukamal KJ, Grønbaek M. Prospective study of alcohol drinking patterns and coronary heart disease in women and men. BMJ 2006;332:1244–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Institute on Alcohol Abuse and Alcoholism. Apparent Per Capita Alcohol Consumption: National, State, and Regional Trends, 1977–2017. Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health 2019. Available at: https://pubs.niaaa.nih.gov/publications/surveillance113/CONS17.htm. [Google Scholar]
- 21.Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol 2017;70:913–922. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization ed. Global strategy to reduce the harmful use of alcohol. Geneva: World Health Organization; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wakeman SE, Herman G, Wilens TE, Regan S. The prevalence of unhealthy alcohol and drug use among inpatients in a general hospital. Subst Abuse 2020;41:331–339. [DOI] [PubMed] [Google Scholar]
- 24.Saitz R, Freedner N, Palfai TP, Horton NJ, Samet JH. The severity of unhealthy alcohol use in hospitalized medical patients. J Gen Intern Med 2006;21:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary Care Validation of a Single-Question Alcohol Screening Test. J Gen Intern Med 2009;24:783–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of Randomized Control Trials Addressing Brief Interventions in Heavy Alcohol Drinkers. J Gen Intern Med 1997;12:274–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Drummond C, Deluca P, Coulton S, Bland M, Cassidy P, Crawford M, Dale V, Gilvarry E, Godfrey C, Heather N, McGovern R, Myles J, Newbury-Birch D, Oyefeso A, Parrott S, Patton R,Perryman K, Phillips T, Shepherd J, Touquet R, Kaner E. The Effectiveness of Alcohol Screening and Brief Intervention in Emergency Departments: A Multicentre Pragmatic Cluster Randomized Controlled Trial. PLOS ONE 2014;9:e99463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kypri K. Randomized Controlled Trial of Web-Based Alcohol Screening and Brief Intervention in Primary Care. Arch Intern Med 2008;168:530. [DOI] [PubMed] [Google Scholar]
- 29.Smothers BA, Yahr HT, Ruhl CE. Detection of Alcohol Use Disorders in General Hospital Admissions in the United States. Arch Intern Med 2004;164:749–756. [DOI] [PubMed] [Google Scholar]
- 30.Wu S-I, Liu I, Fang C-K, Hsu C-C, Sun Y-W. Prevalence and detection of alcohol use disorders among general hospital inpatients in eastern Taiwan. Gen Hosp Psychiatry 2006;28:48–54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.