Abstract
Robotic surgery has emerged as an alternative to laparoscopic surgery and it has also been applied to pancreatectomy. With the increase in the number of robotic pancreatectomies, several studies comparing robotic pancreatectomy and conventional open or laparoscopic pancreatectomy have been published. However, the use of robotic pancreatectomy remains controversial. In this review, we aimed to provide a comprehensive overview of the current status of robotic pancreatectomy. Various aspects of robotic pancreatectomy and conventional open or laparoscopic pancreatectomy are compared, including the benefits, limitations, oncological efficacy, learning curves, and costs. Both robotic pancreatoduodenectomy and distal pancreatectomy have favorable or comparable outcomes to conventional procedures, and robotic pancreatectomy has the potential to be an alternative to open or laparoscopic procedures. However, there are still several disadvantages to robotic platforms, such as prolonged operative duration and the high cost of the procedure. These disadvantages will be improved by developing instruments, overcoming the learning curve, and increasing the number of robotic pancreatectomies. In addition, robotic pancreatectomy is still in the introductory period in most centers and should only be used in accordance with strict indications.
Keywords: robotic distal pancreatectomy, robotic pancreatectomy, robotic pancreatoduodenectomy
In this review, we aimed to provide comprehensive overview of the current status of robotic pancreatectomy.
![]()
1. INTRODUCTION
Robotic distal pancreatectomy (RDP) and robotic pancreatoduodenectomy (RPD) were first described in 2002 and 2003, respectively. 1 , 2 Several systematic reviews and cohort studies have subsequently shown that robotic pancreatectomy has better or comparable perioperative outcomes compared with conventional open or laparoscopic pancreatectomy. Therefore, in the future, robot pancreatectomy could become an alternative to conventional surgery; however, its use is still controversial. To promote a better understanding of robotic pancreatectomy, we reviewed its current status and future perspectives.
2. CURRENT TRENDS IN ROBOTIC PANCREATECTOMY
Considering the number of studies on robotic pancreatectomy, its use is gradually expanding. However, there have been few reports of its trend of use based on national databases. Recently, Hoehn et al 3 investigated the trends in robotic pancreatectomy use between 2010 and 2016 in the USA using the National Cancer Database (NCDB). During the survey period, RPD and RDP were performed in 799 and 823 cases, respectively. The annual number of cases of RPD and RDP during that period increased from 33 to 225 and from 18 to 220, respectively. In addition, the proportion of robotic pancreatectomies performed relative to conventional open or laparoscopic procedures also increased (RPD: from 2% to 7%; RDP: from 4% to 16%). The use of robotic pancreatectomy has increased; however, most centers perform a low volume of robotic surgeries (RPD: 82% of centers average < one case/year; RDP: 87% average < one case/year), while few centers perform > three cases per year (RPD: five [3%] centers; RDP: one [1%] center). Over the entire survey period, only 5% and 2% of centers performed ≥ 20 cases of RPD and RDP, respectively. These findings suggest that although robot pancreatectomy seems to be widely performed in the USA, most institutions are low‐volume centers and may still be in the introductory period for robot pancreatectomy. However, the database was focused on pancreatic ductal adenocarcinoma (PDAC) or neuroendocrine tumors, and these centers may have experience with robotic pancreatectomy for benign cases or other types of periampullary cancer.
3. ROBOTIC PANCREATODUODENECTOMY
Pancreatoduodenectomy (PD) is one of the most complex surgical procedures, and its mortality is reported to be 2.0%‐6.5%. 4 , 5 , 6 A recent systematic review of 1593 cases of RPD reported a mortality rate of 3.3% (in‐hospital mortality or 90‐day mortality). 7 Xourafas et al 8 analyzed 409 cases from the American College of Surgeons National Surgical Quality Improvement Program (ACS‐NSQIP) data and reported an overall mortality rate of 2.18%. Nassour et al 6 analyzed 626 cases of PDAC from the NCDB and reported a 90‐day mortality rate of 4.0%. Moreover, data from experienced centers have revealed 90‐day mortality rates of 2.7%‐3.1%. 9 , 10 These data suggest that the mortality rates of RPD seem to be equivalent to those of open pancreatoduodenectomy (OPD). A significant inverse relationship between hospital volume and the mortality of PD 11 and laparoscopic pancreatoduodenectomy (LPD) 12 has been reported. Although there have been no reports on the relationship between hospital volume and RPD, the relationships could be similar to those observed with OPD or LPD. Therefore, to minimize mortality in the early phase of the learning curve, RPD should be initially introduced in high‐volume hospitals. In Japan, the institutions that perform RPD are strictly limited to high‐volume PD hospitals that meet institutional criteria (Figure 1).
FIGURE 1.
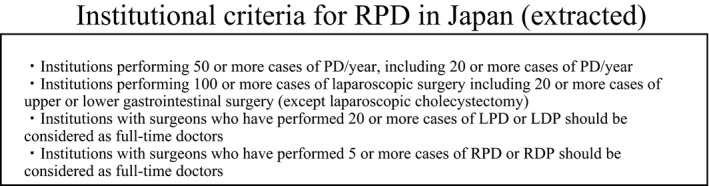
Institutional criteria for RPD in Japan (extracted)
There are limited reports regarding the learning curve of RPD. 9 , 13 , 14 , 15 Shi et al 9 investigated 450 cases of RPD and found that there were two inflection points around cases 100 and 250 that resulted in three phases of learning: phase I, case 1 to 100 (steady improvement phase); phase II, case 101 to 250 (plateau phase); and phase III, case 251 to 450 (more rapid improvement phase). The mean operative duration and estimated blood loss in phase I (378.4 ± 98.4 min and 414.5 ± 444.5 mL, respectively) decreased in phase II (305.5 ± 61.4 min and 321.8 ± 271.9 mL, respectively) and decreased further in phase III (278.2 ± 76.8 min and 213.4 ± 173.0 mL, respectively); the authors also showed that the incidence of postoperative pancreatic fistula (POPF) in the last 350 cases was significantly lower than that in the first 100 cases (30.0% vs 15.1%, P = .003). Although they concluded that the operative outcomes significantly improved after 250 cases, they acknowledged that it would be difficult to replicate their study at other centers due to the large sample size. Boone et al 13 investigated 200 consecutive cases of RPD and found two inflection points around cases 80 and 140; Zhang et al 15 investigated 100 cases and found that the flexion points were around 40 and 60 cases; and Shyr et al 14 investigated 61 cases of RPD and found that it took only 20 cases to overcome the learning curve. These findings suggest that the inflection point for operative duration is dependent on the cases investigated. In fact, in the analysis of 450 cases described above, the operative duration and blood loss decreased even when comparing the 1‐50 cases group (405.4 ± 112.9 min and 410.0 ± 563.5 mL, respectively) to the 51‐100 cases group (351.4. ± 74.5 min and 315.8 ± 264.7 mL, respectively). The operative duration decreased continuously with an increase in the surgeon's experience. To shorten the learning curve and standardize the procedure, frequent feedback with video clips and training with simulation are important.
Regarding the indication for surgery, RPD has been performed across a wide spectrum of pathologies from benign to malignant PDAC tumors, and several institutions have reported RPD for PDAC with vascular resection. 16 , 17 , 18 , 19 Therefore, there seems to be no absolute contraindication to RPD. However, Shi et al 9 contended that although malignant tumors should not be considered a contraindication for RPD, patients with large tumors or severe vascular invasion should be excluded, even in high‐volume centers. Between 2015 and 2016, a worldwide survey on the opinions of minimally invasive pancreatoduodenectomy (MIPD), including both laparoscopic and robotic procedures, was completed by 435 hepatopancreatobiliary surgeons. In the survey, the most frequently cited contraindication for MIPD was arterial tumor involvement (83%) followed by venous tumor involvement (66%) and involvement of other organs (62%). Conversely, 21% of surgeons considered PDAC to be a contraindication for MIPD. 20 Initial RPD procedures should consist of easier cases, such as non‐obese and non‐malignant cases without concomitant pancreatitis; subsequently, the selection criteria for RPD may become progressively more difficult as more experience is gained.
There have been few reports regarding RPD accompanied by vascular resection and reconstruction of the superior mesenteric/portal vein (RPD‐VR; Table 1a). 16 , 17 , 18 These reports compared RPD cases with and without vascular resection. All the reports showed that the operative duration was longer and the estimated blood loss was larger in the RPD‐VR group than in the RPD alone group. Although there was no statistically significant difference, conversion and mortality rates were higher in the RPD‐VR group (10.0%) than in the RPD alone group (3.0%‐6.8%; Table 1a). While all the reports described RPD‐VR as a safe and feasible procedure in selected patients when performed by surgeons experienced in RPD, the reported resection and reconstruction methods were heterogeneous in each center (Table 1b). Beane et al 17 analyzed the largest number of RPD‐VR cases (50 cases) and reported that most resection and reconstruction methods were partial (tangential) resection with a linear stapler or closure with suture (Table 1b). Usually, the indication for partial resection is limited to cases with portal vein invasion, and most cases with PV invasion require segmental resection with end‐to‐end anastomosis or interposition graft. There are only a few such cases analyzed to date (Table 1 b). In addition, the reported mortality rate of RPD‐VR is 8.0%‐14.3%, even in high‐volume centers where RPD‐VR was introduced after an initial experience of 50‐80 cases. 17 , 18 Considering the relatively high rates of mortality and the limited reports on RPD‐VR, the feasibility of RPD‐VR has not yet been confirmed. The indication should be carefully considered and the procedure should be performed only in experienced high‐volume center hospitals.
TABLE 1.
(a) List of studies regarding RPD with vascular resection (b) List of studies regarding RPD with vascular resection
| (a) | Number | Conversion rate | Operation time | Blood loss | 90‐day mortality | Complication (CD ≥ 3) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RPD alone | RPD‐VR | RPD alone | RPD‐VR | P | RPD alone | RPD‐VR | P | RPD alone | RPD‐VR (g) | P | RPD alone | RPD‐VR | P | RPD alone | RPD‐VR | P | |
| Kauffmann et al 16 ) | 116 | 14 | NA | NA | NA | 522 min | 641 min | <.0001 | 420 g | 1110 g | <.0001 | 1.7% | 14.3% | .060 | 17.2% | 28.6% | .290 |
| Beane et al 17 ) | 330 | 50 | 3.0% | 10.0% | .035 | 337 min | 419 min | .004 | 200 g | 275 g | .006 | 2.8% | 8.0% | .080 | 22.7% a | 28% a | .412 |
| Marino et al 18 ) | 73 | 10 | 6.8% | 10.0% | .634 | 525 min | 642 min | .003 | 290 g | 620 g | .002 | 4.1% | 10.0% | .546 | 11.0% | 40.0% | .004 |
| (b) Reconstruction method | Kauffamann et al 16 | Beane et al 17 | Marino et al 18 , a |
|---|---|---|---|
| n = 14 | n = 50 | n = 10 | |
| Tangential resection with direct closure by suture | 0 | 16 | 2 |
| Tangential resection with linear stapler | 0 | 27 | 0 |
| Tangential resection with patch | 1 | 6 | 1 |
| Segmental resection and venous‐to‐venous anastomosis | 5 | 1 | 5 |
| Interposition graft | 8 | 0 | 2 |
Abbreviations: NA, not applicable; RPD‐VR; robotic pancreatoduodenectomy with vascular resection.
Clavien‐Dindo greater than grade 2
There have been few reports regarding the cost of RPD. Baker et al 21 reported that operating charges were significantly higher in RPD than in OPD (US$50 535 vs US$32 309, P < .001); however, total inpatient charges were similar between the two groups. Kowalsky et al reported that total 30‐day costs were equivalent for OPD and RPD. These findings suggest that although the operative cost itself was higher in RPD, the shorter hospital stay and reduced complication rates may contribute to the equivalence of RPD and OPD in terms of hospital charges.
3.1. Comparison between robotic and open pancreatoduodenectomy
A recent meta‐analysis of 18 non‐randomized studies compared RPD and OPD in 13 639 patients (RPD; 1593, OPD; 12 046) 7 (Table 2 a). The analysis showed that although the operative duration was significantly longer in RPD than in OPD (461.1 ± 84 vs 384.2 ± 73.8 min, P = .0004), blood loss was significantly lower in RPD (352.1 ± 174.1 vs 588.4 ± 219.4 mL, P = .003). However, there was no significant difference between RPD and OPD in terms of mortality (3.3% vs 2.8%), POPF (17.9% vs 15.9%), delayed gastric emptying (16.8% vs 16.1%), postoperative hemorrhage (11.0% vs 14.6%), postoperative stay (13.7 ± 5.5 vs 15.9 ± 6.5 day), and reoperation and readmission rates.
TABLE 2.
(a) List of studies comparing RPD and OPD (b) List of studies comparing RPD and LPD
| (a) RPD vs OPD | Comment | Conversion | P‐value | Mortality | P‐value | Morbidity | P‐value | POPF | P‐value | Operative time | P‐value | Blood loss | P‐value | OS | P‐value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Podda et al 7 | Systematic review | 90‐day | Overall | Overall | |||||||||||
| RPD (n = 1593) | 4.7% | ‐ | 3.3% | .840 | 64.4% | .120 | 17.9% | .810 | 461 min | .000 | 352 ml | .003 | N.A | NA | |
| OPD (n = 12 046) | ‐ | 2.8% | 68.1% | 15.9% | 384 min | 588 ml | N.A | ||||||||
| Girgis et al 23 | BMI ≥ 30.0 kg/m2 | 30‐day | CD ≥ 3 | Grade B C | |||||||||||
| RPD (n = 70) | 0.0% | ‐ | 1.4% | .368 | 35.7% | 1.000 | 12.9% | .039 | 381 min | .003 | 250ml | .001 | N.A | NA | |
| OPD (n = 75) | ‐ | 5.3% | 36.0% | 28.0% | 428 min | 500ml | N.A | ||||||||
| Nassour et al 6 | National data (NCDB) | 90‐day | |||||||||||||
| RPD (n = 626) | 14.7% | ‐ | 3.8% | .061 | NA | NA | NA | NA | NA | NA | NA | NA | 22.0 M | .755 | |
| OPD (n = 17,205) | ‐ | 5.6% | NA | NA | NA | NA | 21.8 M | ||||||||
| Shyr et al 24 | Level 3 dissection | 90‐day | CD ≥ 3 | Grade B C | |||||||||||
| RPD (n = 36) | 2.9% | ‐ | 2.8% | 1.000 | 13.9% | NA | 19.4% | .082 | 576 min | .137 | 263 ml | <.001 | 85.70% | .699 | |
| OPD (n = 19) | ‐ | 0.0% | 0.0% | 0.0% | 600 min | 600 ml | 85.70% | ||||||||
| (b) RPD vs LPD | |||||||||||||||
| Kamarajah et al 25 | Systematic review | 30‐day | CD ≥ 3 | overall | |||||||||||
| RPD (n = 1025) | 12.0% | <.001 | 2.0% | .80 | 42.0% | .90 | 19.0% | .90 | 405 min | .3 | 220 ml | .1 | NA | NA | |
| LPD (n = 2437) | 26.0% | 3.0% | 41.0% | 19.0% | 418 min | 287 ml | NA | ||||||||
| Liu et al 26 ) | overall | overall | overall | ||||||||||||
| RPD (n = 27) | 0.0% | .980 | 4.0% | .98 | 29.6% | .28 | 14.3% | .89 | 387 min | .015 | 219 ml | .01 | NA | NA | |
| LPD (n = 25) | 4.0% | 0.0% | 44.0% | 20.0% | 442 min | 334 ml | NA | ||||||||
| Nassour et al 27 | National data (NCDB) | 90‐day | |||||||||||||
| RPD (n = 165) | 17.0% | 0 | 4.8% | .93 | NA | NA | NA | NA | NA | NA | NA | NA | 20.7 M | .445 | |
| LPD (n = 1,458) | 27.6% | 5.6% | NA | NA | NA | NA | 22.7 M | ||||||||
Abbreviations: OPD, open pancreatoduodenectomy; POPF, postoperative pancreatic fistula; RPD, robotic pancreatoduodenectomy; NCDB, National Cancer Database (in the USA).
Varley et al 22 recently investigated morphometric risk factors of adverse outcomes after PD. They found that low average psoas density (APD) was associated with poor postoperative outcomes and defined APD as a high‐risk morphometric feature. Postoperative outcomes (hospital stay and non‐home discharge) in patients with low APD (≤50th percentile) were improved with RPD. In obese patients (BMI ≥ 30 kg/m2), Girgis et al 23 reported that RPD was associated with significantly better perioperative outcomes than OPD in terms of operative duration (381 vs 428 min, P = .003), blood loss (250 vs 500 ml, P = .001), transfusion rates (17% vs 33%, P = .003), and pancreatic fistula (13% vs 28%, P = .039). In addition, the robotic approach remained a significant factor protecting against POPF (odds ratio [OR] 0.33, P = .019). These findings suggest that RPD is safe and feasible and may have a potential benefit, especially for high‐risk patients, compared to the open procedure.
Regarding oncological outcomes, Nassour et al 6 analyzed the data of the NCDB and reported that the number of harvested lymph nodes was higher in RPD than in OPD, and there was no significant difference in positive margin status and 30‐ or 90‐day mortality between the two groups. In addition, the median overall survival was similar between the two groups. Shyr et al 24 reported the feasibility of mesopancreatic level 3 dissection (en bloc mesopancreatic resection with right hemi‐circumferential pl‐SMA dissection). Compared with level 2 dissection, robotic level 3 dissection was safely performed with higher R0 resection rates (94.7% vs 72.2%) and without an increase in mortality or perioperative complications. Compared with OPD, level 3 dissection in RPD had favorable outcomes in terms of blood loss and chyle leakage. These findings suggest that RPD showed favorable outcomes in blood loss and comparable perioperative outcomes to OPD, including cases of PDAC.
3.2. Comparison between robotic and laparoscopic pancreatoduodenectomy
RPD is reported to be a safe and feasible alternative to OPD in selected patients. The other alternative to RPD is LPD. Therefore, the clinical question is: which procedure is superior between RPD and LPD? There are few reports comparing RPD and LPD in a single institution (Table 2 b). This is because institutions mainly perform either RPD or LPD and not both. Kamarajah et al 25 collected data from six comparative studies and showed RPD was associated with lower conversion rates (12% in RPD vs 26% in LPD, OR: 0.45, 95% confidence interval [CI]: 0.36‐0.56, P < .001), transfusion rates (10% in RPD vs 19% in LPD, OR: 0.60, 95% CI: 0.44‐0.83, P = .002), and shorter hospital stays (mean: 11 vs 12 days, P < .001); the harvested lymph nodes were larger in RPD than in LPD (mean: 13 vs 12, P < .001). They also collected 38 non‐comparative single‐arm studies of either RPD or LPD and found that although statistical analysis was not performed, conversion rates were lower in RPD (6%) than in LPD (8%). Liu et al 26 compared RPD (n = 27) and LPD (n = 25) in a single institution and found that RPD showed more favorable outcomes than LPD in terms of shorter operative time (mean 387 vs 442 min, P = .015). Although the number analyzed was small, the striking notion in this study was the shorter operative time in RPD. The authors mentioned that although additional docking time was needed in RPD, the convenience of suture and knot tying in the robotic surgical system shortened the entire operative duration.
Nassour et al 27 compared 165 cases of RPD and 1458 cases of LPD using the NCDB review from 2010 to 2013 and found that the conversion rates were less frequent in RPD than in LPD (17.0% vs 27.6%, P = .003). They also revealed no significant difference in the mean number of harvested lymph nodes (19.3% vs 17.2%, P = .081), positive margin status (17.6% vs 20.4%, P = .289), mean length of stay (11.8% vs 11.5%, P = .144), and 90‐day mortality (4.8% vs 5.6%, P = .680) between the two groups; furthermore the median overall survival for PDAC was comparable between LPD and RPD (20.7 vs 22.7 months). Recently, Ricci et al’s 28 systematic review comparing various types of minimally invasive pancreatic resections found that RPD was the best approach when considering the R0 resection and mortality ratios as outcomes of efficacy and safety, respectively. These findings suggest that RPD is a superior procedure to LPD in terms of a lower conversion rate and may be the safest approach to achieve a R0 resection.
3.3. Hybrid pancreatoduodenectomy
Hybrid PD combines the use of robots and laparoscopy wherein resection is performed laparoscopically and reconstruction is performed robotically. 29 , 30 , 31 Kim et al 31 compared 153 cases of hybrid PD and 710 cases of OPD using propensity score matching (PSM) analysis. Similar to the comparison between RPD and OPD, the operative duration was longer in hybrid PD than in OPD (361.2 ± 88.1 vs 307.7 ± 86.0 min, P < .001). However, mortality (1.3% vs 0.7%, P = .352) and overall complications (24.7% vs 26.8%, P = .670), including clinically relevant POPF (6.7% vs 6.9%, P > .999), were similar to those of OPD. Oncological outcomes, such as the number of harvested lymph nodes (17.0% vs 16.6%, P = .793), R0 resection rates (96.7% vs 93.3%, P = .527), and 2‐year overall survival (84.4% vs 77.8%, P = .898), were equivalent to those of OPD.
The robotic approach may be an alternative to the laparoscopic approach in the future. However, there are still several disadvantages to the laparoscopic approach, such as less instrument development and difficulties in positioning the patient during surgery. PD is a highly complex procedure associated with elaborate resection and reconstruction. It may be challenging to introduce pure RPD without any experience of robotic procedures. If the surgeon and institution are familiar with LPD, hybrid PD may be an optional procedure, especially in the introductory period of RPD and in challenging cases that have a high possibility of conversion during resection. 32
4. ROBOTIC DISTAL PANCREATECTOMY
The mortality rate of RDP does not appear to be high. Although Rosemury et al 33 reported a 30‐day mortality rate of 3.0% (three of 100 cases) for RDP, most single‐center analysis reports showed a 90‐day mortality rate of 0%. 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 In an analysis of a high‐volume center, Zhou et al 42 collected data on 515 cases of RDP for systematic review and found a 90‐day mortality rate of 0.19%. Weng et al 43 reported a 90‐day mortality rate of 0.5% following 219 cases of RDP. Watson et al 44 analyzed 145 cases of PDAC from a nationwide database in the USA and reported a 90‐day mortality rate of 0.9%. These data suggest that RDP was safely introduced and performed in both non‐experienced and experienced centers.
Shakir et al 45 analyzed the learning curve of RDP in 100 cases and found that the initial operative duration of 331 min decreased to 266 min and 210 min after the first 20 and 40 cases, respectively. Their analysis also showed a reduction in operative duration after the initial 10 cases. Napoli et al 46 analyzed 55 cases of RDP and showed a significant decrease in operative duration after 10 cases (421.1 min to 248.9 min). As described above, the threshold of the learning curve is dependent on the cases analyzed, and the definition is sometimes arbitrary; in addition, it also depends on each surgeon's previous experience with ODP and LDP. Considering these findings, as an international consensus suggests, 10‐20 RDP cases are needed to surpass the learning curve. 32
4.1. Robotic distal pancreatectomy vs open distal pancreatectomy
Zhou et al 47 reviewed seven retrospective studies comparing RDP and ODP with meta‐analysis and found that RDP was associated with lower estimated blood loss, lower blood transfusion rates, shorter hospital stay, and lower postoperative mortality than ODP (Table 3 a). Weng et al 43 conducted a relatively large‐scale single‐center analysis comparing 219 cases of RDP and ODP for patients with benign and low‐grade malignancy using PSM analysis. They showed that RDP had favorable outcomes in terms of operative duration (120 vs 175 min, P < .001), estimated blood loss (50 vs 200 ml, P < .001), and infection rate (4.6% vs 12.3%, P = .006). Similarly, Magge et al 36 found that the operative duration was shorter in RDP than in ODP using data from an experienced high‐volume center. However, most reports, including the analysis based on a national database, showed longer operative duration in RDP relative to ODP. 8 Thus, RDP has less blood loss and comparable or favorable perioperative outcomes to those of OPD.
TABLE 3.
(a) List of studies comparing RDP and ODP (b) List of studies comparing RDP and LDP
| Comment | Conversion | P‐value | 90‐day Mortality | P‐value | Morbidity (CD ≥ 3) | P‐value | POPF | P‐value | Operative time | P‐value | Blood loss | P‐value | Spleen preservation | P‐value | R0 ratio | P‐value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (a) RDP vs ODP | |||||||||||||||||
| Zhou et al 47 | Systematic review | 90‐day | CD ≥ 3 | Grade B C | |||||||||||||
| RDP (n = 515) | NA | ‐ | 0.2% | .030 | 15.2% | .500 | 13.8% | .220 | no difference | .580 | 247 ml less in RDP | <.001 | no difference | .170 | 0.0% | .740 | |
| ODP (n = 1,749) | ‐ | 1.4% | 23.3% | 11.4% | 90.4% | ||||||||||||
| Weng et al 43 ) | PSM for benign to LGM tumor | 90‐day | CD ≥ 3 | Grade B C | |||||||||||||
| RDP (n = 219) | 0.5% | ‐ | 0.5% | 1.00 | 4.1% | 1.00 | 14.6% | .249 | 120 min | <.001 | 50 ml | <.001 | 63.5% | <.001 | 95.4% | .445 | |
| ODP (n = 219) | ‐ | 0.5% | 3.7% | 18.7% | 175 min | 200ml | 26.5% | 97.3% | |||||||||
| (b) RDP vs LDP | |||||||||||||||||
| Kamarajah et al 48 | CD ≥ 3 | Grade B C | |||||||||||||||
| RDP (n = 793) | Systematic review | 8.0% | <.001 | N.A | NA | 12.0% | .78 | 8.0% | .29 | 28 min | <.001 | no difference | .070 | 33.0% | .220 | 95.0% | .970 |
| LDP (n = 2,319) | 21.0% | N.A | 15.0% | 8.0% | shorter in LDP | 21.0% | 89.0% | ||||||||||
| Liu et al 34 * | 90‐day | CD ≥ 3 | Grade B C | * | |||||||||||||
| RDP (n = 102) | PSM | 2.9% | .05 | 0.0% | ‐ | 4.9% | NA | 12.7% | NA | 207 min | .419 | 100 ml | .698 | 95.5% | .001 | NA | NA |
| LDP (n = 102) | 9.8% | 0.0% | 5.9% | 6.9% | 200 min | 100 ml | 52.4% | NA | |||||||||
| De et al 40 | 90‐day | CD ≥ 3 | Grade B C | ||||||||||||||
| RDP (n = 37) | PSM | 13.5% | .53 | 0.0% | ‐ | 10.8% | .308 | 27.0% | .519 | 240 min | .095 | 100 ml | .698 | NA | NA | NA | NA |
| LDP (n = 66) | 15.2% | 0.0% | 6.1% | 28.8% | 230 min | 125 ml | NA | NA | |||||||||
| Qu et al 38 * | 90‐day | CD ≥ 3 | Grade B C | ||||||||||||||
| RDP (n = 35) | PSM for PDAC | 5.7% | .040 | 0.0% | ‐ | 5.7% | NA | 0.0% | NA | 223 min | .3 | 100 ml | .120 | NA | NA | 100% | .310 |
| LDP (n = 35) | 22.9% | 0.0% | 8.6% | 2.9% | 207 min | 200 ml | NA | 97.1% | |||||||||
| Watson et al 48 ) | National data (NCDB) | 90‐day | |||||||||||||||
| RDP (n = 145) | 15.2% | .02 | 0.9% | .077 | NA | NA | NA | NA | NA | NA | NA | N.A | NA | NA | 81.4% | .403 | |
| LDP (n = 660) | 24.4% | 4.7% | NA | NA | NA | NA | NA | 83.5% | |||||||||
| Yang et al 41 | 90‐day | CD ≥ 3 | Grade B C | ||||||||||||||
| RDP (n = 37) | Spleen preservation | 2.7% | .62 | 0.0% | ‐ | 10.8% | .521 | 8.1% | .664 | 313 min | .000 | 201 ml | .443 | 91.9% | .012 | NA | NA |
| LDP (n = 41) | 7.3% | 0.0% | 17.5% | 4.9% | 246 min | 294 ml | 68.3% | NA | |||||||||
Abbreviations: LDP, laparoscopic distal pancreatectomy; LGM, low‐grade malignant; NCDB, National Cancer Database (in the USA); PSM, propensity score matching; RDP, robotic distal pancreatectomy; POPF, postoperative pancreatic fistula.
4.2. Robotic distal pancreatectomy vs laparoscopic distal pancreatectomy
Although there have been several reports comparing RDP and LDP (Table 3 b), the number of cases analyzed was relatively small. The systematic review and meta‐analysis by Kamarajah et al 48 comparing RDP (n = 793) and LDP (n = 2319) revealed that although the operative duration was significantly longer in cases of RDP (P < .001) than in cases of LDP, RDP showed favorable outcomes in conversion rates (8% vs 21%, OR: 0.48, P < .001) and hospital stay (mean: 1 days shorter in RDP, P < .001). Furthermore, there were no significant differences in the 90‐day reoperation and readmission rates or in major complications, including POPF. Recently, three retrospective analyses comparing RDP and LDP with PSM have been published (Table 3 b). 34 , 38 , 40 In one of these three reports, Liu et al 34 reported that the conversion rates were significantly lower in association with RDP than with LDP (2.9% and 9.8%, P = .045), while De et al 40 showed no significant difference. Qu et al 38 analyzed only cases of PDAC with PSM and showed significantly lower conversion rates in RDP than in LDP (5.7% and 22.9%, P = .04). Watson et al 49 analyzed the NCDB and showed the same results (15.2% in RDP vs 24.4% in LDP, P = .016). Thus, RDP is favorable in terms of lower rates of conversion to laparotomy and comparable postoperative outcomes. Yang et al 41 focused on RDP with spleen preservation and found that spleen preservation rates were higher in the RDP group than in the LDP group (91.9% vs 68.3%, P = .012). Moreover, among spleen‐preserving cases, splenic vessel preservation was significantly higher in the RDP group than in the LDP group (73.0% vs 39.0%, P = .006). Using PSM analysis, Liu et al 34 also reported significantly higher spleen and splenic vessel preservation rates in RDP than in LDP for patients with non‐malignant moderate tumors (tumor size 3‐5 cm; 95.5% vs 52.4%; P = .001, 59.1% vs 19.0%; P = .007, respectively). The splenic artery and vein have small branches that run behind the pancreas; thus, splenic vessel preservation is sometimes challenging in laparoscopic procedures. The multidirectional endo‐wrist function of the robot platform may be suitable for splenic vessel preservation.
Regarding PDAC, Watson et al’s 49 comparison of RDP (n = 145) and LDP (n = 660) using the NCDB found that RDP was associated with a higher lymph node retrieval number (15.9 vs 13.4, P = .0098) and that the R0 ratio was comparable between the two groups. Pairwise comparisons demonstrated that RDP had a higher survival rate than both LDP (P = .0183) and ODP (P = .0019), while there was no significant difference between LDP and ODP (P = .0789). Conversely, Qu et al 38 compared RDP and LDP with PSM analysis and showed no difference in overall survival. Although the report from NCDB was striking, the national cohort data were retrospective and RDP included more stage 0 cases than LDP and ODP; therefore, the data should be interpreted with caution.
Cost‐effectiveness has also been reported. Souche et al 35 found that the mean intraoperative cost was significantly higher in RDP (€7070 vs €3174, P < .001). The total 90‐day cost, including initial hospitalization and rehospitalization, remained significantly higher in cases of RDP compared to LDP (€13 611 vs €12 509, P < .001). The balance between hospital income and costs was negative in the RDP group compared to that in the LDP group (–€1269 vs €1395, P < .001), while Rodriguez et al 37 reported that the total cost, including the surgical procedure and postoperative outcomes, was highest in ODP, mainly because of prolonged hospitalization. Although the calculation of cost is difficult, surgical cost would be highest for the robotic procedure.
5. EDUCATION AND ROBOT PANCREATECTOMY
A high level of psychomotor skill is required to perform minimally invasive pancreatic resection (MIPR) safely. Thus, MIPR training is critical for the safe introduction and expansion of MIPR. 44 Accordingly, the University of Pittsburgh has designed a training system for robotic pancreatectomy. 50 The training system comprises five steps: Step 1 consists of virtual reality simulation with virtual and inanimate reality models; Step 2 includes training with inanimate bio tissue; Step 3 involves video library training; Step 4 includes an intraoperative evaluation; and Step 5 consists of skill maintenance with ongoing assessment. Step 1 includes 24 modules and trainees must master all steps before progressing to Step 2. The video library training in Step 3 is performed throughout all states of the curriculum. After the completion of each step, an improvement of outcomes was found in both steps. RPD is a complex procedure; therefore, these steps are reasonable to master handling the instrument, and the program should be disseminated and adopted by surgeons, especially those who have never performed robotic surgeries.
6. CONCLUSION
The findings of this review suggest that robotic pancreatectomy is a safe and feasible procedure. It might be an alternative to open or laparoscopic procedures in the future. However, there are still several disadvantages to robotic platforms, such as prolonged operative duration and the high cost of the procedure itself. However, the development of surgical instruments and a new robotic platform as well as an increase in the number of robotic procedures in the future will reduce its cost. In addition, robotic pancreatectomy is still in the introductory period in most centers. Surgeons should perform robotic pancreatectomy with strict indications. To date, all published studies have been retrospective analyses; RCTs comparing robotic pancreatectomy and conventional laparoscopic or open procedures should be planned in the future.
CONFLICT OF INTEREST
Dr Kohei Nakata and Dr Masafumi Nakamura have no conflicts of interest or financial ties to disclose.
DATA SHARING AND DATA ACCESSIBILITY
None.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.com) for English language editing.
Nakata K, Nakamura M. The current status and future directions of robotic pancreatectomy. Ann Gastroenterol Surg. 2021;5:467–476. 10.1002/ags3.12446
REFERENCES
- 1. Melvin WS, Needleman BJ, Krause KR, Schneider C, Wolf RK, Michler RE, et al. Computer‐enhanced robotic telesurgery. Initial experience in foregut surgery. Surg Endosc. 2002;16(12):1790–2. [DOI] [PubMed] [Google Scholar]
- 2. Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138(7):777–84. [DOI] [PubMed] [Google Scholar]
- 3. Hoehn RS, Nassour I, Adam MA, Winters S, Paniccia A, Zureikat AH. National Trends in Robotic Pancreas Surgery. J Gastrointest Surg. 2020. [DOI] [PubMed] [Google Scholar]
- 4. Hasegawa H, Takahashi A, Kakeji Y, Ueno H, Eguchi S, Endo I, et al. Surgical outcomes of gastroenterological surgery in Japan: Report of the National Clinical Database 2011–2017. Ann Gastroenterol Surg. 2019;3(4):426–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Liu Z, Peneva IS, Evison F, Sahdra S, Mirza DF, Charnley RM, et al. Ninety day mortality following pancreatoduodenectomy in England: has the optimum centre volume been identified? HPB (Oxford). 2018;20(11):1012–20. [DOI] [PubMed] [Google Scholar]
- 6. Nassour I, Winters SB, Hoehn R, Tohme S, Adam MA, Bartlett DL, et al. Long‐term oncologic outcomes of robotic and open pancreatectomy in a national cohort of pancreatic adenocarcinoma. J Surg Oncol. 2020;122(2):234–42. [DOI] [PubMed] [Google Scholar]
- 7. Podda M, Gerardi C, Di Saverio S, Marino MV, Davies RJ, Pellino G, et al. Robotic‐assisted versus open pancreaticoduodenectomy for patients with benign and malignant periampullary disease: a systematic review and meta‐analysis of short‐term outcomes. Surg Endosc. 2020;34(6):2390–409. [DOI] [PubMed] [Google Scholar]
- 8. Xourafas D, Ashley SW, Clancy TE. Comparison of Perioperative Outcomes between Open, Laparoscopic, and Robotic Distal Pancreatectomy: an Analysis of 1815 Patients from the ACS‐NSQIP Procedure‐Targeted Pancreatectomy Database. J Gastrointest Surg. 2017;21(9):1442–52. [DOI] [PubMed] [Google Scholar]
- 9. Shi Y, Wang W, Qiu W, Zhao S, Wang J, Weng Y, et al. Learning Curve From 450 Cases of Robot‐Assisted Pancreaticoduocectomy in a High‐Volume Pancreatic Center: Optimization of Operative Procedure and a Retrospective Study. Ann Surg. 2019. [DOI] [PubMed] [Google Scholar]
- 10. Zureikat AH, Beane JD, Zenati MS, Al Abbas AI, Boone BA, Moser AJ, et al. 500 Minimally Invasive Robotic Pancreatoduodenectomies: One Decade of Optimizing Performance. Ann Surg. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nakata K, Yamamoto H, Miyata H, Kakeji Y, Seto Y, Yamaue H, et al. Definition of the objective threshold of pancreatoduodenectomy with nationwide data systems. J Hepatobiliary Pancreat Sci. 2020;27(3):107–13. [DOI] [PubMed] [Google Scholar]
- 12. Kantor O, Talamonti MS, Sharpe S, Lutfi W, Winchester DJ, Roggin KK, et al. Laparoscopic pancreaticoduodenectomy for adenocarcinoma provides short‐term oncologic outcomes and long‐term overall survival rates similar to those for open pancreaticoduodenectomy. Am J Surg. 2017;213(3):512–5. [DOI] [PubMed] [Google Scholar]
- 13. Boone BA, Zenati M, Hogg ME, Steve J, Moser AJ, Bartlett DL, et al. Assessment of quality outcomes for robotic pancreaticoduodenectomy: identification of the learning curve. JAMA Surg. 2015;150(5):416–22. [DOI] [PubMed] [Google Scholar]
- 14. Shyr BU, Chen SC, Shyr YM, Wang SE. Learning curves for robotic pancreatic surgery‐from distal pancreatectomy to pancreaticoduodenectomy. Medicine (Baltimore). 2018;97(45):e13000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhang T, Zhao ZM, Gao YX, Lau WY, Liu R. The learning curve for a surgeon in robot‐assisted laparoscopic pancreaticoduodenectomy: a retrospective study in a high‐volume pancreatic center. Surg Endosc. 2019;33(9):2927–33. [DOI] [PubMed] [Google Scholar]
- 16. Kauffmann EF, Napoli N, Menonna F, Vistoli F, Amorese G, Campani D, et al. Robotic pancreatoduodenectomy with vascular resection. Langenbecks Arch Surg. 2016;401(8):1111–22. [DOI] [PubMed] [Google Scholar]
- 17. Beane JD, Zenati M, Hamad A, Hogg ME, Zeh HJ 3rd, Zureikat AH. Robotic pancreatoduodenectomy with vascular resection: Outcomes and learning curve. Surgery. 2019;166(1):8–14. [DOI] [PubMed] [Google Scholar]
- 18. Marino MV, Giovinazzo F, Podda M, Gomez Ruiz M, Gomez Fleitas M, Pisanu A, et al. Robotic‐assisted pancreaticoduodenectomy with vascular resection. Description of the surgical technique and analysis of early outcomes. Surg Oncol. 2020;35:344–50. [DOI] [PubMed] [Google Scholar]
- 19. Shyr BU, Chen SC, Shyr YM, Wang SE. Surgical, survival, and oncological outcomes after vascular resection in robotic and open pancreaticoduodenectomy. Surg Endosc. 2020;34(1):377–83. [DOI] [PubMed] [Google Scholar]
- 20. van Hilst J, de Rooij T, Abu Hilal M, Asbun HJ, Barkun J, Boggi U, et al. Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB (Oxford). 2017;19(3):190–204. [DOI] [PubMed] [Google Scholar]
- 21. Baker EH, Ross SW, Seshadri R, Swan RZ, Iannitti DA, Vrochides D, et al. Robotic pancreaticoduodenectomy: comparison of complications and cost to the open approach. Int J Med Robot. 2016;12(3):554–60. [DOI] [PubMed] [Google Scholar]
- 22. Varley PR, Zenati MS, Klobuka A, Tobler J, Hamad A, Hogg ME, et al. Does robotic pancreaticoduodenectomy improve outcomes in patients with high risk morphometric features compared to the open approach. HPB (Oxford). 2019;21(6):695–701. [DOI] [PubMed] [Google Scholar]
- 23. Girgis MD, Zenati MS, Steve J, Bartlett DL, Zureikat A, Zeh HJ, et al. Robotic approach mitigates perioperative morbidity in obese patients following pancreaticoduodenectomy. HPB (Oxford). 2017;19(2):93–8. [DOI] [PubMed] [Google Scholar]
- 24. Shyr BU, Shyr BS, Chen SC, Shyr YM, Wang SE. Mesopancreas level 3 dissection in robotic pancreaticoduodenectomy. Surgery. 2020;169(2):362–8. [DOI] [PubMed] [Google Scholar]
- 25. Kamarajah SK, Bundred J, Marc OS, Jiao LR, Manas D, Abu Hilal M, et al. Robotic versus conventional laparoscopic pancreaticoduodenectomy a systematic review and meta‐analysis. Eur J Surg Oncol. 2020;46(1):6–14. [DOI] [PubMed] [Google Scholar]
- 26. Liu R, Zhang T, Zhao Z‐M, Tan X‐L, Zhao G‐D, Zhang X, et al. The surgical outcomes of robot‐assisted laparoscopic pancreaticoduodenectomy versus laparoscopic pancreaticoduodenectomy for periampullary neoplasms: a comparative study of a single center. Surg Endosc. 2017;31(6):2380–6. [DOI] [PubMed] [Google Scholar]
- 27. Nassour I, Choti MA, Porembka MR, Yopp AC, Wang SC, Polanco PM. Robotic‐assisted versus laparoscopic pancreaticoduodenectomy: oncological outcomes. Surg Endosc. 2018;32(6):2907–13. [DOI] [PubMed] [Google Scholar]
- 28. Ricci C, Casadei R, Taffurelli G, Pacilio CA, Ricciardiello M, Minni F. Minimally Invasive Pancreaticoduodenectomy: What is the Best "Choice"? A Systematic Review and Network Meta‐analysis of Non‐randomized Comparative Studies. World J Surg. 2018;42(3):788–805. [DOI] [PubMed] [Google Scholar]
- 29. Walsh RM, Chalikonda S. How I Do It: Hybrid Laparoscopic and Robotic Pancreaticoduodenectomy. J Gastrointest Surg. 2016;20(9):1650–7. [DOI] [PubMed] [Google Scholar]
- 30. Xu DB, Zhao ZM, Xu Y, Liu R. Hybrid pancreatoduodenectomy in laparoscopic and robotic surgery: a single‐center experience in China. Surg Endosc. 2020. [DOI] [PubMed] [Google Scholar]
- 31. Kim HS, Kim H, Kwon W, Han Y, Byun Y, Kang JS, et al. Perioperative and oncologic outcome of robot‐assisted minimally invasive (hybrid laparoscopic and robotic) pancreatoduodenectomy: based on pancreatic fistula risk score and cancer/staging matched comparison with open pancreatoduodenectomy. Surg Endosc. 2020. [DOI] [PubMed] [Google Scholar]
- 32. Liu R, Wakabayashi GO, Palanivelu C, Tsung A, Yang K, Goh BKP, et al. International consensus statement on robotic pancreatic surgery. Hepatobiliary Surg Nutr. 2019;8(4):345–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rosemurgy AS, Luberice K, Krill E, Castro M, Espineira GR, Sucandy I, et al. 100 Robotic Distal Pancreatectomies: The Future at Hand. Am Surg. 2020;86(8):958–64. [DOI] [PubMed] [Google Scholar]
- 34. Liu R, Liu Q, Zhao ZM, Tan XL, Gao YX, Zhao GD. Robotic versus laparoscopic distal pancreatectomy: A propensity score‐matched study. J Surg Oncol. 2017;116(4):461–9. [DOI] [PubMed] [Google Scholar]
- 35. Souche R, Herrero A, Bourel G, Chauvat J, Pirlet I, Guillon F, et al. Robotic versus laparoscopic distal pancreatectomy: a French prospective single‐center experience and cost‐effectiveness analysis. Surg Endosc. 2018;32(8):3562–9. [DOI] [PubMed] [Google Scholar]
- 36. Magge DR, Zenati MS, Hamad A, Rieser C, Zureikat AH, Zeh HJ, et al. Comprehensive comparative analysis of cost‐effectiveness and perioperative outcomes between open, laparoscopic, and robotic distal pancreatectomy. HPB (Oxford). 2018;20(12):1172–80. [DOI] [PubMed] [Google Scholar]
- 37. Rodriguez M, Memeo R, Leon P, Panaro F, Tzedakis S, Perotto O, et al. Which method of distal pancreatectomy is cost‐effective among open, laparoscopic, or robotic surgery? Hepatobiliary Surg Nutr. 2018;7(5):345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Qu L, Zhiming Z, Xianglong T, Yuanxing G, Yong XU, Rong L, et al. Short‐ and mid‐term outcomes of robotic versus laparoscopic distal pancreatosplenectomy for pancreatic ductal adenocarcinoma: A retrospective propensity score‐matched study. Int J Surg. 2018;55:81–6. [DOI] [PubMed] [Google Scholar]
- 39. Hong S, Song KB, Madkhali AA, Hwang K, Yoo D, Lee JW, et al. Robotic versus laparoscopic distal pancreatectomy for left‐sided pancreatic tumors: a single surgeon's experience of 228 consecutive cases. Surg Endosc. 2020;34(6):2465–73. [DOI] [PubMed] [Google Scholar]
- 40. De Pastena M, Esposito A, Paiella S, Surci N, Montagnini G, Marchegiani G, et al. Cost‐effectiveness and quality of life analysis of laparoscopic and robotic distal pancreatectomy: a propensity score‐matched study. Surg Endosc. 2020. [DOI] [PubMed] [Google Scholar]
- 41. Yang SJ, Hwang HK, Kang CM, Lee WJ. Revisiting the potential advantage of robotic surgical system in spleen‐preserving distal pancreatectomy over conventional laparoscopic approach. Ann Transl Med. 2020;8(5):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhou J, Xiong L, Miao X, Liu J, Zou H, Wen Y. Outcome of robot‐assisted pancreaticoduodenectomy during initial learning curve versus laparotomy. Sci Rep. 2020;10(1):9621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Weng Y, Jin J, Huo Z, Shi Y, Jiang YU, Deng X, et al. Robotic‐assisted versus open distal pancreatectomy for benign and low‐grade malignant pancreatic tumors: a propensity score‐matched study. Surg Endosc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Vining CC, Hogg ME. How to train and evaluate minimally invasive pancreas surgery. J Surg Oncol. 2020;122(1):41–8. [DOI] [PubMed] [Google Scholar]
- 45. Shakir M, Boone BA, Polanco PM, Zenati MS, Hogg ME, Tsung A, et al. The learning curve for robotic distal pancreatectomy: an analysis of outcomes of the first 100 consecutive cases at a high‐volume pancreatic centre. HPB (Oxford). 2015;17(7):580–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Napoli N, Kauffmann EF, Perrone VG, Miccoli M, Brozzetti S, Boggi U. The learning curve in robotic distal pancreatectomy. Updates Surg. 2015;67(3):257–64. [DOI] [PubMed] [Google Scholar]
- 47. Zhou J, Lv Z, Zou H, Xiong LI, Liu Z, Chen W, et al. Up‐to‐date comparison of robotic‐assisted versus open distal pancreatectomy: A PRISMA‐compliant meta‐analysis. Medicine (Baltimore). 2020;99(23):e20435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kamarajah SK, Sutandi N, Robinson SR, French JJ, White SA. Robotic versus conventional laparoscopic distal pancreatic resection: a systematic review and meta‐analysis. HPB (Oxford). 2019;21(9):1107–18. [DOI] [PubMed] [Google Scholar]
- 49. Watson MD, Baimas‐George MR, Thompson KJ, Iannitti DA, Ocuin LM, Baker EH, et al. Improved oncologic outcomes for minimally invasive left pancreatectomy: Propensity‐score matched analysis of the National Cancer Database. J Surg Oncol. 2020;122(7):1383–1392. [DOI] [PubMed] [Google Scholar]
- 50. Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, et al. The Miami International Evidence‐based Guidelines on Minimally Invasive Pancreas Resection. Ann Surg. 2020;271(1):1–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None.


