Abstract
Arthrodesis of the first metatarsophalangeal (MTP) joint has been established as the “gold standard” for the treatment of several first ray disorders, due to its perceived efficacy and the consistently reported good results in the literature. Arthrodesis is a commonly performed procedure for the treatment of end stage arthritis, rheumatoid arthritis with severe deformity, selected cases of severe hallux valgus (with or without signs of degenerative joint disease), as well as a salvage procedure after failed previous operation of the first ray. The goals of a successful 1st MTP arthrodesis are pain alleviation and deformity correction in order to restore a comfortable gait pattern and to improve shoe wear. Several techniques have been reported with several proposals regarding the preparation of the articular surfaces and the method of definitive fixation. As with any given surgical procedure, various complications may occur after arthrodesis of the 1st MTP joint, namely delayed union, nonunion, malunion, irritating hardware, etc.
Keywords: First metatarsophalangeal joint arthrodesis, Indications, Surgical techniques, Complications
Core Tip: Disorders of the first ray are quite common in foot and ankle surgery, as multiple pathologies can lead to degeneration and may cause stiffness to the first metatarsophalangeal (MTP) joint. If non-operative treatment fails, arthrodesis of the first MTP joint is a well-established surgical option which has demonstrated very satisfactory results. Herein, we examine the various indications for this procedure, and the different surgical techniques, regarding joint preparation and fixation constructs, that we have at our disposal in order to obtain optimum results.
INTRODUCTION
The first metatarsophalangeal (MTP) joint consists of the convex articular surface of the first metatarsal head, articulating with the corresponding elliptic, swallow, and concave base of the proximal phalanx of the first toe. The plantar articular surface of the first metatarsal head is unique, as it bears two well defined facets which are separated by an anteroposteriorly oriented central crest. The facets accommodate the tibial and fibular sesamoid bones, encased in each tendon of the flexor hallucis brevis. The joint is enclosed by a fibrous capsule that attaches close to the articular margins and extends more proximally at the plantar surface. The ligamentous complex which stabilizes the joint is composed by a collateral ligament on each side of the metatarsal, and a plantar and deep transverse transmetatarsal ligament. Blood supply comes from the first dorsal and plantar arteries of the medial digital branches, while innervation is from the medial plantar nerve, the medial dorsal cutaneous nerve and the terminal branch of the deep peroneal nerve[1].
The first MTP joint allows for flexion – extension, limited abduction and adduction and some degree of longitudinal rotation. Based on the literature, the joint has a total passive range of motion (ROM) of approximately 110°, which is the sum of 35° of plantar flexion and 75° of dorsiflexion[2,3]. However, the active ROM, even in healthy individuals, is reduced. During ambulation the first MTP joint is slightly dorsiflexed in most of the stance phase, whereas in late stance phase the joint reaches a peak of 50° to 60° of dorsiflexion and remains at a range of 30° to 40° of dorsiflexion during swing phase[4]. In various pathology, such as hallux rigidus, significant kinematic changes are noticed as a result of uncoupling of the normal center of rotation between the proximal phalanx and the metatarsal head[5].
INDICATIONS
Arthrodesis of the first MTP joint is a commonly performed procedure for the treatment of end stage arthritis (Hallux rigidus stage III and IV). Surgical treatment is usually indicated in symptomatic patients with arthritis who have failed to respond to conservative management including activity modifications, over the counter medication, intra-articular corticosteroid injections, accommodative footwear, special orthotics and other symptomatic measures. Other proposed treatments for treating severe hallux rigidus include total joint replacement, hemi arthroplasty, resection arthroplasty and interposition arthroplasty. All these interventions though, have not yield the same high efficacy and functional results which have established arthrodesis as the gold standard in the treatment of this pathology. Arthrodesis demonstrates significantly better outcomes in terms of pain alleviation and functional satisfaction, as well as lower revision rates, lower complication rates and faster return to normal activity[6].
First MTP joint arthrodesis should also be considered as the treatment of choice in other severe pathology affecting the Hallux such as rheumatoid arthritis (RA), gout and post traumatic arthritis[7]. It is further considered in selected cases of severe hallux valgus (with or without signs of degenerative joint disease), with rather increased intermetatarsal and hallux valgus angle, concomitant medial column instability, transfer metatarsalgia or in elderly[8].
Arthrodesis of the 1st MTP joint has also been widely proposed as a salvage procedure after failed procedures of the first ray, including failed previous osteotomies for hallux valgus correction resulting in recurrent deformity, iatrogenic hallux varus or avascular necrosis, as well as salvage after failed resectional and replacement arthroplasties or failed cheilectomy[9-12]. First MTP arthrodesis is also indicated in hallux valgus secondary to neuromuscular disorders, in primary hallux varus, in arthritis secondary to infection and in rigid plantarflexion deformities[13-15].
Relative contraindications regarding the use of arthrodesis of the first MTP joint include the early stages of hallux rigidus (stages I and II), where joint-preserving osteotomies are preferable. Absolute contraindications are the presence of compromised soft tissues, infection, rigid scar tissue formation with direct adhesion of the skin to the bone or the presence of chronic ulcers, where the other alternatives including amputation of the great toe should be considered as a preferable treatment option.
EPIDEMIOLOGY, SYMPTOMS, CLINICAL AND RADIOLOGIC EVALUATION
The first MTP joint is considered the most common arthritic site in the foot. This condition affects nearly 10% of adults; however, radiographic evidence of arthritic changes may be present in 20% to 48% of adults older than 40 years old[16,17]. Hallux rigidus is frequently bilateral, and more than half of the patients report a family history of this specific pathology[18]. Symptomatic arthritis of the first MTP joint is characterized by debilitating pain, reduced range of motion, especially dorsiflexion, and disability to perform activities such as running, stairs climbing, and push-ups. The gait mechanics is altered, as the patients attempt to offload the hallux overloading the lateral column. Compression neuritis of the dorsomedial cutaneous nerve and discomfort with certain types of shoe wear are common problems due to the presence of prominent dorsomedial osteophytes[19].
Several inflammatory joint diseases such as RA, widely affect the forefoot. Pain caused by synovitis or arthritis of the first MTP joint is often the initial symptom and it has been reported that within the first 3 years of the onset of rheumatoid arthritis, approximately 65% of the patients have some degree of MTP joint involvement. It is estimated that more than 60% of the patients with chronic involvement will develop a severe hallux valgus deformity and/or subluxation and dislocation of the lesser MTP joints. Therefore, 5%-22% of these patients will require some type of surgical treatment[20-22].
The foot must be evaluated in both seated and standing positions. The seated position facilitates ROM assessment, while the standing position provides more information regarding the dynamic alignment and function of the hallux. In the presence of arthritis, the joint is tender dorsally, with often present palpable osteophytes, limited ROM with less than 10° of dorsiflexion in severe cases, while pain is elicited even in midrange of passive motion.
Radiographic evaluation of hallux rigidus requiring arthrodesis (grade 3 and 4) consists of standard standing anteroposterior, and lateral foot radiographs. Substantial joint space narrowing, flattening and widening of the metatarsal head, formation of periarticular dorsal, lateral and even medial osteophytes both proximally and distally at the joint, irregular or enlarged sesamoids and subchondral sclerosis are the most common and significant findings[18].
Hallux valgus deformity requiring a first MTP arthrodesis is usually characterized by severe HV and IM angle (more than 40 and 20 degrees, respectively) and secondary degenerative changes of the first MTP joint[8,23].
SURGICAL TECHNIQUES
The goals of a successful first MTP arthrodesis are pain alleviation and deformity correction in order to restore a comfortable gait pattern and to improve shoe wear. Several techniques have been reported in the literature with several proposals regarding the preparation of the articular surfaces and the method of definitive fixation.
The most commonly used surgical incision is the dorsal longitudinal which is centered over the first MTP joint, but a medial incision has also been utilized as a safe alternative in the presence of severe scarring in the dorsal aspect of the Hallux. This later approach has the disadvantage of not facilitating supplementary dorsal plating, but the surgeon should wisely balance the strength of fixation and the maximum potential of soft tissue healing. Dissection should always be meticulous, taking care to elevate full thickness flaps with adequate mobilization of the extensor hallucis longus (EHL) tendon and protection of the neurovascular bundles[24].
There are a few recent reports of endoscopic lateral release of the first MTP joint and subsequent arthroscopic arthrodesis in selected groups of patients. The selection criteria reported in those studies were severe hallux valgus deformity, degenerative and rheumatoid arthritis, adequate bone quality and no signs of transfer metatarsalgia. Lateral release of the adductor hallucis tendon and the lateral capsule-ligamentous complex of the 1st MTP joint are performed through a toe web and a plantar portal in order to convert the deformity into a more flexible one. Adequate release facilitates the arthroscopic removal of the cartilage, the microfractures to the fusion surfaces and the definitive fixation with 2 crossed cannulated screws[25,26].
Spherical cup-and-cone articular surface preparation techniques are currently the most widely used, whereas peg and socket techniques as well as utilization of planar cuts have also been thoroughly reported in the literature. Cup and cone techniques utilizing cannulated reamers are relatively easy by a technical point of view and rather reproducible. Such techniques provide a significant surface contact area thus enhancing the potential for bone healing by means of fusion and allow for easy intraoperative positioning in all planes. Finally, they offer greater stability, minimizing the potential bone loss and the potential shortening, which are commonly encountered in other preparation techniques, and have been shown to be biomechanically superior when fixation is applied in comparison to the other preparation techniques[27]. Peg and socket techniques have the advantage of providing inherent stability, but they may cause shortening, significant bone loss and are technically demanding[28,29]. Planar cuts have the advantage of being quick and technically easy, but they may also lead to significant shortening and bone loss, mainly in cases where repositioning is required[30].
Stable internal fixation with compression across the fusion site has been established as the standard of care regarding the most preferable fixation technique. Several reports have proposed the sole use of plates, single or two lag screw constructs with variations of either cannulated or solid as well as crossed or parallel, and more often a combination of plates and screws. More recently, the use of memory compression or pure titanium staples has also been described[31-35]. Biomechanical studies comparing several fixation techniques have demonstrated that a dorsal plate in combination with a lag screw across the fusion site have been proven to provide the most stable fixation constructs comparing to those provided with a single plate, sole lag screws, staples or (K)-wire fixation[36,37].
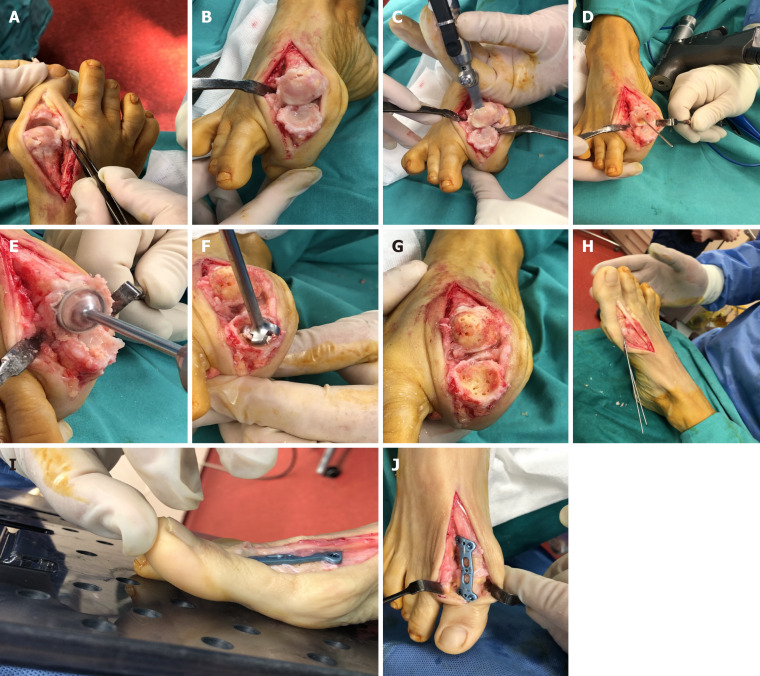
For the last 20 years, the authors routinely utilize a dorsal midline approach (Figure 1A), in order to gain adequate access to the joint and ease the positioning of the arthrodesis as well as the placement of the implants. The joint capsule is divided longitudinally just medial to the EHL; the tendon is then retracted laterally and the collateral ligaments and the capsule are reflected from the 1st metatarsal head (Figure 1B). The joint surfaces are being prepared in a standard fashion. Initially, all dorsal osteophytes as well as a part of the medial eminence are removed, and a minimal flat cut is made to the head of the 1st metatarsal with the use of an oscillating saw (Figure 1C). This preliminary partial cartilage or sclerotic subchondral bone removal facilitates subsequent reaming over a guidewire which is inserted to the center of the 1st metatarsal head (Figure 1D). Hemispherical cup and cone reamers are used in order to remove the articular surfaces and create concentric concave and convex surfaces of bleeding subchondral bone (Figure 1E and F). Reaming should be done on full speed in a gentle, concentric tapping motion to avoid excessive bony resection and metatarsal shortening. The prepared surfaces are then perforated multiple times with a K-wire in order to promote fusion (Figure 1G). These two surfaces are then provisionally reduced and fixed with two K-wires in the considered optimum position (Figure 1H). The sagittal alignment is being checked intraoperatively both by C-ARM guidance and by using a flat tray simulating weight bearing. Therefore, the 1st MTP joint is positioned in a way that allows the pulp of the great toe to rest 5-10 mm above the flat surface with simulated weight bearing (Figure 1I). Valgus alignment is set to 10 degrees, rotation is kept to neutral and final checks are made to ensure that the dorsiflexion angle is within the range of 15 to 20 degrees. Any remaining dorsal prominences are then removed to allow proper seating of the plate. A pre-contoured titanium low profile neutralization plate is applied dorsally (Figure 1J), with at least four locking titanium screws and the fixation is additionally secured with an interfragmentary compression screw placed in a distal-inferomedial to proximal-superolateral direction to achieve compression across the MTP joint. The provisional K wires are removed and the position of the hallux is again checked both fluoroscopically and clinically. Any minor local defects are filled with bone graft taken from the reamers and the wound is closed in layers. Gauges and compression bandage is applied. The patients are allowed to fully weight bear immediately in a heel wedged velcro shoe for six to eight weeks.
Figure 1.
Surgical technique. A: A dorsal midline approach provides adequate access to the joint; B: Extensor hallucis longus tendon is laterally retracted and adequate collateral ligament and capsule reflection provides excellent working space; C: A minimal flat cut is made to the head of the 1st metatarsal utilizing an oscillating saw; D: A guidewire is inserted to the center of the 1st metatarsal head; E and F: Hemispherical cup and cone reamers are used in order to remove the articular surfaces; G: Concave and convex surfaces of bleeding subchondral bone have been prepared with multiple perforations; H: Provisional fixation with two K- wires in the considered optimum position; I: The sagittal alignment is being checked intraoperatively using a flat tray simulating weight bearing. The 1st metatarsophalangeal joint is positioned in a way that allows the pulp of the great toe to rest 5-10 mm above the flat surface; J: Final position of the plate.
In the setting of severe osseous defects, commonly encountered after failed previous hallux surgery, the main goal is to restore the normal length of the first ray, thus avoiding the overload of the lesser metatarsal heads which could lead to transfer metatarsalgia. Therefore, any remaining defects are filled with either autologous bone graft or bone substitutes. In cases of minor defects, these may be filled with cancellous bone taken from either the calcaneus, or the distal/proximal tibial metaphysis. Larger defects are usually filled with structural corticocancellous grafts taken from the anterior iliac crest.
COMPLICATIONS
As with any given surgical procedure, various complications may occur from a first MTP arthrodesis, namely delayed union, nonunion, malunion, wound dehiscence, seroma, infection, osteomyelitis, hallux ischemia, nerve damage, hematoma, failed or prominent and irritating hardware, and hallux interphalangeal joint arthritis[38-40].
In an effort to investigate the incidence of these complications, Roukis et al[40] performed a retrospective review of 2818 feet from 37 studies and reported an average nonunion rate of 5.4%, regardless of the reported fixation technique with just 32.7% of them being symptomatic. Average malunion rate was found to be 6.1%, while the incidence of symptomatic hardware necessitating removal was 8.5%, regardless the type of fixation being used[40]. These figures roughly represent 50% of those that had been previously reported in the literature, regarding the incidence of malunion, nonunion and hardware removal after arthrodesis of the first MTP joint[30,39,41].
A rather common metabolic pathology that may complicate the outcome is diabetes mellitus. Anderson et al[42] reported that although first MTP arthrodesis is overall an effective and beneficial procedure in patients with diabetes mellitus, those with peripheral neuropathy have an increased risk for mild and moderate complications. 35.5% of the study’s diabetic patients had one or more mild to moderate complications but only a small number of those required revision surgery. 68% of the study’s diabetic patients with peripheral neuropathy had one or more mild to moderate complications (wound dehiscence, infection, delayed or no bone healing). This is significantly higher than the results of non-diabetic patients who had approximately 10% of complications[42].
The most commonly reported complications, namely malunion and nonunion, usually occur due to inadequate surgical technique and/or poor patient’s compliance. Positioning of the hallux is of paramount importance in order to obtain proper foot function and optimal shoe fit. Malunion can occur in one or more of the sagittal, frontal, and transverse planes. Sagittal plane malposition, especially excessive dorsiflexion is poorly tolerated by the patient due to increased plantar pressure at the 1st MTP joint and concomitant abutment of the hallux against the shoe wear, whereas excessive plantarflexion significantly increases pressure on the big toe during heel off. Malrotation may also represent a problem as it causes painful callosities as well as painful nail deformities. Finally, malunion in the transverse plane, namely varus malposition, usually causes painful abutment of the medial aspect of the hallux against the shoe.
The main three factors leading to nonunion are: inadequate joint preparation, mechanical failure of the fixation construct being used and lack of patient’s compliance. Risk factors leading to nonunion break down into 2 categories, the surgeon-dependent and patient-dependent. Thus, it is of paramount importance to the surgeon to select the preparation technique and fixation method which is familiar with, as well as to select those patients with factors predisposing for a successful outcome.
DISCUSSION
Arthrodesis of the first MTP joint has been established as the “gold standard” for the treatment of several first ray disorders, due to its perceived efficacy along with the consistently reported good results in the literature. Several studies (Level II evidence) have compared arthrodesis with hemiarthroplasty and Keller resection arthroplasty of the first MTP joint. Arthrodesis consistently demonstrated equivalent or superior results with lower complication rate. The procedure alleviates pain, and maintains stability and alignment of the first ray, thus providing better functional outcomes, lower revision rates, reduced hospital stay, as well as faster return to normal activity[43,44].
Despite the fact that first MTP joint arthrodesis has been established as a reliable treatment option for several disorders of the first ray, there is no evidence based documentation of its potential superiority, comparing to other interventions, when it is applied to any given pathological entity. Desmarchelier et al[45] compared the functional outcomes and the complications rate in two groups of patients who had been treated for hallux valgus deformity with either a Scarf osteotomy or a first MTP joint arthrodesis. The authors reported that there was no statistically significant difference in the complications rate and the postoperative pain level (AOFAS score: 35.6 ± 6.5 in the Scarf group and 34.5 ± 5.9 in the MTP arthrodesis group) between the two groups. The overall satisfaction rate was similar to the Scarf and the MTP arthrodesis groups, with 91.4% vs 90% of very satisfied or satisfied patients respectively, but when the authors utilized more function specific evaluation tools such as SF 36-a general quality of life score-, the Foot Function Index, and the Foot and Ankle Ability Measure[42], they found a statistically significant difference favoring MTP arthrodesis[45]. The issues arising from the later report are those of a study that was solely based on a postoperative questionnaire with no pre-operative scores available, as well as that the leading pathologies in the two groups were not completely similar.
Hyer et al[46] investigated the fusion rate and time interval to fusion in two groups of patients with either hallux rigidus or rheumatoid arthritis who received a first MTP joint arthrodesis as a definitive procedure. In a total of 155 first MTP fusions, 116 (74.83%) had been performed for the treatment of hallux rigidus and 39 (25.16%) for rheumatoid arthritis. The overall fusion rate was 89% in the hallux rigidus group and 94% in the rheumatoid arthritis group, but the difference was not statistically significant different. There was also no statistically significant difference in the clinical outcome. Finally, the time interval to fusion was statistically significantly shorter in the rheumatoid arthritis group comparing to the hallux rigidus group (93 and 113 d, respectively)[46]. It should be noted though, that a number of intraoperative technical variables such as the method of joint preparation, the use of autologous bone marrow aspiration, as well as the use of any concomitant surgery were not taken into account.
First MTP joint arthrodesis has been established as an open procedure, but there are recent proposals of percutaneous as well as arthroscopic approaches. The increased interest in arthroscopy along with the evolution of modern techniques and instrumentation have led a few surgeons to perform an arthroscopically assisted arthrodesis of the 1st MTP joint for the treatment of hallux rigidus and other pathology of the first MTP joint. Although the later approach is often proposed during the last decade it is rarely performed, thus there is a lack of adequate evidence demonstrating its efficacy. The reason for the lack of increased number of reports is clearly the technical complexity and the steep learning curve of such a procedure, requiring additional training and more refined instrumentation. The most common complication encountered with this technique is failure to achieve fusion[26,47,48]. The recent invasion of minimally invasive surgery (MIS) techniques, with small incisions and reduced soft tissue dissection compared to open surgery, rely on the theoretical advantages of reduced wound healing complications, smaller scars, faster recovery and reduced infection rate. The current literature reporting on the safety and effectiveness of minimally invasive arthrodesis remains scarce and its potential advantages over open surgery are still a matter of debate. Therefore, more prospective studies are required providing adequate level of evidence of any potential benefit of MIS comparing to standard 1st MTP arthrodesis[49,50].
A literature review of the several proposed joint preparation methods, demonstrates that the use of cup and cone technique provides biomechanically superior results comparing to those obtained by other techniques. Curtis et al[27] in a biomechanical study, reported that the cup and cone joint preparation provided statistically significant greater stiffness than planar cuts excision. The authors also noticed that the method of fixation was less important than the joint preparation technique[27]. Flavin et al[34] concluded that the combination of the cup and cone joint preparation technique with the use of a dorsal contoured plate provided the best operative results with lower complications rate. Brodsky et al[51] in a prospective gait analysis study, reported that there was statistically significant increased stability on the involved foot, better weight bearing function and increased ankle push-off power when arthrodesis had been achieved with cup and cone reamers. Singh et al[52] conducted a cadaveric study in an effort to evaluate the incidence of transfer metatarsalgia related to the amount of bone shortening after various joint preparation techniques. The authors reported that, despite the presumed superiority of the cup and cone technique, the post-procedure length of the first ray was similar in both cup and cone as well as flat cut techniques. The issue arising from this study is that there was no consistent method of measurement of the exact amount of cartilage and subchondral bone removed utilizing each technique, thus the results might not be completely accurate[52].
There are multiple reports of first MTP joint arthrodesis with a variety of fixation techniques. A significant number of retrospective clinical as well as biomechanical studies favor the use of a dorsal precontoured plate in combination with an interfragmentary lag screw over the other reported methods of fixation. This later type of fixation has been proved to be an efficient and reproducible method to achieve proper alignment of the Hallux, high fusion rate as well as safer postoperative mobilization. Politi et al[37] performed a biomechanical study comparing the strength of fixation of five commonly utilized techniques in first MTP joint arthrodesis. They used saw bone models applying dorsiflexion force across the fused joint thus simulating the forces produced during the gait cycle. According to their results the combination of a dorsal plate with an oblique lag screw provided the best results followed by a sole lag screw fixation while the use of a single dorsal plate or Kirschner wire fixation, provided the weakest constructs[37]. The use of 2 crossed screws, although a commonly reported method of fixation, was not assessed in this study. This later method was tested in a different biomechanical study, which demonstrated that a single intramedullary screw fixation was stronger and stiffer thus biomechanically superior comparing to two crossed screws fixation[36]. In a cadaveric study, constructs provided by either a small six hole plate with an interfragmentary screw or by two crossed lag screws were stressed to failure by using a computer-integrated materials tester. The plate and lag screw fixation construct provided statistically significant greater stiffness and ultimate load to failure[53]. Despite the aforementioned results, the fixation methods of either a single lag screw, 2 crossed cannulated screws or titanium staples are still in use, as there are several studies demonstrating similar rates and time to fusion comparing to those with the plate and lag screw construct. Moreover, the use of these two fixation methods are regarded to be significantly more cost effective in achieving fusion of the first MTP joint, with a lower rate of additional surgery for hardware removal[31,32,35].
CONCLUSION
First MTP joint arthrodesis is a very useful and a highly effective procedure for a variety of disorders of the first ray, with a relative low rate of complications. An ideal arthrodesis should be properly positioned, easily reproduced and demonstrate an excellent functional outcome. Factors affecting the success of this type of surgery include careful selection of patients relying on individuals’ profile, meticulous surgical technique, and adequate postoperative rehabilitation regime.
Footnotes
Conflict-of-interest statement: Nothing to disclose.
Manuscript source: Invited manuscript
Peer-review started: February 14, 2021
First decision: April 6, 2021
Article in press: July 12, 2021
Specialty type: Orthopedics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu P, Sergi C S-Editor: Wang JL L-Editor: A P-Editor: Wang LL
Contributor Information
Panagiotis Koutsouradis, Department of Foot and Ankle Reconstructive Surgery, Mediterraneo Hospital, Athens 16675, Greece. panoskouts85@gmail.com.
Olga D Savvidou, First Department of Orthopedic Surgery, National and Kapodistrian University of Athens, “ATTIKON” Hospital, Athens 12462, Greece.
Emmanouil D Stamatis, Department of Foot and Ankle Reconstructive Surgery, Mediterraneo Hospital, Athens 16675, Greece.
References
- 1.Coughlin MJ, Saltzman CL, Anderson RB. Mann's surgery of the foot and ankle. Maryland Heights: Mosby, 2014. [Google Scholar]
- 2.Buell T, Green DR, Risser J. Measurement of the first metatarsophalangeal joint range of motion. J Am Podiatr Med Assoc . 1988;78:439–448. doi: 10.7547/87507315-78-9-439. [DOI] [PubMed] [Google Scholar]
- 3.Shereff MJ, Bejjani FJ, Kummer FJ. Kinematics of the first metatarsophalangeal joint. J Bone Joint Surg Am . 1986;68:392–398. [PubMed] [Google Scholar]
- 4.Rajczy RM, McDonald PR, Shapiro HS, Boc SF. First metatarsophalangeal joint arthrodesis. Clin Podiatr Med Surg . 2012;29:41–49. doi: 10.1016/j.cpm.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Botek G, Anderson MA. Etiology, pathophysiology, and staging of hallux rigidus. Clin Podiatr Med Surg . 2011;28:229–243, vii. doi: 10.1016/j.cpm.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 6.McNeil DS, Baumhauer JF, Glazebrook MA. Evidence-based analysis of the efficacy for operative treatment of hallux rigidus. Foot Ankle Int . 2013;34:15–32. doi: 10.1177/1071100712460220. [DOI] [PubMed] [Google Scholar]
- 7.Mann RA, Oates JC. Arthrodesis of the first metatarsophalangeal joint. Foot Ankle . 1980;1:159–166. doi: 10.1177/107110078000100305. [DOI] [PubMed] [Google Scholar]
- 8.Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: intermediate results. Foot Ankle Int . 2005;26:783–792. doi: 10.1177/107110070502601001. [DOI] [PubMed] [Google Scholar]
- 9.Machacek F Jr, Easley ME, Gruber F, Ritschl P, Trnka HJ. Salvage of a failed Keller resection arthroplasty. J Bone Joint Surg Am . 2004;86:1131–1138. doi: 10.2106/00004623-200406000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Myerson MS, Miller SD, Henderson MR, Saxby T. Staged arthrodesis for salvage of the septic hallux metatarsophalangeal joint. Clin Orthop Relat Res . 1994:174–181. [PubMed] [Google Scholar]
- 11.Myerson MS, Schon LC, McGuigan FX, Oznur A. Result of arthrodesis of the hallux metatarsophalangeal joint using bone graft for restoration of length. Foot Ankle Int . 2000;21:297–306. doi: 10.1177/107110070002100405. [DOI] [PubMed] [Google Scholar]
- 12.Schuh R, Trnka HJ. First metatarsophalangeal arthrodesis for severe bone loss. Foot Ankle Clin . 2011;16:13–20. doi: 10.1016/j.fcl.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 13.Robinson AH, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br . 2005;87:1038–1045. doi: 10.1302/0301-620X.87B8.16467. [DOI] [PubMed] [Google Scholar]
- 14.Rammelt S, Zwipp H. Reconstructive Surgery after Compartment Syndrome of the Lower Leg and Foot. Eur J Trauma Emerg Surg . 2008;34:237. doi: 10.1007/s00068-008-7163-4. [DOI] [PubMed] [Google Scholar]
- 15.Wu KK. First metatarsophalangeal fusion in the salvage of failed hallux abducto valgus operations. J Foot Ankle Surg . 1994;33:383–395. [PubMed] [Google Scholar]
- 16.Roddy E, Thomas MJ, Marshall M, Rathod T, Myers H, Menz HB, Thomas E, Peat G. The population prevalence of symptomatic radiographic foot osteoarthritis in community-dwelling older adults: cross-sectional findings from the clinical assessment study of the foot. Ann Rheum Dis . 2015;74:156–163. doi: 10.1136/annrheumdis-2013-203804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilder FV, Barrett JP, Farina EJ. The association of radiographic foot osteoarthritis and radiographic osteoarthritis at other sites. Osteoarthritis Cartilage . 2005;13:211–215. doi: 10.1016/j.joca.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 18.Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am . 2003;85:2072–2088. [PubMed] [Google Scholar]
- 19.Keiserman LS, Sammarco VJ, Sammarco GJ. Surgical treatment of the hallux rigidus. Foot Ankle Clin . 2005;10:75–96. doi: 10.1016/j.fcl.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Coughlin MJ. Rheumatoid forefoot reconstruction. A long-term follow-up study. J Bone Joint Surg Am . 2000;82:322–341. [PubMed] [Google Scholar]
- 21.Matricali GA, Boonen A, Verduyckt J, Taelman V, Verschueren P, Sileghem A, Corluy L, Westhovens R. The presence of forefoot problems and the role of surgery in patients with rheumatoid arthritis. Ann Rheum Dis . 2006;65:1254–1255. doi: 10.1136/ard.2005.050823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van der Leeden M, Steultjens MP, Ursum J, Dahmen R, Roorda LD, Schaardenburg DV, Dekker J. Prevalence and course of forefoot impairments and walking disability in the first eight years of rheumatoid arthritis. Arthritis Rheum . 2008;59:1596–1602. doi: 10.1002/art.24188. [DOI] [PubMed] [Google Scholar]
- 23.Tourné Y, Saragaglia D, Zattara A, Maire JP, Picard F, Montbarbon E, Charbel A. Hallux valgus in the elderly: metatarsophalangeal arthrodesis of the first ray. Foot Ankle Int . 1997;18:195–198. doi: 10.1177/107110079701800402. [DOI] [PubMed] [Google Scholar]
- 24.Rammelt S, Panzner I, Mittlmeier T. Metatarsophalangeal Joint Fusion: Why and How? Foot Ankle Clin . 2015;20:465–477. doi: 10.1016/j.fcl.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Lui TH. Arthroscopic First Metatarsophalangeal Arthrodesis for Repair of Fixed Hallux Varus Deformity. J Foot Ankle Surg . 2015;54:1127–1131. doi: 10.1053/j.jfas.2015.06.027. [DOI] [PubMed] [Google Scholar]
- 26.Lui TH. Arthroscopic Arthrodesis of the First Metatarsophalangeal Joint in Hallux Valgus Deformity. Arthrosc Tech . 2017;6:e1481–e1487. doi: 10.1016/j.eats.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Curtis MJ, Myerson M, Jinnah RH, Cox QG, Alexander I. Arthrodesis of the first metatarsophalangeal joint: a biomechanical study of internal fixation techniques. Foot Ankle . 1993;14:395–399. doi: 10.1177/107110079301400705. [DOI] [PubMed] [Google Scholar]
- 28.Humbert JL, Bourbonnière C, Laurin CA. Metatarsophalangeal fusion for hallux valgus: indications and effect on the first metatarsal ray. Can Med Assoc J . 1979;120:937–941, 956. [PMC free article] [PubMed] [Google Scholar]
- 29.Moynihan FJ. Arthrodesis of the metatarso-phalangeal joint of the great toe. J Bone Joint Surg Br . 1967;49:544–551. [PubMed] [Google Scholar]
- 30.Coughlin MJ. Arthrodesis of the first metatarsophalangeal joint with mini-fragment plate fixation. Orthopedics . 1990;13:1037–1044. doi: 10.3928/0147-7447-19900901-16. [DOI] [PubMed] [Google Scholar]
- 31.Asif M, Qasim SN, Kannan S, Bhatia M. A Consecutive Case Series of 166 First Metatarsophalangeal Joint Fusions Using a Combination of Cup and Cone Reamers and Crossed Cannulated Screws. J Foot Ankle Surg . 2018;57:462–465. doi: 10.1053/j.jfas.2017.10.026. [DOI] [PubMed] [Google Scholar]
- 32.Besse JL, Chouteau J, Laptoiu D. Arthrodesis of the first metatarsophalangeal joint with ball and cup reamers and osteosynthesis with pure titanium staples Radiological evaluation of a continuous series of 54 cases. Foot Ankle Surg . 2010;16:32–37. doi: 10.1016/j.fas.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 33.Choudhary RK, Theruvil B, Taylor GR. First metatarsophalangeal joint arthrodesis: a new technique of internal fixation by using memory compression staples. J Foot Ankle Surg . 2004;43:312–317. doi: 10.1053/j.jfas.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 34.Flavin R, Stephens MM. Arthrodesis of the first metatarsophalangeal joint using a dorsal titanium contoured plate. Foot Ankle Int . 2004;25:783–787. doi: 10.1177/107110070402501105. [DOI] [PubMed] [Google Scholar]
- 35.Wassink S, van den Oever M. Arthrodesis of the first metatarsophalangeal joint using a single screw: retrospective analysis of 109 feet. J Foot Ankle Surg . 2009;48:653–661. doi: 10.1053/j.jfas.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 36.Molloy S, Burkhart BG, Jasper LE, Solan MC, Campbell JT, Belkoff SM. Biomechanical comparison of two fixation methods for first metatarsophalangeal joint arthrodesis. Foot Ankle Int . 2003;24:169–171. doi: 10.1177/107110070302400212. [DOI] [PubMed] [Google Scholar]
- 37.Politi J, John H, Njus G, Bennett GL, Kay DB. First metatarsal-phalangeal joint arthrodesis: a biomechanical assessment of stability. Foot Ankle Int . 2003;24:332–337. doi: 10.1177/107110070302400405. [DOI] [PubMed] [Google Scholar]
- 38.Beertema W, Draijer WF, van Os JJ, Pilot P. A retrospective analysis of surgical treatment in patients with symptomatic hallux rigidus: long-term follow-up. J Foot Ankle Surg . 2006;45:244–251. doi: 10.1053/j.jfas.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 39.Beeson P. The surgical treatment of hallux limitus/rigidus: a critical review of the literature. Foot . 2004;14:6–22. [Google Scholar]
- 40.Roukis TS. Nonunion after arthrodesis of the first metatarsal-phalangeal joint: a systematic review. J Foot Ankle Surg . 2011;50:710–713. doi: 10.1053/j.jfas.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 41.Yee G, Lau J. Current concepts review: hallux rigidus. Foot Ankle Int . 2008;29:637–646. doi: 10.3113/FAI.2008.0637. [DOI] [PubMed] [Google Scholar]
- 42.Anderson JJ, Hansen M, Rowe GP, Swayzee Z. Complication rates in diabetics with first metatarsophalangeal joint arthrodesis. Diabet Foot Ankle . 2014;5 doi: 10.3402/dfa.v5.24649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc . 2002;92:102–108. doi: 10.7547/87507315-92-2-102. [DOI] [PubMed] [Google Scholar]
- 44.Raikin SM, Ahmad J, Pour AE, Abidi N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J Bone Joint Surg Am . 2007;89:1979–1985. doi: 10.2106/JBJS.F.01385. [DOI] [PubMed] [Google Scholar]
- 45.Desmarchelier R, Besse JL, Fessy MH French Association of Foot Surgery (AFCP) Scarf osteotomy versus metatarsophalangeal arthrodesis in forefoot first ray disorders: comparison of functional outcomes. Orthop Traumatol Surg Res . 2012;98:S77–S84. doi: 10.1016/j.otsr.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 46.Hyer CF, Morrow S. Successful arthrodesis of the first metatarsophalangeal joint in patients with inflammatory and noninflammatory arthritis: a comparative analysis. J Foot Ankle Surg . 2014;53:291–294. doi: 10.1053/j.jfas.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 47.Stroud CC. Arthroscopic arthrodesis of the ankle, subtalar, and first metatarsophalangeal joint. Foot Ankle Clin . 2002;7:135–146. doi: 10.1016/s1083-7515(02)00003-7. [DOI] [PubMed] [Google Scholar]
- 48.Vaseenon T, Phisitkul P. Arthroscopic debridement for first metatarsophalangeal joint arthrodesis with a 2- versus 3-portal technique: a cadaveric study. Arthroscopy . 2010;26:1363–1367. doi: 10.1016/j.arthro.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 49.Bauer T. Percutaneous First Metatarsophalangeal Joint Fusion. Open Orthop J . 2017;11:724–731. doi: 10.2174/1874325001711010724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hodel S, Viehöfer A, Wirth S. Minimally invasive arthrodesis of the first metatarsophalangeal joint: A systematic literature review. Foot Ankle Surg . 2020;26:601–606. doi: 10.1016/j.fas.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 51.Brodsky JW, Baum BS, Pollo FE, Mehta H. Prospective gait analysis in patients with first metatarsophalangeal joint arthrodesis for hallux rigidus. Foot Ankle Int . 2007;28:162–165. doi: 10.3113/FAI.2007.0162. [DOI] [PubMed] [Google Scholar]
- 52.Singh B, Draeger R, Del Gaizo DJ, Parekh SG. Changes in length of the first ray with two different first MTP fusion techniques: a cadaveric study. Foot Ankle Int . 2008;29:722–725. doi: 10.3113/FAI.2008.0722. [DOI] [PubMed] [Google Scholar]
- 53.Buranosky DJ, Taylor DT, Sage RA, Sartori M, Patwardhan A, Phelan M, Lam AT. First metatarsophalangeal joint arthrodesis: quantitative mechanical testing of six-hole dorsal plate versus crossed screw fixation in cadaveric specimens. J Foot Ankle Surg . 2001;40:208–213. doi: 10.1016/s1067-2516(01)80020-x. [DOI] [PubMed] [Google Scholar]