Abstract
A 54-year-old male patient applied to our clinic with a sudden and painless loss of vision in his right eye. He was suffering from COVID-19. His best-corrected visual acuity of the right eye was finger counting from 30 cm. The fundus examination revealed the presence of a ‘cherry-red spot’ appearance in the right eye. In optical coherence tomography imaging, hyper-reflectivity was observed in the inner retinal layers as well as increased retinal thickness in the right eye. In fundus fluorescein angiography, delayed arterial filling and prolonged arteriovenous transit time were observed in the right eye. The patient was diagnosed with central retinal artery occlusion after the COVID-19 infection. In this study, we report this case and its management.
Keywords: retina, macula
Background
The ongoing COVID-19 pandemic has been caused by SARS-CoV-2 associated with inflammation-induced multiorgan involvement and haemostatic changes, thereby leading to severe coagulopathy.1 These vascular pathologies cause arterial thrombosis, venous thromboembolic events and local microthrombosis.2 However, the effects of the inflammatory and procoagulant status of COVID-19 on the retinal vascular system are currently unknown. In this study, we report a case of central retinal artery occlusion (CRAO) after SARS-CoV-2 infection.
Case presentation
A 54-year-old male patient applied to the emergency department with complaints of fever, anosmia and dry cough for 1 day. On admission, SARS-CoV-2 infection was concluded to be positive through the PCR molecular test in nasopharyngeal samples, leading to a diagnosis of COVID-19. Hospitalisation was not required. As such, he started using hydroxychloroquine, azithromycin, favipiravir and anticoagulant enoxaparin therapy. Three weeks after the onset of the COVID-19 symptoms, he arrived at our clinic at 4:00 with a sudden and painless loss of vision in his right eye. On the ocular examination, the best-corrected visual acuity (BCVA) of the right eye was finger counting from 30 cm and 20/20 on the left eye according to the Snellen chart. Further, the relative afferent pupillary defect was detected in his right eye (Marcus Gunn pupilla). The biomicroscopic examination was normal and intraocular pressure (IOP) was within the normal range for both eyes. The fundus examination revealed the presence of a ‘cherry-red spot’ in the right eye due to mild ischaemic retinal oedema. The left eye appeared normal.
Investigations
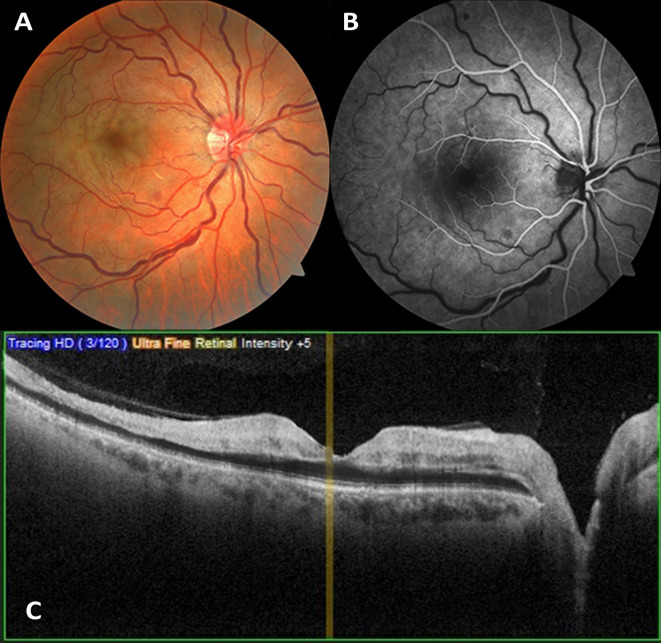
Fundus photographs were taken (figure 1A). In the fundus fluorescein angiography (FFA) (Topcon, Japan), delayed arterial filling and prolonged arteriovenous transit time were observed in the right eye (figure 1B). Additionally, hyper-reflectivity on the inner retinal layers and increased retinal thickness in the right eye (337 mm on the right and 286 mm on the left) were observed through the macular optical coherence tomography (OCT) imaging (Nidek RS-3000, Gamagori, Japan). The reflectivity was decreased at the outer retinal layers (figure 1C). The patient was diagnosed with CRAO. He was suffering from COVID-19 and did not have any chronic systemic diseases. The patient’s COVID-19 reverse transcriptase PCR test was positive; the D-dimer level was 1041 ng/ml (normal range: 80–630 ng/mL); the C reactive protein level was 128.29 mg/L (normal range: 0–5 mg/L); the ferritin level was 458.53 ng/ml (normal range: 21–274 ng/mL); the platelet count was 486×109/L (normal range: 150–450×109/L) and the fibrinogen level was 405.1 g/L (normal range: 180–400 g/L). Furthermore, the MRI did not reveal any findings related to an acute ischaemic event. In the carotid Doppler USG, no vascular pathological findings were found. All these tests were performed in another hospital before he arrived at our clinic.
Figure 1.
(A) In fundus photography, the temporal side of the retina appears white as a result of cloudy swelling caused by oedema; as the central fovea is devoid of nerve fibre and ganglion cell layers, its orange reflex stands out, causing the ‘cherry-red spot’ appearance (since the photo was taken 2 hours after the onset of the patient’s complaints, the cherry-red spot appearance was not completely formed). (B) In fundus fluorescein angiography, delayed arterial filling and prolonged arteriovenous transit time were observed in the right eye. (C) In optical coherence tomography imaging, hyper-reflectivity at inner retinal layers increased macular thickness and decreased reflectivity in the outer retinal layers were observed.
Treatment
After diagnosis, we started immediate treatment for the patient, according to previously reported studies and guidelines.3 We primarily administered an intravenous injection of 20% mannitol and performed an anterior chamber paracentesis on his right eye. Subsequently, we started administering a topical brimonidine drop and dorzolamide/timolol combination drops two times per day; moxifloxacin/dexamethasone combination drops four times a day; 125 mg of acetazolamide orally once a day and 100 mg of acetylsalicylic acid orally once a day. The patient was referred to another centre for hyperbaric oxygen therapy on the same day.
Outcome and follow-up
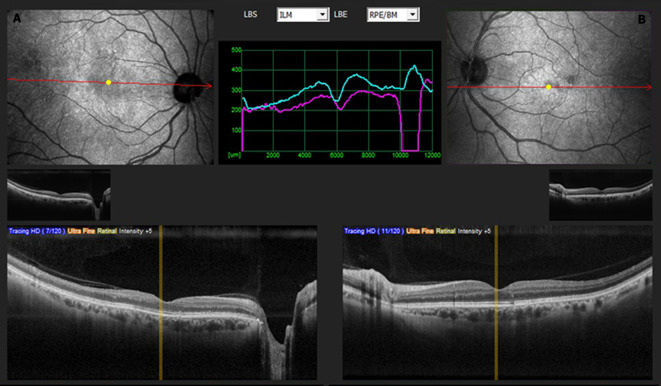
After 3 months, the patient’s BCVA improved to 12/20 (Snellen chart). The fundus examination revealed that retinal oedema and the ‘cherry-red spot’ image had disappeared. The OCT imaging demonstrated a decrease in the reflectivity and thickness of the inner retinal layers and localised atrophy of the neurosensory retina (figure 2).
Figure 2.
The optical coherence tomography image of the patient after 3 months. (A) In the right eye, a decrease in the reflectivity and thickness of the inner retinal layers and localised atrophy of the neurosensory retina were observed. (B) The left eye had a normal appearance.
Discussion
It has been reported that COVID-19 is frequently associated with high coagulation and thromboembolic events in addition to causing extracorporeal thrombosis, deep vein thrombosis and pulmonary emboli.1 4–6 The postmortem analysis presented the direct viral infection of endothelial cells, diffuse endothelial inflammation leading to endothelial dysfunction and, consequently, a procoagulant state.7 Despite the lack of predisposing factors, COVID-19 pneumonia has been detected as an aggravating factor in acute venous thromboembolism.8 Moreover, although patients are affected by venous thromboembolism in most cases, there are increasing reports of arterial thromboembolic complications from COVID-19, which highlights the thrombogenicity of the SARS-CoV-2 infection.9
Arterial thrombus leading to stroke and the acute coronary syndrome is related to antiphospholipid immunoglobulin, increased thrombocyte activity, D-dimer level and fibrinogen level.2 In our patient as well, the fibrinogen level, D-dimer level and platelet count were high. In addition, our patient had some non-arterial predisposing factors such as male gender and smoking. All these arterial and non-arterial risk factors, fundus examination findings, FFA and OCT images and all examination results confirm that the diagnosis of CRAO is most likely associated with COVID-19.1 2 10
It has been reported that the thrombotic vascular endothelial microenvironment caused by COVID-19 may be an accelerating factor that leads to the development of CRAO.10 To the best of our knowledge, only three retinal artery occlusions associated with COVID-19 have been reported (table 1).10–12 The range of ages of patients shown in table 1 is 54–60 (average 55.3 years old) for all male patients. While two patients had hypertension, one patient had only obesity and our patient had no underlying disease. The period from onset of COVID-19 to diagnosis of CRAO was between 2 weeks and 2 months. While pneumonia developed in two patients, acute respiratory failure and septic shock developed in one patient and there was no systemic involvement in our patient. All patients used hydroxychloroquine and all patients, except our patient, used tocilizumab. The visual symptoms in all patients were sudden and painless vision loss. An intensive ophthalmological treatment was applied only in our case due to early diagnosis. In the fundus examination at presentation, all patients had mild-to-significant retinal whitening. The final visual acuity improved from light perception to counting fingers in only one case except our case.
Table 1.
The summary of reported cases associated with COVID-19 and central retinal artery occlusion (CRAO)
| Case reports | Age/sex | Underlying diseases | Period from onset of COVID-19 to diagnosis of CRAO | Clinical features of COVID-19 | Treatment of COVID-19 | Visual symptoms | Ophthalmological treatment | Fundus examination at presentation and final | Visual acuity at presentation and final | Assessment |
| Montesel et al10 | 59 years old, male | Hypertension Hyperuricemia |
2 months | Pneumonia Renal failure |
Hydroxychloroquine Lopinavir/ritonavir Tocilizumab Broad-spectrum antibiotics |
Painless vision loss | N/A | At presentation: Severe arterial narrowing and retinal whitening in the macular region with loss of the physiological macular reflex Final: The loss of the foveal depression and ganglion cell layer atrophy |
LP-CF | Most likely |
| Dumitrascu et al12 | 48 years old, male | Obesity | In the sixth week of patient’s hospitalisation | Acute respiratory failure Septic shock Fungemia |
Apixaban Hydroxychloroquine Tocilizumab Enoxaparin |
Sudden and painless loss of vision | N/A | At presentation: Mild optic disc oedema, retinal whitening consistent with retinal oedema and mildly attenuated retinal vessels Final: N/A |
No LP—N/A | Most likely |
| Acharya et al11 | 60 years old, male | Hypertension Stable coronary artery disease Chronic obstructive pulmonary disease |
In the second week of patient’s hospitalisation | Pneumonia Cytokine release syndrome |
Hydroxychloroquine Azithromycin Tocilizumab |
Painless vision loss | N/A | At presentation: Optic nerve had slightly indistinct margins and a cherry-red spot with significant retinal whitening Final: N/A |
No LP—N/A | Most likely |
| Current report | 54 years old, male | None | 3 weeks | None | Hydroxychloroquine Azithromycin Favipiravir Enoxaparin |
Sudden and painless loss of vision | Intravenous 20% mannitol Anterior chamber paracentesis Acetazolamide Hyperbaric oxygen therapy |
At presentation: Cherry-red spot appearance with mild retinal whitening Final: Localised atrophy of the neurosensory retina and decrease in the reflectivity and thickness of the inner retinal layers |
CF—12/20 | Most likely |
CF, counting fingers; LP, light perception; N/A, not applicable.
In the first report,11 CRAO appeared in the second week of the patient’s hospitalisation, 3 days after discharge from the intensive care unit (ICU). In the second case,12 CRAO occurred in the sixth week of hospitalisation while the patient was under apixaban anticoagulant therapy. In the third report,10 CRAO was diagnosed 2 months after the onset of COVID-19 symptoms. Unlike other cases, ours did not have a history of hospitalisation or ICU stay. In addition, CRAO developed 3 weeks after the onset of COVID-19 symptoms in our case, which was shorter than the other two cases.10 12
In our patient, we quickly reduced the IOP with the help of medical therapy, followed by performing an anterior chamber paracentesis. Subsequently, we referred him to another centre for hyperbaric oxygen therapy. After 3 months, the patient’s BCVA in the right eye reached 12/20 (Snellen Scale). Unlike the other three reported cases, visual acuity improved significantly in our case after an early diagnosis and urgent treatment. This report shows that, in patients who develop sudden vision loss after COVID-19, CRAO should definitely be considered and immediate treatment should be started for good visual outcomes. Additionally, anticoagulation with different agents has not been shown to be an effective treatment of CRAO.3
Marinho et al13 observed that 12 patients aged between 25 and 69 years presented hyper-reflective lesions at the ganglion cell and inner plexiform layers in the papillomacular region as revealed via OCT imaging after COVID-19. Additionally, in four patients, cotton-wool spots and microhaemorrhages were observed in the retina. Furthermore, visual acuities and pupillary reflexes were normal in all patients, with no inflammatory findings. As such, the retinal lesions related to COVID-19 seem to be a part of a generalised ischaemic microvascular process.14 Zago Filho et al15 also reported a case of COVID-19 -related ocular inflammation (uveitis) and outer retinal abnormalities. Casagrande et al16 showed that the viral RNA of SARS-CoV-2 could be detected in the retina of patients with COVID-19. Therefore, new clinical features of this pathology in the eye and, more specifically, in the retina are likely to emerge soon.
In conclusion, the effects of COVID-19 and the associated inflammatory and procoagulant state on the retinal vascular system are still under investigation.17 18 Therefore, further research should be conducted on this subject and care should be taken regarding retinal vascular diseases, intraocular inflammation and ophthalmological emergencies in patients with COVID-19.
Patient’s perspective.
I experienced a sudden visual loss in my right eye 3 weeks after the diagnosis of COVID-19. I was very anxious about whether my vision loss would be permanent. After the operation and the treatment, my visual acuity has increased again, and I can see better now.
Learning points.
The effects of the inflammatory and procoagulant status of COVID-19 on the retinal vascular system are currently under investigation. Additionally, COVID-19 can cause ophthalmological emergencies such central retinal artery occlusion (CRAO).
In patients who develop sudden vision loss after COVID-19, CRAO should definitely be considered a differential diagnosis.
The immediate treatment in patients with CRAO is very critical in terms of final visual acuity.
Footnotes
Contributors: Both authors contributed to the study conception, design, material preparation, data collection and analysis, commented on previous versions of the manuscript and read and approved the final manuscript. The first draft of the manuscript was written by FU.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
The patient signed an informed written consent form before the operation.
Ethics approval
This study was approved by Institutional Review Board (Konyagoz Eye Hospital, 2021/3).
References
- 1.Levi M, Thachil J, Iba T, et al. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol 2020;7:e438–40. 10.1016/S2352-3026(20)30145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iba T, Levy JH, Levi M, et al. Coagulopathy of coronavirus disease 2019. Crit Care Med 2020;48:1358–64. 10.1097/CCM.0000000000004458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chronopoulos A, Schutz JS. Central retinal artery occlusion-A new, provisional treatment approach. Surv Ophthalmol 2019;64:443–51. 10.1016/j.survophthal.2019.01.011 [DOI] [PubMed] [Google Scholar]
- 4.Miesbach W, Makris M. COVID-19: coagulopathy, risk of thrombosis, and the rationale for anticoagulation. Clin Appl Thromb Hemost 2020;26:1076029620938149:107602962093814. 10.1177/1076029620938149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood 2020;135:2033–40. 10.1182/blood.2020006000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020;382:e38. 10.1056/NEJMc2007575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417–8. 10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danzi GB, Loffi M, Galeazzi G. And COVID-19 pneumonia: a random association? Eur Heart J 2020;41:1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levolger S, Bokkers RPH, Wille J, et al. Arterial thrombotic complications in COVID-19 patients. J Vasc Surg Cases Innov Tech 2020;6:454–9. 10.1016/j.jvscit.2020.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montesel A, Bucolo C, Mouvet V. Case report: central retinal artery occlusion in a COVID-19 patient. Front Pharmacol 2020;23:588384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Acharya S, Diamond M, Anwar S, et al. Unique case of central retinal artery occlusion secondary to COVID-19 disease. IDCases 2020;21:e00867. 10.1016/j.idcr.2020.e00867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dumitrascu OM, Volod O, Bose S, et al. Acute ophthalmic artery occlusion in a COVID-19 patient on apixaban. J Stroke Cerebrovasc Dis 2020;29:104982–4. 10.1016/j.jstrokecerebrovasdis.2020.104982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marinho PM, Marcos AAA, Romano AC, et al. Retinal findings in patients with COVID-19. Lancet 2020;395:1610. 10.1016/S0140-6736(20)31014-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duh EJ. Seeking clarity on retinal findings in patients with COVID-19. Lancet 2020;396:e39. 10.1016/S0140-6736(20)31913-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zago Filho LA, Lima LH, Melo GB, et al. Vitritis and outer retinal abnormalities in a patient with COVID-19. Ocul Immunol Inflamm 2020;28:1298–300. 10.1080/09273948.2020.1821898 [DOI] [PubMed] [Google Scholar]
- 16.Casagrande M, Fitzek A, Püschel K, et al. Detection of SARS-CoV-2 in human retinal biopsies of deceased COVID-19 patients. Ocul Immunol Inflamm 2020;28:721–5. 10.1080/09273948.2020.1770301 [DOI] [PubMed] [Google Scholar]
- 17.Aşıkgarip N, Temel E, Hızmalı L, et al. Retinal vessel diameter changes in COVID-19 infected patients. Ocul Immunol Inflamm 2021;26:1–7. 10.1080/09273948.2020.1853783 [DOI] [PubMed] [Google Scholar]
- 18.Invernizzi A, Torre A, Parrulli S, et al. Retinal findings in patients with COVID-19: results from the SERPICO-19 study. EClinicalMedicine 2020;27:100550. 10.1016/j.eclinm.2020.100550 [DOI] [PMC free article] [PubMed] [Google Scholar]