Abstract
We report a case of a 46-year-old woman who presented with a midline neck mass 2 years after total thyroidectomy for Graves’ disease. Despite levothyroxine treatment withdrawal, she remained biochemically with subclinical hyperthyroidism. Her thyroid stimulating hormone receptor antibodies were consistently elevated. Neck ultrasonography revealed an infrahyoid solid nodule and pertechnetate scintigraphy confirmed an increased uptake at the same level, without any uptake in the thyroid bed. Treatment with methimazole 5 mg/day was initiated with clinical improvement and achievement of euthyroidism. After that, she received 10 mCi of radioactive iodine. Since then, she experienced regression of the neck mass and is doing well on a replacement dose of levothyroxine. Recurrence of Graves’ disease in ectopic thyroid following total thyroidectomy is extremely rare. This diagnose should be considered in patients who underwent total thyroidectomy and remained with thyrotoxicosis despite decreasing the levothyroxine dose.
Keywords: endocrinology, thyroid disease
Background
Ectopic thyroid tissue (ETT) is a rare endocrine condition with an estimated prevalence of 1/100 000–300 000 people.1 ETT results from thyroid embryogenesis defects during its passage from the floor of the primitive foregut to its pretracheal position.2 ETT occurs more frequently in women.3 Lingual thyroid is the most frequent type, representing approximately 90% of the reported cases.1
The mechanisms involved in thyroid morphogenesis are not fully understood. Some transcription factors, such as TITF1, PAX8, HHEX and FOXE1, seem to play a central role in the thyroid morphogenesis and differentiation process.1 4 Patients with ETT are generally euthyroid, asymptomatic and usually discovered as an incidentaloma,1 4 although ETT can also present with mass effect symptoms or thyroid dysfunction.5 Hypothyroidism occurs in about 33% of patients with ETT and hyperthyroidism is extremely rare.6 Regarding definitive treatment options for Graves’ disease, total thyroidectomy provides the lowest risk of persistent or recurrent hyperthyroidism.7 Despite that, some reports of recurrence of Graves’ disease following total thyroidectomy in remnant thyroid tissue or ectopic thyroid have been rarely described.1 8 9
Case presentation
A 46-year-old woman with diagnosis of Graves’ disease underwent total thyroidectomy in 2015 with a benign histopathology reporting diffuse hyperplasia. Since thyroidectomy, the patient was being treated with levothyroxine 100 µg/day. Two years after surgery, a slow-growing midline neck nodule was noticed. The patient denied dysphonia, visual and compressive symptoms. Despite decreasing the dose and withdrawal of levothyroxine, she remained with subclinical hyperthyroidism. Blood test showed suppressed thyroid stimulating hormone (TSH) levels (<0.01 µUI/mL, reference range 0.27–4.20 µUI/mL), normal free T4 concentration (1.2 ng/dL, reference range 0.8–1.76 ng/dL) and elevated TSH-receptor antibodies (TSH-R-Ab) (33.1 U/L, normal <1.58 U/L). Thyroid peroxidase antibody (563 UI/mL, normal <35 UI/mL) and thyroglobulin antibody (2454 UI/mL, normal <115 UI/mL) were increased.
Investigations
A neck ultrasound was performed and revealed a well-defined solid nodule, hyperechoic, 2.13×1.27×2.92 cm in the infrahyoid topography (figure 1), without any evidence of orthotopic thyroid tissue. Doppler evaluation demonstrated a diffusely increased vascularity, characteristic of Graves’ disease. To determine the cause of her recurrent hyperthyroidism, pertechnetate scintigraphy was performed, which revealed elevated uptake in the median cervical superior region, localised at the infrahyoid area, at the same level as described in the neck ultrasound, without any evidence of uptake in the thyroid bed (figure 2).
Figure 1.
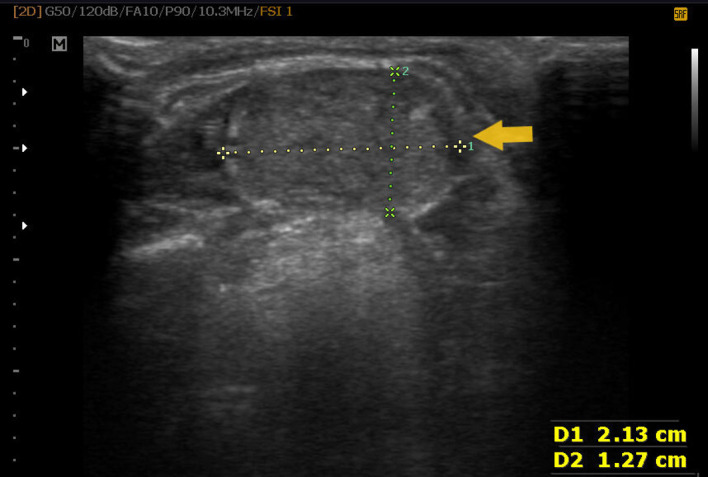
Ultrasonography of the neck shows a 2.13×1.27 cm hyperechoic nodule at the infrahyoid area (arrow).
Figure 2.
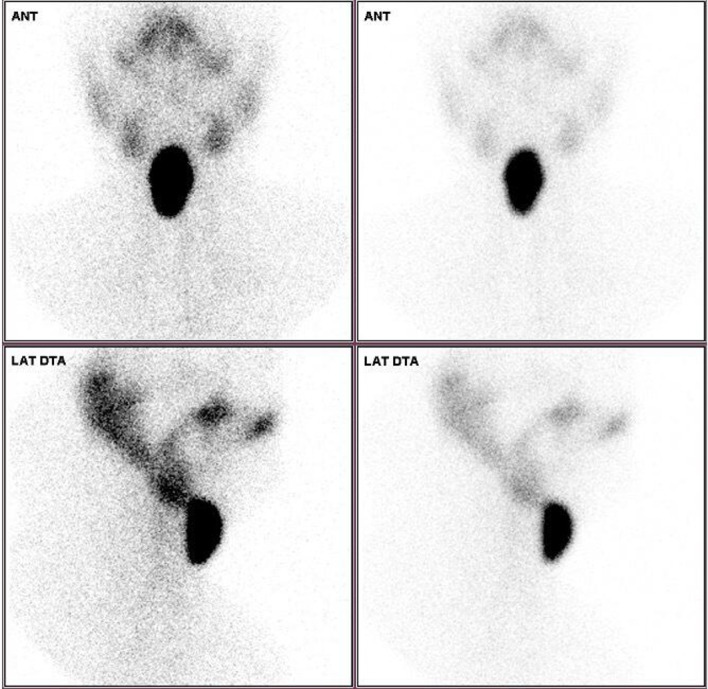
Pertechnetate scintigraphy revealed an increased uptake at the infrahyoid area without any uptake in the thyroid bed.
Treatment
A diagnosis of recurrence of Graves’ disease in ETT was established and she initiated treatment with methimazole 5 mg/day with clinical improvement and achievement of euthyroidism after 6 weeks. The patient received 10 mCi of radioactive iodine 131 after 12 months of therapy with methimazole.
Outcome and follow-up
Since radioactive iodine ablation, she experienced regression of the midline neck mass and is currently euthyroid with levothyroxine 75 µg/day.
Discussion
Graves’ disease is an autoimmune condition and represents the most frequent cause of thyrotoxicosis in iodine-repleted regions.10 Thyrotoxicosis following total thyroidectomy is mainly iatrogenic due to excessive thyroid hormone replacement. After excluding this hypothesis, the differential diagnosis should include other rare aetiologies as functional ETT or thyroid remnant.11
ETT results from embryogenesis defects during the migration of the gland from the foramen caecum to its pretracheal position. Autopsy data suggest a prevalence of ETT between 7% and 10%.8 Lingual thyroid represents the most frequent type (90% of reported cases), while sublingual ETT is rarely encountered.1 12 Sublingual ETT may be suprahyoid, infrahyoid or at the level of the hyoid bone.5
The majority of patients with ETT are asymptomatic and euthyroid.13 14 Clinical presentation may vary according to ETT location, size, growth and possible associated thyroid dysfunction.1 Hypothyroidism occurs in about 33% of patients with ectopic thyroid and thyrotoxicosis arising from ETT is exceptionally rare.6 An ETT containing pathological characteristics of Graves’ disease was reported in diverse topographies, such as submandibular,15 lingual,13 adrenal glands16 and ovary.17 In some of these reported cases, the diagnose of ETT was performed after thyroidectomy, like our patient.2 18
The exact mechanism of Graves’ disease recurrence in ETT after total thyroidectomy is not completely understood. However, it is proposed that circulating TSH-R-Ab may have a stimulatory effect on ETT, leading to thyroid hormone production and release, as well as the growth of the ETT.8 9
In our case, the infrahyoid ectopic thyroid presented as an anterior midline neck nodule 2 years after total thyroidectomy. As our patient remained with subclinical hyperthyroidism despite levothyroxine treatment withdrawal and her TSH-R-Ab levels were elevated, we consider the hypothesis of Graves’ disease recurrence in ETT. Thyroid scintigraphy is currently the gold standard for the diagnosis of ETT.1 19 Ultrasound scanning of the neck with Doppler was important to characterise the neck mass and to confirm the absence of eutopic thyroid.
Surgical resection of the ETT is indicated in case of associated compressive symptoms, bleeding or malignancy suspicion.1 17 20 In our case, the patient was submitted to radioactive iodine resulting in resolution of symptoms, without recurrence of Graves’ disease after 2 years of follow-up.
In conclusion, in patients with recurrent Graves' disease following total thyroidectomy, the diagnose of functional ETT should be considered, especially if no remnant tissue is found.17
Learning points.
Recurrence of Graves’ disease after surgery in ectopic thyroid tissue (ETT) is extremely rare.
Thyrotoxicosis after total thyroidectomy is mostly iatrogenic and rarely due to functional ETT.
Clinicians should consider the diagnosis of functional ETT in patients with recurrence of Graves’ disease following surgery, especially if no remnant tissue is found.
ETT may become hormonally active in the presence of thyroid stimulating hormone receptor antibodies.
Footnotes
Contributors: CC wrote the manuscript. CF, CS and JSD cooperated in the writing of the manuscript. CS and CC were involved in patient management and collection of data.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer-reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Noussios G, Anagnostis P, Goulis DG, et al. Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol 2011;165:375–82. 10.1530/EJE-11-0461 [DOI] [PubMed] [Google Scholar]
- 2.Guerra G, Cinelli M, Mesolella M, et al. Morphological, diagnostic and surgical features of ectopic thyroid gland: a review of literature. Int J Surg 2014;12(Suppl 1):S3–11. 10.1016/j.ijsu.2014.05.076 [DOI] [PubMed] [Google Scholar]
- 3.Adelchi C, Mara P, Melissa L, et al. Ectopic thyroid tissue in the head and neck: a case series. BMC Res Notes 2014;7:790. 10.1186/1756-0500-7-790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Felice M, Di Lauro R. Thyroid development and its disorders: genetics and molecular mechanisms. Endocr Rev 2004;25:722–46. 10.1210/er.2003-0028 [DOI] [PubMed] [Google Scholar]
- 5.Ibrahim NA, Fadeyibi IO. Ectopic thyroid: etiology, pathology and management. Hormones 2011;10:261–9. 10.14310/horm.2002.1317 [DOI] [PubMed] [Google Scholar]
- 6.Gu T, Jiang B, Wang N, et al. New insight into ectopic thyroid glands between the neck and maxillofacial region from a 42-case study. BMC Endocr Disord 2015;15:70. 10.1186/s12902-015-0066-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ross DS, Burch HB, Cooper DS, et al. 2016 American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 2016;26:1343–421. 10.1089/thy.2016.0229 [DOI] [PubMed] [Google Scholar]
- 8.Basaria S, Cooper DS. Graves' disease and recurrent ectopic thyroid tissue. Thyroid 1999;9:1261–4. 10.1089/thy.1999.9.1261 [DOI] [PubMed] [Google Scholar]
- 9.Jakibchuk K, Ali S, Samantray J. Recurrence of Graves’ disease in ectopic thyroid tissue. BMJ Case Rep 2018;30:bcr-2017-221566. 10.1136/bcr-2017-221566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahaly GJ, Bartalena L, Hegedüs L, et al. 2018 European thyroid association guideline for the management of Graves' hyperthyroidism. Eur Thyroid J 2018;7:167–86. 10.1159/000490384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cunha FM, Rodrigues E, Oliveira J, et al. Graves’ disease in a mediastinal mass presenting after total thyroidectomy for nontoxic multinodular goiter: a case report. J Med Case Rep 2016;10:1–6. 10.1186/s13256-016-0878-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoon JS, Won KC, Cho IH, et al. Clinical characteristics of ectopic thyroid in Korea. Thyroid 2007;17:1117–21. 10.1089/thy.2007.0004 [DOI] [PubMed] [Google Scholar]
- 13.Kim MS, Kong YH, Lee DY. A case of subclinical hypothyroidism with lingual and right Pretracheal ectopic thyroid. J Clin Res Pediatr Endocrinol 2015;7:148–50. 10.4274/jcrpe.1791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamijo K. Lingual thyroid associated with Graves' disease and Graves' ophthalmopathy. Thyroid 2005;15:1407–8. 10.1089/thy.2005.15.1407 [DOI] [PubMed] [Google Scholar]
- 15.Kumar R, Gupta R, Bal CS, et al. Thyrotoxicosis in a patient with submandibular thyroid. Thyroid 2000;10:363–5. 10.1089/thy.2000.10.363 [DOI] [PubMed] [Google Scholar]
- 16.Wang S-C, Hung S-W, Lee C-H, et al. Ectopic thyroid tissue in the adrenal gland mimicking a pheochromocytoma. J Endourol Case Rep 2017;3:149–51. 10.1089/cren.2017.0080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sitasuwan T, Hanamornroongruang S, Peerapatdit T, et al. Coexistence of Graves' disease and unilateral functioning struma ovarii: a case report. BMC Endocr Disord 2015;15:68. 10.1186/s12902-015-0060-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winters R, Christian RC, Sofferman R. Thyrotoxicosis due to ectopic lateral thyroid tissue presenting 5 years after total thyroidectomy. Endocr Pract 2011;17:70–3. 10.4158/EP10071.CR [DOI] [PubMed] [Google Scholar]
- 19.Chawla M, Kumar R, Malhotra A. Dual ectopic thyroid: case series and review of the literature. Clin Nucl Med 2007;32:1–5. 10.1097/01.rlu.0000249590.70176.58 [DOI] [PubMed] [Google Scholar]
- 20.Iglesias P, Olmos-García R, Riva B, et al. Iodine 131 and lingual thyroid. J Clin Endocrinol Metab 2008;93:4198–9. 10.1210/jc.2008-0909 [DOI] [PubMed] [Google Scholar]


