Abstract
Atrial septal defect (ASD) is the most common congenital heart disease observed in adult. Several ECG findings are considered sensitive for the diagnosis of ASD. We describe a 50 years old man who displayed Crochetage sign, incomplete right bundle branch block (IRBBB) and right ventricular strain pattern on ECG. Crochetage sign is highly specific for ASD and it correlates with shunt severity. The diagnostic specificity for ASD increases if the R waves have both Crochetage patterns and IRBBB. It is important not to confuse Crochetage signs with IRBBB abnormalities on ECG. Our patient was ultimately diagnosed with a large ASD measuring 3 cm with bidirectional shunt and concomitant pulmonary thrombosis. This illustrates that high suspicion of the ASD with the use of good-old ECG signs remains relevant in this modern era. This also reminds us that patients with Eisenmenger syndrome are at higher risk for pulmonary thrombosis.
Keywords: cardiovascular medicine, arrhythmias, valvar diseases, venous thromboembolism
Background
Unlike many congenital heart diseases, atrial septal defect (ASD) may first be diagnosed in adulthood as the clinical presentation may be vague and unnoticeable.1 2 Although echocardiography remains the mainstay tool for the diagnosis of ASD, ECG can be used as an inexpensive screening tool for ASD.3 One of the ECG findings in ASD is Crochetage sign, which is a specific sign for ASD of ostium secundum type.4 The specificity and sensitivity of Crochetage sign is further increased with the presence of right bundle branch block (RBBB) in ECG.4
ASD may remain asymptomatic, but in some patients, it may lead to pulmonary hypertension, Eisenmenger syndrome, heart failure, arrhythmias or even paradoxical embolism.1 2 There has been several case reports of patients with ASD presenting with pulmonary thromboembolism, namely patients with Eisenmenger,5 or after closure of ASD,6 and even in patients with left atrial thrombus passing through the defect causing pulmonary embolism.7
Case presentation
A 50-year-old man was diagnosed to have congenital heart disease 15 years prior during health check-up but subsequently defaulted follow-up. He presented to our centre with reports of shortness of breath for 3 months, which worsened on exertion, associated with orthopnoea, paroxysmal nocturnal dyspnoea and productive cough. Clinically, he had finger clubbing with fixed splitting of second heart sound and the absence of cyanosis. Lungs were clear on auscultation and there was no pedal oedema, oxygen saturation under room air was 95%–98%.
Investigations
Arterial blood gas taken under room air showed type 1 respiratory failure, potential of hydrogen (pH): 7.48, partial pressure oxygen: 61, partial pressure carbon dioxide: 28, bicarbonate: 23, base excess: −2.6. Admission ECG showed sinus tachycardia, right axis deviation, P pulmonale, partial RBBB with Crochetage sign-notched R wave in II, III, aVF, right ventricular strain picture with ST depression and T inversions in II, III, aVF (figure 1). Transoesophageal echocardiography showed secundum ASD of 3 cm with bidirectional shunt, blood clot in the right pulmonary artery and sign of pulmonary hypertension (figures 2–4). Chest radiograph showed cardiomegaly, dilated pulmonary artery and increased pulmonary vascular markings (figure 5). We proceeded with CT pulmonary angiogram which revealed a long segment eccentric chronic thrombus in the right main pulmonary artery and the ascending and descending right pulmonary arteries. There was also a filling defect in the left pulmonary artery extending to the left superior pulmonary artery in keeping with thrombosis. Further history showed no other risk factor of pulmonary embolism (Figure 6).
Figure 1.
ECG showing Crochetage sign (red arrow) with incomplete right bundle branch block.
Figure 2.
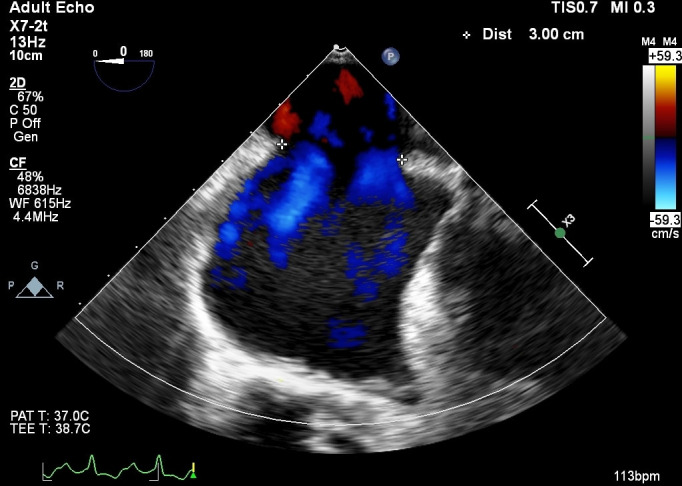
Atrial septal defect measuring 3 cm in size.
Figure 3.

Pulsed wave Doppler showing bidirectional shunt.
Figure 4.

Right pulmonary artery clot (red arrow).
Figure 5.

Chest X-ray showing cardiomegaly and dilated pulmonary artery and increased pulmonary vascular markings.
Figure 6.
CT pulmonary angiogram showing filling defect in right and left pulmonary arteries (red arrow).
Treatment
During his stay in the hospital, he further desaturated under room air and was tachypnoeic, with respiratory rate of 42 breaths per min, as well as hypotensive, blood pressure 81/51. He was then treated as a case of large ASD with massive pulmonary embolism complicated by pulmonary hypertension where subsequently thrombolysed with intravenous streptokinase along with inotropic support in view of massive pulmonary embolism and haemodynamically compromised. Ultrasound Doppler of the lower limbs showed no deep vein thrombosis. He was then discharged well with warfarin
Outcome and follow-up
On 3 months follow-up, he had improved symptomatically and planned for right heart study after resolution of pulmonary embolism.
Discussion
Patients with ASDs may be asymptomatic or present with vague signs and symptoms. As a result, many patients with ASD are first diagnosed during adulthood or even in older age.3 Early diagnosis of ASD is beneficial as it can lead to debilitating complications if left undiagnosed.1 Thus, it is of paramount importance to have a high index of ECG suspicion in patients with suggestive history and physical examination and certain electrocardiographic signs, which can later be confirmed with echocardiography.3
Patients with uncomplicated ASD may have normal ECGs,1 but there are a few ECG changes that may trigger suspicion of ASD. These include prolonged PR interval, QRS complex interval and incomplete RBBB.1 Different types of ASDs can have different ECG changes as well. Patients with primum ASD can have left axis deviation with first-degree heart block, whereas those with secundum ASDs can have right axis deviation with incomplete RBBB.1 Sinus venosus ASDs may show ectopic atrial pacemaker, for example, inverted P waves in inferior leads.1 Crochetage sign on the other hand is an independent ECG sign of ostium secundum ASD.4
Crochetage sign is defined as a notch that resembles the work of a crochet needle, characteristically at the rising edge or peak of the R wave in inferior leads of II, III, aVF.2 8 The presence of Crochetage sign was highly specific for ASD with specificity reaches 92%–100% if present in all three inferior leads.3 It also correlates with shunt severity and the incidence of Crochetage sign was shown to be higher in the group with ≥5 mm ASD size.2 Thus, Crochetage sign may represent a large left-to-right shunt in patients with ASD. On the other hand, Crochetage sign may also be seen in other conditions. Heller et al in 1996 observed that it is present in at least one inferior lead in 35.7% of patients with ventricular septal defect, 23.3% of patients with pulmonary stenosis, 10.6% of patients with Cor pulmonale and 7.4% of normal person.2
It is important not to confuse Crochetage signs with incomplete RBBB (IRBBB) abnormalities on ECG. Incomplete RBBB is when the QRS duration is between 80 and 120 ms with a R’ or r’ in lead V1 or V2 and a wide S wave in lead V6.2 It may be differentiated where Crochetage pattern typically appears at the starting point of QRS wave within 80 ms, while IRBBB abnormality often at the end of QRS.2 Crochetage sign also independent of the incomplete RBBB pattern and various studies reported that diagnostic specificity for ASD increases if the R waves have both Crochetage patterns and IRBBB.2 Among the patients with ASD who underwent surgical closure, 35.1% of them had the disappearance of Crochetage sign on ECG while the IRBBB remained due to right ventricular overload.2 8 Usually, patients with ASD will have sinus rhythm; however, atrial arrhythmias such as atrial fibrillation or supraventricular tachycardia is not uncommonly seen at third or fourth decades of life.9
Beside cardiac arrhythmia, ASD also associated with young stroke in young as a result of paradoxical embolism.3 The presence of Crochetage sign in young patients presenting with cryptogenic stroke maybe an indicator of an underlying patent foramen ovale and warrants an echocardiographic evaluation.1 8
There have been numerous reports of patients with ASDs presenting with pulmonary thromboembolism similar to our patient.5 7 10 11 The possible explanation of pulmonary thrombosis can be due to embolisation from other sites, hypercoagulable state, primary pulmonary hypertension or Eisenmenger syndrome.5 Patients with Eisenmenger syndrome has a 21%–29% risk for pulmonary artery thrombus formation and in these subgroups of patients, it is postulated that in situ thrombosis formation rather than distant side embolisation leading to pulmonary thrombosis.5 Thus, pulmonary arterial hypertension with concomitant Eisenmenger syndrome is an important clinical consideration when dealing with patent with proximal thrombus in pulmonary arteries.5
In summary, our patient had a combination of typical Crochetage sign ECG, large ASD and massive pulmonary embolism. High suspicion of the ASD with the use of good-old ECG signs is remaining relevant in this modern era.
Patient’s perspective.
I first realised something was amiss when I was working as a security guard in Singapore approximately 20 years ago. I had to walk long distances due to the nature of my work and I found that I became breathless more easily than my counterpart.
When it was time to renew my permit to work in Singapore, I went through a body check-up and my doctor told me I had a hole in my heart. He suggested that I received treatment in my home country as the cost would have been very expensive in Singapore. Of course, my working permit was not renewed.
I took up a job as a van and lorry driver once I was back in Malaysia. While driving, I had episodes of dizziness and shortness of breath. There was an instance when I thought I was going to crash if I continued driving, thus I parked my car by the roadside and rested for approximately 20 min.
I sought treatment in government hospital in Johor, Malaysia, and the doctors were kind enough to arrange for further treatment in National Heart Institute of Malaysia. I stayed there for about 4 days and was investigated further. They told me I had a big hole in my heart and it would be difficult to close. I was hit with a hospital bill of approximately RM20 000 and I only had about RM1000 in my pocket. The hospital administration was kind enough to refer me to social welfare and I was charged with only RM500
I was lost to follow-up as I became busy with work and children. Recently, my shortness of breath worsened and I came to the hospital again. I was told to have blood clot in my lungs and I had to take blood thinners. I have been taking the meds ever since and have been coming for follow-up regularly. My doctor told me I will have another scan of my lungs to reassess the blood clots and decide on next course of treatment. I lost my wife recently and I have stopped working ever since. My daughter now cares for my two teenage boys while I stay alone doing household chores as much as my breath allows.
Learning points.
Crochetage sign is an independent ECG sign of ostium secundum atrial septal defect (ASD).
Crochetage sign may represent a large left-to-right shunt in patients with ASD.
The diagnostic specificity for ASD increases if the R waves have both Crochetage patterns and incomplete right bundle branch block.
Patients with Eisenmenger syndrome are at higher risk for pulmonary artery thrombus formation.
Acknowledgments
I would like to thank echocardiographer Mr Sailesh for helping us with the scans.
Footnotes
Contributors: NK identified this case as potential case report and was involved in the management of the case. NK also performed the literature research, drafted and revised the case report, obtained consent from the patient and obtained the images for the case report. She is the guarantor. WJL performed the literature search, revised the case report, becoming the corresponding person for this case for case report submission. HSK contributed in proofreading and revising the case report critically and gave final approval for the version being published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Bayar N, Arslan Şakir, Köklü E, et al. The importance of electrocardiographic findings in the diagnosis of atrial septal defect. Kardiol Pol 2015;73:331–6. 10.5603/KP.a2014.0240 [DOI] [PubMed] [Google Scholar]
- 2.Shen L, Liu J, Li J-K, et al. The significance of Crochetage on the R wave of an electrocardiogram for the early diagnosis of pediatric secundum atrial septal defect. Pediatr Cardiol 2018;39:1031–5. 10.1007/s00246-018-1857-0 [DOI] [PubMed] [Google Scholar]
- 3.Heller J, Hagège AA, Besse B, et al. "Crochetage" (notch) on R wave in inferior limb leads: a new independent electrocardiographic sign of atrial septal defect. J Am Coll Cardiol 1996;27:877–82. 10.1016/0735-1097(95)00554-4 [DOI] [PubMed] [Google Scholar]
- 4.Singh H, Pannu AK, Dahiya N, et al. 'Crochetage' sign of atrial septal defect. QJM 2020;113:133–4. 10.1093/qjmed/hcz142 [DOI] [PubMed] [Google Scholar]
- 5.Lee C-W, Huang S-S, Huang P-H. Pulmonary arterial thrombosis in a patient with an atrial septal defect and Eisenmenger syndrome. Korean Circ J 2012;42:772–5. 10.4070/kcj.2012.42.11.772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Busch T, Lotfi S, Sirbu H, et al. Fatal pulmonary embolism after atrial septal defect closure in a paediatric patient. Scand Cardiovasc J 1999;33:187–8. 10.1080/14017439950141858 [DOI] [PubMed] [Google Scholar]
- 7.Ishihara Y, Hara H, Saijo T, et al. Left atrial thrombus causing pulmonary embolism by passing through an atrial septal defect. Circ J 2002;66:109–10. 10.1253/circj.66.109 [DOI] [PubMed] [Google Scholar]
- 8.Bhattacharyya PJ. 'Crochetage' sign on ECG in secundum ASD: clinical significance. BMJ Case Rep 2016;2016. 10.1136/bcr-2016-217817. [Epub ahead of print: 08 Oct 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gatzoulis MA, Freeman MA, Siu SC, et al. Atrial arrhythmia after surgical closure of atrial septal defects in adults. N Engl J Med 1999;340:839–46. 10.1056/NEJM199903183401103 [DOI] [PubMed] [Google Scholar]
- 10.Dinesh Kumar US, Nareppa U, Shetty SP, et al. Right ventricular thrombus in case of atrial septal defect with massive pulmonary embolism: a diagnostic dilemma. Ann Card Anaesth 2016;19:173–6. 10.4103/0971-9784.173043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tien-Yu W, Lan W-R, Hou CJ-Y, et al. Intracardiac thrombi, pulmonary embolism, atrial septal defect, and polycythemia vera. Acta Cardiologica Sinica 2018;24:217–20. [Google Scholar]




