Abstract
Background
An estimated 140 000 refugees from Burma have resettled to the USA since 2009, comprising 21% of total resettlement in the USA over the last decade. Our objective was to describe patterns of longitudinal health outcomes in a cohort of Karen refugees resettled in the USA for 5 years, and to translate these findings to a primary healthcare context.
Methods
The study was a retrospective cohort study focused on the analysis of the first 5 years of electronic health records of a sample of 143 Karen refugees who were initially resettled between May 2011 and May 2013.
Results
Through descriptive, inferential and survival statistics, we described patterns of retention in primary care, biometric trends, condition prevalence and survival probabilities. Highest prevalence health conditions documented at any point in the 5-year period included diagnoses or symptoms associated with pain (52%); gastrointestinal disturbance (41%); metabolic disorder (41%); infectious process (34%); mental health condition (31%) and central nervous system disorder (24%).
Conclusions
This study is the first retrospective longitudinal analysis of patterns of health in Karen refugees originating from Burma and resettled to the USA. Findings identified in the 5-year, the post-resettlement period provided important clinical insights into the health trajectories of war-affected populations. Burden of illness was high although results did not demonstrate the extent of trauma-associated physical health conditions reported in the literature. Indicators such as significant increases in body mass index (BMI), the overall prevalence of dyslipidaemia and others suggested that the cohort may be exhibiting an early trajectory towards the development of these conditions. Authors summarize potential protective factors experienced by the cohort that promoted aspects of health frequently challenged in forced migration.
Keywords: Burma, mental health, physical health, refugee, resettlement, trauma
Key Messages.
Key clinical insights provided on longitudinal health trajectories of a war-affected group.
Burden of illness across the cohort was high and consistent with literature.
Factors such as bilingual/bicultural clinic services are likely protective.
Health outcomes in war-affected populations are multidetermined.
Introduction
Approximately 140 000 refugees from Burma have resettled to the USA since 2009, comprising 21% of refugees resettled over the last decade (1). Karen refugees, an ethnic minority in Burma, endured a protracted civil war and significant war traumas including torture, extrajudicial killing, burning of villages, forced labour and conflict-related sexual violence (2–4). In 2017, we reported physical correlates of this trauma and associations with patterns of health among Karen refugees (5).
Prior research documents associations between trauma from torture or war and mental and physical health disturbances including posttraumatic stress disorder (PTSD), common sequelae of torture. Though mechanisms through which trauma is expressed physiologically continue to be investigated, the emergence of pain and somatic disorders in relation to inflammatory processes align with relevant conceptual models (6). The declining health of refugees over time is more recently documented and contributes to an understanding of the enduring effects of trauma, specifically associations between mental, cardiovascular, metabolic and neurological disturbances and past conflict-exposure (7,8).
Chronic disease prevalence is an important index of health in refugee populations over time. Rhodes et al. reported lower rates of diabetes, hypertension and hyperlipidaemia among African refugees at baseline compared to controls, but 5 years later found that diabetes and hyperlipidaemia were no longer statistically different than controls (9).
Additionally, though hypertension diagnoses remained statistically lower than controls, rates of hypertension, diabetes and hyperlipidaemia increased significantly in the study period. Refugee men have higher rates of cardiovascular-related deaths (10) and mortality rates among refugees were higher for stroke and diabetes (11). Among adult refugees with a mental health diagnosis, rates of hypertension, diabetes, tobacco use and overweight/obesity were higher compared to counterparts without a mental health diagnosis (12). Additionally, the greater the burden of chronic diseases, the greater the severity of reported PTSD and depression symptoms (8).
Current and ongoing stressors in resettlement, including housing and food insecurity, violence and discrimination, access to healthcare, language barriers and low-wage employment, also play significant roles in health status in the years following resettlement (13–17). Additionally, research has documented a lack of culturally responsive treatment options and care coordination services for people with refugee backgrounds (18). Integrated behavioural healthcare in primary care settings is one promising approach for addressing psychosocial stressors and wellbeing for resettled war-affected patients, especially those with complex health conditions (19,20). However, limited research describing specific, longitudinal patterns of health in the post-resettlement period is a barrier to the implementation of targeted clinical support and interventions.
Objective
The present article describes findings from a subsequent 5-year retrospective cohort analysis, the first longitudinal follow up study on the physical and mental health of Karen refugees. Our objective is to describe patterns of longitudinal health outcomes in a cohort of Karen refugees resettled in the USA for 5 years, and to translate these findings to a primary healthcare context. We report an overall prevalence of health conditions and describe patterns of new diagnoses and how emerging diagnoses were distributed over the 5-year study period. We summarize retention in primary care and consider how this and other factors such as BMI may help to predict trends over time and facilitate early intervention.
Methods
Study design
The study was a retrospective cohort study that analysed the first 5 years of electronic health records of a sample of Karen refugees who initially resettled between May 2011 and May 2013. The 5-year retrospective analysis was conducted in partnership with a mid-size primary care clinic, situated within a large health care system. The clinic is located in the most densely populated community of Karen people in the twin cities metro area and offers extensive bilingual/bicultural resources for the diverse population it serves. Study participants were enrolled and screened within the first 3 months of resettlement between May 2011 and May 2013. The clinic continued to provide primary care to a majority of the members of the cohort during the follow-up period.
Participants
The study team abstracted retrospective health encounter data from the electronic records of Karen refugees over the age of 18 years who: (i) presented for their Refugee Health Screening Exam between May 2011 and May 2013 and (ii) were orally administered the Family Demographic Questionnaire and the Refugee Mental Health Screening Tool during an earlier study phase (4).
Procedure
Participants were contacted by a Karen bilingual/bicultural worker by phone to obtain verbal consent. Participants were read a standardized telephone script description of the study procedures and offered the opportunity to ask questions. Participants were asked if they continued to receive care at the primary study partner clinic or where else they had established primary care. Upon consenting to access the 5-year period of health records, the participant address was verified and they were mailed a copy of the translated consent form. Of the 147 potential participants who were located in the records, four declined to participate in the study.
Data collection
The study team reviewed all clinic encounters from the initial public health screening through the present date or termination of care at the clinic. We abstracted key health variables from participants’ charts using the 64-item structured health history abstraction tool. Within the tool, social/demographic, vital sign and laboratory values were free text fields. Diagnostic/problem/symptomatic data and health behaviour information were coded as dichotomous ‘yes’ or ‘no’ values and specific diagnoses, problems and symptoms were also collected via open text fields. For example, ‘digestive diseases’ could be selected on the health history abstraction form and ‘gastroesophageal reflux disease (GERD)’ specified in an open field. An ‘other significant long-term/chronic issues’ field also allowed abstractors to code less common diagnoses and problems. Determination of diagnoses, problems and symptoms were made by healthcare providers and documented in visit progress notes or added to the electronic medical record (EMR) patient problem list. Health data was immediately de-identified and entered into a REDCap project database. Data entry was verified for accuracy by a second study team member.
Quantitative variables
The 64-item structured data extraction tool included social and demographic data, biometric data recorded at the first and last visits, problems and diagnoses identified in progress notes or the problem list, lab values and use of alcohol, tobacco or betel nut. This tool was developed by Hoffman et al. to ascertain baseline health characteristics at the time of resettlement (5). When there were too few observations of a specific problem, variables were collapsed into broader categories for analysis, for example, hypercholesterolemia was incorporated into ‘metabolic disorders’. We extracted a total of 340 health variables that were collapsed into 12 categories.
Statistical analysis
Primary analyses included descriptive, inferential and survival statistics. Baseline mental and physical health data collected at the initial resettlement exam were integrated with 5 years of data extracted from clinic encounters. Statistically significant results were evaluated for the need to adjust outcomes by known covariates, such as age. Survival statistics, such as Kaplan–Meier (KM) curves, were used to visualize longitudinal mental and physical health outcomes. Survival analysis was used to examine the length of time between arrival and the identification of a health condition recorded in the EMR. Given the impossibility of ascertaining the date of diagnosis for conditions that occurred prior to resettlement, we artificially coded some conditions as developed at day 1. This enabled the KM curve to show rates at screening and end prevalence. Data were censored at the latest documented visit in the EMR. Statistical analyses were performed using SAS version 9.420 with statistical significance set at p < 0.05 and statistical trends considered at p < 0.1, given the small sample.
Results
Table 1 shows the demographic characteristics of the cohort, which consisted of 143 patients including 72 women (50%). At the time of resettlement, the mean age of the sample was 34 (SD = 14), range 18–80 years.
Table 1.
Demographic description of a cohort of 143 resettled Karen refugees (2011–13).
| Mean | SD | Range | |
|---|---|---|---|
| N | % | ||
| Age | 34.0 | 14.5 | 18–80 |
| Children, came with to USA | 87 | 61% | |
| Number of children | 2.2 | 1.1 | 1–6 |
| Education, years | 6.9 | 3.7 | 1–14 |
| Time in camp, years | 13.7 | 5.1 | 6–32 |
| Sex | |||
| Female | 72 | 50% | |
| Male | 71 | 50% | |
| Marital status | |||
| Single | 45 | 31% | |
| Married | 81 | 57% | |
| Widowed | 12 | 8% | |
| Divorced/separated | 3 | 2% | |
| Unknown | 2 | 1% | |
| CDC BMI classification (baseline) | |||
| Underweight | 5 | 5% | |
| Normal | 79 | 72% | |
| Overweight | 22 | 20% | |
| Obese | 4 | 4% | |
| WHO BMI risk points (baseline) | |||
| Underweight | 5 | 5% | |
| Normal | 59 | 54% | |
| Overweight | 38 | 35% | |
| Obese | 8 | 7% |
We were able to locate 147 of the original 177 participants (4) within health system medical records to extract data for the current study. The 30 study participants who could not be located likely had updates or corrections made to their name and/or birthdate recorded during the study period. Our previous analysis of baseline physical health characteristics included 111 participants from the original cohort (5). The current study used an upgraded EMR technology that included the use of a ‘sounds-like’ feature to identify additional participants. Eleven participant medical records from the original analysis could not be located for this study.
Retention in primary care
No follow up visits were recorded for 18 (13%) participants, who were screened at initial resettlement but lost to follow up. At 1 year, an additional 26 participants were lost to follow up. Males were less likely to remain in primary care beyond 1 year (χ2(1, N = 143) = 3.49, P = 0.06). Younger participants were significantly more likely to leave care within the first year of resettlement (M = 27.3, SD = 9.0) than those retained beyond one year (M = 37.0, SD = 15.4), t = 3.85, P < 0.001. Of the 125 participants who presented for at least one follow-up encounter, 57 (50%) participants completed the full 5-year study period within the care of the primary clinic partner and 87 (61%) had >3 years of follow up. Throughout the 5-year study period, 16 participants reported establishing primary care elsewhere and two were reported deceased.
Biometric data
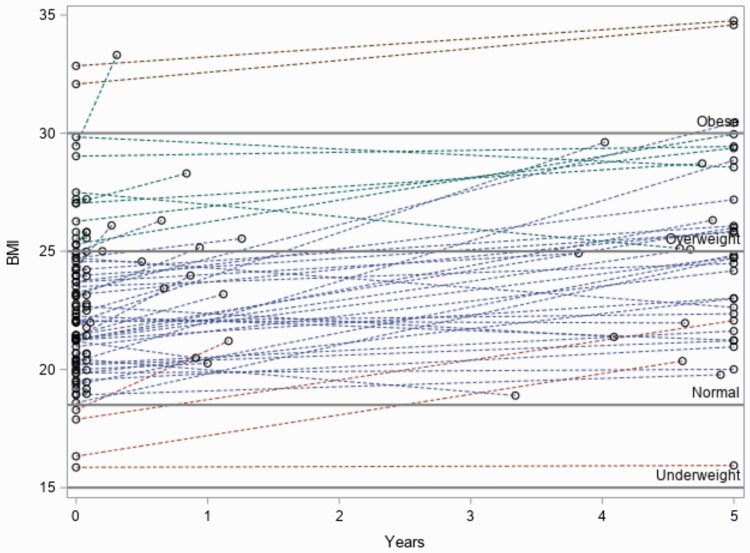
The study team extracted BMI (n = 65), blood pressure (n = 101) and heart rate (n = 97) at the initial health screening exam and last recorded encounter. Participants were excluded from these calculations if one or both timepoints were missing from the chart. Systolic blood pressure (SBP) increased on average by 6.2 points (SD = 14.7, P < 0.001). Diastolic blood pressure (DBP) increased on average by 3.7 points (SD = 10.7, P < 0.001). Heart rate increased 2.8 beats per minute (SD = 13.1, P < 0.05). BMI increased or stayed the same in 55 (85%); increased in 47 (72%); and increased by >1 unit in 36 participants (55%). Overall BMI scores increased by an average of 1.9 units (t-value = 5.41, P < 0.001, SD = 2.8). Increase in BMI was significantly higher in females than males (t-value = 2.49, P < 0.05, 2.7 (3.1) versus 1.0 (2.1), respectively). Figure 1 shows BMI assessments at baseline and the final recorded clinic encounter. Participants initially classified as normal gained 1.7 (SD = 2.4) BMI units on average. Those initially classified as underweight gained 2.8 (SD = 1.9) BMI units on average. Participants initially classified as overweight or obese gained on average 2.2 (SD = 4.6) and 2.2 (SD = 0.42) BMI units, respectively.
Figure 1.
BMI change over time in a cohort of 143 resettled Karen refugees.
Condition prevalence
Table 2 shows the overall disease burden and a comparison of disease prevalence at initial resettlement with cumulative diagnoses over 5 years. Among the overall highest prevalence health conditions documented at any point in the 5-year period, 52% reported pain; 41% were diagnosed or had symptoms of a gastrointestinal disturbance; 41% were diagnosed or reported symptoms consistent with a metabolic disorder; 34% were diagnosed with an infectious process; 31% were diagnosed with a mental health condition and 24% were diagnosed or reported symptoms consistent with a central nervous system disorder. Hepatitis B diagnosis was prominent among men in the sample (25%); all but one case identified at the initial refugee health screening exam were men. New diagnoses of pain (n = 51), gastrointestinal disturbance (n = 50), mental health condition (n = 37), sleep/fatigue disturbances (n = 27), respiratory conditions (n = 26), central nervous system disturbances (n = 25) and cardiac conditions (n = 14) in the 5-year post-resettlement period were recorded.
Table 2.
Health conditions at two time points in a cohort of 143 resettled Karen refugees: baseline resettlement and overall prevalence
| At Resettlement |
All Dx ever | |||
|---|---|---|---|---|
| N = 143 | ||||
| Pain | 23 | 16 | 74 | 52 |
| Back | 11 | 8 | 46 | 32 |
| Headache | 5 | 3 | 20 | 14 |
| GI | 9 | 6 | 59 | 41 |
| Stomach | 5 | 3 | 27 | 19 |
| Constipation | 1 | 1 | 16 | 11 |
| NV | 0 | 0 | 13 | 9 |
| Gerd | 0 | 0 | 13 | 9 |
| Metabolic | 44 | 31 | 58 | 41 |
| Dyslipidaemia | 44 | 31 | 58 | 41 |
| DM Type 2 | 0 | 0 | 6 | 4 |
| Obesity (dx) | 0 | 0 | 3 | 2 |
| Infection | 30 | 21 | 48 | 34 |
| HepB | 23 | 16 | 23 | 16 |
| CNS Neuro | 10 | 7 | 35 | 24 |
| Dizziness | 8 | 6 | 30 | 21 |
| Eye and vision | 22 | 15 | 35 | 24 |
| Derm | 10 | 7 | 34 | 24 |
| Resp | 4 | 3 | 30 | 21 |
| Sleep/fatigue | 3 | 2 | 30 | 21 |
| Insomnia | 3 | 2 | 23 | 16 |
| Cardiac | 16 | 11 | 30 | 21 |
| Hypertension | 8 | 6 | 17 | 12 |
| Nutrition | 3 | 2 | 21 | 15 |
| Vitamin D deficiency | 3 | 2 | 19 | 13 |
| Mental health | 12 | 8 | 45 | 31 |
| PTSD | 6 | 4 | 25 | 17 |
| Depression combo | 2 | 1 | 20 | 14 |
| Anxiety | 4 | 3 | 10 | 7 |
| Substance use including Nic | 27 | 19 | 40 | 28 |
| Substance use | 15 | 10 | 22 | 15 |
| Substance abuse | 2 | 1 | 6 | 4 |
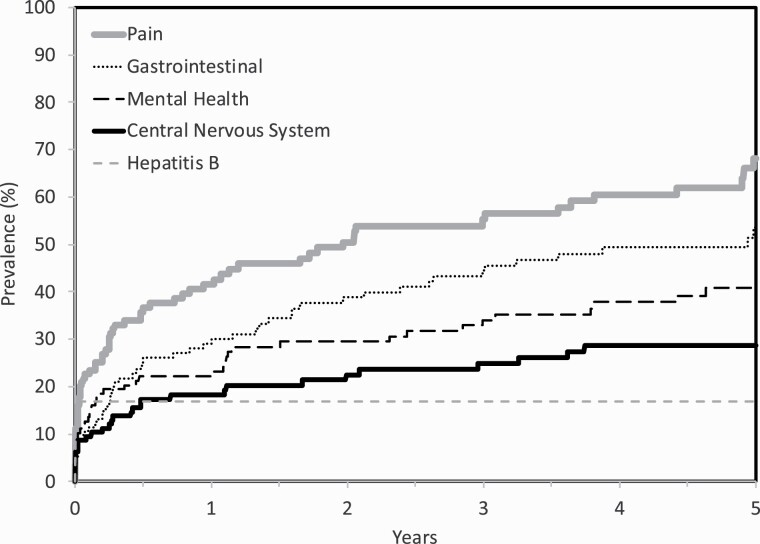
Disease probability
Disease probabilities were calculated for high prevalence and conceptually important health conditions to visually represent disease burden, potential clinical points of intervention, and disease progression patterns (Fig. 2). We used KM estimates versus raw percentages because KM estimates included censored participants and therefore demonstrated greater relevance to population health. In all cases, KM confidence intervals included raw percentages.
Figure 2.
Kaplan–Meier disease probability curves for pain, gastrointestinal disturbances, central nervous system disturbances, mental health conditions over the 5-year resettlement period.
Discussion
This study is the first retrospective longitudinal analysis of patterns of the health of resettled Karen refugees. Findings provide important clinical insights into health trajectories experienced by war-affected populations. The sample resided in an urban area in a state with a relatively established network of support for refugees. The sample demonstrated good retention in a primary care clinic with programs adapted to meet the needs of Karen patients. The clinic care model employs eight full-time Karen staff, provides bicultural care coordination and language accessible transportation assistance.
Despite these strengths, the burden of illness across the cohort was high. Physiologic symptoms included gastrointestinal disturbances, central nervous system disturbances, mental health conditions and pain. We observed higher rates of new-onset sleep/fatigue, respiratory, central nervous system and cardiac system disturbances relative to other identified conditions. These findings are consistent with literature that describes an overall health decline in war-affected individuals and the prevalence of cardiometabolic and other physiologic disturbances attributed to underlying systemic inflammation associated with PTSD (21–23). These conditions emerged gradually over the 5-year resettlement period emphasizing the importance of continued engagement in primary care.
To enhance the interpretation of results, we compared results to data on health indicators for Asian Americans and Southeast Asians in the USA (24,25). Foreign-born Asian Americans represent 70% of Asian Americans in the USA. The ethnicity is underrepresented in disaggregated population health data, and particularly disproportionate in cardiovascular health indicators (26). Rates of dyslipidaemia in our sample were higher than reference norms, where reference percentages of men (27.3) and women (24.4) age 20 and older developed hypercholesterolemia (25). Otherwise, disease prevalence in the cohort did not surpass reference norms.
Rates of new-onset obesity, hypertension, respiratory conditions, pain and statistically and clinically significant increases in blood pressure suggested a potential for continued health decline in the cohort. Of the 11 physical system categories reported in Table 2, 87% of participants reported at least one complaint, with an average of 3.6 complaints (median = 3). Among participants, 12.5% (n = 18) reported no physical health concerns; 11.8% (n = 17) reported no physical or mental health concerns. Rates of mental health conditions in our sample reflect a concerning trend in the prevalence of severe mental illness identified both in refugee studies and reference norms, and represent an important focus for ongoing surveillance and intervention. Back pain was among the highest prevalence complaints recorded. Conclusions that back pain and headaches are psychosomatic must be carefully evaluated. In this population, back pain may be associated with forced portering, a form of torture that involved being forced to carry heavy loads. These may be physical injuries that are closely associated with PTSD as the pain serves as a reminder of trauma. Physical therapy interventions that restore function and optimize mobility may be effective in these circumstances.
Rates of obesity in the cohort were lower than standard US-based BMI classifications (24,27). However, the extent of movement at the extremes of the scale provided a nuanced look at the potential trends in BMI patterns over time. When compared to WHO recommended action points for Asian populations, which vary from US standards, the sample demonstrated a higher tendency towards overweight/obesity (28). Overweight/obesity is a predictor of metabolic disturbances in trauma-exposed populations and may be an early indicator of predisposition towards more complex conditions (9,29). As research increasingly highlights longitudinal trajectories post-migration, nutritional status, weight gain and weight class are emerging themes (30–38). A study of refugee adults resettled in the USA found that proportions of obesity increased from 39.6% to 58.9% among men and 55.1% to 74.5% among women over 10 years (30). Region of origin, baseline weight and duration in the USA were significant risk factors. Generational patterns of overweight/obesity, nutrition inequity and targeted screening and intervention are important clinical considerations in refugee health.
The prevalence of gastrointestinal disturbances is multifactorial. The finding is aligned with literature describing the health effects of dysbiosis and the contributing roles of physiological and psychological stressors to alterations in the gut microbiota (35). In Hmong and Karen refugee populations, the post-resettlement acquired microbiome demonstrated reduced functional effectiveness, with a duration of decline that theoretically persists for generations (36). A potential contributing factor to gastrointestinal disturbances observed in refugees that has not been examined is the administration of presumptive treatment for intestinal parasites and malaria prior to resettlement (37). The prevalence of Helicobacter pylori bacterial infection/colonization of the gastrointestinal (GI) tract is also a possible reason for increased GI problems/symptoms/malignancies in the Southeast Asian population (38).
The importance of effective history taking with refugees has been emphasized (39). The KM disease probability curve for Hepatitis B demonstrates this point. We reported active Hepatitis B infection among 23 males (M = 32, SD =13.1, median = 28 years of age), 75% were less than 36 years old. All cases of Hepatitis B were diagnosed at the resettlement screening. Discussions with clinic partners in the interpretation of this finding revealed anecdotal reports of tattooing with shared needles as a common camp practice among young Karen males. Effective history taking facilitates the construction of a clinical picture that can be useful in targeted screening and intervention programs. Overseas refugee medical immunization protocols are robust, and in the post-resettlement period the Karen community has demonstrated high compliance with routine immunization. That said, in the context of COVID-19 and planning for vaccine distribution in refugee communities, thorough assessments of immunity and discussions around vaccination facilitated by bilingual/bicultural navigators are an essential function of primary care.
Limitations
As a retrospective study, data were limited to documentation of historical health assessments in the EMR. We included representation from the provider group on our study team, though this does not completely mitigate variation in individual documentation practices. Participation in health interventions such as prescription medications and psychosocial programs were generally not recorded in the EMR and thus is largely unknown. If health interventions were mentioned, we did not have to follow up data on participation and/or compliance with these programs. Five years is an abbreviated time to capture significant clinical outcomes. Our sample was small, so findings have limited external validity.
Conclusion
Results of this 5-year retrospective analysis did not demonstrate the extent of trauma-associated physical health conditions reported in the literature. Indicators such as significant increases in BMI, the overall prevalence of dyslipidaemia, and others suggested that the cohort may be exhibiting an early trajectory towards the development of these conditions. Reports of pain and other somatic conditions were common, which we attributed to early effects of systemic inflammation observed in trauma-exposed individuals and psychological/psychosomatic causes.
It is possible that health patterns observed in the sample are explained by historical war trauma exposure. However, it is more likely that observed health outcomes are multidetermined, explained both by historical trauma and ongoing resettlement stressors that further underlying predisposition to poor clinical outcomes. Whether and how trauma from war persists and interacts with post-resettlement stressors and contributes to the declining patterns of health observed in refugee groups is an important consideration. It is essential to consider protective factors, for example, the size and strength of the local Karen community (40). The quick evolution of community support systems, Karen grocers, faith institutions and cultural events may provide insulation against the rapid adoption of unhealthy cultural and diet patterns in the USA. Refugee communities could benefit from additional education about the health risks of lifestyle factors, particularly when those discussions are facilitated by bilingual/bicultural navigators. Our sample is unique because our average age was relatively young. We attribute results to observations made at a mid-point of a trajectory that we believe, left unaddressed, will further impact physiologic systems and overall health.
Declarations
Funding: Research reported in this publication was supported by the University of Minnesota Office of the Vice President for Research and the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number K12HD055887. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All authors have no conflicts of interest to report. We acknowledge the Center for Victims of Torture, headquartered in St. Paul, Minnesota, for their contributions to data collection in earlier study phases.
Conflict of interest: All authors have no conflicts of interest to report.
Ethics: Institutional review board (IRB) approval was obtained from HealthEast (now M Health Fairview) Care System (HE 17 07 001/July 5, 2017) and the University of Minnesota (STUDY00000215/24 August 2017).
Data availability statement
The data that support the findings of this study are available from the corresponding author, SH, upon reasonable request.
References
- 1. Blizzard B, Batalova J. Refugees and asylees in the United States. Online J Migrat Policy Inst 2019. https://www.migrationpolicy.org/article/refugees-and-asylees-united-states-2018 (accessed on 10 January 2020). [Google Scholar]
- 2. IHRC. Legal Memorandum: War Crimes and Crimes Against Humanity in Eastern Myanmar. 2014. Retrieved from http://hrp.law.harvard.edu/wp-content/uploads/2014/11/2014.11.05-IHRC-Legal-Memorandum.pdf (accessed on 10 January 2020).
- 3. Schweitzer RD, Brough M, Vromans L, Asic-Kobe M. Mental health of newly arrived Burmese refugees in Australia: contributions of pre-migration and post-migration experience. Aust N Z J Psychiatry 2011; 45(4): 299–307. [DOI] [PubMed] [Google Scholar]
- 4. Shannon PJ, Vinson GA, Wieling E, Cook T, Letts J. Torture, war trauma, and mental health symptoms of newly arrived Karen refugees. J Loss Trauma 2015; 20(6): 577–90. [Google Scholar]
- 5. Hoffman SJ, Robertson CL, Shannon PJet al. Physical correlates of torture exposure in Karen refugees. J Loss Trauma 2017; 22(2): 135–49. [Google Scholar]
- 6. van der Kolk BA. The body keeps the score: memory and the evolving psychobiology of posttraumatic stress. Harv Rev Psychiatry 1994; 1(5): 253–65. [DOI] [PubMed] [Google Scholar]
- 7. Steel Z, Chey T, Silove Det al. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA 2009; 302(5): 537–49. [DOI] [PubMed] [Google Scholar]
- 8. LeMaster JW, Broadbridge CL, Lumley MAet al. Acculturation and post-migration psychological symptoms among Iraqi refugees: a path analysis. Am J Orthopsychiatry 2018; 88(1): 38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rhodes CM, Chang Y, Percac-Lima S. Development of obesity and related diseases in African refugees after resettlement to United States. J Immigr Minor Health 2016; 18(6): 1386–91. [DOI] [PubMed] [Google Scholar]
- 10. Hollander AC, Bruce D, Ekberg Jet al. Longitudinal study of mortality among refugees in Sweden. Int J Epidemiol 2012; 41(4): 1153–61. [DOI] [PubMed] [Google Scholar]
- 11. DesMeules M, Gold J, McDermott Set al. Disparities in mortality patterns among Canadian immigrants and refugees, 1980–1998: results of a national cohort study. J Immigr Minority Health 2005; 7(4): 221–32. [DOI] [PubMed] [Google Scholar]
- 12. Mulugeta W, Xue H, Glick Met al. Burden of mental illness and non-communicable diseases and risk factors for mental illness among refugees in Buffalo, NY, 2004–2014. J Racial Ethn Health Disparities 2019; 6(1): 56–63. [DOI] [PubMed] [Google Scholar]
- 13. Kaltenbach E, Schauer M, Hermenau K, Elbert T, Schalinski I. Course of mental health in refugees-a one year panel survey. Front Psychiatry 2018; 9: 352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Campbell MR, Mann KD, Moffatt S, Dave M, Pearce MS. Social determinants of emotional well-being in new refugees in the UK. Public Health 2018; 164: 72–81. [DOI] [PubMed] [Google Scholar]
- 15. Tingvold L, Vaage AB, Allen Jet al. Predictors of acculturative hassles among Vietnamese refugees in Norway: results from a long-term longitudinal study. Transcult Psychiatry 2015; 52(5): 700–14. [DOI] [PubMed] [Google Scholar]
- 16. Morville AL, Amris K, Eklund M, Danneskiold-Samsøe B, Erlandsson LK. A longitudinal study of changes in asylum seekers ability regarding activities of daily living during their stay in the asylum center. J Immigr Minor Health 2015; 17(3): 852–9. [DOI] [PubMed] [Google Scholar]
- 17. Mölsä M, Kuittinen S, Tiilikainen M, Honkasalo ML, Punamäki RL. Mental health among older refugees: the role of trauma, discrimination, and religiousness. Aging Ment Health 2017; 21(8): 829–37. [DOI] [PubMed] [Google Scholar]
- 18. Shannon, PJVinson GA, Horn TL, Lennon E. Defining effective care coordination for mental health referrals of refugee populations in the United States. Ethnicity Health 2018; 1–19. 10.1080/13557858.2018.1547369 [DOI] [PubMed] [Google Scholar]
- 19. Esala JJ, Hudak L, Eaton A, Vukovich M. Integrated behavioral health care for Karen refugees: a qualitative exploration of active ingredients. Int J Migrat Health Social Care 2018; 14(2): 133–45. [Google Scholar]
- 20. SAS Institute. Base SAS 9.4 Procedures Guide. SAS Institute; 2015. [Google Scholar]
- 21. Lin CE, Chung CH, Chen LFet al. Risk of incident hypertension, diabetes, and dyslipidemia after first posttraumatic stress disorder diagnosis: a nationwide cohort study in Taiwan. Gen Hosp Psychiatry 2019; 58: 59–66. [DOI] [PubMed] [Google Scholar]
- 22. Hung YH, Cheng CM, Lin WCet al. Post-traumatic stress disorder and asthma risk: a nationwide longitudinal study. Psychiatry Res 2019; 276: 25–30. [DOI] [PubMed] [Google Scholar]
- 23. Kumari R, Mukhopadhyay A. Psychological trauma and resulting physical illness: a review. SIS J Projective Psychol Mental Health. 2020; 27(2): 98–104. [Google Scholar]
- 24. Health of Asian or Pacific Islander Population . National Center for Health Statistics. 2018. https://www.cdc.gov/nchs/fastats/asian-health.htm (accessed on 10 January 2020).
- 25. Gordon NP, Lin TY, Rau J, Lo JC. Aggregation of Asian-American subgroups masks meaningful differences in health and health risks among Asian ethnicities: an electronic health record based cohort study. BMC Public Health 2019; 19(1): 1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. National Institute on Minority Health and Health Disparities. The Center for Asian Health Engages Communities in Research to Reduce Asian American Health Disparities. 2016. https://www.nimhd.nih.gov/news-events/features/training-workforce-dev/center-asianhealth.html (accessed on 10 January 2020).
- 27. Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today 2015; 50(3): 117–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Who EC. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. London, England: Lancet; 2004; 363(9403): 157. [DOI] [PubMed] [Google Scholar]
- 29. Careyva B, LaNoue M, Bangura Met al. The effect of living in the United States on body mass index in refugee patients. J Health Care Poor Underserved 2015; 26(2): 421–30. [DOI] [PubMed] [Google Scholar]
- 30. Mulugeta W, Glick M, Min Jet al. Longitudinal changes and high-risk subgroups for obesity and overweight/obesity among refugees in Buffalo, NY, 2004–2014. J Racial Ethn Health Disparities 2018; 5(1): 187–94. [DOI] [PubMed] [Google Scholar]
- 31. Sandell AMD, Baker RD, Maccarone J, Baker SS. Health status and anthropometric changes in resettled refugee children. J Pediatr Gastroenterol Nutr 2017; 65(5): 569–73. [DOI] [PubMed] [Google Scholar]
- 32. Zwi K, Woodland L, Williams Ket al. Protective factors for social-emotional well-being of refugee children in the first three years of settlement in Australia. Arch Dis Child 2018; 103(3): 261–8. [DOI] [PubMed] [Google Scholar]
- 33. Olson BG, Kurland Y, Rosenbaum PF, Hobart TR. Rapid weight gain in pediatric refugees after US immigration. J Immigr Minor Health 2017; 19(2): 263–6. [DOI] [PubMed] [Google Scholar]
- 34. Dawson-Hahn E, Pak-Gorstein S, Matheson Jet al. Growth trajectories of refugee and nonrefugee children in the United States. Pediatrics 2016; 138(6): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Karl JP, Hatch AM, Arcidiacono SMet al. Effects of psychological, environmental and physical stressors on the gut microbiota. Front Microbiol 2018; 9: 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vangay P, Johnson AJ, Ward TLet al. US immigration westernizes the human gut microbiome. Cell 2018; 175(4): 962–972.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Treatment Schedules for Presumptive Parasitic Infections . https://www.cdc.gov/immigrantrefugeehealth/guidelines/overseas/interventions/interventions.html (accessed on 10 January 2020).
- 38. Quach DT, Vilaichone RK, Vu KVet al. Helicobacter pylori infection and related gastrointestinal diseases in southeast Asian countries: an expert opinion survey. Asian Pac J Cancer Prev 2018; 19(12): 3565–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shannon PJ. Refugees’ advice to physicians: how to ask about mental health. Fam Pract 2014; 31(4): 462–6. [DOI] [PubMed] [Google Scholar]
- 40. Miller KE, Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. Soc Sci Med 2010; 70(1): 7–16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, SH, upon reasonable request.