Abstract
We sought to gain insights into the impacts of COVID-19 and associated control measures on health and health care of patients from low- and middle-income countries with cardiovascular disease, diabetes, and mental health conditions, using an online survey during the COVID-19 pandemic. The most common concern for the 1487 patients who took part was contracting COVID-19 when they accessed health care. Of those infected with COVID-19, half said that their health had been worse since being infected. Collectively, most people reported an increase in feelings of stress and loneliness. The COVID-19 pandemic has led to a range of health care impacts on patients with noncommunicable diseases, including constraints on access to care and health effects, particularly mental well-being.
Keywords: patient perspectives, diabetes mellitus, cardiovascular disease, depression, anxiety, survey, COVID-19
Introduction
The COVID-19 pandemic has impacted millions of lives, with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus infecting more than 175 million people worldwide (as of June 13, 2021) and causing more than 3.7 million deaths (1). People living with noncommunicable diseases (NCDs) are at higher risk of developing severe COVID-19-related illness and death (2). Noncommunicable diseases kill an estimated 41 million people each year, and more than 85% of premature deaths due to NCDs occur in low- and middle-income countries (LMICs) (3).
Primary care services, such as community health providers, family health practices (general practices), and pharmacies, are essential for delivering frontline primary care for patients with NCDs in LMICs (4). During emergencies and pandemics, primary care services may become overwhelmed, compromising routine care provision and ongoing NCDs management (5). With COVID-19 case numbers increasing daily by the thousands in some countries (1), prevention and management of new cases presents a huge challenge for already stretched and underresourced health care systems in many LMICs. Consequently, not only are people with NCDs more vulnerable to becoming seriously ill if infected with the SARs-CoV-2 virus (2) but also may be unable to access treatment to manage their illnesses due to the increased burden of the pandemic on health resources.
Previous emergencies and pandemics have disrupted the ability to meet the essential needs of NCD patients (6,7). Evacuation of large populations and destruction of health infrastructure by Hurricane Katrina emphasized the vulnerability of NCD management during disasters in a wealthy nation like the United States (6). More recently, major disasters in Lebanon (8) and Japan (7) have demonstrated that critical gaps remain in managing both individual adherence and the ongoing supply of essential medications, and in maintaining regular visits and treatment of NCDs during disasters. Communicable disease outbreaks have contributed to lower rates of clinic attendance by patients (9,10) and lower medication adherence (5). Health care systems have reported similar findings since the advent of the COVID-19 pandemic (11,12), especially in LMICs (13,14), where the impact of the pandemic is more pronounced (15) due to preexisting health care weaknesses and economic disparities (16).
In a recent survey conducted by the World Health Organization (WHO), Ministries of Health reported that the COVID-19 pandemic had severely disrupted prevention and treatment services for NCDs (17). Seventy-five percent of the 163 countries surveyed reported service disruptions due to the pandemic. The most common reasons for discontinuing or reducing services were cancellations of planned treatments, closure of population-based screening programs, decrease in public transport availability, and a lack of staff because of health workers being reassigned to support COVID-19 services. Although the WHO survey also found that many countries had used alternative strategies to help the continuity of care for NCDs, it is unclear what impact these strategies have on patient care. Research to date has been high level (12,13,17) and fails to capture insights into the day-to-day effects of COVID-19 on the lives of patients with NCDs in LMICs and countries with high NCD burdens.
Aim
To gain insights into the impacts of COVID-19 on the health and health care of patients with NCDs in a selection of countries with high NCD burdens.
Methods
Design
We developed an online survey alongside a survey of health care workers and with reference to previous surveys conducted during disease outbreaks and natural disasters (18,19). The survey included questions about the personal impacts of COVID-19 on their health status and lifestyle and about respondents’ health care–seeking behaviors.
Study Population
Patients were eligible to participate if they were ≥18 years, had one or more NCD, and lived in one of the selected countries in the following 3 regions: Association of Southeast Asian Nations (ASEAN): Malaysia, Thailand, Philippines; Africa and the Middle East (AFME): Gulf Cooperation Council, Egypt, South Africa; and Latin America (LATAM): Brazil, Mexico, Argentina. We pragmatically selected countries from all those fitting an archetype defined by high NCD burden and varying degrees of readiness to combat NCDs (20). Most were LMICs but we also included the Gulf Cooperation Council, a group of high-income countries that have a high NCD burden and inadequate preparedness to combat NCDs, consistent with the LMIC archetype (20). We aimed to recruit 250 participants from each country.
Methods
We recruited respondents through an invitation to participate administered via the International Alliance of Patient Organizations, and their offices and partner organizations in each country. We invited potential respondents by email and through social media posts sent through patient advocacy groups and NCDs alliances. The survey was distributed between September 21, 2020, and November 2, 2020, and was available in English and 5 other languages: Thai, Arabic, Portuguese, Spanish, and Malay. We obtained ethical approval from the Auckland Health Research Ethics Committee (Ref: AH3064). We collected data on patient demographic characteristics (age, sex, country), diagnosed NCDs, and health status before and during COVID-19.
Statistical Analysis
We used the SAS software package version 9.4 (Copyright© SAS Institute Inc) for data analyses. We summarized demographic information as frequencies for categorical variables and means (standard deviation) for continuous variables, and further summarized by location. We compared categorical variables, using χ2 tests to assess statistical significance (P ≤ .05).
Results
Demographic Information
One thousand four hundred and eighty-seven patients responded to the survey. The mean age was 43.9 years (SD = 15.9), and two-thirds (66.6%) were female (Table 1). The largest proportions of respondents came from Argentina (37.0%), followed by Thailand (18.0%). As shown in Table 1, the most frequently reported conditions were diabetes (59.7%), high blood pressure (26.5%), and “other chronic condition” (23.4%). High blood pressure was the most reported condition by respondents from the Philippines (59.1%) and “other chronic condition” for South Africa (57.7%) and Thailand (46.1%).
Table 1.
Patient Demographic Characteristics by Country Summarized by Frequency (%).
| Characteristics | Variables | Thailand (n = 267) | Philippines (n = 110) | GCC (n = 77) | Egypt (n = 48) | South Africa (n = 97) | Brazil (n = 120) | Mexico (n = 197) | Argentina (n = 550) |
|---|---|---|---|---|---|---|---|---|---|
| Age | Mean (SD) | 46.6 (12.5) | 53.4 (12.5) | 43.6 (12.0) | 43.9 (13.1) | 47.5 (11.3) | 50.2 (17.8) | 40.2 (18.8) | 39.9 (16.2) |
| Sex | Male | 98 (36.7) | 35 (31.8) | 27 (35.1) | 24 (50.0) | 15 (15.5) | 30 (25.0) | 77 (39.1) | 166 (30.2) |
| Female | 169 (63.3) | 73 (66.4) | 49 (63.6) | 24 (50.0) | 82 (84.5) | 90 (75.0) | 118 (59.9) | 380 (69.1) | |
| Prefer not to answer | - | - | - | - | - | - | 1 (0.5) | 3 (0.5) | |
| Chronic condition | High blood pressure | 68 (25.5) | 65 (59.1) | 28 (36.4) | 28 (58.3) | 26 (26.8) | 38 (31.7) | 51 (25.9) | 89 (16.2) |
| High/raised cholesterol | 29 (10.9) | 24 (21.8) | 14 (18.2) | 21 (43.8) | 18 (18.6) | 22 (18.3) | 17 (8.6) | 68 (12.4) | |
| Cardiovascular disease | 17 (6.4) | 10 (9.1) | 14 (18.2) | 8 (16.7) | 2 (2.1) | 6 (5.0) | 5 (2.5) | 23 (4.2) | |
| Diabetes | 29 (10.9) | 37 (33.6) | 50 (64.9) | 30 (62.5) | 9 (9.3) | 70 (58.3) | 169 (85.8) | 489 (88.9) | |
| Depression | 15 (5.6) | 5 (4.5) | 3 (3.9) | - | 40 (41.2) | 10 (8.3) | 6 (3.0) | 14 (2.5) | |
| Anxiety | 6 (2.2) | 6 (5.5) | 3 (3.9) | 2 (4.2) | 25 (25.8) | 15 (12.5) | 8 (4.1) | 24 (4.4) | |
| Other chronic conditions | 123 (46.1) | 15 (13.6) | 27 (35.1) | 16 (33.3) | 56 (57.7) | 22 (18.3) | 13 (6.6) | 75 (13.6) | |
| Frequency of GP visits in 6 months before COVID-19 | More than once a month | 30 (11.2) | 3 (2.7) | 4 (5.2) | 3 (6.3) | 4 (4.1) | 3 (2.5) | 9 (4.6) | 25 (4.5) |
| Once a month | 49 (18.4) | 13 (11.8) | 40 (51.9) | 14 (29.2) | 5(5.2) | 9 (7.5) | 94 (47.7) | 110 (20.0) | |
| Every other month | 107 (40.1) | 22 (20.0) | 9 (11.7) | 5 (10.4) | 18 (18.6) | 25 (20.8) | 30 (15.2) | 134 (24.4) | |
| Twice | - | 16 (14.5) | 15 (19.5) | 15 (31.3) | 17 (17.5) | 16 (13.3) | 29 (14.7) | 119 (21.6) | |
| Once | - | 29 (26.4) | 5 (6.5) | 11 (22.9) | 37 (38.1) | 56 (46.7) | 21 (10.7) | 118 (21.5) | |
| Never | 63 (23.6) | 27 (24.5) | 2 (2.6) | - | 16 (16.5) | 11 (9.2) | 12 (6.1) | 43 (7.8) | |
| Rating of overall health in 6 months before COVID | Excellent | 20 (7.5) | 5 (4.5) | 1 (1.3) | 1 (2.1) | 8 (8.2) | 15 (12.5) | 7 (3.6) | 38 (6.9) |
| Very good | 46 (17.2) | 39 (35.5) | 3 (3.9) | - | 21 (21.6) | 49 (40.8) | 49 (24.9) | 239 (43.5) | |
| Good | 129 (48.3) | 50 (45.5) | 60 (77.9) | 30 (62.5) | 32 (33.0) | 40 (33.3) | 103 (52.3) | 209 (38.0) | |
| Fair | 39 (14.6) | 15 (13.6) | 10 (13.0) | 15 (31.3) | 30 (30.9) | 10 (8.3) | 35 (17.8) | 54 (9.8) | |
| Poor | 30 (11.2) | 1 (0.9) | 1 (1.3) | 2 (4.2) | 5 (5.2) | 6 (5.0) | 3 (1.5) | 9 (1.6) | |
| Rating of overall health today | Excellent | 12 (4.5) | 6 (5.5) | - | - | 8 (8.2) | 13 (10.8) | 7 (3.6) | 30 (5.5) |
| Very good | 52 (19.5) | 35 (31.8) | 8 (10.4) | 2 (4.2) | 14 (14.4) | 48 (40.0) | 43 (21.8) | 164 (29.8) | |
| Good | 144 (53.9) | 46 (41.8) | 53 (68.8) | 28 (58.3) | 33 (34.0) | 37 (30.8) | 89 (45.2) | 236 (42.9) | |
| Fair | 32 (12.0) | 19 (17.3) | 15 (19.5) | 15 (31.3) | 32 (33.0) | 20 (16.7) | 54 (27.4) | 103 (18.7) | |
| Poor | 25 (9.4) | 4 (3.6) | 1 (1.3) | 3 (6.3) | 10 (10.3) | 2 (1.7) | 4 (2.0) | 16 (2.9) |
Most respondents rated their overall health status as positive (good, very good, or excellent) both in the 6 months before COVID-19 (80.6%) and at the time of the survey (74.6%; Table 1). Health status ratings in the 6 months before COVID-19 were highest in Argentina (88.6%) and Brazil (86.6%) and lowest in Egypt (64.6%) and South Africa (62.8%); current health status ratings were highest in Brazil (81.6%) and Argentina (78.2%), and lowest in Egypt (62.5%) and South Africa (56.6%).
Fewer than 30% reported visiting their GP once or more a month before COVID-19, and 11.8% reported that they did not visit their GP in the 6 months before COVID-19. We observed significant regional differences (P < .001): almost one-quarter of respondents from ASEAN reported no visits to their GP in the 6 months before COVID-19, compared to only 8% in AFME and LATAM.
Personal Impact of COVID-19
Most respondents (57.0%) reported that there was no change in their chronic health condition in the last 4 weeks, while similar proportions reported that their condition was worse (19.0%) or better (19.4%). There were significant differences between regions (P = .001): fewer respondents in the ASEAN region reported that their chronic condition had worsened (9.3%), whereas fewer respondents in the AFME region reported that their condition was better (4.8%). Just over half of them reported that their chronic condition was about the same since the COVID-19 pandemic (51.4%). Still, more than one-third (33.3%) reported that their condition was harder to manage, and 10.3% reported that it was easier to manage. There were significant differences by region (P < .001). In AFME, 75% of respondents reported no change in condition or management, while 41.3% of LATAM respondents reported that controlling their condition was more challenging.
Five percent of respondents reported that they had been infected or became ill with COVID-19. Of those infected, half noted that their chronic condition was worse since being infected with COVID-19, 43.8% reported no change, and 6.3% said their condition was better.
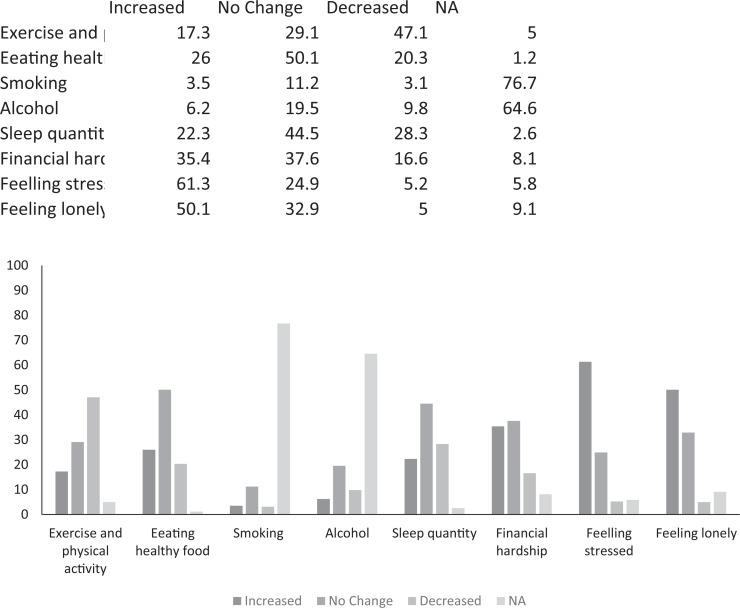
Lifestyle Changes
Almost half of the respondents (47.1%) reported that exercise and physical activity had decreased, while half (49.8%) stated that there had been no change in consumption of healthy food since the onset of the pandemic (Figure 1). Alcohol and smoking were not relevant for most participants (60.8% and 76.5%, respectively); where relevant, most reported that there had been no change in these behaviors (Figure 1). Almost half (44.5%) of respondents reported no change in sleep quantity, with 28.3% indicating their sleep quantity had deteriorated. Similar proportions reported no change, or an increase, in financial hardship (37% and 35.5%, respectively).
Figure 1.
Patients reports of change in lifestyle factors.
Most respondents reported that feelings of stress had increased (61.5%), and half (50.1%) indicated that feelings of isolation or loneliness had increased (Figure 1). Increased feelings of stress and isolation or loneliness were less pronounced in Thailand (48.7% and 21.7%, respectively), Philippines (54.5% and 39.1%), and GCC (35.1% and 36.4%). The proportion of respondents reporting increased financial hardship was highest in Egypt (62.5%), and the proportion reporting decreased physical activity and exercise was greatest in LATAM (57.8%) countries.
Health Care–Seeking Behaviors
Most respondents reported they had seen a health care professional either in person or remotely (ie, via telehealth) during the pandemic (63.0%), although this differed considerably by region: most respondents had not seen a health care professional in Egypt (83.3%), and GCC (81.8%). Fewer than 10% had been hospitalized (visited an emergency department or admitted to a hospital) to manage their NCD, during the COVID-19 pandemic.
Sixteen percent of respondents reported that they had missed a dose or prescription, and 31.1% said they had difficulty accessing a routine visit relating to their NCD since the COVID-19 pandemic. Of those who experienced problems accessing a regular visit, about two-thirds (60.0%) reported that they had had difficulty seeing a family doctor or GP. There was no significant difference in patients reporting missed prescriptions or clinic visits across regions or countries (P > .05). The most common reasons for missing a medication dose were forgetting (28.1%) and fear about contracting COVID-19 (20.4%). The most frequently endorsed reasons for missing a routine visit were fear of contracting COVID-19 (36.5%), being told not to attend by the doctor or clinic (33.7%), and being unable to access the clinic due to lockdown orders or quarantine (27.0%). Overall, the most common alternative to face-to-face consultations was telephone consultation (32.2%), although this varied significantly by region (P < .001). Between the ASEAN, LATAM, and AFME regions, the most common alternative methods were telephone consultation (23.8%), e-prescriptions (41.6%), and home-delivered medication (47.3%), respectively.
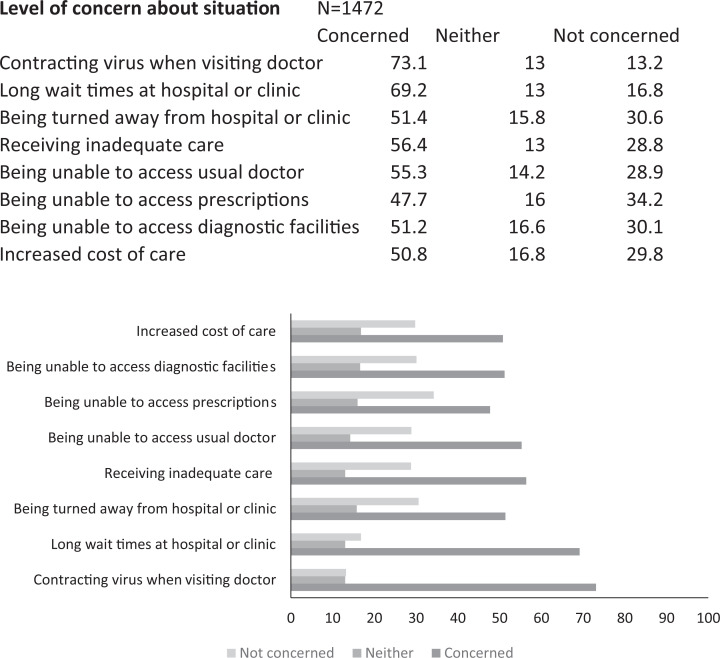
When asked about their level of concern about a variety of situations during the COVID-19 outbreak (Figure 2), most respondents reported feeling somewhat or very concerned about contracting COVID-19 if they needed to get unrelated care from their doctor (70.9%), and long wait times at a hospital or clinic (66.8%). The lowest reported concern was being unable to access prescriptions (45.7%). Although the number of participants in some regions was insufficient to draw any strong inferences, we noted differences between regions for all the concerns. The AFME region had the highest proportions of respondents reporting being “very concerned” about contracting COVID-19 when they needed to get care from their doctor (54.8% vs ASEAN 33.1% and LATAM 33.3%), long wait times (52.5% vs ASEAN 27.8% and LATAM 39.4%), being turned away (42.8% vs ASEAN 14.3% and LATAM 26.4%), and increased cost of care (40.5% vs ASEAN 21.7% and LATAM 31.1%).
Figure 2.
Patients level of concern about situations during COVID-19 pandemic.
Discussion
To the best of our knowledge, this is the first study to present the patients’ perspective on the impact of COVID-19 on patients with NCDs in LMICs and countries with a high NCD burden. The study is also unique in recruiting patients through patient advocacy organizations rather than through health care providers. Previous studies investigating the impacts of COVID-19 on NCD care have focused solely on the health care worker perspective (13,14). Also, the high numbers of participants in some countries will enable subsequent detailed analyses.
However, there were several limitations. Firstly, we used an online survey to collect data. The denominator population (the number of potential respondents) is, therefore, unknown. Secondly, by using convenience and opportunistic sampling methods, we may have missed responses from some groups. We sent the surveys to a pool of potential participants with a specific condition (ie, patient groups for diabetes, depression, etc), so our sample does not reflect the prevalence of those conditions in each country. For example, there was an apparent oversampling of patients with diabetes. Likewise, our respondents may be limited to those with better access to internet infrastructure and more experience with online surveys. These features limit the generalizability of the findings. Thirdly, our target was 250 respondents in each country, but we could only attain the target for 2 countries (Argentina and Thailand). Finally, the survey relied on unvalidated self-reporting of symptom severity or change in condition rather than objective measures (eg, self-monitoring). Patients were asked to reflect on health in the last 4 weeks to limit recall bias, but this may limit the extent to which change in symptoms could be detected.
Bringing the patient lens to bear reveals the lived experience of patients with COVID-19. Around 1 in 20 patients reported having been infected with COVID-19. Most patients who had become infected with COVID-19 perceived that their chronic condition had deteriorated. Similar proportions of patients reported no change in their NCD in the last month as reported that their condition was better. In contrast, a greater proportion of respondents said their condition was harder to manage compared to those reporting that it was easier to manage. Further analysis indicated significant differences in changes and management of NCDs by region, particularly between the ASEAN and LATAM regions. These geographic differences in condition and management could reflect different government responses to COVID-19 and the differing levels of lockdown. However, they do not appear to be reflected in the stringency of public health measures as reported by the Oxford COVID-19 Government Response Tracker (21). A more plausible explanation is that the ability to manage NCDs differs by type of NCD, and the most common NCD reported by respondents varied by country due to the different patient networks publicizing the study in each country.
Many patients reported that they had difficulty accessing routine health care visits and missed doses of medicines or visits. A survey of frontline health care workers in LMICs reported fewer NCD patient visits to clinics since the COVID-19 pandemic began (22). When asked why this was, over half the physicians and pharmacists responded that patients were reluctant to visit clinics (22). This finding is consistent with those of our survey, where the main reason for missing visits and one of the main reasons for missing medications was the fear of contracting COVID-19. Difficulty accessing routine health care visits due to infection control measures (eg, lockdown) was exacerbated by patients’ reluctance to visit health care settings due to fear of infection. The impact of COVID-19 has likely worsened since our survey, with the emergence of new, more transmissible variants of COVID-19 and many nations returning to more restrictive public health measures (23).
Around 1 in 10 patients reported that they had not visited their GP in the 6 months before the COVID-19 pandemic began, suggesting the presence of long-standing unaddressed gaps in care. This finding is especially concerning because more than half of all patients reported having diabetes, a condition that requires at least annual monitoring by a health care worker (24). Alarmingly, most patients indicated that COVID-19 had impacted their mental health adversely in terms of increased feelings of stress and loneliness since the pandemic. These results are similar to those from high-income countries where levels of stress, anxiety, and depression have increased, and levels of exercise and physical activity have decreased (25,26). Public health measures frequently included recommendations for self-isolation for individuals with NCDs due to increased vulnerability, thus leading to reduced social interactions and increased feelings of loneliness and isolation (12), factors that have been associated with increased NCD risk, especially cardiovascular disease and stroke (27). There is a compelling case to be made for promoting exercise and physical activity interventions as a means of coping with increased levels of stress and depression during lockdowns—notwithstanding limitations on the ability to exercise outdoors. Future research is needed to consider how LMICs can support and promote greater engagement of patients with NCDs in physical activity during times of increased stress and anxiety. Of note, while research in high-income countries has shown an increase in alcohol and tobacco consumption (28), many of our respondents appeared to be nondrinkers and nonsmokers.
Some findings were remarkably consistent across countries. For instance, the most prominent concerns for patients during the COVID-19 outbreak were contracting COVID-19 when they needed to visit a doctor for unrelated care, and long wait times at the hospital or clinic. Around half of all patients were concerned about being unable to access prescriptions. With high levels of stress and anxiety reported by those respondents during the COVID-19 pandemic, concern about contracting the virus is not unexpected, especially for those in high-risk categories like people with NCDs (29). The patients’ ability to have routine checkups and fill prescriptions is vital to the ongoing high-quality care of NCDs patients. Community pharmacists in LMICs have been able to continue delivering critical services to NCD patients during the COVID-19 pandemic (30). If pharmacists were empowered to do some of the health care tasks or services for NCD patients traditionally provided by physicians, the burden on physicians could be reduced (31).
Future research should investigate how to improve the care of these patients, potentially by expanding the use of technology (eg, such as e-prescriptions and telehealth consultations) the use of which varied by country. As noted, the role of community pharmacists in a clinical context in LMICs during such crises should be strengthened. Community pharmacists are increasingly involved in patient care beyond medicine dispensing, including monitoring of blood pressure, blood lipids or glucose, patient counseling, education on disease management, and medication adherence (32,33). The potential to strengthen community pharmacists’ role is especially pertinent given the upcoming rollout of the COVID-19 vaccines and the additional burden this will place on health care systems and face-to-face health services already disrupted by the pandemic.
Conclusion
In summary, our study sheds light on a range of issues for patients with NCDs in LMICs. Despite the challenges faced, most patients have demonstrated resilience and an ability to adapt to challenging circumstances during the COVID-19 pandemic. However, mental health support is critical, and maintaining access to services and medications is vital to sustaining patients with NCDs in the face of obstacles presented by pandemics and other emergencies.
Acknowledgments
The authors acknowledge the following organizations for their support in distributing the survey to patients: Association for the Care of Diabetes in Argentina; Federacion Mexican de Diabetes; International Diabetes Federation; Heart to Heart Foundation; Philippine Alliance of Patient Organizations; Multiple Sclerosis South Africa; Egyptian NCD Alliance; Eastern Mediterranean NCD Alliance; International Alliance of Patient Organizations.
Authors’ Note: This research was approved by the Auckland University Human Ethics Committee (Ref: AH3064). All procedures in this research were conducted in accordance with the Auckland University Human Ethics Committee (Ref: AH3064) approved protocols. Online consent was obtained from the patients for their anonymized information to published in this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: K.S., A.M., and P-.H.H. are employees of Viatris.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by Viatris (formerly Upjohn, a Division of Pfizer).
ORCID iDs: Ratna Devi  https://orcid.org/0000-0002-9817-3836
https://orcid.org/0000-0002-9817-3836
Jessica McCormack  https://orcid.org/0000-0002-6389-9610
https://orcid.org/0000-0002-6389-9610
Amanda Calder  https://orcid.org/0000-0002-0948-2224
https://orcid.org/0000-0002-0948-2224
Pai-Hui Huang  https://orcid.org/0000-0001-6782-8011
https://orcid.org/0000-0001-6782-8011
References
- 1. World Health Organization. WHO coronavirus disease (COVID-19) dashboard. 2020. Accessed July 14, 2021. https://covid19.who.int/
- 2. World Health Organization. Report of WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). World Health Organization; 2020. [Google Scholar]
- 3. World Health Organization. Noncommunicable diseases. 2018. Accessed August 24, 2020. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- 4. Joint Learning Innitiative. Human Resources for Health: Overcoming the Crisis. Global Equity Initiative, Havard University; 2004. [Google Scholar]
- 5. Ochi S, Hodgson S, Landeg O, Mayner L, Murray V. Disaster-driven evacuation and medication loss: a systematic literature review. PLoS Curr. 2014;6:ecurrents.dis.fa417630b417566a417630c417637dfdbf945910edd417696. doi:10.1371/currents.dis.fa417630b566a0c7dfdbf945910edd96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Horn RB, Kirsch TD. Disaster response 2.0: noncommunicable disease essential needs still unmet. Am J Public Health. 2018;108:S202–S203. doi:10.2105/AJPH.2018.304604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Murakami A, Sasaki H, Pascapurnama DN, Egawa S. Noncommunicable diseases after the great east japan earthquake: systematic review, 2011-2016. Disaster Med Public Health Prep. 2018;12:396–407. doi:10.1017/dmp.2017.63 [DOI] [PubMed] [Google Scholar]
- 8. Devi S. Lebanon faces humanitarian emergency after blast. Lancet. 2020;396:456. doi:10.1016/S0140-6736(20)31750-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kelly B, Squiers L, Bann C, Stine A, Hansen H, Lynch M. Perceptions and plans for prevention of Ebola: results from a national survey. BMC Public Health. 2015;15:1136. doi:10.1186/s12889-015-2441-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chang H-J, Huang N, Lee C-H, Hsu YJ, Hsieh CJ, Chou YJ. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004;94:562–564. doi:10.2105/ajph.94.4.562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Prescott K, Baxter E, Lynch C, Jassal S, Bashir A, Gray J. COVID-19: how prepared are front-line healthcare workers in England? J Hosp Infect. 2020;105:142–145. doi:10.1016/j.jhin.2020.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Palmer K, Monaco A, Kivipelto M, Onder G, Maggi S, Michel JP, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. 2020;32:1189–1194. doi:10.1007/s40520-020-01601-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Siedner MJ, Kraemer JD, Meyer MJ, Harling G, Mngomezulu T, Gabela P, et al. Access to primary healthcare during lockdown measures for COVID-19 in rural South Africa: an interrupted time series analysis. BMJ Open. 2020;10:e043763. doi:10.1136/bmjopen-2020-043763% [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sharma SK, Mudgal SK, Sharma P. Healthcare professionals preparedness for COVID-19 pandemic: a cross-sectional survey in Northern India. Natl J Community Med. 2020;11:248–253. [Google Scholar]
- 15. Slama S, Kim H-J, Roglic G, Boulle P, Hering H, Varghese C, et al. Care of non-communicable diseases in emergencies. Lancet. 2017;389:326–330. doi:10.1016/S0140-6736(16)31404-0 [DOI] [PubMed] [Google Scholar]
- 16. Allotey P, Davey T, Reidpath DD. NCDs in low and middle-income countries—assessing the capacity of health systems to respond to population needs. BMC Public Health. 2014;14:S1. doi:10.1186/1471-2458-14-S2-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment. Geneva. 2020. Accessed July 14, 2021. https://www.who.int/teams/noncommunicable-diseases/covid-19
- 18. Muruganandam P, Neelamegam S, Menon V, Alexander J, Chaturvedi SK. COVID-19 and severe mental illness: impact on patients and its relation with their awareness about COVID-19. Psychiatry Res. 2020;291:113265. doi:10.1016/j.psychres.2020.113265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tomio J, Sato H, Mizumura H. Interruption of medication among outpatients with chronic conditions after a flood. Prehosp Disaster Med. 2010;25:42. doi:10.1017/s1049023x00007652 [DOI] [PubMed] [Google Scholar]
- 20. Pfizer Upjohn. Leading the conversation on noncommunicable diseases worldwide: an evidence-based review of key research and strategies to develop sustainable solutions. Upjohn. 2020. Accessed July 14, 2021. https://cdn.pfizer.com/pfizercom/Upjohn_NCD_White_Paper-24JAN2020.pdf
- 21. Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav. 2021;5:529–538. doi:10.1038/s41562-021-01079-8 [DOI] [PubMed] [Google Scholar]
- 22. Bullen C, McCormack JC, Calder A, Parag V, Subramaniam K, Majumdar A, et al. The impact of COVID-19 on the care of people living with non-communicable diseases in low- and middle-income countries: an online survey of frontline healthcare workers in nine countries. Primary Health Care Res Dev. 2021; doi:10.1017/S146342362100030X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kirby T. New variant of SARS-CoV-2 in UK causes surge of COVID-19. Lancet Respir J. 2021;9:E20–E21. doi:10.1016/S2213-2600(21)00005-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Diabetes New Zealand. Annual diabetes check-up. 2020. Accessed July 14, 2021. https://www.diabetes.org.nz/diabetes-check-ups
- 25. Carroll N, Sadowski A, Laila A, Hruska V, Nixon M, Ma DWL, et al. The impact of COVID-19 on health behavior, Stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12:2352. doi:10.3390/nu12082352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, et al. A nationwide survey of psychological distress among italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17:3165. doi:10.3390/ijerph17093165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102:1009–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stanton R, , To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. Int J Environ Res Public Health. 2020;17:4065. doi:10.3390/ijerph17114065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization. NCDs, mental health and COVID-19. 2020.
- 30. International Pharmaceutical Federation. COVID-19: Guidelines for Pharmacists and the Pharmacy Workforce. The Hauge, International Pharmaceutical Federatoin; 2020. [Google Scholar]
- 31. Ganju A, Goulart AC, Ray A, Majumdar A, Jeffers BW, Llamosa G, et al. Systemic solutions for addressing non-communicable diseases in low- and middle-income countries. J Multidiscip Healthc. 2020;13:693–707. doi:10.2147/JMDH.S252300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mossialos E, Courtin E, Naci H, Benrimoj S, Bouvy M, Farris K, et al. From “retailers” to health care providers: transforming the role of community pharmacists in chronic disease management. Health Policy. 2015;119:628–39. [DOI] [PubMed] [Google Scholar]
- 33. International Pharmaceutical Federation (FIP). The role of pharmacists in non-communicable diseases. The Hague, International Pharmaceutical Federation; 2019. Accessed July 14, 2021. https://www.fip.org/file/4338 [Google Scholar]