Abstract
Known gaps exist between what patients value and institutions prioritize. We sought to incorporate patients’ reasons for valuing family medicine into a new Mission and Vision statement by deploying brief surveys to a convenience sample of patients. We conducted descriptive quantitative analyses of demographics and inductive content analysis of written responses. Patients returned 92 (20%) of 450 questionnaires. Responders were 63% female, mean age of 47 years. Patients noted distinguishing features of family medicine were (1) continuity of care, (2) all-encompassing care, and (3) trusted referrals. Some patients reported not knowing there was a distinction between family medicine and other primary care.
Keywords: patient voice, patient experience, qualitative research, mission statement
Introduction
A shared mission and vision statement are important to quality care (1,2). Teams that share a common sense of purpose perform better and have greater satisfaction and meaning in their work (3 –5), and incorporation of patients’ experiences into health care delivery is increasingly being recognized as critical to high-value health care (3). Known gaps exist between what patients value and what institutions prioritize (4). Past research has shown that including patients in decisions that impact their health and about how care is designed and delivered can improve patient engagement and outcomes (3,5,6). Involving patients in mission statement development has a significantly positive relationship to institutional performance as it relates to the mission (1).
Due to the transformation of our practice over 15 years, including implementing team-based care, our department desired an updated mission statement that would have meaning for both staff and patients. Our previous mission statement, noted below, did not include teamwork, continuity, or comprehensive care language. All are critical aspects of high performing primary care (7).
The Mayo Clinic Department of Family Medicine is committed to providing the highest quality health care to individuals, families, and the community, and will support its staff in the improvement of services, advancement of medicine, and scholarly activity.
Family medicine is a unique specialty that encompasses care over the entire life spectrum (newborns to seniors) as well as to multiple generations of families. A core value for Family Medicine is relationship-based, patient-centered care, which includes the voice of our patients as partners in the care we provide (7 –10). In keeping with these values, we sought to include patient input during the creation of this updated mission statement.
Method
The Mayo Clinic Family Medicine Department is an academic medical department that cares for 70 000 patients across 5 clinical sites. Scope of practice includes full-spectrum care across the life span for all clinicians. A minority of the clinicians practice maternity care. All clinicians included in this study had a primary panel of patients. Clinician participation was voluntary. This was a quality improvement project, and therefore, IRB approval was not sought. Patients were not identifiable based upon their survey responses.
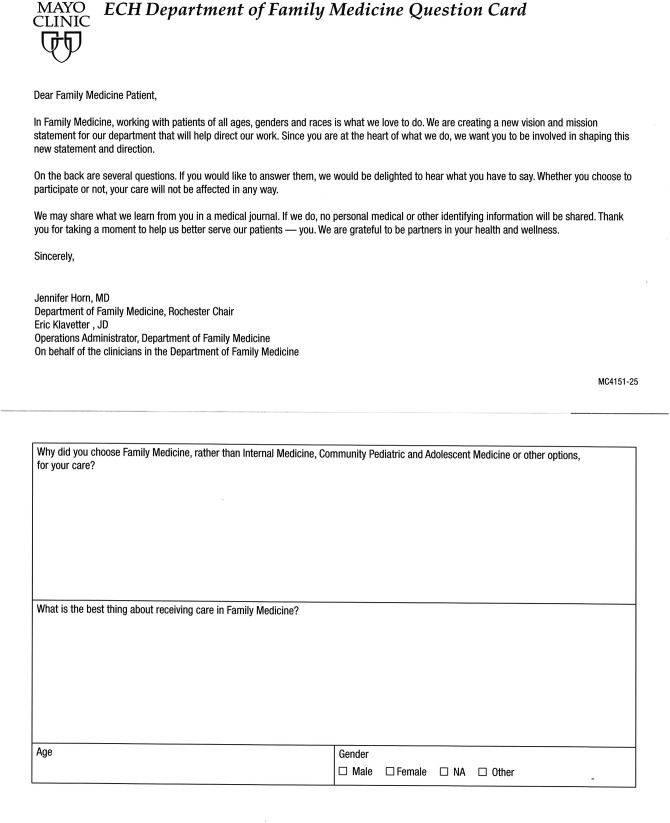
We used a cross-sectional paper patient questionnaire that included 2 open-ended questions and 3 demographic questions (Figure 1). Questionnaires were collected with a convenience sampling approach. Five questionnaires each were given to all Family Medicine clinicians at each site. Practitioners included 60 Medical Doctor/Doctor of Osteopathy and 30 Nurse Practitioner/Physician Assistant clinicians. Clinicians were instructed to distribute the questionnaire to their patients during the outpatient clinic day during a 1-week distribution and collection period. Patients were given a description of the project and a personal invitation to participate. Patient demographics were entered into excel and we conducted descriptive statistical analyses to characterize the sample. Written responses to the open-ended questions were typed verbatim and imported into Nvivo 12 Software. We used conventional qualitative inductive content analysis to summarize patient responses (11). Given the pragmatic and rapid nature of the project, K.B. was the only coder for the data. She read the full data set to get familiarized with the data, and then coded each patient’s answer inductively. Wherever possible, she used patient-provided language to name codes. After the initial round of coding was completed, codes were grouped into categories. For example, the codes “comfort level,” “compassion,” “diligence,” “easy to understand recommendations,” “good care,” “knowledgeable,” and “reassuring” were grouped into a category named “quality of care.” Questions 1 and 2 were tagged separately in the data so responses could be sorted by question. After coding was completed, a summary of the findings was used for the creation of the mission and vision statement.
Figure 1.
Patient questionnaire.
Results
Ninty Family Medicine clinicians were given 450 questionnaires to distribute. Patients returned 92 (20%) questionnaires. Responders were 63% female with a mean age of 47 years. Patients noted that key distinguishing characteristics of care in Family Medicine were (1) continuity of care by the same clinician for the whole family, (2) all-encompassing care across a variety of health care situations, and (3) trusted referrals to specialists. Patients reported the best thing about receiving care in family medicine was (1) the “small town clinic feel,” including being known personally, and (2) friendly staff. Table 1 reflects example quotes from patient questionnaires for each of these themes and subthemes. Some patients reported not knowing there was a distinction between family medicine and other primary care or that their choice was driven by location.
Table 1.
Examples of Patient Quotes From Questionnaire.
| Themes/subthemes | Example patient quotes |
|---|---|
| Distinguishing features of family medicine | |
|
“My entire family can be seen by the same doctor and all of our needs can be taken care of all at once, and the provider knows my family.” “I really wanted to see the same MD throughout pregnancy, labor, and after. I didn’t want to choose a pediatrician and I didn’t want to see a different midwife each appointment with a possibility of needing to change services any.” |
|
“I feel like [physician name] in family medicine knows me and my health concerns so well. I can bring up any question and get a professional answer. She truly knows and keeps track of my family history.” “We like how it can meet all of our needs. They have great staff, and it’s easy to get to. We also like their perspective. They have you do what is best for your child.” |
|
“I like to have the “whole experience” where the doctor is aware of my overall health and all that is related to it. I feel that if things need more attention they will point me in the right direction for ongoing care.” “I’ve been coming to Family Medicine for years. Family Medicine takes care of my needs but will refer me onto specialties if needed.” |
| Best thing about receiving care in family medicine | |
|
“The personal care—I have never felt so comfortable with medical staff before and always feel like I’m the only patient of the day because I never feel rushed.” “[Clinic name] is handy, smaller, and easier to get to. Family medicine is like having a small town doctor who takes care of multiple issues and conditions.” |
|
“Easy access, personal doctors, wonderful nurses and assistants.” “[Physician name] is amazing. She is personal with me and my son. I can reach out to her, and she will respond in a timely manner.” |
Reflective of what we learned from patients, we revised both our mission and vision statements.
Our mission: As a team, we partner with our patients on their care through all stages of life, listening, teaching, and growing with them.
Our vision: To touch our patients throughout their lives with warmth and personalized care based on the highest levels of learning, education, and expertise, partnering with the communities we serve.
Discussion
We used a cross-sectional questionnaire to pragmatically include patients’ voice in developing a new Family Medicine mission statement. Our results highlighted that our statement should include topics that patients value including continuity of care for the whole family across diverse health care needs and the personal team-based connection. This is reflected in the mission statement with words and phrases such as “throughout all stages of life” and “partner.” The accompanying vision statement also reflects these patient priorities in the reference to continuity and the words “warmth,” “personalized,” and “partnering.” Our results also highlight an opportunity to market family medicine as distinguishable from other primary care specialties, and the simplicity of incorporating patient voices into health care delivery design.
Strengths of this project included the ability to incorporate the voices of our patients in the work through the analysis of quotations. The relative simplicity of the design allowed rapid turnover of results to move quickly on the mission/vision statement development process. Flexible and creative processes and the involvement of patients have been associated with both institutional buy-in and improved performance (3).
Limitations
Limitations included minimal demographic and practice information and convenience sampling. Anonymized responses meant we were unable to compare responses by clinician type or scope of practice. Participation was voluntary for both clinician and patients. Although some clinicians embraced the project others were disinterested, which may have contributed to the relatively low response rate.
Biography
Jennifer Horn, MD is an assistant professor in the department of family medicine at Mayo Clinic in Rochester, MN, USA. In addition to practicing Family medicine caring for patients of all ages in the Rochester community she is a practice leader with interests in practice optimization and the provision of high value care for all.
Summer V. Allen, MD is an Assistant Professor in the Department of Family Medicine at the Mayo Clinic, in Rochester, Minnesota. Her family medicine practice includes obstetrical care and focuses on women’s health and patient education. Dr. Allen has research interests which include understanding what it means to engage patients in care, improving their experience with care (including cancer survivorship transition to primary care) and patient care innovation (including minimally disruptive medicine and shared decision making).
Kasey R. Boehmer, PhD, MPH, NBC-HWC is an assistant professor of health services research in the Division of Health Care Delivery Research and Knowledge and Evaluation Research (KER) Unit at Mayo Clinic in Rochester, MN, USA. Her primary research interest is the translation of evidence-based care for patients with chronic conditions into practice in a manner that is consistent with patients’ capacity to access that care and enact self-management. She is an expert in qualitative and mixed methods research, both of which she uses to better understand the patient experience of living with chronic illness.
Jennifer L. Pecina, MD is an associate professor in the Department of Family Medicine at Mayo Clinic in Rochester, MN USA. Her research focuses on telemedicine modalities.
Footnotes
Authors’ Note: Presentations: NAPCRG Annual Meeting, Chicago, IL, 11/12/2019. Mayo Clinic Karolinska Institute Annual Meeting, Stockholm Sweden, 9/23/2019. This project was deemed a quality improvement project and not subject to IRB review. Surveys were collected anonymously and collected information could not be used to identify patients. Informed consent was not obtained because this project was designated as quality improvement.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Mayo Clinic Department of Family Medicine.
ORCID iD: Kasey R. Boehmer, MPH, PhD  https://orcid.org/0000-0002-5637-6803
https://orcid.org/0000-0002-5637-6803
References
- 1. Bart CK, Tabone JC. Mission statements in Canadian not-for-profit hospitals: does process matter? Health Care Manage Rev. 2000;25:45–63. [DOI] [PubMed] [Google Scholar]
- 2. Ginter P, Swayne L, Duncan W. Strategic Management of Health Care Organizations. 3rd ed. Blackwell Business; 1998. [Google Scholar]
- 3. Mohammed K, Nolan MB, Rajjo T, Shah ND, Prokop LJ, Varkey P, et al. Creating a patient-centered health care delivery system: a systematic review of health care quality from the patient perspective. Am J Med Qual. 2016;31:12–21. [DOI] [PubMed] [Google Scholar]
- 4. Nelson WA, Forcino RC, Elwyn G. Patient-centered organizational statements: merely rhetoric? a survey of health care leaders. Health Care Manag (Frederick). 2017;36:342–6. [DOI] [PubMed] [Google Scholar]
- 5. Boivin A, Lehoux P, Lacombe R, Burgers J, Grol R. Involving patients in setting priorities for healthcare improvement: a cluster randomized trial. Implement Sci. 2014;9:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368:201–3. [DOI] [PubMed] [Google Scholar]
- 7. Bodenheimer T, Ghorob A, Willard-Grace R, Grumbach K. The 10 building blocks of high-performing primary care. Ann Fam Med. 2014;12:166–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kroenke K. The many C’s of primary care. J Gen Intern Med. 2004;19:708–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Phillips WR, Haynes DG. The domain of family practice: scope, role, and function. Fam Med. 2001;33:273–7. [PubMed] [Google Scholar]
- 10. Martin JC, Avant RF, Bowman MA, Bucholtz JR, Dickinson JR, Evans KL, et al. The future of family medicine: a collaborative project of the family medicine community. Ann Fam Med. 2004; 2 suppl 1:S3–S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]