Abstract
This study was to investigate the incidences of DVT in lower extremities after pelvic fracture before and after operation, and explore the risk factors. The records of patients with pelvic fractures receiving operation were collected. The patients were examined by preoperative and postoperative ultrasonography, and divided into thrombosis group and non-thrombosis group according to the preoperative and postoperative ultrasonographic results. Totally, 128 patients with pelvic fractures were included in this study. The incidence of DVT was 21.09% preoperatively, and increased to 35.16% postoperatively. Peripheral DVT constituted 92.60% and 86.67% of preoperative and postoperative DVTs, respectively. The results showed that age (odds ratio [OR] = 1.07; 95% CI: 1.01-1.12; P = 0.013), fracture classification (OR = 3.80; 95% CI: 1.31-11.00; P = 0.014) and D-dimer at admission (OR = 1.04; 95% CI: 1.00-1.08; P = 0.029) were independent risk factors of preoperative DVT, and female (OR = 0.21; 95% CI: 0.06-0.81; P = 0.023) was independent protective factor. In addition, age (OR, 1.06; 95% CI, 1.00-1.11; P = 0.026), operative blood transfusion (OR, 1.34; 95% CI, 1.05-1.72; P = 0.020) were independent risk factors of postoperative DVT. In conclusion, the DVT prevention strategy has not changed the high incidence of DVT in pelvic fractures, and orthopedic surgeons should pay more attention to perioperative DVT. When a male or patient with Tile-C type pelvic fracture is at admission, it is should be reminded that the screening the DVT in lower extremities. In addition, the surgeon should stanch bleeding completely, to reduce the blood transfusion and formation of DVT.
Keywords: deep vein thrombosis, ultrasonography, pelvic fracture, risk factor, preoperative, postoperative
Introduction
Pelvic fractures are often associated with prolonged hospitalization, poor function and sometimes life-threatening conditions. 1 Following by the trauma itself, immobilization, blood loss, comorbidity and operation, some patients often suffered perioperative deep vein thrombosis (DVT) of the lower extremities. 2 Even, the DVT after fracture is a high risk of fatal pulmonary embolism in some patients. 3 Traditional, chemical thromboprophylaxis 4 and mechanical thromboprophylaxis 5 are well-established routines in the treatment of DVT after these fractures.
The incidence of DVT in pelvic fractures is reported to range from 3% 6 to 23%, 7 even 43.28%, 8 in recent studies. However, previous studies only focused on the percentage of DVT, not detailed analysis of DVTs from pelvic fracture. In fact, there are so many factors would influence the formation of DVT possibly, especially the operation. Originally, visceral injury is so commonly associated with disruption of the pelvic girdle, a description of the proximity of these structures to the skeleton is in order. 9 Duration the surgery, the stoppa or ilioinguinal approach or minimally invasive are often chosen for the patients, so the damage of soft tissue, especially superficial and deep femoral vein, will be aggravated in the operation. Thus, we consider that operation is also a vital factor influencing the formation of DVT in the lower extremities.
In this retrospective study, it is aimed to investigate the incidences of DVT in lower extremities after pelvic fracture before and after operation, to explore the risk factors of perioperative DVT in pelvic fracture.
Methods
Ethical Statement
This study retrospectively analyzed the data of patients with pelvic fractures who were admitted between January, 2017, and December, 2019 in Xi’an Honghui Hospital. The study was approved by the ethical board of Xi’an Jiaotong University.
Included and Excluded Criterion for Patients
The inclusion criteria were as follows: a) age of ≥ 16 years; b) pelvic fractures that require surgical treatment; c) the results of preoperative and postoperative ultrasonography were available. Exclusion criteria: a) delayed pelvic fractures, defined as injuries without receiving surgical treatment within 3 weeks after injury, b) open soft tissue fractures, c) serious medical problems without tolerating surgery, d) poor compliance patients, e) patients with contraindications to pharmacological thromboprophylaxis: at high risk of stroke or bleeding.
Preventing Strategy
The consecutive patients with pelvic fractures admitted to the hospital were routinely assessed using the risk assessment profile for thromboembolism score (RAPT) to determine the risk of thromboembolism. 10 We also assessed patients for contraindications for using of low molecular weight heparins (LMWH). For patients without contraindications, LMWH (3800 IU/0.4 mL once per day, Fraxiparine; Glaxo Wellcome Production, GlaxoSmithKline) was injected subcutaneously to prevent DVT when admitted to hospital. Usually, the anticoagulation treatment was given several hours after hemodynamic stabilization. Mechanical thromboprophylaxis (foot intermittent pneumatic compression sleeve, 20 minutes twice a day) was used to prevent DVT. 11 Blood samples were collected within 2 hours after admission, 1 day preoperatively, and 1 day postoperatively.
We used ultrasonography to diagnose the DVT. The diagnostic criteria of DVT are incompressibility of vein, filling defect of cavity, and lack of doppler signal. Patients were examined preoperatively and postoperatively. All patients underwent ultrasonography of the double lower extremities on the day before the scheduled surgery and between the third and fifth day after surgery. DVTs were classified into 3 types: central (femoral and iliac veins), peripheral (calf muscle, fibular, anterior/posterior tibial and popliteal veins), and mixed thrombosis (both central and peripheral thromboses). 12
Based on the results of the ultrasonography, the patients were divided into 2 groups: thrombosis group and no thrombosis group. The thrombosis group was defined as patients suffering DVT, and the no thrombosis group was defined as patients without DVT. For patients without thrombosis, LMWH (3800 IU/0.4 mL once per day, Fraxiparine; Glaxo Wellcome Production, GlaxoSmithKline) was continuously injected subcutaneously to prevent DVT. For patients with thrombosis, LMWH (3800 IU/0.4 mL, twice per day) was injected subcutaneously to treat the DVT. When preoperative ultrasonography results showed a central or mixed thrombosis, an inferior vena cava (IVC) filter was used to prevent the risk of pulmonary embolism. The thromboprophylaxis was stopped 12 hours before surgery and restarted 24 hours after surgery. When the patients were discharged, the protocol was changed to rivaroxaban for 35 days after operation.
Statistics Analysis
Statistical analysis was performed using the SPSS Version 25.0 (SPSS Inc., Chicago, Illinois, USA). The measurement data was analyzed to determine if the data is normally distributed. The statistical analysis utilized the independent sample t-test if it is normally distribution. Non-normally distributed variables were shown as minimum and maximum, and rank sum test was used to compare the differences. For the enumeration data, chi-square test was used. Multivariate analysis was used to detect the risk factors. The difference was statistically significant if P < 0.05.
Results
Patient Characteristics
Totally, 128 patients with pelvic fractures who were admitted to our hospital were included. The patients’ mean age was 44.04 years. Forty-five patients were female and 83 patients were male. In the stability of classification, there were 6, 70, 52 patients in Tile A, B and C subgroup, respectively. All the patients received the operation duration the hospital. Open reduction was used in 101 patients, closed reduction was used in 22 patients and 5 patients received the open reduction plus closed reduction. As for the operative strategy, there were 99, 18, 5, 1, 5 patients received plates, cannulated screw, external fixator, pedicle screw, plates combined cannulated screw, respectively. There were 4 patients suffered the placement of IVC filter in all patients before operation, and IVCs were taken out after operation. No fatal bleeding events or pulmonary embolism was found in these patients. No death was recorded duration the hospital.
Incidence of Preoperative DVT
Twenty-seven patients (21.09%) had thrombosis and 101 had no thrombosis (Table 1). Of these cases, 25 (19.53%) were peripheral DVTs; and 2 (1.56%), mixed DVT. Peripheral DVTs constituted 92.60% (25/27) of all DVTs. Symptomatic DVTs were found in 12 patients, 44.4% of all DVTs.
Table 1.
Univariate Analysis of Preoperative DVT Risk in Patients With Pelvic Fractures.
| No thrombosis | Thrombosis | Overall | t/Chi-square/Z | P | |
|---|---|---|---|---|---|
| No. of patients | 101 | 27 | 128 | ||
| Age | 41.22 ± 14.60 | 54.59 ± 9.96 | 44.04 ± 14.77 | −5.564 | <0.001 |
| Gender | |||||
| Female | 40 | 5 | 45 | 4.155 | 0.042 |
| Male | 61 | 22 | 83 | ||
| Fracture classification | |||||
| Tile A | 5 | 1 | 6 | 7.127 | 0.028 |
| Tile B | 61 | 9 | 70 | ||
| Tile C | 35 | 17 | 52 | ||
| Medical morbidity | |||||
| Hypertension | 2 | 6 | 8 | 0.000 | 1.000 |
| Diabetes | 2 | 1 | 3 | 0.000 | 1.000 |
| Coronary heart disease | 4 | 1 | 5 | 0.000 | 1.000 |
| Arrhythmia | 3 | 1 | 4 | 0.000 | 1.000 |
| Associated trauma | 38 | 13 | 51 | 0.985 | 0.321 |
| History of tumor | 1 | 0 | 1 | 0.000 | 1.000 |
| Preoperative blood transfusion | 29 | 12 | 41 | 2.422 | 0.120 |
| BMI | 21.99 ± 3.48 | 21.35 ± 3.46 | 21.86 ± 3.47 | 0.848 | 0.398 |
| Days between fracture and hospitalization (days) | 3.76 ± 5.05 [0,30] | 3.81 ± 4.75 [0,18] | 3.77 ± 4.97 [0,30] | −0.048 | 0.961 |
| Days between fracture and operation (days) | 9.15 ± 5.71 | 9.22 ± 5.05 | 9.16 ± 5.56 | −0.061 | 0.951 |
| ASA classification | |||||
| 1 | 21 | 2 | 23 | 10.761 | 0.013 |
| 2 | 56 | 10 | 66 | ||
| 3 | 23 | 14 | 37 | ||
| 4 | 1 | 1 | 2 | ||
| Serum markers | |||||
| HGB at admission (mg/L) | 112.26 ± 19.86 | 106.46 ± 24.38 | 111.02 ± 20.93 | 1.256 | 0.212 |
| HCT at admission (%) | 34.43 ± 9.13 | 32.15 ± 7.98 | 33.95 ± 8.92 | 1.158 | 0.249 |
| HGB at preoperative 1 day (mg/L) | 112.03 ± 17.93 | 105.50 ± 14.40 | 110.56 ± 17.323 | 1.335 | 0.186 |
| HCT at preoperative 1 day (%) | 34.03 ± 4.20 | 32.36 ± 4.05 | 33.65 ± 4.20 | 1.413 | 0.162 |
| D-dimer at admission (mg/L) | 10.11 ± 11.91 [0.80,62.60] | 20.31 ± 16.83 [4.05,71.09] | 12.24 ± 13.66 [0.80,71.09] | −3.475 | 0.001 |
| FIB at admission (mg/L) | 4.38 ± 4.27 [1.45,32.10] | 3.32 ± 1.33 [1.47,5.95] | 4.16 ± 3.87 [1.45,32.10] | 1.219 | 0.225 |
| D-dimer at preoperative 1 day (mg/L) | 8.09 ± 7.13 [0.79,32.50] | 12.25 ± 17.14 [3.08,69.56] | 9.34 ± 11.08 [0.79,69.56] | −0.906 | 0.378 |
Univariate Analysis of Preoperative DVT
No statistical differences were observed in medical morbidity, preoperative blood transfusion, body mass index (BMI), days between fracture and hospitalization, days between fracture and operation, serum markers (excluding D-dimer at admission) in 2 groups. However, there were more males in thrombosis group (P = 0.042), and the patients was older than non-thrombosis group (P < 0.001). In addition, fracture classification (P = 0.028), ASA classification (P = 0.013), D-dimer at admission (P = 0.001) were vital contributing factors to thrombosis, showing in Table 1.
Multivariate Analysis of Preoperative DVT
A multivariate analysis was used to detect the risk factors by entering age, gender, fracture classification, ASA classification, D-dimer at admission. The results showed that age (odds ratio [OR] = 1.07; 95% CI: 1.01-1.12; P = 0.013), fracture classification (OR = 3.80; 95% CI: 1.31-11.00; P = 0.014) and D-dimer at admission (OR = 1.04; 95% CI: 1.00-1.08; P = 0.029) were independent risk factors of preoperative DVT, and female (OR = 0.21; 95% CI: 0.06-0.81; P = 0.023) was independent protective factor, showing in Figure 1.
Figure 1.
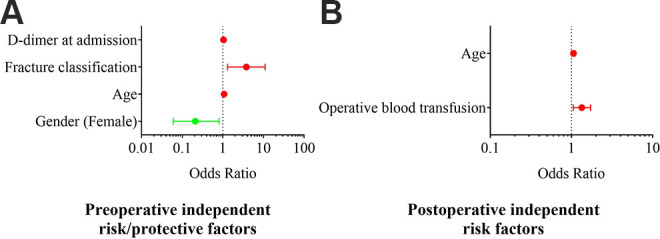
The independent risk or protective factors for preoperative and postoperative DVT in multivariate analysis. A, Preoperative factors. B, Postoperative factors.
Incidence of Postoperative DVT
After the operation, 45 (35.16%) patients suffered thrombosis and 83 patients no thrombosis (64.84%). Of the cases, 39 (30.47%) were peripheral DVT, 3 (2.34%) were central DVT, and 3 (2.34%) were mixed DVT. Peripheral DVTs constituted 86.67% (39/45) of all DVTs (Table 2). Symptomatic DVTs were found in 16 patients, 35.56% of all DVTs.
Table 2.
Univariate Analysis of Postoperative DVT Risk in Patients With Pelvic Fractures.
| No thrombosis | Thrombosis | Overall | t/Chi-square/Z | P | |
|---|---|---|---|---|---|
| No. of patients | 83 | 45 | 128 | ||
| Age | 39.98 ± 14.60 | 51.53 ± 11.97 | 44.04 ± 14.77 | −4.543 | <0.001 |
| Gender | |||||
| Female | 33 | 12 | 45 | 2.194 | 0.139 |
| Male | 50 | 33 | 83 | ||
| Fracture classification | |||||
| Tile A | 4 | 2 | 6 | 8.663 | 0.013 |
| Tile B | 53 | 17 | 70 | ||
| Tile C | 26 | 26 | 52 | ||
| Medical morbidity | |||||
| Hypertension | 6 | 2 | 8 | 0.057 | 0.811 |
| Diabetes | 3 | 0 | 3 | 0.461 | 0.497 |
| Coronary heart disease | 3 | 2 | 5 | 0.000 | 1.000 |
| Arrhythmia | 2 | 2 | 4 | 0.010 | 0.921 |
| Associated trauma | 34 | 17 | 51 | 0.124 | 0.725 |
| History of tumor | 1 | 0 | 1 | 0.000 | 1.000 |
| Preoperative blood transfusion | 26 | 15 | 41 | 0.054 | 0.816 |
| BMI | 22.04 ± 3.21 | 21.51 ± 3.91 | 21.86 ± 3.47 | 0.820 | 0.414 |
| Days between fracture and hospitalization (Days) | 3.84 ± 5.20 [0,18] | 3.64 ± 4.56 [0,30] | 3.77 ± 4.97 [0,30] | 0.215 | 0.830 |
| Days between fracture and operation (Days) | 9.20 ± 5.74 | 9.09 ± 5.26 | 9.16 ± 5.56 | 0.112 | 0.911 |
| ASA classification | |||||
| 1 | 19 | 4 | 23 | 12 | 0.007 |
| 2 | 47 | 19 | 66 | ||
| 3 | 16 | 21 | 37 | ||
| 4 | 1 | 1 | 2 | ||
| Reduction | |||||
| Open reduction | 65 | 36 | 101 | 1.964 | 0.375 |
| Closed reduction | 16 | 6 | 22 | ||
| Open reduction + closed reduction | 2 | 3 | 5 | ||
| Surgical fixation | |||||
| Plates | 64 | 35 | 99 | 2.428 | 0.658 |
| Cannulated screw | 12 | 6 | 18 | ||
| External fixator | 4 | 1 | 5 | ||
| Pedicle screw | 1 | 0 | 1 | ||
| Plates + cannulated screw | 2 | 3 | 5 | ||
| Length of hospital | 10.64 ± 4.91 | 12.20 ± 6.29 | 11.19 ± 5.46 | −1.554 | 0.123 |
| Duration of operation (Mins) | 181.93 ± 99.41 | 219.44 ± 124.24 | 195.12 ± 109.78 | −1.864 | 0.065 |
| Operative blood transfusion (U) | 2.29 ± 2.03 [0,8] | 3.24 ± 2.35 [0,8] | 2.63 ± 2.17 [0,8] | −2.423 | 0.017 |
| Blood loss (ml) | 475.06 ± 384.43 [10,2400] | 611.33 ± 514.17 [20,2000] | 522.97 ± 437.36 [10,2400] | −1.696 | 0.092 |
| Liquid transfusion (ml) | 2500.00 ± 903.11 | 2688.89 ± 997.320 | 2566.41 ± 937.77 | −1.089 | 0.278 |
| Serum markers | |||||
| HGB at admission (mg/L) | 112.36 ± 20.79 | 108.73 ± 21.20 | 111.02 ± 20.93 | 0.924 | 0.357 |
| HCT at admission (%) | 34.70 ± 9.85 | 32.65 ± 6.93 | 33.95 ± 8.92 | 1.230 | 0.221 |
| HGB at preoperative 1 day (mg/L) | 112.33 ± 18.75 | 107.82 ± 14.77 | 110.56 ± 17.32 | 1.075 | 0.286 |
| HCT at preoperative 1 day (%) | 34.37 ± 4.24 | 32.56 ± 3.96 | 33.65 ± 4.20 | 1.800 | 0.076 |
| HGB at postoperative 1 day (mg/L) | 107.48 ± 12.53 | 103.33 ± 22.15 | 105.97 ± 16.72 | 1.302 | 0.195 |
| HCT at postoperative 1 day (%) | 32.07 ± 3.40 | 30.70 ± 6.36 | 31.57 ± 4.72 | 1.316 | 0.193 |
| D-dimer at admission (mg/L) | 9.68 ± 11.66 [2.10,58.57] | 16.81 ± 15.80 [0.80,62.26] | 12.24 ± 13.66 [0.80,62.26] | −2.818 | 0.006 |
| FIB at admission (mg/L) | 4.33 ± 4.57 [1.47,14.20] | 3.86 ± 2.11 [1.45,32.10] | 4.16 ± 3.87 [1.45,32.10] | 0.637 | 0.525 |
| D-dimer at preoperative 1 day (mg/L) | 6.60 ± 5.17 [2.23,69.56] | 13.46 ± 15.70 [0.79,22.20] | 9.34 ± 11.09 [0.79,69.56] | −1.889 | 0.072 |
| FIB at preoperative 1 day (mg/L) | 4.60 ± 1.15 [2.59,7.15] | 4.22 ± 1.16 [2.77,7.22] | 4.44 ± 1.15 [2.59,7.22] | 1.11 | 0.273 |
| D-dimer at postoperative 1 day (mg/L) | 7.08 ± 5.07 [1.79,45.90] | 11.66 ± 10.74 [0.28,26.10] | 8.78 ± 7.94 [0.28,45.90] | −2.406 | 0.020 |
| FIB at postoperative 1 day (mg/L) | 4.23 ± 1.39 [1.85,8.30] | 4.18 ± 1.50 [1.74,7.28] | 4.21 ± 1.43 [1.74,8.30] | 0.161 | 0.872 |
Univariate Analysis of Postoperative DVT
No statistically significant differences in gender, medical morbidity, preoperative blood transfusion, BMI, days between fracture and hospitalization, days between fracture and operation, reduction, surgical fixation, length of hospital, duration of operation, blood loss, liquid transfusion, serum markers (excluding D-dimer at admission and D-dimer at postoperative 1 day) in 2 groups. However, the patients in thrombosis group were older than non-thrombosis group (P < 0.001). In addition, fracture classification (P = 0.013), ASA classification (P = 0.007), operative blood transfusion (P = 0.017), D-dimer at admission (P = 0.006) and D-dimer at postoperative 1 day (P = 0.020) were vital contributing factors to thrombosis, showing in Table 2.
Multivariate Analysis of Postoperative DVT
A multivariate analysis results showed that age (OR, 1.06; 95% CI, 1.00-1.11; P = 0.026), operative blood transfusion (OR, 1.34; 95% CI, 1.05-1.72; P = 0.020) were independent risk factors of postoperative DVT, showing in Figure 1.
The Changes of DVT From Pre-Operation to Post-Operation
The dynamic changes of DVT before and after operation are shown in Figure 2. In the 128 patients, 78 cases showed no changes in hospitalization. New DVT were arose in 23 patients after operation, and peripheral DVT constituted 78.26% (18/23) of all new DVTs. There were 5 cases with DVTs disappeared after operation.
Figure 2.
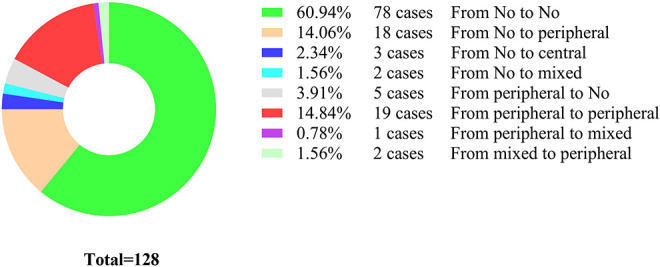
The changes of DVT from pre-operation to post-operation.
Discussion
DVT is one of the common complications after fractures. Now days, there are so many guidelines about chemical thromboprophylaxis and mechanical thromboprophylaxis 13 in the preventing and treatment of DVT. However, we found that the incidence of DVT in pelvic fractures was not low in this study. It is 21.09% preoperatively, and increased to 35.16% postoperatively. These percentages were correspondence to the wide range of 3% 6 to 43% 8 in other studies. However, the previously published studies did not report the preoperative and postoperative incidences respectively. In this retrospective study, it is aimed to investigate the incidences of DVT in lower extremities after pelvic fracture before and after operation, to show the change of DVT between pre-operation and post-operation in pelvic fracture.
In this retrospective study, we have found: a. After the operation, the incidence of DVT was increased 14.06%, there were 23 patients suffering new DVT and 5 cases of DVT disappeared after operation; b. Peripheral DVT constituted 92.60% and 86.67% of preoperative and postoperative DVTs, respectively; c. Symptomatic DVT constituted 44.4% and 35.56% of all preoperative and postoperative DVTs, respectively; d. Age, fracture classification and D-dimer at admission were independent risk factors of preoperative DVT, and female was independent protective factor; e. Age and blood transfusion were independent risk factors of postoperative DVT.
In practice, the factor of Tile-C type pelvic fracture or male was easy to format thrombosis. When a male or patient with this type pelvic fracture was at admission, the surgeon should reminder the screening the DVT in lower extremities. In addition, duration the surgery, the surgeon should stanch bleeding completely, to reduce the blood transfusion. The aim of this strategy is to reduce the incidence of perioperative DVT.
Many factors contribute to the development of thrombosis after fracture. 14,15 In this study, we found age was an identified and sustained risk factor affecting the perioperative DVT. This result is similar to the studies from Chang et al 16 and Tan et al. 17 As for the preoperative risk factors, we need to notice that fracture classification is an important item. In this study, we choose Tile classification of pelvic fractures 18 to classify the subgroup. In 128 patients, type A, B, C was 4.68%, 54.68%, 40.63% of all patients, respectively. In this study, we only included the patients receiving the operation, so type A is less than type B and C. Thus, the incidence of DVT in type C was 32.69% preoperatively, comparing to 16.67% in type A and 12.86% in type B; and 50% postoperatively, comparing to 33.33% in type A and 24.29% in type B. Tile type C is complete disruption of the posterior arch, defining as rotationally and vertically unstable. Tile C is often associated with more serious visceral injury than type A and B. When to the risk factor of D-dimer at admission, it has been reported the relationship to DVT by so many studies. 16 In the field of thrombosis, the female is sometimes recognized as the risk factor 19,20 in most studies. However, we found female was a protective factor in the pelvic fracture. The incidence of preoperative DVT in female was 11.11% (5/45), taking 18.51% (5/27) of all DVT. The incidence of postoperative DVT in female was 26.67% (12/45), taking 26.67% (12/45) of all DVT. The reason might be from that the female often suffer the mild fracture type in this study. In our experience, there are many females with mild or moderate injury receiving the no-surgical treatment.
As for the postoperative risk factor, we found the operative blood transfusion was associated with the postoperative DVT. In the study, the mean volume in thrombosis group was 3.24 U, comparing to 2.29 U in no thrombosis group. Usually, the more blood loss or operative time, the more blood transfusion. However, there was no statistical difference in items of blood loss or operative time between two groups, only a slight trend that blood loss was more and operative time is longer.
Also, there are some limitations in this study. Firstly, the study is case-control design, and the sample of pelvic fracture is not too large enough, only 128 cases. The level of evidence was moderate. In fact, the annual incidence of pelvic fracture is not high, only 14.3/100,000 in recent years. 21 In addition, to avoid the confounding factor, we only included the patients receiving the operation. Secondly, there were many other factors affecting the formation of DVT, but we did not completely collect these indicators. Therefore, a multicenter prospective study with a large sample size will help explore the present situation of DVT in patients with pelvic fractures.
Conclusions
In conclusion, the DVT prevention strategy has not changed the high incidence of DVT in pelvic fractures, and orthopedic surgeons should pay more attention to perioperative DVT. When a male or patient with Tile-C type pelvic fracture is at admission, it is should be reminded that the screening the DVT in lower extremities. In addition, the surgeon should stanch bleeding completely, to reduce the blood transfusion and formation of DVT.
Abbreviations
DVT, Deep vein thrombosis, LMWH, Low molecular weight heparin, BMI Body mass index, ASA, American Society of Anesthesiologists, OR Odds ratio.
Footnotes
Authors’ Note: Conceptualization: Yun Yan and Ping Liu; Data curation: Baobao Zhang, Jie Yang, Yan Zhang, Lei Zhang, Dan Wang, Jing Gao and Lianzhi He; Formal analysis: Pengfei Wang, Yan Zhuang and Kun Zhang; Roles/Writing-original draft: Yun Yan and Ping Liu. The survey was implemented by Xi’an Honghui Hospital. According to relevant regulations, the data could not be shared. The study was approved by the ethical board of Xi’an JiaoTong University (No. 2014026).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Social Development Foundation of Shaanxi Province (Grant numbers 2017ZDXM-SF-009, 2019ZDLSF01-09).
ORCID iD: Yun Yan  https://orcid.org/0000-0002-6552-9365
https://orcid.org/0000-0002-6552-9365
References
- 1. Lundin N, Huttunen TT, Berg HE, et al. Increasing incidence of pelvic and acetabular fractures. A nationwide study of 87,308 fractures over a 16-year period in Sweden. Injury. 2021;52(6):1410–1417. [DOI] [PubMed] [Google Scholar]
- 2. Berning BJ, Magnotti LJ, Lewis RH, et al. Impact of chemoprophylaxis on thromboembolism following operative fixation of pelvic fractures [published online December 23, 2020]. Am Surg. 2020:3134820982577. [DOI] [PubMed] [Google Scholar]
- 3. Brill JB, Badiee J, Zander AL, et al. The rate of deep vein thrombosis doubles in trauma patients with hypercoagulable thromboelastography. J Trauma Acute Care Surg. 2017;83(3):413–419. [DOI] [PubMed] [Google Scholar]
- 4. Di Nisio M, van Es N, Buller HR. Deep vein thrombosis and pulmonary embolism. Lancet. 2016;388(10063):3060–3073. [DOI] [PubMed] [Google Scholar]
- 5. Nam JH, Kim DH, Yoo JH, et al. Does preoperative mechanical prophylaxis have additional effectiveness in preventing postoperative venous thromboembolism in elderly patients with hip fracture?—Retrospective case-control study. PLoS One. 2017;12(11):e0187337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schellenberg M, Benjamin E, Inaba K, et al. When is it safe to start pharmacologic venous thromboembolism prophylaxis after pelvic fractures? A prospective study from a level I trauma center. J Surg Res. 2021;258:272–277. [DOI] [PubMed] [Google Scholar]
- 7. Heelan AA, Freedberg M, Moore EE, et al. Worth looking! venous thromboembolism in patients who undergo preperitoneal pelvic packing warrants screening duplex. Am J Surg. 2020;220(6):1395–1399. [DOI] [PubMed] [Google Scholar]
- 8. Wu L, Cheng B. Analysis of perioperative risk factors for deep vein thrombosis in patients with femoral and pelvic fractures. J Orthop Surg Res. 2020;15(1):597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tile M, Helfet D, Kellam J. Fractures of the Pelvis and Acetabulum. Lippincott Williams & Wilkins; 2015. [Google Scholar]
- 10. Greenfield LJ, Proctor MC, Rodriguez JL, et al. Posttrauma thromboembolism prophylaxis. J Trauma. 1997;42(1):100–103. [DOI] [PubMed] [Google Scholar]
- 11. Fu Y, Liu P, Xu X, et al. Deep vein thrombosis in the lower extremities after femoral neck fracture: a retrospective observational study. J Orthop Surg (Hong Kong). 2020;28(1):2309499019901172. [DOI] [PubMed] [Google Scholar]
- 12. Liu XC, Chen XW, Li ZL, et al. Anatomical distribution of lower-extremity deep venous thrombosis in patients with acute stroke. J Stroke Cerebrovasc Dis. 2020;29(7):104866. [DOI] [PubMed] [Google Scholar]
- 13. Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S–e496S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen F, Xiong JX, Zhou WM. Differences in limb, age and sex of Chinese deep vein thrombosis patients. Phlebology. 2015;30(4):242–248. [DOI] [PubMed] [Google Scholar]
- 15. Park MS, Perkins SE, Spears GM, et al. Risk factors for venous thromboembolism after acute trauma: a population-based case-cohort study. Thromb Res. 2016;144:40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chang W, Wang B, Li Q, et al. Study on the risk factors of preoperative deep vein thrombosis (DVT) in patients with lower extremity fracture. Clin Appl Thromb Hemost. 2021;27:10760296211002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tan Z, Hu H, Deng X, et al. Incidence and risk factors for deep venous thrombosis of lower extremity after surgical treatment of isolated patella fractures. J Orthop Surg Res. 2021;16(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tile M. Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg. 1996;4(3):143–151. [DOI] [PubMed] [Google Scholar]
- 19. Takemoto T, Soh J, Ohara S, et al. The prevalence and risk factors associated with preoperative deep venous thrombosis in lung cancer surgery. Surg Today. 2021;doi:10.1007/s00595-021-02243-3 [DOI] [PubMed] [Google Scholar]
- 20. Qu SW, Cong YX, Wang PF, et al. Deep vein thrombosis in the uninjured lower extremity: a retrospective study of 1454 patients with lower extremity fractures. Clini Appl Thromb Hemost. 2021;27:1076029620986862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Verbeek DO, Ponsen KJ, Fiocco M, et al. Pelvic fractures in the Netherlands: epidemiology, characteristics and risk factors for in-hospital mortality in the older and younger population. Eur J Orthop Surg Traumatol. 2018;28(2):197–205. [DOI] [PubMed] [Google Scholar]


