Abstract
Background
Ivermectin mass drug administration (MDA) could accelerate malaria elimination in the Greater Mekong Subregion. This study was performed to characterize the bionomics of Anopheles in Surat Thani province, Thailand.
Methods
Mosquitoes were collected via human landing collections between February and October 2019. Anopheles mosquitoes were morphologically identified to species. Primary Anopheles malaria vectors were dissected to assess parity status, and a subset were evaluated for molecular identification and Plasmodium detection.
Results
A total of 17,348 mosquitoes were collected during the study period; of these, 5777 were Anopheles mosquitoes. Morphological studies identified 15 Anopheles species, of which the most abundant were Anopheles minimus (s.l.) (87.16%, n = 5035), An. dirus s.l. (7.05%, n = 407) and An. barbirostris s.l. (2.86%, n = 165). Molecular identification confirmed that of the An. minimus s.l. mosquitoes collected, 99.80% were An. minimus (s.s.) (n = 484) and 0.2% were An. aconitus (n = 1), of the An. dirus (s.l.) collected, 100% were An. baimaii (n = 348), and of the An. maculatus (s.l.) collected, 93.62% were An. maculatus (s.s.) (n = 44) and 6.38% were An. sawadwongporni (n = 3). No Anopheles mosquito tested was Plasmodium positive (0/879). An average of 11.46 Anopheles were captured per collector per night. There were differences between species in hour of collection (Kruskal–Wallis H-test: χ2 = 80.89, P < 0.0001, n = 5666), with more An. barbirostris (s.l.) and An. maculatus (s.l.) caught earlier compared to An. minimus (s.l.) (P = 0.0001 and P < 0.0001, respectively) and An. dirus (s.l.) (P = 0.0082 and P < 0.001, respectively). The proportion of parous An. minimus (s.l.) captured by hour increased throughout the night (Wald Chi-square: χ2 = 17.31, P = 0.000, odds ratio = 1.0535, 95% confidence interval 1.0279–1.0796, n = 3400). Overall, An. minimus (s.l.) parity was 67.68% (2375/3509) with an intra-cluster correlation of 0.0378. A power calculation determined that an An. minimus (s.l.) parity reduction treatment effect size = 34%, with four clusters per treatment arm and a minimum of 300 mosquitoes dissected per cluster, at an α = 0.05, will provide 82% power to detect a significant difference following ivermectin MDA.
Conclusions
The study area in Surat Thani province is an ideal location to evaluate the impact of ivermectin MDA on An. minimus parity.
Graphical abstract

Keywords: Anopheles, Plasmodium, Malaria, Thailand, Surat Thani, Parity
Background
In 2019, an estimated 229 million cases of malaria occurred worldwide, with approximately 239,000 cases reported from the Greater Mekong Subregion (GMS). Between 2010 and 2019, the number of malaria cases in the GMS fell by 90%, and the target of the countries within the GMS is to eliminate malaria by 2030 [1]. Malaria transmission in the GMS is complex, with various Anopheles species in the Dirus complex, Minimus complex and the Maculatus group having been recognized as the primary malaria vectors in the region. From the Minimus complex, Anopheles minimus (s.s.) is the primary malaria vector and can be found across Thailand and the GMS [2–6]. There are two members of the An. dirus complex that are primary malaria vectors; of these, An. dirus (s.s.) occurs east of the Thai–Myanmar border, and An. baimaii occurs west of the Thai–Myanmar border [2, 6, 7]. Additionally, members of the An. maculatus group are considered to be primary vectors that contribute to malaria transmission, including An. maculatus (s.s.) [2, 4, 5] and to a lesser extent An. sawadwongporni [2, 4, 6], with the latter identified as a malaria vector in southern Thailand [2]. Members within a species complex differ in their behavioral characteristics, which in turn drives Plasmodium transmission dynamics; therefore, an accurate identification of mosquitoes is essential to design and evaluate vector control methods in the GMS.
The diversity of vector species, insecticide resistance and increasing antimalarial drug resistance are some of the greatest challenges for malaria elimination in the GMS [8]. Moreover, the outdoor-feeding, outdoor-resting and early-evening feeding behaviors of GMS malaria vectors [9–11] also limit the effectiveness of indoor residual spraying (IRS) and long-lasting insecticide-treated nets (LLINs). Therefore, novel vector control measures which target these outdoor-feeding vectors could accelerate malaria elimination in the GMS. The mass drug administration (MDA) of ivermectin to humans has been suggested as a possible malaria parasite transmission control tool as it directly kills Anopheles that feed on treated people, regardless of blood-feeding time or location. Evidence from West Africa has shown that a single ivermectin MDA can kill wild An. gambiae (s.l.) [12, 13], shift the population age structure [13], reduce the Plasmodium falciparum sporozoite rate [13, 14] and that repeated ivermectin MDAs reduce clinical falciparum malaria episodes [15]. In the GMS, at human-relevant concentrations, ivermectin is lethal to An. dirus, An. minimus, An. sawadwongporni and An. campestris, and it inhibits the development (i.e. sporogony) of Plasmodium vivax in An. dirus and An. minimus [16]. A clinical trial demonstrated that An. dirus fed blood from persons treated with ivermectin (400 µg/kg) within 6 days post ivermectin administration had a 50% reduced survival rate; the reduction in An. minimus survival increased to 90% when they were fed blood from treated persons up to 10 days post drug administration [17]. This evidence has inspired a large-scale cluster randomized trial in Thailand to assess the effect of ivermectin MDA on entomological and parasitological parameters of malaria transmission.
Evaluating vector control interventions for malaria in the GMS is difficult as transmission occurs primarily in the forest due to Anopheles habitat preference, combined with sporadic human entry into the forest for various agricultural and economic pursuits, not all of which are legal [18, 19]. However, most vector control interventions (e.g. LLINs and IRS) are applied in the village setting where transmission is less likely to occur, and thus they do not directly target the areas of active Plasmodium transmission. Thailand has dramatically reduced its malaria burden and has set the goal to eliminate malaria by 2024. Indeed, from 2000 to 2019, there was a 96% reduction in number of malaria cases, from 159,120 to 5832, but the ratio of Thai to non-Thai cases has increased from 57 to 72% demonstrating that there are still active foci of transmission in Thailand [20]. This reduction in malaria complicates evaluation of Anopheles vector control interventions in Thailand due to low rates of Plasmodium transmission. To evaluate the effect of ivermectin MDA, a site in Thailand needed to be selected where persons live and work with active malaria transmission. Rubber plantations in Thailand offer an ideal location for Anopheles vector control intervention evaluation, as mature rubber plantations tend to be located in hilly areas adjacent to natural forests, both of which are ideal habitats for primary malaria vector proliferation. Rubber tappers live and work in the same environment, and tappers work throughout the night exposed to wild Anopheles; consequently, rubber tappers have higher rates of malaria than non-rubber tappers [21–23]. Indeed, a seven-province wide survey of case data from malaria clinics in Thailand from 2013 to 2016 found that 60.1% (3330/5541) of P. falciparum cases were identified from rubber tappers [23].
Of all the provinces in Thailand, Surat Thani province has the largest rubber plantation coverage, approximately 3829 km2 [24], and is one of the few provinces affected by malaria that is not along an international border. Interestingly, in Surat Thani, the dominant malaria species infecting humans is P. falciparum, accounting for 77.58% (519/669) of all malaria cases from 2015 to 2019 [25]. Plasmodium falciparum is the ideal parasite to assess during vector control interventions as it is most sensitive to transmission interruption due to its non-relapsing nature. A cross-sectional molecular malaria survey conducted in Surat Thani in 2019 demonstrated that persons who stayed outdoors during the night-time were at the highest risk of malaria infection [26]. In that study, three districts in Surat Thani province, namely the Phanom, Vibhavadi and Khiri Rat Nikhom districts, were selected for evaluation based on their malaria case incidence comprising 65.13% (338/519) P. falciparum cases between 2015 and 2019 and high rubber plantation coverage. Historically, IRS with 5% deltamethrin has been performed in villages with a higher malaria case burden, but this control measure ceased in Phanom and Vibhavadi in 2015 and in Khiri Rat Nikhom in 2016. LLINs are widely distributed throughout all three districts by government and non-governmental organizations. Daytime indoor thermal fogging for Aedes aegypti control with 1% deltamethrin or 25% cypermethrin still occurs focally and sporadically in response to local dengue cases (personal communication, Surat Thani Vector-borne Diseases Control Center 11.3, Surat Thani, Thailand).
Little information regarding Anopheles vector bionomics in Surat Thani has been published. The largest study conducted in Surat Thani to date reported a total of 3778 Anopheles mosquitoes collected from February 2015 to December 2016 via human landing collection (HLC) in Phanom district [27]. In the same study, six Anopheles species were collected, including An. dirus (s.l.), An. minimus (s.l.), An. maculatus (s.l.), An. barbirostris (s.l.), An. hycranus (s.l.) and An. tessellatus. The predominant species was An. minimus (s.l.), comprising 87.19% of Anopheles collected. The highest mosquito densities were found between March and May in both years [27]. Molecular identification has verified the presence of An. maculatus (s.s.) in Phanom district [28] and An. minimus (s.s.) in Khiri Rat Nikhom district [29]. Due to active P. falciparum transmission, asymptomatic malaria observation, presence of primary malaria vectors and an ideal environment for evaluating a vector control intervention, Surat Thani province was selected as the study area to evaluate the impact of ivermectin MDA on entomological and parasitological parameters. Due to decreasing rates of Plasmodium transmission in Thailand, entomological (i.e. mosquito population age structure) and parasitological (i.e. human malaria prevalence) outcomes will be used to assess ivermectin MDAs. The unexpectedly low prevalence of malaria in the study sites [26] necessitates a strong emphasis on the former.
Baseline entomological surveillance utilizing the mosquito HLC method were performed to evaluate vector abundance, composition, landing activity and parity rates linked to molecular identification in Surat Thani in 2019. These efforts were undertaken to determine whether the study area was appropriate to evaluate the impact of ivermectin MDA on An. minimus population age structure (i.e. parity).
Methods
Ethics statement
This study was approved by the Walter Reed Army Institute of Research (WRAIR #2430), the Human Research Protection Office (HRPO Log No. 19919.2a/A-19919.2b) and the Ethical Review Committee for Research in Human Subjects, Ministry of Public Health, Thailand (Thai MoPH Ref No. 25/2560).
Description and maps of field sites
Field site description
Collection sites were located in Khiri Rat Nikhom, Phanom and Vibhavadi districts, in Surat Thani province (651 km south of Bangkok). Villages with higher malaria case burden, as reported by local Vector Borne Disease Units, were selected from each district. Populations and house locations were mapped (see section Mapping process), and cluster sizes of approximately 300–500 persons were established. In total, 13 clusters were selected for entomological evaluation: five clusters in Khiri Rat Nikhom, four clusters in Phanom and four clusters in Vibhavadi. Khiri Rat Nikhom district is located in the center of Surat Thani province (9°1′48″N, 98°57′12″E), with its western part located in the forested hills of the Phuket mountain range adjacent to Khao Sok National Park and its eastern part mostly consisting of flat terrain. Phanom is located in the southwest of the province (8°51′18″N, 98°48′48″E) and is covered by mountains and forest. Its northwestern part is protected by the Khao Sok National Park and its southwestern part is protected by the Khlong Phanom National Park. Vibhavadi is a small district situated in the north-central portion of the province (9°14′20″N, 98°58′44″E) and is covered by mountain and forest. The western part of the district is protected by the Kaeng Krung National Park and Khlong Yan Wildlife Sanctuary. In Surat Thani, the dry season occurs from January to February, and the rainy season lasts from March to September; heavy monsoon rains occur October to December.
Mapping process
Latitude and longitude coordinates of all houses and HLC locations were captured using a 60CSx GPS unit (Garmin, Olathe, KS, USA). The open-source QGIS software was used to generate maps for each cluster. The terrain data were derived from a topographic map with elevation contour lines at 25 m.
Collection, morphological identification and parity evaluation of mosquitoes
Mosquito collection
Adult mosquitoes were collected from February to October 2019 for two consecutive nights per cluster per month, with the exception of Vibhavadi where collections began in June. Mosquitoes were collected by the HLC method. Mosquito collector volunteers were local Thai residents, non-pregnant and non-breastfeeding adults (age 18–62 years) who were capable of providing informed consent and capable of comprehending the HLC method. A canopy was constructed at each outdoor collection site to protect the mosquito collector volunteers from the elements. There were two collection sites per cluster each night. Collection sites were chosen based on proximity to a forest or rubber plantation, presence of a house nearby for access to water and electricity and close proximity to potential An. minimus (s.l.) larval habitat. Efforts were made to sample as many areas in each cluster that met the above criteria and were safely accessible. If a collection site yielded few or no Anopheles, then the site was switched to a new location the following night. At each collection site, two mosquito collector volunteers worked together from 18:00 h to 24:00 h and then replaced by two other collectors from 24:00 h to 06:00 h. Collections occurred for 50 min of each hour, followed by a 10-min break. Volunteers were instructed to wear double-layer clothing. Each collector exposed only their legs and captured mosquitoes as soon as they landed on them using a plastic collection tube sealed with a cotton ball. The mosquitoes were then transferred to collection cups grouped by hour of collection and separated by each volunteer. The cups were kept in a Styrofoam box and covered with moist towel to keep the mosquitoes humid and alive during transport back to the field station.
Mosquito morphological identification and parity dissections
At the field station, mosquitoes were transferred to plastic knockdown chambers and anesthetized with triethylamine (Flynap®; Carolina Biological Supply Co., Burlington, NC, USA) for 2 min, following which they were identified morphologically under a dissecting stereomicroscope (Stemi 305; Carl Zeiss AG, Oberkochen, Germany) using a standard key of adult Anopheles of Thailand [30]. All primary Anopheles species, such as the An. dirus complex and An. maculatus group, and a subset of 20 An. minimus complex per collector pair per site from 18:00 h to 24:00 h and from 24:00 h to 06:00 h were dissected to remove their ovaries. Once mosquitoes were anesthetized, they were placed in plastic Petri dishes and care was taken to keep the mosquitoes in an ice-chilled cooler with a damp towel to maintain humidity. Thus, almost all mosquitoes were alive at the point of ovary dissection. Ovaries were dissected with minuten pins in a drop of bottled Crystal water, a brand of marketed water commonly found throughout Thailand. The last two abdominal segments were gently pulled apart from the abdomen, and the ovaries were separated from the remaining internal organs and transferred to an individual well on a 12-well slide. The slide was then allowed to air dry, and care was taken to observe each ovary before total evaporation of water to assess parity status. Determination of parity status was based on the presence of coiled (nulliparous) and uncoiled (parous) tracheole skeins viewed at ×10 and ×40 magnification with a compound microscope (model B-190TB; Optika Srl, Ponteranica, Italy) and images of the ovaries were taken for reference. On occasion, if the primary reviewer had doubts on the parity status, then a second reviewer was consulted. The mosquito sample was then bisected between the thorax and the abdomen and stored in labeled 2-ml centrifuge tubes with silica gel desiccant. Processed mosquitoes were shipped back to the Armed Forces Research Institute of Medical Sciences in Bangkok for molecular species identification and Plasmodium infection evaluation of the thorax.
Molecular methods for Anopheles and Plasmodium identification
DNA extraction method
The DNA extraction method involved adding 700 µl of phosphate buffer saline (pH 7.4) and 4.5-mm steel beads (Copperhead; Crosman Corporation, Bloomfield, NY, USA) to a 2-ml tube containing an individual mosquito thorax or abdomen, followed by homogenization in the TissueLyser II (Qiagen, Hilden, Germany) at 22 Hz for 2 min. The mosquito suspension was then centrifuged at 12,000 rpm for 5 min, and a 250-µl aliquot of the supernatant was used for DNA extraction according to the QIAsymphony® DNA Minikit and Tissue LC 200 DSP protocol in the fully automated QIAsymphony® SP system (Qiagen). The DNA was eluted in 50 μl and stored at − 20 °C until further use. DNA/RNA-free distilled water was included in the extraction process as a negative extraction control.
Molecular methods for Anopheles sibling species identification
To identify anopheline sibling species, multiplex allele-specific PCR (AS-PCR) assays were used to examine the internal transcribed spacer 2 (ITS2) region of DNA and distinguish the members of the Dirus complex [An. dirus (s.s.), An. scanloni, An. cracens, An. baimaii, An. nemophilous] [31], the Maculatus group [An. maculatus (s.s.), An. pseudowillmori, An. sawadwongporni, An. rampae, An. dravidicus] [32] and the Funestus group [An. minimus (s.s.), An. harrisoni, An. aconitus, An. varuna, An. pampanai] [33]. Previously published protocols [31–34] were used, with the following modifications. The amplification was carried out using total volumes of 25 μl, with the final optimized reaction conditions as follows: (i) 1× GoldStar Best Master mix (GoldStar DNA Polymerase, dNTP, PCR stabilizer and enhancer); (ii) three specific primer cocktails, each containing four or five different primer pairs to discriminate between species with 400 nM for the primers specific for the Funestus group and Maculatus group and 500 nM for the primers specific for the Dirus complex; (iii) 4% dimethyl sulfoxide (DMSO) was included only for Dirus complex reactions; (iv) a universal forward primer, located in the conserved region of the 5.8S gene, and species-specific reverse primers in the ITS2 spacer region were employed to amplify a portion of the mosquito ITS2 region; and (v) 1 μl of genomic DNA was used as template. Positive mosquito controls [i.e. An. minimus (s.s.), An. dirus (s.s.), An. sawadwongporni]) were obtained from mosquito colonies maintained at the Armed Forces Research Institute of Medical Science Department of Entomology. Negative DNA/RNA-free distilled water controls were included.
Amplifications were performed in a T100 DNA thermal cycler (Bio-Rad, Hercules, CA, USA) under the following PCR conditions. For the Maculatus group, the cycling program started with an initial denaturation at 95 °C, 10 min; then denaturation at 94 °C/1 min, primer annealing at 55 °C/30 s, extension at 72 °C/30 s for 35 cycles; and a final extension at 72 °C for 10 min. The amplification conditions for the Dirus complex were the same as those for the Maculatus group, except that the annealing time was 15 s instead of 30 s. For the Funestus group, which contains the Minimus complex, the cycling program started with an initial denaturation at 95 °C, 10 min; then amplification at 94 °C/30 s, 45 °C/30 s, 72 °C/40 s for 35 cycles; and a final extension at 72 °C for 10 min. The amplified PCR products were subjected to DNA fragment analysis using the QIAxcel Advanced System (Qiagen) according to the manufacturer’s instructions. Briefly, 10 μl of PCR product was analyzed with the QIAxcel DNA Fast Analysis Cartridge (Qiagen), using the DM190 method and QX 15-bp/1-kb alignment markers. Fragment sizes were calculated using the BioCalculator (Qiagen).
DNA sequencing and data analysis
To confirm the results of multiplex AS-PCR assays, a representative of each anopheline group was selected for confirmation with the ITS2 rDNA gene in the DNA sequencing assays. Amplification of the ITS2 rDNA gene from mosquito DNA extracts was conducted using universal primer ITS2A (5′-TGT GAA CTG CAG GAC ACA T-3′) and ITS2B (5′-TAT GCT TAA ATT CAG GGG GT-3′) [35, 36]. Reactions were performed in a T100 DNA thermal cycler (Bio-Rad). PCR reaction mixtures (25 μl) consisted of 2 µl of mosquito DNA extract, 0.1 U of AmpliTaq® Gold DNA Polymerase (Life Technologies, Thermo Fisher Scientific, Carlsbad, CA, USA), 1× Gold buffer, 0.2 mM of dNTP, 2 mM of MgCl2 and 0.2 µM of each primer. The PCR cycling program consisted of an initial denaturation step at 94 °C, 10 min; then 94 °C/30 s, 60 °C/1 min, 72 °C/1 min for 37 cycles; and a final extension step at 72 °C for 5 min. The size of the PCR product was determined using the QIAxcel Advanced System as described above. The PCR product was cleaned by the ExoSAP-IT™ PCR Products Clean-up kit: 2 µl of ExoSAP-IT™ was added directly to 5 µl of PCR reaction product, incubated at 37 °C for 15 min and then at 80 °C for 15 min. The ITS2 rDNA gene PCR product was sequenced using the Bigdye® Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, Waltham, MA, USA) according to Applied Biosystems’ protocol with forward and reverse universal ITS2A and ITS2B primers and run on a SeqStudio Genetic Analyzer (Life Technologies). Forward and reverse nucleotide sequence data for each sample were assembled using the Sequencher 5.1 software package (Gene Code Corp., Ann Arbor, MI, USA). The Anopheles species were identified by phylogenetic analysis. Briefly, the MUSCLE algorithm was used for sequence alignment in Molecular Evolutionary Genetics Analysis (MEGA) 6.0 software [37]. Maximum likelihood trees were constructed with the best fit model of nucleotide substitution with bootstrapping (1000 replicates) using MEGA 6.0 software as described by Tamura et al. [37].
Real-time PCR for detection of Plasmodium
Real-time PCR for Plasmodium detection from Anopheles thoraxes was performed using a 7500 Fast Real-time PCR System (Life Technologies). The primers and probes were modified from a previously published protocol of Kimura et al. [38] using the 18S subunit of rRNA of Plasmodium spp. as a target gene as follows: forward P2F (5′-TAT TCA GAT GTC AGA GGT GAA ATT C-3′), reverse P2R (5′-GAA CCC AAA GAC TTT GAT TTC TCA T-3′) and Plasmodium Genus Probe (5′-FAM- ACG ATC AGA TAC CGT CGT AAT CTT-BHQ2-3′). The real-time PCR reaction (25 µl) consisted of 10 µl of KAPA PROBE FAST qPCR Master Mix (2×) (Roche, Branford, CT, USA) containing KAPA Taq HotStart DNA Polymerase, dNTPs, MgCl2, stabilizers, 0.3 µl of each 20 µM primer, 1 µl of 10 µM probe, 1 µl of mosquito DNA extract and 8.2 µl of nuclease-free water. Plasmodium falciparum- and P. vivax-infected An. dirus (s.s.) served as positive controls and uninfected An. dirus as negative controls and were included in every run. The thermocycler conditions included initial steps at 50 °C, 2 min and 95 °C, 2 min; then amplification at 95 °C/15 min, 60 °C/30 min for 40 cycles; the cut-off values were set automatically at every run. All positive samples were confirmed for Plasmodium species by nested PCR.
Nested PCR Analysis for Plasmodium species differentiation
Nested PCR was performed using two amplification processes as described by Kimura et al. [38] to identify four Plasmodium species: P. falciparum, P. vivax, P. ovale and P. malariae. The nested PCR was performed in a T100 DNA thermal cycler (Bio-Rad). For the first PCR reaction, the reaction mixture (20 µl) consisted of 1× PCR Gold Buffer II (50 mM KCl, 15 mM Tris–HCl, pH 8.0), 1.5 mM MgCl2, 200 μM dNTP, 0.4 μM of each specific outer primer set (P1F and P2R), 0.25 U of Amplitaq Gold™ DNA polymerase and 1 µl of DNA template. The cycling conditions of the first PCR were: 94 °C, 10 min; then 92 °C/30 s, 60 °C/90 s, 72 °C/1 min for 35 cycles. Nuclease-free water was used as a negative control. The amplified fragment was analyzed using the Qiaxcel Advanced System with an expected size of around 140–160 bp. For the second PCR, the product of the first PCR reaction was diluted (1:50) with nuclease-free water and used as a template in the second PCR reaction. The reaction mixture of the second PCR reaction (20 µl) and the cycling program were the same as those of the first PCR reaction, except that the reverse specific primers were used instead of the P2R primer. The expected product (about 110 bp) of each Plasmodium species was determined using the Qiaxel Advanced System as described above.
Statistical analysis
Mosquito diversity per cluster was estimated using the Shannon–Wiener index [39] and the Simpson index [40]. The number of Anopheles caught per night was calculated by assessing the total number of Anopheles captured at one HLC site divided by two for the pair of collectors used at each location; this number was then used to calculate the mean number of Anopheles. The median mosquito catching time was calculated, and the comparison of the distribution of mosquito catching times among groups were assessed using the non-parametric Kruskal–Wallis H-test; pairwise comparisons for significantly different groupings were performed using the post-hoc Dunn’s multiple comparisons test to account for the multiple comparisons using Prism version 7.2 (GraphPad Software, San Diego, CA, USA). Parity by cluster and hour was assessed by a logistic regression model, and the clustering of outcomes was accounted for by using the robust standard errors. The sample size and power calculations for a cluster randomized trial were performed using the clustersampsi command in STATA version 14 (StataCorp, College Station, TX, USA).
Results
Topographical maps
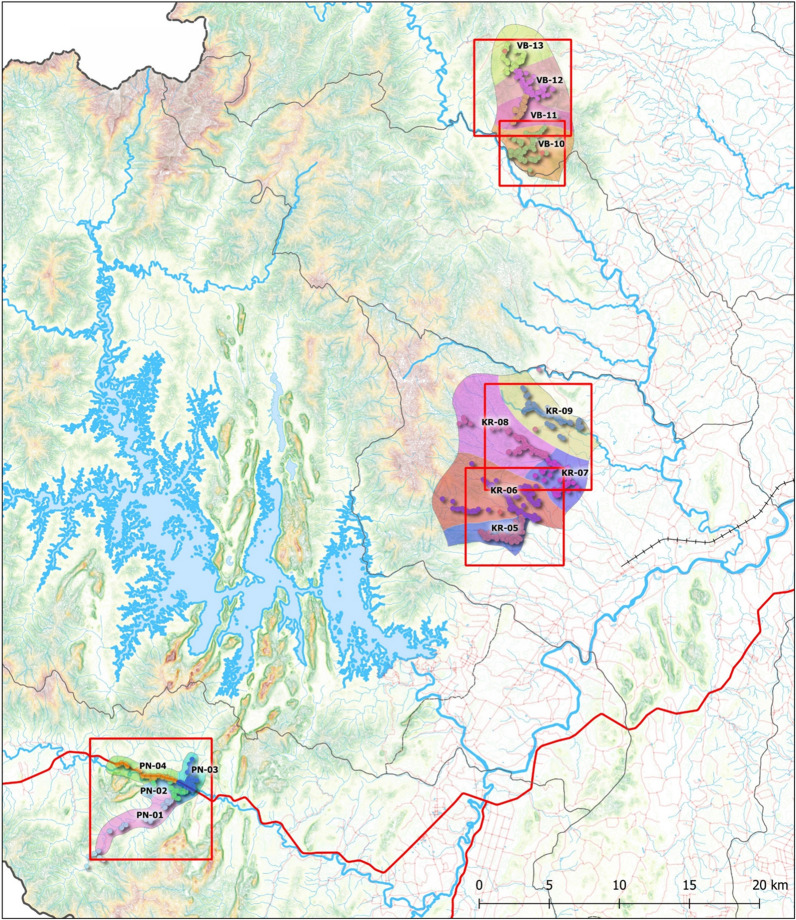
A terrain map of Surat Thani province with the clusters evaluated from Phanom (PN), Khiri Rat Nikhom (KR) and Vibhavadi (VB) districts is shown in Fig. 1. Figure 2 is a zoomed-in version of Fig. 1, with the terrain maps depicting the house and mosquito collection locations for each of the 13 clusters evaluated in this study.
Fig. 1.
Cluster locations that were surveyed for Anopheles mosquitoes in 2019 and surrounding terrain features. KR Khiri Rat Nikhom, PN Phanom, VB Vibhavadi
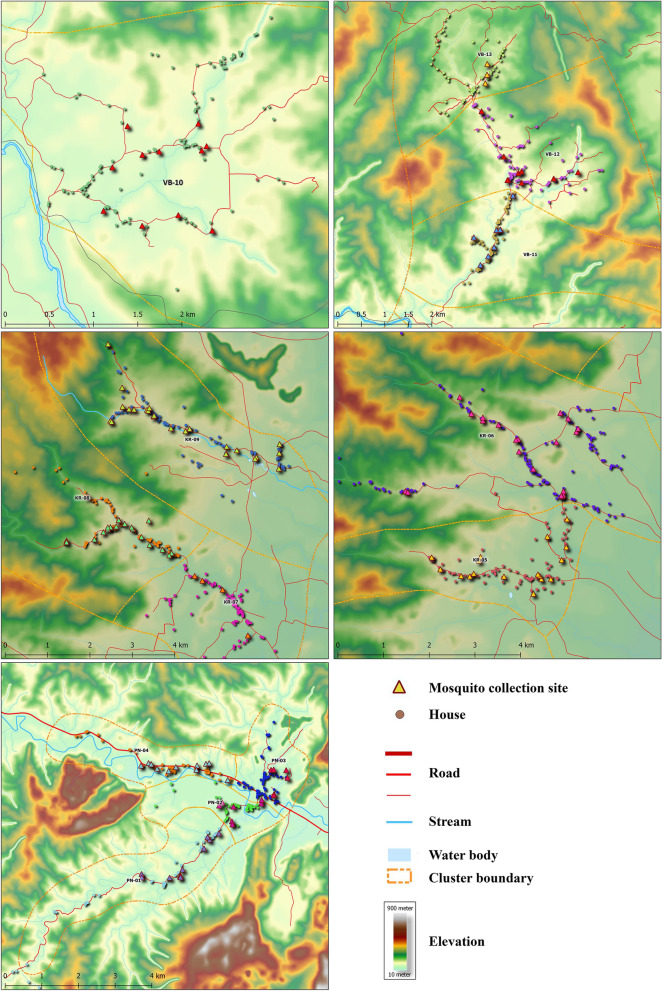
Fig. 2.
Enlarged (zoomed-in) terrain maps for each group of clusters surveyed in 2019. Houses (circles) and mosquito collection sites (triangles) are marked along with cluster boundaries (dashed lines). As much of the cluster as was safely accessible was surveyed for mosquito collections
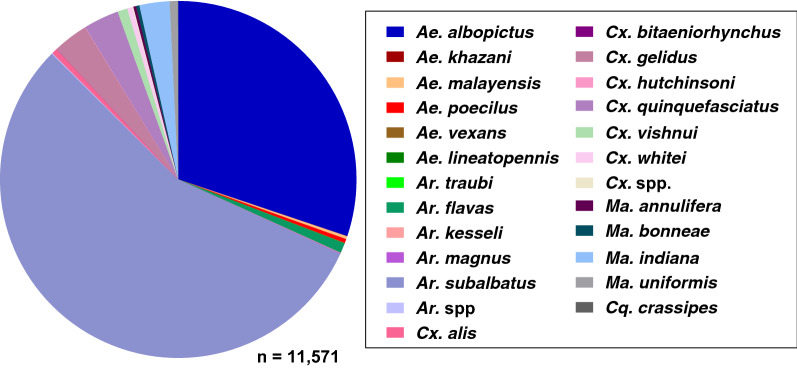
Species composition and abundance
In 13 clusters from three districts, a total of 17,348 adult female mosquitoes were collected, representing six genera: Armigeres (37.78% of total female mosquitoes collected), Anopheles (33.32%), Aedes (20.58%), Culex (5.62%), Mansonia (2.69%) and Coqullitettedia (0.01%). A total of 23 culicine mosquito species were identified from 11,571 collected specimens, of which the most abundant were Ar. subalbatus (55.59%), Ae. albopictus (30.15%), Cx. gelidus (3.21%), Cx. quinquefasciatus (3.21%) and Ma. indiana (2.73%), with the remaining 18 culicine species each comprising < 1% of the total collection (Fig. 3).
Fig. 3.
Proportion of the culicine species in the 11,571 mosquitoes captured from Surat Thani in 2019. Ae. Aedes, Ar. Armigeres, Cq. Coquilletidia, Cx. Culex, Ma. Mansonia
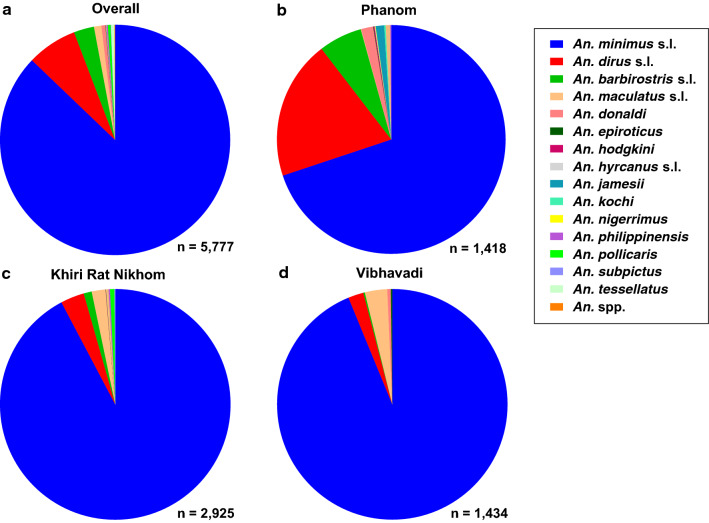
Fifteen Anopheles species were morphologically identified from a total of 5777 specimens, of which ten belonged to the subgenus Cellia and five to the subgenus Anopheles. The predominant Anopheles captured at the study site were primary or suspected vectors and, listed in order of decreasing abundance, were: Anopheles minimus (s.l.) (87.17%; n = 5035), An. dirus (s.l.) (7.05%; n = 407), An. barbirostris (s.l.) (2.86%; n = 165) and An. maculatus (s.l.) (1.04%; n = 60). The remaining 11 species comprised 1.79% of the total Anopheles captured: An. donaldi (n = 32), An. tessellatus (n = 27), An. pollicaris (n = 23), An. philippinensis (n = 11), An. subpictus (n = 3), An. epiroticus (n = 2), An. hodgkini (n = 2), An. nigerrimus (n = 2), An. hyrcanus (s.l.) (n = 1), An. jamesii (n = 1) and An. kochi (n = 1). Only 0.09% (n = 5) of Anopheles specimens could not be morphologically identified to the species level (Fig. 4a).
Fig. 4.
Proportion of Anopheles species identified morphologically overall (a) and by district (b–d)
Overall, An. minimus (s.l.) was the most abundant Anopheles species captured across all three districts, representing 69.89% of captured Anopheles species in Phanom, 92.27% in Khiri Rat Nikhom and 93.79% in Vibhavadi (Fig. 4a–d). The second and third most abundant Anopheles species by district were An. dirus (s.l.) and An. barbirostris (s.l.) in Phanom (19.68 and 6.14%, respectively) (Fig. 4b), An. dirus (s.l.) and An. maculatus (s.l.) in Khiri Rat Nikhom (3.32 and 1.91%, respectively) (Fig. 4c) and An. barbirostris (s.l.) and An. dirus (s.l.) in Vibhavadi (3.14 and 2.16%, respectively) (Fig. 4d). Of the total Anopheles captured (n = 5777), primary and secondary malaria vectors comprised 95.26% of the total Anopheles collected.
The Shannon–Wiener index and Simpson index were calculated per cluster for all species collected and for only the Anopheles species collected. For all species captured, no clear difference in mosquito diversity was found across the three districts, with the four clusters (PN-01, PN-04, KR-09, VB-10) of highest diversity occurring in each of the three districts. However, for Anopheles species, the four Phanom clusters had the highest diversity (Table 1).
Table 1.
Total number of mosquitoes and Anopheles collected, and their respective Shannon–Wiener and Simpson indices, for each cluster
| Number of mosquitoes and Anopheles collected and related indices | Cluster | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PN-01 | PN-02 | PN-03 | PN-04 | KR-05 | KR-06 | KR-07 | KR-08 | KR-09 | VB-10 | VB-11 | VB-12 | VB-13 | |
| Total collected (n) | 2026 | 822 | 1049 | 1051 | 1518 | 2518 | 689 | 2351 | 1576 | 946 | 614 | 1586 | 577 |
| Total Shannon-Wiener Index | 1.77 | 1.24 | 1.45 | 1.79 | 1.54 | 1.45 | 1.72 | 1.46 | 1.71 | 1.74 | 1.43 | 1.25 | 1.13 |
| Total Simpson Index | 4.45 | 1.91 | 2.88 | 4.35 | 3.32 | 3.23 | 3.90 | 3.50 | 4.08 | 3.98 | 3.18 | 2.91 | 2.63 |
| Anopheles collected (n) | 751 | 58 | 173 | 434 | 429 | 832 | 323 | 858 | 474 | 413 | 201 | 733 | 87 |
| Anopheles Shannon-Wiener Index | 2.07 | 3.25 | 1.52 | 1.49 | 1.20 | 1.20 | 1.24 | 1.11 | 1.13 | 1.20 | 1.32 | 1.04 | 1.29 |
| Anopheles Simpson Index | 0.97 | 1.36 | 0.69 | 0.67 | 0.45 | 0.42 | 0.43 | 0.25 | 0.32 | 0.39 | 0.53 | 0.11 | 0.48 |
Mosquitoes identified only to genera were not included in the totals or species diversity calculations
KR Khiri Rat Nikhom district, PN Phanom district, VB Vibhavadi district
The average number of Anopheles specimens collected per volunteer per night is shown in Table 2. Overall, nightly HLCs did not vary by district for all Anopheles, with an average of 11.46 Anopheles captured per collector per night. There were no differences in mean number of An. minimus (s.l.) captured per collector per night across the three districts. However, more An. dirus (s.l.) were captured per person per night from Phanom, and more An. maculatus (s.l.) were captured per person per night from Khiri Rat Nikhom, while fewer An. barbirostris (s.l.) were captured per person per night from Khiri Rat Nikhom (Table 2).
Table 2.
Mean number of Anopheles specimens collected per volunteer per night by district
| Study sites | An. minimus (s.l.) | An. dirus (s.l.) | An. barbirostris (s.l.) | An. maculatus (s.l.) | All Anopheles |
|---|---|---|---|---|---|
| PN | 7.50 (3.50, 11.50) | 2.11 (1.02, 3.20) | 0.64 (0.34, 0.93) | 0.01 (0.01, 0.02) | 10.70 (5.95, 15.46) |
| KR | 9.91 (7.88, 11.94) | 0.35 (0.23, 0.47) | 0.12 (0.07, 0.17) | 0.20 (0.10, 0.30) | 10.73 (8.64, 12.82) |
| VB | 13.47 (7.13, 19.81) | 0.31 (0.12, 0.50) | 0.45 (0.18, 0.72) | 0.03 (0.01, 0.06) | 14.46 (8.14, 20.78) |
| All districts | 9.99 (8.06, 11.92) | 0.81 (0.49, 1.12) | 0.32 (0.22, 0.42) | 0.12 (0.06, 0.07) | 11.46 (9.43, 13.50) |
Values are presented as the mean with the 95% confidence interval (CI) in parentheses. Bolded values represent within-species CIs that do not overlap other the CIs of other districts
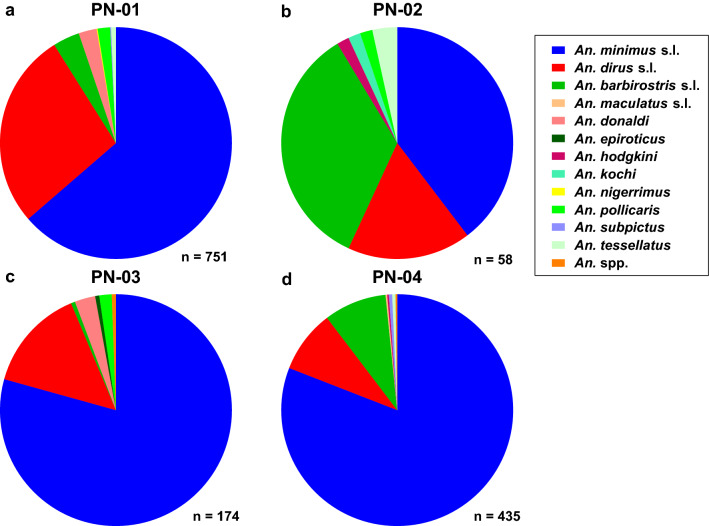
In Phanom, 12 Anopheles species were morphologically identified from four clusters. Anopheles minimus (s.l.) was the most abundant Anopheles species captured across all four clusters (Fig. 5a–d), and the second and third most abundant Anopheles species by cluster were An. dirus (s.l.) and An. barbirostris (s.l.) in PN-01 (Fig. 5a), An. barbirostris (s.l.) and An. dirus (s.l.) in PN-02 (Fig. 5b), An. dirus (s.l.) and An. donaldi in PN-03 (Fig. 5c) and An. barbirostris (s.l.) and An. dirus (s.l.) in PN-04 (Fig. 5d).
Fig. 5.
Morphological composition of Anopheles identified from the four clusters (a–d; PN-01–PN-04) in Phanom district
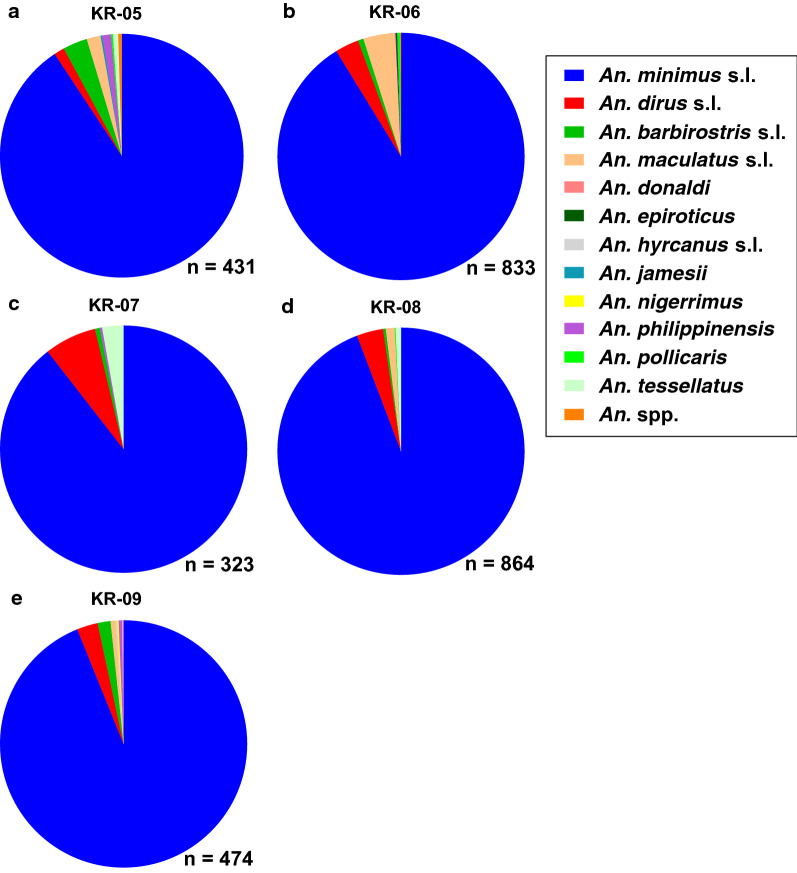
In Khiri Rat Nikhom, 12 Anopheles species were morphologically identified from five clusters. Anopheles minimus (s.l.) was the most abundant Anopheles species captured across all five KR clusters (Fig. 6a–e), and the second and third most abundant Anopheles species by cluster were An. barbirostris (s.l.) and An. maculatus (s.l.) in KR-05 (Fig. 6a), An. maculatus (s.l.) and An. dirus (s.l.) in KR-06 (Fig. 6b), An. dirus (s.l.) and An. tesselatus in KR-07 (Fig. 6c), An. dirus (s.l.) and An. maculatus (s.l.) in KR-08 (Fig. 6d) and An. dirus (s.l.) and An. barbirostris (s.l.) in KR-09 (Fig. 6e).
Fig. 6.
Morphological composition of Anopheles identified from the five clusters (a–e; KR-05–KR-09) in Khiri Rat Nikhom district
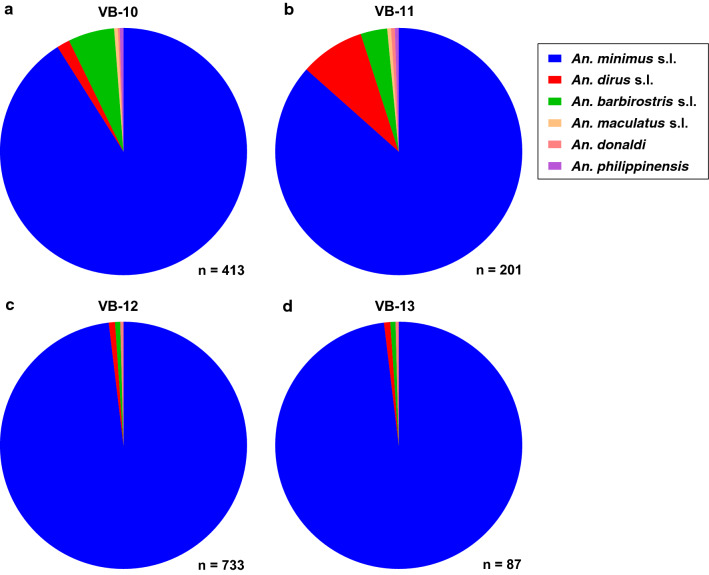
In Vibhavadi, only six Anopheles species were morphologically identified from four clusters. Anopheles minimus (s.l.) was the most abundant Anopheles species captured across all four VB clusters (Fig. 7a–d), and the second and third most abundant Anopheles species by cluster were An. barbirostris (s.l.) and An. dirus (s.l.) in VB-10 and VB-13 (Fig. 7a, d) and An. dirus (s.l.) and An. barbirostris (s.l.) in VB-11 and VB-12 (Fig. 7b, c).
Fig. 7.
Morphological composition of Anopheles identified from four clusters (a–d; VB-10–VB-13) in Vibhavadi district
A total of 879 Anopheles were identified molecularly to species level by AS-PCR or sequencing. Of the Funestus group, which contains the Minimus complex, 99.80% (n = 484) were An. minimus (s.s.) and 0.20% (n = 1) were An. aconitus. The Dirus complex was 100% (n = 347) An. baimaii. Of the Maculatus group, 93.62% (n = 44) were An. maculatus (s.s.) and 6.38% (n = 3) were An. sawadwongporni. One An. epiroticus and one An. nigerrimus specimen were identified by sequencing. The Barbirostris group members were identified to species level based on morphology. Of the Barbirostris group, 69.37% (n = 154) were An. barbirostris, 14.42% (n = 32) were An. donaldi, 10.36% (n = 23) were An. pollicaris, 4.95% (n = 11) were An. campestris and 0.90% (n = 2) were An. hodgkini.
Plasmodium infection status
None of the 879 Anopheles mosquitoes tested were Plasmodium positive.
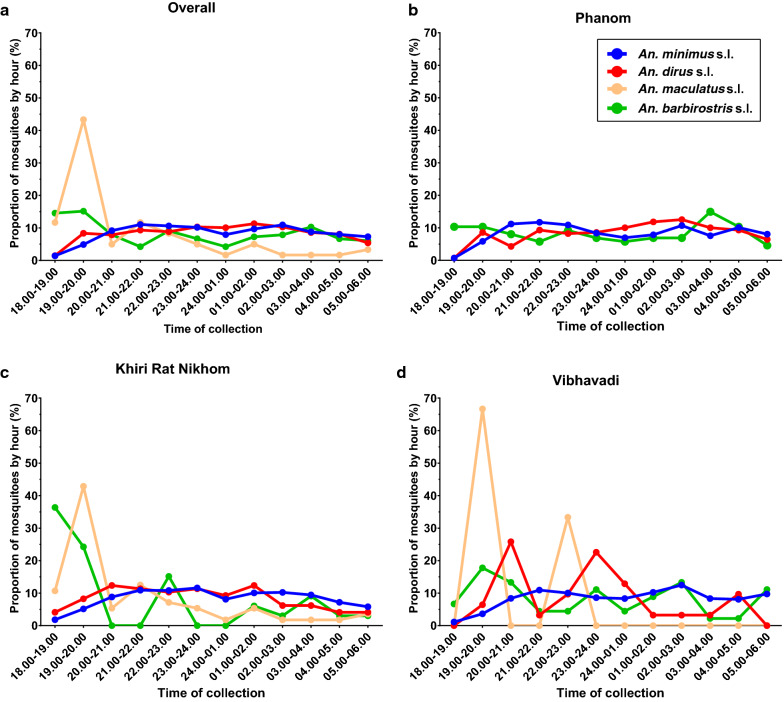
Anopheles mosquito collection by time
Overall, there were significant differences in hour of collection by species (Kruskal–Wallis H-test: χ2 = 80.89, df = 3, P < 0.0001, n = 5666) with significantly more An. barbirostris (s.l.) and An. maculatus (s.l.) caught earlier in the night compared to An. minimus (s.l.) (Dunn’s multiple comparison test: P = 0.0001, P < 0.0001, respectively) and An. dirus (s.l.) (Dunn’s multiple comparison test: P = 0.0082, P < 0.001, respectively). Overall, almost 60% of An. maculatus (s.l.) and 30% of the An. barbirsostris (s.l.) were captured between 18:00 h and 20:00 h (Fig. 8a). In Phanom, there were no significant differences (Kruskal–Wallis H-test: χ2 = 6.892, df = 2, P = 0.0754, n = 1358) in time of Anopheles capture between the species (Fig. 8b), although too few An. maculatus (s.l.) (n = 1) were captured to be included in the analysis. In Khiri Rat Nikhom, there were significant differences in hour of collection by species (Kruskal–Wallis H-test: χ2 = 82.19, df = 3, P < 0.0001, n = 2884), with significantly more An. barbirostris (s.l.) and An. maculatus (s.l.) caught earlier in the night compared to An. minimus (s.l.) (Dunn’s multiple comparison test: P < 0.0001, P < 0.0001, respectively) and An. dirus (s.l.) (Dunn’s multiple comparison test: P = 0.0164, P < 0.001, respectively). In Vibhavadi, there were significant differences in hour of collection by species (Kruskal–Wallis H-test: χ2 = 21.61, df = 2, P < 0.0001, n = 1424), with significantly more An. minimus (s.l.) caught later in the night compared to An. dirus (s.l.) (Dunn’s multiple comparison test: P = 0.0108) and An. barbirostris (s.l.) (Dunn’s multiple comparison test: P = 0.0457). Too few An. maculatus (s.l.) (n = 3) were captured in Vibhavadi to be included in the analysis. Interestingly, there were significant differences in capture times across all three districts for An. minimus (s.l.) (Kruskal–Wallis H-test: χ2 = 16.66, df = 2, P = 0.0002, n = 5035), An. dirus s.l. (Kruskal–Wallis H-test: χ2 = 17.4, df = 2, P = 0.0002, n = 407) and An. barbirostris (s.l.) (Kruskal–Wallis H-test: χ2 = 12.61, df = 2, P = 0.0018, n = 165). Anopheles minimus (s.l.) were captured later in the night in Vibhavadi district compared to Phanom district (Dunn’s multiple comparison test: P = 0.0275) and Khiri Rat Nikhom district (Dunn’s multiple comparison test: P = 0.0002). Anopheles dirus (s.l.) were captured later in the night in Phanom compared to Khiri Rat Nikhom (Dunn’s multiple comparison test: P = 0.0023) and Vibhavadi (Dunn’s multiple comparison test: P = 0.0088). Anopheles barbirostris (s.l.) were captured earlier in the night in Khiri Rat Nikhom compared to Phanom (Dunn’s multiple comparison test: P = 0.0013) and Vibhavadi (Dunn’s multiple comparison test: P = 0.0273).
Fig. 8.
Proportion of Anopheles species collected by hour from all districts (a), Phanom (b), Khiri Rat Nikhom (c) and Vibhavadi (d)
Anopheles mosquito parity status
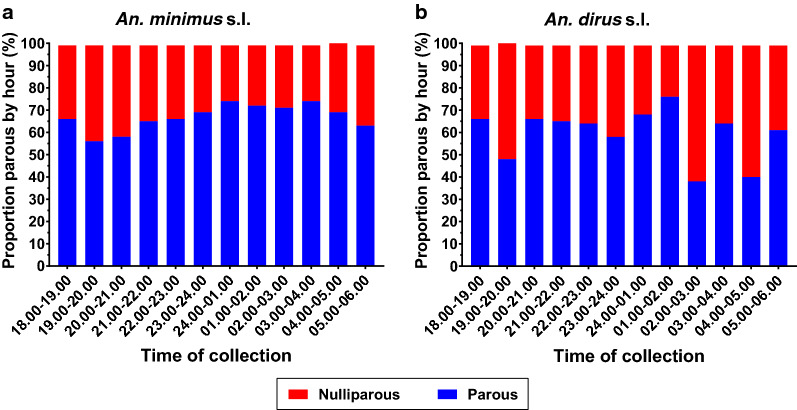
A total of 3509 An. minimus (s.l.) and 322 An. baimaii were dissected to determine parity. Across the three districts the proportion of parous An. minimus (s.l.) and An. dirus (s.l.) ranged from 51.71 to 71.64% and from 55.32 to 74.71%, respectively (Table 3).
Table 3.
Number and proportion of parous and nulliparous An. minimus (s.l.) and An. dirus (s.l.) by district
| Study sites | An. minimus (s.l.) | An. dirus (s.l.) | ||||||
|---|---|---|---|---|---|---|---|---|
| Parous (n) | Nulliparous (n) | Total (n) | Parity (%) | Parous (n) | Nulliparous (n) | Total (n) | Parity (%) | |
| PN | 287 | 268 | 555 | 51.71 | 130 | 105 | 235 | 55.32 |
| KR | 1437 | 569 | 2006 | 71.64 | 65 | 22 | 87 | 74.71 |
| VB | 651 | 297 | 948 | 68.67 | 18 | 12 | 30 | 60.00 |
| Total | 2375 | 1134 | 3509 | 67.68 | 213 | 139 | 352 | 60.51 |
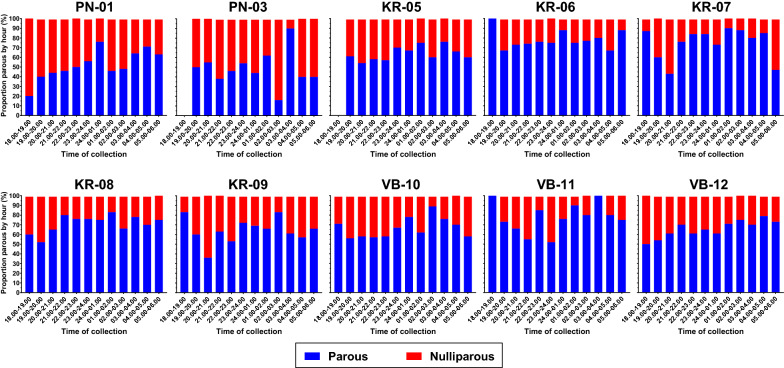
Overall, there was a significant increasing trend in the proportion of parous An. minimus (s.l.) captured by hour throughout the night [Wald Chi-square: χ2 = 17.31, P = 0.000, odds ratio (OR) 1.0535, 95% confidence interval (CI) 1.0279–1.0796, n = 3400] (Fig. 9a). Only clusters with > 100 dissected An. minimus (s.l.) were included in the analyses (i.e. PN-01, PN-03, KR-05, KR-06, KR-07, KR-08, KR-09, VB-10, VB-11, VB-12). While all clusters showed an increasing trend in the proportion of parous An. minimus (s.l.) throughout the night (Fig. 10), only PN-01 and VB-12 were significant (Table 4). For An. dirus (s.l.) there was no significant trend in the proportion of parous mosquitoes by hour throughout the night (Wald Chi-square: χ2 = 0.46, P = 0.497, OR 0.9702, 95% CI 0.8891–1.0587, n = 229) (Fig. 9b). Only clusters with > 20 dissected An. dirus (s.l.) (i.e. PN-01, PN-03, PN-04) were included in the analysis.
Fig. 9.
Proportion of Anopheles minimus (a) and An. dirus (b) that were parous or nulliparous collected per hour from all clusters with at least 100 dissected An. minimus and 20 dissected An. dirus
Fig. 10.
Proportion of Anopeles minimus (s.l.) that were parous or nulliparous collected per hour by cluster (n = 3400)
Table 4.
Trend in parity by hour and cluster for Anopheles minimus (s.l.) (n = 3400)
| Clustera | P-value | OR (95% CI) | n |
|---|---|---|---|
| PN-01 | 0.002 | 1.1083 (1.0393–1.1819) | 392 |
| PN-03 | 0.680 | 1.0250 (0.9117–1.1523) | 121 |
| KR-05 | 0.251 | 1.0493 (0.9665–1.1393) | 335 |
| KR-06 | 0.438 | 1.0298 (0.9563–1.1089) | 501 |
| KR-07 | 0.884 | 1.0069 (0.9180–1.1044) | 280 |
| KR-08 | 0.102 | 1.0520 (0.9900–1.1180) | 595 |
| KR-09 | 0.250 | 1.0478 (0.9676–1.1347) | 282 |
| VB-10 | 0.530 | 1.0217 (0.9555–1.0925) | 329 |
| VB-11 | 0.133 | 1.1141 (0.9675–1.2829) | 146 |
| VB-12 | 0.034 | 1.0824 (1.0059–1.1646) | 419 |
n number of mosquitoes dissected, OR odds ratio
aAll clusters showed an increasing trend in the proportion of parous An. minimus (s.l.) throughout the night (Fig. 10), but the trend was only significant for PN-01 and VB-12 (bold)
Power calculation
The purpose of this field study was to assess the potential of Surat Thani to serve as the location for future entomological evaluation of ivermectin MDAs. As Plasmodium infection rates in Anopheles in the GMS are extremely low, either survival or parity become the ideal metrics to measure. However, capturing indoor-resting, blood-fed Anopheles in the GMS is very difficult, rendering assessment of mosquito survival as done previously in Africa [12, 13] impossible. The power calculation to assess the impact of ivermectin MDA on mosquito parity was based on An. minimus (s.l.) as it is a primary malaria vector, the most abundant Anopheles species captured in Surat Thani (87.16%; 5035/5777) and the most ivermectin-sensitive malaria vector in the GMS evaluated to date [16, 17]. Parity rates (P0 = 67.68%; 2375/3509) from ten clusters wherein > 100 An. minimus (s.l.) were collected and dissected were used to calculate an intra-cluster correlation (ICC) value to be used for sample size calculations. Individual mosquito parity results were assessed with a random effects logistic regression model to obtain an ICC of 0. 0378. To demonstrate an effect, based on a two-sided α = 0.05, a parity rate at baseline and in control villages of P0 = 67.68%, a treatment effect size = 34% reduction, meaning treatment villages with a parity rate of P1 = 44.67% after MDA, and an ICC = 0.0378 requires at least four clusters per treatment arm and a minimum of 300 mosquitoes dissected per cluster to provide 82% power. A conservative treatment effect size of 34% was predicted based on a previously developed model for ivermectin MDA [41] parameterized with An. minimus (s.s.) ivermectin susceptibility data [17]. This treatment effect size is reasonable and supported by the following: (i) ivermectin MDAs in West Africa reduced the parity rate in An. gambiae by 30% [13]; (ii) An. minimus [7-day lethal concentration 50 (LC50) = 14.7 ng/ml) [17] is more susceptible to ivermectin than An. gambiae (7-day LC50 = 15.9 ng/ml) [42]; and (iii) we plan to administer 400 µg/kg ivermectin at our field site whereas 150–200 µg/kg was used in the West Africa MDA trials [13].
Discussion
This study represents the most intensive and detailed analysis of Anopheles bionomics from Surat Thani province, Thailand. These surveys were conducted to determine which clusters in Surat Thani were most appropriate for evaluation of the entomological impacts of ivermectin MDA on Anopheles. Most (95.26%) of the Anopheles species collected from Phanom, Khiri Rat Nikhom and Vibhavadi districts were primary or secondary malaria vectors. In addition to detailed hourly collection data, this study presents data on the parity status throughout the night for the primary malaria vectors, An. dirus (s.l.) and An. minimus (s.l.). Finally, a power calculation was performed to determine the number of clusters that should be utilized to assess the impact of ivermectin MDA on An. minimus parity.
Surat Thani is unique in that it is a malarious province in Thailand that is not located along an international border. It has some of the highest rainforest coverage in the GMS and the highest rubber plantation coverage in Thailand, making it an ideal habitat for malaria vectors in the GMS. Indeed, of the 15 species captured in these surveys, 11 were either primary malaria vectors [An. minimus (s.l.), An. dirus (s.l.), An. maculatus (s.l.)], secondary malaria vectors [An. epiroticus] or suspected malaria vectors [An. barbirostris (s.l.), An. hodgkini, An. hyrcanus (s.l.), An. nigerrimus, An. philippinensis, An. kochi, An. tessellatus]. An. minimus (s.l.) accounted for 87.16% (5035/5777) and An. dirus (s.l.) 7.15% (407/5777) of the total Anopheles collected., respectively. Molecular identification confirmed that of all An. minimus (s.l.) collected, 99.80% were An. minimus (s.s.) (n = 484) and 0.2% were An. aconitus (n = 1), and of all An. dirus (s.l.) collected, 100% were An. baimaii (n = 348). Since the secondary and suspected vectors were captured in such low numbers, it is likely that the primary malaria vectors, An. minimus (s.s.) and An. baimaii, are largely responsible for Plasmodium transmission in the study area. However, as no specimens were Plasmodium positive (0/879), it cannot be confirmed that these vectors are solely responsible for transmission. A previous study in Ubon Ratchathani province, in northeastern Thailand, reported that suspected malaria vectors An. barbirostris (s.l.), An. philippinensis and An. hyrcanus (s.l.) are highly zoophagic, feeding mostly on cattle [43]. Since we only used the HLC method, this feeding preference may explain the low abundance of these species in the study area, making it difficult to rule them out as possible contributors to Plasmodium transmission in Surat Thani. One limitation of this study is the lack of assessment on the proximity of the mosquito collection sites to potential influential factors, such as the forest, larval habitat and livestock populations.
Primary malaria vectors in the GMS tend to be collected more frequently outdoors than indoors [9–11]. Since the aim of this study was to collect as many human host-seeking Anopheles as possible, all HLCs were performed outdoors. Results from a cross-sectional survey in Surat Thani in the same study area where HLCs were performed indicated that staying outdoors is a primary risk factor for asymptomatic Plasmodium carriage, suggesting that most of the transmission occurs outside the home [26]. This finding reinforces the potential usefulness of ivermectin MDA in the GMS as it can target the Anopheles malaria vector regardless of location or time.
Vibhavadi had the fewest number of Anopheles species collected, with only six species, and Anopheles species diversity was similar to that in Khiri Rat Nikhom, which were both lower than species diversity in Phanom (Table 1). This reduced Anopheles diversity in Vibhavadi could be due in part to seasonality and the limited sampling duration from July to October, while mosquitoes were collected from February to October in Khiri Rat Nikhom and Phanom. Another interesting point about mosquito collections in Vibhavadi was that An. minimus (s.l.) were captured later in the night compared to Phanom (P = 0.0275) and Khiri Rat Nikhom (P = 0.0002). This could be due to the production of durian in Vibhavadi as thermal fogging with malathion occurs at night-time for the control of several durian crop pests, in particular Scirtothrips dorsalis (Order Thysanoptera; Family Thripidae) and Allocaridara malayensis (Order Homoptera; Family Psyllidae), and this fogging was observed at some of the mosquito collection sites during HLCs in Vibhavadi clusters. Vibhavadi has the fourth highest coverage (1.33%) of durian plantation of the 19 districts in Surat Thani, with Khiri Rat Nikhom having the eighth highest coverage (0.33%) and Phanom the twelfth highest coverage (0.18%) [44].
The abundance of An. dirus (s.l.) varied among districts, with the greatest numbers captured in Phanom, likely due to geographical (Figs. 1, 2) and biological characteristics as the Phanom study site is surrounded by national parks comprised of primary old growth rain forest and steep hillsides. Furthermore, rubber plantations adjacent to the forest create a suitable habitat for An. dirus (s.l.) proliferation [7, 22]. Anopheles dirus (s.l.) were captured later in the night in Phanom compared to Khiri Rat Nikhom (P = 0.0023) and Vibhavadi (P = 0.0088), but this may have been an artifact due to the smaller number of An. dirus (s.l.) captured in Khiri Rat Nikhom and Vibhavadi districts.
These surveys recorded some members of the Barbirostris group in Surat Thani for the first time, including An. hodgkini, An. donaldi and An. pollicaris. However, it is possible that these species may have been identified as An. barbirostris (s.l.) previously as they are difficult to distinguish morphologically [27]. Future work in the study area should identify the members of the Barbirostris group by molecular methods as not all species in this group are malaria vectors [45]. Anopleles sawadwongporni was also recorded for the first time in Surat Thani, but this species may not have been identified in previous surveys due to lack of molecular species identification [27]. Anopheles baimaii is also a newly recorded species for Surat Thani, likely missed previously due to the lack of molecular species identification. It is somewhat surprising that more members of the Dirus complex were not identified because An. dirus (s.s.), An. cracens, An. nemophilous and An. scanloni have been observed in the adjacent provinces of Phang Nga, Krabi, Nakhon Si Thammarat and Ranong [7].
There were no Plasmodium-positive Anopheles (0/879) specimens detected. However, this is not very surprising as the likelihood of finding sporozoite-infected Anopheles in the GMS is very low, typically lower than 1:1000 [11]. This is why the population age structure (i.e. parity rate) was selected as the primary entomological outcome indicator to assess impact of ivermectin MDA on Anopheles populations in Surat Thani. This study found an overall An. minimus (s.l.) parity of 67.68% (2375/3509), which is comparable with the results of other surveys in Thailand [3, 4, 46, 47]. Similar to the results reported by Sithiprasana et al. [3], little fluctuation in An. minimus (s.l.) parity was observed from cluster to cluster, with an ICC value of 0.0378. For An. minimus (s.l.), there was a significant trend of increasing parity by hour of collection, suggesting that older An. minimus tend to feed later at night (Fig. 9a), but no trend was observed for An. dirus (s.l.) (Fig. 9b). A power calculation determined that an An. minimus (s.l.) parity reduction treatment effect size = 34%, with four clusters per treatment arm and a minimum of 300 mosquitoes dissected per cluster at an α = 0.05 will provide 82% power to detect a significant difference in the population age structure (i.e. parity). Due to reduced malaria cases and transmission in Surat Thani [26], evaluation of the Anopheles parity rate is expected to provide a valuable outcome to assess the impact of ivermectin MDA on malaria transmission.
Conclusions
An abundance of Anopheles primary malaria vectors were captured in Surat Thani. This study illustrates that Surat Thani will be an ideal field site for evaluating the impacts of ivermectin MDA on local Anopheles population age structure.
Acknowledgements
We are grateful to the staff of the Surat Thani Vector-Borne Diseases Control Center 11.3 and the Surat Thani Vector-Borne Diseases Control Units in Phanom, Kiri Rat Nikhom and Vibhavadi districts for their kind support and assistance. We thank the village chiefs, village health volunteers and community members who facilitated the field work. Our sincere thanks go to all mosquito collector volunteers for their assistance with field collections, and to the community for allowing us to work in their villages. We thank Dr. Hannah Slater for assistance with model estimation of effect of ivermectin MDA on An. minimus parity. We thank Dr. Alvaro Molina-Cruz for providing P. falciparum-positive An. dirus (s.s.) specimens. We thank Bousaraporn Tippayachai and Sommai Promsathaporn for their assistance with processing mosquitoes for molecular identification.
Disclaimer
Material has been reviewed by the Walter Reed Army Institute of Research. There is no objection to its presentation and/or publication. The opinions or assertions contained herein are the private views of the author, and are not to be construed as official, or as reflecting true views of the Department of the Army or the Department of Defense. The investigators have adhered to the policies for protection of human subjects as prescribed in AR 70–25.
Abbreviations
- AS-PCR
Allele-specific PCR
- DMSO
Dimethyl sulfoxide
- GMS
Greater Mekong Subregion
- HLC
Human landing collection
- HRPO
Human Research Protection Office
- ICC
Intra-cluster correlation
- IRS
Indoor residual spraying
- KR
Khiri Rat Nikhom
- LLINs
Long-lasting insecticide-treated nets
- MDA
Mass drug administration
- MEGA
Molecular evolutionary genetics analysis
- MoPH
Ministry of Public Health
- PN
Phanom
- VB
Vibhavadi
- WRAIR
Walter Reed Army Institute of Research
Authors’ contributions
NW, KCK designed the study; NW, OK, KCK, PT, UN performed mosquito collections and field processing; PS, KK, AK, WN performed mapping efforts; JS, RT performed molecular analyses; SC, MM, KCK performed statistical analyses; ST, VS, SAD, PWM, WN, JSP, JS provided administrative oversight; NW, KCK wrote the first draft. All authors read and approved the final manuscript.
Funding
This study was funded by the Congressionally Directed Medical Research Program (PR150881). The funders had no role in the design, analysis, interpretation, or writing of the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Walter Reed Army Institute of Research (WRAIR#2430), the Human Research Protection Office (HRPO Log No. 19919.2a/A-19919.2b), and the Ethical Review Committee for Research in Human Subjects, Ministry of Public Health, Thailand (Thai MoPH Ref No. 25/2560). All mosquito collectors were enrolled by appointed Vector-Borne Disease Control center staff.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Narenrit Wamaket, Email: narenritwamaket@gmail.com.
Oranicha Khamprapa, Email: auranicha_k@hotmail.com.
Sittinont Chainarin, Email: sittinont.c@gmail.com.
Panisa Thamsawet, Email: Panisa.tw@gmail.com.
Ubolrat Ninsaeng, Email: jeabubolrat@hotmail.com.
Suttipong Thongsalee, Email: laksutt@gmail.com.
Veerast Suwan, Email: veerast_2522@hotmail.com.
Jira Sakolvaree, Email: JiraS.ca@afrims.org.
Ratree Takhampunya, Email: RatreeT.fsn@afrims.org.
Silas A. Davidson, Email: silas.a.davidson.mil@mail.mil
Patrick W. McCardle, Email: patrick.mccardle.mil@afrims.org
Patiwat Sa-angchai, Email: patiwat.saa@mahidol.edu.
Mavuto Mukaka, Email: mavuto@tropmedres.ac.
Kirakorn Kiattibutr, Email: kirakorn.kia@mahidol.edu.
Amnat Khamsiriwatchara, Email: amnatk@biophics.org.
Wang Nguitragool, Email: wang.ngu@mahidol.edu.
Jetsumon Sattabongkot, Email: jetsumon.pra@mahidol.edu.
Jeeraphat Sirichaisinthop, Email: grphat@gmail.com.
Kevin C. Kobylinski, Email: kobylinskikevin@yahoo.com
References
- 1.World Health Organization. World malaria report 2020: 20 years of global progress and challenges. 2020. Geneva: World Health Organization. https://www.who.int/publications/i/item/9789240015791. Accessed 20 Jan 2021.
- 2.Rattanarithikul R, Konishi E, Linthicum K. Detection of Plasmodium vivax and Plasmodium falciparum circumsporozoite antigen in anopheline mosquitoes collected in southern Thailand. Am J Trop Med Hyg. 1996;54(2):114–21. doi: 10.4269/ajtmh.1996.54.114. [DOI] [PubMed] [Google Scholar]
- 3.Sithiprasasna R, Linthicum K, Liu G, Jones J, Singhasivanon P. Some entomological observations on temporal and spatial distribution of malaria vectors in three villages in northwestern Thailand using a geographic information system. Southeast Asian J Trop Med Public Health. 2003;34(3):505–16. [PubMed] [Google Scholar]
- 4.Zollner G, Sattabongkot J, Vaughan J, Kankaew P, Robert L, Thimasarn K, et al. Longitudinal evaluation of malaria epidemiology in an isolated village in Western Thailand: I. Study site and adult Anopheline bionomics. Southeast Asian J Trop Med Public Health. 2016;47(3):341–65. [PubMed] [Google Scholar]
- 5.Sriwichai P, Samung Y, Sumruayphol S, Kiattibutr K, Kumpitak C, Payakkapol A, et al. Natural human Plasmodium infections in major Anopheles mosquitoes in western Thailand. Parasites Vectors. 2016;9:e17. doi: 10.1186/s13071-016-1295-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwansomboon N, Chaumeau V, Kittiphanakun P, Cerqueira D, Corbel V, Chareonviriyaphap T. Vector bionomics and malaria transmission along the Thailand-Myanmar border: a baseline entomological survey. J Vector Ecol. 2017;42(1):84–93. doi: 10.1111/jvec.12242. [DOI] [PubMed] [Google Scholar]
- 7.Obsomer V, Defourny P, Coosemans M. The Anopheles dirus complex: spatial distribution and environmental drivers. Malar J. 2007;6:e26. doi: 10.1186/1475-2875-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cui L, Yan G, Sattabongkot J, Chen B, Cao Y, Fan Q, et al. Challenges and prospects for malaria elimination in the Greater Mekong Subregion. Acta Trop. 2012;121(3):240–5. doi: 10.1016/j.actatropica.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Bortel W, Trung H, Hoi L, Ham N, Chut N, Luu N, et al. Malaria transmission and vector behaviour in a forested malaria focus in central Vietnam and the implications for vector control. Malar J. 2010;9:e373. doi: 10.1186/1475-2875-9-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trung H, van Bortel W, Sochantha T, Keokenchanh K, Briët O, Coosemans M. Behavioural heterogeneity of Anopheles species in ecologically different localities in southeast Asia: a challenge for vector control. Trop Med Int Health. 2005;10(3):251–62. doi: 10.1111/j.1365-3156.2004.01378.x. [DOI] [PubMed] [Google Scholar]
- 11.Sinka M, Bangs M, Manguin S, Chareonviriyaphap T, Patil A, Temperley W, et al. The dominant Anopheles vectors of human malaria in the Asia-Pacific region: occurrence data, distribution maps and bionomic précis. Parasites Vectors. 2011;4:e89. doi: 10.1186/1756-3305-4-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sylla M, Kobylinski K, Gray M, Chapman P, Sarr M, Rasgon J, et al. Mass drug administration of ivermectin in south-eastern Senegal reduces the survivorship of wild-caught, blood fed malaria vectors. Malar J. 2010;9:e365. doi: 10.1186/1475-2875-9-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alout H, Krajacich B, Meyers J, Grubaugh N, Brackney D, Kobylinski K, et al. Evaluation of ivermectin mass drug administration for malaria transmission control across different west African environments. Malar J. 2014;13:e417. doi: 10.1186/1475-2875-13-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kobylinski K, Sylla M, Chapman P, Sarr M, Foy B. Ivermectin mass drug administration to humans disrupts malaria parasite transmission in senegalese villages. Am J Trop Med Hyg. 2011;85(1):3–5. doi: 10.4269/ajtmh.2011.11-0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foy B, Alout H, Seaman J, Rao S, Magalhaes T, Wade M, et al. Efficacy and risk of harms of repeat ivermectin mass drug administrations for control of malaria (RIMDAMAL): a cluster-randomised trial. Lancet. 2019;393(10180):1517–26. doi: 10.1016/S0140-6736(18)32321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kobylinski K, Ubalee R, Ponlawat A, Nitatsukprasert C, Phasomkulsolsil S, Wattanakul T, et al. Ivermectin susceptibility and sporontocidal effect in Greater Mekong Subregion Anopheles. Malar J. 2017;16:e280. doi: 10.1186/s12936-017-1923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kobylinski K, Jittamala P, Hanboonkunupakarn B, Pukrittayakamee S, Pantuwattana K, Phasomkulsolsil S, et al. Safety, pharmacokinetics, and mosquito-lethal effects of ivermectin in combination with dihydroartemisinin-piperaquine and primaquine in healthy adult Thai subjects. Clin Pharmacol Ther. 2020;107(5):1221–30. doi: 10.1002/cpt.1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Erhart A, Ngo D, Phan V, Ta T, Van Overmeir C, Speybroeck N, et al. Epidemiology of forest malaria in central Vietnam: a large scale cross-sectional survey. Malar J. 2005;4:e58. doi: 10.1186/1475-2875-4-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prothero R. Malaria, forests and people in southeast Asia. Singap J Trop Geogr. 1999;20(1):76–85. doi: 10.1111/1467-9493.00044. [DOI] [Google Scholar]
- 20.Division of Vector Borne Diseases, Department of Disease Control, Ministry of Public Health. Malaria online: the digital surveillance system for Thailand malaria elimination. Thailand: Department of Disease Control Ministry of Public Health Thailand. 2019; p 1–46.
- 21.Singhasivanon P, Thimasarn K, Yimsamran S, Linthicum K, Nualchawee K, Dawreang D, et al. Malaria in tree crop plantations in south-eastern and western provinces of Thailand. Southeast Asian J Trop Med Public Health. 1999;30(3):399–404. [PubMed] [Google Scholar]
- 22.Bhumiratana A, Sorosjinda-Nunthawarasilp P, Kaewwaen W, Maneekan P, Pimnon S. Malaria-associated rubber plantations in Thailand. Travel Med Infect Dis. 2013;11(1):37–50. doi: 10.1016/j.tmaid.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Chujun S, Chaivisit P, Chutinantakul A. Epidemiological characteristics and factors related to malarial disease in Thai and migrant patients in the upper part of southern Thailand. Dis Control J. 2019;45(4):380–91. [Google Scholar]
- 24.Office of Agricultural Economics. Rubber: a total planting area, total harvesting area, total yield, yield per rai, for country level, regions level, and provincial level. 2018. http://www.oae.go.th/view/1/ตารางแสดงรายละเอียดยางพารา/TH-TH. Accessed 19 May 2020.
- 25.Thailand Ministry of Health. Thailand Malaria Elimination Program. 2019. http://203.157.41.215/malariaR10/index_v2.php. Accessed 21 April 2020.
- 26.Shimizu S, Chotirat S, Dokkulab N, Hongchad I, Khowsroy K, Kiattibutr K, et al. Malaria cross-sectional surveys identified asymptomatic infections of Plasmodium falciparum, Plasmodium vivax and Plasmodium knowlesi in Surat Thani, a southern province of Thailand. Int J Infect Dis. 2020;96:445–51. doi: 10.1016/j.ijid.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 27.Aumaung B, Sevana J, Sinakom B, Yongchaitrakol S, Muernrat Y. Study on long lasting insecticidal nano jacket (LLINJ) for malaria vector control. Dis Control J. 2019;44(4):448–58. [Google Scholar]
- 28.Muenworn V, Sungvornyothin S, Kongmee M, Polsomboon S, Bangs M, Akrathanakul P, et al. Biting activity and host preference of the malaria vectors Anopheles maculatus and Anopheles sawadwongporni (Diptera: Culicidae) in Thailand. J Vector Ecol. 2009;34(1):62–9. doi: 10.1111/j.1948-7134.2009.00008.x. [DOI] [PubMed] [Google Scholar]
- 29.Tainchum K, Kongmee M, Manguin S, Bangs M, Chareonviriyaphap T. Anopheles species diversity and distribution of the malaria vectors of Thailand. Trends Parasitol. 2015;31(3):109–19. doi: 10.1016/j.pt.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Rattanarithikul R, Harrison B, Harbach R, Panthusiri P, Coleman R, Panthusiri P. Illustrated keys to the mosquitoes of Thailand. IV. Anopheles. Southeast Asian J Trop Med Public Health. 2006;37:1–128. [PubMed] [Google Scholar]
- 31.Walton C, Handley J, Kuvangkadilok C, Collins F, Harbach R, Baimai V, et al. Identification of five species of the Anopheles dirus complex from Thailand, using allele-specific polymerase chain reaction. Med Vet Entomol. 1999;13(1):24–32. doi: 10.1046/j.1365-2915.1999.00142.x. [DOI] [PubMed] [Google Scholar]
- 32.Walton C, Somboon P, O'Loughlin S, Zhang S, Harbach R, Linton Y, et al. Genetic diversity and molecular identification of mosquito species in the Anopheles maculatus group using the ITS2 region of rDNA. Infect Genet Evol. 2007;7(1):93–102. doi: 10.1016/j.meegid.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Garros C, Koekemoer L, Coetzee M, Coosemans M, Manguin S. A single multiplex assay to identify major malaria vectors within the African Anopheles funestus and the Oriental An. minimus groups. Am J Trop Med Hyg. 2004;70(6):583–90. doi: 10.4269/ajtmh.2004.70.583. [DOI] [PubMed] [Google Scholar]
- 34.Marcombe S, Maithaviphet S, Bobichon J, Phommavan N, Nambanya S, Corbel V, et al. New insights into malaria vector bionomics in Lao PDR: a nationwide entomology survey. Malar J. 2020;19(1):e396. doi: 10.1186/s12936-020-03453-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beebe N, Saul A. Discrimination of all members of the Anopheles punctulatus complex by polymerase chain reaction–restriction fragment length polymorphism analysis. Am J Trop Med Hyg. 1995;53(5):478–81. doi: 10.4269/ajtmh.1995.53.478. [DOI] [PubMed] [Google Scholar]
- 36.Saeung A, Baimai V, Otsuka Y, Rattanarithikul R, Somboon P, Junkum A, et al. Molecular and cytogenetic evidence of three sibling species of the Anopheles barbirostris Form A (Diptera:Culicidae) in Thailand. Parasitol Res. 2008;102(3):499–507. doi: 10.1007/s00436-007-0788-0. [DOI] [PubMed] [Google Scholar]
- 37.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol Biol Evol. 2013;30(12):2725–9. doi: 10.1093/molbev/mst197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kimura M, Kaneko O, Liu Q, Zhou M, Kawamoto F, Wataya Y, et al. Identification of the four species of human malaria parasites by nested PCR that targets variant sequences in the small subunit rRNA gene. Parasitol Int. 1997;46(2):91–5. doi: 10.1016/S1383-5769(97)00013-5. [DOI] [Google Scholar]
- 39.Shannon C. A mathematical theory of communication. Bell System Tech J. 1948;27(3):379–423. doi: 10.1002/j.1538-7305.1948.tb01338.x. [DOI] [Google Scholar]
- 40.Simpson E. Measurement of diversity. Nature. 1949;163:688. doi: 10.1038/163688a0. [DOI] [Google Scholar]
- 41.Slater H, Walker P, Bousema T, Okell L, Ghani A. The potential impact of adding ivermectin to a mass treatment intervention to reduce malaria transmission: a modelling study. J Infect Dis. 2014;210(12):1972–80. doi: 10.1093/infdis/jiu351. [DOI] [PubMed] [Google Scholar]
- 42.Kobylinski K, Foy B, Richardson J. Ivermectin inhibits the sporogony of Plasmodium falciparum in Anopheles gambiae. Malar J. 2012;11:e381. doi: 10.1186/1475-2875-11-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marasri N, Overgaard H, Sumarnrote A, Thanispong K, Corbel V, Chareonviriyaphap T. Abundance and distribution of Anopheles mosquitoes in a malaria endemic area along the Thai-Lao border. J Vector Ecol. 2017;42(2):325–34. doi: 10.1111/jvec.12273. [DOI] [PubMed] [Google Scholar]
- 44.Office of the Permanent Secretary for Ministry of Agriculture and Cooperatives. Surat Thani provincial product information: durian. 2015. https://www.opsmoac.go.th/suratthani-dwl-files-401091791958. Accessed 19 May 2020.
- 45.Brosseau L, Udom C, Sukkanon C, Chareonviriyaphap T, Bangs M, Saeung A, et al. A multiplex PCR assay for the identification of five species of the Anopheles barbirostris complex in Thailand. Parasites Vectors. 2019;12(1):e223. doi: 10.1186/s13071-019-3494-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gingrich J, Weatherhead A, Sattabongkot J, Pilakasiri C, Wirtz R. Hyperendemic malaria in a Thai village: dependence of year-round transmission on focal and seasonally circumscribed mosquito (Diptera: Culicidae) habitats. J Med Entomol. 1990;27(6):1016–26. doi: 10.1093/jmedent/27.6.1016. [DOI] [PubMed] [Google Scholar]
- 47.Rattanarithikul R, Linthicum K, Konishi E. Seasonal abundance and parity rates of Anopheles species in southern Thailand. J Am Mosq Control Assoc. 1996;12(1):75–83. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.