Abstract
COVID-19 forced the human population to rethink its way of living. The threat posed by the potential spread of the virus via an airborne transmission mode through ventilation systems in buildings and enclosed spaces has been recognized as a major concern. To mitigate this threat, researchers have explored different technologies and methods that can remove or decrease the concentration of the virus in ventilation systems and enclosed spaces. Although many technologies and methods have already been researched, some are currently available on the market, but their effectiveness and safety concerns have not been fully investigated. To acquire a broader view and collective perspective of the current research and development status, this paper discusses a comprehensive review of various workable technologies and methods to combat airborne viruses, e.g., COVID-19, in ventilation systems and enclosed spaces. These technologies and methods include an increase in ventilation, high-efficiency air filtration, ionization of the air, environmental condition control, ultraviolet germicidal irradiation, non-thermal plasma and reactive oxygen species, filter coatings, chemical disinfectants, and heat inactivation. Research gaps have been identified and discussed, and recommendations for applying such technologies and methods have also been provided in this article.
Keywords: COVID-19, Airborne virus ventilation, Enclosed space, Buildings
1. Introduction
COVID-19 forced the human population to adapt rapidly in the wake of the new, highly contagious virus. The forms of transmission are not entirely understood; however, it is accepted that the virus can become airborne through respiratory droplets that either directly contact another person, or evaporate and become droplet nuclei that may stay suspended as an aerosol for an extended period of time (Santos et al., 2020; Peters et al., 2020; Dancer et al., 2020). These aerosols may travel through ventilation systems in buildings and enclosed spaces, eventually invading other areas away from any infected individuals (Correia et al., 2020; Li et al., 2007). Although there is some debate on the severity of the threat posed by these airborne droplets, it is accepted that this mode of transmission cannot be ignored for typically enclosed spaces. Furthermore, a recent study even suggests that airborne transmission may be the dominant mode of transportation (Bazant and Bush, 2021).
Although COVID-19 is not fully understood, many lessons have been learned from previous airborne viruses such as tuberculosis and the various strains of influenza (Li et al., 2007; Riley, 1982). From a very basic understanding of how viruses propagate, it is understood that a certain amount of a virus needs to enter an uninfected individual to increase the viral load and create a new infection. Traditionally, this is defined as a quantum in epidemiological literature, which is the number of infectious airborne particles required to infect 63 % of individuals in an enclosed space (Riley et al., 1978), and serves as a foundational basis for many models attempting to quantify the probability of infection from exposure to a pathogen. To evaluate the risk posed to an individual exposed to a pathogen, a mathematical model proposed by Gammaitoni and Nucci (1997), and furthered by Buonanno et al. (2020a) and Bazant and Bush (2021) can be considered. This model is predicated upon the assumption of a well-mixed room, which is supported in literature (Nicas and Miller, 1999; Buonanno et al., 2020b; Stilianakis and Drossinos, 2010) and simply assumes that particles are uniformly distributed throughout an enclosed space instead of forming a small aerosol cloud subject to diffusion around an infected individual. Mathematically, the quanta emission rate can be expressed as:
| (1) |
where is the quanta emission rate, is the viral load of the sputum from an infected individual, is the inhalation rate, is the droplet volume concentration expelled from an infected individual, is the number of viral particles required to initiate an infection, and is the quanta-to-plaque forming unit conversion parameter. Thus, the concentration of quanta at a given time t in an enclosed space may be expressed as:
| (2) |
where represents the initial number of quanta in the space, represents the infectious viral removal rate, represents the number of infectious subjects, and represents the volume of the enclosed space being considered. Following this, the dose of quanta received by an individual over an interval of time, T, is:
| (3) |
Thus, the probability of an infection can be expressed as the simplified exponential dose-response model:
| (4) |
From an inspection of Equation (4), it may be seen that when the dose of quanta is equal to one that the probability of infection for an individual is roughly 63 %. Of particular interest towards mitigating the probability of infection is the infectious viral removal rate, IVRR. Bazant and Bush (2021) defined the IVRR as the sum of the individual removal rates:
| (5) |
where is the air exchange rate, is the combined air filtration rate and droplet settling in air duct rate, is the sedimentation rate, is the inactivation rate, and r is the radius of the particle. It is worth noting that except for the air exchange rate, all of the other mechanisms to either inactivate or remove the virus from a space are functions of the size of the particle in which the virus is being transported. With the addition of Equation (5), a relationship has been established between the probability of an individual becoming infected and the IVRR, and it may be seen that an increase in the removal rates will decrease the probability of infection. Thus, several basic factors may be considered as possible methods to address the removal of viral particles from an enclosed space to decrease the probability of an infection. These are simply increasing the fresh air supply and consequently decreasing the concentration of quanta, increasing the filtration rate for an HVAC system, increasing the deposition rate of the viral particles to surfaces, and increasing the viral inactivation. Although different by definition, increasing the deposition rate of the viral particles may be considered as similar to increasing the sedimentation rate. Sedimentation implies that particles settle to the ground or other surfaces due to gravitational forces. However, airborne particles may also deposit to walls and other surfaces due to mechanisms such as diffusion, which would be unnatural for particle sedimentation.
The Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) both corroborate the removal of the viral particles via air exchange (Centers for Disease Control and Prevention, 2021; Ding et al., 2020) and recommend increasing the fresh air supply as a straightforward way to decrease the concentration of the viral particles in an enclosed space. Air ionization may also be used to increase the removal rate of viral particles from an enclosed space by increasing filtration efficiency and particle deposition. Several methods exist to sterilize the air and render the virus harmless, thus increasing the viral inactivation rate and alleviating the need to remove the particles from the air. In this regard, a traditionally popular technology to combat airborne viruses is Ultraviolet Germicidal Irradiation (UVGI). Directly controlling the environmental conditions of a space has also been proposed to create an adverse environment for viruses, thereby increasing the natural viral inactivation rate. This specifically includes controlling the temperature and relative humidity of a space to ensure an overall hostile environment. Non-thermal plasma and reactive oxygen species present other alternatives for viral inactivation that have been proven effective against bacteria and other microbes. Another possible method utilizes filter coatings that facilitate viral inactivation by mechanisms such as the natural antiviral properties of materials or by directly damaging the virus. Chemical disinfectants have also been proven to effectively eliminate viruses from surfaces, and they may provide other solutions to increase viral inactivation. Finally, super-heated sterilization may present another viable solution for inactivating viral particles, although it has traditionally been used to sterilize surgical equipment on a smaller scale. The identified technologies and methods mentioned above are discussed in the following sections.
1.1. Increased ventilation and HVAC Operation/HEPA filters and filter upgrades
Reiterating the previous section, based upon the current knowledge of COVID-19 it is understood that the virus has three possible modes of transmission. These are transmission via direct contact such as touching a contaminated surface, transmission through large respiratory droplets, and transmission through small respiratory droplets, sometimes called droplet nuclei (Santos et al., 2020; Stilianakis and Drossinos, 2010). It is a well-documented phenomenon that liquid aerosols, such as those that carry a virus, can evaporate to smaller droplets that may potentially remain airborne for extended periods (Riley, 1982; Davis, 1982; Lim et al., 2008; Wells, 1934). However, it is debatable whether the smaller droplets constitute a serious threat compared to the other two modes of transmission (Peters et al., 2020; Dancer et al., 2020). The overall consensus remains that although the exact magnitude of the threat posed by the airborne particles is unknown, the threat itself remains viable and should be addressed. Furthermore, while a complete understanding is still lacking, it may be inferred that an airborne transmission mode is entirely possible due to the rapid spread of the virus (Correia et al., 2020), and there is even recent support for the idea that the airborne transmission mode may play the dominant role in an enclosed space (Bazant and Bush, 2021). This is especially true for enclosed spaces such as commercial and office buildings whose HVAC systems are not complex and will not act as a buffer for the spread of a virus through small airborne droplets (Chirico et al., 2020). Thus, the role of airborne transmission of COVID-19 through small respiratory droplets cannot be ignored in addressing its spread and reducing the probability of a healthy individual from becoming infected.
Regarding the mitigation of the small airborne droplets, it is important to have some context about a few factors affecting host infection and the airborne transmission mode itself, specifically how the droplets behave as an aerosol. Kohanski et al. (2020) identified four factors that influence the risk of indoor aerosol transmission: 1) aerosol properties, 2) indoor airflow, 3) virus-specific factors, and 4) host-specific factors. The aerosol properties involve the mobility of the particles, such as the diffusion rate and the particle settling rate, while the indoor airflow influences exposure and the local concentration of airborne particles, where it is known that the size of the liquid particles is distributed over a range and evolve based upon the conditions of the surrounding environment through evaporation (Bazant and Bush, 2021; Nicas and Miller, 1999; Stilianakis and Drossinos, 2010; Wells, 1934). It is worth noting here that the size of the particles will directly affect their mobility and settling rate, as smaller particles are more susceptible to diffusion and other transport mechanisms while larger particles are more susceptible to settling (Hinds, 1999). Furthermore, although the size of the virus is approximately 0.125 μm (Donaldsson et al., 2020), the virus typically travels in droplets usually submicron in scale with radii typically between 0.1 μm and 5.0 μm with the distribution being dependent on the type of exhalation from an individual (Bazant and Bush, 2021). The virus-specific and host-specific factors determine how much of a virus an individual can be exposed to before becoming infected, as well as the survivability of the virus itself. This is related to the concept of a quantum, discussed earlier as the amount of a virus that will cause a 63 % chance of an infection in a healthy and susceptible individual. Thus, a primary factor influencing an infection from a virus is simply the number of viral particles an individual is exposed to. From this, it is implied, regarding the airborne particles, that either exposure to a high concentration of particles over a shorter period of time or a low concentration of particles over longer periods will both lead to an infection. This is supported by inspection of Equations (2), (3)), where it may be seen that a change in the number concentration of quanta in a specified volume, or a change in the time interval will both affect the dosage an individual receives. Therefore, it is clear to see how the recommendations of the CDC and the WHO regarding the ventilation controls are effective towards addressing the concentration of the airborne particles and subsequently reduce the probability of infection (Centers for Disease Control and Prevention, 2021; Ding et al., 2020). It is important to realize that depending on the type of enclosed space, there will typically be a natural ventilation corresponding to a number of Air Changes per Hour (ACH) between 0.34/hr – 20/hr, which may be considered as analogous to the removal rate (Bazant and Bush, 2021). Thus, these numbers may be improved upon by intentionally increasing these values. This method includes ensuring that the system is operating properly, installing clean filters, upgrading to more effective filters, increasing the fresh air supply delivered by an HVAC system, and using fans to promote airflow. However, applying this method is also as simple as opening a window, as this would effectively reduce the concentration of airborne particles by introducing fresh outdoor air to an enclosed space.
Based upon the characteristics of the aerosol, namely the particle size, conventional air filters may also be effective in mitigating the spread of COVID-19 (Francisco et al., 2020). Mechanical air filters remove particles through the primary capture mechanisms of interception, impaction, and diffusion, where the dominant capture mechanism is a function of the velocity of the particle and the size of the particle. Smaller particles are more susceptible to diffusion, whereas larger particles are more susceptible to impaction and interception. The removal rates of mechanical air filters are directly related to their capture efficiency, which is by definition less than 20 % to greater than 75 % efficient for MERV 1–16 filters (What is a MERV rating? 2021), and greater than or equal to 99.97 % efficient for High-Efficiency Particulate Air (HEPA) filters. The removal rate may be thought of as the fraction of air that is cleaned as it passes through the filter. Particle capture may also be facilitated by incorporating electrical principles, such as imparting a charge to the particle or filter media itself in order to promote an attraction between the two, thereby increasing the rate of particle capture. Thus, concepts such as air ionization may also be coupled with air filtration to improve the removal of the airborne particles from an enclosed space and are discussed in the following section. However, simply operating a properly maintained and configured HVAC system, and ensuring the cleanliness of the system and that proper air filters are installed, are also likely to decrease the probability of spreading COVID-19 (Nembhard et al., 2020).
1.2. Ionization of the air
Air ions may be generated through various means with the intent to impart a charge to an aerosol in order to expedite the deposition of the particles to a surface, such as a wall or filter media. The ions impart a charge to the airborne particles through a diffusion process, increasing the electrical mobility and deposition of the particles to a surface, as even a neutrally charged object will attract a positively or negatively charged particle (Uk Lee et al., 2004). Positive, negative, and bipolar mixes of air ions are effective in improving the particle removal rate from the air, although each kind can affect the removal rate differently (Hyun et al., 2017). It is interesting to note that the efficiency of the particle removal is dependent on the emission rate of ions within an enclosed space (Sawant et al., 2012). Grinshpun et al. (2005) suggested that the volume of the space itself may also affect the rate of particle removal. As the airborne particles become charged, they interact with other particles in the environment, where like charges will repel each other and increase overall particle motion. The authors suggested that the deposition rate of the particles increased from this interaction between the charged particles, and also because of image charging on surfaces, which will attract particles and cause deposition as well. However, for enclosed spaces it was suggested that the effect from the interactions between the particles and surfaces that increased movement and deposition was diminished in larger spaces, where the particles simply have further to travel to deposit, the concentration of air ions may be less, and the distribution of ions within the space is less likely to be uniform. It is also worth noting that a large portion of available research focuses on fine and ultrafine particles, with most of the work analyzing particles of smoke in a relatively small and enclosed space. This may impart a bias to the efficacy of air ions if they are applied to a more realistic setting, with potentially larger airborne particles in larger spaces. To illustrate this, Sawant et al. (Sawant and Jadhav, 2012) noted in their experiments that different kinds of smoke were removed at different efficiencies, implying that the particles will respond uniquely based upon factors not considered in the experiments. Overall, the cited literature reports high removal efficiencies between 79 % and 100 %, although these experiments were conducted in closed and unventilated spaces over relatively long periods of time (Uk Lee et al., 2004; Sawant et al., 2012; Grinshpun et al., 2005; Sawant and Jadhav, 2012).
Although still a seemingly promising technology, generating air ions is not without potential drawbacks. Specifically, ozone is a common byproduct of generating air ions and may easily be created using a corona discharge technique (Jiang et al., 2018). It has been well established that the toxicity of ozone is a function of its concentration and that exposure can lead to numerous long-term and short-term effects, causing damage and complications in the lungs and respiratory system, eliciting an immune system activation, and is associated with respiratory-related mortality (Nuvolone et al., 2018). A small dosage of constant ozone exposure causes the lungs to overstimulate and can result in incapacitation (Lippmann, 1989; Krishna et al., 1997). The generation of ozone is a complex chemical reaction that is dependent on the energy level of the electrons generated during the process required for generating air ions (Chen and Davidson, 2002; Pekárek, 2003). Of particular importance is the fact that both the number of electrons generated, and by extension the ion emission rate, and the ozone generation rate are proportional to the input power (Yehia et al., 2000). This implies that there exists a balance between an increased ion emission rate, therefore an increased particle deposition rate, and an elevated ozone generation rate. However, it is quite possible to create air ions and achieve the desired result as far as the increased decay rate of particles in the air without generating large amounts of ozone. One such example is by using an electrostatic precipitator (Sung et al., 2019). In the cited study, it is noteworthy that within the closed environment, the device used to generate the ions, and thus clean the air, achieved a Clean Air Delivery Rate (CADR) of 0.6 m3/min – 1.6 m3/min, which was higher than a HEPA filter sized for a space of equivalent volume, while also generating nearly no ozone. Electrostatic precipitators do not rely solely upon air ions to cause increased particle deposition and use unipolar ions to charge particles within an electric field, where the charged particles are then attracted to a collection plate (Hinds, 1999). Furthermore, it is worth noting that electrostatic precipitators induce a local deposition of particles onto the collection plate, whereas a simple air ion emitter will likely cause an increased particle deposition to all surfaces within an enclosed space. Plant-based ionizers also exist and are commercially available (Suwardi et al., 2021), and offer another seemingly viable and effective alternative to generate air ions without also generating ozone. The cited study reported a CADR equal to approximately 4 m3/min. It is worth noting that the CADR can be considered as comparable to the ACH regarding the application to removal rates (Bazant and Bush, 2021).
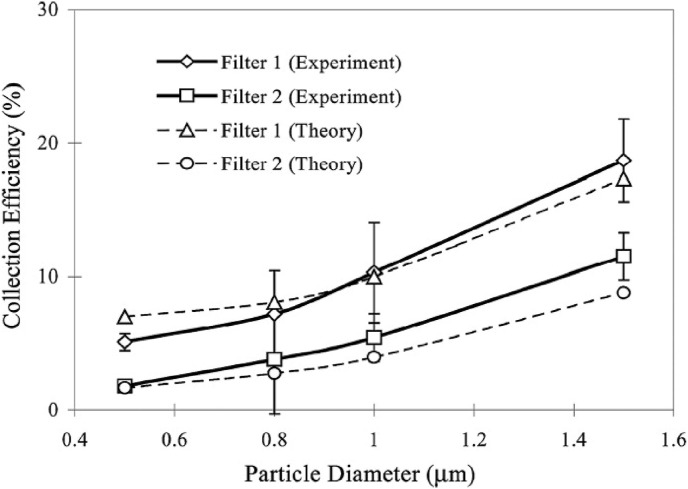
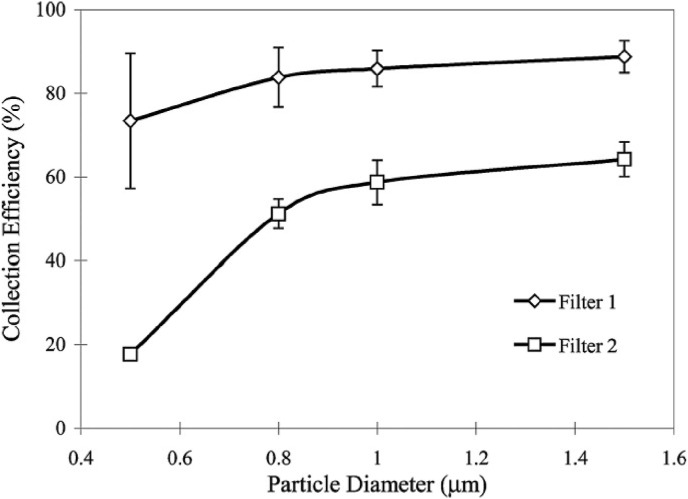
An alternative application of air ion emitters is to couple the generation of air ions with conventional HVAC filters to increase their particle removal efficiency. Simply put, an ion emitter installed in an HVAC duct in close proximity to an air filter, even a low-efficiency filter, can significantly increase the particle capture efficiency. When an ion emitter is used near a filter, the cloud of ions not only charges the airborne particles, but the individual ions deposit onto the filter fibers, which creates an overall charge on the fibers and an electric field (Agranovski et al., 2006). However, the particles that are charged from the ion cloud will have the same polarity as the fibers charged from the deposited ions, resulting in a repulsive force between the two. Although there will not be an attraction, the like-charge is still likely to affect the motion of the incoming airborne particles due to the repulsive force, and thus will still drastically increase the efficacy of the filter. Experiments have shown that the addition of an ion emitter in close proximity upstream to an air filter significantly increases the removal efficiency of solid particles used in a laboratory setting as well as other types of particles, including liquid particles carrying a strain of influenza (Agranovski et al., 2006; Huang et al., 2008). The cited literature reports filter efficiency increases over a wide range, from 5 % to 75 % (Hyun et al., 2017; Agranovski et al., 2006; Huang et al., 2008; Park et al., 2009). This concept is illustrated in Fig. 1, Fig. 2 , where Fig. 1 represents the experimental and theoretical results of a typical low-efficiency HVAC filter without utilizing an ion emitter, and Fig. 2 represents the experimental results with the use of an ion emitter (Agranovski et al., 2006). Furthermore, the use of a carbon fiber brush has the potential not only to increase the ion emission rate but also to decrease or eliminate ozone generation (Park et al., 2009). Of particular interest in these experiments were the particles used. All were small, as is expected of the liquid particles carrying the COVID-19 virus, but these experiments also did not rely on smoke to determine the particle removal rate increase from the air when the ions were generated. Thus, this illustrates the applicability of air ion technology to other situations besides very small smoke particles.
Fig. 1.
Filter efficiency without ionizer, illustrating theoretical and experimental results of low-efficiency fibrous HVAC filter media (Agranovski et al., 2006).
Fig. 2.
Filter efficiency with ionizer, illustrating the experimental efficiency of low-efficiency fibrous HVAC filters (Agranovski et al., 2006).
1.3. Environmental conditions
Controlling the environmental conditions of an enclosed space directly may offer a viable solution to increasing the inactivation rate of the virus. This claim is preliminarily based upon studies that analyze environmental factors such as weather conditions, temperature, and relative humidity and correlate these factors to the reported number of cases (Kroumpouzos et al., 2020). Specifically, it seems that temperature and relative humidity are the primary factors, and that relatively cold and dry environments increase the chances of the virus spreading (Mecenas et al., 2020). Furthermore, an increase in both temperature and relative humidity was associated with a decrease in reported new cases of the virus (Wu et al., 2020). It is interesting to note that an increase in the temperature by 1 °C was associated with a greater decrease in reported cases than a 1 % increase in relative humidity, although both were independently associated with a decrease in the reported cases. However, not all of the research conducted in this area agrees with the previous study completely. Temperature, absolute humidity, and diurnal temperature were all studied regarding the effects they had on the number of reported deaths from COVID-19 in Wuhan, China (Ma et al., 2020), where it was found that although the temperature and absolute humidity were correlated with a decrease in reported deaths, the diurnal temperature range corresponded to an increase in deaths. Another study was conducted (Shi et al., 2020), that analyzed temperature and absolute humidity, where no significant relationship between the absolute humidity and the spread of COVID-19 was found, but evidence was found that the transmission rate decreased with an increasing temperature.
When considering the previously cited work, it is important to realize that correlating temperature and relative humidity, perhaps related to the environmental conditions and season, leave numerous variables unaccounted for that may profoundly impact the spread of the virus. For example, warm and sunny weather may induce an increased number of travelers and activity among the residents of a city and would therefore skew the data as a confounding variable. Furthermore, human factors such as an increase in the accuracy of testing and increasing the efficiency in contact tracing and the reported number of cases also possibly skews the data. Yuan et al. (2020) address these issues specifically. Interestingly, these authors also note that the range of temperatures and relative humidities are often very small, and thus provide an unreliable correlation outside of the range studied. Most notably, they suggested that humidity plays a more important role in the propagation of the virus than temperature. This was directly related to the survivability of the airborne virus, as the virus is transmitted through liquid droplets. An ideal range of relative humidity was proposed where an optimal balance between liquid evaporation and viral deactivation exists (Yuan et al., 2020; Yang et al., 2012). In this range, the liquid droplets will evaporate, and the virus will be more prone to deactivation through an increase in the concentration of salts found in the droplets. However, if the humidity is higher than this range then the droplet will be less apt to evaporate, but the virus is more likely to survive due to the lower concentration of salts. If the humidity is lower than this range then the liquid droplet will evaporate and reduce in size, thus remaining airborne for a longer period of time and crystallizing the salts, removing their effect on the inactivation of the virus (Ding et al., 2020; Yang et al., 2012). It is worth noting that although the survivability of the virus increased in both the upper and lower ranges compared to the ideal range in between, the upper range yielded a lower survivability than the lower range. In the cited literature, the ideal range was given as between 40 and 70 %, with the most effective relative humidity given as approximately 50–60 %. Furthermore, it was suggested that cool and dry environments may also reduce the ability of an individual's immune system to combat the virus, as well as increasing the survivability of the virus within the environment.
Although many variables are not considered with studies analyzing atmospheric variables and the number of reported cases or deaths, there has been work done using surrogate viruses and their survivability related to the relative humidity and temperature of their environment (Chan et al., 2011; Casanova et al., 2010). In these studies, a relationship between a lower relative humidity and temperature and the survivability of the viruses was stated and it was suggested that cooler and dryer environments possibly prolong their survival, reiterating the studies previously cited. Furthermore, it was also established that increasing values of both relative humidity and temperature decreased the survivability of the viruses. Therefore, although there remains some disagreement on the validity of correlating weather patterns and other atmospheric phenomena with the increase or decrease of COVID-19 cases, a reasonable argument can be made that warmer and more humid conditions are less favorable to the spread and survivability of the virus and will increase its inactivation rate. Although the former set proposes a range with a ceiling beyond which the survivability increases, this is consistent with the previously cited work, and the latter set simply states that an unbounded increase is effective. Relating this to a removal rate focuses on the relative humidity of an enclosed space instead of the temperature. This is because an appreciable decrease in the survivability of the virus over a reasonably short period of time was observed at high temperatures well above expected room temperatures for a conditioned space (Chan et al., 2011; Casanova et al., 2010). Bazant and Bush (2021) estimated the inactivation rate from the relative humidity as linear and ranging from 0.0/hr – 0.63/hr.
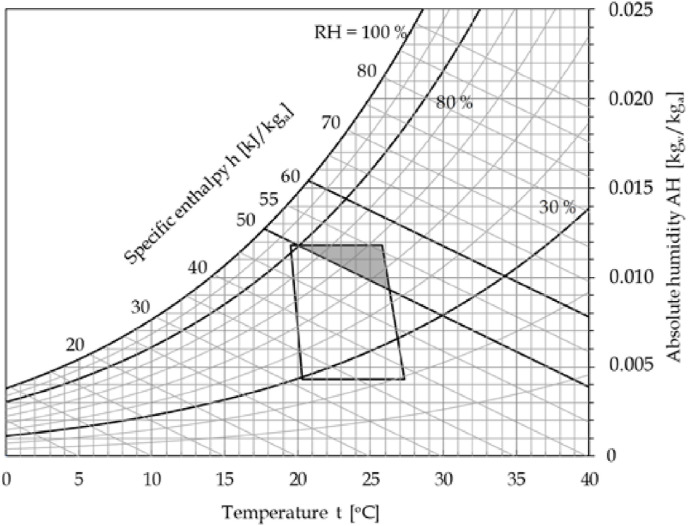
Relating the cited work together, one may conclude that there is enough evidence to suggest that an increase in temperature and maintaining the relative humidity at a certain point creates adverse conditions for the survivability of the virus. However, many times an enclosed space is maintained at conditions designed to be comfortable to its occupants. This may inadvertently create favorable conditions for the survival of the virus within the air and on surfaces, increasing its transmissibility. To combat this, Spena et al. (2020) propose a set of thermodynamic conditions focused on a range of enthalpies and relative humidities that a space may be maintained at to create an unsuitable environment for the virus. Specifically, the authors proposed a range of conditions between specific enthalpies of 50–60 kJ/kg-dry air, and relative humidities between 30 and 80 %. Furthermore, it was noted that a smaller sub-region exists that also corresponds to the American Society of Heating, Refrigerating and Air-Conditioning Engineer's (ASHRAE) recommended comfort zone, thus possibly enabling both a comfortable and safer environment. Fig. 3 illustrates the suggested zone bounded by the given enthalpies and relative humidities, where the darkened region represents the overlap between this zone and the ASHRAE recommended comfort zone. This introduces a particularly interesting option for addressing the transmission of COVID-19, as it opens the possibility of mitigating the spread by simply operating an existing HVAC system to achieve a certain range of conditions. However, it is worth noting that this method has not been researched thoroughly, although the implications remain promising.
Fig. 3.
The thermodynamic range for thermal comfort and suggested conditions for decreased viral survivability (Spena et al., 2020).
1.4. Ultraviolet germicidal irradiation
Prior to the arrival of the COVID-19 pandemic, research on ultraviolet (UV) light's ability to sterilize surfaces and the air had been performed and produced encouraging results. UVGI has been used as early as the twentieth century to sanitize surgical equipment and water systems (Kowalski and Bahnfleth, 2000a, 2000b; Kowalski, 2001). The next iteration of applications moved onto ventilation systems during the 1930s: an upper room UVGI system was installed in a school's ventilation system because of a large measles outbreak. This ventilation upgrade led to a reduction of measles cases within the school (Kowalski and Bahnfleth, 2000b; Riley, 1972; Reed, 2010). There are other numerous examples of facilities that have resorted to installing a UVGI system to combat airborne outbreaks and received positive results, especially against tuberculosis (Riley, 1972; Reed, 2010). Since these early applications, the designs of UVGI systems have evolved into more energy-efficient and compact arrangements (Mikaeva et al., 2020; Vranay et al., 2020).
UVGI systems do not remove microorganisms. UV photons that are emitted from UV light lamps are absorbed and corrupt the virus's DNA and RNA, which removes the virus's ability to replicate itself (Vranay et al., 2020; Raeiszadeh and Adeli, 2020). The most effective wavelength band is the C band, also known as UVC, ranging from wavelengths of 100–280 nm with the most effective wavelength being 254 nm (Foarde et al., 2006). Based on early research of COVID-19 and its inactivation rate due to UVGI, the virus appears to be more resistant than other viruses and bacteria (Raeiszadeh and Adeli, 2020). This means that a longer exposure time is needed to sterilize COVID-19 compared to other microorganisms. The dosage delivered to the pathogen is determined by multiplying the exposure time to the UV light by the average irradiance from the light (Kowalski and Bahnfleth, 2014). The exact amount of UV dosage required to inactivate COVID-19 is not certain as various studies have produced a range of results. For example, to deactivate 90 % of the airborne COVID-19 particles, a range of 0.7–4.0 mJ/cm2 has been determined as necessary (Raeiszadeh and Adeli, 2020; Walker and Ko, 2007). This dosage range is still 1.5–2 times less than what is required to deactivate viruses on surfaces since aerosols have no obstructions for protection from the corrupting UV photons (Raeiszadeh and Adeli, 2020; Tseng and Li, 2005). Due to these uncertainties, there are no guidelines or standards of exact dosage requirements. However, the reported inactivation efficiencies range from 70.61 % to 100 % (Vranay et al., 2020; Raeiszadeh and Adeli, 2020; Tseng and Li, 2005; Beggs et al., 2006). Testing continues to further our understanding of the complexities of the biological characteristics, specifically the susceptibility of microorganisms to damage by UV light and by extension the dosage requirements (Beggs et al., 2006; Kowalski and Bahnfleth, 2004).
There are various options available to apply UVGI technology, such as placing UV lamps in the upper one-third of a room (upper room UV), portable air circulating units with internal lamps, and the most common design of installing UV lamps directly in the building's ventilation system (Vranay et al., 2020; Beggs et al., 2006). Fig. 4 provides an example of a ventilation system layout with the addition of a UVGI system. UVGI systems are typically designed to fit the needs of a specific building, as different buildings have unique and different styles of HVAC systems that affect certain characteristics such as air speed, relative humidity, temperature, and volume of moving air (Kowalski, 2001; Vranay et al., 2020). Regardless of these characteristics, the UV lamps should be placed in the direct center of the air duct and produce an arc length the span of the duct width to ensure that there is UV light exposure in all directions (Kowalski and Bahnfleth, 2014). However, as previously mentioned, no comprehensive standard currently exists due to the lack of quality data, making the ability to recommend a standard design challenging (Beggs et al., 2006; Bahnfleth et al., 2005).
Fig. 4.
Typical diagram of an HVAC system with UVGI integration (Menzies et al., 2003).
No solution is perfect, and there a few potential apprehensions when considering the addition of a UVGI system. UV rays are known to accelerate the rate of decay for different materials, especially polymers such as those used in sealing ductwork and filter seals (Vranay et al., 2020). However, this may be avoided by using a reflective material for the duct regarding a UVGI system addition, which coincidentally also happens to be the best material selection for the efficacy of a UVGI system. A reflective material such as aluminum or magnesium oxide would resist the decaying effects while simultaneously improving the field intensity of the UV light (Kowalski and Bahnfleth, 2000b; Kowalski, 2001; Reed, 2010). Another concern is the potential of a viral mutation. The risk of mutation is always present with any form of defense against a virus, as viruses and bacteria are known to adapt in order to survive (Raeiszadeh and Adeli, 2020; Norval, 2006). In addition to possible viral mutations, UV light has also been proven to mutate other microorganisms such as skin cells in humans, which can lead to cancer (Beggs et al., 2006; Narayanan et al., 2010). This implies that humans should limit exposure to UV radiation to ensure the absorbed dose is within limited and safe amounts. Finally, a UV wavelength of 185 nm is also known to generate ozone, the implication of which has been briefly described in the Air Ionization section. To mitigate this issue, glass may be installed where the UV rays are emitted since it can absorb this wavelength of light (Vranay et al., 2020). Overall, the risks and rewards must be analyzed when considering the addition of a UVGI system. UVGI systems have been proven to be effective against various microorganisms many times, but it remains unpredictable how a virus may react over longer periods of time. However, if there is no UV exposure to any individuals when the systems are designed and installed, the risk of harming building residents is ultimately low. Finally, the cost of retrofitting or installing additional HVAC equipment must eventually be considered. Lee et al. (2009) conducted a cost analysis in 2009 investigating the addition of a UVGI system or air filter upgrades. The analysis indicated that a UVGI system could cost as low as 21 % of the cost to upgrade to an equally efficient MERV 12 filter. This analysis considered the cost of installation, replacements, and energy consumption. Although the analysis cannot be considered relevant for accurate costing information due to the expected market changes over time, it is useful to establish that UVGI technology may not be prohibitively costly to implement. Regardless of the current potential for the applications of this technology and the strong evidence for successful viral inactivation, there remains a need for future work to define a standard for designing and implementing UVGI systems.
1.5. Non-thermal plasma and reactive oxygen species
Plasma is the result of constant ionization at the atomic level. It is comprised of continual interactions between photons, ions, electrons, and excited and non-excited molecules (Moreau et al., 2008). Non-Thermal Plasma (NTP) is usually generated by sending an electric charge through an inert gas. This causes the molecules of the gas to reach a thermal equilibrium where electrons will leave the gaseous atoms and react with the atmospheric oxygen, creating Reactive Oxygen Species (ROS) such as OH, O2, H2O2, and O3.
NTP has been used since the beginning of the century to disinfect food and water (Moreau et al., 2008; López et al., 2019). One possible way of generating NTP is to use the method of Dielectric Barrier Discharge (DBD) to generate plasma jets or plumes at atmospheric pressure. A possible configuration of such a device is illustrated in Fig. 5 . Using DBD, ROS has been proven to be effective in the inactivation of bacteria and other microbes (Ma et al., 2008; Hernández-Díaz et al., 2021). Other work has also explored its effect on airborne bacteria, where it was shown to be between 20 % and 70 % effective at inactivating some, although less effective in inactivating bacteria that were resistant to oxidizing agents compared to those that were not (Lai et al., 2016; Martin et al., 2008). Although shown to be effective towards bacteria and other microbes, the question remains whether NTP and ROS are effective towards viral inactivation. However, regarding the use of DBD applied to an HVAC system, a packed bed DBD reactor has been shown to induce a reduction of the MS2 bacteriophage by 99.5 % (Xia et al., 2019). Although only similar to viruses such as COVID-19 or the various influenza strains, bacteriophages are considered to be good models for the study of airborne viruses as they are safe to use and can have some of the same features that viruses exhibit (Turgeon et al., 2014).
Fig. 5.
Schematic of a DBD packed-bed reactor (Xia et al., 2019).
The COVID-19 pandemic has renewed the possibilities of using NTP as a common option for air and surface sterilization, where portable NTP systems may potentially provide a new method for inactivation. Portable, small NTP devices are capable of efficient inactivation of viral agents, such as COVID-19 RNA (Bisag et al., 2020), where the study reported a 99.98 % inactivation of both bacteria and COVID-19. A sterilized portable DBD plasma system could introduce highly effective, small air filters into individual rooms, and also provide a means to sterilize relatively small items placed into a closed chamber coupled with an NTP device (Sharma and Sharma, 2020).
The obstacle that prevents NTP generators from becoming a common sterilization device is the generation of ozone. The process by which NTP produces ozone is the same as that discussed in the Air Ionization section regarding the phenomenon responsible for the formation of ozone, although the focus and aim of the process is different. As has been established, exposing humans to ozone directly would be extremely harmful and dangerous, and therefore NTP technologies capable of addressing this potential hazard should be examined when considering this method to increase the viral removal rate. A Multipin Corona Discharge (MPCD) reactor has been shown to be more efficient and produce less ozone in a smaller setup (Hernández-Díaz et al., 2021). The hazard of ozone may also be addressed with an ozone filter or another disposal operation and may reduce the related dangers, but implementing these technologies would require extra planning and may not be readily installed into an operating HVAC system (Xia et al., 2019).
Relatively recent studies exist relating NTP to the disinfection of food, water, and hard surfaces (Moreau et al., 2008; Ma et al., 2008). These were mainly inspired in the 1990s to search for a replacement for the heat sterilization of materials. NTP generators developed for airborne applications are being more widely investigated regarding their success against pathogens including COVID-19, MS2, and the Newcastle virus (Xia et al., 2019; Bisag et al., 2020; Schiappacasse et al., 2020). However, the main drawback to NTP being applied as an airborne pathogen inactivation method remains the generation of ozone.
1.6. Filter coatings
Specifically, regarding fibrous filters, nanoparticles may be used as a coating to add an additional layer of protection to inactivate captured viral particles. Thus, any of the particles that may become detached from the filter and resuspended in the air would be incapable of causing an infection in a person. Joe et al. (2014) used silicon dioxide nanoparticles surface coated with silver nanoparticles (combined and termed as SA particles) to coat a fibrous filter and challenged it with an aerosolized MS2 bacteriophage. An illustration of the SA particles coating some fibers may be seen in Fig. 6 . The authors determined that an optimal coating amount exists that takes advantage of the antiviral properties of the coating as well as the increased capture efficiency while also avoiding an unnecessary increase in pressure drop. Similarly, Carbon Nanotubes (CNTs) may be used to coat a glass fiber (Park and Hwang, 2014), and an illustration may be seen in Fig. 7 . In the cited study, the added coating increased particle filtration efficiency by 33 % and the antiviral efficiency was 92 % overall, where the inactivation of the viral particles from the CNTs was attributed to mechanical damage of the cell's surface upon contact. Alternatively, titanium dioxide (TiO2) and crystal-violet nanocomposites (CV) may be used to create an air filter that is visible-light-activated for viral particle inactivation (Heo et al., 2020). Using visible light, the filter coating produces ROS with the CV-TiO2 combination, resulting in a 99.98 % inactivation and a 99.99 % filtration rate. To improve the viability of a filter coated with CV-TiO2 nanoparticles operating in humid and moist conditions, molecules of 1H,1H,2H,2H-perfluorooctyltriethoxysila (PFOTES) may be introduced to the nanocomposites in the filter, successfully hydro-proofing the fibers (Pazokifard et al., 2012). Another alternative filter coating is dialdehyde starch, which is a cheap compound made from general corn or wheat starch (Woo et al., 2012) which was used to coat the fibers of three different filters and tested with the MS2 bacteriophage in the cited study. When the starch was present, the survivability of the MS2 decreased to as low as 30 %. Filters were tested with a starch concentration of only up to 4 %, due to higher concentrations resulting in the filters becoming too fragile to adequately perform. Finally, tea tree and eucalyptus oils have also been applied as coatings and used as natural disinfectants (Pyankov et al., 2012). The oils were used to coat different filters and challenged against a strain of the influenza virus, where both oils were shown to inactivate the filtered virus within 5–10 min.
Fig. 6.
Silicon dioxide and silver nanoparticle fiber coating (Joe et al., 2014).
Fig. 7.
Carbon nanotube fiber coating (Park and Hwang, 2014).
Silver nanoparticle inactivation research is still in its infancy, however, it has shown promise with influenza strains, hepatitis B, and polioviruses (Chen and Liang, 2020). Furthermore, in recent studies TiO2 exhibits antiviral and cancer inactivation capabilities, and targeted TiO2 can be a safe alternative to harmful chemical treatments in the biomedical field (Ziental et al., 2020). However, since the inactivation using TiO2 is through ROS, the generation of ozone must be addressed upon installation (Monge et al., 2010). Given the current state of the technologies and the current trends in research and development, the nanoparticle market may be described as available and growing (Skyspring, 2021; Sigma-Aldrich, 2021). The natural disinfectants, dialdehyde starch, tea tree oil, and eucalyptus oils are available to purchase and are safe for use. However, their inactivation and filtration rates are not competitive compared to other sources of inactivation in this section (Woo et al., 2012; Pyankov et al., 2012).
1.7. Chemical disinfectants
Aerosol inactivation agents are common in residential and industrial areas, where they may be introduced into an HVAC system to aid in the inactivation of pathogens present within the air. Illustrating this concept, a study administered chlorine dioxide (ClO2) gas to mice at a concentration of 0.03 ppm for 15 min along with a strain of the influenza virus (Ogata and Shibata, 2008). It was reported that infection was prevented for all of the test subjects, thus demonstrating the efficacy towards the inactivation of the influenza virus. Engineered water nanostructures (EWNS) may also provide a solution to increase the removal rate of infectious viral particles. EWNS are molecules of water vapor that are first condensed and then altered by electrospraying (Pyrgiotakis et al., 2014). The water vapor molecules can be absorbed from the atmosphere, creating a closed-loop disinfecting cycle, where the electrospraying excites the condensed water vapor and generates EWNS, which are subsequently ejected back to the environment. EWNS contains the ROS molecules hydroxyl and superoxide, which induce little to no toxicological effects, allowing for the possibility of a small space air filter. In one study, EWNS reduced a flu sample by 94 % while producing less than 1 ppm of superoxide (Vaze et al., 2019). Finally, dry fogging also presents a potential technology to increase the viral removal rate and uses an aerosolized mixture of peroxyacetic acid and hydrogen peroxide (aPAA-HP). The dry fog may be delivered to a space and dispersed through the HVAC ventilation system to provide a readily available and convenient method of application. aPAA-HP has previously been tested using multiple viral and spore agents, including COVID-19 (Schinköthe et al., 2020). The purpose of the cited study was to determine the protocols of using aPAA-HP necessary to effectively disinfect a facility, where it was demonstrated that dry fogging was highly effective.
Overall, chemical inactivation presents many possibilities. Chlorine dioxide has shown strong antibacterial and antiviral attributes, but it is still undergoing testing as it is toxic to humans when ingested. However, rats continually exposed to low doses over a period of 24 h for 6 months experienced no effects when exposed to a concentration 0.1 ppm or less (Akamatsu et al., 2012). It is noteworthy that the Occupational Health and Safety Administration (OSHA) permits a maximum exposure of ClO2 to 0.1 ppm for human workers over an 8-h period (Occupational Safety and Health Administration, 2020). EWNS shows promise as a method of disinfecting an enclosed space and increasing the viral removal rate with its closed-loop functionality for recycling air from the surrounding environment to inactivate pathogens, and it could be very applicable if it were to become more commercially available (Pyrgiotakis et al., 2014). Dry fogging has been tested as a critical disinfectant in medical facilities, but would likely be impractical in a common, everyday scenario such as a commercial or residential application. However, in the case of another pandemic or dangerous outbreak, it could be beneficial towards disinfecting areas of a workplace exposed by infected employees (Schinköthe et al., 2020).
1.8. Heat inactivation
It is possible to inactivate COVID-19 within 5 min when exposing it to an environment at 70 °C, and 30 s while exposing it to an environment at 95 °C while suspended in a serum (Batéjat et al., 2021; Chin et al., 2020). Axial heating has been shown to be extremely effective in this regard at low flow rates. Using this method in a small-scale chamber, the MS2 bacteriophage inactivation rate was 99.996 % (Grinshpun et al., 2010). Massachusetts Institute of Technology's (MIT) chemical and nuclear engineering departments have developed a mask that utilizes heat inactivation, where the air intake is filtered through a packed bed of heated copper, thus acting like a small, personal filter with self-inactivation (Faucher et al., 2020).
A filter made from nickel foam has also been developed to inactivate COVID-19 using the application of heat (Yu et al., 2020). The nickel filter in the cited work was heated to 200 °C and successfully eliminated 99.8 % of COVID-19 in a single pass, as well as eliminated 99.9 % of anthrax spores tested. Regarding the physical characteristics of the filter, the nickel foam had a pore range of approximately 50–500 μm and a thread diameter of about 65 μm. This technology is still under development but shows promise in residential applications. Of particular interest towards the safety and potential commonplace use of this technology is the temperature of the air after being superheated and passing through the filter. However, the air cools to near room temperature after moving a short distance (4 cm post-filter in the study) due to the short exposure time from the heated filter elements.
Inactivation from a combustion process may be accomplished by exposing airborne pathogens to halogens, such as iodine and chlorine, where the halogens react with and inactivate the pathogens in the airstream (Grinshpun et al., 2012). Combustion was highly effective with inactivation, and it is most efficient with iodide compounds as fuel (Grinshpun et al., 2013). Inactivation from heat alone is also possible while utilizing the aforementioned combustion process, as a flame can burn at sufficiently high temperatures based upon the halogenic fuel used (Grinshpun et al., 2013; Aly et al., 2014). However, it is worth noting that halogens are also capable of inactivation separate from the flame in the airstream, thus decreasing the heat added to the air in an HAVC or exhaust system (Aly et al., 2014).
The heat inactivation mask in development by MIT shows promise for future applications, especially assuming the possibility of another pandemic outbreak. As of now though, the total cost and manufacturing requirements are still unknown. Combustion and heat inactivation in the airstream causes complications regarding maintaining a certain comfort level in a space using an HVAC system. However, heat inactivation is a sterilization technique that is highly effective and has been used extensively in almost every industry and other common applications, such as household cooking (Hugo, 1995). Combustion inactivation attempts to relieve some of the heat added to an HVAC system by using halogenic compounds as inactivation agents, thus improving the inactivation rate by alternative means besides heat addition (Grinshpun et al., 2012, 2013). It is important to note though that this option will pollute the air and cause issues for a closed HVAC system, possibly causing more strain on installed HVAC filters. However, heat inactivation alone through a self-heated device has potential and could be readily fitted into an existing duct system, such as the nickel foam filter device discussed above, although this technology is still in the early stages of development (Yu et al., 2020).
2. Conclusion
Several recommendations may be made based upon current research and published guidelines. In summary, a layered approach that combines several of the proposed methods is recommended. This is because none of the individual methods are likely to completely remove the viral airborne particles from an enclosed space, and a layered approach may potentially avoid the pitfall of diminishing returns from a single method of viral removal. The ideal approach may be unique for each situation to ensure the maximum removal of airborne particles containing COVID-19 and would depend on factors such as the ability to introduce fresh air to a space, or the configuration of a previously installed HVAC system. It is worth noting again that the conceptual basis for the different technologies discussed above to increase the viral particle removal rate is predicated upon several simplifying assumptions. Namely, these are assumptions surrounding the infectivity and survivability of COVID-19, and that an enclosed space is well-mixed. The infectivity and survivability of COVID-19 are directly related to the concept of a quantum, and the amount of the virus that a healthy individual can ingest before becoming infected as well as the time that the airborne virus may be exposed before inactivation. The well-mixed room assumption simplifies predictive models by assuming that an enclosed space has a uniform distribution of viral particles, but in doing so ignores the realistic dynamic effects induced by proximity to an infected individual. Table 1 suggests advantages, disadvantages, and research gaps for each category of methods. In summary of the individual methods:
-
•
Ventilating an enclosed space provides an effective way to reduce the concentration of airborne particles carrying the COVID-19 virus. This may be as simple as opening a window or increasing the fresh air supply for an HVAC system.
-
•
Air filters are a proven technology to remove particles from the air. The liquid droplets that the COVID-19 virus uses to spread will behave as other known aerosols, following the same patterns for droplet evaporation, particle travel, and diffusion throughout and environment. Thus, a properly sized air filter is known to be effective in the removal of these small airborne droplets. Furthermore, even a medium-efficiency air filter will be effective and will impact the performance of an already-in-place HVAC system less than a HEPA filter will, or some other filter that will induce a larger pressure drop.
-
•
Air ionization provides a promising method to reduce the number of airborne particles by increasing their deposition rate to walls and other surfaces. However, this does not necessarily inactivate the virus, and the argument can be made that this may increase the chance of transmitting the virus through contact. A potential disadvantage related to air ionization is the generation of ozone. However, the mechanisms of ozone generation are understood relatively well for this method, and there exist options to mitigate an unsafe amount from being introduced into an enclosed space.
-
•
Environmental controls show promise to create an environment that is adverse to the survival of the virus. Cool and dry environments are known to increase the chances of infection, where it is suggested that a cool environment increases the survival rate of the virus, and a dry environment causes the airborne droplets to evaporate to a higher degree, thus causing them to remain airborne for a longer period of time and increasing the survivability of the virus. To combat this, a warmer environment is recommended, but equally important is a range of humidities that will maintain comfort, but also reduce unnecessary and excessive evaporation of the airborne droplets.
-
•
UVGI offers a promising solution to inactivate viruses, which has been proven to work in other situations similar to the current situation with COVID-19. It may be installed in existing HVAC systems, or the upper portion of a room to reduce the exposure of people to possibly harmful radiation at sufficient doses. Some potential disadvantages of UVGI technology are the possible generation of ozone and the degradation of materials exposed to ultraviolet radiation. However, using glass to absorb the wavelength of light responsible for ozone generation presents a potentially effective way to address this issue. Also, using reflective materials in the duct not only circumvents material degradation, but it will also improve the efficacy of viral inactivation.
-
•
Nanoparticles offer a solution to increase the efficiency of a fibrous filter while also providing a method to inactivate captured viral particles. However, the addition of nanoparticles to filter media also increases the pressure drop across the filter, increasing the impact of implementing this technology to an existing HVAC system.
-
•
Non-thermal plasma has been used to inactivate bacteria and various airborne pathogens including the MS2 bacteriophage with varying levels of success. Like UVGI, it is possible to install a portable air sterilizing device in a room or a duct to inactivate a virus. However, since NTP relies on the generation of ROS, unacceptable levels of ozone may likely be generated. This may be mitigated depending on the form of NTP generation, such as an MPCD reactor, or by using an ozone filter.
-
•
Chemical disinfectants have been suggested and used to inactivate viruses in enclosed spaces, and research exists suggesting that their implementation is highly effective. Some of the disinfectants discussed are not harmful to humans, but more research is required to quantify the effectiveness of these methods in addition to the safety concerns regarding an application with HVAC systems.
-
•
Using an elevated air temperature to inactivate the virus has also been proven to be effective. It is possible to expose the viral particles to a small-scale heat source, such as an axial heating element or a heated metal filter in a duct, offering a possible solution to the inactivation of viral particles in an HVAC system. Furthermore, using combustion to generate halogens in an airstream is effective at deactivating viral particles while also reducing the amount of heat added to a system. However, the introduction of additional pollutants from combustion, and additional heat to a system from the heat inactivation method in general, is undesirable.
-
•
There is an observed lack of useable cost analysis data regarding the implementation of the technologies presented.
-
•
The reported efficiencies and removal rates of the presented technologies are not necessarily directly comparable to each other. For example, the removal rate of a mechanical filter is dependent on the filter's efficiency and the supplied room's volume and airflow rate, while several of the reported values for the efficiency of air ionization are from experiments conducted in sealed enclosures with no air circulation. The reader is referred to the work of Bazant and Bush (2021) for an in-depth discussion on the calculation of the removal rates.
Table 1.
Summary of removal methods by category.
| Category | Reference | Advantages | Disadvantages | Research Gaps |
|---|---|---|---|---|
| HVAC | (Santos et al., 2020; Correia et al., 2020; Li et al., 2007; Centers for Disease Control and Prevention, 2021; Ding et al., 2020; Chirico et al., 2020; Donaldsson et al., 2020; Francisco et al., 2020) |
|
|
|
| Air Ionization | (What is a MERV rating? 2021; Nembhard et al., 2020; Uk Lee et al., 2004; Hyun et al., 2017; Sawant et al., 2012; Pekárek, 2003; Yehia et al., 2000; Sung et al., 2019; Suwardi et al., 2021; Agranovski et al., 2006) |
|
|
|
| Environmental Conditions | (Huang et al., 2008; Park et al., 2009; Kroumpouzos et al., 2020; Mecenas et al., 2020; Wu et al., 2020; Ma et al., 2020; Shi et al., 2020; Yuan et al., 2020; Yang et al., 2012; Chan et al., 2011) |
|
|
|
| Ultra-Violet Germicidal Irradiation (UVGI) | (Casanova et al., 2010; Spena et al., 2020; Kowalski and Bahnfleth, 2000a, 2000b, 2004, 2014; Kowalski, 2001; Riley, 1972; Reed, 2010; Mikaeva et al., 2020; Vranay et al., 2020; Raeiszadeh and Adeli, 2020; Foarde et al., 2006; Walker and Ko, 2007; Tseng and Li, 2005; Beggs et al., 2006; Bahnfleth et al., 2005; Menzies et al., 2003; Norval, 2006) |
|
|
|
| Non-Thermal Plasma (NTP) | (Narayanan et al., 2010; Lee et al., 2009; Moreau et al., 2008; López et al., 2019; Ma et al., 2008; Hernández-Díaz et al., 2021; Lai et al., 2016; Martin et al., 2008; Xia et al., 2019; Turgeon et al., 2014; Bisag et al., 2020; Sharma and Sharma, 2020; Schiappacasse et al., 2020) |
|
|
|
| Filter Coatings | (Joe et al., 2014; Park and Hwang, 2014; Heo et al., 2020; Pazokifard et al., 2012; Woo et al., 2012; Pyankov et al., 2012; Chen and Liang, 2020; Ziental et al., 2020; Monge et al., 2010; Skyspring, 2021; Sigma-Aldrich, 2021) |
|
|
|
| Chemical Disinfectants | (Ogata and Shibata, 2008; Pyrgiotakis et al., 2014; Vaze et al., 2019; Schinköthe et al., 2020; Akamatsu et al., 2012; Occupational Safety and Health Administration, 2020) |
|
|
|
| Heat Inactivation | (Batéjat et al., 2021; Chin et al., 2020; Grinshpun et al., 2010, 2012, 2013; Faucher et al., 2020; Yu et al., 2020; Aly et al., 2014; Hugo, 1995) |
|
|
|
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This material is based upon work supported by the U.S. Department of Energy Office of Environmental Management under Award Number: DE-EM0003163.
References
- Agranovski I.E., Huang R., Pyankov O.V., Altman I.S., Grinshpun S.A. Enhancement of the performance of low-efficiency HVAC filters due to continuous unipolar ion emission. Aerosol Sci. Technol. 2006;40(11):963–968. [Google Scholar]
- Akamatsu A., Lee C., Morino H., Miura T., Ogata N., Shibata T. Six-month low level chlorine dioxide gas inhalation toxicity study with two-week recovery period in rats. J. Occup. Med. Toxicol. 2012;7(1):2. doi: 10.1186/1745-6673-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aly Y., Zhang S., Schoenitz M., Hoffmann V.K., Dreizin E.L., Yermakov M., Indugula R., Grinshpun S.A. Iodine-containing aluminum-based fuels for inactivation of bioaerosols. Combust. Flame. 2014;161(1):303–310. [Google Scholar]
- Bahnfleth W., Kowalski W.J., Freihaut J. Standard and guideline for UVGI air treatment systems. Indoor Air. 2005;104(December 2014):3464–3468. [Google Scholar]
- Batéjat C., Grassin Q., Manuguerra J.-C., Leclercq I. Heat inactivation of the severe acute respiratory syndrome coronavirus 2. J. Biosaf. Biosecurity. 2021;3(1):1–3. doi: 10.1016/j.jobb.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazant M.Z., Bush J.W.M. A guideline to limit indoor airborne transmission of COVID-19. Proc. Natl. Acad. Sci. Unit. States Am. 2021;118(17) doi: 10.1073/pnas.2018995118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beggs C.B., Noakes C.J., Sleigh P.A., Fletcher L.A., Kerr K.G. Methodology for determining the susceptibility of airborne microorganisms to irradiation by an upper-room UVGI system. J. Aerosol Sci. 2006;37(7):885–902. [Google Scholar]
- Bisag A., Isabelli P., Laurita R., Bucci C., Capelli F., Dirani G., Gherardi M., Laghi G., Paglianti A., Sambri V., Colombo V. Cold atmospheric plasma inactivation of aerosolized microdroplets containing bacteria and purified SARS-CoV-2 RNA to contrast airborne indoor transmission. Plasma Process. Polym. 2020;17(10):1–8. [Google Scholar]
- Buonanno G., Morawska L., Stabile L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: prospective and retrospective applications. Environ. Int. 2020;145(August):106112. doi: 10.1016/j.envint.2020.106112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonanno G., Stabile L., Morawska L. Estimation of airborne viral emission: quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020;141(May):105794. doi: 10.1016/j.envint.2020.105794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76(9):2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Feb. 9, 2021. COVID-19 ventilation FAQs; pp. 1–8.https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html [Online]. Available. [Google Scholar]
- Chan K.H., Peiris J.S.M., Lam S.Y., Poon L.L.M., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011;2011 doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Davidson J.H. Ozone production in the positive DC corona discharge: model and comparison to experiments. Plasma Chem. Plasma Process. 2002;22(4):495–522. [Google Scholar]
- Chen L., Liang J. An overview of functional nanoparticles as novel emerging antiviral therapeutic agents. Mater. Sci. Eng. C. 2020;112(March):110924. doi: 10.1016/j.msec.2020.110924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020;1(1):e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirico F., Sacco A., Bragazzi N.L., Magnavita N. Can air-conditioning systems contribute to the spread of SARS/MERS/COVID-19 infection? Insights from a rapid review of the literature. Int. J. Environ. Res. Publ. Health. 2020;17(17):1–11. doi: 10.3390/ijerph17176052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correia G., Rodrigues L., Gameiro da Silva M., Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med. Hypotheses. 2020;141(April):109781. doi: 10.1016/j.mehy.2020.109781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dancer S.J., Tang J.W., Marr L.C., Miller S., Morawska L., Jimenez J.L. Putting a balance on the aerosolization debate around SARS-CoV-2. J. Hosp. Infect. 2020;105(3):569–570. doi: 10.1016/j.jhin.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis E.J. Transport phenomena with single aerosol particles. Aerosol Sci. Technol. 1982;2(2):121–144. [Google Scholar]
- Ding J., Yu C.W., Cao S.J. HVAC systems for environmental control to minimize the COVID-19 infection. Indoor Built Environ. 2020;29(9):1195–1201. [Google Scholar]
- Donaldsson S., Naver L., Jonsson B., Drevhammar T. COVID-19: minimising contaminated aerosol spreading during CPAP treatment. Arch. Dis. Child. Fetal Neonatal Ed. 2020;105(6):669–671. doi: 10.1136/archdischild-2020-319431. [DOI] [PubMed] [Google Scholar]
- Faucher S., James Lundberg D., Anna Liang X., Cindy Jin X., Phillips R., Parviz D., Buongiorno J., Strano M. 2020. A Virucidal Face Mask Based on the Reverse-Flow Reactor Concept for Thermal Inactivation of SARS-CoV-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foarde K., Franke D., Webber T., Hanley J., Owen K., Koglin E. 2006. Biological Inactivation Efficiency by HVAC In-Duct Ultraviolet Light Systems Projecting Air Purifier. [Google Scholar]
- Francisco P.W., Emmerich S.J., Schoen L.J., Hodgson M.J., Mccoy W.F., Miller S.L., Li Y., Kong H., Olmsted R.N., Sekhar C., Parsons S.A., Wargocki P. 2020. ASHRAE Position Document on Airborne Infectious Diseases by ASHRAE Board of Directors. [Google Scholar]
- Gammaitoni L., Nucci M.C. Using a mathematical model to evaluate the efficacy of TB control measures. Emerg. Infect. Dis. 1997;3(3):335–342. doi: 10.3201/eid0303.970310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinshpun S.A., Mainelis G., Trunov M., Adhikari A., Reponen T., Willeke K. Evaluation of ionic air purifiers for reducing aerosol exposure in confined indoor spaces. Indoor Air. 2005;15(4):235–245. doi: 10.1111/j.1600-0668.2005.00364.x. [DOI] [PubMed] [Google Scholar]
- Grinshpun S.A., Adhikari A., Li C., Yermakov M., Reponen L., Johansson E., Trunov M. Inactivation of aerosolized viruses in continuous air flow with axial heating. Aerosol. Sci. Technol. 2010;44(11):1042–1048. [Google Scholar]
- Grinshpun S.A., Adhikari A., Yermakov M., Reponen T., Dreizin E., Schoenitz M., Hoffmann V., Zhang S. Inactivation of aerosolized Bacillus atrophaeus (BG) endospores and MS2 viruses by combustion of reactive materials. Environ. Sci. Technol. 2012;46(13):7334–7341. doi: 10.1021/es300537f. [DOI] [PubMed] [Google Scholar]
- Grinshpun S.A., Schoenitz M., Dreizin E., Adhikari A., Reponen T., Yermakov M. 2013. Inactivation of Aerosolized Biological Agents Using Filled Nanocomposite Materials. [Google Scholar]
- Heo K.J., Jeong S., Bin, Shin J., Hwang G.B., Ko H.S., Kim Y., Choi D.Y., Jung J.H. Water-repellent TiO2-organic dye-based air filters for efficient visible-light-activated photochemical inactivation against bioaerosols. Nano Lett. 2020;21(4):1576–1583. doi: 10.1021/acs.nanolett.0c03173. [DOI] [PubMed] [Google Scholar]
- Hernández-Díaz D., Martos-Ferreira D., Hernández-Abad V., Villar-Ribera R., Tarrés Q., Rojas-Sola J.I. Indoor PM2.5 removal efficiency of two different non-thermal plasma systems. J. Environ. Manag. 2021;278(October 2020):111515. doi: 10.1016/j.jenvman.2020.111515. [DOI] [PubMed] [Google Scholar]
- Hinds W.C. John Wiley & Sons, Inc; 1999. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. [Google Scholar]
- Huang R., Agranovski I., Pyankov O., Grinshpun S. Removal of viable bioaerosol particles with a low-efficiency HVAC filter enhanced by continuous emission of unipolar air ions. Indoor Air. 2008;18(2):106–112. doi: 10.1111/j.1600-0668.2007.00512.x. [DOI] [PubMed] [Google Scholar]
- Hugo W.B. A brief history of heat, chemical and radiation preservation and disinfection. Int. Biodeterior. Biodegrad. 1995;36(3–4):197–217. [Google Scholar]
- Hyun J., Lee S.G., Hwang J. Application of corona discharge-generated air ions for filtration of aerosolized virus and inactivation of filtered virus. J. Aerosol Sci. 2017;107(February):31–40. doi: 10.1016/j.jaerosci.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang S.Y., Ma A., Ramachandran S. Negative air ions and their effects on human Health and air quality improvement. Int. J. Mol. Sci. 2018;19(10) doi: 10.3390/ijms19102966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe Y.H., Woo K., Hwang J. Fabrication of an anti-viral air filter with SiO2-Ag nanoparticles and performance evaluation in a continuous airflow condition. J. Hazard Mater. 2014;280:356–363. doi: 10.1016/j.jhazmat.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohanski M.A., Lo L.J., Waring M.S. Review of indoor aerosol generation, transport, and control in the context of COVID-19. Int. Forum Allergy Rhinol. 2020;10(10):1173–1179. doi: 10.1002/alr.22661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalski W. Design and optimization of UVGI air disinfection systems A thesis in architectural engineering by. Configurations. 2001;August [Google Scholar]
- Kowalski W.J., Bahnfleth W.P. UVGI design basics. Print. Circuit Des. 2000;18(9):100–110. [Google Scholar]
- Kowalski W.J., Bahnfleth W.P. Effective UVGI system design through improved modeling. ASHRAE Trans. 2000;106(November) [Google Scholar]
- Kowalski W.J., Bahnfleth W.P. Proposed standards and guidelines for UVGI air disinfection. IUVA News. 2004;6(1):20–25. [Google Scholar]
- Kowalski W.J., Bahnfleth W.P. 2014. A SPECULAR MODEL FOR UVGI AIR DISINFECTION SYSTEMS. December. [Google Scholar]
- Krishna M.T., Springall D., Meng Q.H., Withers N., Macleod D., Biscione G., Frew A., Polak J., Holgate S. Effects of ozone on epithelium and sensory nerves in the bronchial mucosa of healthy humans. Am. J. Respir. Crit. Care Med. 1997;156(3 I):943–950. doi: 10.1164/ajrccm.156.3.9612088. [DOI] [PubMed] [Google Scholar]
- Kroumpouzos G., Gupta M., Jafferany M., Lotti T., Sadoughifar R., Sitkowska Z., Goldust M. COVID-19: a relationship to climate and environmental conditions? Dermatol. Ther. 2020;33(4):8–9. doi: 10.1111/dth.13399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai A.C.K., Cheung A.C.T., Wong M.M.L., Li W.S. Evaluation of cold plasma inactivation efficacy against different airborne bacteria in ventilation duct flow. Build. Environ. 2016;98:39–46. [Google Scholar]
- Lee B., Bahnfleth W., Auer K. 11th International IBPSA Conference - Building Simulation 2009. Scotland; Glasgow: 2009. Life-cycle cost simulation of in-duct ultraviolet germicidal irradiation systems; pp. 1159–1166. [Google Scholar]
- Li Y., Leung G.M., Tang J.W., Yang X., Chao C.Y.H., Lin J.Z., Lu J.W., Nielsen P.V., Niu J., Qian H., Sleigh A.C., Su H.-J.J., Sundell J., Wong T.W., Yuen P.L. Role of ventilation in airborne transmission of infectious agents in the built Environment ;? A multidisciplinary systematic review. Indoor Air. 2007;17(1):2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- Lim E.W.C., Heng Koh S., Kuang Lim L., Hoon Ore S., Kiat Tay B., Ma Y., Wang C.H. Experimental and computational studies of liquid aerosol evaporation. J. Aerosol Sci. 2008;39(7):618–634. [Google Scholar]
- Lippmann M. Health effects of ozone A critical review. J. Air Pollut. Contr. Assoc. 1989;39(5):672–695. doi: 10.1080/08940630.1989.10466554. [DOI] [PubMed] [Google Scholar]
- López M., Calvo T., Prieto M., Múgica-Vidal R., Muro-Fraguas I., Alba-Elías F., Alvarez-Ordóñez A. A review on non-thermal atmospheric plasma for food preservation: mode of action, determinants of effectiveness, and applications. Front. Microbiol. 2019;10(APR) doi: 10.3389/fmicb.2019.00622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Zhang G.J., Shi X.M., Xu G.M., Yang Y. Chemical mechanisms of bacterial inactivation using dielectric barrier discharge plasma in atmospheric air. IEEE Trans. Plasma Sci. 2008;36(4 PART 3):1615–1620. [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin D.J.H., Denyer S.P., McDonnell G., Maillard J.Y. Resistance and cross-resistance to oxidising agents of bacterial isolates from endoscope washer disinfectors. J. Hosp. Infect. 2008;69(4):377–383. doi: 10.1016/j.jhin.2008.04.010. [DOI] [PubMed] [Google Scholar]
- Mecenas P., da Rosa Moreira Bastos R.T., Rosário Vallinoto A.C., Normando D. Effects of temperature and humidity on the spread of COVID-19: a systematic review. PloS One. 2020;15(9 September):1–21. doi: 10.1371/journal.pone.0238339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzies D., Popa J., Hanley J.A., Rand T., Milton D.K. Effect of ultraviolet germicidal lights installed in office ventilation systems on workers' Health and wellbeing: double-blind multiple crossover trial. Lancet. 2003;362(9398):1785–1791. doi: 10.1016/S0140-6736(03)14897-0. [DOI] [PubMed] [Google Scholar]
- Mikaeva S.A., Mikaeva A.S., Brysin A.N. Ultraviolet air disinfection in ventilation and air conditioning systems. IOP Conf. Ser. Mater. Sci. Eng. 2020;913(4) [Google Scholar]
- Monge M.E., George C., D'Anna B., Doussin J.-F., Jammoul A., Wang J., Eyglunent G., Solignac G., Daële V., Mellouki A. Ozone formation from illuminated titanium dioxide surfaces. J. Am. Chem. Soc. 2010;132(24):8234–8235. doi: 10.1021/ja1018755. [DOI] [PubMed] [Google Scholar]
- Moreau M., Orange N., Feuilloley M.G.J. Non-thermal plasma technologies: new tools for bio-decontamination. Biotechnol. Adv. 2008;26(6):610–617. doi: 10.1016/j.biotechadv.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Narayanan D.L., Saladi R.N., Fox J.L. Ultraviolet radiation and skin cancer. Int. J. Dermatol. 2010;49(9):978–986. doi: 10.1111/j.1365-4632.2010.04474.x. [DOI] [PubMed] [Google Scholar]
- Nembhard M.D., Burton D.J., Cohen J.M. Ventilation use in nonmedical settings during COVID-19: cleaning protocol, maintenance, and recommendations. Toxicol. Ind. Health. 2020;36(9):644–653. doi: 10.1177/0748233720967528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicas M., Miller S.L. A multi-zone model evaluation of the efficacy of upper-room Air ultraviolet germicidal irradiation. Appl. Occup. Environ. Hyg. 1999;14(5):317–328. doi: 10.1080/104732299302909. [DOI] [PubMed] [Google Scholar]
- Norval M. The effect of ultraviolet radiation on human viral infections. Photochem. Photobiol. 2006;82(6):1495. doi: 10.1562/2006-07-28-IR-987. [DOI] [PubMed] [Google Scholar]
- Nuvolone D., Petri D., Voller F. The effects of ozone on human Health. Environ. Sci. Pollut. Res. 2018;25(9):8074–8088. doi: 10.1007/s11356-017-9239-3. [DOI] [PubMed] [Google Scholar]
- Occupational Safety and Health Administration Chlorine dioxide. 2020. https://www.osha.gov/chemicaldata/chemResult.html?recNo=16 OSHA Occup. Chem. Database [Online]. Available:
- Ogata N., Shibata T. Protective effect of low-concentration chlorine dioxide gas against influenza A virus infection. J. Gen. Virol. 2008;89(1):60–67. doi: 10.1099/vir.0.83393-0. [DOI] [PubMed] [Google Scholar]
- Park K.-T., Hwang J. Filtration and inactivation of aerosolized bacteriophage MS2 by a CNT air filter fabricated using electro-aerodynamic deposition. Carbon N. Y. 2014;75:401–410. doi: 10.1016/j.carbon.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J.-H., Yoon K.-Y., Kim Y.-S., Byeon J.H., Hwang J. Removal of submicron aerosol particles and bioaerosols using carbon fiber ionizer assisted fibrous medium filter media. J. Mech. Sci. Technol. 2009;23(7):1846–1851. [Google Scholar]
- Pazokifard S., Mirabedini S.M., Esfandeh M., Farrokhpay S. Fluoroalkylsilane treatment of TiO 2 nanoparticles in difference PH values: characterization and mechanism. Adv. Powder Technol. 2012;23(4):428–436. [Google Scholar]
- Pekárek S. Non-thermal plasma ozone generation. Acta Polytech. 2003;43(6) [Google Scholar]
- Peters A., Parneix P., Otter J., Pittet D. Putting some context to the aerosolization debate around SARS-CoV-2. J. Hosp. Infect. 2020;105(2):381–382. doi: 10.1016/j.jhin.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyankov O.V., Usachev E.V., Pyankova O., Agranovski I.E. Inactivation of airborne influenza virus by tea tree and Eucalyptus oils. Aerosol Sci. Technol. 2012;46(12):1295–1302. [Google Scholar]
- Pyrgiotakis G., McDevitt J., Bordini A., Diaz E., Molina R., Watson C., Deloid G., Lenard S., Fix N., Mizuyama Y., Yamauchi T., Brain J., Demokritou P. A chemical free, nanotechnology-based method for airborne bacterial inactivation using engineered water nanostructures. Environ. Sci. Nano. 2014;1(1):15–26. doi: 10.1039/C3EN00007A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raeiszadeh M., Adeli B. A critical review on ultraviolet disinfection systems against COVID-19 outbreak: applicability, validation, and safety considerations. ACS Photonics. 2020;7(11):2941–2951. doi: 10.1021/acsphotonics.0c01245. [DOI] [PubMed] [Google Scholar]
- Reed N.G. The history of ultraviolet germicidal irradiation for air disinfection. Publ. Health Rep. 2010;125(1):15–27. doi: 10.1177/003335491012500105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley R.L. The ecology of indoor atmospheres: airborne infection in hospitals. J. Chron. Dis. 1972;25:421–423. doi: 10.1016/0021-9681(72)90204-4. [DOI] [PubMed] [Google Scholar]
- Riley R.L. Indoor airborne infection. Environ. Int. 1982;8(1–6):317–320. [Google Scholar]
- Riley E.C., Murphy G., Riley R.L. Airborne spread of measles in a suburban elementary school. Am. J. Epidemiol. 1978;107(5):421–432. doi: 10.1093/oxfordjournals.aje.a112560. [DOI] [PubMed] [Google Scholar]
- Santos A.F., Gaspar P.D., Hamandosh A., Aguiar E. B. de, Guerra Filho A.C., Souza H. J. L. de. Best practices on HVAC design to minimize the risk of COVID-19 infection within indoor environments. Braz. Arch. Biol. Technol. 2020;63 [Google Scholar]
- Sawant V.S., Jadhav D.B. vol. 30. 2012. pp. 63–67. (Laboratory Experiments on Aerosol Removal by Negative Air Ions). [Google Scholar]
- Sawant V.S., Meena G.S., Jadhav D.B. Effect of negative air ions on fog and smoke. Aerosol Air Qual. Res. 2012;12(5):1007–1015. [Google Scholar]
- Schiappacasse C., Peng P., Zhou N., Liu X., Zhai J., Cheng Y., Shao J., Verma V., Singh N., Chen P., Janni K.A., Liang Y., Noll S., Ruan R.R. Inactivation of aerosolized Newcastle Disease virus with non-thermal plasma. Appl. Eng. Agric. 2020;36(1):55–60. [Google Scholar]
- Schinköthe J., Scheinemann H.A., Diederich S., Freese H., Eschbaumer M., Teifke J.P., Reiche S. Airborne disinfection by dry fogging efficiently inactivates severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), mycobacteria, and bacterial spores and shows limitations of commercial spore carriers. Appl. Environ. Microbiol. 2020;87(3):1–14. doi: 10.1128/AEM.02019-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S.K., Sharma A. Sterilization of microorganisms contaminated surfaces and its treatment with dielectric barrier discharge plasma. Trans. Indian Natl. Acad. Eng. 2020;5(2):321–326. doi: 10.1007/s41403-020-00124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yan H., Li X., Zhao C., Liu W., He M., Tang S., Xi S. The impact of temperature and absolute humidity on the coronavirus Disease 2019 (COVID-19) outbreak - evidence from China. medRxiv. 2020;77 [Google Scholar]
- Sigma-Aldrich . Sigma-Aldrich; 2021. Titanium(IV) Oxide - Nanopowder, 21 Nm Primary Particle Size (TEM), ≥99.5% Trace Metals Basis. [Google Scholar]
- Skyspring . Skyspring Nanomater. inc; 2021. Silicon Dioxide Nanoparticles/Nanopowder (98.7%, 20nm) [Google Scholar]
- Spena A., Palombi L., Corcione M., Carestia M., Spena V.A. On the optimal indoor air conditions for sars-cov-2 inactivation. An enthalpy-based approach. Int. J. Environ. Res. Publ. Health. 2020;17(17):1–15. doi: 10.3390/ijerph17176083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilianakis N.I., Drossinos Y. Dynamics of infectious Disease transmission by inhalable respiratory droplets. J. R. Soc. Interface. 2010;7(50):1355–1366. doi: 10.1098/rsif.2010.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung J.H., Kim M., Kim Y.J., Han B., Hong K.J., Kim H.J. Ultrafine particle cleaning performance of an ion spray electrostatic air cleaner emitting zero ozone with diffusion charging by carbon fiber. Build. Environ. 2019;166(August) [Google Scholar]
- Suwardi A., Ooi C.C., Daniel D., Tan C.K.I., Li H., Liang O.Y.Z., Tang Y.K., Chee J.Y., Sadovoy A., Jiang S.-Y., Ramachandran S., Ye E., Kang C.W., Cheong W.C.D., Lim K.H., Loh X.J. The efficacy of plant-based ionizers in removing aerosol for COVID-19 mitigation. Research. 2021;2021:1–11. doi: 10.34133/2021/2173642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng C.C., Li C.S. Inactivation of virus-containing aerosols by ultraviolet germicidal irradiation. Aerosol Sci. Technol. 2005;39(12):1136–1142. [Google Scholar]
- Turgeon N., Toulouse M.-J., Martel B., Moineau S., Duchaine C. Comparison of five bacteriophages as models for viral aerosol studies. Appl. Environ. Microbiol. 2014;80(14):4242–4250. doi: 10.1128/AEM.00767-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uk Lee B., Yermakov M., Grinshpun S.A. Removal of fine and ultrafine particles from indoor air environments by the unipolar ion emission. Atmos. Environ. 2004;38(29):4815–4823. doi: 10.1016/j.atmosenv.2004.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaze N., Pyrgiotakis G., McDevitt J., Mena L., Melo A., Bedugnis A., Kobzik L., Eleftheriadou M., Demokritou P. Inactivation of common hospital acquired pathogens on surfaces and in air utilizing engineered water nanostructures (EWNS) based nano-sanitizers. Nanomed. Nanotechnol. Biol. Med. 2019;18:234–242. doi: 10.1016/j.nano.2019.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vranay F., Pirsel L., Kacik R., Vranayova Z. Adaptation of HVAC systems to reduce the spread of COVID-19 in buildings. Sustainability. 2020;12(23):9992. [Google Scholar]
- Walker C.M., Ko G. Effect of ultraviolet germicidal irradiation on viral aerosols. Environ. Sci. Technol. 2007;41(15):5460–5465. doi: 10.1021/es070056u. [DOI] [PubMed] [Google Scholar]
- Wells W.F. On airborne infection. Study II: droplets and droplet nuclei. Am. J. Epidemiol. 1934;20(3):611–618. [Google Scholar]
- Woo M.H., Grippin A., Wu C.Y., Baney R.H. Use of dialdehyde starch treated filters for protection against airborne viruses. J. Aerosol Sci. 2012;46:77–82. doi: 10.1016/j.jaerosci.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., Du M., Liu M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:1–7. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia T., Kleinheksel A., Lee E.M., Qiao Z., Wigginton K.R., Clack H.L. Inactivation of airborne viruses using a packed bed non-thermal plasma reactor. J. Phys. D Appl. Phys. 2019;52(25) doi: 10.1088/1361-6463/ab1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Elankumaran S., Marr L.C. Relationship between humidity and influenza A viability in droplets and implications for influenza's seasonality. PloS One. 2012;7(10):e46789. doi: 10.1371/journal.pone.0046789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehia A., Abdel-Salam M., Mizuno A. On assessment of ozone generation in dc coronas. J. Phys. D Appl. Phys. 2000;33(7):831–835. [Google Scholar]
- Yu L., Peel G.K., Cheema F.H., Lawrence W.S., Bukreyeva N., Jinks C.W., Peel J.E., Peterson J.W., Paessler S., Hourani M., Ren Z. Catching and killing of airborne SARS-CoV-2 to control spread of COVID-19 by a heated air disinfection system. Mater. Today Phys. 2020;15:100249. doi: 10.1016/j.mtphys.2020.100249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S., Jiang S.C., Li Z.L. Do humidity and temperature impact the spread of the novel coronavirus? Front. Public Heal. 2020;8(May):8–11. doi: 10.3389/fpubh.2020.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziental D., Czarczynska-Goslinska B., Mlynarczyk D.T., Glowacka-Sobotta A., Stanisz B., Goslinski T., Sobotta L. Titanium dioxide nanoparticles: prospects and applications in medicine. Nanomaterials. 2020;10(2):387. doi: 10.3390/nano10020387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- What is a MERV rating? 2021. https://www.epa.gov/indoor-air-quality-iaq/what-merv-rating-1 United States Environ. Prot. Agency [Online]. Available: