Abstract
Objective:
To evaluate differences in discomfort levels between patients treated with aligners and traditional fixed orthodontic appliances.
Materials and Methods:
This blinded, prospective, randomized equivalence two-arm parallel trial allocated 41 adult Class I nonextraction patients to either traditional fixed appliance (6 males and 12 females) or aligner (11 males and 12 females) treatment. Patients completed daily discomfort diaries following their initial treatment appointment, after 1 month and after 2 months. They recorded their levels of discomfort at rest, while chewing, and while biting, as well as their analgesic consumption and sleep disturbances.
Results:
Both treatment modalities demonstrated similar levels of initial discomfort. There were no significant sex differences. Patients in the traditional fixed appliances group reported significantly (P < .05) greater discomfort than patients in the aligner group during the first week of active treatment. There was significantly more discomfort while chewing than when at rest. Traditional patients also reported significantly more discomfort than aligner patients after the first and second monthly adjustment appointments. Discomfort after the subsequent adjustments was consistently lower than after the initial bonding or aligner delivery appointments. A higher percentage of patients in the fixed-appliance group reported taking analgesics during the first week for dental pain, but only the difference on day 2 was statistically significant.
Conclusions:
Patients treated with traditional fixed appliances reported greater discomfort and consumed more analgesics than patients treated with aligners. This trial was not registered.
Keywords: Discomfort, Pain, Invisalign, Traditional brackets
INTRODUCTION
Pain and discomfort are common side effects of orthodontic treatment.1–3 Fear of pain is one of the primary reasons that patients fail to seek orthodontic care.4 Pain has a negative effect on patients' compliance,5 oral hygiene, and missed appointments.6 Its effects on patients' daily lives is a major reason for discontinuance of orthodontic treatment.7
The vast majority of orthodontic patients experience pain while in treatment.1 Pain patterns associated with traditional fixed appliances have been well established,1,8–10 peaking approximately 24 hours after the initiation of treatment, and decreasing thereafter.1 While the first week of treatment has been extensively studied, pain and physical discomfort experienced by patients further into treatment have not been thoroughly investigated.
Since their introduction to the market in 1997 by Align Technologies, clear aligners have quickly become one of the preferred orthodontic appliances for patients who are concerned with esthetics. It was initially shown that traditional braces were approximately 25% more painful during the first week of treatment than was Invisalign.11 It was also reported that pain was greater in patients treated with aligners than with fixed braces.12 Recently, Fujiyama et al. showed more pain with fixed appliances than with aligners but differences were statistically significant at only some of the time points.13 None of the previous studies evaluating pain among aligner patients randomly assigned their treatment modalities, which increases the likelihood of biased results.
The primary objective of this study was to compare the discomfort levels produced by traditional fixed appliances and Invisalign (Align Technology, Santa Clara, Calif) aligners at multiple time points. Secondarily, the study sought to compare their effects on pain medication usage and sleep disturbances.
MATERIALS AND METHODS
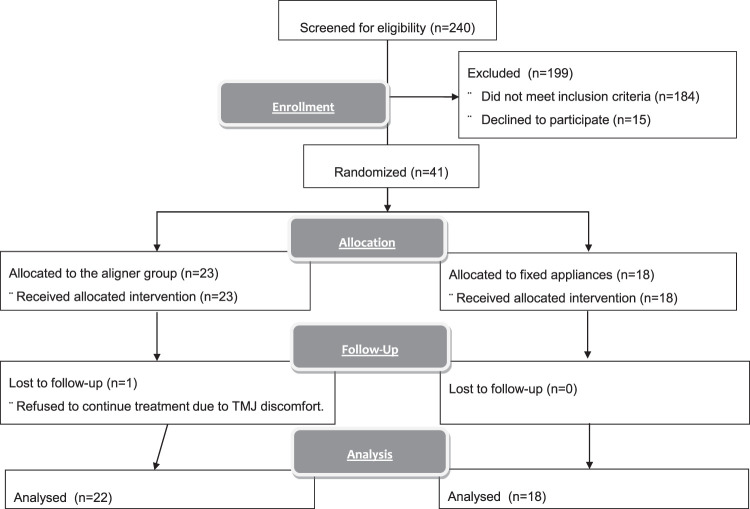
The sample was recruited from an ongoing study conducted by the Department of Orthodontics at Texas A&M University Baylor College of Dentistry. Based on the reported effect size for pain,1,9 power analysis indicated that 16 patients per group were needed for an alpha of 0.05 and a power of 95. Of the 240 individuals who responded to posted recruiting announcements, 184 did not qualify (Figure 1). An additional 15 patients declined to participate after they were informed that they could be allocated to either treatment group. There were 41 patients admitted to the study (17 males, 24 females). The study was approved by the Texas A&M University Baylor College of Dentistry IRB (Approval 2012-21-BCD). The patients were recruited between September 2013 and May 2015.
Figure 1.
Diagram of patient flow through the study.
The patients were allocated using Microsoft Excel simple randomization (generated by author P.H.B.). The subjects were enrolled and assigned to the interventions by K.C.J. and H.J.; data were collected by D.W.W. This was a two-arm parallel trial, conducted to determine whether the 23 subjects allocated to the aligner group experienced the same level of discomfort as the 18 patients allocated to the traditional group. Patients had to fulfill the following criteria:
Inclusion Criteria
Class I molar and canine relationships
Nonextraction treatment
Maxillary and mandibular crowding of 4 mm or less
No missing teeth (from second molar to second molar).
Exclusion Criteria
Anterior or posterior crossbites
Anterior or lateral open bites
Severe deep bites
Maxillary overjet exceeding 3 mm
Impacted teeth (other than third molars)
Unwilling to be treated with either Invisalign or traditional clear braces
Patients were treated by two clinicians, with one performing all the ClinChecks and about 90% of the bandings and debondings. Those patients in the aligner group had either a polyvinylsiloxane impression made or were scanned using an iTero scanner. A series of removable polyurethane aligners was fabricated using Align Technology's ClinCheck software. All composite attachments were placed at the initial aligner delivery appointment. Patients were given two sets of aligners and instructed to wear the first set for 22 hours per day for 2 weeks; they changed to the new set of trays on the 15th day. Evaluation appointments were scheduled every month. There were no important changes to the methods after commencement of the trial.
The traditional fixed appliances consisted of American Orthodontics' Radiance clear brackets in the maxillary arch (0.018-inch MBT prescription), and stainless steel brackets in the mandibular arch. The mandibular brackets used were a 0.018 × 0.028-inch Alexander prescription (American Orthodontics, Sheboygan, Wisc). Brackets and tubes were bonded to the maxillary and mandibular teeth from second molar to second molar at the same appointment. A sequence of copper NiTi (0.016-inch and 0.017 × 0.025-inch) and stainless steel (0.016 × 0.022-inch and 0.017 × 0.025-inch) wires were used. Because the patients had mild malocclusions, all the copper NiTi wires could be fully engaged at the initial appointment. Patients were scheduled for appointments every month. All treatments were conducted in the research clinic of the orthodontic department, Texas A&M University Baylor College of Dentistry.
Assessments were based on daily discomfort diaries. The first was completed immediately following initial bonding or delivery of Invisalign trays, and each day for 7 days. Patients also completed diaries for 4 days after each of their subsequent adjustment appointments (ie, after 1 and 2 months). Four days was chosen because patients have been shown previously to adapt to the pain and discomfort of orthodontics within the first 3–5 days.2,5,14
The daily diaries, which consisted of eight questions, were collected at the adjustment appointments. To establish a baseline and assess reliability, the first question asked about the worst discomfort ever experienced. The next four questions asked about the amounts of discomfort they were experiencing currently, the last time they chewed, when they bite down on their back teeth, and when they bite down on the front teeth. All responses were recorded on a 10-cm visual analog scale (VAS), using No Discomfort and Worst Discomfort as anchors. The VAS was measured by one blinded investigator (D.W.W.) to the nearest 0.01 mm using a digital caliper. The secondary outcomes assessed whether the patient's sleep was affected and the frequency of analgesic consumption. Four of the 123 diaries were either lost or not returned.
Statistical Analysis
All statistics were calculated using SPSS version 18 software (SPSS Inc, Chicago, Ill). Due to skewness and kurtosis of the results, medians and interquartile ranges were used to describe the results, and group differences were compared using the nonparametric Mann-Whitney test. Significance level for all tests was set at P < .05.
RESULTS
Based on the first question, both treatment groups demonstrated strong rating reliability, with intraclass correlations ranging from 0.917 to 0.986.
Initial Adjustment
Immediately following appliance placement, the patients in the traditional group reported low levels of discomfort (Table 1). They then showed significant (P < .05) increases in discomfort (300%–500%) that peaked between the first and third day. The greatest discomfort was reported when chewing and biting on the front teeth. Following the peak, there was a gradual reduction in discomfort over the next 4–5 days, ending at levels similar to or slightly above those reported at baseline. Patients in the traditional treatment group reported significantly more discomfort while chewing than at rest. They also reported greater discomfort when biting down on their front than back teeth during the first few days, but the differences were not statistically significant.
Table 1.
Discomfort (Measured as % of 10-cm Visual Analog Scale [VAS]) Associated With Invisalign and Traditional Orthodontic Treatment at Initial Delivery or Appliance Placement, Described Using Medians (Med) and Interquartile Ranges (Bold = probability of change < .05)
| Question |
Baseline |
Day |
|||||||||||||
| Day 1 |
Day 2 |
Day 3 |
Day 4 |
||||||||||||
| 25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
|
| Current discomfort | |||||||||||||||
| Invisalign | 3.3 | 11.87 | 17.1 | 7.1 | 13.59 | 36.9 | 8.3 | 13.08 | 36.7 | 4.6 | 10.68 | 39.2 | 6.1 | 11.31 | 20.4 |
| Traditional | 4.6 | 10.62 | 22.1 | 21.0 | 26.79 | 46.4 | 26.8 | 28.92 | 46.7 | 17.0 | 32.85 | 53.0 | 12.8 | 26.85 | 54.2 |
| Prob. | .564 | .138 | .073 | .039 | .029 | ||||||||||
| Last time chewed | |||||||||||||||
| Invisalign | 1.5 | 7.57 | 19.1 | 8.5 | 13.41 | 27.1 | 8.0 | 15.58 | 42.2 | 2.0 | 9.01 | 44.2 | 0.9 | 10.28 | 36.4 |
| Traditional | 3.1 | 8.59 | 24.8 | 30.6 | 43.00 | 60.6 | 31.6 | 39.20 | 70.4 | 21.7 | 46.91 | 65.1 | 12.5 | 34.76 | 66.5 |
| Prob. | .780 | .051 | .043 | .023 | .015 | ||||||||||
| Back teeth | |||||||||||||||
| Invisalign | 2.1 | 9.84 | 15.7 | 6.6 | 10.78 | 30.3 | 8.7 | 14.34 | 35.3 | 2.1 | 10.12 | 23.4 | 0.7 | 9.13 | 19.7 |
| Traditional | 4.5 | 14.85 | 22.2 | 25.8 | 37.11 | 57.8 | 27.3 | 30.78 | 42.6 | 22.1 | 30.75 | 56.7 | 10.5 | 33.82 | 44.5 |
| Prob. | .138 | .026 | .051 | .012 | .021 | ||||||||||
| Front teeth | |||||||||||||||
| Invisalign | 1.6 | 12.70 | 23.2 | 10.0 | 21.19 | 61.8 | 11.9 | 20.33 | 57.6 | 4.3 | 13.12 | 58.5 | 0.5 | 11.04 | 35.0 |
| Traditional | 4.4 | 20.18 | 29.5 | 38.6 | 50.43 | 60.3 | 26.0 | 48.26 | 66.0 | 23.4 | 46.53 | 58.8 | 13.0 | 23.84 | 64.0 |
| Prob. | .423 | .188 | .078 | .043 | .056 | ||||||||||
Table 1.
Extended
| Day | ||||||||
| Day 5 |
Day 6 |
Day 7 |
||||||
| 25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
| 0.0 | 5.70 | 11.2 | 0.2 | 5.54 | 16.7 | 0.0 | 3.19 | 13.1 |
| 13.7 | 17.83 | 36.8 | 10.3 | 15.03 | 26.3 | 77.0 | 13.80 | 26.5 |
| .004 | .011 | .008 | ||||||
| 0.0 | 4.32 | 17.7 | 0.2 | 4.00 | 15.7 | 0.0 | 3.20 | 10.4 |
| 14.9 | 24.05 | 54.9 | 14.5 | 21.67 | 34.5 | 11.4 | 18.80 | 29.2 |
| .002 | .010 | .001 | ||||||
| 0.0 | 4.94 | 12.3 | 0.2 | 5.62 | 12.8 | 0.0 | 3.23 | 10.8 |
| 11.4 | 24.18 | 38.6 | 9.7 | 20.52 | 30.5 | 6.2 | 18.75 | 26.8 |
| .002 | .012 | .010 | ||||||
| 0.0 | 8.36 | 18.0 | 0.3 | 6.63 | 19.9 | 0.0 | 2.92 | 13.3 |
| 15.7 | 22.64 | 49.1 | 5.8 | 18.16 | 44.1 | 7.0 | 18.08 | 32.4 |
| .043 | .043 | .011 | ||||||
Aligners produced a similar pattern of discomfort. Initially, patients reported low levels of discomfort, followed by slight increases (50%–100%), peaking after the first or second day. Discomfort levels then decreased slowly over the rest of the first week. By day 7, patients in the aligner group experienced minimal discomfort, consistently less than baseline discomfort.
There were no statistically significant group differences at baseline (Table 1). Between day 1 and day 7, the traditional group consistently demonstrated greater discomfort than did the aligner group. Discomfort was significantly higher in the traditional group during most of the first week, with statistically significant differences after 2–3 days.
Subsequent Adjustments
Discomfort after the first and second monthly adjustments was also consistently less for aligner than traditional treatment. Many of the group differences after the first month's adjustment were statistically significant (Tables 2 and 3). For both groups, the discomfort levels reported at subsequent adjustments peaked at much lower levels than after initial bonding or Invisalign delivery.
Table 2.
Discomfort (Measured as % of 10-cm VAS) Associated With Invisalign and Traditional Orthodontic Treatment for the First Month's Adjustment, Described Using Medians (Med) and Interquartile Ranges (Bold = probability of change < .05)
| Question |
Baseline |
Day |
|||||||||||||
| Day 1 |
Day 2 |
Day 3 |
Day 4 |
||||||||||||
| 25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
|
| Current discomfort | |||||||||||||||
| Invisalign | 1.07 | 6.37 | 36.53 | 0.33 | 5.05 | 29.27 | 0.17 | 4.19 | 23.46 | 0.00 | 3.56 | 16.58 | 0.00 | 2.40 | 17.85 |
| Traditional | 7.62 | 16.17 | 37.32 | 10.83 | 16.87 | 33.13 | 12.81 | 19.64 | 29.27 | 6.67 | 10.58 | 19.73 | 8.38 | 16.33 | 21.94 |
| Prob. | .081 | .045 | .041 | .087 | .119 | ||||||||||
| Last time chewed | |||||||||||||||
| Invisalign | 1.19 | 5.58 | 34.07 | 1.16 | 5.16 | 42.76 | 0.17 | 4.19 | 23.46 | 0.00 | 3.58 | 16.58 | 0.00 | 2.40 | 17.85 |
| Traditional | 9.91 | 23.04 | 40.88 | 12.15 | 20.72 | 37.42 | 11.33 | 20.84 | 33.25 | 7.59 | 12.93 | 19.62 | 9.37 | 12.70 | 22.93 |
| Prob. | .037 | .049 | .049 | .063 | .056 | ||||||||||
| Back teeth | |||||||||||||||
| Invisalign | 0.36 | 5.64 | 16.08 | 0.29 | 3.72 | 22.84 | 0.28 | 3.48 | 13.01 | 0.00 | 2.94 | 11.59 | 0.00 | 2.96 | 12.55 |
| Traditional | 6.73 | 17.49 | 34.46 | 11.33 | 20.62 | 32.49 | 10.48 | 21.27 | 27.49 | 7.90 | 11.08 | 17.01 | 8.84 | 12.91 | 20.65 |
| Prob. | .049 | .014 | .034 | .041 | .051 | ||||||||||
| Front teeth | |||||||||||||||
| Invisalign | 1.68 | 6.35 | 38.21 | 1.77 | 3.86 | 41.01 | 1.70 | 4.01 | 21.38 | 0.17 | 4.67 | 11.37 | 0.30 | 4.91 | 15.17 |
| Traditional | 7.30 | 22.33 | 44.31 | 8.63 | 16.14 | 43.39 | 11.07 | 20.13 | 30.48 | 8.29 | 10.64 | 23.50 | 8.53 | 14.85 | 23.37 |
| Prob. | .127 | .146 | 0.127 | .102 | .110 | ||||||||||
Table 3.
Discomfort (Measured as % of 10-cm VAS) Associated With Invisalign and Traditional Orthodontic Treatment for the Second Month's Adjustment, Described Using Medians (Med) and Interquartile Ranges
| Question |
Baseline |
Day |
|||||||||||||
| Day 1 |
Day 2 |
Day 3 |
Day 4 |
||||||||||||
| 25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
25% |
Med |
75% |
|
| Current discomfort | |||||||||||||||
| Invisalign | 5.55 | 7.50 | 24.66 | 4.38 | 9.21 | 24.58 | 3.16 | 11.05 | 23.99 | 1.35 | 6.60 | 16.02 | 1.17 | 4.32 | 18.87 |
| Traditional | 11.02 | 23.26 | 30.73 | 14.77 | 22.39 | 32.43 | 11.26 | 19.06 | 38.30 | 7.04 | 15.15 | 25.70 | 6.19 | 12.16 | 26.74 |
| Prob. | .169 | .116 | .128 | .067 | .105 | ||||||||||
| Last time chewed | |||||||||||||||
| Invisalign | 4.81 | 8.47 | 32.87 | 5.33 | 8.14 | 28.85 | 4.35 | 6.32 | 25.50 | 2.46 | 6.85 | 12.79 | 1.23 | 7.12 | 20.36 |
| Traditional | 10.22 | 24.15 | 33.91 | 7.43 | 23.39 | 35.59 | 7.88 | 20.77 | 32.15 | 9.46 | 17.93 | 24.66 | 6.98 | 13.61 | 25.98 |
| Prob. | .259 | .141 | .141 | .095 | .202 | ||||||||||
| Back teeth | |||||||||||||||
| Invisalign | 2.88 | 7.63 | 29.17 | 3.02 | 4.70 | 29.41 | 0.33 | 5.98 | 22.04 | 0.26 | 3.41 | 11.64 | 0.00 | 1.88 | 16.78 |
| Traditional | 6.90 | 21.27 | 34.35 | 9.51 | 21.43 | 36.74 | 11.20 | 22.17 | 32.15 | 6.39 | 15.55 | 22.99 | 5.17 | 12.33 | 23.29 |
| Prob. | .220 | .094 | .076 | .060 | .068 | ||||||||||
| Front teeth | |||||||||||||||
| Invisalign | 3.80 | 6.47 | 32.66 | 5.17 | 7.90 | 29.06 | 4.05 | 9.64 | 28.49 | 2.22 | 6.82 | 14.32 | 1.01 | 6.24 | 19.92 |
| Traditional | 13.8 | 25.96 | 38.90 | 12.64 | 28.99 | 33.81 | 9.49 | 21.76 | 28.98 | 8.52 | 15.57 | 26.08 | 8.16 | 13.83 | 21.37 |
| Prob. | .185 | .141 | .141 | .193 | .220 | ||||||||||
The pattern of discomfort after the first and second monthly aligner adjustments was similar. Baseline discomfort was generally less than reported at the initial adjustments and then slowly decreased over the next 4 days (Figure 2A). With traditional treatment, baseline discomfort after the first and second month was generally higher than baseline discomfort after initial bonding (Figure 2B). Like the aligner group, the discomfort decreased gradually over the next 4 days. However, unlike during the first week of treatment, discomfort did not increase substantially following the 1- and 2-month adjustments. Discomfort after initial bonding was significantly higher than after the first-month adjustments for both the Invisalign and traditional groups.
Figure 2.
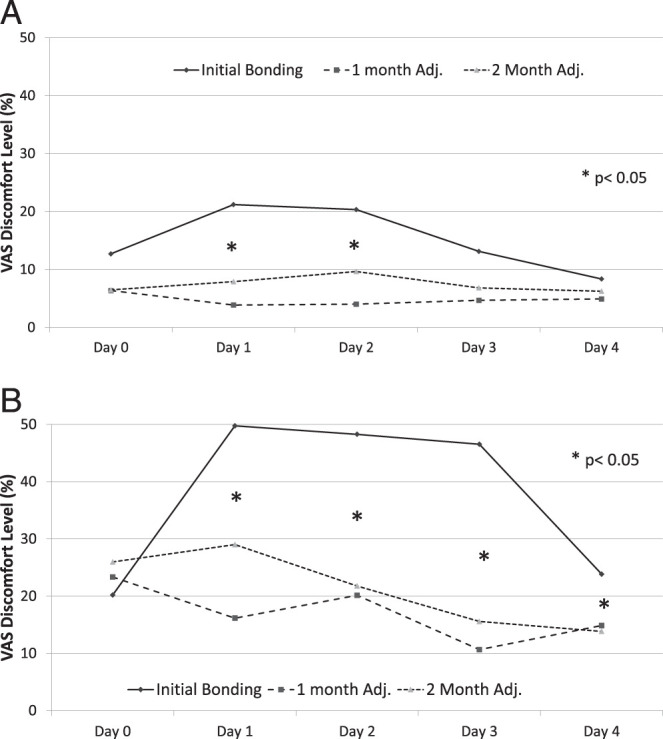
Median discomfort levels for (A) aligner and (B) traditional patients at initial bonding, and 1- and 2-month adjustments when biting on their front teeth.
Analgesic Consumption
Approximately 45% of patients in the traditional group took medication during the first 2 days, with numbers decreasing thereafter (Figure 3). The percentage of aligner patients taking medication increased by 11% during the first day and then decreased. While the percentages of patients taking medication was consistently greater in the traditional than aligner group, only the 50% difference on day 2 was statistically significant. Medications taken after the first and second adjustments showed no clear pattern and no statistically significant differences between the traditional and the Invisalign treatments (Table 4).
Figure 3.
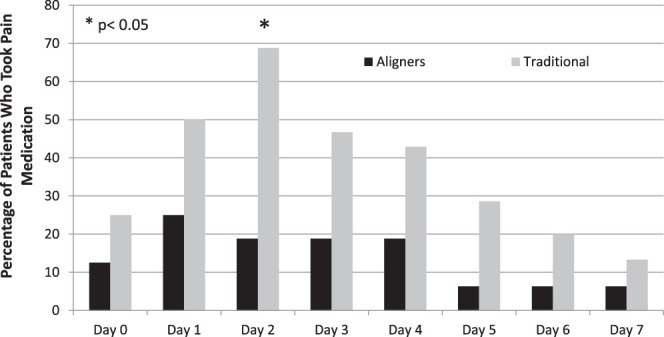
Percentages of patients who took medications for tooth pain during the first week.
Table 4.
Percentages of Patients Who Took Medications for Tooth Pain After the First-, Second-, and Sixth-Month Adjustments
| Adjustment |
Baseline |
Day |
|||
| Day 1 |
Day 2 |
Day 3 |
Day 4 |
||
| First adjustment | |||||
| Invisalign | 6.3 | 12.5 | 6.3 | 6.3 | 12.5 |
| Traditional | 23.1 | 16.7 | 0 | 7.7 | 9.1 |
| Prob. | 0.191 | 0.755 | 0.359 | 0.879 | 0.782 |
| Second adjustment | |||||
| Invisalign | 15.4 | 15.4 | 8.3 | 7.7 | 8.3 |
| Traditional | 9.1 | 0.0 | 0.0 | 0.0 | 0.0 |
| Prob. | 0.642 | 0.174 | 0.328 | 0.347 | 0.328 |
| Sixth adjustment | |||||
| Invisalign | 30.0 | 40.0 | 30.0 | 20.0 | 20.0 |
| Traditional | 22.2 | 22.2 | 0.0 | 0.0 | 0.0 |
| Prob. | 0.701 | 0.405 | 0.090 | 0.180 | 0.357 |
Sleep Disturbance
There was no consistent pattern and no statistically significant intergroup differences in the percentage of patients who had sleep disturbances during the first week. The frequency of patients reporting sleep disturbances decreased from approximately 30% on the first day to 15% on the seventh day, with no significant group differences (Table 5).
Table 5.
Percentages of Patients Who Had Sleep Disturbance From Tooth Pain After the First-, Second-, and Sixth-Month Adjustments
| Adjustment |
Day |
|||
| Day 1 |
Day 2 |
Day 3 |
Day 4 |
|
| First adjustment | ||||
| Invisalign | 18.8 | 18.8 | 18.8 | 18.8 |
| Traditional | 16.7 | 15.4 | 7.7 | 14.8 |
| Prob. | 0.887 | 0.811 | 0.390 | 0.488 |
| Second adjustment | ||||
| Invisalign | 23.1 | 16.7 | 7.7 | 8.3 |
| Traditional | 0.0 | 0.0 | 0.0 | 0.0 |
| Prob. | 0.089 | 0.156 | 0.347 | 0.328 |
| Sixth adjustment | ||||
| Invisalign | 10.0 | 10.0 | 0.0 | 0.0 |
| Traditional | 22.2 | 12.5 | 12.5 | 12.5 |
| Prob. | 0.466 | 0.867 | 0.250 | 0.250 |
DISCUSSION
Discomfort of patients treated with traditional fixed appliances increased dramatically during the first 24 hours after appliance placement; it peaked after 24–48 hours and then decreased steadily to baseline levels. Previous studies evaluating orthodontic pain/discomfort have also shown marked increases during the first 24 hours, followed by gradual decreases over the subsequent 6–7 days, to values similar to those observed at appliance placement.1,8,9,11,13 Increased discomfort over the first 24 hours correlates with an acute inflammatory response.15 Initial orthodontic forces cause discomfort through compression of the PDL, which leads to ischemia, edema, and the release of proinflammatory mediators during the first 24–48 hours. These inflammatory mediators, such as prostaglandins (eg, PgE) and interleukins (eg, IL-1β), sensitize nociceptors in the PDL and lower the discomfort threshold.16,17 The levels of PgE and IL-1β found in gingival crevicular fluid peak 24 hours after initiation of orthodontic force and fall to baseline after 7 days.18 The gradual reduction in pain observed over the course of the first week may be attributed to the decrease of inflammatory mediators in the PDL.
Peak discomfort during the first week produced by traditional appliances appears to depend on the archwire used. Patients in the traditional fixed appliances group reported peak discomfort that was approximately 33% of their worst discomfort imaginable. This is similar to levels reported for superelastic NiTi (29%) and less than peak discomfort reported for nitinol (42%).1,8 Initial nitinol archwires probably produce higher peak discomfort than superelastic NiTi archwires because they produce greater amounts of force.19,20 The current study used 0.016-inch copper NiTi archwires which, when loaded 2 mm, generate 47 g of force. Classic nitinol generates 180 g of force when loaded under the same conditions.20
Traditional fixed appliances produced more discomfort during the first week of treatment than did aligners. While baseline values were similar, discomfort between days 2 and 7 was significantly higher in the traditional group. Significantly less pain among aligner than traditional patients has been reported previously.11,13 Aligners may produce less discomfort because they are removable appliances, which are generally more comfortable than fixed appliances.5,21 Removable appliances provide intermittent forces, which allow the tissues to reorganize before compressive forces are reapplied.22
Aligners are also more comfortable than traditional fixed appliances after the first and second month's adjustments. Similar differences have been reported 3 and 5 weeks after appliance delivery.13 Reduced discomfort with aligners can be explained by proinflammatory mediators such as IL-1β. Over the short term, mediators increase sensitization by activating receptor-associated kinases and ion channels. Over the long term, they induce the transcriptional upregulation of receptors, leading to hyperalgesia.17 If fixed appliances cause greater initial discomfort due to an increased inflammatory response, then it is possible that patients with fixed appliances have more sensitized nociceptors, which affects their pain perception following subsequent adjustments.
Both treatments demonstrated less discomfort at the subsequent than at the initial adjustments, as previously suggested.13 Assuming a decrease in the pain threshold immediately after orthodontic forces are placed,23 the same stimulus should generate less painful signals months into treatment.
For patients in the traditional group, discomfort while chewing was significantly higher than at rest. Inflammatory mediators, such as substance P, have been shown to be present in the PDL following initiation of orthodontic forces.24 These mediators are believed to sensitize the nociceptors in the PDL.14 Chewing could compress previously sensitized nociceptors and stimulate a more painful signal than at rest. Importantly, this phenomenon was evident only in the traditional group, suggesting greater sensitivity of their nociceptors due to the continuous forces used.
Invisalign's new SmartTrack (Align Technology, Santa Clara, Calif) material appears to be more comfortable for patients than previously manufactured clear aligner materials. Patients in the aligner group reported small increases (17% of maximum) in discomfort that peaked during the first 24 hours and then decreased to baseline levels at day 7. Miller et al., who found a similar pattern between baseline and day 7, reported peak pain values at 40% of maximum.11 Although more studies are needed, this supports Invisalign's claims that SmartTrack may provide greater patient comfort than did the original material.25
Fixed appliances require more pain medication than aligners. Analgesic consumption closely mirrored the pattern of discomfort at rest during the first week of treatment. There was an increase in analgesic consumption during the first 24–48 hours, followed by a gradual return to baseline levels. Pain medication intake and pain levels during the first week have been previously associated.11 This association was not evident at subsequent adjustments, perhaps because patients were in less pain and did not require pain control.
CONCLUSIONS
-
•
Traditional fixed appliances produced significantly more discomfort than did aligners.
-
•
During the first 3 days after bonding, there was significantly more discomfort when chewing than when at rest for patients treated with traditional appliances.
-
•
Patients treated with aligners and traditional appliances reported significantly less discomfort at subsequent adjustments than after the initial bonding or appliance delivery.
-
•
Consumption of analgesics closely mirrored the levels of discomfort reported by patients during the first week of treatment.
ACKNOWLEDGMENTS
This research was partially funded by the Robert E. Gaylord Endowed Chair in Orthodontics and by Align Technology.
REFERENCES
- 1.Scheurer PA, Firestone AR, Burgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18:349–357. doi: 10.1093/ejo/18.4.349. [DOI] [PubMed] [Google Scholar]
- 2.Kvam E, Gjerdet NR, Bondevik O. Traumatic ulcers and pain during orthodontic treatment. Community Dent Oral Epidemiol. 1987;15:104–107. doi: 10.1111/j.1600-0528.1987.tb00493.x. [DOI] [PubMed] [Google Scholar]
- 3.Lew KK. Attitudes and perceptions of adults towards orthodontic treatment in an Asian community. Community Dent Oral Epidemiol. 1993;21:31–35. doi: 10.1111/j.1600-0528.1993.tb00715.x. [DOI] [PubMed] [Google Scholar]
- 4.Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod. 1985;12:179–188. doi: 10.1179/bjo.12.4.179. [DOI] [PubMed] [Google Scholar]
- 5.Sergl HG, Klages U, Zentner A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofac Orthop. 1998;114:684–691. doi: 10.1016/s0889-5406(98)70201-x. [DOI] [PubMed] [Google Scholar]
- 6.Krukemeyer AM, Arruda AO, Inglehart MR. Pain and orthodontic treatment. Angle Orthod. 2009;79:1175–1181. doi: 10.2319/121308-632R.1. [DOI] [PubMed] [Google Scholar]
- 7.Haynes S. Discontinuation of orthodontic treatment relative to patient age. J Dent. 1974;2:138–142. doi: 10.1016/0300-5712(74)90041-4. [DOI] [PubMed] [Google Scholar]
- 8.Jones M, Chan C. The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofacial Orthop. 1992;102:373–381. doi: 10.1016/0889-5406(92)70054-e. [DOI] [PubMed] [Google Scholar]
- 9.Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989;96:47–53. doi: 10.1016/0889-5406(89)90228-x. [DOI] [PubMed] [Google Scholar]
- 10.Young AN, Taylor RW, Taylor SE, Linnebur SA, Buschang PH. Evaluation of preemptive valdecoxib therapy on initial archwire placement discomfort in adults. Angle Orthod. 2006;76:251–259. doi: 10.1043/0003-3219(2006)076[0251:EOPVTO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Miller KB, McGorray SP, Womack R, et al. A comparison of treatment impacts between Invisalign aligner and fixed appliance therapy during the first week of treatment. Am J Orthod Dentofacial Orthop. 2007. 131:302 e1–e9. [DOI] [PubMed]
- 12.Shalish M, Cooper-Kazaz R, Ivgi I, et al. Adult patients' adjustability to orthodontic appliances. Part I: a comparison between labial, lingual, and Invisalign. Eur J Orthod. 2012;34:724–730. doi: 10.1093/ejo/cjr086. [DOI] [PubMed] [Google Scholar]
- 13.Fujiyama K, Honjo T, Suzuki M, Matsuoka S, Deguchi T. Analysis of pain level in cases treated with Invisalign aligner: comparison with fixed edgewise appliance therapy. Prog Orthod. 2014;15:64. doi: 10.1186/s40510-014-0064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bergius M, Kiliaridis S, Berggren U. Pain in orthodontics. A review and discussion of the literature. J Orofac Orthop. 2000;61:125–137. doi: 10.1007/BF01300354. [DOI] [PubMed] [Google Scholar]
- 15.Krishnan V, Davidovitch Z. Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop. 2006. 129:469 e1–e32. [DOI] [PubMed]
- 16.Dray A. Inflammatory mediators of pain. Br J Anaesth. 1995;75:125–131. doi: 10.1093/bja/75.2.125. [DOI] [PubMed] [Google Scholar]
- 17.Opree A, Kress M. Involvement of the proinflammatory cytokines tumor necrosis factor-alpha, IL-1 beta, and IL-6 but not IL-8 in the development of heat hyperalgesia: effects on heat-evoked calcitonin gene-related peptide release from rat skin. J Neurosci. 2000;20:6289–6293. doi: 10.1523/JNEUROSCI.20-16-06289.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grieve WG, III, Johnson GK, Moore RN, Reinhardt RA, DuBois LM, Prostaglandin (PGE) and interleukin-1 beta (IL-1 beta) levels in gingival crevicular fluid during human orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 1994;105:369–374. doi: 10.1016/s0889-5406(94)70131-8. [DOI] [PubMed] [Google Scholar]
- 19.Fernandes LM, Ogaard B, Skoglund L. Pain and discomfort experienced after placement of a conventional or a superelastic NiTi aligning archwire. A randomized clinical trial. J Orofac Orthop. 1998;59:331–339. doi: 10.1007/BF01299769. [DOI] [PubMed] [Google Scholar]
- 20.Nakano H, Satoh K, Norris R, et al. Mechanical properties of several nickel-titanium alloy wires in three-point bending tests. Am J Orthod Dentofacial Orthop. 1999;115:390–395. doi: 10.1016/s0889-5406(99)70257-x. [DOI] [PubMed] [Google Scholar]
- 21.Stewart FN, Kerr WJ, Taylor PJ. Appliance wear: the patient's point of view. Eur J Orthod. 1997;19:377–382. doi: 10.1093/ejo/19.4.377. [DOI] [PubMed] [Google Scholar]
- 22.Thilander B. Tissue Reactions in Orthodontics, in Orthodontics: Current Principles and Techniques. Philadelphia: Mosby;; 2011. pp. 253–286. [Google Scholar]
- 23.Soltis JE, Nakfoor PR, Bowman DC. Changes in ability of patients to differentiate intensity of forces applied to maxillary central incisors during orthodontic treatment. J Dent Res. 1971;50:590–596. doi: 10.1177/00220345710500031101. [DOI] [PubMed] [Google Scholar]
- 24.Nicolay OF, Davidovitch Z, Shanfeld JL, Alley K. Substance P immunoreactivity in periodontal tissues during orthodontic tooth movement. Bone Miner. 1990;11:19–29. doi: 10.1016/0169-6009(90)90012-5. [DOI] [PubMed] [Google Scholar]
- 25.SmartTrack Aligner Material. Available from: http://provider.invisalign.com/smarttrack Accessed on 10 May 2016.