Abstract
Objective:
To evaluate the skeletal, dental, and soft tissue effects of the Forsus Fatigue Resistant Device (FRD) used with miniscrew anchorage and compare them with those of the conventional Forsus FRD.
Materials and Methods:
This study was carried out on 38 patients. These patients were randomly allocated into three groups. The 14 patients in group 1 (aged 12.76 ± 1.0 years) were treated with the FRD appliance. In group 2, the 15 patients (aged 12.52 ± 1.12 years) received treatment with FRD using miniscrew anchorage, and the 9 patients in group 3 (aged 12.82 ± 0.9 years) received no treatment as a control group. Linear and angular measurements were made on lateral cephalograms before and immediately after Forsus treatment. Data were analyzed statistically using paired t-, ANOVA, and Tukey tests.
Results:
Class I molar relationship and overjet correction were achieved in both treatment groups. Although mandibular growth was statistically nonsignificant, there was a significant headgear effect on the maxilla. Mandibular incisor proclination, maxillary incisor retroclination, and distalization of maxillary molars were significant in both treatment groups. However, no significant differences were found between the treatment groups.
Conclusions:
Class II correction was mainly dentoalveolar in both treatment groups. Use of miniscrews with Forsus did not enhance mandibular forward growth nor prevent labial tipping of the mandibular incisors.
Keywords: Forsus, Miniscrew, Fixed functional appliance, Class II malocclusion
INTRODUCTION
Class II malocclusion is one of the most commonly seen problems in daily orthodontic practice. McNamara1 reported that mandibular retrusion is the main etiological factor in Class II malocclusion rather than maxillary protrusion. Therefore, several types of functional appliances have been advocated for the treatment of Class II malocclusion with mandibular retrusion, such as fixed functional devices that have the advantage of not depending upon patient cooperation. Moreover, they can be used simultaneously with orthodontic brackets.
The Forsus appliance produces continuous orthopedic forces that can be controlled by varying the pushrod size to the desired force level as well as by adding crimped stops, depending on the clinical application.2 However, dentoalveolar side effects may limit skeletal correction.3 Several studies have recently focused on minimizing these effects.4–7
Only two available studies6,7 have shown the effects of using FRD with miniscrew anchorage. They reported that Class II correction was totally dentoalveolar, and unfortunately, miniscrew anchorage did not enhance mandibular forward growth. Both studies used different radiographic assessment methods. Moreover, there was controversy regarding some findings of these two studies, such as the exact effect on the maxilla, and only one study reported soft tissue changes. A recent systematic review8 concluded that the use of skeletally anchored functional appliances can prevent mandibular incisor proclination; however, this finding should be interpreted with caution because of variability in the means of skeletal anchorage used in different studies with the FFA including miniscrews and miniplates, as well as variation in methods of indirect anchorage including thick steel wire, wire ligature, and elastic ligature. Pooling of results from different studies with such variation could be inappropriate. Moreover, a mean reduction of −1.43° may not make enough clinical difference to encourage clinicians to use two miniscrews or miniplates with the FFA. The effect of using orthodontic miniscrews with the FRD were difficult to comprehend and, therefore, additional investigation is needed to analyze the skeletal, dental, and soft tissues changes associated with miniscrew-anchored FRD.
Specific Objective or Hypothesis
The aim of the present study was to evaluate the skeletal, dental, and soft tissue effects of the miniscrew-anchored FRD and compare it with conventional FRD. The null hypothesis was that there would be no difference in skeletal, dental, or soft tissue changes among treatment and control groups.
MATERIALS AND METHODS
Trial Design
This study was a single-center, randomized clinical trial. No changes occurred during the trial.
Participants, Eligibility Criteria, and Settings
The study design was approved by the Research Ethics Committee of Faculty of Dentistry, Tanta University, Egypt.
Patients were included according to following criteria:
Skeletal Class II malocclusion with mandibular retrognathia (ANB > 4.5°, SNB < 76°)
Normal vertical growth pattern (SN-MP angle in 25°–35° range)
Minimal or no crowding in the mandibular arch (0–5 mm), based on Little's irregularity index9
No extracted or missing permanent teeth (third molars excluded)
Undergoing circumpubertal phase of skeletal development (CVMI 2–4)
No medical history or systemic disease that could affect normal growth of the body or jaws.
The cervical vertebrae maturation index (CVMI) was used for patient selection. CVMI 2, 3, and 4 stages, which correspond to the circumpubertal growth period, were defined by lateral cephalometric radiographs.10 Written informed consent and assent forms were obtained from the parents and children after we explained the treatment procedures in detail for all participants.
Sample Size Calculation
Sample size calculation was based on the ability to detect a clinically meaningful difference in mandibular length of 2 mm (± 1.5 mm), with an alpha error of 0.05 and a test power of 80%. The calculation was carried out using software G* Power (Universität Düsseldorf, Germany). The recommended sample size was 12 patients in each group. To compensate for a possible dropout rate of 20% during the study period, 15 patients were included in each group.
Randomization
Patients were randomly assigned using a computer-generated random list. The patients were randomly allocated into three groups using sequentially numbered, opaque, sealed envelopes.
Group 1 (12.76 ± 1.0 years): nine females and six males were treated with a conventional FRD. Group 2 (12.52 ± 1.12 years): 10 females and 5 males were treated with a miniscrew-anchored FRD. Group 3 (12.82 ± 0.9 years): untreated nine females and six males were used as a control group to compensate for the effects of growth on the treatment groups, as it was not possible to determine whether the skeletal changes were due to growth or treatment. The total observation period was about 6 months on average, and transition from one CVM stage to another generally takes at least 1 year. Thus, this observation period would not have affected the treatment plan for those patients. All control patients started their treatment immediately after termination of the observation period.
Interventions
All patients were treated with a nonextraction approach using 0.022-inch-slot MBT brackets (Ormco Corp, Orange, Calif) bonded to both arches. Mandibular canines were bonded with Damon 3MX brackets (Ormco), which have a square vertical slot (0.018 × 0.018-inch). Leveling was done until stainless steel archwires (0.019 × 0.025-inch) could be engaged passively in both arches. Both archwires were cinched back, teeth were figure-8 ligated, and anchorage was reinforced with a maxillary transpalatal arch to prevent buccal tipping of maxillary molars. In group 1, the FRD was selected and inserted following the manufacturer's instructions, that is, into the headgear tube of the maxillary molars; the pushrod was hooked onto the mandibular archwire distal to the canine brackets.
For group 2 patients, miniscrews (1.6 × 10 mm; MCT Tech, South Korea) were inserted bilaterally between the mandibular canine and first premolar roots at the level of the mucogingival junction. A segment of 0.016 × 0.016-inch stainless steel wire was shaped and inserted between the vertical slot of the mandibular canine bracket and the hole in the miniscrew neck to establish indirect anchorage (Figure 1).
Figure 1.
Forsus used with miniscrews.
Patients were observed every 4 weeks. During each follow-up visit, if the spring module was compressed more than 2.5 mm above the stop on the push rod, reactivation was performed by attaching a crimp onto the push rod to provide 1.5 mm of activation. The FRD and miniscrews were removed when an edge-to-edge incisor relationship had been achieved with a Class I or overcorrected Class I canine and molar relationship. This was achieved in a mean time of 6.06 ± 0.76 months in group 1 and 6.42 ± 1.04 months in group 2 (Figures 2 and 3). The fixed appliances were left in place using light Class II elastics to stabilize the results and avoid relapse. To settle the occlusion after FRD removal, light intermaxillary box elastics were used, and the mandibular archwire was replaced with a lighter, more flexible wire.
Figure 2.
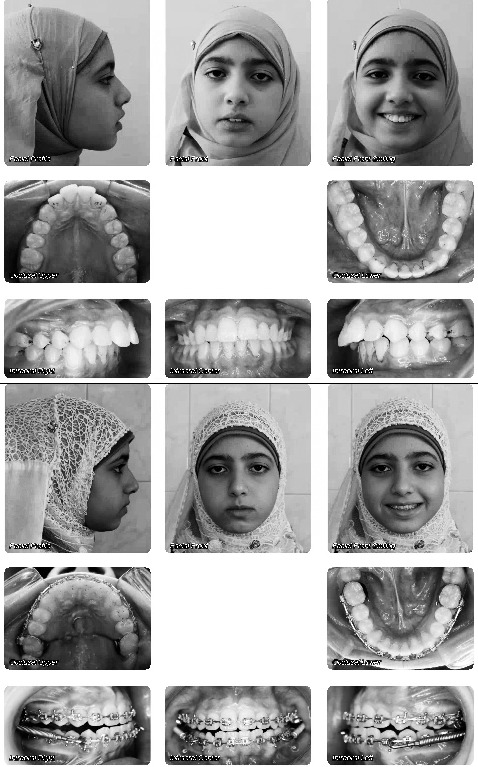
Intraoral and extraoral photos of a group 1 (Forsus) patient before and after treatment.
Figure 3.
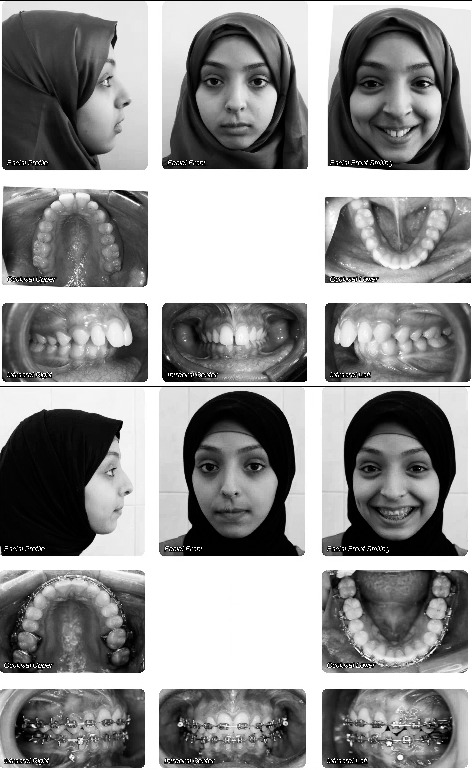
Intraoral and extraoral photos of a group 2 (Forsus with miniscrew) patient before and after treatment.
Outcomes
The main outcomes of the study were the skeletal and dentoalveolar changes. The secondary outcomes were the soft tissue changes after treatment.
Cephalometric Analysis
Lateral cephalometric radiographs were taken by a single technician on the same radiographic machine immediately before insertion (T1) and after removal of the FRD and miniscrews (T2) to compare treatment outcomes. All landmarks were digitized and measurements were recorded using Dolphin Imaging software version 11.8 ( Dolphin Imaging, Chatsworth, Calif).
Reliability
To minimize any method error, all measurements were performed twice by the same investigator. The radiographs were remeasured after 1 month and the readings compared. A tolerance limit of 0.5 mm and 0.5° was established for the difference between the first and second observations of linear and angular measurements, respectively. If the limit was exceeded, a new tracing and measurement were made and the aberrant one discarded.
Blinding
Blinding of both patient and operator to the intervention was impossible. However, the investigator who analyzed the cephalograms was blinded regarding the origin of the films and the group to which the individual subjects belonged. All data were labeled with numbers and sent to the statistician, who was also blinded to the patients' groups. For the control group, it was impossible to be completely blinded as there were no appliances in the patients' mouths, but blinding was achieved regarding the time point of the cephalograms.
Statistical Analysis
Statistical analysis was performed with SPSS Version 21.0 (SPSS Inc, Chicago, Ill). The Shapiro-Wilk test showed that the data were normally distributed (P > .05), thus, parametric tests were used. Paired t-tests were performed to detect changes within each group. ANOVA was used for comparing mean changes among the three groups. If a statistically significant difference was found (P < .05), a Tukey multiple-comparison test was used to identify which groups were different.
RESULTS
Participants Flow and Patient Attrition
A CONSORT diagram is shown in Figure 4, demonstrating all patients recruited into the study.
Figure 4.
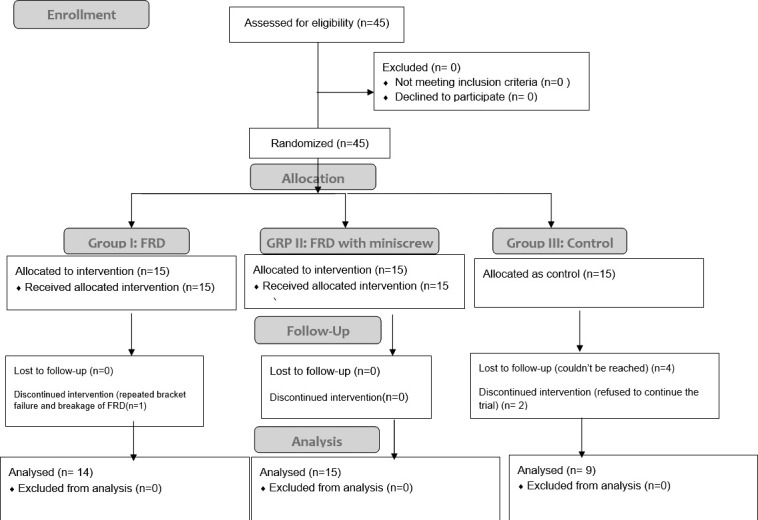
CONSORT diagram showing the flow of subjects in the study.
Baseline Data
Groups were well matched regarding patient ages and treatment duration as there were no significant differences among all groups (P > .05; Table 1). There were no significant differences in male-to-female ratios in the treatment and control groups (P > .05), which excluded any potential effects of gender on craniofacial size and changes. There were no statistically significant differences among the three groups at T1 for any analyzed cephalometric parameters (Table 2). Skeletal, dental, and soft tissue changes between T1 and T2 for all groups are shown in Table 3. Comparisons among all groups are shown in Table 4.
Table 1.
Comparison of the Mean Age and Treatment Duration Among Three Study Groups*
| Group 1 (n = 14) |
Group 2 (n = 15) |
Group 3 (n = 9) |
ANOVA |
|||||
| Variables |
Mean |
SD |
Mean |
SD |
Mean |
SD |
F |
P |
| Age | 12.76 | 1.00 | 12.53 | 1.12 | 12.82 | 0.90 | 0.29 | .750 |
| Duration | 6.06 | 0.76 | 6.42 | 1.04 | 6.07 | 0.25 | 0.88 | .420 |
P > .05 (Nonsignificant).
Table 2.
Pretreatment Mean Values of All Parameters in Each Group and Significance Values of the Differences Among the Three Groups*
| Measurements |
Group 1 (Forsus) |
Group 2 (Forsus with Miniscrews) |
Group 3 (Control) |
ANOVA | |||
| Mean |
SD |
Mean |
SD |
Mean |
SD |
Sig |
|
| SNA (°) | 81.471 | 4.047 | 83.400 | 4.805 | 83.156 | 4.024 | .460 |
| SNB (°) | 74.064 | 3.167 | 75.200 | 5.140 | 75.222 | 2.978 | .704 |
| ANB (°) | 7.429 | 2.801 | 8.213 | 1.701 | 7.922 | 1.762 | .628 |
| MP-SN (°) | 29.550 | 5.888 | 27.527 | 6.415 | 31.978 | 4.561 | .200 |
| LFH (ANS-Me) (mm) | 63.279 | 5.344 | 62.573 | 4.107 | 59.267 | 5.062 | .144 |
| TFH (N-Me) (mm) | 108.764 | 7.191 | 107.567 | 5.643 | 103.300 | 5.921 | .132 |
| Co-Gn (mm) | 106.686 | 6.589 | 105.787 | 5.137 | 103.211 | 6.792 | .410 |
| LFH/TFH (%) | 54.507 | 1.708 | 54.980 | 1.986 | 53.789 | 1.573 | .302 |
| Wits appraisal (mm) | 7.082 | 2.157 | 6.923 | 1.258 | 7.211 | 1.650 | .646 |
| U1-NA (mm) | 4.690 | 2.681 | 4.517 | 1.561 | 5.533 | 2.121 | .054 |
| U1-NA (°) | 20.936 | 6.617 | 20.040 | 5.727 | 26.533 | 5.319 | .058 |
| L1-NB (mm) | 7.529 | 3.003 | 6.127 | 1.665 | 5.522 | 2.103 | .112 |
| L1-NB (°) | 32.114 | 5.372 | 30.527 | 4.169 | 29.878 | 7.550 | .598 |
| Overjet (mm) | 6.543 | 1.266 | 7.980 | 1.292 | 10.033 | 2.993 | .672 |
| Overbite (mm) | 4.210 | 1.031 | 4.400 | 1.829 | 5.733 | 1.708 | .051 |
| U6-PT vertical (mm) | 16.093 | 3.625 | 16.847 | 3.603 | 14.222 | 5.119 | .075 |
| Lower lip to E-plane (mm) | 3.036 | 2.542 | 2.807 | 3.265 | 2.200 | 2.845 | .307 |
| Upper lip to E-plane (mm) | 0.221 | 2.566 | 1.160 | 2.488 | 1.378 | 2.877 | .796 |
| Nasolabial angle (Col-Sn-UL) (°) | 108.000 | 11.539 | 113.733 | 10.610 | 109.178 | 7.628 | .506 |
P > .05 (Nonsignificant).
Table 3.
Changes in Cephalometric Skeletal, Dental, and Soft Tissue Measurements in All Groups
| Measurements |
Treatment Time |
Group 1 (Forsus) |
Group 2 (Forsus With Miniscrews) |
Group 3 (Control) |
||||||
| Mean |
SD |
Sig |
Mean |
SD |
Sig |
Mean |
SD |
Sig |
||
| SNA (°) | T1 | 81.47 | 4.04 | .005* | 83.4 | 4.8 | <.001** | 83.15 | 4.02 | .148 |
| T2 | 80.95 | 3.97 | 82.6 | 4.62 | 83.72 | 3.91 | ||||
| T2−T1 | −0.51 | 0.57 | −0.79 | 0.504 | 0.56 | 1.06 | ||||
| SNB (°) | T1 | 74.06 | 3.16 | .242 | 75.2 | 5.14 | .277 | 75.22 | 2.97 | .145 |
| T2 | 74.22 | 3.17 | 75.37 | 5.01 | 75.8 | 2.68 | ||||
| T2−T1 | 0.15 | 0.48 | 0.17 | 0.593 | 0.57 | 1.07 | ||||
| ANB (°) | T1 | 7.42 | 2.8 | <.001** | 8.21 | 1.7 | <.001** | 7.92 | 1.76 | 1 |
| T2 | 6.72 | 3.12 | 7.24 | 1.49 | 7.92 | 1.58 | ||||
| T2−T1 | −0.7 | 0.62 | −0.97 | 0.647 | 0 | 0.68 | ||||
| MP-SN (°) | T1 | 29.55 | 5.88 | .219 | 27.52 | 6.41 | .067 | 31.97 | 4.56 | .067 |
| T2 | 30.07 | 5.99 | 28.2 | 6.09 | 31.07 | 4.94 | ||||
| T2−T1 | 0.52 | 1.51 | 0.67 | 1.311 | −0.9 | 1.27 | ||||
| LFH (ANS-Me) (mm) | T1 | 63.27 | 5.34 | .013* | 62.57 | 4.1 | <.001** | 59.26 | 5.06 | .149 |
| T2 | 64.38 | 4.95 | 64.02 | 4.06 | 59.88 | 4.14 | ||||
| T2−T1 | 1.1 | 1.43 | 1.45 | 1.173 | 0.62 | 1.16 | ||||
| AFH (N-Me) (mm) | T1 | 108.76 | 7.19 | .057 | 107.56 | 5.64 | <.001** | 103.3 | 5.92 | .021* |
| T2 | 110.06 | 6.23 | 109.86 | 5.39 | 105.34 | 4.47 | ||||
| T2−T1 | 1.3 | 2.32 | 2.29 | 1.729 | 2.04 | 2.13 | ||||
| Co-Gn (mm) | T1 | 106.68 | 6.58 | .417 | 105.78 | 5.13 | .1 | 103.21 | 6.79 | .019* |
| T2 | 107.3 | 5.29 | 106.81 | 5.3 | 105.84 | 5.83 | ||||
| T2−T1 | 0.61 | 2.74 | 1.02 | 2.258 | 2.63 | 2.7 | ||||
| LFH/AFH (%) | T1 | 54.5 | 1.7 | .269 | 54.98 | 1.98 | .779 | 53.78 | 1.57 | .155 |
| T2 | 54.83 | 1.85 | 55.05 | 2.2 | 53.43 | 1.7 | ||||
| T2−T1 | 0.32 | 1.06 | 0.07 | 0.991 | −0.35 | 0.67 | ||||
| Wits appraisal (mm) | T1 | 7.08 | 2.15 | <.001** | 6.92 | 1.25 | <.001** | 7.21 | 1.65 | .102 |
| T2 | 3.74 | 2.57 | 2.27 | 1.14 | 6.1 | 1.96 | ||||
| T2−T1 | −3.33 | 2.23 | −4.64 | 1.554 | −1.11 | 1.8 | ||||
| U1-NA (mm) | T1 | 4.69 | 2.68 | .014* | 4.51 | 1.56 | .006* | 5.53 | 2.12 | .164 |
| T2 | 2.71 | 2.01 | 1.95 | 1.69 | 6.01 | 2.21 | ||||
| T2−T1 | −1.98 | 2.06 | −2.56 | 1.368 | 0.47 | 0.93 | ||||
| U1-NA (°) | T1 | 20.93 | 6.61 | <.001** | 20.04 | 5.72 | <.001** | 26.53 | 5.31 | .062 |
| T2 | 14.05 | 5.92 | 11.94 | 4.95 | 28.36 | 3.94 | ||||
| T2−T1 | −6.88 | 4.15 | −8.1 | 4.47 | 1.83 | 2.53 | ||||
| L1-NB (mm) | T1 | 7.529 | 3 | <.001** | 6.12 | 1.66 | <.001** | 5.52 | 2.1 | .101 |
| T2 | 9.02 | 3.18 | 7.42 | 1.62 | 5.83 | 2.25 | ||||
| T2−T1 | 1.5 | 0.97 | 1.29 | 1.069 | 0.31 | 0.5 | ||||
| L1-NB (°) | T1 | 32.11 | 5.37 | <.001** | 30.52 | 4.16 | .001** | 29.87 | 7.55 | .919 |
| T2 | 38.11 | 7.52 | 35.22 | 4.06 | 29.95 | 8 | ||||
| T2−T1 | 6 | 2.96 | 4.7 | 4.047 | 0.07 | 2.22 | ||||
| Overjet (mm) | T1 | 6.54 | 1.26 | <.001** | 7.98 | 1.29 | <.001** | 10.03 | 2.99 | .126 |
| T2 | 2.06 | 1.17 | 2.42 | 0.7 | 10.56 | 2.54 | ||||
| T2−T1 | −4.47 | 1.59 | −5.55 | 1.453 | -0.53 | 0.93 | ||||
| Overbite (mm) | T1 | 4.21 | 1.03 | <.001** | 4.4 | 1.82 | <.001** | 5.73 | 1.7 | .963 |
| T2 | 2.41 | 0.94 | 1.69 | 0.97 | 5.71 | 2.36 | ||||
| T2−T1 | −1.8 | 0.95 | −2.7 | 1.985 | −0.02 | 1.39 | ||||
| U6-PT Vertical (mm) | T1 | 16.09 | 3.62 | <.001** | 16.84 | 3.6 | <.001** | 14.22 | 5.11 | .185 |
| T2 | 14.1 | 3.87 | 14.9 | 4.19 | 14.88 | 5.06 | ||||
| T2−T1 | −1.98 | 1.44 | −1.94 | 1.348 | 0.66 | 1.38 | ||||
| Lower lip to E-Plane (mm) | T1 | 3.03 | 2.54 | .968 | 2.8 | 3.26 | .688 | 2.2 | 2.84 | .443 |
| T2 | 3.01 | 2.96 | 2.58 | 3.06 | 2.8 | 3.94 | ||||
| T2−T1 | −0.02 | 1.99 | −0.22 | 2.142 | 0.6 | 2.23 | ||||
| Upper lip to E-Plane (mm) | T1 | 0.22 | 2.56 | .012* | 1.16 | 2.48 | <.001** | 1.37 | 2.87 | .222 |
| T2 | −0.74 | 2.64 | −0.84 | 2.13 | 2.31 | 2.61 | ||||
| T2−T1 | −0.96 | 1.23 | −2 | 1.45 | 0.93 | 2.11 | ||||
| Nasolabial angle (Col-Sn-UL) (°) | T1 | 108 | 11.53 | .021* | 113.73 | 10.61 | <.001** | 109.17 | 7.62 | .863 |
| T2 | 113.68 | 8.84 | 124.38 | 7.99 | 109.47 | 6.76 | ||||
| T2−T1 | 5.68 | 8.12 | 10.653 | 8.84 | 0.28 | 4.85 | ||||
> .05 (nonsignificant).
P ≤ .05 (significant).
P ≤ .001 (highly significant).
Table 4.
Comparison of Cephalometric, Skeletal, Dental, and Soft Tissue Mean Changes Among Groups 1, 2, and 3
| Measurements |
ANOVA |
Tukey's Post Hoc Tests |
||||||
| F |
P |
Gps 1 & 2 |
Gps 1 & 3 |
Gps 2 & 3 |
||||
| Diff |
P |
Diff |
P |
Diff |
P |
|||
| SNA (°) | 11.284 | <.001** | −0.279 | .532 | 1.081 | .002* | 1.360 | <.001** |
| SNB (°) | 1.195 | .315 | 0.016 | .998 | 0.421 | .348 | 0.404 | .366 |
| ANB (°) | 6.428 | .004* | −0.273 | .500 | .700 | .042* | .973 | .003* |
| MP-SN (°) | 4.101 | .025* | 0.152 | .953 | −1.421 | .054 | −1.573 | .028* |
| LFH (ANS-Me) (mm) | 0.441 | .647 | 0.423 | .659 | 0.050 | .996 | −0.373 | .777 |
| N-Me (mm) | 1.475 | .243 | 0.800 | .544 | 1.460 | .226 | 0.660 | .723 |
| Co-Gn (mm) | 4.278 | .022* | 1.550 | .206 | 2.957 | .018* | 1.407 | .357 |
| LFH/TFH (%) | 1.111 | .341 | −0.110 | .950 | −0.594 | .332 | −0.484 | .467 |
| Wits appraisal (mm) | 20.080 | <.001** | 0.366 | .836 | 4.341 | <.001** | 3.975 | <.001** |
| U1-NA (mm) | 17.892 | <.001** | −0.960 | .210 | 2.777 | <.001** | 3.737 | <.001** |
| U1-NA (°) | 19.226 | <.001** | −1.214 | .693 | 8.719 | <.001** | 9.933 | <.001** |
| L1-NB (mm) | 4.801 | .014* | −0.207 | .823 | −1.188 | .014* | −.982 | .045* |
| L1-NB (°) | 9.213 | .001** | −1.300 | .546 | −5.922 | .001** | −4.622 | .006* |
| Overjet (mm) | 55.688 | <.001** | −1.075 | .115 | 5.011 | <.001** | 6.086 | <.001** |
| Overbite (mm) | 8.551 | .001** | −0.971 | .221 | 1.713 | .035* | 2.684 | .001** |
| U6-PT vertical (mm) | 12.238 | <.001** | 0.046 | .996 | 2.652 | <.001** | 2.606 | <.001** |
| Lower lip to E-plane (mm) | 0.443 | .645 | −0.205 | .963 | 0.621 | .771 | 0.827 | .625 |
| Upper lip to E-plane (mm) | 9.784 | <.001** | −1.036 | .194 | 1.897 | .021* | 2.933 | <.001** |
| Nasolabial angle (Col-Sn-UL) | 5.019 | .012* | 4.968 | .216 | −5.397 | .253 | −10.36 | .009* |
> .05 (nonsignificant).
P ≤ .05 (significant).
P ≤ .001 (highly significant).
Skeletal Measurements
In the anteroposterior dimension, there was a significant decrease in the SNA angle (0.51° ± 0.57°, P < .05; 0.79 ± 0.5, P ≤ .001) and a highly significant decrease in the ANB angle (0.70° ± 0.62°, P ≤ .001; 0.97° ± 0.65°, P ≤ .001) for groups 1 and 2, respectively. Although there was an increase in SNB angle and mandibular length, this was not statistically significant (P > .05). Vertically, there was a significant increase in lower facial height (Group 1: −1.11 mm ± 1.43 mm, P < .05; Group 2: −1.45 mm ± 1.17 mm, P ≤ .001). There were no statistically significant differences for any skeletal measurements between the treatment groups (P > .05; Table 4).
Dental Measurements
In groups 1 and 2, the maxillary incisors showed significant retrusion as evident from changes in U1-NA angle (6.89° ± 4.16°, P ≤ .001; 2.56° ± 1.36°, P ≤ .001, respectively). The mandibular incisors exhibited highly significant proclination; L1-NB angle (−6.0° ± 2.93°, P ≤ .001; −4.70° ± 4.04°, P ≤ .001) in groups 1 and 2, respectively. There was a significant reduction in overjet (4.48 ± 1.59 mm, P < .05; 5.53 ± 1.45, P < .05) and overbite (1.8 ± 0.95, P < .05; 2.7 ± 1.98, P < .05). The maxillary molars exhibited highly significant distal movement; U6-PT mm (1.98 ± 1.44, P ≤ .001; 1.94 ± 1.34, P ≤ .001). For all dental measurements, there were no significant differences (P > .05) between the treatment groups (Table 4).
Soft Tissue Measurements
There was significant retraction of the upper lip in both treatment groups as demonstrated by upper lip to E-plane (P < .05). The lower lip did not show any significant change in relation to the E-plane (P > .05).
Harms
There was no looseness or mobility in the miniscrews of group 2; however, inflammation of gingival tissues near the miniscrews was reported in three cases.
DISCUSSION
Treatment was performed during the circumpubertal phases of skeletal development, which has been reported to be an optimal time for stimulation of mandibular growth.11 Indirect anchorage was adopted for the present study to avoid direct orthopedic load on the miniscrews, which—originally designed to withstand routine orthodontic forces—could increase the risk of of miniscrew failure.12
Skeletal Changes
Both treatment groups showed a significant decrease in the SNA angle that could be attributed to posteriorly directed forces acting on the maxilla (headgear effect) that may effectively restrict maxillary forward growth. This result is in agreement with previous studies that have reported similar findings.3,13,14 However, other studies reported that FRD had no significant effect on maxillary growth. Oztoprak et al.15 and Aslan et al.6 explained this controversy by variance in treatment age, different treatment mechanics, or treatment duration.
Mandibular size in both treatment groups exhibited no significant increases, indicating that the FRD did not stimulate forward mandibular growth. This finding was in accordance with those of other studies which reported little or no effect on mandibular growth.3,6,13,15,16 In contrast, several studies concluded that significant mandibular growth could be achieved by the use of this appliance.4,13,17,18 This difference might be attributed to treatment duration (6 months), which may be not enough for mandibular growth to take place.6,13,14,19 Both treatment groups exhibited a significant reduction in ANB, which can be attributed to a reduction in SNA. Similar findings of a decrease in ANB were reported in several studies.7,15,20
Although the treatment groups exhibited posterior mandibular rotation, this change was not statistically significant. Similarly, Aslan et al.6 reported nonsignificant changes in the mandibular plane angle in both treatment groups. On the contrary, several studies reported significant mandibular rotation with the skeletally anchored FRD appliance.5,17,21 This contradiction might be related to differences in the sample groups, different treatment durations, or different treatment mechanics. There was a significant increase in lower facial height in both treatment groups. Similar findings have been reported.5,17,18 This may be attributed to downward and forward forces from the appliance which resulted in a new mandibular position that enhanced vertical condylar growth and, subsequently, increased lower facial height.17 Contradictory to the findings of the present study, Oztoprak et al.15 found no significant change in facial height, postulating that this was due to their study sample being in the postpeak growth period. Similarly, other researchers found no significant changes in facial height.22,23
Dental Changes
The distally directed force of the FRD transmitted through the heavy archwire to the maxillary incisors in both treatment groups could have caused their significant retrusion.17 This finding is in accordance with those of previous Forsus studies.6,17,24,25 Liu et al.26 reported that upper anterior tooth retrusion would result in backward movement of A point with a consequent decrease in SNA°.
Both treatment groups showed significant mandibular incisor protrusion which is still one of the major disadvantages of FRD that could result in early correction of the overjet and, consequently, limit skeletal correction.17 Contradictory to other studies,6,7 which reported that the miniscrew-anchored FRD could limit mandibular incisor protrusion, we observed no significant difference between treatment groups; hence, the use of miniscrew anchorage did not minimize this unfavorable outcome. This difference may be attributed to the size of the wire segment used for connecting the miniscrew with the mandibular canine bracket. In the present study, a segment of 0.016 × 0.016-inch stainless steel was used because it was the largest wire size that could be inserted in the vertical slot (0.018 × 0.018-inch) of the mandibular canine bracket. Elkordy et al.7 used a 0.019 × 0.025-inch stainless steel wire segment connected to the miniscrew and bonded to the labial surface of the mandibular canines. Whereas Aslan et al.6 established indirect anchorage by using an 0.018 × 0.025-inch stainless steel wire between the vertical slot of the mandibular canine bracket and the miniscrew slot.
Significant reduction in overjet and overbite was evident in both treatment groups, which was related to the maxillary incisor retroclination and mandibular incisor proclination, suggesting total dentoalveolar effects of the appliance. This finding is in agreement with other studies.6,7,25 In accordance with other studies,3,7,18 the maxillary molar exhibited significant distal movement in both treatment groups, which can be attributed to the distal vector of force of the appliance.
Comparison of mean differences between groups 1 and 2 revealed no significant differences in any dental parameters, indicating that miniscrews did not prevent or even limit the dentoalveolar effects of the FRD. This finding is in disagreement with that of other studies reporting that the miniscrew-anchored Forsus limited mandibular incisor proclination6,7 and increase maxillary molar distal movement.7
Soft Tissue Changes
Significant upper lip retrusion was observed in both treatment groups as measured by upper lip to the E-plane. This was in accordance with previous studies5,13,15,17 and can be attributed to the heavy distal forces acting on the maxillary arch and subsequent retrusion of the maxillary incisors.17 In contrast to some studies4–6,27 that reported significant lower lip protrusion, we found nonsignificant lower lip protrusion. This was in accordance with other studies,15,17 which reported similar findings. Turkkahraman et al.17 suggested that the variation among studies might be due to differences in soft tissue reference lines and measurements. Possible contributors to the lower lip position are mandibular position, which did not show any significant forward movement, and the maxillary incisors, which showed significant retrusion. The nasolabial angle was significantly increased in both treatment groups. This may be attributed to retrusion of the maxillary incisors, allowing the upper lip to move posteriorly.27 These treatment outcomes confirm those reported by other studies15,28 that found similar soft tissue changes.
Limitations
The results of the present study should be interpreted with caution. The small sample size together with patient attrition could have affected the accuracy of the results. Moreover, the treatment duration of FRD (6 months) may be not enough for mandibular growth to take place and may be considered as a drawback of the FRD.
Generalizability
Despite the limited sample size, the results of this study could be applied to similar patients with Class II malocclusion.
CONCLUSIONS
-
•
The Forsus FRD effectively corrected Class II malocclusion in both the conventional and miniscrew-anchored treatment groups, mainly through dentoalveolar changes. Due to the short treatment duration of the FRD (6 months), which may be not enough for mandibular growth to take place, a longer use of the appliance might have resulted in more skeletal effects.
-
•
The use of miniscrews as a means of anchorage with FRD did not enhance forward mandibular growth or limit proclination of the lower incisors.
REFERENCES
- 1.McNamara JA., Jr Components of Class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51:177–202. doi: 10.1043/0003-3219(1981)051<0177:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.El-Sheikh MM, Godfrey K, Manosudprasit M, Viwattanatipa N. Force-deflection characteristics of the fatigue-resistant device spring: an in vitro study. World J Orthod. 2007;8:30–36. [PubMed] [Google Scholar]
- 3.Jones G, Buschang PH, Kim KB, Oliver DR. Class II non-extraction patients treated with the Forsus fatigue resistant device versus intermaxillary elastics. Angle Orthod. 2008;78:332–338. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 4.Celikoglu M, Buyuk SK, Ekizer A, Unal T. Treatment effects of skeletally anchored Forsus FRD EZ and Herbst appliances: a retrospective clinical study. Angle Orthod. 2016;86:306–314. doi: 10.2319/040315-225.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unal T, Celikoglu M, Candirli C. Evaluation of the effects of skeletal anchoraged Forsus FRD using miniplates inserted on mandibular symphysis: a new approach for the treatment of Class II malocclusion. Angle Orthod. 2015;85:413–419. doi: 10.2319/051314-345.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aslan BI, Kucukkaraca E, Turkoz C, Dincer M. Treatment effects of the Forsus fatigue resistant device used with miniscrew anchorage. Angle Orthod. 2014;84:76–87. doi: 10.2319/032613-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elkordy SA, Abouelezz AM, Fayed MM, Attia KH, Ishaq RA, Mostafa YA. Three-dimensional effects of the mini-implant-anchored Forsus fatigue resistant device: a randomized controlled trial. Angle Orthod. 2016;86:292–305. doi: 10.2319/012515-55.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elkordy SA, Aboelnaga AA, Salah Fayed MM, AboulFotouh MH, Abouelezz AM. Can the use of skeletal anchors in conjunction with fixed functional appliances promote skeletal changes? A systematic review and meta-analysis. Eur J Orthod. 2016;38:532–545. doi: 10.1093/ejo/cjv081. [DOI] [PubMed] [Google Scholar]
- 9.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 10.Baccetti T, Franchi L, McNamara JA. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 11.Singh S, Singh M, Saini A, Misra V, Sharma VP, Singh GK. Timing of myofunctional appliance therapy. J Clin Pediatr Dent. 2010;35:233–240. doi: 10.17796/jcpd.35.2.9572h13218806871. [DOI] [PubMed] [Google Scholar]
- 12.Luzi C, Verna C, Melsen B. Guidelines for success in placement of orthodontic mini-implants. J Clin Orthod. 2009;43:39–44. [PubMed] [Google Scholar]
- 13.Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E, Baccetti T. Effectiveness of comprehensive fixed appliance treatment used with the Forsus fatigue resistant device in Class II patients. Angle Orthod. 2011;81:678–683. doi: 10.2319/102710-629.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giuntini V, Vangelisti A, Masucci C, Defraia E, McNamara JA, Jr, Franchi L. Treatment effects produced by the Twin-block appliance vs the Forsus fatigue resistant device in growing Class II patients. Angle Orthod. 2015;85:784–789. doi: 10.2319/090514-624.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oztoprak MO, Nalbantgil D, Uyanlar A, Arun T. A cephalometric comparative study of Class II correction with Sabbagh universal spring (SUS(2)) and Forsus FRD appliances. Eur J Dent. 2012;6:302–310. [PMC free article] [PubMed] [Google Scholar]
- 16.Cacciatore G, Ghislanzoni LT, Alvetro L, Giuntini V, Franchi L. Treatment and posttreatment effects induced by the Forsus appliance: a controlled clinical study. Angle Orthod. 2014;84:1010–1017. doi: 10.2319/112613-867.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turkkahraman H, Eliacik SK, Findik Y. Effects of miniplate anchored and conventional Forsus fatigue resistant devices in the treatment of Class II malocclusion. Angle Orthod. 2016;86:1026–1032. doi: 10.2319/122515-887.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karacay S, Akin E, Olmez H, Gurton AU, Sagdic D. Forsus nitinol flat spring and Jasper Jumper corrections of Class II Division 1 malocclusions. Angle Orthod. 2006;76:666–672. doi: 10.1043/0003-3219(2006)076[0666:FNFSAJ]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Phan KL, Bendeus M, Hagg U, Hansen K, Rabie AB. Comparison of the headgear activator and Herbst appliance—effects and post-treatment changes. Eur J Orthod. 2006;28:594–604. doi: 10.1093/ejo/cjl052. [DOI] [PubMed] [Google Scholar]
- 20.Cacciatore G, Alvetro L, Defraia E, Ghislanzoni LT, Franchi L. Active-treatment effects of the Forsus fatigue resistant device during comprehensive Class II correction in growing patients. Korean J Orthod. 2014;44:136–142. doi: 10.4041/kjod.2014.44.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Celikoglu M, Unal T, Bayram M, Candirli C. Treatment of a skeletal Class II malocclusion using fixed functional appliance with miniplate anchorage. Eur J Dent. 2014;8:276–280. doi: 10.4103/1305-7456.130637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pancherz H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod. 1982;82:104–113. doi: 10.1016/0002-9416(82)90489-4. [DOI] [PubMed] [Google Scholar]
- 23.Covell DA, Jr, Trammell DW, Boero RP, West R. A cephalometric study of Class II Division 1 malocclusions treated with the Jasper Jumper appliance. Angle Orthod. 1999;69:311–320. doi: 10.1043/0003-3219(1999)069<0311:ACSOCI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Heinig N, Goz G. Clinical application and effects of the Forsus spring. a study of a new Herbst hybrid. J Orofac Orthop. 2001;62:436–450. doi: 10.1007/s00056-001-0053-6. [DOI] [PubMed] [Google Scholar]
- 25.Gunay EA, Arun T, Nalbantgil D. Evaluation of the immediate dentofacial changes in late adolescent patients treated with the Forsus FRD. Eur J Dent. 2011;5:423–432. [PMC free article] [PubMed] [Google Scholar]
- 26.Liu YH, Ding WH, Liu J, Li Q. Comparison of the differences in cephalometric parameters after active orthodontic treatment applying mini-screw implants or transpalatal arches in adult patients with bialveolar dental protrusion. J Oral Rehabil. 2009;36:687–695. doi: 10.1111/j.1365-2842.2009.01976.x. [DOI] [PubMed] [Google Scholar]
- 27.Upadhyay M, Yadav S, Nagaraj K, Uribe F, Nanda R. Mini-implants vs fixed functional appliances for treatment of young adult Class II female patients. Angle Orthod. 2012;82:294–303. doi: 10.2319/042811-302.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuroda S, Yamada K, Deguchi T, Kyung HM, Takano-Yamamoto T. Class II malocclusion treated with miniscrew anchorage: comparison with traditional orthodontic mechanics outcomes. Am J Orthod Dentofacial Orthop. 2009;135:302–309. doi: 10.1016/j.ajodo.2007.03.038. [DOI] [PubMed] [Google Scholar]



