Abstract
Background
Female urethral stricture (FUS) represents a sporadic condition. There is a lack of data and standardized guidelines on diagnostics and therapeutics. Several surgical techniques have been described for FUS urethroplasty, among which the flap-based or graft-based ones are most reported. Buccal mucosa graft (BMG) represents the gold standard for male urethroplasty, and this can theoretically be applied also to FUS treatment.
Objective
To describe and present preliminary results of a novel minimally invasive technique for buccal mucosa dorsal graft (mini-dorsal BMG) urethroplasty for the treatment of FUS.
Design, setting, and participants
This is a retrospective study on buccal mucosa dorsal graft urethroplasty for the treatment of FUS.
Surgical procedure
Every patient was placed in lithotomic position. Two stiches were placed at 10 and 2 o’clock positions to facilitate the dorsal median urethrotomy. The margins of the incised dorsal urethra at the 12 o’clock position are then dissected from the periurethral tissue. This dissection results in an elliptical raw area between the edges of the urethra over the periurethral tissue. The harvested BMG was fixed with several quilting sutures, using 5-0 and 4-0 absorbable sutures, to cover the raw area. The margins of the graft were sutured to the edges of the incised urethra.
Measurements
A chart review was performed.
Results and limitations
Thirteen patients underwent the mini-dorsal-BMG technique. The median preoperative uroflow was 5.6 (3–13) ml/s, and the median postoperative value was 23.4 (14–58) ml/s.
Conclusions
The mini-dorsal-BMG technique for the treatment of FUS gives good results with low complication rates. Other series and long-term follow-up are necessary to confirm the reproducibility of this technique.
Patient summary
We present the technical aspects and the promising preliminary results of a novel surgical technique for the treatment of female urethral stricture by using the buccal mucosa to correct this invalidating disease.
Keywords: Urethral, Stricture, Female, Urethroplasty, Buccal mucosa
1. Introduction
Female urethral stricture (FUS) is considered an uncommon disease causing 4–18% of female bladder outlet obstructions, which are estimated to cause up to 8% of the lower urinary tract infections in females [1]. The FUS prevalence is probably underestimated because of the lack of data in literature. The main treatment for FUS is often based on periodic urethral dilations end/or self-clean catheterization showing a large variety in terms of intervals between dilations ranging between 1 and 39 mo [2], [3]. Various techniques for female urethral reconstruction have been described, despite the small sample size and the short follow-up. Ventral, dorsal, and dorsolateral surgical approaches have been shown using flaps and free grafts [4], [5], [6], [7], [8], [9], [10]. Many ventral approach used the Martius flap to avoid urethral fistula [4], [11], [12]. The use of buccal mucosa graft (BMG) in reconstructive urethral surgery represents the gold standard for the treatment of nonobstructive urethral strictures in men [13], [14], [15], [16], [17], [18]. Dorsal female urethral reconstruction is based on the dissection of the distal urethra from the surrounding tissue through a suprameatal incision, which is then freed dorsally. The major risk of this approach is the potential damaging of the sphincter or the clitoral bodies [18]. To prevent these issues, we used the technique described by Osman and Chapple [19] for the dorsal-inlay BMG by means of a transurethral approach, without dissection of the dorsal urethra from the surrounding tissues. We aimed to present the novel surgical technique of minimally invasive buccal mucosa dorsal graft (“mini-dorsal BMG”) and preliminary results.
2. Patients and methods
This is a retrospective review of female patients with distal urethral stricture who underwent the mini-dorsal-BMG technique at a single genital reconstructive center between in 2017 and 2019 by a single surgeon expert in male and female urethroplasty (E.B.). All patients provided informed consent before surgery. The inclusion criterion was the diagnosis of FUS. Exclusion criteria were midproximal FUS, complete obstructive urethral stricture, and concomitant urethral pathologies. The diagnostic workup was based on medical history, physical examination, ultrasonography with full bladder and postvoiding residue measurement, urine culture, uroflowmetry, and voiding urethrography. The diagnostic suspect of a urethral stenosis was made in case the passage of 14 Ch catheter was difficult or not possible; this diameter has been considered a criterion for the definition of stenosis in different studies, and for this reason, it was used as a threshold in our experience [3], [19]. Once the diagnostic suspect was made, a urethroscopy was normally performed soon before surgery.
Descriptive statistics are presented as frequencies and relative proportions for categorical variables, or medians/means with corresponding ranges for continuous variables.
2.1. Surgical technique
Prophylactic broad-spectrum antibiotic amoxicillin + clavulanic acid was started preoperatively 1 h before induction of anesthesia and continued for 3 d postoperatively. Patients were normally intubated through the nose in order to free the oral cavity and provide the surgeon with more space. However, oral mucosa graft could be harvested even in the presence of orotracheal intubation, but, in this case, the tube should be reinforced to avoid inadvertent compression by the mouth retractor. A guide wire was inserted in the tight urethra, supported by a plastic cone as an introducer (Fig. 1). After placing stay sutures at 10 and 2 o’clock positions, the dorsal urethra was incised on the midline by an 11-blade scalpel (Fig. 2). The margins of the incised dorsal urethra were dissected from the periurethral tissues by sharp dissection with the help of a Gorget, without lifting the edges of the incised urethra (Fig. 3). This dissection results in a grossly elliptical raw area between the edges of the urethra over the periurethral tissues. The graft was attached with quilting sutures (4-0 and 5-0 absorbable sutures), aiming to prevent the formation of hematomas, thus facilitating its uptake and suturing to the urethral margins (Fig. 4). A 16-Fr urethral Foley catheter was inserted once the stricture was opened. For the buccal mucosa harvest, a Kilner-Doughty mouth retractor was used to expose the donor site, and the Stensen’s duct was identified and marked in proximity of the second molar. Three stay sutures were placed along the edge of the mouth in order to keep the oral mucosa adequately stretched. A 10 ml solution of 2% lidocaine with adrenaline (1:200 000) was injected along the edges of the graft to promote hemostasis and to assist in the dissection of the mucosa. The inner mucosal surface of the cheek was cleaned. Once all submucosa tissue was carefully excised with iris scissors, the graft was tailored according to the site, length, and stricture characteristics. While removing all the submucosa tissue, it was essential to avoid excessive graft thinning, as in these cases the healing process tends to contract. The graft was harvested in an elliptical shape, to facilitate the covering of the donor site. The donor site was carefully closed with interrupted or running 4-0 absorbable sutures. The Foley catheter was left in place for 3 wk. Patients were generally discharged on the 3rd postoperative day. Uroflowmetry, urine cultures, and physical examination also by testing the passage of 16 Ch catheter were repeated every 4 mo in the 1 st year and annually thereafter. Successful reconstruction was defined as normal voiding without the need for any postoperative procedure, including dilation.
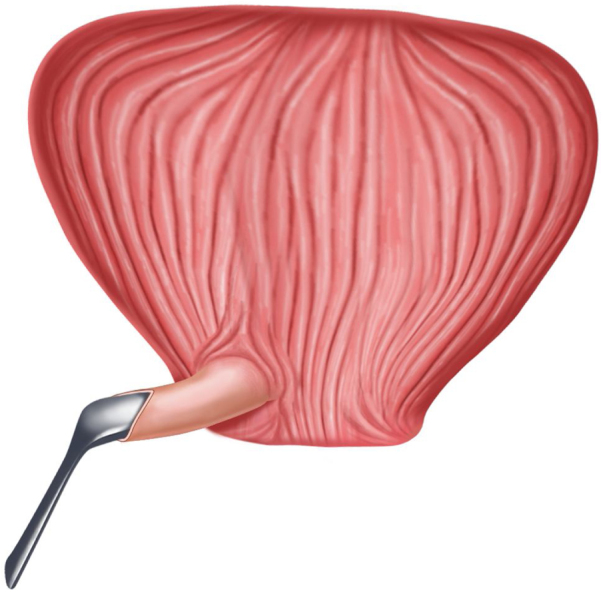
Fig. 1.

Insertion of a guide wire into the tight urethra.
Fig. 2.

Dorsal transurethral incision of the urethra.
Fig. 3.
Creation of an elliptical raw area over the periurethral tissues with the help of a Gorget.
Fig. 4.
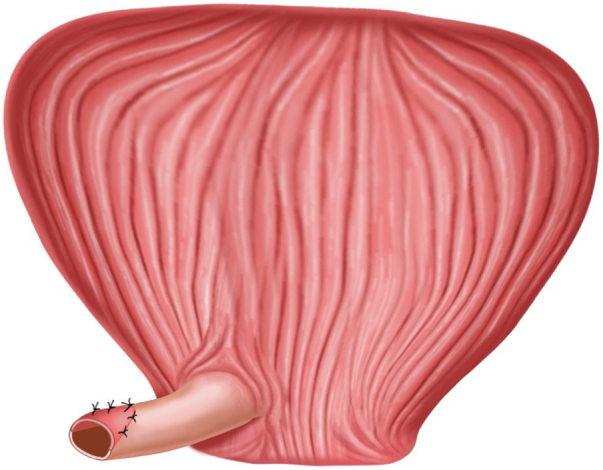
Using 4/0 polyglactin as a quilted suture to secure the graft to the underlying periurethral tissues.
3. Results
A total of 13 patients underwent urethroplasty with the mini-dorsal-BMG technique between 2017 and 2019. The median age at the time of surgery was 56 yr (min-max range: 29–69 yr). All patients, before surgery, had various and significant lower urinary tract symptoms, bladder outlet obstruction, recurrent cystitis, and burning micturition (Table 1). All patients had undergone multiple and periodic transurethral dilations before surgery at different time points before the procedure. Three patients underwent previous urethroplasty. The cause of stenosis was unknown in the majority of patients (84.6%), but it was related to traumatic catheterization in one patient and to the sequelae of radiotherapy in another. The median graft dimensions were 2.25 cm (min-max range: 1.5–3 cm) and 1.75 cm (min-max range: 1–2 cm). The mean operative time was 60 min (min-max range: 45–80 min). No complications appeared soon after surgery, and no further interventions were required. After catheter removal, cystourethrography was never performed because of a very low chance of a urethral fistula formation, avoiding radiation exposure especially to young patients. In all patients, significant improvement was observed in postoperative urinary flow in absence of pain as well as in sexual function, with the exception of a single sexually inactive patient because of a previous gynecologic surgery. The median preoperative uroflowmetry was 5.6 (3–13) ml/s, and the median postoperative value was 23.4 (14–58) ml/s. The median follow-up was 11 mo (min-max range: 7–18 mo), with resolution of the preoperative symptoms in the majority of cases. All the postoperative symptoms were conservatively managed with success. No recurrences have been observed until the latest follow-up.
Table 1.
Preoperative symptoms and patients characteristics.
| Symptom | Preoperative n (%) | Last follow-up n (%) |
|---|---|---|
| Dysuria | 13 (100) | 0 |
| Painful micturition | 13 (100) | 0 |
| Urinary frequency | 8 (62) | 0 |
| Urgency | 1 (8) | 2 (15) |
| Recurrent symptomatic cystitis | 12 (92) | 0 |
| Urinary tract infections with fever | 4 (31) | 0 |
| Acute urinary retention | 3 (23) | 0 |
| Incomplete emptinga | 6 (43) | 0 |
| Urinary incontinence | 2 (15) | 0 |
| Dyspareunia | 2 (17)b | 0 |
Measured by ultrasonography.
Twelve patients were considered at denominator because one patient was not sexually active preoperatively.
4. Discussion
FUS is a challenging disease considering the lack of standard definitions and treatment options. The real prevalence of FUS is unknown, but it is normally considered a rare disease. However, this is probably underestimated because of the absence of large series and because it is generally treated with chronic urethral dilations [2], [3]. There are few series in literature that report surgical or endoscopic treatment of FUS [9]. The use of BMG in male urethral reconstruction for the treatment of nonobstructive urethral stricture is considered the gold standard. Barbagli et al [13] introduced the dorsal grafting procedure through a dorsal urethrotomy approach. Simultaneously, Morey and McAninch [14] reported their results obtained with the ventral graft technique. Asopa et al [20], thereafter, described the dorsal graft urethroplasty using a ventral urethrotomy approach. In female patients, the use of buccal mucosa has been described in few series with dorsal BMG or ventral BMG [4], [5], [6], [7], [8], [9], [10], [11], [12], [21]. For the ventral BMG, all articles described the use of a Martius flap to cover urethroplasty and avoid urethral fistula. The dorsal approach were described in literature with complete dissection of the urethra from the surrounding tissues [6], [7], [9], [10], [21]. We use the concept described by Asopa et al [20] considering the anatomy of the female urethral sphincter. According to recent anatomical publications [22], the tridimensional aspect of the female urethral sphincter is peculiar and characterized by a U geometry (Fig. 5), which surrounds the distal lateral walls of the vagina. The aim of our novel technique is to preserve as much urethra/periurethral tissues as possible, avoiding a wide dissection of the urethra but creating the space for the BMG by the dorsal incision through transurethral lumen. The dorsal dissection of the distal urethra protects against the damage of the internal urinary sphincter that surrounds the urethra only in the medium-proximal segment [22]. There are few important technical aspects that should be highlighted. First, the respect of the urethral integrity protects from urinary incontinence and urethral damage, maintaining the urethral axial integrity as much as possible and reducing the ischemic damage. Second, the buccal mucosa guarantees effective resolution of the stricture with minimal morbidity. Third, the dorsal approach for the distal strictures protects from urethral fistulas.
Fig. 5.
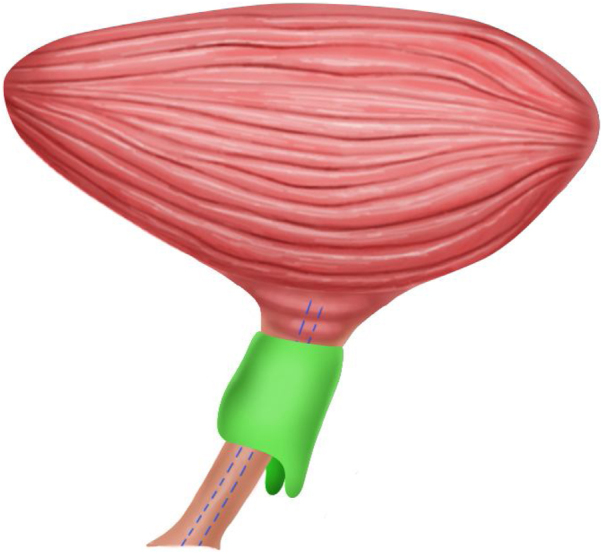
Shape of the female urethral sphincter.
The dorsal approach provides better mechanical support to any graft/flap while also having a well-vascularized tissue [6], [7], [10], [19]. The possibility to damage the sphincter in the mini-dorsal BMG is minimized by the small dorsal incision that does not reach the urethral sphincter area [22]. Thus, we use the mini-dorsal-BMG technique only for distal FUS. The possible damage of the clitoral bodies is improbable because of the distance of the neurovascular bundles from the distal urethra [23], [24]. The vast majority of the published studies assessing reconstructive techniques are small descriptive series with different definitions and diagnostic criteria as well as outcome measures, limiting data comparisons. The overall success rate reported in literature was 94% at a mean follow-up of 14.8 mo [9]. The majority of these studies continue to support the established evidence that urethroplasty in these patients is potentially very successful with a low incidence of complications. However, this should be done by dedicated surgeons in high-volume centers.
This study has some limitations. First, this is a retrospective study; second, patients were not all surgery naïve; and third, the number of cases is relatively small.
5. Conclusions
The mini-dorsal BMG is a novel surgical technique for the treatment of FUS. We report the first series of patients treated with this technique showing good peri- and postoperative results. This technique should be executed by dedicated surgeons in high-volume centers for the treatment of urethral disease. Long follow-up and comparative prospective series are needed to support our findings.
Author contributions: Federico Germinale had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Berdondini, Margara.
Acquisition of data: Collura, Germinale, Kurti, Gianluca Muto.
Analysis and interpretation of data: Tosco.
Drafting of the manuscript: Tosco, Berdondini.
Critical revision of the manuscript for important intellectual content: Giovanni Muto.
Statistical analysis: Tosco, Collura, Germinale.
Obtaining funding: None.
Administrative, technical, or material support: None.
Supervision: Giovanni Muto, Berdondini, Giacobbe.
Other: None.
Financial disclosures: Federico Germinale certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Associate Editor: Guillaume Ploussard
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.euros.2020.12.001.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Hoag N., Ju Chee J. Surgical management of female urethral strictures. Transl Androl Urol. 2017;6(Suppl 2):S76–80. doi: 10.21037/tau.2017.01.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith A.L., Ferlise V.J., Rovner E.S. Female urethral strictures: successful management with long-term clean intermittent catheterization after urethral dilatation. BJU Int. 2006;98:96–99. doi: 10.1111/j.1464-410X.2006.06206.x. [DOI] [PubMed] [Google Scholar]
- 3.Osman N.I., Mangera A., Chapple C.R. A systematic review of surgical techniques used in the treatment of female urethral stricture. Eur Urol. 2013;64:965–973. doi: 10.1016/j.eururo.2013.07.038. [DOI] [PubMed] [Google Scholar]
- 4.Flisser AJ, Blaivas JG. Outcome of urethral reconstructive surgery in a series of 74 women. J Urol. 2003;169:2246–2249. doi: 10.1097/01.ju.0000061763.88247.16. [DOI] [PubMed] [Google Scholar]
- 5.Montorsi F., Salonia A., Centemero A. Vestibular flap urethroplasty for strictures of the female urethra. Impact on symptoms and flow patterns. Urol Int. 2002;69:12–16. doi: 10.1159/000064353. [DOI] [PubMed] [Google Scholar]
- 6.Tsivian A, Sidi AA. Dorsal graft urethroplasty for female urethral stricture. J Urol. 2006;176:611–613. doi: 10.1016/j.juro.2006.03.055. [DOI] [PubMed] [Google Scholar]
- 7.Migliari R., Leone P., Berdondini E., De Angelis M., Barbagli G., Palminteri E. Dorsal buccal mucosa graft urethroplasty for female urethral strictures. J Urol. 2006;176(4 Pt 1):1473–1476. doi: 10.1016/j.juro.2006.06.043. [DOI] [PubMed] [Google Scholar]
- 8.Simonato A., Varca V., Esposito M., Carmignani G. Vaginal flap urethroplasty for wide female stricture disease. J Urol. 2010;184:1381. doi: 10.1016/j.juro.2010.06.042. [DOI] [PubMed] [Google Scholar]
- 9.Rehder P., Glodny B., Pichler R., Exeli L., Kerschbaumer A., Mitterberger M.J. Dorsal urethroplasty with labia minora skin graft for female urethral strictures. BJU Int. 2010;106:1211–1214. doi: 10.1111/j.1464-410X.2010.09240.x. [DOI] [PubMed] [Google Scholar]
- 10.Goel A., Paul S., Dalela D., Sankhwar P., Sankhwar S.N., Singh V. Dorsal onlay buccal mucosal graft urethroplasty in female urethral stricture disease: a single-center experience. Int Urogynecol J. 2014;25:525–530. doi: 10.1007/s00192-013-2249-x. [DOI] [PubMed] [Google Scholar]
- 11.Mukhtar B.M.B., Spilotros M., Malde S., Greenwell T.J. Ventral-onlay buccal mucosa graft substitution urethroplasty for urethral stricture in women. BJU Int. 2017;120:710–716. doi: 10.1111/bju.13970. [DOI] [PubMed] [Google Scholar]
- 12.Berglund R.K., Vasavada S., Angermeier K., Rackley R. Buccal mucosa graft urethroplasty for recurrent stricture of female urethra. Urology. 2006;67:1069–1071. doi: 10.1016/j.urology.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 13.Barbagli G., Selli C., Tosto A., Palminteri E. Dorsal free graft urethroplasty. J Urol. 1996;155:123–126. [PubMed] [Google Scholar]
- 14.Morey AF, McAninch JW. When and how to use buccal mucosal grafts in adult bulbar urethroplasty. Urology. 1996;48:194–198. doi: 10.1016/S0090-4295(96)00154-9. [DOI] [PubMed] [Google Scholar]
- 15.Raber M., Naspro R., Scapaticci E. Dorsal onlay graft urethroplasty using penile skin or buccal mucosa for repair of bulbar urethral stricture: results of a prospective single center study. Eur Urol. 2005;48:1013–1017. doi: 10.1016/j.eururo.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Palminteri E., Manzoni G., Berdondini E. Combined dorsal plus ventral double buccal mucosa graft in bulbar urethral reconstruction. Eur Urol. 2008;53:81–90. doi: 10.1016/j.eururo.2007.05.033. [DOI] [PubMed] [Google Scholar]
- 17.Barbagli G., Kulkarni S.B., Fossati N. Long-term followup and deterioration rate of anterior substitution urethroplasty. J Urol. 2014;192:808–813. doi: 10.1016/j.juro.2014.02.038. [DOI] [PubMed] [Google Scholar]
- 18.Horiguchi A. Substitution urethroplasty using oral mucosa graft for male anterior urethral stricture disease: current topics and reviews. Int J Urol. 2017;24:493–503. doi: 10.1111/iju.13356. [DOI] [PubMed] [Google Scholar]
- 19.Osman NI, Chapple CR. Contemporary surgical management of female urethral stricture disease. Curr Opin Urol. 2015;25:341–345. doi: 10.1097/MOU.0000000000000186. [DOI] [PubMed] [Google Scholar]
- 20.Asopa H.S., Garg M., Singhal G.G., Singh L., Asopa J., Nischal A. Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. Urology. 2001;58:657–659. doi: 10.1016/s0090-4295(01)01377-2. [DOI] [PubMed] [Google Scholar]
- 21.Sharma G.K., Pandey A., Bansal H. Dorsal onlay lingual mucosal graft urethroplasty for urethral strictures in women. BJU Int. 2010;105:1309–1312. doi: 10.1111/j.1464-410X.2009.08951.x. [DOI] [PubMed] [Google Scholar]
- 22.Wallner C., Dabhoiwala N.F., DeRuiter M.C., Lamers W.H. The anatomical components of urinary continence. Eur Urol. 2009;55:932–943. doi: 10.1016/j.eururo.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 23.O’Connell HE, DeLancey JO. Clitoral anatomy in nulliparous, healthy, premenopausal volunteers using unenhanced magnetic resonance imaging. J Urol. 2005;173:2060–2063. doi: 10.1097/01.ju.0000158446.21396.c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yavagal S., de Farias T.F., Medina C.A., Takacs P. Normal vulvovaginal, perineal, and pelvic anatomy with reconstructive considerations. Semin Plast Surg. 2011;25:121–129. doi: 10.1055/s-0031-1281481. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


