Abstract
Background
Retzius-sparing robotic-assisted radical prostatectomy (RS-RARP) has improved urinary function compared with standard robotic-assisted radical prostatectomy (S-RARP). As RS-RARP spares the dorsal vascular complex, pelvic fascia, and anterior abdominal fascia, it may also lower the incidence of “neglected” postprostatectomy sequelae such as penile shortening, Peyronie’s disease, and inguinal hernias.
Objective
To determine whether there are patient-perceived differences in penile shortening, Peyronie’s disease, and inguinal hernia rates among men undergoing RS-RARP versus S-RARP.
Design, setting, and participants
Researchers uninvolved in clinical care and blinded to surgical approach surveyed 60 RS-RARP versus 57 S-RARP men with validated patient-reported items to assess penile shortening, Peyronie’s disease, and inguinal hernia sequelae following surgery.
Intervention
RS-RARP versus S-RARP.
Outcome measurements and statistical analysis
Univariate differences between the two cohorts were analyzed using Student t test. Logistic regression was used to analyze variables associated with postoperative penile shortening. Cox proportional hazards models were used to assess the risk of developing Peyronie’s disease and inguinal hernia postoperatively.
Results and limitations
RS-RARP was associated with less patient-reported penile shortening (41.7% vs 64.9%, p = 0.012), Peyronie’s disease (0% vs 8.7%, p = 0.020), and inguinal hernia (0.0% vs 13.0%, p = 0.004). In adjusted analyses, RS-RARP (odds ratio [OR] 0.24, 95% confidence interval [CI] 0.09–0.63, p = 0.004) was associated with lower odds of penile shortening, while a higher body mass index was associated with increased odds of penile shortening (OR 1.13, 95% CI 1.01–1.26, p = 0.037). RS-RARP was not associated with a decreased risk of Peyronie’s disease on Cox proportion hazard model; however, these models are limited due to a limited number of events in our cohort. Limitations include retrospective design, patient-reported outcomes, and small cohorts.
Conclusions
RS-RARP is associated with less patient-reported penile shortening and may decrease the risk of Peyronie’s disease and postoperative inguinal hernia development. These new findings add to research, showing improved urinary continence and quality of life following RS-RARP; however, a prospective study is needed to validate these findings.
Patient summary
Retzius-sparing robotic-assisted radical prostatectomy (RS-RARP) is an evolving surgical technique for prostate cancer treatment, which has shown improved postoperative urinary control compared with the standard technique, likely due to preservation of natural pelvic anatomy. Our findings suggest that the preservation of normal pelvic anatomy during RS-RARP may also reduce the risk of postprostatectomy penile shortening, Peyronie’s disease, and inguinal hernia.
Keywords: Robotic-assisted surgery, Retzius-sparing prostatectomy, Sexual function, Peyronie’s disease, Inguinal hernia
Take Home Message
Retzius-sparing robotic-assisted radical prostatectomy (RS-RARP) is an evolving surgical technique for prostate cancer treatment that has shown improved postoperative urinary control compared with the standard technique, likely due to the preservation of natural pelvic anatomy. Our findings suggest that the preservation of normal pelvic anatomy during RS-RARP may also reduce the risk of postprostatectomy penile shortening, Peyronie’s disease, and inguinal hernia.
1. Introduction
Most research on robotic-assisted radical prostatectomy (RARP) adverse events beyond the perioperative period focuses on the recovery of urinary and sexual function. While these are significant life-altering patient-centered outcomes, other “hidden” risks, including adverse events such as penile shortening, Peyronie’s disease, and inguinal hernia impact survivorship significantly. A 3-mo post–radical prostatectomy (RP) survey of men at a high-volume academic referral center indicated that no patient remembered counseling about the risks of penile shortening and Peyronie’s disease [1].
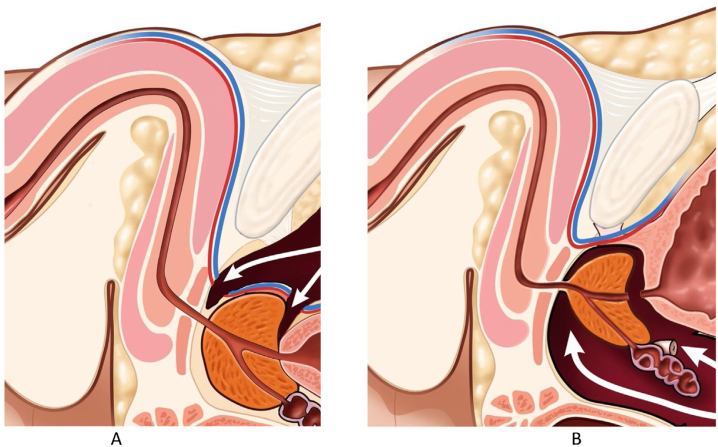
Standard RARP (S-RARP) and retropubic RP includes dissecting the bladder from the anterior abdominal wall, followed by division of the dorsal vascular complex (Fig. 1A). Physiologically, division of arterial tributaries to the penis is thought to result in penile shortening [2]. Similarly, preserving accessory pudendal arteries during RP improves recovery of erectile function [3]. Peyronie’s disease, an inflammatory process leading to penile deformity (precluding intercourse, in extreme cases), has a much higher incidence after RP (15.9%) than the general population [4]. Finally, adverse events such as inguinal hernia occur in 7.5–13.7% of men after RP [5].
Fig. 1.
Sagittal pelvic view during (A) standard RARP and (B) Retzius-sparing RARP. Disruption of the dorsal vascular complex at both the bladder neck and the prostate apex during standard RARP contributes to penile shortening and Peyronie’s disease. The dorsal vascular complex is left intact during Retzius-sparing RARP (Fig. 1B). RARP = robotic-assisted radical prostatectomy.
In 2010, Galfano et al [6] described Retzius-sparing RARP (RS-RARP), a technique that preserves pelvic fascial anatomy as well as the dorsal vascular complex (Fig. 1B) in contrast to S-RARP. In addition, by virtue of the entire RS-RARP dissection being below the endopelvic fascia, accessory pudendal arteries are completely preserved. Finally, there is no separation of the bladder from the anterior abdominal wall during RS-RARP. The transversalis fascia and other supporting abdominal fasciae are left intact, thus likely preventing inguinal hernia sequelae.
Our RS-RARP comparative series is the third study, published from a US medical center, to demonstrate an 80% reduction in the risk of urinary incontinence at 12 mo and is also the first to demonstrate improved overall patient quality of life following surgery [7]. Given our finding of improved overall quality of life, we sought to determine whether RS-RARP has additional anatomic advantages through a patient survey of neglected and potentially hidden RP adverse events that impact survivorship negatively.
2. Patients and methods
Our study design and surgical technique have been described previously [7]: 140 consecutive RARPs were performed by a single surgeon (K.J.K.), with the first 70 undergoing S-RARP and the last 70 undergoing RS-RARP following the surgeon’s change in approach. For the present study, outcome assessors not involved in clinical care and blinded to surgical approach surveyed 60 RS-RARP versus 57 S-RARP procedures using validated items for penile shortening and Peyronie’s disease from prior studies [2], [8]. The item for penile shortening was developed from in-depth interviews with men undergoing RP, and face validity was assured by having an investigator accompany the patient to ensure accurate interpretation while they completed the items [2]. The item queries: “Is your penile length subjectively shorter compared to before prostatectomy (yes vs no)?” The item for Peyronie’s disease was validated through blinded clinical examination with 100% sensitivity and 99.4% specificity, and asks the following question: “Have you noticed any new penile curvature or deformity in a flaccid or erect state following prostatectomy?” [8]. Finally, we conducted a medical history and asked: “Have you been diagnosed or treated for an inguinal hernia following prostatectomy?”
The mean follow-up was 14 mo for RS-RARP and 55 mo for S-RARP. Baseline preoperative characteristics (age and baseline Expanded Prostate Cancer Index for Clinical Practice [EPIC-CP] score), perioperative variables (nerve-sparing procedure, estimated blood loss, and console time), postoperative outcomes (complications, and need for adjuvant radiation or hormonal therapy), as well as patient-reported outcomes were compared utilizing Student t test, with p < 0.05 considered significant. A nerve-sparing procedure was defined as bilateral intrafascial nerve sparing, combined interfascial and intrafascial nerve sparing, and bilateral interfascial nerve sparing in any patient. Non–nerve sparing was defined as unilateral nerve sparing or bilateral extrafascial nerve sparing.
Multivariable logistic regression was utilized to analyze variables associated with penile shortening following surgery. Cox proportional hazards models were utilized to assess association of RS-RARP with postoperative Peyronie’s disease and inguinal hernia. Variables for the model were included if p < 0.2 on univariate analysis.
3. Results
Table 1 summarizes patient baseline characteristics and perioperative outcomes. RS-RARP had significantly more men with higher Gleason grade groups (p = 0.038) and lower mean estimated blood loss (187 vs 325 ml, p < 0.001) than S-RARP.
Table 1.
Baseline characteristics and perioperative results of RS-RARP and S-RARP cohorts
| RS-RARP (N = 60) |
S-RARP (N = 57) |
p value | |
|---|---|---|---|
| Age (yr), mean | 61.4 | 61.1 | 0.811 |
| BMI (kg/m2), mean | 29.5 | 27.9 | 0.066 |
| Charlson Comorbidity Index, mean | 4.0 | 3.9 | 0.510 |
| Preoperative PSA, mean | 7.9 | 8.8 | 0.470 |
| Preoperative Gleason group, n (%) | |||
| 1 | 9 (15.0) | 19 (33.3) | 0.038 |
| 2 | 21 (35.0) | 22 (38.6) | |
| 3 | 15 (25.0) | 10 (17.5) | |
| 4 | 13 (21.7) | 3 (5.3) | |
| 5 | 2 (3.3) | 3 (5.3) | |
| Preop potency, n (%) | 60 (100.0) | 60 (100.0) | 1.000 |
| Preop EPIC-CP sexual function score, mean | 3.0 | 2.5 | 0.391 |
| Any nerve sparing, n (%) | 51 (85.0) | 48 (84.2) | 0.907 |
| EBL (ml), mean | 187 | 325 | 0.000 |
| Console time (min), mean | 128 | 128 | 1.000 |
| Postoperative complication, n (%) | 4 (6.8) | 7 (12.3) | 0.316 |
BMI = body mass index; EBL = estimated blood loss; EPIC-CP = Expanded Prostate Cancer Index for Clinical Practice; Preop = preoperative; PSA = prostate-specific antigen; RS-RARP = Retzius-sparing robotic-assisted radical prostatectomy; S-RARP = standard robotic-assisted radical prostatectomy.
RS-RARP versus S-RARP (Table 2) was significantly associated with less penile shortening (41.7% vs 66.7%, p = 0.012), Peyronie’s disease (0% vs 8.7%, p = 0.020), and fewer inguinal hernias (0.0% vs 12.3%, p = 0.006).
Table 2.
Outcomes of answers to survey questions regarding penile shortening, deformity, and inguinal hernia development
| RS-RARP (N = 60) |
S-RARP (N = 57) |
p value | |
|---|---|---|---|
| Penile shortening | 25 (41.7) | 37 (66.7) | 0.012 |
| Peyronie's disease | 0 (0.0) | 5 (8.7) | 0.020 |
| Inguinal hernia | 0 (0.0) | 7 (12.3) | 0.006 |
RS-RARP = Retzius-sparing robotic-assisted radical prostatectomy; S-RARP = standard robotic-assisted radical prostatectomy.
In adjusted analyses (Table 3), RS-RARP (odds ratio [OR] 0.24, 95% confidence interval [CI] 0.09–0.63, p = 0.004) was independently associated with a lower risk of postoperative penile shortening. Conversely, a higher body mass index (BMI) was associated with a higher risk of postoperative penile shortening (OR 1.13, 95% CI 1.01–1.26, p = 0.037).
Table 3.
Multivariate logistic regression determining factors influencing postoperative penile shortening
| Variable | Odds ratio | 95% Confidence interval | p value | |
|---|---|---|---|---|
| Age | 0.99 | 0.92 | 1.07 | 0.926 |
| BMI | 1.13 | 1.01 | 1.26 | 0.037 |
| RS-RARP vs S-RARP | 0.24 | 0.09 | 0.63 | 0.004 |
| Nerve sparing | 0.26 | 0.06 | 1.12 | 0.071 |
| Prostate weight | 1.01 | 0.99 | 1.04 | 0.426 |
| Preoperative EPIC sexual domain score | 1.01 | 0.86 | 1.18 | 0.922 |
| Postoperative potency | 0.94 | 0.55 | 1.62 | 0.835 |
BMI = body mass index; EPIC = Expanded Prostate Cancer Index; RS-RARP = Retzius-sparing robotic-assisted radical prostatectomy; S-RARP = standard robotic-assisted radical prostatectomy.
There were no significant variables related to the risk of developing postoperative Peyronie’s disease or inguinal hernia (Table 4, Table 5).
Table 4.
Cox proportional hazards model to assess the risk of postoperative Peyronie’s disease
| Variable | Hazard ratio | 95% Confidence interval | p value | |
|---|---|---|---|---|
| Time from surgery | 0.99 | 0.98 | 1.01 | 0.626 |
| RS-RARP vs S-RARP | 0.98 | 0.47 | 2.03 | 0.947 |
| Nerve sparing | 0.95 | 0.51 | 1.74 | 0.856 |
| Preoperative EPIC sexual domain score | 0.99 | 0.93 | 1.06 | 0.823 |
| Postoperative potency | 1.04 | 0.81 | 1.32 | 0.780 |
EPIC = Expanded Prostate Cancer Index; RS-RARP = Retzius-sparing robotic-assisted radical prostatectomy; S-RARP = standard robotic-assisted radical prostatectomy.
Table 5.
Cox proportional hazards model to assess the risk of postoperative inguinal hernia
| Variable | Hazard ratio | 95% Confidence interval | p value | |
|---|---|---|---|---|
| Time from surgery | 0.99 | 0.99 | 1.01 | 0.858 |
| Age | 1.01 | 0.98 | 1.04 | 0.643 |
| RS-RARP vs S-RARP | 1.06 | 0.56 | 2.01 | 0.866 |
| Console time | 0.99 | 0.99 | 1.01 | 0.714 |
| Estimated blood loss | 1.00 | 0.99 | 1.00 | 0.679 |
RS-RARP = Retzius-sparing robotic-assisted radical prostatectomy; S-RARP = standard robotic-assisted radical prostatectomy.
4. Discussion
Studies demonstrate that RS-RARP leads to early recovery of urinary function [6], [9]. However, there are a few studies that have follow-up at 1 yr and beyond, and our series was the first to demonstrate that urinary continence advantages of RS-RARP persists at 12 mo utilizing the EPIC-CP score, a validated patient-reported quality of life questionnaire [7]. Moreover, we hypothesized that anatomic differences in surgical approach may confer additional benefits for RS-RARP. The “hidden” post-RP complications such as penile shortening, Peyronie’s disease, and inguinal hernia may be long-term complications that may also mitigated by RS-RARP. Our study has several important findings. First, RS-RARP was associated with fewer patient-reported adverse events such as penile shortening. Up to 55% of men report penile shortening after RP [2], which is somewhat lower than our finding of 66.7% of patients. Gontero et al [10] studied postprostatectomy penile shortening, noting that the most severe penile shortening, measured by stretched penile length, occurred at the time of catheter removal, which remained significant over 1 yr postoperatively, with a mean decrease of 1.3 and 2.3 cm in flaccid and stretched penile length, respectively. This causes bother, worsens quality of life, and lowers self-esteem [2]. While differences in penile length and circumference have been noted as a sequela of RP, the precise etiology remains unclear [11]. In the study by Gontero et al [10], nerve-sparing technique and recovery of erectile function have been associated with preservation of penile length. However, all patients underwent retropubic RP with division of the dorsal vascular complex. Therefore, the effect of dorsal vascular complex preservation remains unknown. Lei et al [12] were the first to describe the presence of two arterioles that are severed during the division of the dorsal vascular complex with S-RARP. These arterioles supply the corpora cavernosum, and vascular preservation may attenuate penile shortening.
Data increasingly show the role of the pelvic floor in erectile health [13]. Another possible contributing factor for penile shortening during S-RARP may be the change of the structural support from dropping the bladder away from the anterior abdominal wall and entering the endopelvic fascia. Preservation of the pelvic fascial support with RS-RARP may help preserve the penile length lost in comparison with conventional RP. Many have posited that the loss of urethral length leads to penile shortening within the 1st year following surgery; however, changes in urethral length after RP normalized 1 yr following surgery. Kadono et al [14] measured membranous urethral length by magnetic resonance imaging, finding shortening 10 d after RP but reversal of this shortening 12 mo after RP. RS-RARP avoids arterial disruption and preserves the fascial support of the bladder and the membranous urethra, thus potentially mitigating the loss of membranous urethral seen following RP.
Second, no RS-RARP patient experienced Peyronie’s disease, while 8.3% of S-RARP patients experienced Peyronie’s disease, which is both statistically and clinically significant. Peyronie’s disease has been reported in up to 15.9% of men following prostatectomy [4]. The pathophysiology of postprostatectomy Peyronie’s disease remains unclear, although Peyronie’s disease may result from microvascular injury, resulting in fibrin deposition and trapping within the tunica albuginea that surrounds the corpora, which causes pathological fibrosis and plaque formation [15].Preservation of the arterioles in the dorsal vascular complex may prevent corporal injury leading to Peyronie’s disease. This is supported by Iacono et al [16], who found significantly increased collagen deposition on post-RP cavernosal biopsy with a corresponding decrease in elastic and smooth muscle fibers. They postulated that both denervation and ischemia resulting from the disruption of nervous and arterial supply to the penis led to these histological changes, which may explain post-RP penile shortening as well as Peyronie’s disease. While RS-RARP was not associated with a decreased risk of postoperative Peyronie’s disease in our Cox proportional hazards model, given the overall rarity of events in our cohort, these models may not be robust enough to provide any significance.
Third, on adjusted analysis we found that nerve sparing and postoperative potency were not associated with penile length preservation. Similarly, Savoie et al [11] performed a prospective study on post-RP penile length and also found that potency did not predict shortening. The association of nerve sparing with less penile shortening supports the theory that neurogenic injury can lead to postoperative collagen deposition and erectile dysfunction [16]; however, this was not significant in our group, although it approached significance. Future studies with more power are needed to determine whether nerve-sparing procedures affect postoperative penile shortening. We also found that men with a higher BMI were more likely to experience shortening. While obese men have been found to have worse potency outcomes following RP [17], to our knowledge, the finding of increased penile shortening in obese men is a novel finding. Additionally, in contrast to Kadono et al [14], we did not find prostate weight to have a significant association with the postoperative loss of penile length.
Finally, no RS-RARP patients developed adverse events such as inguinal hernia compared with 14.6% of S-RARP patients. The incidence of post-RP adverse events such as inguinal hernia ranges from 7.5% to 13.7%. These are usually indirect hernias and manifest within 2–3 yr following surgery [5]. Disruption of Hesselbach’s triangle when releasing the bladder from the anterior abdominal wall and violating the transversalis fascia, as well as possible disruption of the deep inguinal ring, is thought to be a contributing factor [18]. During RS-RARP, the anterior abdominal wall is left undisturbed, thus avoiding these risk factors for hernia development. This is clinically significant, as development of symptomatic inguinal hernia leads to pain, poor quality of life, and potential need for surgical repair [18]. While RS-RARP was not associated with a decreased risk of inguinal hernia development on Cox proportional hazards model, given that there were no events in the RS-RARP group, we feel that this is due to a lack of overall events to make this model meaningful, which also highlights the need for further study with increased power to confirm our hypothesis.
Our study must be interpreted within the context of the study design. RS-RARP is a novel and promising surgical approach; however, with new techniques, published series are relatively small and follow-up is limited. A recent survey indicated that it is limited to 30 centers worldwide [19]. Similarly, our major limitation is the small sample size and limited follow-up. This is likely more significant for our Peyronie’s disease and inguinal hernia findings, as Tal et al [4] found that the mean time to the development of Peyronie’s disease is 13.9 mo, while Alder et al [5] found that most developed within 2–3 yr, and therefore the S-RARP group has had longer time at risk. Additionally, our small sample size did not allow us to discover a significant association between RS-RARP and reduced postoperative Peyronie’s disease and inguinal hernia in our Cox proportional hazards model. However, given the complete lack of these events in the RS-RARP group, we still feel that our hypothesis is valid and more power is needed in future study to confirm this. These limitations are less significant for penile shortening as many studies have shown that penile length is usually shortest within 1 yr, and our RS-RARP study population had shorter follow-up than the S-RARP study population [14]. Additionally, there has been no other study examining these outcomes following RS-RARP, and our findings should be considered hypothesis generating and lead to a future prospective study in larger cohorts. Second, this is a retrospective study and our survey measures patient-reported outcomes rather than objective physical examination findings such as stretched penile length (which approximates erect penile length) [10], plaque formation or penile curvature, or inguinal bulge with Valsalva. However, patient distress and bother are patient centered and are not elicited by physical examination findings, and are the driver of patient-initiated care rather than physical examination findings. Moreover, surgical repair of inguinal hernias is an objective endpoint, but may undercapture the difference in these sequelae between surgical techniques.
5. Conclusions
Our study suggests that the differences in the anatomic approach between RS-RARP and S-RARP may result in less patient-perceived penile shortening, Peyronie’s disease, and inguinal hernia sequelae. These findings should be considered as hypothesis generating and should lead to a further prospective study with greater power and longer follow-up to examine the role of dorsal vascular complex and pelvic fascia sparing during RS-RARP in preventing such sequelae.
Author contributions: Keith J. Kowalczyk had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Kowalczyk, Davis, Hu.
Acquisition of data: O'Neill, Lee.
Analysis and interpretation of data: Kowalczyk, Davis, Hu, Orzel, Rubin.
Drafting of the manuscript: Kowalczyk, Davis, Hu.
Critical revision of the manuscript for important intellectual content: Kowalczyk, Davis, Hu, Orzel, Rubin.
Statistical analysis: Kowalczyk.
Obtaining funding: None.
Administrative, technical, or material support: Kowalczyk.
Supervision: Kowalczyk.
Other: None.
Financial disclosures: Keith J. Kowalczyk certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Acknowledgements: Medical illustrations were done by David Klemm, Georgetown University Medical Center, Washington, DC, USA.
Associate Editor: Guillaume Ploussard
References
- 1.Deveci S., Gotto G.T., Alex B., O’Brien K., Mulhall J.P. A survey of patient expectations regarding sexual function following radical prostatectomy. BJU Int. 2016;118:641–645. doi: 10.1111/bju.13398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carlsson S., Nilsson A.E., Johansson E., Nyberg T., Akre O., Steineck G. Self-perceived penile shortening after radical prostatectomy. Int J Impot Res. 2012;24:179–184. doi: 10.1038/ijir.2012.13. [DOI] [PubMed] [Google Scholar]
- 3.Mulhall J.P., Secin F.P., Guillonneau B. Artery sparing radical prostatectomy--myth or reality? J Urol. 2008;179:827–831. doi: 10.1016/j.juro.2007.10.021. [DOI] [PubMed] [Google Scholar]
- 4.Tal R., Heck M., Teloken P., Siegrist T., Nelson C.J., Mulhall J.P. Peyronie’s disease following radical prostatectomy: Incidence and predictors. J Sex Med. 2010;7:1254–1261. doi: 10.1111/j.1743-6109.2009.01655.x. [DOI] [PubMed] [Google Scholar]
- 5.Alder R., Zetner D., Rosenberg J. Incidence of inguinal hernia after radical prostatectomy: a systematic review and meta-analysis. J Urol. 2020;203:265–274. doi: 10.1097/JU.0000000000000313. [DOI] [PubMed] [Google Scholar]
- 6.Galfano A., Ascione A., Grimaldi S., Petralia G., Strada E., Bocciardi A.M. A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery. Eur Urol. 2010;58:457–461. doi: 10.1016/j.eururo.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Egan J., Marhamati S., Carvalho F. Retzius-sparing robot-assisted radical prostatectomy leads to durable improvement in urinary function and quality of life versus standard robot-assisted radical prostatectomy without compromise of oncologic efficacy: single surgeon series and step-by-step. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.05.010. Jun 11;S0302-2838(20)30350-X. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 8.Carlsson S., Nilsson A.E., Johansson E. The prevalence of Peyronie’s disease: results of a large survey. BJU Int. 2001;88:727–730. doi: 10.1046/j.1464-4096.2001.02436.x. [DOI] [PubMed] [Google Scholar]
- 9.Eden C.G., Moschonas D., Soares R. Urinary continence four weeks following Retzius-sparing robotic radical prostatectomy: The UK experience. J Clin Urol. 2018;11:15–20. [Google Scholar]
- 10.Gontero P., Galzerano M., Bartoletti R. New insights into the pathogenesis of penile shortening after radical prostatectomy and the role of postoperative sexual function. J Urol. 2007;178:602–607. doi: 10.1016/j.juro.2007.03.119. [DOI] [PubMed] [Google Scholar]
- 11.Savoie M., Kim S.S., Soloway M.S. A prospective study measuring penile length in men treated with radical prostatectomy for prostate cancer. J Urol. 2003;169:1462–1464. doi: 10.1097/01.ju.0000053720.93303.33. [DOI] [PubMed] [Google Scholar]
- 12.Lei Y., Alemozaffar M., Williams S.B. Athermal division and selective suture ligation of the dorsal vein complex during robot-assisted laparoscopic radical prostatectomy: description of technique and outcomes. Eur Urol. 2011;59:235–243. doi: 10.1016/j.eururo.2010.08.043. [DOI] [PubMed] [Google Scholar]
- 13.Cohen D., Gonzalez J., Goldstein I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sex Med Rev. 2016;4:53–62. doi: 10.1016/j.sxmr.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Kadono Y., Machioka K., Nakashima K. Changes in penile length after radical prostatectomy: investigation of the underlying anatomical mechanism. BJU Int. 2017;120:293–299. doi: 10.1111/bju.13777. [DOI] [PubMed] [Google Scholar]
- 15.Devine C.J., Somers K.D., Jordan G.H., Schlossberg S.M. Proposal: trauma as the cause of the Peyronie’s lesion. J Urol. 1997;157:285–290. doi: 10.1016/s0022-5347(01)65361-8. [DOI] [PubMed] [Google Scholar]
- 16.Iacono F., Giannella R., Somma P., Manno G., Fusco F., Mirone V. Histological alterations in cavernous tissue after radical prostatectomy. J Urol. 2005;173:1673–1676. doi: 10.1097/01.ju.0000154356.76027.4f. [DOI] [PubMed] [Google Scholar]
- 17.Wiltz A.L., Shikanov S., Eggener S.E. Robotic radical prostatectomy in overweight and obese patients: oncological and validated-functional outcomes. Urology. 2009;73:316–322. doi: 10.1016/j.urology.2008.08.493. [DOI] [PubMed] [Google Scholar]
- 18.Chen H.R., Ting H.K., Kao C.C. Robot-assisted radical prostatectomy may induce inguinal hernia within the first 2 years: an 11-year single-surgeon experience of &400 cases. Medicine (Baltimore) 2018;97:e12208. doi: 10.1097/MD.0000000000012208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olivero A., Galfano A., Piccinelli M. Retzius-sparing robotic radical prostatectomy for surgeons in the learning curve: a propensity score-matching analysis. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.05.010. Jun 11;S0302-2838(20)30350-X. Online ahead of print. [DOI] [PubMed] [Google Scholar]