Abstract
Introduction
The aim of this study was to assess the short-term functional outcomes and the efficacy of hemostasis performed with holmium laser performed following prostatic hydroablation with the Aquabeam® system.
Material and methods
Between June 2019 and July 2020, 53 consecutive patients underwent Aquabeam® with our modified hemostasis approach with holmium laser. The following standard preoperative assessments were retrospectively recorded: prostate volume; International Prostate Symptom Score (IPSS) and Quality of Life (IPSS-QoL); uroflowmetry including Qmax and post void residual volume (PVR).
Results
Fifty-three patients consecutively underwent aquablation and holmium laser hemostasis. Median age at surgery, median prostate-specific antigen (PSA) and median prostate volume were 62 years (IQR: 57–66), 2.95 ng/ml (IQR: 1.6–4.8) and 55 ml (IQR: 43–65), respectively.
Median operative time was 60 minutes (IQR: 40–80). Median catheterization time and length of hospital stay were 2 days (IQR: 1–3) for both parameters. The median hemoglobin decrease between the preoperative values and those assessed on the second day was equal to 1.25 g/dl (IQR: 0.7–1.85).
Continence rate was 100% at catheter removal. Thirty-six patients (72%) reported anterograde ejaculation preservation. IPSS (6, 3–21) and Qmax (19, 9–26) changed dramatically between baseline and 3 months follow-up.
Conclusions
The combination of Aquabeam® and holmium laser energy for hemostasis is a safe, reproducible technique to relieve moderate lower urinary tract symptoms (LUTS) in men with benign prostatic hyperplasia (BPH) while preserving ejaculation in younger and sexually active individuals. The short-term results showed a lower rate of complications; the encouraging functional results confirm that this can be a valid surgical approach for treatment of BPH.
Keywords: benign prostatic hyperplasia, Aquabeam®, holmium laser
INTRODUCTION
Benign prostatic hyperplasia (BPH) is one of the most common age-related medical disease in men, with a troublesome impact on quality of life and a non-negligible social burden. Bothersome lower urinary tract symptoms (LUTS) affect more than 40% of ≥40 years male individuals with BPH [1]. The treatment options for male LUTS widely range from watchful waiting to oral medications to surgical procedures.
In terms of the surgical treatment of BPH, transurethral resection of the prostate (TURP) is considered as the gold standard in patients with benign prostatic enlargement with a prostate volume <80 ml [2]. Recently, different laser techniques have become available for surgical treatment of BPH; and several studies, including randomized controlled trials, demonstrated equivalent early- and long-term functional outcomes as compared to TURP [3–6] and open prostatectomy (OP) [7, 8], even in case of large prostate volume (>80 ml) [9–10]. Therefore, holmium laser enucleation of prostate (HoLEP) is currently defined by the International European Guidelines [2] as an effective alternative to TURP and open prostatectomy (OP), with several advantages of the minimally invasive approach, including shorter catheterization time and hospital stay, reduced blood loss and lower amount of blood transfusions [3, 4, 7, 9, 11]. However, TURP and laser surgical procedures (e.g. HoLEP, ThuLEP, etc.) are burdened by a high rate of functional sequelae that negatively impact the quality of life of patients (such as retroejaculation). With this in mind, new surgical approaches have been introduced to treat BPH, which allow to obtain excellent functional results in terms of preservation of antegrade ejaculation and to decrease postoperative irritative symptoms.
Aquablation utilizes a high-velocity saline stream to resect parenchymal tissue, a waterjet technique having first been described in canine liver resection [12]. Waterjet technology was then adapted for use in human liver resection, with further experience showing that the technique was feasible in neurosurgical, pulmonary and bladder tumor resections [12, 13, 14]. This technology has been further developed for use in prostatic ablation in the Aquabeam® (PROCEPT BioRobotics, Redwood Shores, CA, USA) system which utilizes a minimally invasive, image-guided, high-velocity waterjet for prostate ablation. In the available literature, one of the limitations of this technique is the impossibility to perform adequate hemostasis following ablation of the prostate tissue. In particular, in almost all the trials, hemostasis is recommended through the use of bipolar energy. Having a significant experience in the use of laser technology in the treatment of BPH, the aim of our study was to assess the short-term functional outcomes and the efficacy of hemostasis performed with holmium laser performed after prostatic hydroablation with Aquabeam® in a single cohort of patients.
MATERIAL AND METHODS
Patients and preoperative assessment
Between June 2019 and July 2020, 53 consecutive patients underwent Aquabeam® with our modified hemostasis approach with holmium laser. All the procedures were performed by two trained urologists who have already completed their learning curve for prostate aquablation and with a significant experience in the use of holmium laser. The following standard preoperative assessment were retrospectively recorded: prostate volume; International Prostate Symptom Score (IPSS) and Quality of Life (IPSS-QoL); uroflowmetry including Qmax and post void residual volume (PVR). In suspicious cases (of prostate cancer [increase of prostate-specific antigen (PSA), digital rectal examination positive] we discussed with the patient the possibility of magnetic resonance imaging (MRI) of the prostate [15, 16], and in presence of a radiological lesion we performed ‘in-bore’ MRI-guided prostate biopsy or fusion biopsy [17, 18]. The study was conducted in accordance with the principles issued in the Helsinki Declaration for Human Rights. Each patient enrolled signed an informed consent form which described the principles and purposes of the study, the methods of carrying out the various diagnostic techniques and any inherent risks. The study was not submitted to an ethics committee because the two surgical techniques are not experimental and are already used in urological surgery.
Surgical technique
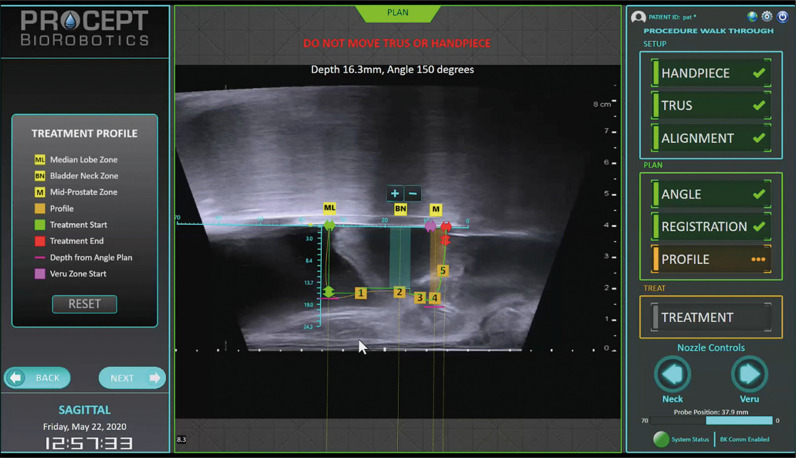
Each patient underwent surgery under general anaesthesia. Prostatic adenoma ablation was performed using the Aquabeam® System. Preoperatively, a transrectal prostatic ultrasound with a transrectal linear probe (BK 5000® ultrasound system) was performed to assess the prostate volume, the morphology of the gland (including the presence of calcifications, middle lobe, etc.) and, to guide the procedure. Subsequently, a 24 Fr handpiece probe was inserted in the prostatic urethra and locked into place using a rigid arm fixed to the bed. The ultrasound-guided and endoscopic check allows for the placement of the handpiece at the level of the verumontanum, anterior to the external sphincter. Under real-time prostate visualization with transrectal ultrasound the operator used a console to contour the target tissue (Figure 1). Under visual and ultrasound control, the tissue ablation was performed robotically with a high velocity waterjet while sparing verumontanum, ejaculatory ducts and muscle tissue.
Figure 1.
Planning of Waterjet treatment.
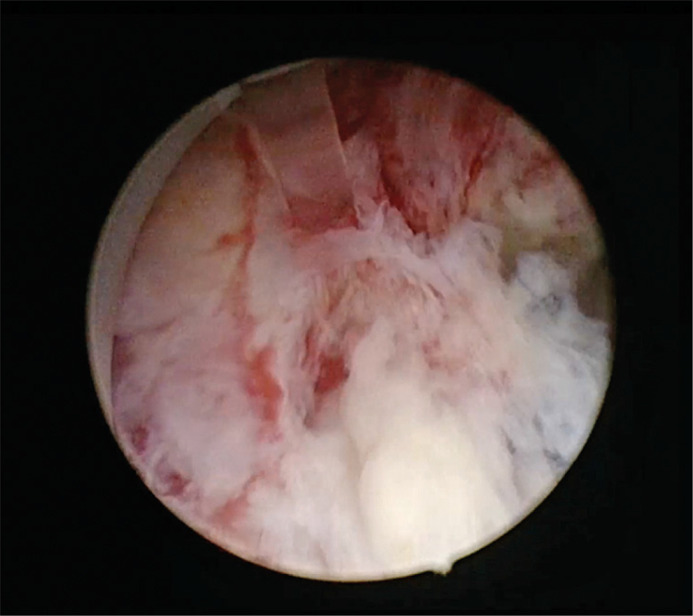
After aquablation, the handpiece and the ultrasound probe were removed; the hemostasis was performed with a continuous-flow 26 Fr resectoscope (Karl-Storz), a distal bridge to hold the fiber, a video camera, a 550 µm holmium laser end-fire fiber connected to the laser generator (Lumenis Versa Pulse 120W) and saline irrigation. Coagulation setting was 60 W (2 J x 30 Hz long pulse). In order to minimize the thermal damage generated by the holmium laser, selective hemostasis was performed only on the major bleeding sources (Figure 2). The main sources of bleeding were generally observed at the level of the bladder neck (at 10 and at 2 o’clock positions) and at the level of the anterior surface of the prostate. No hemostasis was performed in the proximity of the verumontanum in order not to damage the structures of the ejaculatory ducts. To conclude the procedure, a 22 Fr Dufour silicon catheter was placed (with continue bladder irrigation). Postoperatively, the bladder irrigation was stopped on the first postoperative day and the catheter was removed on the second postoperative day.
Figure 2.
Effect of holmium laser hemostasis on prostatic tissue.
Statistical analysis
Data were analysed using Statistical Package for Social Science (SPSS) version 21 for Macintosh.
Continuous variables have been reported as means, standard deviation (SD) or medians and interquartile ranges (IQR), respectively. Categorical variables were reported as frequencies with percentages.
RESULTS
Overall, 53 patients consecutively underwent aquablation and holmium laser hemostasis at our institution.
Table 1 shows patients’ characteristics. Median age at surgery, median PSA and median prostate volume were 62 years (IQR: 57–66), 2.95 ng/ml (IQR: 1.6–4.8) and 55 ml (IQR: 43–65), respectively. In regards to medical therapy for BPH, 37 patients took daily α1-blocker therapy, 6 patients the 5-ARI and 7 patients were taking combination therapy.
Table 1.
Baseline patients’ characteristics
| Age (years) Median (IQR) Range |
62 (57–66) 50;81 |
| Prostate volume (ml) Median (IQR) Range |
55 (43–65) 25;90 |
| Preoperative Qmax (ml/s) Median (IQR) Range |
9 (6.2–10) 4;11.3 |
| Preoperative IPSS Median (IQR) Range |
19 (17–22) 14;35 |
| Preoperative indwelling catheter [n (%)] | 6 (11.3) |
| Preoperative PSA (ng/ml) Median (IQR) Range |
2.95 (1.6–4.8) 0.46;15 |
| Preoperative medical treatment [n (%)] Alpha-lytic 5-ARI Combined treatment |
37 (69.8) 6 (11.3) 7 (13.2) |
| Operative time (min) Median (IQR) Range |
60 (40–80) 25;168 |
IQR – interquartile range; IPSS – International Prostate Symptom Score; PSA – prostate-specific antigen; n – number; 5-ARI – 5-alpha-reductase inhibitors
Median preoperative Qmax, preoperative IPSS and preoperative IPSS-QoL were 9 ml/s (IQR: 6.2–10), 19 (IQR: 17–22) and 3 (IQR: 2–4), respectively.
The perioperative outcomes are reported in Table 2. Median operative time was 60 minutes (IQR: 40–80). Median catheterization time and length of hospital stay were 2 days (IQR: 1–3) in both cases. The median hemoglobin decrease between the preoperative values and those assessed on the second day was equal to 1.25 g/dl (IQR: 0.7–1.85).
Table 2.
Postoperative results
| Catheterization time (d) Median (IQR) |
2 (1–3) 1;3 |
| Hemoglobin decrease (g/dL) Median (IQR) Range |
1.25 (0.7–1.85) -0.6; 6.1 |
| Length of stay (d) Median (IQR) |
2 (1–3) 1;3 |
| Overall complications, n. (%) | 2 (3.8) |
| Complication severity, n. (%) Clavien-Dindo I Clavien-Dindo III |
1 (1.9) 1 (1.9) |
| Preserved ejaculation | 36 (72%) |
| Postoperative IPSS (3 months) Median (IQR) Range |
6 (5–8) 3;21 |
| Postoperative Qmax (3 months) Median (IQR) Range |
19 (15–21) 9;26 |
d – days; IQR – interquartile range; IPSS – International Prostate Sypmtom Score
Continence rate was 100% at catheter removal. Only 2 low-grade Clavien complications (3.8%) were recorded, without any major complications (Clavien ≥3).
Thirty-six patients (72%) reported preserved ejaculation. IPSS (6, 3–21) and Qmax (19, 9–26) changed dramatically between baseline and 3 months follow-up.
DISCUSSION
The management for BPH remains complex and comprises surgical and pharmacologic therapies. In offering the best treatment to the patient, it is necessary to balance therapeutic efficacy and the possibility of adverse events or negative sequelae, especially in choosing the appropriate surgical approach. Last but not least, it is very important to evaluate the costs and economic impacts of surgical procedures [19]. In the current guidelines TURP is considered the gold standard therapy for LUTS due to BPH of small/medium prostate volume (<80 ml); in the literature it is regarded as the most commonly performed surgical procedure for treatment of BPH [20]. Actually, HoLEP has gained wide consensus, establishing a new size-independent surgical gold standard for BPH treatment in large volume prostate (>80 ml) with excellent results in terms of LUTS and hemostasis [21].
Despite excellent long-term efficacy in terms of relieving BPH symptoms, this surgical technique does not lack its complications and sequelae. In particular, the high rate of loss of antegrade ejaculation significantly compromises the quality of life of patients. As shown in some epidemiological studies, absence of ejaculation affects sexual activity and global quality of life [22, 23]. Concerning the complications regarding TURP, Madersbacher et al. reported an overall incidence of secondary procedures (TURP, transurethral incision of prostate (lTUIP) or urethrotomy) after TURP of 5.8%, 12.3% and 14.7% at one, five and eight years after surgery in a series of 20,671 men in Austria [24]. Similarly, Wasson et al. reported a 5% re-operation rate in a series of 188,000 patients who underwent TURP during a 5-year follow-up period [25]. Also, when a particular device was used in order to improve TURP performance, the negative impact on sexual performance is quite high [26]. In this scenario, in recent years we have seen the introduction of new approaches for the surgical treatment of BPH in order to obtain better results in terms of reduction of LUTS due to BPH and satisfactory functional results (such as maintaining antegrade ejaculation) [27, 28]. Aquablation combines real-time, multidimensional imaging, autonomous robotics and heat-free waterjet ablation for targeted, controlled and immediate removal of prostate tissue for the treatment of LUTS caused by BPH. The principal trials available in the literature have demonstrated the non-inferiority compared to TURP in the treatment of medium / large prostatic adenomas and excellent functional results [29, 30, 31]. In these trials, hemostasis after Aquabeam® was achieved using focal, non-resective electrocautery or low pressure inflation of a Foley balloon catheter in the prostatic fossa [32]. Catheterization and bladder irrigation were left to local investigator discretion. In the WATER I study [29], the safety and efficacy of aquablation was compared to TURP for the treatment of BPH; about the result of hemostasis after the procedure, postoperative hemoglobin decreased from 14.9 to 13.0 in the aquablation group and from 14.7 to 13.7 in the TURP group (p 1⁄4 0.0002); only a single aquablation case required blood transfusion. Mean hospital stay was 1.4 days in each group and the urinary catheter was removed at a median of 1 day after surgery in each group. In their experience, Gilling et al. [33] showed that monopolar or bipolar cautery can be used for local hemostasis, whereas laser energy coagulation is ineffective. In our experience, as a high-volume centre for HoLEP, holmium laser represents a safety and effective surgical approach for treatment of BPH in small, medium and large prostates. For this reason, we have tested the efficacy of holmium laser hemostasis performed after Aquabeam®. In our study, the results in terms of postoperative haemoglobin decrease are similar to the results of a study which used the monopolar and bipolar energy for cautery. The time of catheterization was 48 hours and no case of blood transfusion was observed. In terms of complications we observed 2 cases of low-grade Clavien grade, with a case of urinary tract infection and one of mild haematuria, which were resolved with oral antibiotics and bladder irrigation lasting less than 24 hours, respectively. Additionally, each subjective and objective voiding parameter (IPSS, QoL, Qmax, PVR) improved postoperatively. No secondary procedures were recorded during our 3 month follow up. In our study, we found a postoperative preserved ejaculation in 72% of patients. In the literature, the ejaculatory function rates were over 80% in patients with medium/large prostate [34] This is lower than the 90% antegrade ejaculation preservation reported by the WATER trial focusing on small to moderate-sized prostate treated with aquablation [30]. As for maintenance of sexual quality of life, specifically antegrade ejaculation, it is a major concern in many patients, the higher probability of preserving antegrade ejaculation represents a significant improvement compared to established surgical techniques. In our series, the slight decrease in ejaculation rate, with respect to the literature, is probably secondary to the use of holmium laser in coagulation; in particular the possible thermal and mechanical damage of anatomical structures responsible of anterograde ejaculation on the bladder neck and around the verumontanum may be the reason; further anatomical studies are needed to confirm this theory.
This study has some limitations predominantly related to its retrospective design. Additional limitations to this study are the lack of a control group, the short-term follow-up and the small size of the cohort. However, our data showed an effective hemostasis performed with holmium laser following Aquabeam® and functional results substantially in line with the available literature. Full data validation requires longer follow-up and prospective randomized trials with larger cohorts.
CONCLUSIONS
The combination of Aquabeam® and holmium laser energy for hemostasis is a safe, reproducible technique to treat moderate LUTS in men with BPH while preserving ejaculation in younger and sexually active individuals. The short-term results showed a lower rate of complications and the encouraging functional results attest that this can be a valid surgical approach for the treatment of BPH. Long-term data and randomized trials are needed to validate this theory.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.De Ridder D, Roumeguere T, Kaufman L. Urgency and other lower urinary tract symptoms in men aged ≥40 years: a Belgian epidemiological survey using the ICIQ-MLUTS questionnaire. Int J Clin Pract. 2015;69:358–365. doi: 10.1111/ijcp.12541. [DOI] [PubMed] [Google Scholar]
- 2.Gravas S, Cornu JN, Gacci M, et al. Management of Non-neurogenic Male LUTS. European Association of Urology Guidelines; 2019. [Google Scholar]
- 3.Lourenco T, Pickard R, Vale L, et al. Alternative approaches to endoscopic ablation for benign enlargement of the prostate: systematic review of randomised controlled trials. BMJ. 2008;337:a449. doi: 10.1136/bmj.39575.517674.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007;94:1201–1208. doi: 10.1002/bjs.5916. [DOI] [PubMed] [Google Scholar]
- 5.Montorsi F, Naspro R, Salonia A, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2- center prospective randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2008;179(5 Suppl):S87–S90. doi: 10.1016/j.juro.2008.03.143. [DOI] [PubMed] [Google Scholar]
- 6.Kuntz RM, Ahyai S, Lehrich K, Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electro- cautery resection of the prostate: a randomized prospective trial in 200 patients. J Urol. 2004;172:1012–1016. doi: 10.1097/01.ju.0000136218.11998.9e. [DOI] [PubMed] [Google Scholar]
- 7.Naspro R, Suardi N, Salonia A, et al. Holmium laser enucleation of the prostate versus open prostatectomy for prostates >70 g: 24- month follow-up. Eur Urol. 2006;50:563–568. doi: 10.1016/j.eururo.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008;53:160–166. doi: 10.1016/j.eururo.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 9.Busetto GM, Del Giudice F, D'Agostino D, et al. Efficacy and safety of Finasteride (5 alpha-reductase inhibitor) monotherapy in patients with benign prostatic hyperplasia: A critical review of the literature. Arch Ital Urol Androl. 2020;91:205–210. doi: 10.4081/aiua.2019.4.205. [DOI] [PubMed] [Google Scholar]
- 10.Leonardo C, Lombardo R, Cindolo L, et al. What is the standard surgical approach to large volume BPE? Systematic review of existing randomized clinical trials. Minerva Urol Nefrol. 2020;72:22–29. doi: 10.23736/S0393-2249.19.03589-6. [DOI] [PubMed] [Google Scholar]
- 11.Busetto GM, Del Giudice F, Maggi M, et al. Surgical blood loss during holmium laser enucleation of the prostate (HoLEP) is not affected by short-term pretreatment with dutasteride: a double-blind placebo-controlled trial on prostate vascularity. Aging (Albany NY) 2020;12:4337–4347. doi: 10.18632/aging.102883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papachristou DN, Barters R. Resection of the liver with a water jet. Br J Surg. 1982;69:93–94. doi: 10.1002/bjs.1800690212. [DOI] [PubMed] [Google Scholar]
- 13.Piek J, Oertel J, Gabb MR. Waterjet dissection in neurosurgical procedures: clinical results in 35 patients. J Neurosurg. 2002;96:690–696. doi: 10.3171/jns.2002.96.4.0690. [DOI] [PubMed] [Google Scholar]
- 14.Shekarriz H, Shekarriz B, Upadhyay J, Bürk C, Wood DP, Jr, Bruch HP. Hydro-jet assisted laproscopic partial nephrectomy intial experience in a porcine model. J Urol. 2000;163:1005–1008. [PubMed] [Google Scholar]
- 15.Porreca A, Giampaoli M, Bianchi L, et al. Preoperative multiparametric prostate magnetic resonance imaging: a safe clinical practice to reduce incidental prostate cancer in Holmium laser enucleation of the prostate. Cent European J Urol. 2019;72:106–112. doi: 10.5173/ceju.2019.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giampaoli M, Bianchi L, D'agostino D, et al. Can preoperative multiparametric MRI avoid unnecessary prostate biopsies before holmium laser enucleation of the prostate? Preliminary results of a multicentric cohort of patients. Minerva Urol Nefrol. 2019;71:524–530. doi: 10.23736/S0393-2249.19.03463-5. [DOI] [PubMed] [Google Scholar]
- 17.D'Agostino D, Romagnoli D, Giampaoli M, et al. ‘In-Bore’ MRI-Guided Prostate Biopsy for Prostate Cancer Diagnosis: Results from 140 Consecutive Patients. Curr Urol. 2020;14:22–31. doi: 10.1159/000499264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D'Agostino D, Mineo Bianchi F, Romagnoli D, et al. MRI/TRUS FUSION guided biopsy as first approach in ambulatory setting: Feasibility and performance of a new fusion device. Arch Ital Urol Androl. 2020;91:211–221. doi: 10.4081/aiua.2019.4.211. [DOI] [PubMed] [Google Scholar]
- 19.Schiavina R, Bianchi L, Giampaoli M. Holmium laser prostatectomy in a tertiary Italian center: A prospective cost analysis in comparison with bipolar TURP and open prostatectomy. Arch Ital Urol Androl. 2020;23:92. doi: 10.4081/aiua.2020.2.82. [DOI] [PubMed] [Google Scholar]
- 20.Reich O, Gratzke C, Stief CG. Techniques and long-term results of surgical procedures for BPH. Eur Urol. 2006;49:970–978. doi: 10.1016/j.eururo.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 21.Busetto GM, Del Giudice F, Maggi M, et al. Surgical blood loss during holmium laser enucleation of the prostate (HoLEP) is not affected by short-term pretreatment with dutasteride: a double-blind placebo-controlled trial on prostate vascularity. Aging (Albany NY) 2020;12:4337–4347. doi: 10.18632/aging.102883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Porreca A, Noale M, Artibani W, et al. Disease-specific and general health-related quality of life in newly diagnosed prostate cancer patients: the Pros-IT CNR study. Health Qual Life Outcomes. 2018;16:122. doi: 10.1186/s12955-018-0952-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noale M, Maggi S, Artibani W, et al. Pros-IT CNR: an Italian prostate cancer monitoring project. Aging Clin Exp Res. 2017;29:165–172. doi: 10.1007/s40520-017-0735-6. [DOI] [PubMed] [Google Scholar]
- 24.Madersbacher S, Lackner J, Brössner C, et al. Reoperation, myocardial infarction and mortality after transurethral and open prostatectomy: a nation-wide, long-term analysis of 23,123 cases. Eur Urol. 2005;47:499–504. doi: 10.1016/j.eururo.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 25.Wasson JH, Bubolz TA, Lu-Yao GL, Walker-Corkery E, Hammond CS, Barry MJ. Transurethral resection of the prostate among medicare beneficiaries: 1984 to 1997. For the Patient Outcomes Research Team for Prostatic Diseases. J Urol. 2000;164:1212–1215. [PubMed] [Google Scholar]
- 26.D'Addessi A, Porreca A, Foschi N, Racioppi M. Thick loop prostatectomy in the endoscopic treatment of benign prostatic hyperplasia: results of a prospective randomised study. Urol Int. 2005;74:114–117. doi: 10.1159/000083280. [DOI] [PubMed] [Google Scholar]
- 27.Porreca A, Mineo Bianchi F, D'Agostino D, et al. Ejaculation Sparing Bladder Neck Incision with Holmium Laser in Patients with Urinary Symptoms and Small Prostates: Short-Term Functional Results. Urol Int. 2019;103:102–107. doi: 10.1159/000499410. [DOI] [PubMed] [Google Scholar]
- 28.Cacciamani G, UHNA F, Tafuri A, et al. Anterograde ejaculation preservation after endoscopic treatments in patients with bladder outlet obstruction: systematic review and pooled-analysis of randomized clinical trial. Minerva Urologica e Nefrologica. 2019;71:427–434. doi: 10.23736/S0393-2249.19.03588-4. [DOI] [PubMed] [Google Scholar]
- 29.Gilling P, Barber N, Bidair M, et al. WATER: a double-blind, randomized, controlled trial of Aquablation vs transurethral resection of the prostate in benign prostatic hyperplasia. J Urol. 2018;199:1252–1261. doi: 10.1016/j.juro.2017.12.065. [DOI] [PubMed] [Google Scholar]
- 30.Bhojani N, Nguyen DD, Kaufman RP, Jr, Elterman D, Zorn KC. Comparison of <100 cc prostates and >100 cc prostates undergoing aquablation for benign prostatic hyperplasia. World J Urol. 2019;37:1361–1368. doi: 10.1007/s00345-018-2535-9. [DOI] [PubMed] [Google Scholar]
- 31.Nguyen D, Barber N, Bidair M, et al. Waterjet Ablation Therapy for Endoscopic Resection of prostate tissue trial (WATER) vs WATER II: comparing Aquablation therapy for benign prostatic hyperplasia in 30-80 and 80-150 mL prostates. BJU Int. 2020;125:112–122. doi: 10.1111/bju.14917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhojani N, Bidair M, Zorn KC, et al. Aquablation for benign prostatic hyperplasia in large prostates (80–150 cc): 1-year results. Urology. 2019;129:1–7. doi: 10.1016/j.urology.2019.04.029. [DOI] [PubMed] [Google Scholar]
- 33.Gilling P, Reuther R, Kahokehr A, Fraundorfer M. Aquablationdimage-guided robot-assisted waterjet ablation of the prostate: initial clinical experience. BJU Int. 2016;117:923. doi: 10.1111/bju.13358. [DOI] [PubMed] [Google Scholar]
- 34.Bhojani N, Nguyen DD, Kaufman RP, Jr, Elterman D, Zorn KC. Comparison of <100 cc prostates and >100 cc prostates undergoing aquablation for benign prostatic hyperplasia. World J Urol. 2019;37:1361–1368. doi: 10.1007/s00345-018-2535-9. [DOI] [PubMed] [Google Scholar]