Abstract
Background.
Research exploring the longitudinal course of posttraumatic stress disorder (PTSD) symptoms has documented four modal trajectories (low, remitting, high, and delayed), with proportions varying across studies. Heterogeneity could be due to differences in trauma types and patient demographic characteristics.
Methods.
This analysis pooled data from six longitudinal studies of adult survivors of civilian-related injuries admitted to general hospital emergency departments (EDs) in six countries (pooled N = 3,083). Each study included at least three assessments of the Clinician-Administered PTSD Scale in the first post-trauma year. Latent class growth analysis determined the proportion of participants exhibiting various PTSD symptom trajectories within and across the datasets. Multinomial logistic regression analyses examined demographic characteristics, type of event leading to the injury, and trauma history as predictors of trajectories differentiated by their initial severity and course.
Results.
Five trajectories were found across the datasets: Low (64.5%), Remitting (16.9%), Moderate (6.7%), High (6.5%), and Delayed (5.5%). Female gender, non-white race, prior interpersonal trauma, and assaultive injuries were associated with increased risk for initial PTSD reactions. Female gender and assaultive injuries were associated with risk for membership in the Delayed (vs. Low) trajectory, and lower education, prior interpersonal trauma, and assaultive injuries with risk for membership in the High (vs. Remitting) trajectory.
Conclusions.
The results suggest that over 30% of civilian-related injury survivors admitted to EDs experience moderate-to-high levels of PTSD symptoms within the first post-trauma year, with those reporting assaultive violence at increased risk of both immediate and longer-term symptoms.
Keywords: Posttraumatic stress, traumatic injuries, latent class growth analysis, resilience
Introduction
The majority of people will be exposed to one or more potentially traumatic events (PTE) in their lifetime (Kessler et al., 2017, Kessler et al., 1995, Nickerson et al., 2012). It is now well known that there is substantial heterogeneity in psychological responses to such events. This variability is reflected in the lifetime prevalence of posttraumatic stress disorder (PTSD), which has been consistently estimated at less than 10 percent across studies worldwide (for a review, see (Lowe et al., 2015).
From a longitudinal perspective, it has been theorized that there exists a range of patterns of PTSD symptom progression, including persisting low symptoms, initially high symptoms that either quickly or gradually remit, delayed-onset symptoms, and chronically moderate or high symptoms (Bonanno and Diminich, 2013, Norris et al., 2009). The existence of such subpopulations aligns with the results of longitudinal studies that used person-centered statistical methods, such as latent class growth analysis (LCGA), to search for classes of growth and decline in PTSD symptoms (Andruff et al., 2009, Jung and Wickrama, 2008, Van de Schoot, 2015). In the past decade, there has been a proliferation of such studies in the aftermath of traumatic events, including sexual assault, military deployment, and traumatic injury (Berntsen et al., 2012, Bonanno et al., 2012, Galatzer-Levy et al., 2013, Norris et al., 2009, Steenkamp et al., 2012).
A recent review of 67 studies of mental health (not exclusively PTSD symptoms) in the aftermath of PTEs provided evidence for four prototypical trajectories in relatively consistent proportions (Galatzer-Levy et al., 2018). The modal trajectory in this review was characterized by consistently low post-trauma symptoms, which the authors termed Resilience, with an average of 65.7% of participants exhibiting this pattern across studies. The other three trajectories were characterized by initially high symptoms that remitted over time (Recovery; 20.8%), consistently high symptoms (Chronic; 10.6%), and initially low symptoms that increased over time (Delayed Onset; 8.9%). Despite this consistency, the authors observed marked heterogeneity in the proportion of participants in each of the prototypical trajectories across studies.
Several factors could underlie the heterogeneity in trajectories across studies. First, as noted by Galatzer-Levy and colleagues (2018), sample characteristics likely influence the proportion of participants in each trajectory. One important characteristic appears to be the type of PTE to which participants were exposed, such that a consistently low trajectory is more common following less severe PTEs (e.g., Fink et al., 2017). A second source of heterogeneity could be timing of assessment, with the length of follow-up across trajectory studies ranging from months to several years post-trauma. Few studies have concluded within the first year following trauma exposure (for exceptions, see, e.g., (Berntsen et al., 2012, deRoon-Cassini et al., 2010, Dickstein et al., 2010, Steenkamp et al., 2012), which is arguably the time during which survivors might most readily have access to mental health services and interventions are most optimal, thereby reducing long-term costs associated with chronic symptoms. Finally, a range of assessment instruments has been utilized and, although this source of heterogeneity remains empirically unexplored, it remains possible that it could influence patterns of results. Few studies have used the gold-standard assessment of PTSD symptoms, the Clinician-Administered PTSD Scale (CAPS; (Blake et al., 1995); for exceptions, see (Boasso et al., 2015, Nash et al., 2015).
Addressing these three key sources of heterogeneity – type of PTE, timing of assessment, and assessment instrument – could yield more definitive information about the proportion of survivors likely to exhibit the four prototypical trajectories in the first post-trauma year. One context in which such information would be useful would be emergency departments (EDs), wherein survivors of traumatic injuries frequently present for immediate care. For example, in the United States in 2016, nearly 39 million injury survivors were treated in EDs, representing over 20 percent of primary diagnoses (Rui et al., 2016). Insight into what percentage of potentially traumatic injury survivors might be in need of services at different times during the first trauma year would help allocate scarce resources to prevent and treat of PTSD symptoms.
Addressing the heterogeneity in trajectory studies could also provide clinically useful information into the factors that predict trajectory membership. In an ED context, knowledge of such factors could inform targeted outreach efforts. Several factors have been identified that decrease the likelihood of a consistently low symptom trajectory, including demographic characteristics (e.g., female gender, low socioeconomic status), greater event severity, and prior trauma exposure (Bonanno et al., 2012, Bryant et al., 2015, Lowe et al., 2014, Pietrzak et al., 2013).
However, the literature has generally not explored predictors of trajectory membership with explicit attention to the two key elements that differentiate trajectories, that is, their starting points (i.e., intercepts) and how they change over time (i.e., slopes). Predicting intercept and slope terms is the goal of conventional latent growth curve models; however, these models are not appropriate for contexts in which subpopulations of growth are hypothesized, such as mental health in the aftermath of trauma (Jung and Wickrama, 2008). Strategically developing models predicting trajectory membership could provide similar information in the aftermath of trauma. For example, identifying predictors of trajectories that start with high, versus low, PTSD symptoms could shed light upon which survivors are likely to need immediate care after discharge. In contrast, analyses that focus on changes in symptoms over time – for example, membership in a consistently high trajectory versus a symptom recovery trajectory, or membership in a delayed-onset trajectory versus a consistently low trajectory – would help identify characteristics of survivors who might be in need of longer-term services.
The current study aimed to advance the literature on PTSD symptom trajectories by pooling data from six studies that each included survivors of civilian-related injuries severe enough to warrant ED admission, and that each had at least three post-trauma assessments of PTSD within the first year of trauma exposure using the CAPS. We first documented the proportion of participants in each trajectory both within and across the six datasets, and then developed predictive models to elucidate the factors associated with both initial PTSD reactions and the course of PTSD symptoms over time, including demographic characteristics, type of event leading to the injury, and history of trauma exposure. By documenting the prevalence and predictors of PTSD symptom trajectories in the pooled sample, we sought to provide more generalizable information about the short-term mental health needs of potentially traumatic injury survivors reporting to EDs. To our knowledge, this is the first study to analyze PTSD symptom trajectories using pooled data.
Method
Data from this study came from the International Consortium to Predict PTSD (ICPP), a collaboration to pool longitudinal studies of hospital admissions for civilian trauma-related incidents around the world. Articles published between 1997 and 2015 were screened for eligibility, including assessment of all 17 DSM-IV PTSD symptoms at two or more time points, starting early after trauma exposure. Lead authors of identified studies were invited to join the consortium and provide itemized data. Additional information on identification of studies and efforts to pool data can be found elsewhere (Qi et al., 2018). The current analysis included studies with least three assessments of PTSD symptoms using the Clinician-Administered PTSD Scale (CAPS; (Blake et al., 1995) within the first post-trauma year. Six studies met these criteria: the Multisite Acute Stress Disorder study (Multisite ASD; (Bryant et al., 2008), Jerusalem Trauma Outreach and Prevent Study (JTOPS; (Shalev et al., 2012), Tachikawa Cohort of Motor Vehicle Accidents (TCOM; (Matsuoka et al., 2009), Ohio Motor Vehicle Accident study (Ohio-MVA; (Delahanty et al., 2003), Zurich Intensive Care Unit study (Zurich ICU; (Hepp et al., 2008), and the Amsterdam Cortisol study (Mouthaan et al., 2014), each representing a different country (Australia, Israel, Japan, United States, Switzerland, and the Netherlands, respectively). Investigators of the six studies obtained informed consent from participants using procedures approved by their local institutional review boards. The pooled sample consisted of 3,083 participants.
Measures
PTSD symptoms.
PTSD symptoms were measured in each study with the CAPS (Blake et al., 1995), which is considered the “gold standard” assessment tool for PTSD. Participants reported on symptoms specifically in reference to the civilian-related injury leading to their hospital admission. The CAPS uses structured interviews to assess DSM-IV PTSD Criteria B (intrusive symptoms, e.g., unwanted memories and unpleasant dreams about the event), C (avoidance and numbing symptoms, e.g., avoidance of thoughts and feelings related to the event, feelings of detachment or estrangement from others) and D (hyperarousal symptoms, e.g., difficulty falling or staying asleep, difficulty concentrating). Each symptom is rated on frequency and intensity from 0 to 4, and symptom severity scores are calculated as the sum of all frequency and intensity ratings, ranging from 0 to 136 (Weathers et al., 1999). The CAPS has been found to have good psychometric properties across a range of clinical and research settings (Weathers et al., 2001), including high inter-rater reliability, test-retest reliability, and internal consistency (Blake et al., 1995, Hovens et al., 1994).
Predictors.
Two categories of predictors were included in the analysis. First, demographics that were assessed across all six studies were included: age quartiles (reference = <27 years of age), gender (reference = male), race (reference = white), level of education (reference = secondary education or more), and marital status (reference = married/living with a partner at baseline). Second, we included dummy variables indicating the type of incident leading to the injury, including motor vehicle accidents (MVA), other accidents, and assaults. MVA was used as the reference category as it was the most common precipitating incident in the pooled sample. We also included a variable for prior trauma severity including a history of non-interpersonal trauma or interpersonal trauma (reference = no prior trauma). In addition to these categories of predictors, we also controlled for the data source using dummy variables, with the source contributing the most participants to the pooled sample (Multisite ASD) as the reference group. For variables missing responses (race, education, marital status, prior trauma), an indicator for missingness was included.
Data Analysis
Data analysis consisted of four steps. First, descriptive analyses were conducted in R version 3.5 (Team, 2013). Means and standard deviations of the CAPS for each time point, and frequencies of covariates were computed. One-way analysis of variance tests were conducted to examine whether CAPS severity varied significantly across studies at each time point. Chi-square tests were conducted to assess for significant variation across studies on all covariates.
Second, latent class growth analyses (LCGA) were conducted in Mplus 8.0 (Muthén and Muthén, 1998) for each dataset. Based on prior research (Galatzer-Levy et al., 2018), we decided a priori to utilize the four-class solution from each dataset. However, models with classes ranging from 1 to 6 were conducted for descriptive purposes, and various statistical criteria (e.g., Bayesian information criteria, entropy, average posterior probabilities, Lo-Mendel-Rubin likelihood ratio test) were recorded, as per recommended guidelines (e.g., Jung & Wickrama, 2007; Andruff et al., 2009; Berlin et al., 2014). All models included both linear and quadratic growth terms. Given that five of the six datasets only had three data points for PTSS, the variance of intercept and growth terms for all models were constrained to facilitate convergence (Andruff et al., 2009; Berlin et al., 2014). Data points were anchored at the number of months since ED admission for each wave of the given study; assessments at <1 month were anchored at 0.5 months. Trajectories from the four-class model for each dataset were labeled based on intercept and slope terms with the following terms: (1) Low, (2) Moderate-Low, (3) Moderate, (4) Remitting, (5) Fast Remitting, (6) High, and (7) Delayed. The six datasets were then pooled, with trajectory membership included as a categorical variable, and the frequencies of predictor variables were computed.
Third, a series of predictive models was conducted using R version 3.5 (Team, 2013). Univariate differences in frequency of risk predictors between participants across studies and trajectories were assessed using likelihood-ratio χ2 tests. Multivariable binary logistic regression models including all predictors simultaneously were then fit to estimate factors affecting initial PTSD reactions and course. Initial PTSD reactions were assessed from models predicting a Low trajectory versus any other trajectory, and a Low trajectory versus a High trajectory. Factors affecting PTSD course were assessed from models of a Low trajectory versus a Delayed trajectory, and a High trajectory versus a Remitting trajectory. Model fit was evaluated using Efron’s R2, the Brier Score, and the Area Under the Receiver of the Receiver Operating Characteristic (AUC).
Fourth, a series of supplementary analyses was conducted. Multivariable logistic regressions were repeated leaving one study out at a time to assess whether individual studies influenced the relationships between predictors and trajectories. Subsequently, two multivariable multinomial logistic regressions compared predictors’ effects on initial PTSD reactions and course. First, a model predicting the Delayed and High trajectories versus the Low trajectory was fit to compare predictors of consistently high symptoms versus symptoms that onset later. A second model was fit predicting Low and Remitting trajectories versus the High trajectory comparing the predictors of consistently low symptoms with those that remitted over time. For both models, two multivariable multinomial logistic regressions were fit for each predictor to test the consistency of effect across outcomes. Predictors were first constrained to be equal across both outcomes and in the second regression predictors could vary by outcome. A likelihood ratio test was then used to compare model fits and indicate whether predictors’ effects varied by outcome.
Results
Descriptive Statistics
Table 1 shows descriptive statistics for predictor variables. Significant variation was found across age quartiles (, p < .001), gender (, p < .001), education (, p < .001), and marital status (, p < .001). Rates of prior non-interpersonal (27.7–43.7%) and interpersonal trauma (24.7–59.5%) ranged across studies with prior trauma not assessed in the Zurich ICU study (, p < .001). White participants made up a majority of five studies except for TCOM where 100% of the participants were non-white (, p < .001). Significant differences in index trauma type were reported across studies as two studies (TCOM and Ohio-MVA) recruited motor vehicle accidents (, p < .001). Significant differences in mean CAPS severity across studies were found for three time points: <1 month (F1 = 4.49, p = .034), 1 month (F3 = 340.39, p < .001), and 6 months (F4 = 27.27 p < .001).
Table 1.
Descriptive Data for Included Studies and the Pooled ICPP Dataset
| Variable | Multisite ASD | JTOPS | TCOM | Ohio-MVA | Zurich ICU | Amsterdam Cortisol | ICPP | χ2df; p-value |
|---|---|---|---|---|---|---|---|---|
| Age Quartile | χ215=122.89 | |||||||
| <27 | 272 (26.1%) | 181 (24.6%) | 59 (33.9%) | 87 (30.4%) | 36 (29.8%) | 119 (16.4%) | 754 (24.5%) | p < .001 |
| 27–37 | 231 (22.2%) | 263 (35.8%) | 39 (22.4%) | 52 (18.2%) | 24 (19.8%) | 180 (24.8%) | 789 (25.6%) | |
| 38–48 | 283 (27.2%) | 146 (19.9%) | 28 (16.1%) | 81 (28.3%) | 29 (24%) | 179 (24.7%) | 746 (24.2%) | |
| >48 | 255 (24.5%) | 145 (19.7%) | 48 (27.6%) | 66 (23.1%) | 32 (26.4%) | 248 (34.2%) | 794 (25.8%) | |
| Gender | χ25=105.1 | |||||||
| Male | 761 (73.1%) | 379 (51.6%) | 126 (72.4%) | 163 (57%) | 91 (75.2%) | 462 (63.6%) | 1982 (64.3%) | p <.001 |
| Female | 280 (26.9%) | 356 (48.4%) | 48 (27.6%) | 123 (43%) | 30 (24.8%) | 264 (36.4%) | 1101 (35.7%) | |
| Race | χ210=1707.19 | |||||||
| White | 622 (59.8%) | 735 (100%) | 0 (0%) | 262 (91.6%) | 99 (81.8%) | 650 (89.5%) | 2368 (76.8%) | p <.001 |
| Non-White | 69 (6.6%) | 0 (0%) | 174 (100%) | 23 (8%) | 0 (0%) | 64 (8.8%) | 330 (10.7%) | |
| Missing | 350 (33.6%) | 0 (0%) | 0 (0%) | 1 (0.3%) | 22 (18.2%) | 12 (1.7%) | 385 (12.5%) | |
| Education | χ210=233.68 | |||||||
| Secondary or Greater | 692 (66.5%) | 594 (80.8%) | 139 (79.9%) | 261 (91.3%) | 105 (86.8%) | 569 (78.4%) | 2360 (76.5%) | p <.001 |
| Less than Secondary | 234 (22.5%) | 86 (11.7%) | 35 (20.1%) | 24 (8.4%) | 16 (13.2%) | 152 (20.9%) | 547 (17.7%) | |
| Missing | 115 (11%) | 55 (7.5%) | 0 (0%) | 1 (0.3%) | 0 (0%) | 5 (0.7%) | 176 (5.7%) | |
| Marital Status | χ210=188.05 | |||||||
| Married/living with partner | 459 (44.1%) | 343 (46.7%) | 77 (44.3%) | 120 (42%) | 52 (43%) | 393 (54.1%) | 1444 (46.8%) | p <.001 |
| Single/not living with partner | 476 (45.7%) | 337 (45.9%) | 97 (55.7%) | 165 (57.7%) | 69 (57%) | 332 (45.7%) | 1476 (47.9%) | |
| Missing | 106 (10.2%) | 55 (7.5%) | 0 (0%) | 1 (0.3%) | 0 (0%) | 1 (0.1%) | 163 (5.3%) | |
| Prior Trauma | χ215=1104.56 | |||||||
| No prior trauma | 133 (12.8%) | 195 (26.5%) | 38 (21.8%) | 15 (5.2%) | 0 (0%) | 90 (12.4%) | 471 (15.3%) | p <.001 |
| Prior non-interpersonal trauma | 288 (27.7%) | 234 (31.8%) | 76 (43.7%) | 120 (42%) | 0 (0%) | 278 (38.3%) | 996 (32.3%) | |
| Prior interpersonal trauma | 619 (59.5%) | 224 (30.5%) | 43 (24.7%) | 127 (44.4%) | 0 (0%) | 357 (49.2%) | 1370 (44.4%) | |
| Missing | 1 (0.1%) | 82 (11.2%) | 17 (9.8%) | 24 (8.4%) | 121 (100%) | 1 (0.1%) | 246 (8%) | |
| Trauma Type | χ210=558.12 | |||||||
| MVA | 674 (64.7%) | 604 (82.2%) | 174 (100%) | 286 (100%) | 75 (62%) | 476 (65.6%) | 2289 (74.2%) | p <.001 |
| Other accidents | 310 (29.8%) | 41 (5.6%) | 0 (0%) | 0 (0%) | 46 (38%) | 218 (30%) | 615 (19.9%) | |
| Assaults (intentional harm) | 57 (5.5%) | 90 (12.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 32 (4.4%) | 179 (5.8%) | |
| Mean CAPS Severity (SD) | Fdf, p-value | |||||||
| <1 month | 18.12 (16.81) | 21.5 (15.14) | 18.47 (16.67) | F1 = 4.49, p =.034 | ||||
| 1 month | 56.77 (25.14) | 19.71 (17.64) | 26.02 (21.24) | 22.04 (19.98) | 36.74 (27.89) | F3 = 340.39, p < .001 | ||
| 3 months | 20.25 (20.88) | 18.53 (17.71) | 19.84 (20.18) | F1 = 1.55 p = .214 | ||||
| 6 months | 29.33 (25.77) | 15.64 (16.13) | 20.21 (19.21) | 14.79 (13.84) | 17.93 (18.84) | 22.47 (22.27) | F4 = 27.27 p < .001 | |
| 9 months | 31.51 (26.73) | 31.51 (26.73) | N/A | |||||
| 1 year | 19.03 (21.91) | 16.88 (20.96) | 18.56 (19.64) | 16.69 (15.12) | 15.69 (17.23) | 17.84 (20.07) | F4 = 2.04 p = .086 | |
Note. df = degrees of freedom; CAPS = Clinician-Administered PTSD Scale; SD = Standard Deviation;
Latent Class Growth Analysis
Statistical information on all of the LCGA models examined for each dataset are provided in Supplemental Tables 1–6. The number and percentage in each trajectory across studies from the four-class solution are presented in Table 2. A Low trajectory and High trajectory were common to all six studies. Moderate-low and Fast Remitting trajectories were only found in one study each. Participants in these trajectories were combined with those in the Moderate and Remitting categories, respectively, resulting in five unique trajectories. Supplemental Table 7 provides growth terms and descriptive data for participants with most likely membership in each trajectory from each dataset. Observed means for each dataset and the pooled sample are plotted in Figure 1.
Table 2.
Number of participants in each trajectory and the percentage each trajectory encompasses in each individual study and the pooled ICPP dataset.
| Trajectory | Multisite ASD | JTOPS | TCOM | Ohio-MVA | Zurich ICU | Amsterdam Cortisol | ICPP |
|---|---|---|---|---|---|---|---|
| Low | 750 (72%) | 292 (40%) | 137 (79%) | 229 (80%) | 88 (73%) | 491 (68%) | 1987 (64%) |
| Moderate-Low | - | - | - | - | - | 153 (21%) | - |
| Moderate | - | - | - | - | - | 54 (7%) | 207 (7%) |
| Remitting | 86 (8%) | 139 (19%) | 25 (14%) | 23 (8%) | 19 (16%) | - | 521 (17%) |
| Fast remitting | - | 229 (31%) | - | - | - | - | - |
| High | 63 (6%) | 75 (10%) | 6 (3%) | 18 (6%) | 9 (7%) | 28 (4%) | 199 (6%) |
| Delayed | 142 (14%) | - | 6 (3%) | 16 (6%) | 5 (4%) | - | 169 (5%) |
| N | 1041 (34%) | 735 (24%) | 174 (6%) | 286 (9%) | 121 (4%) | 726 (24%) | 3083 (100%) |
Figure 1.
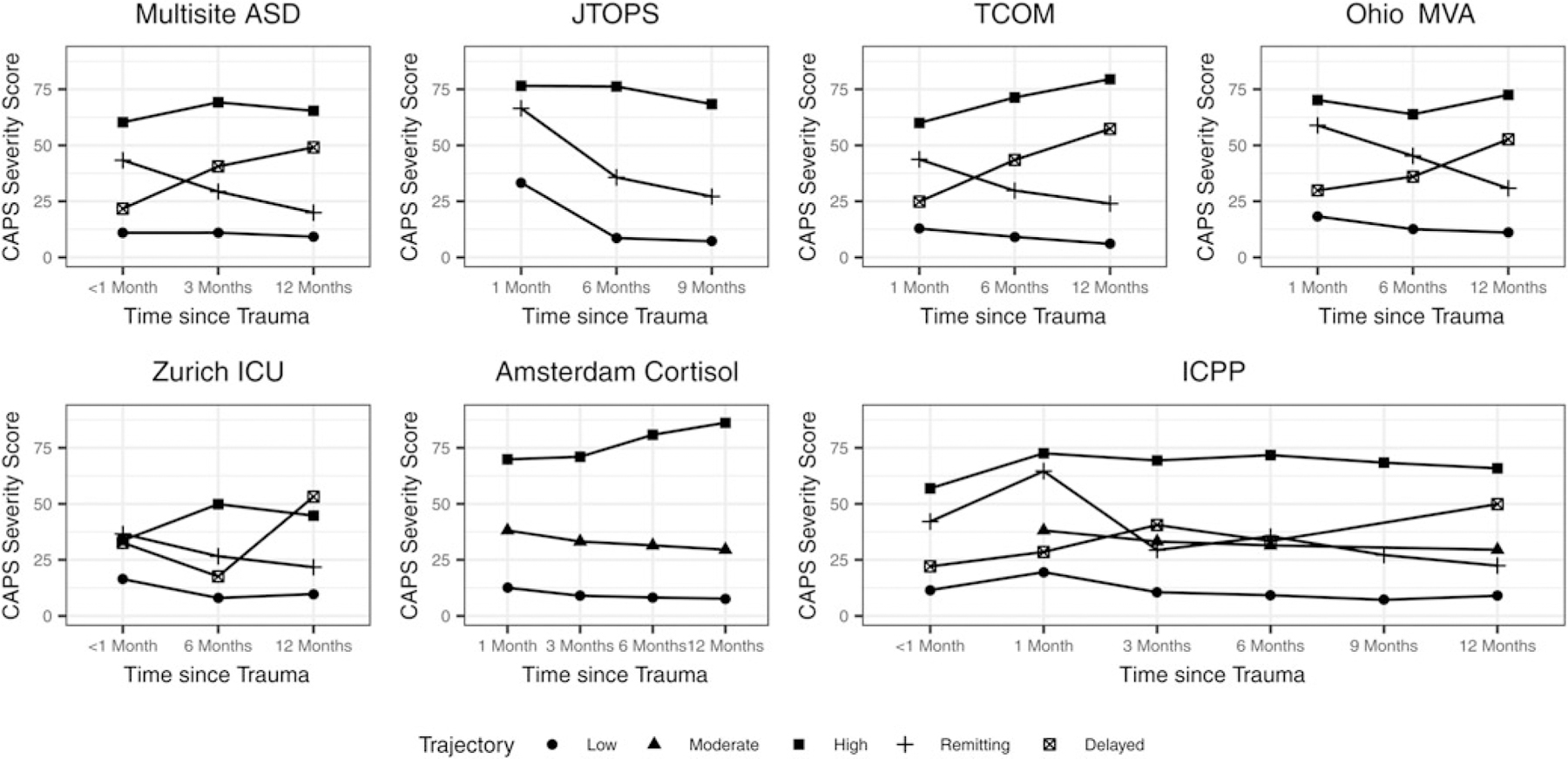
Plot of estimated mean values at each time point for trajectories from the four-class latent growth analysis. In JTOPS, the Fast-remitting and Remitting categories were combined and in the Amsterdam Cortisol study the Moderate-low and Moderate categories were combined. CAPS = Clinician-Administered PTSD Scale.
Table 3 shows the descriptive data for participants in each of the five trajectories for the pooled dataset. Significant differences were found across age quartiles (, p < .001), gender (, p < .001), race (, p <.001), education (, p < .001), marital status (, p <.001), prior interpersonal trauma (, p < .001), and index trauma (, p < .001).
Table 3.
Number of participants and the percentage encompassed in each predictor category across trajectories and in the pooled ICPP dataset.
| Variable | Low | Moderate | Remitting | High | Delayed | ICPP | χ2df; p-value |
|---|---|---|---|---|---|---|---|
| Age Quartile | χ212=61.46 | ||||||
| <27 | 501 (25.2%) | 29 (14%) | 145 (27.8%) | 37 (18.6%) | 42 (24.9%) | 754 (24.5%) | p < .001 |
| 27–37 | 476 (24%) | 60 (29%) | 158 (30.3%) | 59 (29.6%) | 36 (21.3%) | 789 (25.6%) | |
| 38–48 | 451 (22.7%) | 58 (28%) | 114 (21.9%) | 65 (32.7%) | 58 (34.3%) | 746 (24.2%) | |
| >48 | 559 (28.1%) | 60 (29%) | 104 (20%) | 38 (19.1%) | 33 (19.5%) | 794 (25.8%) | |
| Gender | χ24=112.29 | ||||||
| Male | 1400 (70.5%) | 110 (53.1%) | 258 (49.5%) | 98 (49.2%) | 116 (68.6%) | 1982 (64.3%) | p < .001 |
| Female | 587 (29.5%) | 97 (46.9%) | 263 (50.5%) | 101 (50.8%) | 53 (31.4%) | 1101 (35.7%) | |
| Race | χ28=64.09 | ||||||
| White | 1491 (75%) | 175 (84.5%) | 441 (84.6%) | 147 (73.9%) | 114 (67.5%) | 2368 (76.8%) | p < .001 |
| Non-White | 233 (11.7%) | 26 (12.6%) | 34 (6.5%) | 21 (10.6%) | 16 (9.5%) | 330 (10.7%) | |
| Missing | 263 (13.2%) | 6 (2.9%) | 46 (8.8%) | 31 (15.6%) | 39 (23.1%) | 385 (12.5%) | |
| Education | χ28=74.02 | ||||||
| Secondary or Greater | 1542 (77.6%) | 172 (83.1%) | 404 (77.5%) | 118 (59.3%) | 124 (73.4%) | 2360 (76.5%) | p < .001 |
| Less than Secondary | 361 (18.2%) | 33 (15.9%) | 72 (13.8%) | 55 (27.6%) | 26 (15.4%) | 547 (17.7%) | |
| Missing | 84 (4.2%) | 2 (1%) | 45 (8.6%) | 26 (13.1%) | 19 (11.2%) | 176 (5.7%) | |
| Marital Status | χ28=54.73 | ||||||
| Married/living with partner | 953 (48%) | 107 (51.7%) | 222 (42.6%) | 90 (45.2%) | 72 (42.6%) | 1444 (46.8%) | p < .001 |
| Single/not living with partner | 953 (48%) | 100 (48.3%) | 252 (48.4%) | 88 (44.2%) | 83 (49.1%) | 1476 (47.9%) | |
| Missing | 81 (4.1%) | 0 (0%) | 47 (9%) | 21 (10.6%) | 14 (8.3%) | 163 (5.3%) | |
| Prior Trauma | χ212=156.09 | ||||||
| No prior trauma | 297 (14.9%) | 18 (8.7%) | 115 (22.1%) | 19 (9.5%) | 22 (13%) | 471 (15.3%) | p <.001 |
| Prior non-interpersonal trauma | 700 (35.2%) | 70 (33.8%) | 150 (28.8%) | 45 (22.6%) | 31 (18.3%) | 996 (32.3%) | |
| Prior interpersonal trauma | 848 (42.7%) | 119 (57.5%) | 182 (34.9%) | 111 (55.8%) | 110 (65.1%) | 1370 (44.4%) | |
| Missing | 142 (7.1%) | 0 (0%) | 74 (14.2%) | 24 (12.1%) | 6 (3.6%) | 246 (8%) | |
| Trauma Type | χ28=124.83 | ||||||
| MVA | 1449 (72.9%) | 153 (73.9%) | 415 (79.7%) | 143 (71.9%) | 129 (76.3%) | 2289 (74.2%) | p <.001 |
| Other accidents | 472 (23.8%) | 41 (19.8%) | 54 (10.4%) | 22 (11.1%) | 26 (15.4%) | 615 (19.9%) | |
| Assaults (intentional harm) | 66 (3.3%) | 13 (6.3%) | 52 (10%) | 34 (17.1%) | 14 (8.3%) | 179 (5.8%) | |
Note. df = degrees of freedom
Predicting Trajectory Membership
Table 4 summarizes the results of the initial PTSD reactions and course prediction models.
Table 4.
Results of Models Predicting Trajectory Membership for Initial PTSD Reaction Models and PTSD Course Models (OR [95% CI]).
| Variables | Initial PTSD Reaction Models | PTSD Course Models | ||
|---|---|---|---|---|
| All Other (1) vs. Low (0) | High (1) vs. Low (0) | Delayed (1) vs. Low (0) | High (1) vs. Remitting (0) | |
| Intercept | 0.17*** [0.12–0.24] | 0.01*** [0–0.02] | 0.17*** [0.09–0.32] | 0.21* [0.08–0.54] |
| Age Quartile | ||||
| 27–37 | 1.15 [0.91–1.45] | 1.65* [1.03–2.65] | 1.14 [0.69–1.89] | 1.63 [0.93–2.84] |
| 38–48 | 1.49* [1.17–1.91] | 2.38** [1.46–3.87] | 1.67* [1.04–2.69] | 2.26* [1.27–4.04] |
| >48 | 0.92 [0.71–1.18] | 0.96 [0.56–1.66] | 0.96 [0.56–1.64] | 1.81 [0.96–3.39] |
| Difference | χ23=19.71; p < .001 | χ23=20.71; p < .001 | χ23=7.28; p = .064 | χ23=7.7; p = .053 |
| Gender | ||||
| Female | 2*** [1.69–2.36] | 2.63*** [1.9–3.65] | 1.56* [1.07–2.27] | 1.14 [0.78–1.68] |
| Difference | χ21=64.91; p < .001 | χ21=33.48; p < .001 | χ21=5.36; p = .021 | χ21=0.45; p = .504 |
| Race | ||||
| Non-White | 1.6* [1.12–2.3] | 2.66* [1.38–5.12] | 0.83 [0.4–1.72] | 0.96 [0.28–3.27] |
| Missing | 1.19 [0.88–1.61] | 1.38 [0.78–2.44] | 0.74 [0.46–1.19] | 0.69 [0.34–1.4] |
| Difference | χ22=7.29; p = .026 | χ22=9.02; p = .011 | χ22=1.66; p = .437 | χ22=1.08; p = .584 |
| Education | ||||
| Less than Secondary | 1.16 [0.93–1.43] | 2.83*** [1.93–4.15] | 0.72 [0.45–1.16] | 1.89* [1.16–3.09] |
| Missing | 2.05* [1.19–3.55] | 4.59* [1.84–11.46] | 2.37 [0.95–5.92] | 2.89 [0.99–8.49] |
| Difference | χ22=7.92; p = .019 | χ22=34.83; p < .001 | χ22=5.7; p = .058 | χ22=9.19; p = .01 |
| Marital Status | ||||
| Single/not living with partner | 1.07 [0.89–1.28] | 0.95 [0.66–1.36] | 1.03 [0.71–1.51] | 0.77 [0.49–1.2] |
| Missing | 0.94 [0.52–1.71] | 0.81 [0.28–2.35] | 0.62 [0.21–1.87] | 0.64 [0.2–2.05] |
| Difference | χ22=0.59; p = .745 | χ22=0.19; p = .91 | χ22=0.84; p = .657 | χ22=1.68; p = .432 |
| Prior Trauma | ||||
| Prior non-interpersonal | 1.01 [0.78–1.3] | 1.54 [0.84–2.8] | 0.59 [0.32–1.07] | 1.71 [0.87–3.37] |
| Prior interpersonal | 1.65*** [1.29–2.12] | 3.2*** [1.83–5.61] | 1.33 [0.8–2.24] | 2.57* [1.34–4.93] |
| Missing | 1.88* [1.17–3.03] | 3.54* [1.44–8.66] | 0.44 [0.05–3.54] | 1.73 [0.69–4.29] |
| Difference | χ23=35.19; p < .001 | χ23=26.05; p < .001 | χ23=14.49; p = .002 | χ23=8.61; p = .035 |
| Trauma Type | ||||
| Other accidents | 0.65** [0.52–0.81] | 0.61 [0.37–1.02] | 0.49* [0.31–0.79] | 0.55 [0.28–1.08] |
| Assaults (intentional harm) | 2.31*** [1.65–3.25] | 4.74*** [2.86–7.85] | 2.67* [1.32–5.4] | 2.09* [1.17–3.71] |
| Difference | χ22=42.05; p < .001 | χ22=44.06; p < .001 | χ22=18.55; p < .001 | χ22=10.48; p < .001 |
| Study | ||||
| JTOPS | 3.94*** [3.07–5.06] | 4.03*** [2.45–6.61] | - | 0.27*** [0.15–0.49] |
| TCOM | 0.56* [0.33–0.94] | 0.39 [0.13–1.16] | 0.31* [0.11–0.94] | 0.35 [0.08–1.55] |
| Ohio-MVA | 0.61* [0.43–0.87] | 1.22 [0.64–2.33] | 0.32** [0.18–0.58] | 1.12 [0.5–2.54] |
| Zurich ICU | 0.92 [0.49–1.73] | 1.77 [0.57–5.47] | 0.83 [0.09–7.78] | 0.98 [0.29–3.39] |
| Amsterdam Cortisol | 1.42* [1.13–1.8] | 0.92 [0.54–1.56] | - | - |
| Difference | χ25=187.15; p < .001 | χ25=46.75; p < .001 | χ25=17.52; p = .004 | χ25=30.39; p < .001 |
| N | 3083 | 2186 | 2156 | 720 |
| Efron’s R2 | 0.15 | 0.14 | 0.12 | 0.24 |
| Brier | 0.2 | 0.07 | 0.06 | 0.15 |
| AUC | 0.73 | 0.79 | 0.83 | 0.77 |
Note:
p < .05
p < .01
p < .001;
AUC = Area Under the Curve of the Receiver Operator Characteristic.
Initial PTSD reaction models.
Logistic regression predicting Any Other trajectory versus the Low trajectory found that third quartile of age (OR = 1.49, 95% CI: 1.17–1.91), female gender (OR = 2.00, 95% CI: 1.69–2.36), non-white race (OR = 1.6, 95% CI: 1.12–2.30), prior interpersonal trauma (OR = 1.65, 95% CI: 1.29–2.12), and experiencing an assault as the index trauma (OR = 2.31, 95% CI: 1.65–3.25) increased the risk for being in Any Other trajectory, while experiencing a non-MVA accident decreased risk (OR = 0.65, 95% CI: 0.52–0.81). Descriptive statistics for the All Other trajectories versus Low trajectory are available in Supplemental Table 8.
For the PTSD onset model of High versus Low trajectories a similar pattern was found with second (OR = 1.65, 95% CI: 1.03–2.65) and third quartile of age (OR = 2.38, 95% CI: 1.46 −3.87), female gender (OR = 2.63, 95% CI: 1.90–3.65), non-white race (OR = 2.66, 95% CI: 1.38–5.12), having less than a secondary education (OR = 2.83, 95% CI: 1.93–4.15), prior interpersonal trauma (OR = 3.20, 95% CI: 1.83–5.61), and experiencing an assault as the index trauma (OR = 4.74, 95% CI: 2.86–7.85) increasing the risk for being in the High trajectory.
PTSD course models.
Female gender increased risk for being in the Delayed versus the Low trajectory (OR = 1.56, 95% CI: 1.07–2.27), as did experiencing an assault (OR = 2.67, 95% CI: 1.32–5.40), while experiencing a non-MVA accident decreased risk (OR = 0.49, 95% CI: 0.31–0.79). Prior trauma experience was overall statistically significant (p = .002), although no specific trauma type was individually predictive. Descriptive statistics for the Low versus Delayed trajectories are available in Supplemental Table 9.
In the High versus Remitting model, having less than a secondary education (1.89, 95% CI: 1.16–3.09), prior interpersonal trauma (OR=2.57, 95% CI: 1.34–4.93), and experiencing an assault (OR=2.09, 95% CI: 1.17–3.71) increased risk for being in the High trajectory. Descriptive statistics for the High versus Remitting analysis are available in Supplemental Table 10.
Supplementary Analyses
Across all models, study dummy variables were significant indicating differences existed in the prevalence of the outcome trajectories. Logistic regressions without each study were concordant with the pooled results (see Supplemental Figures 1–3).
Results from the multinomial regression found all predictors were significantly stronger predictors of initial PTSD onset compared to course of PTSD symptoms (p<.001; see Supplemental Tables 11 and 12).
Discussion
The current study included data from six studies of hospital admissions for civilian-related injuries, evaluating initial PTSD reactions and the course of PTSD symptoms over the first post-trauma year. Based on previous research, we first examined four-class trajectory models for the six studies. Consistently low and consistently high symptom trajectories were found across all studies, whereas other trajectories (e.g., recovery, moderate, delayed) were not. When we pooled data from the six studies, initial PTSD reaction models showed that female gender, non-white race, prior interpersonal trauma, and assaultive injuries were robust risk factors for initial PTSD reactions. In PTSD course models, female gender and assaultive injuries increased the risk of membership in the Delayed versus Low trajectory group. Among those with initially high symptoms, lower education, prior interpersonal trauma, and assaultive injuries increased risk of membership in the High versus Remitting trajectory group.
Our examination of prototypical patterns of trajectories revealed that consistently low and consistently high PTSD symptoms are robust post-trauma trajectories. These findings align with a large body of literature documenting the presence of these trajectories among people who have been exposed to potentially traumatic events (Galatzer-Levy et al., 2018). Results suggest that practitioners working with injury survivors can expect that a majority of survivors will report consistently low symptoms over the first year, while a minority of survivors will report consistently high symptoms over the first year.
On the other hand, other trajectories, including a Remitting trajectory, were not apparent across studies. This is in contrast to findings from the recent review of PTSD trajectories by Galatzer-Levy and colleagues (2018), which found Recovery to be the second most commonly observed trajectory across 54 studies. Galatzer-Levy and colleagues noted that substantive differences in populations (e.g., police force workers versus civilians) were associated with heterogeneity in their estimates. However, for the current study it is less likely, although not impossible, that substantive population differences are the reason we observed heterogeneity in estimates. This is because a major strength of this study is the inclusion of data from similar populations (i.e., those presenting at hospitals for civilian related injuries). Instead, it seems more likely that inconsistent findings in this study may be due to contextual factors such as comorbid symptoms, developmental stage, social network characteristics, physical health, or coping styles (Bonanno et al., 2015, Fan et al., 2015, Galatzer-Levy et al., 2018, Lai et al., 2013).
One notable caveat when interpreting the pooled results is that one of the studies (JTOPS) had markedly different proportions of participants with most likely membership in each trajectory than the other five studies. For example, the percentage of participants in the Low trajectory for JTOPS was 40%, compared to 68–80% across the other studies. This is likely due to JTOPS having distinctive inclusion criteria – namely, that eligible participants were required to meet DSM-IV PTSD Criterion A and have acute stress symptoms upon enrollment. This discrepancy illuminates how systematic differences in sampling even within the same trauma context can influence the nature and proportion of PTSS trajectories. The pooled proportion for the Low trajectory is therefore likely an underestimate for the population of adult survivors of civilian-related injuries admitted to EDs, whereas the pooled proportions for the trajectories in JTOPS characterized by temporary or chronic symptom elevations (Remitting, Fast remitting, and High) are likely overestimates.
When we evaluated risk factors for initial PTSD reactions, the risk factors we identified (i.e., female gender, non-white race, prior interpersonal trauma, and assault) were consistent with prior research (Bryant et al., 2015, Fink et al., 2017, Sripada et al., 2017). These findings suggest that these risk factors should be included in prediction tools to identify survivors at risk for initially high levels of PTSD symptoms as part of routine post-injury psychiatric evaluations.
PTSD course models provided initial evidence that female gender and assaultive injury differentiated between those who were more likely to report delayed symptoms, versus consistently low symptoms. This again provides suggestions for survivors that should be targeted for follow-up. It is unclear why these particular risk factors are important. It is possible female gender may represent other factors, such as women’s greater use of alcohol to cope with PTSD symptoms and gender-related psychobiological stress responses (Olff et al., 2007), that confer risk for delayed reactions. These findings may also represent gender differences in exposure to intervening trauma. For example, female participants might have been more likely to experience interpersonal violence over the course of the studies, thereby heightening their risk for delayed PTSD symptoms (Benjet et al., 2016; McLaughlin et al., 2013). In a similar vein, injuries due to assaultive violence might have been more likely than those due to motor vehicle or other accidents to yield secondary stressors, such as difficulties in social relationships, legal problems, and economic strain, thereby increasing risk for delayed PTSD (Lowe et al., 2017). These are issues that warrant further study.
Finally, several risk factors distinguished between with consistently high versus recovering symptoms. In particular, lower education, prior interpersonal trauma, and assault were predictors of chronic responses. These findings are consistent with prior findings identifying low education and prior interpersonal trauma as risk factors for more symptomatic trajectories (Muzik et al., 2016, Pietrzak et al., 2014). Perhaps most notable were the findings related to assault. Although this finding is consistent with prior research showing assaultive violence to be associated with increased risk for PTSD, relative to other types of trauma (McLaughlin et al., 2013), only one trajectory study to our knowledge has explored whether assaultive trauma is associated with membership in chronically symptomatic trajectories (Lowe et al., 2014). This study, however, did not look at PTSD symptom trajectories in the context of civilian-related injuries in EDs, but rather examined them among urban residents who each reported on symptoms in reference to their self-identified worst trauma from an inventory of potentially traumatic events.
Our findings, in contrast, suggest that, within the context of civilian-related injuries, the nature of the exposure is predictive of trajectory membership, and reflect the importance of identifying trauma-related characteristics that confer risk for distressed trajectories. More generally, the results regarding risk and protective factors are particularly important given their relevance for tiered intervention strategies. As this study focused on civilian trauma, results suggest that providers of psychological services in emergency departments should be mindful of these risk factors, especially in the presence of moderate-to-high levels of initial PTSD symptom presentation. The findings suggest that people in these groups may be particularly vulnerable to persistent symptoms and thus should be targets of outreach efforts.
Several limitations should be considered in interpreting these results. First, although pooling data was a strength of our analysis, variability across the individual studies, including in the timing of assessments and number of cases, could have influenced patterns of results. We accounted for these differences by controlling for source of the data in predictive analyses and replicating analyses excluding one dataset at a time. Second, there was systematically missing data in our predictive analyses, limiting the extent to which our results generalize to the full population of injury survivors. Third, we were only able to study predictors that were assessed across studies. Researchers should work toward developing common batteries for post-trauma research, which would facilitate pooled analyses in the future. Studies should in particular include assessments of pre-trauma psychopathology, which prior work has shown to be a robust predict of PTSD symptoms (DiGangi et al., 2013). Fourth, the studies in the pooled analyses included multiple cultural contexts. Although this increases the generalizability of the study, this approach assumes that PTSD symptom trajectories are a cross-cultural phenomenon. Fifth, this study focused on the first year after traumatic events. Although we consider this first year particularly important in planning intervention and assessment, this decision may have prevented us from capturing patterns that only emerge over a longer period of time. Finally, we included all participants in the analysis, regardless of their initial symptom severity. Although this maximized statistical power and made our findings more generalizable to the population of civilians who present to emergency departments with injuries, it is likely that some participants would not consider their injuries to be traumatic and that a different pattern of results would have emerged had we focused on only those participants who surpassed a certain threshold of baseline distress. Further analyses of these data will explore the latter possibility, providing insight into PTSD symptom trajectories among the population of initially symptomatic injury survivors.
Despite these limitations, the results provide important information about the form and course of PTSD trajectories, and the factors that are associated with both initial PTSD reactions and the course of symptoms over the first post-trauma year. The findings highlight the diversity of responses to potentially traumatic events and the need for researchers and clinicians to approach assessment and treatment with this heterogeneity in mind. Yet, important questions remain. Future research is needed that examines injury across the lifespan to understand the degree to which trajectories may differ by stage of development. In addition, studies with longer follow-up periods and various types of trauma exposure will enable us to understand whether trajectories may change across the post-trauma period or across types of trauma.
Supplementary Material
Acknowledgements:
This work was supported by the National Institute of Mental Health (award number R01MH101227) to A. Shalev, R. Kessler and K. Koenen.
Footnotes
Conflicts of Interest: None.
References
- Andruff H, Carraro N, Thompson A, Gaudreau P & Louvet B (2009). Latent class growth modelling: a tutorial. Tutorials in Quantitative Methods for Psychology 5, 11–24. [Google Scholar]
- Berntsen D, Johannessen KB, Thomsen YD, Bertelsen M, Hoyle RH & Rubin DC (2012). Peace and war: Trajectories of posttraumatic stress disorder symptoms before, during, and after military deployment in Afghanistan. Psychological science 23, 1557–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS & Keane TM (1995). The development of a clinician-administered PTSD scale. Journal of traumatic stress 8, 75–90. [DOI] [PubMed] [Google Scholar]
- Boasso AM, Steenkamp MM, Nash WP, Larson JL & Litz BT (2015). The relationship between course of PTSD symptoms in deployed US Marines and degree of combat exposure. Journal of traumatic stress 28, 73–78. [DOI] [PubMed] [Google Scholar]
- Bonanno GA & Diminich ED (2013). Annual Research Review: Positive adjustment to adversity–trajectories of minimal–impact resilience and emergent resilience. Journal of Child Psychology and Psychiatry 54, 378–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA, Kennedy P, Galatzer-Levy IR, Lude P & Elfström ML (2012). Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabilitation psychology 57, 236. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Romero SA & Klein SI (2015). The temporal elements of psychological resilience: An integrative framework for the study of individuals, families, and communities. Psychological Inquiry 26, 139–169. [Google Scholar]
- Bryant RA, Creamer M, O’Donnell ML, Silove D & McFarlane AC (2008). A multisite study of the capacity of acute stress disorder diagnosis to predict posttraumatic stress disorder. The Journal of clinical psychiatry. [DOI] [PubMed]
- Bryant RA, Nickerson A, Creamer M, O’donnell M, Forbes D, Galatzer-Levy I, McFarlane AC & Silove D (2015). Trajectory of post-traumatic stress following traumatic injury: 6-year follow-up. The British Journal of Psychiatry 206, 417–423. [DOI] [PubMed] [Google Scholar]
- Delahanty DL, Raimonde AJ, Spoonster E & Cullado M (2003). Injury severity, prior trauma history, urinary cortisol levels, and acute PTSD in motor vehicle accident victims. Journal of anxiety disorders 17, 149–164. [DOI] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Mancini AD, Rusch MD & Bonanno GA (2010). Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabilitation psychology 55, 1. [DOI] [PubMed] [Google Scholar]
- Dickstein BD, Suvak M, Litz BT & Adler AB (2010). Heterogeneity in the course of posttraumatic stress disorder: trajectories of symptomatology. Journal of traumatic stress 23, 331–339. [DOI] [PubMed] [Google Scholar]
- Fan F, Long K, Zhou Y, Zheng Y & Liu X (2015). Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychological medicine 45, 2885–2896. [DOI] [PubMed] [Google Scholar]
- Fink DS, Lowe S, Cohen GH, Sampson LA, Ursano RJ, Gifford RK, Fullerton CS & Galea S (2017). Trajectories of posttraumatic stress symptoms after civilian or deployment traumatic event experiences. Psychological Trauma: Theory, Research, Practice, and Policy 9, 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Ankri Y, Freedman S, Israeli-Shalev Y, Roitman P, Gilad M & Shalev AY (2013). Early PTSD symptom trajectories: persistence, recovery, and response to treatment: results from the Jerusalem Trauma Outreach and Prevention Study (J-TOPS). PloS one 8, e70084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Huang SH & Bonanno GA (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical psychology review 63, 41–55. [DOI] [PubMed] [Google Scholar]
- Hepp U, Moergeli H, Buchi S, Bruchhaus-Steinert H, Kraemer B, Sensky T & Schnyder U (2008). Post-traumatic stress disorder in serious accidental injury: 3-year follow-up study. The British Journal of Psychiatry 192, 376–383. [DOI] [PubMed] [Google Scholar]
- Holgersen KH, Klöckner CA, Jakob Boe H, Weisæth L & Holen A (2011). Disaster survivors in their third decade: Trajectories of initial stress responses and long-term course of mental health. Journal of traumatic stress 24, 334–341. [DOI] [PubMed] [Google Scholar]
- Hovens J, Van der Ploeg H, Klaarenbeek M, Bramsen I, Schreuder J & Rivero VV (1994). The assessment of posttraumatic stress disorder: with the Clinician Administered PTSD Scale: Dutch results. Journal of clinical psychology 50, 325–340. [DOI] [PubMed] [Google Scholar]
- Jung T & Wickrama K (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and personality psychology compass 2, 302–317. [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV & Ferry F (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology 8, 1353383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of general psychiatry 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Lai BS, La Greca AM, Auslander BA & Short MB (2013). Children’s symptoms of posttraumatic stress and depression after a natural disaster: Comorbidity and risk factors. Journal of affective disorders 146, 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe SR, Blachman-Forshay J & Koenen KC (2015). Trauma as a public health issue: Epidemiology of trauma and trauma-related disorders. In Evidence based treatments for trauma-related psychological disorders, pp. 11–40. Springer. [Google Scholar]
- Lowe SR, Galea S, Uddin M & Koenen KC (2014). Trajectories of posttraumatic stress among urban residents. American journal of community psychology 53, 159–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuoka Y, Nishi D, Nakajima S, Yonemoto N, Hashimoto K, Noguchi H, Homma M, Otomo Y & Kim Y (2009). The Tachikawa cohort of motor vehicle accident study investigating psychological distress: design, methods and cohort profiles. Social psychiatry and psychiatric epidemiology 44, 333–340. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM & Kessler RC (2013). Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry 52, 815–830. e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouthaan J, Sijbrandij M, Luitse JS, Goslings JC, Gersons BP & Olff M (2014). The role of acute cortisol and DHEAS in predicting acute and chronic PTSD symptoms. Psychoneuroendocrinology 45, 179–186. [DOI] [PubMed] [Google Scholar]
- Muthén L & Muthén B (1998). Mplus User’s Guide, 7th Edn Los Angeles. CA: Muthén & Muthén; 2012. [Google Scholar]
- Muzik M, McGinnis EW, Bocknek E, Morelen D, Rosenblum KL, Liberzon I, Seng J & Abelson JL (2016). PTSD symptoms across pregnancy and early postpartum among women with lifetime PTSD diagnosis. Depression and anxiety 33, 584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash WP, Boasso AM, Steenkamp MM, Larson JL, Lubin RE & Litz BT (2015). Posttraumatic stress in deployed Marines: Prospective trajectories of early adaptation. Journal of Abnormal Psychology 124, 155. [DOI] [PubMed] [Google Scholar]
- Nickerson A, Aderka IM, Bryant RA & Hofmann SG (2012). The relationship between childhood exposure to trauma and intermittent explosive disorder. Psychiatry research 197, 128–134. [DOI] [PubMed] [Google Scholar]
- Norris FH, Tracy M & Galea S (2009). Looking for resilience: Understanding the longitudinal trajectories of responses to stress. Social science & medicine 68, 2190–2198. [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N & Gersons BP (2007). Gender differences in posttraumatic stress disorder. Psychological bulletin 133, 183. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz C, Reissman D, Ozbay F, Sharma V & Crane M (2014). Trajectories of PTSD risk and resilience in World Trade Center responders: an 8-year prospective cohort study. Psychological Medicine 44, 205–219. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Van Ness PH, Fried TR, Galea S & Norris FH (2013). Trajectories of posttraumatic stress symptomatology in older persons affected by a large-magnitude disaster. Journal of psychiatric research 47, 520–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi W, Ratanatharathorn A, Gevonden M, Bryant R, Delahanty D, Matsuoka Y, Olff M, deRoon-Cassini T, Schnyder U & Seedat S (2018). Application of data pooling to longitudinal studies of early post-traumatic stress disorder (PTSD): the International Consortium to Predict PTSD (ICPP) project. European journal of psychotraumatology 9, 1476442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rui P, Kang K & Ashman J (2016). National Hospital Ambulatory Medical Care Survey: 2016 emergency department summary tables.
- Shalev AY, Ankri Y, Israeli-Shalev Y, Peleg T, Adessky R & Freedman S (2012). Prevention of posttraumatic stress disorder by early treatment: results from the Jerusalem Trauma Outreach And Prevention study. Archives of general psychiatry 69, 166–176. [DOI] [PubMed] [Google Scholar]
- Sripada RK, Pfeiffer PN, Rampton J, Ganoczy D, Rauch SA, Polusny MA & Bohnert KM (2017). Predictors of PTSD symptom change among outpatients in the US Department of Veterans Affairs Health Care System. Journal of traumatic stress 30, 45–53. [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Dickstein BD, Salters-Pedneault K, Hofmann SG & Litz BT (2012). Trajectories of PTSD symptoms following sexual assault: Is resilience the modal outcome? Journal of traumatic stress 25, 469–474. [DOI] [PubMed] [Google Scholar]
- Sveen J, Ekselius L, Gerdin B & Willebrand M (2011). A prospective longitudinal study of posttraumatic stress disorder symptom trajectories after burn injury. Journal of Trauma and Acute Care Surgery 71, 1808–1815. [DOI] [PubMed] [Google Scholar]
- Team, R. C. (2013). R: A language and environment for statistical computing.
- Van de Schoot R (2015). Latent growth mixture models to estimate PTSD trajectories. European Journal of Psychotraumatology 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM & Keane TM (1999). Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological assessment 11, 124. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


