Abstract
Postpartum weight retention (PPWR) is a factor that causes permanent obesity and subsequent chronic and noncommunicable diseases. The relationship between depression/stress/anxiety and PPWR has been studied in some articles, but there is no definitive conclusion in this regard. The present systematic review was conducted to investigate the relationship between depression/stress/anxiety and PPWR. An extensive search was performed in the PubMed, Scopus, Embase, Web of Science, Google Scholar, SID, and Magiran, Irandoc databases using Medical Subject Headings terms (or their Persian synonyms) from 2000 to 2020. Inclusion and exclusion criteria were used for articles selection. The quality of the selected articles was assessed using the Newcastle–Ottawa Scale. Out of 371 reviewed articles, 24 articles were selected. The total sample size was 51,613 (range: 49–37,127). The mean of PPWR ranged from 0.5 kg (standard deviation [SD] = 6.49) to 6.4 kg (SD = 8.5). There was a statistically significant relationship between depression/stress/anxiety and PPWR in 12 of 23, 4 of 6, and 3 of 8 studies. This review demonstrates the relationship between depression/stress/anxiety and PPWR. Time of depression/stress/anxiety assessment is an important issue, as well as different measurement tools. Prevention of the mothers’ psychological problems through educational and supportive programs may help to limit PPWR.
Keywords: Anxiety, depression, depression postpartum, gestational weight gain, postpartum weight retention, stress psychological
Introduction
Postpartum weight retention (PPWR) is defined as a difference between weight at some time after delivery and prepregnancy weight.[1,2] It has been suggested as a factor that causes permanent obesity and subsequent chronic and noncommunicable diseases.[3] Therefore, it can be a health problem for women of childbearing age. A systematic review showed that two-third of women 6 months postpartum were weight more than before pregnancy.[4] In the United Kingdom, 73% of women were overweight compared to before pregnancy,[5] as well as 75% in the United States.[6]
Psychological factors can affect PPWR influencing maternal behaviors such as physical activity, diet quality, and breastfeeding behavior.[7] Poor mental health is likely to negatively affect women's ability to engage in healthy lifestyle behaviors that reduce PPWR.[8] Depression and anxiety during pregnancy and postpartum can lead to weight gain.[9] New-onset postpartum depression is associated with more than doubling the risk of retaining at least 5 kg.[10] Stress can be a barrier for postpartum weight loss by contributing to hormonal changes that increase obesity and behaviors such as overeating.[11] Conversely, 0.1 kg of weight loss was reported for each unit increase in stress score.[12]
In a systematic review, the associations between depression/anxiety/body image and weight status 1 year after delivery were examined.[13] Another review has investigated the impact of sleep/stress/depression on PPWR.[14] The associations between anxiety and pregnancy obesity, excessive gestational weight gain, and PPWR were studied in another one.[15] Previous reviews[13,14,15] have some limitations, such as considering a time limitation for postpartum weight measurement as inclusion criteria and evaluation of only English-language articles. Furthermore, none of the previous systematic reviews evaluated the relationship between depression/stress/anxiety and PPWR at the same time. Several valuable studies have been conducted after these reviews.[9,12,16,17,18]
Given the importance of complications caused by PPWR, it is necessary to find the relationship between psychological factors and PPWR, which helps to design prevention programs of psychological problems during and after pregnancy to limit PPWR. The relationship between depression/stress/anxiety and PPWR has been studied in some articles, but there is no definitive conclusion in this regard. Conducting a systematic review investigating depression/stress/anxiety at the same time leads to achieve an overview of the relationship between these essential psychological factors and PPWR, cover the previous reviews gaps, and identify the latest definitive results. Therefore, the present systematic review, which includes Persian-language articles for the first time based on our extensive search, was designed to investigate the relationship between depression/stress/anxiety and PPWR.
Materials and Methods
This systematic review was reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.[19]
Study design and search strategy
This systematic review was designed based on the PICO; Population: The population of postpartum women, Intervention: Depression/stress/anxiety, Comparison: Absence of depression/stress/anxiety, and Outcome: PPWR. To access all published articles in English and Persian, an extensive search was performed in the PubMed, Scopus, Embase, Web of Science, Google Scholar, SID, Magiran, Irandoc databases using an appropriate combination of keywords from the Medical Subject Headings related to: “Postpartum Weight Retention;” “Depression;” “Depression, Postpartum;” “Anxiety;” and “Stress, Psychological” (or the Persian equivalent) from 2000 until the end of June 2020 by two researchers separately. Furthermore, ProQuest was searched and references of articles were reviewed. [Box 1] presents an example of the PubMed search query.
Box 1.
An example of PubMed search query
| (((“Gestational Weight Gain”[Mesh] OR “Weight Gain, Gestational”[tiab] OR “Maternal Weight Gain”[tiab] OR “Weight Gain, Maternal”[tiab] OR “Pregnancy Weight Gain”[tiab] OR “Weight Gain, Pregnancy”[tiab] OR “Postpartum Weight Retention”[tiab] OR “Weight Retention, Postpartum”[tiab]) AND ((“Anxiety”[Mesh] OR “Hypervigilance”[tiab] OR “Nervousness”[tiab] OR “Social Anxiety”[tiab] OR “Anxieties, Social”[tiab] OR “Anxiety, Social”[tiab] OR “Social Anxieties”[tiab]))) |
Selection criteria
English and Persian observational articles (cohort study, cross-sectional, case-control) that examined the relationship between depression/anxiety/stress and PPWR in 2000-2020 were included. Articles were excluded if they were not using prepregnancy/early pregnancy weight for calculating PPWR.
Data extraction
Two reviewers independently searched the databases. After removing duplication, the title and abstract of the articles were assessed in terms of inclusion and exclusion criteria. Then, the full text of the articles was reviewed, ensuring relevancy. Hence, the irrelevant articles, duplicate articles, and conference abstracts without sufficient evidence, such as presentations, were removed.
Quality assessment
To avoid bias, two reviewers independently evaluated the quality of the included articles using the Newcastle–Ottawa Scale to evaluate the quality of nonrandomized studies (Newcastle–Ottawa Cohort Scale version and modified version of it for cross-sectional studies).[20,21]
According to the Newcastle–Ottawa Cohort Scale, the minimum score is 0, and the maximum is 9. Articles with a score of 6 or higher were considered low risk and good quality, and those with a score of <6 were considered high risk and low quality. This scale examines all stages of the study, including sample selection, comparison of the two groups, and outcomes.[21]
An appropriate follow-up period for the outcome is considered 6 months or more in cohort studies. One score is considered for articles with follow-up failure rates up to 25%.[22] Based on the Newcastle–Ottawa Scale adjusted for cross-sectional studies, articles with a score of <4 are considered low quality (ranged 0–10).[20,23] Disagreements between the two reviewers were resolved by discussion with the third researcher.
Results
Out of 371 nonduplicate reviewed articles, 24 articles were selected[2,9,10,12,16,17,18,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] [Figure 1]. The characteristics of the included studies are presented in Table 1. The total sample size was 51,613 (ranging from 49 to 37,127). All of the 24 selected studies had good quality with a low risk of bias [Supplementary Tables 1 and 2]. PPWR was reported as a difference between pre/early pregnancy weight and postpartum weight at different times from 1 month[33] to 18 months[29] postpartum.
Figure 1.
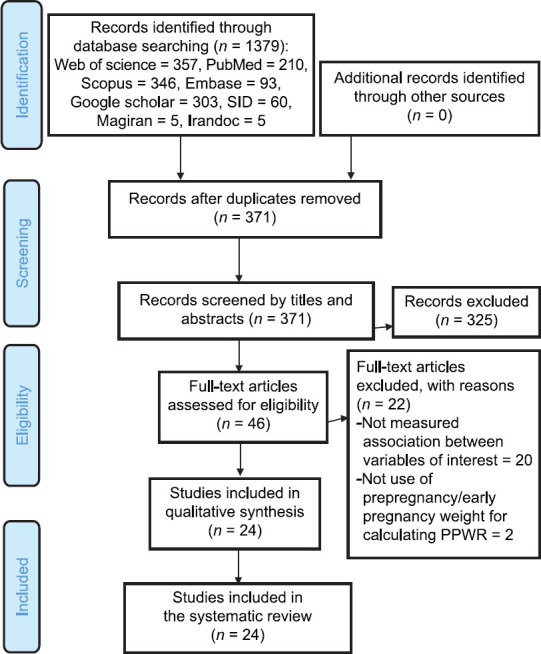
PRISMA flowchart of the present study
Table 1.
The characteristics of the included studies
| Author, year, country | Study design | Sample size | Predictor | Weight measures | Mean PPWR | Quality assessment | |||
|---|---|---|---|---|---|---|---|---|---|
| Depression | Stress | Anxiety | Prepregnancy/early pregnancy | Postpartum | |||||
| Biesmans et al. (2013) Belgium[24] | Prospective cohort | 75 | √ | √ | S | S and M | 12 months (m): 2.3 (SD=2.8) kg | 7 | |
| Bogaerts et al. (2013) Belgium[26] | Prospective cohort | 150 | √ | √ | S | S | 6 months: −1.28 (SD=6.05) (range: −17-19) kg | 7 | |
| Bogaerts et al. (2017) Belgium[25] | Prospective cohort | 220 | √ | S | S | 6 weeks (w): 3.3 (SD=4.1) (range: −7-16.2) kg | 6 | ||
| Collings et al. (2018) Australia[16] | Prospective cohort | 178 | √ | √ | √ | S | S and M | 12 months: 0.5 (SD=6.49) kg | 8 |
| Ertel et al. (2017) USA[17] | Prospective cohort | 2112 | √ | S | M | 6 month: 35% ≥5 kg (mean/SD not reported) | 8 | ||
| Goldstein et al. (2016) USA[12] | Prospective cohort | 360 | √ | √ | S | M | 3 month: 4.6 (SD=7.4) kg | 7 | |
| Gunderson et al. (2008) USA[27] | Prospective cohort | 940 | √ | S | S | 12 month: 0.8 (SD=4.5) (range: −17.3-25.5) kg | 7 | ||
| Herring et al. (2008) USA[10] | Prospective cohort | 850 | √ | S | S | 12 month: 0.6 (range: −16.4-25.5) kg | 7 | ||
| Huang et al. (2010) Taiwan[28] | Cross sectional | 602 | √ | MR | Not reported | 6 month: 2.42 (SD=3.57) kg | 9 | ||
| Oken et al. (2007) USA[2] | Prospective cohort | 902 | √ | S | S | 12 month: 0.6 (range: −17.3-25.5) kg | 7 | ||
| Pedersen et al. (2011) Denmark[29] | Prospective cohort | 37,127 | √ | √ | S | S | 6 month: 1.4 (SD=4.7) kg 18 month: 0.00 (SD=4.8) kg |
7 | |
| Phillips et al. (2014) Australia[30] | Prospective cohort | 126 | √ | √ | √ | S | S | 9 month: 3.69 (SD=5.04) kg | 7 |
| Phillips et al. (2014) Australia[31] | Prospective cohort | 227 | √ | √ | √ | S | S | 3 month: 6.10 (SD=5.56) kg | 6 |
| Riazi et al. (2017) Iran[32] | Cross-sectional | 309 | √ | MR | M | 6 m: 4.04 (SD=3.99) kg | 9 | ||
| Rogers et al. (2016) UK[18] | Prospective cohort | 49 | √ | S | M | 12 month: Mean retained BMI=1.5 kg/m2 (SD=2.4) | 8 | ||
| Salehi-pourmehr et al. (2018) Iran[9] | Prospective cohort | 307 | √ | √ | MR | M | 12 m in: Non-depressed: 1.70 (0.35) kg Depressed: 3.86 (0.98) kg Min/mild anxiety: 1.86 (0.36) kg Mod/severe anxiety: 3.88 (1.08) kg |
8 | |
| Sha et al. (2019) China[33] | Prospective cohort | 924 | √ | M | S and M | 1 month: 5.91 (SD=4.78) kg 3 month: 4.18 (SD=4.81) kg 6 month: 3.25 (SD=4.64) kg 8 month: 2.24 (SD=4.66) kg |
8 | ||
| Siega-Riz et al. (2010) USA[34] | Prospective cohort | 550 | √ | S | M | 3 month: 9.4 (SD±11.4) lb12 month: 5.7 (SD±13.2) lb | 8 | ||
| Straub et al. (2016) USA[35] | Cross-sectional | 696 | √ | MR | M | 6 month: 11.1±18.9 lbs | 9 | ||
| Van poppel et al. (2012) Netherlands[36] | Prospective cohort | 4213 | √ | √ | S | S | 3-5 month: 3.56 (SD=4.58) kg | 6 | |
| Walker (2009) USA[37] | Prospective cohort | 247 | √ | S | M | 12 month: 6.2±8.2 kg | 8 | ||
| Wan Noor Fatehah et al. (2019) Malaysia[39] | Cross-sectional | 226 | √ | S | M | 6 month: 2.6±5.3 kg | 9 | ||
| Whitaker et al. (2014) USA[38] | Prospective cohort | 123 | √ | √ | S | M | 6 month: 5.8 (SD=7.4; range: −12.1-32.9) kg 12 month: 6.4 (SD=8.5; range: −9.7-35.9) kg |
8 | |
| Zanotti et al. (2015) Brazil[40] | Prospective cohort | 145 | √ | S | M | 6 month: 4.8 kg | 7 | ||
SD=Standard deviation, MR=Medical records, S=Self-reported, S and M=Self-reported and measured, M=Measured
Supplementary Table 1.
Quality assessment of cohort studies based on Newcastle-Ottawa quality assessment scale
| Author, year | Selection | Comparability | Outcome | Total score | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the non exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow up of cohorts | ||
| Biesmans et al. (2013)[24] | * | * | * | ** | * | * | 7 | ||
| Bogaerts et al. (2013)[26] | * | * | * | ** | * | * | 7 | ||
| Bogaerts et al. (2017)[25] | * | * | * | ** | * | 6 | |||
| Collings et al. (2018)[16] | * | * | * | ** | * | * | * | 8 | |
| Ertel et al. (2017)[17] | * | * | * | ** | * | * | * | 8 | |
| Goldstein et al. (2016)[12] | * | * | * | ** | * | * | 7 | ||
| Gunderson et al. (2008)[27] | * | * | * | ** | * | * | 7 | ||
| Herring et al. (2008)[10] | * | * | * | ** | * | * | 7 | ||
| Oken et al. (2007)[2] | * | * | * | ** | * | * | 7 | ||
| Pedersen et al. (2011)[29] | * | * | * | ** | * | * | 7 | ||
| Phillips et al. (2014)[30] | * | * | * | ** | * | * | 7 | ||
| Phillips et al. (2014)[31] | * | * | * | ** | * | 6 | |||
| Rogers et al. (2016)[18] | * | * | * | ** | * | * | * | 8 | |
| Salehi -pourmehr et al. (2018)[9] | * | * | * | ** | * | * | * | 8 | |
| Sha et al. (2019)[33] | * | * | * | ** | * | * | * | 8 | |
| Siega-Riz et al. (2010)[34] | * | * | * | ** | * | * | * | 8 | |
| Van poppel et al. (2012)[36] | * | * | * | ** | * | 6 | |||
| Walker (2009)[37] | * | * | * | ** | * | * | * | 8 | |
| Whitaker et al. (2014)[38] | * | * | * | ** | * | * | * | 8 | |
| Zanotti et al. (2015)[40] | * | * | * | ** | * | * | 7 | ||
Supplementary Table 2.
Quality assessment of cross-sectional studies based on Newcastle-Ottawa quality assessment scale
| Author, year | Selection | Comparability | Outcome | Total score | ||||
|---|---|---|---|---|---|---|---|---|
| Representativeness of the sample | Sample size | Nonrespondents | Ascertainment of the exposure | The subjects in different outcome groups are comparable, based on the study design or analysis | Assessment of the outcome | Statistical test | ||
| Huang et al. (2010)[28] | * | * | * | ** | * | ** | * | 9 |
| Riazi et al. (2017)[32] | * | * | ** | ** | ** | * | 9 | |
| Straub et al. (2016)[35] | * | * | ** | ** | ** | * | 9 | |
| Wan Noor Fatehah et al. (2019)[39] | * | * | ** | ** | ** | * | 9 | |
The mean PPWR was variable, ranged from 0.5 kg (standard deviation [SD] = 6.49)[16] at 12 months postpartum to 6.4 kg (SD = 8.5)[38] at the same time. There was considerable variation in the frequency of PPWR, which ranged from 83%[32] at 6 months postpartum to 24.1%[9] 1 year after delivery.
Most studies have defined substantial PPWR (SPPWR) as a weight retention of ≥5 kg. SPPWR ranged from 62.6% at 3 months[31] to 12.1%[29] at 18 months postpartum.
Depression and postpartum weight retention
A total of 23 articles examined the relationship between depression and PPWR[2,9,10,12,16,17,18,24,25,26,27,28,29,30,31,32,33,34,36,37,38,39,40] [Table 2]. A total of 50,917 participants were studied in these articles.
Table 2.
Depression and postpartum weight retention
| Author, year | Measurement time | Measurement tool | Findings |
|---|---|---|---|
| Biesmans et al. (2013)[24] | 3 MPP | EPDS | Positive association (P=0.042) |
| Bogaerts et al.[26] (2013) | Pregnancy, 6 MPP | EPDS | 6 MPP: Association (P<0.20) |
| Bogaerts et al.[25] (2017) | 4, 6 WPP | EPDS | 4 WPP: Association (P<0.05) |
| Final analysis: NA | |||
| Collings et al. (2018)[16] | Pregnancy, 12 MPP | EPDS | NA |
| Ertel et al. (2017)[17] | Pregnancy, 6 MPP | EPDS | NA |
| Goldstein et al. (2016)[12] | Delivery, 3 MPP | PHQ2 | Delivery: Positive association (0.88, 95% CI: 0.12-1.64, P=0.02) |
| Gunderson et al. (2008)[27] | 6 MPP | EPDS | 6 MPP and SPPWR: Association (unadjusted OR=1.98, 95%CI: 1.06-3.71, P=0.03). |
| Herring et al. (2008)[10] | Pregnancy, 6 MPP | EPDS | 6 MPP and SPPWR: Association (adjusted OR=2.54, 95%CI: 1.06-6.09) |
| Antenatal: NA | |||
| Huang et al. (2010)[28] | 6 MPP | BDI | Association (F=2.16, P=0.001) |
| Oken et al. (2007)[2] | 6 MPP | EPDS | NA |
| Pedersen et al. (2011)[29] | Pregnancy, 6 MPP | Taken from | Pregnancy and 6 month PPWR: Association (adjusted OR=1.35; 95% CI, 1.27-1.44, P<0.01) |
| Symptoms checklist-92 | Pregnancy and 18 month PPWR: Association (adjusted OR=1.34; 95% CI: 1.24-1.45) | ||
| Phillips et al. (2014)[30] | 3, 6 MPP | EPDS | NA |
| Phillips et al. (2014)[31] | Pregnancy, 3 MPP | EPDS | Pregnancy: NA |
| 3 MPP: Positive association (r=0.15, P<0.05) | |||
| Riazi et al. (2017)[32] | 6 MPP | EPDS | NA |
| Rogers et al. (2016)[18] | 1, 6, 12 MPP | EPDS | NA |
| Salehi-pourmehr et al. (2018)[9] | Pregnancy, 6-8 WPP, 12 MPP | EPDS | First trimester and 12 month PPWR: Association (aMD 3.416; 95% CI: 1.392-5.441, P=0.001) |
| 6-8 WPP and 12 month PPWR: Association (aMD 3.042; 95% CI 0.538-5.547, P=0.018) | |||
| Sha et al. (2019)[33] | 1 MPP | EPDS | NA |
| Siega-Riz et al. (2010)[34] | 3, 12 MPP | EPDS | NA |
| Van poppel et al. (2012)[36] | Pregnancy, 3-5 MPP | CES-D | NA |
| Walker (2009)[37] | Postdelivery, 6 WPP | CES-D | NA |
| 3, 6, 12 MPP | |||
| Wan Noor Fatehah et al. (2019)[39] | 6 MPP | EPDS | NA |
| Whitaker et al. (2014)[38] | 2, 6, 12 MPP | PSI | 6 MPP and 6 month PPWR: Positive association (t=2.122, P=0.037) |
| Zanotti et al. (2015)[40] | 1, 3, 6 MPP | BDI | Positive association |
MPP=Months postpartum, EPDS=Edinburgh Postnatal Depression Scale, WPP=Weeks postpartum, PSI=Parenting stress index, CES-D=Center for Epidemiological Studies Depression Scale, BDI=Beck depression inventory, PHQ2=Patient Health Questionnaire-2, NA=No association, aMD=Adjusted mean difference
Out of 23 studies, 12 studies (11 cohorts and one cross sectional) showed a significant relationship between depression (at different times from pregnancy to 1 year after delivery) and PPWR. All of the cohort studies reported a positive relationship,[9,10,12,24,26,27,29,31,38,40] and the cross-sectional study indicated an inverse relationship between depression and PPWR (β = −0.10, P < 0.01).[28]
Three groups were found based on measurement time of the depression: during pregnancy (8 studies), during delivery (1 study), or immediately after delivery (1 study), at some time after delivery (23 studies). The highest number of studies evaluated depression at 6 months postpartum (14 studies). Two studies during pregnancy,[9,29] 11 studies after delivery,[9,10,24,25,26,27,28,29,31,38,40] and one study during delivery[12] reported a significant relationship between depression and PPWR.
Stress and postpartum weight retention
Out of 24 selected studies, six studies investigated the relationship between stress and PPWR[12,16,30,31,35,38] [Table 3]. A total of 1710 participants were examined in these studies.
Table 3.
Stress and PPWR
| Author, year | Measurement time | Measurement tool | Findings |
|---|---|---|---|
| Collings et al. (2018)[16] | Pregnancy, 12 MPP | DASS-21 | NA |
| Goldstein et al. 2016)[12] | Delivery, 3 MPP | PSS | 3 MPP: Inverse relationship (−0.13, 95% CI: −0.26-−0.01, P=0.04) |
| Phillips et al. (2014)[30] | 3, 6 MPP | DASS-21 | NA |
| Phillips et al. (2014)[31] | Pregnancy, 3 MPP | DASS-21 | Pregnancy: NA |
| 3 MPP: Positive association (r=0.27, P<0.01) | |||
| 3 MPP and 3 month PPWR: cross-sectional relationships (B=7.41, SEB=3.08, β=0.26, P<0.05) | |||
| Straub et al. 2016)[35] | 6 MPP | Salivary cortisol slope | Inverse relationship (β=−1.90, 95% CI: 0.22-3.58) |
| Whitaker et al. 2014)[38] | 2, 6, 12 MPP | PSI | 2 MPP and 6 month PPWR: Inversely correlation (r=−0.230, P=0.021) |
| 2 MPP and 12 month PPWR: NC | |||
| 6 MPP and 6 month PPWR: NC | |||
| 6 MPP and 12 month PPWR: Positive correlation (t=2.015, P=0.048) | |||
| 12 MPP and 12 month PPWR: NC |
DASS=Depression, anxiety, stress scale, PSS=Perceived Stress Scale, NC=Not correlation, MPP=Months postpartum, WPP=Weeks postpartum
Out of the six studies, four studies reported a significant relationship between stress and PPWR.[12,31,35,38] Two of them showed a positive relationship,[31,38] and two others reported an inverse relationship.[12,35] None of the two studies that measured stress during pregnancy reported a significant association.[16,31]
One study reported a significant marginal relationship between cortisol slope as a biologic marker of stress and PPWR (r2 = 0.07, P = 0.06). When PPWR was considered as a continuous variable, this relationship disappeared.[35]
Anxiety and postpartum weight retention
Out of the 24 selected studies, eight studies examined the relationship between anxiety and PPWR[9,16,25,26,29,30,31,36] [Table 4]. A total of 42,548 participants were examined in these studies. In six studies, anxiety was measured both during pregnancy and after delivery.[9,16,26,29,31,36] Out of the eight studies, three studies reported a positive statistically significant relationship between anxiety during pregnancy and PPWR.[9,26,29] In one study, a significant relationship was only reported between first-trimester anxiety and SPPWR 1 year after delivery.[9] In another one, univariate analysis was reported a significant relationship between anxiety 6 months after delivery and PPWR, but in the final multivariate analysis, this relationship was not reported.[26] None of the other studies reported a significant relationship between postpartum anxiety and PPWR.
Table 4.
Anxiety and postpartum weight retention
| Author, year | Measurement time | Measurement tool | Findings |
|---|---|---|---|
| Bogaerts et al. (2013)[26] | Pregnancy, 6 MPP | STAI | First trimester: Association (P<0.20) |
| 6 MPP: Association (P<0.20) | |||
| Final analysis: First trimester and 6 month PPWR: Positive predictor (β=0.255; P=0.001) | |||
| Bogaerts et al. (2017)[25] | 4, 6 WPP | STAI | NA |
| Collings et al. (2018)[16] | Pregnancy, 12 MPP | DASS-21 | NA |
| Pedersen et al. (2011)[29] | Pregnancy, 6 MPP | Taken from symptoms checklist-92 | Pregnancy and 6 month PPWR: Association (adjusted OR=1.35; 95% CI, 1.27-1.44), P<0.01) |
| Pregnancy and 18 month PPWR: Association (adjusted OR=1.34; 95% CI, 1.24-1.45) | |||
| Phillips et al. (2014)[30] | 3, 6 MPP | DASS-21 | NA (not shown) |
| Phillips et al. (2014)[31] | Pregnancy, 3 MPP | DASS-21 | NA |
| Salehi-pourmehr et al. (2018)[9] | Pregnancy, 6-8 WPP, 12 MPP | BAI-II | First trimester and 12 month SPPWR: Association (aMD 3.050; 95% CI: 0.631-5.470; P=0.014). |
| Van poppel et al. (2012)[36] | Pregnancy, 3-5 MPP | STAI, Developed questionnaire | NA |
BAI=Beck anxiety inventory, STAI=State-Trait Anxiety Inventory, OR=Odds ratio, CI=Confidence interval
Discussion
The present systematic review was conducted to investigate the relationship between depression/stress/anxiety and PPWR. A total of 24 articles were selected. PPWR was measured at 6 or 12 months postpartum in most of the studies, which is similar to previous reviews.[41] The highest mean and the lowest mean of PPWR are similar to the Xiao et al.[14] review.
According to the present review, all of the positive relationships between depression and PPWR were found in prospective cohort design studies. It seems that a cohort study plan is more appropriate to measure the effect of psychological factors on overweight, which takes time.
Depression measurement time was different in studies. Most studies have assessed postpartum depression, which is probably why the most number of significant relationships between depression and PPWR are related to this period. The path of depression during and after pregnancy is an important issue in this regard. McCall-Hosenfeld et al. reported that women who suffer from depression during pregnancy remain depressed or improve slightly during the 1st year after delivery. When the onset of depression is during 12 months after the first delivery, they become increasingly depressed.[42] The results of a meta-analysis showed that the severity of depression decreased over time.[43] These complex relationships make it difficult to determine the right time to measure depression. There should be an appropriate time interval between the onset of depression and the measurement of PPWR. In addition, biological and socioeconomic factors, lifestyle, obstetrical history, and history of mental illness were showed as risk factors for postpartum depression, suggesting to design of prevention programs.[44]
In this systematic review, most of the studies reported a significant relationship between stress and PPWR. A previous review reported different results.[14] Although studies of that review, which were published before 2000, are not included in the present review, some other reasons can explain this difference. Different times of stress measurement in the studies can be the reason for this difference. Stress was measured 6, 12 months, and 2.5 years postpartum in the previous review studies, and it has measured during pregnancy in none of them.[14] These measurement times are different from the present review. Delay in stress measurement may be concurrent with expected postpartum weight loss, which could explain the nonsignificant relationship between stress and PPWR in the previous review studies. In addition, stress was measured using different tools, which may cause different results.
In the present systematic review, a significant relationship was reported between anxiety, mainly during pregnancy, and PPWR. Nagl et al.[15] reviewed three studies in this area, which included in the present systematic review. They achieved different results, probably due to fewer studies. Hartley et al. reported that there was no significant relationship between anxiety symptoms and postpartum weight status.[13] The smaller number of their reviewed studies may be the reason for the mentioned differences. It seems that anxiety during pregnancy can have a positive relationship with increasing PPWR, but this conclusion does not apply to the relationship between postpartum anxiety and PPWR.
Strengths and limitations of the review
The present systematic review has some strengths, including conducting an extensive search in several databases, the high quality of the selected studies, and the selection of both Persian- and English-language articles. However, using different research methods, measurement tools/times in studies made it impossible to conduct a quantitative meta-analysis.
Conclusion
The results of this systematic review indicate the relationship between depression/stress/anxiety and PPWR. However, further researches are recommended for achieving a comprehensive conclusion. It seems that study design, time of depression/stress/anxiety assessment, and different measurement tools were important issues in different results. Faleschini et al. emphasized the protective role of social support in physical behaviors and mental health, which, in turn, affects PPWR.[45] Furthermore, relaxation could reduce stress, anxiety, and depression in pregnant women.[46] HBM model could be a suitable framework to design an educational intervention to improve weight control behaviors among pregnant women.[47] Therefore, educational, interventional, and supportive programs preventing psychological problems during pregnancy and postpartum are suggested reducing the psychological factors’ impact on PPWR.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article is a part of a review of the literature of a PhD thesis at Shahid Beheshti University of Medical Sciences with the code of ethics IR. SBMU. PHARMACY. REC.1398.122. The officials of the faculty, library, and computer unit of Shahid Beheshti University of Medical Sciences are appreciated.
References
- 1.Fadzil F, Shamsuddin K, Wan Puteh SE, Mohd Tamil A, Ahmad S, Abdul Hayi NS, et al. Predictors of postpartum weight retention among urban Malaysian mothers: A prospective cohort study. Obes Res Clin Pract. 2018;12:493–9. doi: 10.1016/j.orcp.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Oken E, Taveras EM, Popoola FA, Rich-Edwards JW, Gillman MW. Television, walking, and diet: Associations with postpartum weight retention. Am J Prev Med. 2007;32:305–11. doi: 10.1016/j.amepre.2006.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bogaerts A, Van den Bergh BR, Ameye L, Witters I, Martens E, Timmerman D, et al. Interpregnancy weight change and risk for adverse perinatal outcome. Obstet Gynecol. 2013;122:999–1009. doi: 10.1097/AOG.0b013e3182a7f63e. [DOI] [PubMed] [Google Scholar]
- 4.Lim S, O'Reilly S, Behrens H, Skinner T, Ellis I, Dunbar J. Effective strategies for weight loss in post-partum women: A systematic review and meta-analysis. Obesity Rev. 2015;16:972–87. doi: 10.1111/obr.12312. [DOI] [PubMed] [Google Scholar]
- 5.Hollis JL, Crozier SR, Inskip HM, Cooper C, Godfrey KM, Harvey NC, et al. Modifiable risk factors of maternal postpartum weight retention: An analysis of their combined impact and potential opportunities for prevention. Int J Obes (Lond) 2017;41:1091–8. doi: 10.1038/ijo.2017.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Endres LK, Straub H, McKinney C, Plunkett B, Minkovitz CS, Schetter CD, et al. Postpartum weight retention risk factors and relationship to obesity at 1 year. Obstet Gynecol. 2015;125:144–52. doi: 10.1097/AOG.0000000000000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Phillips J, King R, Skouteris H. A conceptual model of psychological predictors of postpartum weight retention. J Reproduct Infant Psychol. 2012;30:278–88. [Google Scholar]
- 8.McKinley MC, Allen-Walker V, McGirr C, Rooney C, Woodside JV. Weight loss after pregnancy: Challenges and opportunities. Nutr Res Rev. 2018;31:225–38. doi: 10.1017/S0954422418000070. [DOI] [PubMed] [Google Scholar]
- 9.Salehi-Pourmehr H, Niroomand S, Shakouri SK, Asgarlou Z, Farshbaf-Khalili A. Association between antenatal and postpartum depression and anxiety with weight retention 1 year after childbirth: A longitudinal study. Community Ment Health J. 2018;54:1284–94. doi: 10.1007/s10597-018-0324-y. [DOI] [PubMed] [Google Scholar]
- 10.Herring SJ, Rich-Edwards JW, Oken E, Rifas-Shiman SL, Kleinman KP, Gillman MW. Association of postpartum depression with weight retention 1 year after childbirth. Obesity (Silver Spring) 2008;16:1296–301. doi: 10.1038/oby.2008.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huberty J, Leiferman JA, Kruper AR, Jacobson LT, Waring ME, Matthews JL, et al. Exploring the need for interventions to manage weight and stress during interconception. J Behav Med. 2017;40:145–58. doi: 10.1007/s10865-016-9813-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldstein ND, Rogers S, Ehrenthal DB. The impact of psychosocial stressors on postpartum weight retention. Arch Womens Ment Health. 2016;19:691–4. doi: 10.1007/s00737-016-0613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartley E, Hill B, McPhie S, Skouteris H. The associations between depressive and anxiety symptoms, body image, and weight in the first year postpartum: A rapid systematic review. J Reprod Infant Psychol. 2018;36:81–101. doi: 10.1080/02646838.2017.1396301. [DOI] [PubMed] [Google Scholar]
- 14.Xiao RS, Kroll-Desrosiers AR, Goldberg RJ, Pagoto SL, Person SD, Waring ME. The impact of sleep, stress, and depression on postpartum weight retention: A systematic review. J Psychosom Res. 2014;77:351–8. doi: 10.1016/j.jpsychores.2014.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagl M, Linde K, Stepan H, Kersting A. Obesity and anxiety during pregnancy and postpartum: A systematic review. J Affect Disord. 2015;186:293–305. doi: 10.1016/j.jad.2015.06.054. [DOI] [PubMed] [Google Scholar]
- 16.Collings R, Hill B, Skouteris H. The influence of psychological factors on postpartum weight retention 12 months post-birth. J Reprod Infant Psychol. 2018;36:177–91. doi: 10.1080/02646838.2018.1424323. [DOI] [PubMed] [Google Scholar]
- 17.Ertel KA, Huang T, Rifas-Shiman SL, Kleinman K, Rich-Edwards J, Oken E, et al. Perinatal weight and risk of prenatal and postpartum depressive symptoms. Ann Epidemiol. 2017;27:695–7000. doi: 10.1016/j.annepidem.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rogers SL, Hughes BA, Tomlinson JW, Blissett J. Cortisol metabolism, postnatal depression and weight changes in the first 12 months postpartum. Clin Endocrinol (Oxf) 2016;85:881–90. doi: 10.1111/cen.13150. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. Canada: Department of Epidemiology and Community Medicine, University of Ottawa; [Last accessed on 2020 Jun 01]. The newcastle ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses [Internet] Available from: http://wwwohrica/programs/clinical_epidemiology/oxfordasp . [Google Scholar]
- 22.Rong K, Yu K, Han X, Szeto IM, Qin X, Wang J, et al. Pre-pregnancy BMI, gestational weight gain and postpartum weight retention: A meta-analysis of observational studies. Public Health Nutr. 2015;18:2172–82. doi: 10.1017/S1368980014002523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adib-Hajbaghery Zare M. The barriers to patient education from the viewpoint of nurses in Iran: A systematic review. Nurs Midwifery J. 2017;15:544–58. Persian. [Google Scholar]
- 24.Biesmans K, Franck E, Ceulemans C, Jacquemyn Y, Van Bogaert P. Weight during the postpartum period: What can health care workers do? Matern Child Health J. 2013;17:996–1004. doi: 10.1007/s10995-012-1077-9. [DOI] [PubMed] [Google Scholar]
- 25.Bogaerts A, De Baetselier E, Ameye L, Dilles T, Van Rompaey B, Devlieger R. Postpartum weight trajectories in overweight and lean women. Midwifery. 2017;49:134–41. doi: 10.1016/j.midw.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 26.Bogaerts AF, Van den Bergh BR, Witters I, Devlieger R. Anxiety during early pregnancy predicts postpartum weight retention in obese mothers. Obesity (Silver Spring) 2013;21:1942–9. doi: 10.1002/oby.20352. [DOI] [PubMed] [Google Scholar]
- 27.Gunderson EP, Rifas-Shiman SL, Oken E, Rich-Edwards JW, Kleinman KP, Taveras EM, et al. Association of fewer hours of sleep at 6 months postpartum with substantial weight retention at 1 year postpartum. Am J Epidemiol. 2008;167:178–87. doi: 10.1093/aje/kwm298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang TT, Wang HS, Dai FT. Effect of pre-pregnancy body size on postpartum weight retention. Midwifery. 2010;26:222–31. doi: 10.1016/j.midw.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Pedersen P, Baker JL, Henriksen TB, Lissner L, Heitmann BL, Sørensen TI, et al. Influence of psychosocial factors on postpartum weight retention. Obesity (Silver Spring) 2011;19:639–46. doi: 10.1038/oby.2010.175. [DOI] [PubMed] [Google Scholar]
- 30.Phillips J, King R, Skouteris H. The influence of psychological factors on post-partum weight retention at 9 months. Br J Health Psychol. 2014;19:751–66. doi: 10.1111/bjhp.12074. [DOI] [PubMed] [Google Scholar]
- 31.Phillips J, King R, Skouteris H. The influence of psychological distress during pregnancy on early postpartum weight retention. J Reproduct Infant Psychol. 2014;32:25–40. [Google Scholar]
- 32.Riazi H, Torkashvand R, Mahmoodi Z, Boroomandnia N. Postpartum weight retention and its relation with depression. Koomesh. 2017;19:276–85. Persian. [Google Scholar]
- 33.Sha T, Cheng G, Li C, Gao X, Li L, Chen C, et al. Patterns of women's postpartum weight retention and its associations with maternal obesity-related factors and parity. Int J Environ Res Public Health. 2019;16(22):4510. doi: 10.3390/ijerph16224510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siega-Riz AM, Herring AH, Carrier K, Evenson KR, Dole N, Deierlein A. Sociodemographic, perinatal, behavioral, and psychosocial predictors of weight retention at 3 and 12 months postpartum. Obesity (Silver Spring) 2010;18:1996–2003. doi: 10.1038/oby.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Straub H, Simon C, Plunkett BA, Endres L, Adam EK, Mckinney C, et al. Evidence for a complex relationship among weight retention, cortisol and breastfeeding in postpartum women. Matern Child Health J. 2016;20:1375–83. doi: 10.1007/s10995-016-1934-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Poppel MN, Hartman MA, Hosper K, van Eijsden M. Ethnic differences in weight retention after pregnancy: The ABCD study. Eur J Public Health. 2012;22:874–9. doi: 10.1093/eurpub/cks001. [DOI] [PubMed] [Google Scholar]
- 37.Walker LO. Low-income women's reproductive weight patterns empirically based clusters of prepregnant, gestational, and postpartum weights. Womens Health Issues. 2009;19:398–405. doi: 10.1016/j.whi.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 38.Whitaker K, Young-Hyman D, Vernon M, Wilcox S. Maternal stress predicts postpartum weight retention. Matern Child Health J. 2014;18:2209–17. doi: 10.1007/s10995-014-1470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wan Noor Fatehah WZ, Yong H, Zalilah M, Zulida R, Barakatun Nisak MY. Correlation of pre-pregnancy bmi, sleep and depression with postpartum weight retention among chilbearing age women. Int J Public Health and Clin Sci. 2019;6:148–59. [Google Scholar]
- 40.Zanotti J, Capp E, Wender MC. Factors associated with postpartum weight retention in a Brazilian cohort. Rev Bras Ginecol Obstet. 2015;37:164–71. doi: 10.1590/SO100-720320150005186. [DOI] [PubMed] [Google Scholar]
- 41.Schmitt NM, Nicholson WK, Schmitt J. The association of pregnancy and the development of obesity-results of a systematic review and meta-analysis on the natural history of postpartum weight retention. Int J Obes (Lond) 2007;31:1642–51. doi: 10.1038/sj.ijo.0803655. [DOI] [PubMed] [Google Scholar]
- 42.McCall-Hosenfeld JS, Phiri K, Schaefer E, Zhu J, Kjerulff K. Trajectories of depressive symptoms throughout the peri- and postpartum period: Results from the first baby study. J Womens Health (Larchmt) 2016;25:1112–21. doi: 10.1089/jwh.2015.5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vliegen N, Casalin S, Luyten P. The course of postpartum depression: A review of longitudinal studies. Harv Rev Psychiatry. 2014;22:1–22. doi: 10.1097/HRP.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 44.Ghaedrahmati M, Kazemi A, Kheirabadi G, Ebrahimi A, Bahrami M. Postpartum depression risk factors: A narrative review. J Educ Health Promot. 2017;6:60. doi: 10.4103/jehp.jehp_9_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Faleschini S, Millar L, Rifas-Shiman SL, Skouteris H, Hivert MF, Oken E. Women's perceived social support: Associations with postpartum weight retention, health behaviors and depressive symptoms. BMC Womens Health. 2019;19:143. doi: 10.1186/s12905-019-0839-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nasiri S, Akbari H, Tagharrobi L, Tabatabaee AS. The effect of progressive muscle relaxation and guided imagery on stress, anxiety, and depression of pregnant women referred to health centers. J Educ Health Promot. 2018;7:41. doi: 10.4103/jehp.jehp_158_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abdolaliyan N, Shahnazi H, Kzemi A, Hasanzadeh A. Determinants of the self-efficacy of physical activity for maintaining weight during pregnancy: The application of the health belief model. J Educ Health Promot. 2017;6:93. doi: 10.4103/jehp.jehp_175_16. [DOI] [PMC free article] [PubMed] [Google Scholar]


