Abstract
With the onset of the coronavirus disease 2019 (COVID-19) outbreak, the transformation of the care delivery model from conventional in-person (face to face) to largely virtual or remote care has been accelerated to appropriately allocate resources and constrain the spread of the virus. In this regard, telemedicine is a breakthrough technology to battle against the COVID-19 emergency. Therefore, we sought to identify the telemedicine applications in the COVID-19 pandemic (tele-COVID) according to interaction modes, transmission modalities, and disease categories. This systematic review was conducted through searching five databases including PubMed, Scopus, ProQuest, Web of Science, and Science Direct. Inclusion criteria were studies clearly outlining any use of telemedicine interactive mode during the COVID-19 pandemic, written in English language and published in peer-reviewed journals in 2020. Finally, 43 articles met the inclusion out of the 1118 search results. Telemedicine provides a diversity of interaction modes and modalities affordable by patients and physicians including short message service, E-mail and web portals, secure telephone calls or VOIP, video calls, interactive mobile health applications (m-Health), remote patient monitoring, and video conferencing. Transmission of video data using synchronized video calls via common social media had the highest and exchange of data using store-forward service via secure messaging technology and prerecorded multimedia had the lowest popularity for virtual disease management during the COVID-19 outbreak. Selection of telemedicine communication services and interaction modes with regard to its use-case, disease category, and application plays a significant role in the success of remote disease management infrastructures in this scenario and their implication for a better future healthcare system.
Keywords: Coronavirus, COVID-19, telehealth, telemedicine, virtual care
Introduction
The number of definite cases of coronavirus disease 2019 (COVID-19) is increasing sharply around the world, and as of March 11, 2020, the World Health Organization declared this outbreak a public health emergency.[1,2] As a retroviral disease transmitted by airborne droplets of the severe acute respiratory syndrome-coronavirus-2, it is highly contagious and patients may be catching even without clinical presentation.[3,4] Because there are currently no vaccine or an effective medical cure for COVID-19, major struggles are directed at containing the spread of the virus and flatten the COVID-19 epidemiological peak surge in the worldwide population.[5,6] These mitigation efforts included social-distancing mandates, closure of nonessential businesses, quarantine, suspending large assemblies, and enforcing strict hygiene measures, as well as encouraging residents to shelter in place.[7,8,9,10,11,12] During this unprecedented crisis, health-care facilities have been confronted with the challenge not only for treating COVID-19-afflicted cases but also for managing patients with emergency conditions and those suffering from other acute and chronic illnesses. This challenge necessitates drastic measures comply with imposing social-distancing and “stay-at-home” instructions to reduce the possibility of cross-contamination and nosocomial COVID-19 transmission to patients and medical staffs alike.[13,14] In response to the outbreak, the Centers for Disease Control and Prevention, as well as several national and international health authorities, issued recommendations that telemedicine should be considered for dealing some challenges facing health-care systems in the battle against the COVID-19 crisis.[15,16,17]
Telemedicine involves a variety of digital and telecommunications tools to allow health-care workers to assess, diagnose, monitor, treat, and educate patients “remotely.” With the advent of COVID-19, telemedicine has been a key strategy to continued care for patients while mitigating the spread of virus and conserving valuable health-care resources, particularly personal protective equipment, ventilators, and free intensive care unit (ICU) beds.[18,19] To this end, the health-care settings considerably adjust their practices in order to maximize the utilization of the virtual visits, and avoiding depletion of medical supplies and resources. In this regard, the current outbreak has promptly transitioned how clinicians triage and visit patients because shelter-in-place restrictions were issued throughout the world. Similarly, telemedicine can be predominantly advantageous for individuals who are particularly susceptible to COVID-19, such as cardiopulmonary diseases, diabetes, malignancies, and older adults with underlying health condition to avoid contact with potentially infected patients.[20,21,22,23]
Given the government-imposed severe restrictions on social interactions and travel, telemedicine offers a great potential for eliminating in-person visits during the COVID-19 pandemic while attempting to reduce the transmission of virus to patients, families, and health-care staff.[24,25] Hence, there is a need to change management strategies for enabling effective access to virtual care with strong physician–patient interaction. This raises the question: what telecommunication and informatics infrastructures are needed to provision virtual care during COVID-19 and to combat the crisis outbreak?
Materials and Methods
Our systematic literature review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses standard guideline. It consists of a 27-item checklist in the form of seven main classes and a four-phase flow diagram which describes the identification, screening, eligibility, and inclusion criteria of the articles that fall under the scope of review.[26]
Search strategy and study selection criteria
An extensive search was performed in 2020 to identify full-text valid articles of any design and in any setting dealing with remotely supported disease management via telemedicine during the COVID-19 pandemic.
PubMed, Scopus, Web of Science, Science Direct, and ProQuest databases were reviewed up to June 21, 2020. The following search terms were used (designed using English MeSH keywords and Emtree terms): (COVID-19 OR Novel coronavirus) AND (telemedicine OR telehealth) AND (transmission OR interaction). After adoption of advance search option (search formula: combining key terms, search operators, and search fields (title, title/abstract, and topic)) and applying inclusion and exclusion criteria (via search filter or refine), the titles and abstracts of potentially relevant studies were identified [Table 1].
Table 1.
Search syntax
| Databases | Search syntax |
|---|---|
| Scopus | (Title (COVID-19) or title (novel coronavirus) or title (n-CoV2) and title-abs-key (Telemedicine) or title-abs-key (telehealth) and title-abs-KEY (transmission) or title-abs-key (interaction) and (limit-to (language, “English”)) |
| WOS | Title: (COVID-19) or title: (novel coronavirus) or title: (n-CoV2) and topic: (telemedicine) or topic: (telehealth) and topic: (transmission) or topic: (interaction). refined by: languages: (English ) and publication years: (2020) |
| ProQuest | Ti (COVID-19) or ti (novel coronavirus) or Ti (n-CoV2) and ab (telemedicine) or ab (telehealth) and ab (transmission) and ab (interaction). applied filter: time span: 2020-01-01–2020-06-21 and English |
| PubMed | ((((((COVID-19 [title]) or (coronavirus [title])) or (n-CoV2 [title])) And (telemedicine [title/abstract])) or (telehealth [title/abstract])) and (transmission [title/abstract])) or (interaction [title/abstract]) and language: (English), limited to 2020 |
| Science direct | Title (“COVID-19” OR “novel Coronavirus” OR “n-CoV” and title-abs-key (“telemedicine” OR “telehealth”) and title-abs-key (“transmission” or “interaction”) and English [language], limited to 2020 |
COVID-19=Coronavirus disease 2019
Inclusion and exclusion criteria
In our study, we included every study that reported tele-COVID services with information on their interaction modes, approaches, and timing aspects. Full-text articles were obtained for detailed evaluation, and eligible studies were included in the systematic review. Letters, posters, conferences papers, lectures, duplicated, non-English articles, and articles published before 2020 were excluded. As COVID-19 is a rapidly evolving area, we included preprint literature.
Data extraction and summarizing
We designed a data extraction form to record data, which included the first author; country; year of publication; study design; and interaction modes including, communication type, timing attribute, and disease category. The studies that met our predefined inclusion criteria were screened based on title/abstract by two authors (H: K-A and M: SH), and the studies that completely fulfilled our inclusion criteria were extracted for deeper analysis. Any vagueness during the study selection process was resolved by further discussion and consensus. The results were organized under the following categories: (1) tele-COVID modes, (2) tele- COVID categories, and (3) tele-COVID interaction approaches.
Results
Characteristics of included studies
An extensive search was conducted in selected databases, in order to find the resources regarding tele-COVID types, categories, and interaction modes.
The search was started on June 4, 2020, and the last search was on June 21, 2020. Initial search yielded 1118 potentially relevant papers (202 from PubMed, 86 from WOS, 156 from Scopus, 486 from ProQuest, and 188 from Science Direct); 482 of which remained after omitting the duplicate and non-English resources, as well as those published before 2020, and the document-type ones.
Then by screening the titles/abstracts of remain articles, 246 number of them were also excluded, because their focus was on the tele-COVID technical (hardware and software required for tele-COVID) and administrative (challenges and opportunities of tele-COVID) aspects.
After evaluating 236 full texts for eligibility, 193 full-text articles were excluded due to the absence of comprehensiveness, relevancy, and enough analytical criteria. Finally, 43 articles that satisfied all criteria were included in the study. Figure 1 summarizes the selection process.
Figure 1.
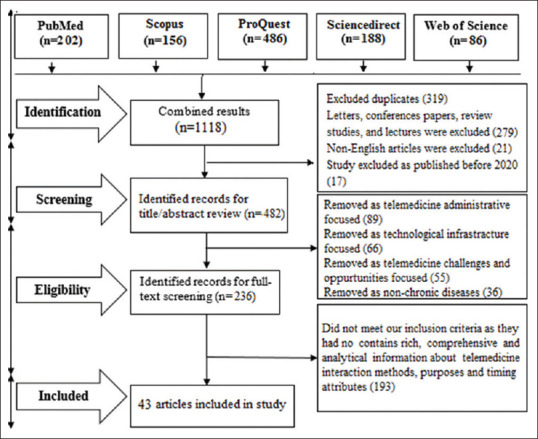
PRISMA chart in the study selection process
The main characteristics of the included studies in the systematic review are shown in Table 2.
Table 2.
Summary characteristic of the included studies in the systematic review
| Row | Author | Country | Journal name | Method | Telemedicine mode |
|---|---|---|---|---|---|
| 1 | Nagra et al. (2020) | The UK | Contact Lens and Anterior Eye | Case study | Tele-ophthalmology via m-health |
| 2 | Pollock et al. (2020) | The USA | American Journal of Otolaryngology | Case study | Tele-ENT visit via telephone and video chat tech |
| 3 | Saleem et al. (2020) | The USA | American Journal of Ophthalmology | Literature review | Tele-optometry via VOIP, video chat messenger, and m-health apps |
| 4 | Shokri et al. (2020) | The USA | American Academy of Facial Plastic and Reconstructive Surgery | Cross-sectional | Live video visits via special social media and application software |
| 5 | Boehm et al. (2020) | Germany | European Urology | Cross-sectional | Tele-urological visit via store-forward |
| 6 | Kang et al. (2020) | The UK | Eye | Retrospective | Tele-ophthalmology via video-conference |
| 7 | Mihalj et al. (2020) | The USA | Best Practice and Research Clinical Anaesthesiology | Descriptive | COVID tele-care via synchronized and a synchronized tech |
| 8 | Shipchandler et al. (2020) | The USA | Otolaryngology–Head And Neck Surgery | Case study | Tele-ENT visit via formal telemedicine platforms |
| 9 | Gutierrez et al. (2020) | The USA | Rural Health | Retrospective | Video-conferencing visits through online platforms or smartphones |
| 10 | Blue et al. (2020) | The USA | World Neurosurgery | Descriptive | Tele-neurology and tele-stroke messenger chat (text and multimedia) |
| 11 | Lee et al. (2020) | China | Head and Neck | Case study | Tele-medical sessions via special messenger apps |
| 12 | Punia et al. (2020) | The USA | Telemedicine and e-Health | Case study | Tele-visit videoconferencing platforms and telephone |
| 13 | Triantafillou et al. (2020) | The USA | Otolaryngology–Head and Neck Surgery | Cross-sectional | Tele-ENT via video visits and call phone |
| 14 | Goodman et al. (2020) | Spain | Medical Internet Research | Clinical trial | Tele-psychology via basic technology and medias (telephone and TV) |
| 15 | Grimes et al. (2020) | The USA | International Urogynecology | Case study | Tele-urogynecology via video-conference visit or basic tech |
| 16 | Moring et al. (2020) | The USA | Traumatic Stress | Cross-sectional | Tele-mental supportive care via VOIP and store-forward tech |
| 17 | Rogers et al. (2020) | The USA | AIDS and Behavior | Case study | HIV telephone scheduling and video consultation via special messenger apps |
| 18 | Smith et al. (2020) | Denmark | Telemedicine and Telecare | Retrospective | Tele-ED video consultations via formal telemedicine platforms |
| 19 | Zhou et al. (2020) | China | Telemedicine and E-Health | Case study | Tele-psychology through online messenger platforms |
| 20 | Ghai et al. (2020) | India | Indian Journal of Anaesthesia | Review | Synchronized and a synchronized tele-consultation |
| 21 | Mann et al. | The USA | American Medical Informatics Association | Cross-sectional | Video-based VUC and NUC |
| 22 | Contreras et al. (2020) | The USA | Gastrointestinal Surgery | Retrospective | Online tele-surgery consultation via special application software’s |
| 23 | Godzinski et al. (2020) | The USA | Urology | Case study | Tele-visit and tele-ED via video-conference and voice-call |
| 24 | Lee et al. (2020) | The USA | Physical Therapy | Literature review | Tele-rehabilitation virtual visit via basic tech |
| 25 | Smith et al. (2020) | The USA | American College of Surgeons | Case study | Outpatient tele-visit via video visit and calling |
| 26 | Gadzinski et al. (2020) | The USA | Nature Reviews Urology | Review | Tele-urology virtual check-in via video-visit and e-visit tech |
| 27 | Prasad et al. (2020) | The USA | Head and neck | Case study | Tele-visit via personal session: Web cam tech |
| 28 | Serper et al. (2020) | The USA | Hepatology | Case study | Tele-hepatology via video base tele-conference |
| 29 | Mgbako et al. (2020) | The USA | AIDS and Behavior | Cross-sectional | HIV tele-care via tele-conference and telephone tech |
| 30 | Peters et al. (2020) | The USA | Diabetes Technology and Therapeutics | Case study | Tele-health visit via video chatting special apps, video image, and telephone |
| 31 | Zughni et al. (2020) | The USA | Otolaryngology–Head and Neck Surgery | Clinical trial | Tele-evaluation for ENT via video-conference and VOIP |
| 32 | Ohannessian et al. (2020) | France | JMIR Public Health and Surveillance | Case study | Tele-consultation via video and audio tech |
| 33 | Prasad et al. (2020) | The USA | Head and Neck | Review | Virtual visit via video-conference |
| 34 | Layfield et al. (2020) | The USA | Head and Neck | Retrospective | Tele-care of heal and neck via telephone or video-based platform |
| 35 | Tenforde et al. (2020) | The USA | Practice Management | Cross-sectional | Tele-treatment via synchronous audiovisual: formal platform |
| 36 | Parikh et al. (2020) | The USA | American College of Cardiology | Retrospective | Online video-conference tele-cardiology via web-cam tech |
| 37 | Aziz et al. (2020) | The USA | American Journal of Perinatology | Cross-sectional | Telehealth virtual visits for maternal care via special messenger apps |
| 38 | Hogland et al. (2020) | Brazil | The Brazilian Journal of Infectious Diseases | Case study | Tele-phone based tele-consultation for HIV care |
| 39 | Berg et al. (2020) | The USA | Pediatric Gastroenterology and Nutrition | Case study | Tele-visit via store-forward, video visit tech. And special social medias |
| 40 | Siniscalchi et al. (2020) | The USA | Digestive and Liver Disease | Cross-sectional | Telemedicine remote visit |
| 41 | Parisien et al. (2020) | The USA | American Academy of Orthopaedic Surgeons | Cross-sectional | Tele-health video-conference and store-forward via special apps |
| 42 | Fatyga et al. (2020) | The USA | Polish Archives of Internal Medicine | Cross-sectional | Tele-supportive diabetic care via basic and store-forward tech |
| 43 | Baidal et al. (2020) | The USA | Obesity (Silver Spring, md) | Review | Tele-health consolation via special video chatting medias and apps |
ENT=Ear, nose, and throat, VOIP=Voice over internet protocol, COVID=Coronavirus disease, HIV=Human immunodeficiency virus, VUC=Virtual urgent care, NUC=Nonvirtual urgent care, JMIR=Journal of Medical Internet Research, AIDS=Acquired immunodeficiency syndrome
Analysis of the results
The included studies published in different journals up to June 21, 2020, were mostly carried out in the USA (33 articles, 76.75%). Five studies (11.63%) were conducted in four European countries: The UK (n = 2), Denmark (n = 1), Germany (n = 1), and France (n = 1). China as the emerging place of novel coronavirus has two articles (4.65%), and each of the other countries including Canada, Brazil, and India has one article (sum, 6.97%).
All included studies had adequate relevance to the subject of this review and categorized in three sections including: (1) tele-COVID modes [Table 3], (2) tele-COVID categories [Table 4], and (3) tele-COVID modalities [Table 5].
Table 3.
Tele-coronavirus disease modes
| Applications | Telemedicine virtual care classes | References |
|---|---|---|
| NUC | Virtual check in | [27,28] |
| Tele-triage | [29,30,31,32,33,34,35,36] | |
| Tele-screening | ||
| Tele-radiology (remote CT scanning) | [27,34] | |
| Tele-laboratory (remote RT-PCR) | ||
| Tele-care | [34,37,38] | |
| Tele-scheduling | [21,38,39] | |
| Tele-education | [7,31,36,40,41,42,43] | |
| Tele-quarantine consultation | [27,28,34,36,44,45,46] | |
| RPM | [40,47] | |
| Tele-rehabilitation | [28,48,49] | |
| Tele-surgery (pre- and post-operation follow-up) | [7,44] | |
| VUC | Emergency care (tele-ED) | [21,31,39,45,50] |
| Critical care (tele-ICU) | [50] |
NUC=Nonvirtual urgent care, VUC=Virtual urgent care, RPM=Remote patient monitoring, CT=Computed tomography, ICU=Intensive care unit, RT-PCR=Reverse transcription-polymerase chain reaction, ED=Emergency department
Table 4.
Tele-coronavirus disease categories
| Categories | Tele-consultation classes | References |
|---|---|---|
| COVID-19-related conditions | Tele-COVID care | [21,31,39,45,50] |
| Nonrelated COVID-19 conditions | Tele-ENT | [17,27,28,30,46,49,51,52,53,54,55,56,57] |
| Tele-supportive | [23,31,34,48,58] | |
| Tele-neuropsychology | [38,43,48,58] | |
| Tele-urology | [29,37,60] | |
| Hepatocellular remote care | [58,61,62] | |
| HIV remote care/treatment | [42,47] | |
| Tele-gastroenterology | [33,36] | |
| Malignancy remote treatment | [51,55] | |
| Tele-obstetric | [63] | |
| Tele-cardiovascular | [64] | |
| Tele-respiratory | [31] | |
| Tele-rehabilitation | [41] | |
| Musculoskeletal remote care | [65] |
ENT=Ear, nose, and throat, COVID-19=Coronavirus disease 2019, HIV=Human immunodeficiency virus
Table 5.
Tele-coronavirus disease modalities
| Timing attributes | Modalities | Platforms | References |
|---|---|---|---|
| Synchronized (real time) | Plain text | Online chat (Chatbot’s) | [45,56,66] |
| SMS | [40,48,49,51,62] | ||
| Websites | [41,43,48,56] | ||
| Web-based portals | [41,43,56] | ||
| Online auto questionnaires | [41,56] | ||
| FAQ | [56] | ||
| Social media messengers[37,39,41,44,45,47,56,61] | |||
| [37,39,47] | |||
| WhatApp | [37,39,47,57] | ||
| [37,39] | |||
| [37,47,56] | |||
| Other medias (linked in, Twitter, Google +) | [27,37,41,44,45,47,61] | ||
| Audio | Call phone | [37,39,41,43,47,48,51] | |
| VOIP | [39,44,51,66] | ||
| Mobile apps | [37,39,41,42,43,45,47,48,49,51,54,55,61,66] | ||
| Video | Telemedicine facility (tele-conference platforms) | [37,39,47,55] | |
| Personal session (webcam technology) | [7,17,27,28,42,45,55,62] | ||
| Video on chat platforms (social medias) | [17,27,37,39,41,42,43,44,45,47,48,49,51,52,54,55,56,61,66] | ||
| Special application software[7,39,43,47,48,52,56,57,61,66] | |||
| Skype | [7,39,40,43,47,48,52,54,55,56,57,60,61,66] | ||
| Zoom meetings | [7,47,52,56,57,60,61] | ||
| Go to meeting | [7,55,56] | ||
| Other (Epic, FaceTime, Doximity, MyChart) | [7,39,40,48,66] | ||
| Mass media (TV, radio) | [43] | ||
| A synchronized (store and forward) | Plain text, text, and numeric, image | [27,34,37,41,44,45,61] | |
| Fax | [17,34,60] | ||
| Outlook Express | [17,60] | ||
| Prerecorded audio and video | Electronic communications systems | [34,47] | |
| Social medias/special apps (e.g., WhatsApp, WeChat, and Zoom) | [52,61] | ||
| Combined (real time+store-forward) | [17,37,39,41,51] |
VOIP=Voice over internet protocol, SMS=Short Message Service, FAQ=Frequently asked question
Tele-COVID categories
The finding of this study demonstrated that telemedicine services for virtual care were classified into nonvirtual urgent care (NUC) and virtual urgent care (VUC) classes. NUC is related to the delivery of virtual health-care services for common, routine, or nonemergency medical conditions. On the other hand, VUC is provision of remote medical services for critical, immediate, or emergency conditions.[67,68] The use of NUC[7,17,27,28,29,30,31,34,37,38,39,41,42,43,44,45,48,49,50,52,56] is more prominent than the emergency applications VUC during the COVID-19 pandemic.[21,31,39,40,45,50] Among tele-COVID services, tele-triage,[29,30,31,32,33,34,35,36] tele-quarantine,[27,28,34,36,44,45,46] and tele-education (distance learning)[7,31,36,40,41,42,43] provision, particularly via social media platforms,[27,37,39,41,44,45,47,56,61] were more significant for tele-COVID. However, other services including tele-screening (tele-CT scan and tele-LAB kit),[63] remote patient monitoring or telemetry,[40,47] tele-surgery,[7,44] and tele-ICU[40,50] have less applied in this pandemic due to their needs for expensive and complex technical infrastructures.
COVID-19 virtual care purposes (tele-COVID applications)
The telemedicine is used to delivery virtual care during current pandemic for COVID-19[21,31,39,50,53,54,61,66] and non-COVID-19-related conditions.[23,27,28,29,30,31,33,34,36,37,38,41,42,43,47,48,49,51,52,53,54,55,56,57,58,61,62,63,64,65] In our literature review, 13 studies reported the application of telemedicine in managing the head-and-neck and ENT morbidities;[17,27,28,30,46,49,51,52,53,54,55,56,57] eight studies reported the application of telemedicine for virtual care of COVID-19;[21,31,39,50,53,54,61,66] five studies were related to the tele-supportive applications such as lifestyle and self-care management for at-risk population;[23,31,34,48,58] four studies reported the management of neuropsychology;[38,43,48,59] six studies were related to the tele-urology[29,37,60] and hepatocellular remotely care;[58,61,62] six studies in the tele-gastroenterology,[33,36] malignancy remotely treatment,[51,55] and HIV virtual care;[42,47] and finally five studies were related to tele-obstetric,[63] tele-cardiovascular,[64] tele-respiratory,[31] tele-rehabilitation,[41] and musculoskeletal remote care.[65] It should be noted that four articles have dealt with more than one condition.[48,55,58,61]
Tele-COVID interaction mode (synchronous vs. asynchronous)
This paper also outlines the dissimilarity between tele-COVID applications in terms of their timing perspective for data transmission during the pandemic. The three types of telemedicine modes are synchronous, asynchronous, and combined. Synchronous virtual meetings that happen in real time, live, and reciprocal modes use noninteractive and store-forward technologies to data transmission between two sides of communication.[50,69] In the current study, the results indicated that real-time interaction modalities, for example, online chatting, telephonic communication, VOIP, and video conference technologies[7,17,27,37,39,40,41,42,43,44,45,47,48,49,51,52,54,55,56,61,62,66] offer immediate and easy-to-use ways of providing care remotely during the current pandemic than store-forward services such as E-mail, fax, forums, file transfer technologies, and prerecorded multimedia.[17,27,34,37,40,41,44,45,52,61] However, some studies suggested the use of combined approach during the COVID-19 pandemic.[17,37,39,41,51] Telemedicine data exchange templates contain different content ranges from plain text, text-numerical, and even image transfer via real-time technologies[40,41,43,45,48,49,51,56,62,66] and nonreal-time platforms;[17,27,34,37,40,41,44,45,61] synchronous[37,39,41,42,43,45,47,48,49,51,54,55,61,66] and asynchronous[47,52,61] voice transfer infrastructures; and finally online video calls or real-time teleconferencing[7,17,27,37,39,40,41,42,43,44,45,47,48,49,51,52,54,55,56,57,61,62,66] and prerecorded (store forward) video transmission technologies.[34,47,52,61]
Discussion
In the COVID-19 pandemic, given the lack of definitive and effective treatment, social isolation and containment strategies[70] have been the best preventive interventions, creating a compelling reason for traditional office encounter alternatives.[46] Application of telemedicine technology, especially with the aim of maintaining social distancing, provides a great potential to minimize the possibility of cross-contamination and nosocomial infections.[71] With this transition, telemedicine is being leveraged with huge quickness and large scale to combat the outbreak.[15,72] In this situation, the delivery of health care throughout the world has brought sweeping changes. One of the most important achievements of this change is coincidence of COVID-19 crisis with incremental adoption of telemedicine services.[73] The COVID-19 emergency also encouraged governments, health authorities, and payers to support extended use of virtual health care. This transition should be regarded as a potential win-win circumstance in every way, which makes for more cost-effectiveness and sustainable health-care systems internationally.[61,74] Hence, the aim of this study was the review of tele-COVID applications to identify the most common and effective services in terms of their interaction mode, time, and purpose.
In the time of the COVID-19 emergency, government-posed social distancing requires crucial importance to establishing communication infrastructures for virtual care models, in which the patient is geographically separated from health-care providers.[74,75] Combining the functions of online conversation and real-time clinical data exchange technologies, technical support can be provided to the emerging need for workflow virtualization. Virtual care delivery can be synchronous or asynchronous. Each mode has different IT infrastructure requirements. Synchronous telemedicine involves virtual meetings that happen in a timely manner, usually involving two-way interaction using audio and video to avoid the need for an in-person visit. Synchronous meetings should be used when conversation is necessary, such as during new patient consultations, preoperative visits, postoperative assessments, and follow-up visits. This session can be conducted for both new and established patients as well as consults. Asynchronous telemedicine involves the collecting, brief, storing, and exchanging of data for a patient or, more often, another provider to review at a later time.[18,50,69]
Some studies have been focused on the application of interaction modalities for providing remotely or virtual care during the COVID-19 pandemic. Mann et al. in their study stated that virtual visits in real-time sessions for VUC cases require an effective open interaction than nonemergency cases (NUC).[39] Shokri and Lighthall, in their study demonstrated that store-and-forward services are appropriate when applied in NUC scenarios or in the routine delivery of patient care.[28] Contreras et al., in their study showed that open two-way interactive is one of the most important factors in the success of these systems in managing COVID-19. Their study also revealed that using real-time interactive methods is more effective and efficient than nonreal-time types.[7] Wosik et al. stated that although real-time video-conferencing is preferable for patients during COVID-19, it is complex, expensive, and requires access to a high-bandwidth internet connection.[74] Mouchtouris et al. stated that rapid adoption of virtual care is depending on a robust telemedicine infrastructure. They also stated the accessibility of high-bandwidth internet connection and complex telecommunication requirements are necessary to facilitate online video-based visits.[76]
Similarly, in the current study, our findings demonstrate that the accessibility to real-time infrastructures for timely transmission video calls and video conference data is most required to meet the needs of patient population according to “stay-at-home” restrictions. It is suggested that during this crisis, customized smartphone apps must be designed in the form of real-time tele-COVID services. In addition, the high capabilities of the mass/social media (such as TV, Facebook, and Telegram) in remote management of these situations should not be overlooked. On the other hand, some basic technologies such as E-mail, online chat, short message service, and telephone calls, despite being simpler and more available, violate effective interaction between patient and provider, particularly in emergency situations. However, due to the importance of maintaining social isolation and the use of tele-COVID for remote disease management, most studies stressed on real-time, live (synchronous), and reciprocal interaction modes.[37,39,41,44,45,47,56,61] Adoption of tele-COVID services with regard to its virtual care modes, purposes, interaction approaches, and scheduling attributes, plays a significant role in preventing latency in information exchanges and network outages.
This study opens opportunities for introducing the available technological and telecommunicational capacities to provide tele-COVID services and maintaining social distances by reducing the need for face-to-face visits. In addition, it will pave the way for health-care industries in designing customized tele-COVID modalities for remote patient management. However, the results will need further investigation from the patients', providers', and IT experts’ perspectives.
While telemedicine precludes the physical examination of a patient, this can be overwhelmed by through using video-enabled conferencing for visits. Furthermore, it allows collection of a range of information prior to a patient's admission, and may therefore be used in preoperative assessment. The standardization of virtual examinations and the privacy concerns related to virtual visits are the next steps in improving the utility of telemedicine during this pandemic. Our systematic review holds three restrictions. Initially, it is likely that some pertinent studies were not taken into account because they have been published in languages other than English (e.g., Chinese). Second, we did not have access to some other databases such as CINAHL and PsycINFO. Finally, due to our search inclusion/exclusion criteria (tele-COVID studies conducted in 2020), we have missed some valuable studies in this field.
Conclusion
The COVID-19 outbreak is converting the telemedicine landscape with rapid transition. In the current crisis, active and consistent patient engagement through robust, applicable, and affordable telemedicine services can help health-care system to successfully manage this contagious. To our knowledge, tele-COVID has the potential to solve many problems in this crisis, but its potential has not yet well described and taken into more consideration from patients’ perspective and literature review. Video calls in the form of social medias or special apps, real-time video-conference platforms, and personal webcam represent a valuable strategy for enabling effective and real-time patient communication and render health-care services, while limitations exist, specifically with technical difficulties and low bandwidths. Finally, designing special communication software (e.g., Zoom, Dogpile, and Epic) or customizing the current messenger apps (e.g., WhatsApp, Telegram, and WeChat) in the context of universal smart phones, is one of the popular and convenience options to provide tele-COVID services.
In conclusion, it is noted that the results of the present study can be used for other possible future pandemics and natural disasters. The future researches should focus on novel telecommunication and telematics approaches especially in the field of new generation and high-bandwidth networks. These innovations could be applied to diminish the destructive effects of probable future pandemics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article is extracted from a research project supported by Abadan University of Medical Sciences with ethical code IR.ABADANUMS.REC.1399.074. We also thank the Research Deputy of Abadan University of Medical Sciences for financially supporting this project.
References
- 1.Araz OM, Ramirez-Nafarrate A, Jehn M, Wilson FA. The importance of widespread testing for COVID-19 pandemic: Systems thinking for drive-through testing sites. Health Syst (Basingstoke) 2020;9:1–5. doi: 10.1080/20476965.2020.1758000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vadukul P, Sharma DS, Vincent P. Massive pulmonary embolism following recovery from COVID-19 infection: Inflammation, thrombosis and the role of extended thromboprophylaxis. BMJ Case Rep. 2020;13:e238168. doi: 10.1136/bcr-2020-238168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bahl P, de Silva C, Bhattacharjee S, Stone H, Doolan C, Chughtai AA, et al. Droplets and Aerosols generated by singing and the risk of COVID-19 for choirs. Clin Infect Dis. 2020 Sep 18;12(41):157. doi: 10.1093/cid/ciaa1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao Y, Chen Q, Guo Q, Chen N, Hou W, Wang Y, et al. Performing EUS during COVID-19 postendemic period: A report from endoscopy center in Wuhan. Endosc Ultrasound. 2020;27:37–46. doi: 10.4103/eus.eus_37_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arefi MF, Poursadeqiyan M. A review of studies on the COVID-19 epidemic crisis disease with a preventive approach. Work. 2020;66:717–29. doi: 10.3233/WOR-203218. [DOI] [PubMed] [Google Scholar]
- 6.Matouk AE. Complex dynamics in susceptible-infected models for COVID-19 with multi-drug resistance. Chaos Solitons Fractals. 2020;140:1–13. doi: 10.1016/j.chaos.2020.110257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Contreras CM, Metzger GA, Beane JD, Dedhia PH, Ejaz A, Pawlik TM. Telemedicine: Patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg. 2020;24:1692–7. doi: 10.1007/s11605-020-04623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gates B. Responding to COVID-19 – A once-in-a-century pandemic? N Engl J Med. 2020;382:1677–9. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 9.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Webb R. COVID-19 and lockdown: living in 'interesting times'. J Wound Care. 2020 May 2;29(5):243. doi: 10.12968/jowc.2020.29.5.243. [DOI] [PubMed] [Google Scholar]
- 12.Mikolajczyk D, Schubert J, Khosrawipour T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020 May 18;27(3):37. doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 Pandemic, Lessons for the Future. Telemed J E Health. 2020 May;26(5):571–573. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 14.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: Challenges and opportunities for innovation. J Adolesc Health. 2020;67:164–71. doi: 10.1016/j.jadohealth.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rockwell KL, Gilroy AS. Incorporating telemedicine as part of COVID-19 outbreak response systems. Am J Manag Care. 2020;26:147–8. doi: 10.37765/ajmc.2020.42784. [DOI] [PubMed] [Google Scholar]
- 16.Fix OK, Serper M. Telemedicine and telehepatology during the COVID-19 pandemic. Clin Liver Dis. 2020;15:187. doi: 10.1002/cld.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang S, Thomas PBM, Sim DA, Parker RT, Daniel C, Uddin JM. Oculoplastic video-based telemedicine consultations: COVID-19 and beyond. Eye (Lond) 2020;34:1–3. doi: 10.1038/s41433-020-0953-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rao SS, Loeb AE, Amin RM, Golladay GJ, Levin AS, Thakkar SC. Establishing telemedicine in an academic total joint arthroplasty practice: Needs and opportunities highlighted by the COVID-19 Pandemic. Arthroplast Today. 2020;6:617–22. doi: 10.1016/j.artd.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu R, Sundaresan T, Reed ME, Trosman JR, Weldon CB, Kolevska T. Telehealth in oncology during the COVID-19 outbreak: Bringing the house call back virtually. JCO Oncol Pract. 2020;16:289–93. doi: 10.1200/OP.20.00199. [DOI] [PubMed] [Google Scholar]
- 20.Al-Benna S. Availability of COVID-19 information from national and international aesthetic surgery society websites. Aesthetic Plast Surg. 2020;44:1043–6. doi: 10.1007/s00266-020-01751-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26:309–13. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489–91. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fatyga E, Dzięgielewska-Gęsiak S, Wierzgoń A, Stołtny D, Muc-Wierzgoń M. The coronavirus disease 2019 pandemic: Telemedicine in elderly patients with type 2 diabetes. Pol Arch Intern Med. 2020;130:452–4. doi: 10.20452/pamw.15346. [DOI] [PubMed] [Google Scholar]
- 24.Reiss AB, De Leon J, Dapkins IP, Shahin G, Peltier MR, Goldberg ER. A Telemedicine approach to Covid-19 assessment and triage. Medicina (Kaunas) 2020 Sep 10;56(9):461. doi: 10.3390/medicina56090461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wahezi SE, Duarte RV, Yerra S, Thomas MA, Pujar B, Sehgal N, et al. Telemedicine during COVID-19 and beyond: A practical guide and best practices multidisciplinary approach for the orthopedic and neurologic pain physical examination. Pain Physician. 2020;23:S205–S238. [PubMed] [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: Telemedicine in a COVID-19 Era. Am J Ophthalmol. 2020;216:237–42. doi: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shokri T, Lighthall JG. Telemedicine in the Era of the COVID-19 pandemic: Implications in facial plastic surgery. Facial Plast Surg Aesthet Med. 2020;22:155–6. doi: 10.1089/fpsam.2020.0163. [DOI] [PubMed] [Google Scholar]
- 29.Boehm K, Ziewers S, Brandt MP, Sparwasser P, Haack M, Willems F, et al. Telemedicine online visits in urology during the COVID-19 pandemic – Potential, risk factors, and patients’ perspective. Eur Urol. 2020;78:16–20. doi: 10.1016/j.eururo.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shipchandler TZ, Nesemeier BR, Parker NP, Vernon D, Campiti VJ, Anthony BP, et al. Telehealth opportunities for the otolaryngologist: A silver lining during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020;163:112–3. doi: 10.1177/0194599820929641. [DOI] [PubMed] [Google Scholar]
- 31.Gutierrez J, Kuperman E, Kaboli PJ. Using telehealth as a tool for rural hospitals in the COVID-19 pandemic response. J Rural Health. 2020 Apr;11:10. doi: 10.1111/jrh.12443. 1111/jrh. 12443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chou E, Hsieh YL, Wolfshohl J, Green F, Bhakta T. Onsite telemedicine strategy for coronavirus (COVID-19) screening to limit exposure in ED. Emerg Med J. 2020;37:335–7. doi: 10.1136/emermed-2020-209645. [DOI] [PubMed] [Google Scholar]
- 33.Del Hoyo J, Aguas M. Implementing telemedicine in inflammatory bowel disease: Is COVID-19 the definitive trigger? Gastroenterol Hepatol. 2020;43:415–7. doi: 10.1016/j.gastrohep.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghai B, Malhotra N, Bajwa SJS. Telemedicine for chronic pain management during COVID-19 pandemic. Indian J Anaesth. 2020;64:456–62. doi: 10.4103/ija.IJA_652_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daggubati LC, Eichberg DG, Ivan ME, Hanft S, Mansouri A, Komotar RJ, et al. Telemedicine for outpatient neurosurgical oncology care: Lessons learned for the future during the COVID-19 pandemic. World Neurosurg. 2020;139:e859–63. doi: 10.1016/j.wneu.2020.05.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berg EA, Picoraro JA, Miller SD, Srinath A, Franciosi JP, Hayes CE, et al. COVID-19 – A guide to rapid implementation of telehealth services: A playbook for the pediatric gastroenterologist. J Pediatr Gastroenterol Nutr. 2020;70:734. doi: 10.1097/MPG.0000000000002749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grimes CL, Balk EM, Crisp CC, Antosh DD, Murphy M, Halder GE, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID-19 pandemic: Review of existing evidence. Int Urogynecol J. 2020;31:1063–89. doi: 10.1007/s00192-020-04314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, et al. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed J E Health. 2020;26:377–9. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 39.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc. 2020;27:1132–5. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gadzinski AJ, Andino JJ, Odisho AY, Watts KL, Gore JL, Ellimoottil C. Telemedicine and eConsults for hospitalized patients during COVID-19. Urology. 2020;141:12–4. doi: 10.1016/j.urology.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee AC. COVID-19 and the advancement of digital physical therapist practice and telehealth. Phys Ther. 2020;100:1054–7. doi: 10.1093/ptj/pzaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rogers BG, Coats CS, Adams E, Murphy M, Stewart C, Arnold T, et al. Development of telemedicine infrastructure at an LGBTQ+ clinic to support HIV prevention and care in response to COVID-19, Providence, RI. AIDS Behav. 2020;24:2743–7. doi: 10.1007/s10461-020-02895-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goodman-Casanova JM, Dura-Perez E, Guzman-Parra J, Cuesta-Vargas A, Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: Survey study. J Med Internet Res. 2020;22:e19434. doi: 10.2196/19434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mihalj M, Carrel T, Gregoric ID, Andereggen L, Zinn PO, Doll D, et al. Telemedicine for preoperative assessment during a COVID-19 pandemic: Recommendations for clinical care. Best Pract Res Clin Anaesthesiol. 2020;34:345–51. doi: 10.1016/j.bpa.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Punia V, Nasr G, Zagorski V, Lawrence G, Fesler J, Nair D, et al. Evidence of a rapid shift in outpatient practice during the COVID-19 pandemic using telemedicine. Telemed J E Health. 2020;26:1301–3. doi: 10.1089/tmj.2020.0150. [DOI] [PubMed] [Google Scholar]
- 46.Triantafillou V, Rajasekaran K. A commentary on the challenges of telemedicine for head and neck oncologic patients during COVID-19. Otolaryngol Head Neck Surg. 2020;163:81–2. doi: 10.1177/0194599820923622. [DOI] [PubMed] [Google Scholar]
- 47.Mgbako O, Miller EH, Santoro AF, Remien RH, Shalev N, Olender S, et al. COVID-19, telemedicine, and patient empowerment in HIV care and research. AIDS Behav. 2020;24:1990–3. doi: 10.1007/s10461-020-02926-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moring JC, Dondanville KA, Fina BA, Hassija C, Chard K, Monson C, et al. Cognitive processing therapy for posttraumatic stress disorder via telehealth: practical considerations during the COVID-19 pandemic. J Trauma Stress. 2020 May;13:10. doi: 10.1002/jts.22544. 1002/jts. 22544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pollock K, Setzen M, Svider PF. Embracing telemedicine into your otolaryngology practice amid the COVID-19 crisis: An invited commentary. Am J Otolaryngol. 2020;41:102490. doi: 10.1016/j.amjoto.2020.102490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation Guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J Am Coll Surg. 2020;231:216–2200. doi: 10.1016/j.jamcollsurg.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee AK, Cho RH, Lau EH, Cheng HK, Wong EW, Ku PK, et al. Mitigation of head and neck cancer service disruption during COVID-19 in Hong Kong through telehealth and multi-institutional collaboration. Head Neck. 2020;42:1454–9. doi: 10.1002/hed.26226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nagra M, Vianya-Estopa M, Wolffsohn JS. Could telehealth help eye care practitioners adapt contact lens services during the COVID-19 pandemic? Cont Lens Anterior Eye. 2020;43:204–7. doi: 10.1016/j.clae.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zughni LA, Gillespie AI, Hatcher JL, Rubin AD, Giliberto JP. Telemedicine and the Interdisciplinary Clinic Model: During the COVID-19 Pandemic and Beyond. Otolaryngol Head Neck Surg. 2020;163:673–5. doi: 10.1177/0194599820932167. [DOI] [PubMed] [Google Scholar]
- 54.Prasad A, Carey RM, Rajasekaran K. Head and neck virtual medicine in a pandemic era: Lessons from COVID-19. Head Neck. 2020;42:1308–9. doi: 10.1002/hed.26174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Prasad A, Brewster R, Newman JG, Rajasekaran K. Optimizing your telemedicine visit during the COVID-19 pandemic: Practice guidelines for patients with head and neck cancer. Head Neck. 2020;42:1317–21. doi: 10.1002/hed.26197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Layfield E, Triantafillou V, Prasad A, Deng J, Shanti RM, Newman JG, et al. Telemedicine for head and neck ambulatory visits during COVID-19: Evaluating usability and patient satisfaction. Head Neck. 2020;42:1681–9. doi: 10.1002/hed.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tenforde AS, Iaccarino MA, Borgstrom H, Hefner JE, Silver J, Ahmed M, et al. Feasibility and high quality measured in the rapid expansion of telemedicine during COVID-19 for sports and musculoskeletal medicine practice. PM&R. 2020;12(9):154. doi: 10.1002/pmrj.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vaishya R, Javaid M, Khan IH, Haleem A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab Syndr. 2020;14:337–9. doi: 10.1016/j.dsx.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sullivan AB, Kane A, Roth AJ, Davis BE, Drerup ML, Heinberg LJ. The COVID-19 crisis: A mental health perspective and response using telemedicine. J Patient Exp. 2020;7:295–301. doi: 10.1177/2374373520922747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gadzinski AJ, Ellimoottil C. Telehealth in urology after the COVID-19 pandemic. Nat Rev Urol. 2020;17:363–4. doi: 10.1038/s41585-020-0336-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peters AL, Garg SK. The silver lining to COVID-19: Avoiding diabetic ketoacidosis admissions with telehealth. Diabetes Technol Ther. 2020;22:449–53. doi: 10.1089/dia.2020.0187. [DOI] [PubMed] [Google Scholar]
- 62.Serper M, Cubell AW, Deleener ME, Casher TK, Rosenberg DJ, Whitebloom D, et al. Telemedicine in liver disease and beyond: Can the COVID-19 crisis lead to action? Hepatology. 2020;72:723–8. doi: 10.1002/hep.31276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aziz A, Zork N, Aubey JJ, Baptiste CD, D’Alton ME, Emeruwa UN, et al. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am J Perinatol. 2020;37:800–8. doi: 10.1055/s-0040-1712121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parikh A, Kumar AA, Jahangir E. Cardio-oncology care in the time of COVID-19 and the role of telehealth. JACC CardioOncol. 2020;2:356–8. doi: 10.1016/j.jaccao.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Parisien RL, Shin M, Constant M, Saltzman BM, Li X, Levine WN, et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:e487–e492. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A call to action. JMIR Public Health Surveill. 2020;6:e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Goodman CW, Brett AS. Accessibility of virtual visits for urgent care among US hospitals: A descriptive analysis. J Gen Intern Med. 2020 May 18;:1–2. doi: 10.1007/s11606-020-05888-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Koziatek CA, Rubin A, Lakdawala V, Lee DC, Swartz J, Auld E, et al. Assessing the impact of a rapidly scaled virtual urgent care in New York City during the COVID-19 pandemic. J Emerg Med. 2020;59:610–8. doi: 10.1016/j.jemermed.2020.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hakim AA, Kellish AS, Atabek U, Spitz FR, Hong YK. Implications for the use of telehealth in surgical patients during the COVID-19 pandemic. Am J Surg. 2020;220:48–9. doi: 10.1016/j.amjsurg.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.El-Lababidi RM, Mooty M, Bonilla MF, Salem NM. Treatment of severe pneumonia due to COVID-19 with peginterferon alfa 2a. IDCases. 2020;21:e00837. doi: 10.1016/j.idcr.2020.e00837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nahm WJ, Badiavas EV, Kirsner RS, Nichols AJ, Harris ZC, Phillips AR, et al. Treating keratinocyte carcinomas with a combination of imiquimod, 5-fluorouracil, and tretinoin using store-and-forward telemedicine in the age of coronavirus disease 2019 to promote social distancing. JAAD Case Rep. 2020;6:931–4. doi: 10.1016/j.jdcr.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chowdhury SR, Sunna TC, Ahmed S. Telemedicine is an important aspect of healthcare services amid COVID-19 outbreak: Its barriers in Bangladesh and strategies to overcome. Int J Health Plann Manage. 2020 Aug 28; doi: 10.1002/hpm.3064. [DOI] [PubMed] [Google Scholar]
- 73.Klein BC, Busis NA. COVID-19 is catalyzing the adoption of teleneurology. Neurology. 2020;94:903–4. doi: 10.1212/WNL.0000000000009494. [DOI] [PubMed] [Google Scholar]
- 74.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957–62. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Olayiwola JN, Magaña C, Harmon A, Nair S, Esposito E, Harsh C, et al. Telehealth as a bright spot of the COVID-19 pandemic: Recommendations from the virtual frontlines (“Frontweb”) JMIR Public Health Surveill. 2020;6:e19045. doi: 10.2196/19045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mouchtouris N, Lavergne P, Montenegro TS, Gonzalez G, Baldassari M, Sharan A, et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–94. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]


