Abstract
Although many studies have examined broad patterns of effects on pregnancy and infant outcomes after disasters, the causes of adverse outcomes are not always clear. Disasters cause interrelated exposure to environmental pollutants, psychological stressors, and lack of health care, and interacts with other social determinants of health. This topical review examines the short- and long-term effects of disasters on pregnancy and how they are mediated by social, behavioral, and environmental effects. In the short term, disasters are associated with physical trauma, adverse environmental exposures, and unstable housing. In the longer term, disasters may lead to relocation, changes in family functioning, and negative economic effects. These aspects of disaster exposure, in turn, lead to lack of access to health care, increased stress and negative mental health outcomes, and negative behavioral changes, including smoking and substance use, poor nutrition, physical overexertion and limited activity, and reduction in breastfeeding. All of these factors interact with social determinants of health to worsen effects on the most vulnerable women, infants, and communities. Few interventions after disasters have been tested. With the increase in disasters due to climate change and the ongoing coronavirus pandemic, the models of effects of disasters and their human health consequences need increasing refinement, and, more importantly, should be applied to interventions that improve disaster prevention, mitigation, and response.
Keywords: disaster, pregnancy, environment, tropical cyclones, birthweight
Introduction
The natural world and human influences work together to create the devastation that follows a major disaster such as a hurricane. Although many studies have examined broad patterns of effects on pregnancy outcomes after disasters,1 the causes of adverse outcomes are not always clear, as there are interrelated environmental pollutant exposures, psychological stressors, lack of health care, all moderated by social determinants of health. Without understanding which aspects of disaster exposure are the most meaningful contributors to adverse outcomes, it will not be possible to establish proactive disaster responses that efficiently target the most important factors and protect pregnant women. This topical review examines the traditionally expected short-term disaster exposures such as storm damage, health care closures as well as environmental and longer-term effects on pregnancy-related outcomes. In this review, we follow the World Health Organization’s definition of disaster, “A serious disruption of the functioning of a community or a society causing widespread human, material, economic or environmental losses which exceed the ability of the affected community or society to cope using its own resources,”2 with a particular focus on the short- and longer term effects of natural and technological disasters. Several possible downstream effects of disaster exposure on pregnant women have been identified, including adverse birth outcomes, pregnancy loss, birth defects, and adverse child development, all of which have potential long-term or lifelong effects.3, 4 Surveillance after Hurricane Katrina found that 3% of evacuees had an emergency room visit for obstetric reasons and 13–15% of evacuees had a need for WIC (Special Supplemental Nutrition Program for Women, Infants and Children) services or birth control,5 suggesting this is not a small population of public health concern. Figure 1 depicts the multidimensional nature of the impact of disasters on pregnant women and infants. The conceptual model demonstrates the complex interactions among physical, chemical, and non-chemical stressors and the impacts on prenatal and perinatal health. Furthermore, the model takes into account the short-term, often more identified effects, as well as the more protracted long-term consequences closely connected to existing burdens of health- and socio-economic disparities.
Figure 1.
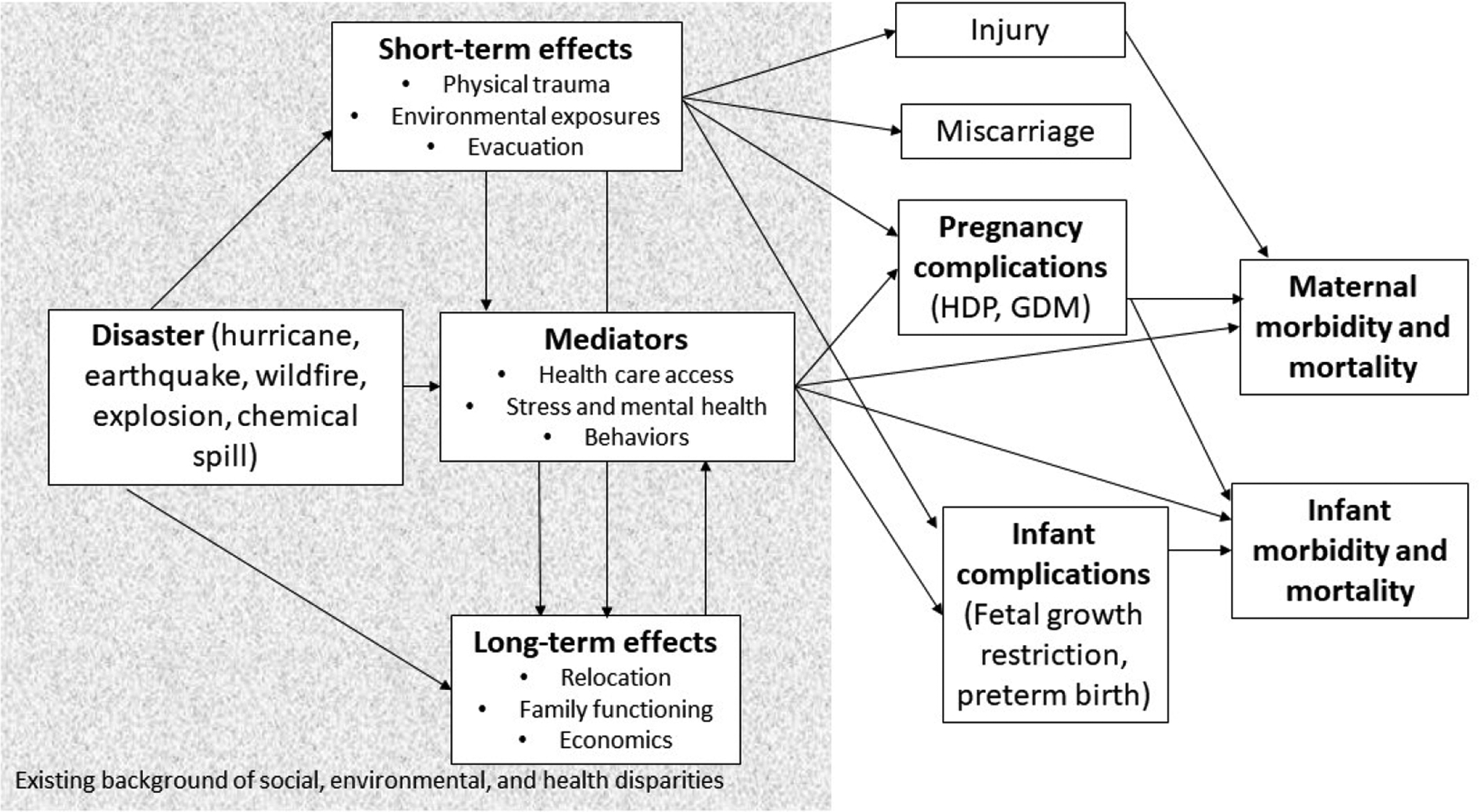
Conceptual model representing the short- and long-term effects of disasters on pregnant women and their infants. Arrows represent causal relationships.
HDP, hypertensive disorders of pregnancy; GDM, gestational diabetes mellitus
Proposed Framework
Short-term effects
Physical trauma
Disasters bring several inherent risks, such as those associated with structural damage and vegetation collapse, involving increased risk of injury for anyone directly exposed. Pregnant women are less likely to be injured than some groups as they are more likely to limit their exposure and are not likely to be called upon for physical labor if others are available.6 Still, reduced mobility and changed reflexes and balance associated with pregnancy may create vulnerability to hazards that might otherwise be avoided.7, 8
Environmental exposures
Many disasters are accompanied by secondary environmental exposures. Hurricanes, earthquakes, or extreme precipitation and/or flooding may cause ruptures of storage tanks of chemicals or other hazards, such as animal waste and heavy metals.9 This was vividly shown when the recent landfall of Hurricane Laura (2020) caused a major fire at a chlorine production plant in Lake Charles, LA.10 Flooding is frequently accompanied by mold infestation, especially in hot and humid climates such as the U.S. Gulf Coast where summer temperatures can reach three digit levels (Fahrenheit).11, 12 Chemical exposure (see13 for review), heat, and mold may cause short and long-term effects on pregnancy health, including increases in congenital anomalies, low birthweight, and preterm birth.14–17
Communities often suffer a double burden of vulnerability associated with exposures to natural disasters and environmental contaminants. Figure 2 illustrates the geography of recent overlapping hazards in Florida. The figure shows the location of hurricanes Irma and Michael that made landfall in Florida in 2017 and 2018 respectively,18 and their interaction with environmental hazards: the U.S Environmental Protection Agency’s regulated abandoned and current hazardous waste facilities19, 20 and the Karenia brevis (“red tide”) algal bloom formed and spread during this period.21 Harmful algal blooms (HAB) are an example of an environmental exposure that has increased in recent years,22, 23 and is of concern to pregnant women given the associations with spontaneous abortions and premature births in animals.24–27 Combined exposures to natural disasters and environmental contaminants increase vulnerability, not only because these increase the overall burden of health-harming exposures, but also because the exposures may interact (i.e., hurricane storm surge may increase community exposure to HAB) possibly potentiating or synergistically impacting the adverse health outcome of concern, in this case adverse birth outcomes.
Figure 2.
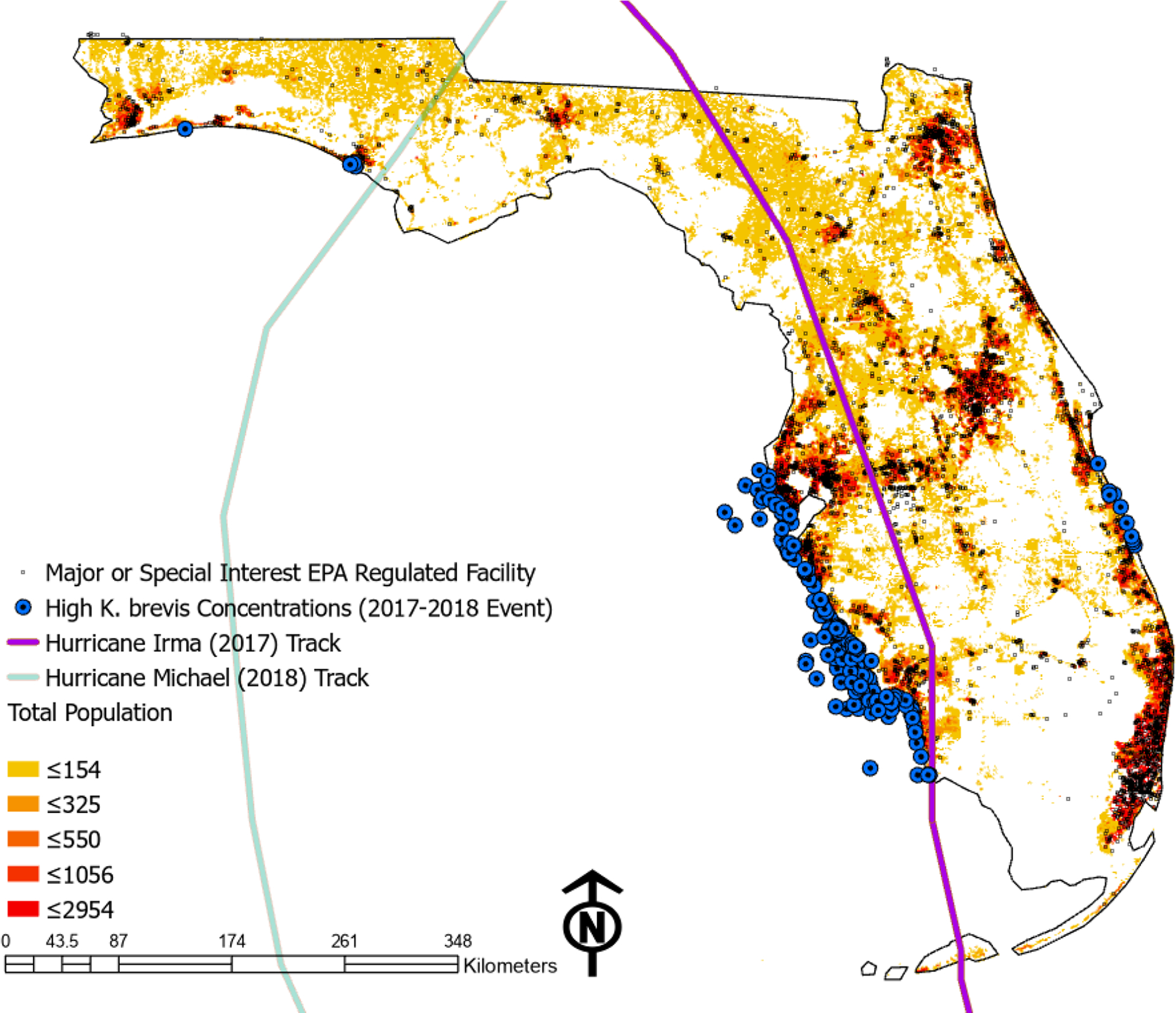
Joint environmental hazards and disasters, Florida, 2017–2018.
Exposure to disasters is also often co-extensive with exposure to extreme temperatures. Extended periods of extreme heat are not historically considered as emergencies under the Pandemic and All Hazard Preparedness Act of 2006 (amended as the Pandemic and All-Hazards Preparedness and Advancing Innovation Act of 2019), although such events would frequently meet the definition of disaster given above. High heat has been associated with placental abruption,28 preterm birth and low birthweight,29, 30 birth defects,31, 32 and stillbirth.33 In many locations, extreme heat co-occurs with high air pollution (PM2.5, O3) levels which are consistently linked to preterm birth, low birthweight, and stillbirth.33 About half of the published extreme heat and air pollution studies found health disparities, where Black mothers faced higher risks of negative birth outcomes from heat exposure than white mothers.33 Lower-income households are less likely to have central air conditioning and more likely to struggle to pay electric bills or repair cooling equipment and experience heat-related illness symptoms.34, 35
Extreme precipitation events in both the cold and warm seasons may also influence birth outcomes. Disasters in winter, such as ice storms, may increase exposure to cold,36 which has sometimes been associated with adverse birth outcomes.37–40 Flooding from tropical storms and hurricanes can lead to increases in disease transmitting mosquitoes, with concomitant increase in the risk of diseases like Zika, dengue, and malaria;41, 42 droughts and flooding can affect triatomine prevalence, leading to changes in risk of Chagas disease.43 These effects on vector-borne infection can be long-term rather than short-term,44 and are associated with congenital anomalies (Zika),45 pre-eclampsia, preterm birth (dengue),46 and vertical transmission of infection (Chagas).47
A defining characteristic of disaster is disruption of housing. Temporary housing is often limited or substandard and may increase exposure to heat and cold. After Hurricane Irma, non-white and poorer households were much less likely to have a generator and backup electricity.48 In addition, lack of electricity means many people use generators, which may lead to carbon monoxide exposure.49 Carbon monoxide poisoning during pregnancy is associated with fetal demise, severe neurological complications, intrauterine growth retardation, preterm delivery, and birth defects.50 Evacuation offers risk of its own – transportation accidents, dehydration, malnutrition, and lack of access to medications or medical care, in some cases requiring evacuation during labor or birth.51 Depending on the severity of disaster and location, quality of housing during the evacuation or in new locations may be poor or nonexistent. All of these are risky for pregnant women; for instance, preterm labor may be triggered by acute trauma,52 physical exertion, environmental exposures, or heat.
Long-term effects
Relocation
Short-term relocation may become long-term relocation, or, in some cases, refugee status. Relocation is associated with worse mental health53 and physical health indicators.54 Pregnant women who are displaced are less likely to access prenatal, delivery, and postnatal care.55 Refugee status is associated with worse mental health,56 maternal mortality, and preterm birth.57
Family functioning
Family functioning is often affected adversely by disasters, starting with basic family structure. Divorce has been found to increase in the aftermath of some disasters (Hurricane Hugo, Southeastern United States, 1989).58 Disasters with a high death toll are likely to lead to an eventual rise in remarriage among widowed people (Wenchuan earthquake, China, 2008),59 and in some cases marriage rates have risen after less severe disasters (Hurricane Hugo).58 Unmarried women and women without partners are at higher risk for pregnancy-related morbidity and adverse birth outcomes,60, 61 as are women who are in abusive or unsupportive relationships.62 Several sociologists and gender theorists have drawn attention to increases in intimate partner violence and child abuse after disaster,63–67 and severe experience of disasters is also often associated with worse self-reported family functioning.68, 69 Women who experience intimate partner violence are at higher risk for pregnancy complications and adverse birth outcomes,70 while women who experience abuse as children may be at higher risk for pregnancy-related morbidity.71–73 Worse family functioning is also associated with worse birth outcomes.73, 74 On the broader scale, disasters impact both individual and community resilience and can disrupt social networks; the National Academies of Sciences, Engineering, and Medicine in its report “Building and Measuring Community Resilience” identified social cohesion as a key factor influencing community resilience.75
Economics
Disasters cause short- and long-term economic effects on the micro and macro scales.76 Job loss is common after disasters (although in some cases rebuilding provides jobs, or changes the composition of the workforce, as the influx of Hispanic workers to New Orleans post-Hurricane Katrina (2005) demonstrated. This tends to be more relevant to men, as many of the positions are in construction, although a growing number of women have also joined the construction sector.). Even among those employed and insured, the money required to replace possessions and to mitigate the disaster through evacuation or, for example, generator purchase, can be substantial. The disparities in pregnancy outcomes between lower- and higher-income families are well-known, as is the association between financial stress and adverse outcomes,77, 78 which may be exacerbated by the negative financial consequences of the disasters.
Short- and long-term mediators
Health care access
Post-disaster, health care providers often close temporarily or permanently. If jobs or savings are lost, lack of insurance or money for services may also make accessing care difficult. Even if care providers are available, the stress of the disaster, evacuation, and demands of recovery and rebuilding may mean that women do not access care as promptly as would be optimal. Access to medications may be limited post-disaster, either from supply chain or economic reasons. Reproductive healthcare is often de-prioritized post-disaster by clinicians, disaster agencies, and the general population, which may lead to lack of availability of birth control.79, 80 Relief agencies’ values may conflict with communities’ beliefs: contraception may be counter to local cultural or religious norms and its provision, especially to adolescents or unmarried people, controversial. Combined with the common post-disaster increase in the need to prevent pregnancy (as many families tend to avoid a pregnancy in the immediate aftermath), this can lead to a large unmet contraceptive need, which may manifest in increases in unplanned pregnancy, as was seen after Hurricane Katrina.81 Unplanned pregnancies, especially under difficult conditions, are associated with worse health outcomes for mothers and babies.82
Prenatal clinics usually close, at least in the short term, after a disaster. Thus, many pregnant women are likely to miss prenatal care visits. Studies post-disaster tend to find an increase in the proportion of women receiving late or inadequate prenatal care (Hurricane Katrina and Michael),83, 84 although the effect is not as consistent as might be expected (Red River flooding, North Dakota, 1997; El Niño floods, Ecuador, 1997–8).85, 86 The likely effect of lapses in prenatal care after disasters is not altogether clear. Some studies indicate that the number of prenatal care visits can be reduced for low-risk women without significant harm to maternal or infant health,87 and prenatal care has not been conclusively demonstrated to reduce low birthweight, although the correlation is strong.88. More directly tied to the ability to access care is treatment for complications such as gestational diabetes, infectious conditions such as HIV and syphilis,89, 90 and potential indications for delivery such as pre-eclampsia and reduced fetal growth. In countries without universal health care, concerns about cost and insurance coverage are barriers to receiving care, even though access to insurance is often expanded post-disaster.91
Stress and mental health
Disasters are a cause of trauma and severe stress, which have been directly linked to several pregnancy complications.92 Stress can raise blood pressure during pregnancy,93 which is an issue in itself and also predisposes to reduced fetal growth and preterm birth.94 Altered levels of stress hormones such as cortisol and CRH have been associated with pregnancy complications,95 particularly preterm birth.96 Stress may also increase vulnerability to infection;97 infections including bacterial vaginosis,98 group B strep,99 chlamydia, and gonorrhea100 all have negative effects on birth outcomes. Disaster exposure is also a risk factor for postpartum depression,101 one of the most common perinatal mental health disorders, and associated with maternal impairment, poorer quality parenting, negative child behavior, and poorer cognitive development.102
Behaviors
Smoking:
Tobacco use is well-known to be associated with pregnancy complications, most notably reduced fetal growth and birthweight, but also preterm birth. In the aftermath of disasters, smokers may smoke more as a response to stress; those who have quit may relapse; and intentions to quit may be postponed.103 Similar considerations apply to other types of substance use,104, 105 and addiction treatment, seldom tailored for pregnant women, may be even less available than usual.
Diet:
Malnutrition in various forms may follow in the aftermath of disasters. In areas where the food supply is insecure, disasters may lead to limited food supplies or even famine; in addition, access to foods rich in essential micronutrients may be limited. For instance, hurricane effects on folic acid-containing foods were believed to be related to a subsequent spike in neural tube defects (Hurricane Gilbert, Jamaica, 1988).106 In settings where food availability is generally good but sometimes uneven, low-income women have been found to be particularly vulnerable to post-disaster food insecurity (Hurricane Katrina).107 In other cases, food quality rather than overall energy intake may be affected. People are likely to prioritize practical (nonperishable) and affective (appetizing, varied) considerations over strictly nutritional ones,108 which can lead to weight gain.109 Severe nutrient restriction is associated with fetal growth restriction and preterm birth, while excessive weight gain is associated with pregnancy complications such as gestational diabetes and pre-eclampsia, as well as labor and delivery complications (shoulder dystocia, caesarean section).110
Physical activity:
Physical overexertion, which may be caused by assisting in disaster cleanup, can trigger preterm birth. Leisure or health-related physical activity, which generally improves health, is likely to be deprioritized post-disaster and exercise facilities, such as gyms or even safe streets or parks for walking or running, may be unavailable (Hurricane Harvey, Texas, 2017).111 Lack of leisure-time activity may negatively affect birth and obstetric outcomes112 and raise the risk of gestational diabetes and hypertension.
Breastfeeding:
Breastfeeding is associated with better health for infant and mother,113 and in a disaster setting, avoids the need for powder and potable water to mix formula. Breastfeeding has sometimes been found to decline post-disaster and formula feeding increase (Great East Japan Earthquake, 2011).114 Many women find breastfeeding difficult without support, which may not be available post-disaster; in addition, milk supply may also be reduced.115 Women may fear breastfeeding if there are chemical exposures.116 Post-disaster, formula is included in relief provisions, which inadvertently may discourage breastfeeding.117
Effects of disasters on maternal and infant outcomes
We have explored the multiple pathways of effects of disasters, which converge on worsened outcomes for mother and infant in the short and long term. Major drivers of maternal morbidity and mortality include pregnancy complications such as hypertensive disorders and gestational diabetes; complications of labor; and cardiovascular conditions. The degree to which these conditions and complications cause sickness and death is strongly predicted by access to quality care. Disasters limit this care directly, by closing clinics and hospitals, and indirectly, by restricting employment possibilities and health insurance. Beyond maternal complications, which directly affect fetal outcomes, major drivers of infant morbidity and mortality are reduced fetal growth and lower gestational age. These are the major focus of our discussion, because other indicators of maternal and infant morbidity are less-studied, in part due to lack of routine data collection or insufficient power to address rarer outcomes, such as maternal and infant mortality.118, 119 These are also strongly affected by maternal exposures, which may include physical trauma and environmental exposures, as well as maternal behaviors and moods that may be worsened by disasters, including health behaviors such as smoking and increased stress levels as noted earlier. The effects of disasters do not, of course, end at birth, and continue to negatively affect maternal postpartum mental health1 and child development.120
Social determinants of health
Although this topic review focuses on downstream effects of disasters, the pre-existing burden of disparities and other social determinants of health cannot be ignored. The National Academies of Science, Engineering, and Medicine identified natural, built, financial, human and cultural, social, and political capitals as social determinants of health (SDH) domains impacting a community’s ability to “bounce back” following disasters (Table 1).75 These six SDH domains influence the ability of a community and its members, including pregnant women, to absorb the impact and recover from disasters.
Table 1.
Domains of community capital and resilience (after75)
| Domain | Examples |
|---|---|
| Natural | ecosystem assets: air, land, water, general environmental quality |
| Built | critical support facilities, residential housing, health facilities, electricity and transportation infrastructure |
| Financial | income levels and equality, employment |
| Human and cultural | demographic characteristics, language competencies, cultural assets and belief systems |
| Social | social networks and connectivity; political, religious, community, and volunteer engagement; sense of belonging |
| Political | access to resources and ability to engage external entities; disaster experience and response structure |
As an example of how these social determinants can influence disaster effects, one study, conducted 5–7 years after Hurricane Katrina, showed African-American pregnant women were more likely than women of other race/ethnicities to have had severe experiences of the hurricane and less likely to perceive that there had been progress in recovery. Severe experiences of Katrina still affected birth outcomes 5–7 years later.121 Analyses of spatial hazards data across the US122 and of hurricane data over 13 years concluded that disasters affected gestational age most in counties classified as socially vulnerable by the CDC.123
Public health implications for disaster planning, response, and resilience
Few controlled trials have addressed health after disasters in pregnant women. Exceptions are interventions after the Fort McMurray fires in Alberta, Canada, which included a randomized trial of bundled interventions including expressive writing exercises.124 However, a similar intervention after Hurricane Harvey was not effective in improving mental health.125 Data collected includes questionnaire data on stress and mental health, and analysis of biomarkers. In other populations, there is increasing use of m-health and E-health interventions, including online interventions after Hurricane Ike (Texas, 2008) to improve mental health and self-efficacy (My Disaster Recovery)126 and Bounce Back Now! after tornadoes in Missouri and Alabama (2011).127 Other programs focus on children rather than mothers, either online (BRAVE online for earthquake, Canterbury, New Zealand, 2011128) or school-based.
Pregnant women have specific needs, including prenatal care; and infants have needs such as diapers, potential supplemental feeding, and childcare. However, interventions that benefit the community as a whole are likely to benefit them, and vice versa – pregnant women and children serve as a concrete symbol of hope and the future.129 Effective financial, community, and services recovery are as likely to be beneficial to physical and mental health in pregnancy as anything else. Supporting communities and helping people support each other is valuable; such support builds self-efficacy, which improves disaster preparedness and recovery as well as mental and physical health,130, 131 including birth outcomes.132
Regardless of type, disasters share common potential adverse outcomes and impacts for pregnant women and infants. Although these results appear quite similar in terms of morbidity and mortality, the pathways have many differing contributing factors. The conceptual model (see Figure 1) illustrates the often synergistic interaction among the different pathways and the resulting impact on maternal and infant morbidity and mortality. This approach allows for opportunities to further delve into the short term, longer term, and overlapping mediators of maternal and child health related to disasters. Our proposed model is supported extensively by the current disaster literature. Nonetheless, research is warranted that allows the individual contributing factors to be assessed, controlling for other factors. Heretofore this has been challenging, absent a viable framework. Our intent is to further the development of in-depth study of disasters on pregnant women and infants by promoting additional perspectives regarding the composition of contributing risk factors. We are currently applying this model to address the effects of Hurricane Michael and associated exposures to HAB, CO, and health care services loss, on pregnant women.
The present coronavirus pandemic provides a unique opportunity for researchers to test our model utilizing international, national, and state level maternal and child health laboratories. Now is also the optimal time to develop data collection instruments that can capture the full breadth of data this conceptual model undergirds. The Gulf of Mexico Research Institute recently published a report outlining a potential system for monitoring human health in the Gulf region;133 such systems should incorporate the ability to examine effects on pregnancy. We welcome the input and feedback of colleagues who accept our challenge to take the study of disasters and their human health consequences to the next stage of refinement, and, more importantly, apply it to interventions that improve prevention, mitigation, and response.
Funding
This project was funded by NIEHS grant, R21ES031020.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Harville E, Xiong X, Buekens P. Disasters and perinatal health:a systematic review. Obstet Gynecol Surv. November 2010;65(11):713–28. doi: 10.1097/OGX.0b013e31820eddbe [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Humanitarian Health Action: Definition: emergencies. Accessed January 13, 2021.
- 3.Callaghan WM, Rasmussen SA, Jamieson DJ, et al. Health concerns of women and infants in times of natural disasters: Lessons learned from Hurricane Katrina. Matern Child Health J. 2007;11:307–311. [DOI] [PubMed] [Google Scholar]
- 4.Keren M, Tyano S. The impact of trauma on the fetus, the infant, and the child. In: Hoven CW, Amsel LV, Tyano S, eds. An international perspective on disasters and children’s mental health. Springer Nature Switzerland AG; 2019:3–20. Integrating psychiatry and primary care; ISSN: 2522–5693 (Print), 2522–5707 (Electronic). [Google Scholar]
- 5.Illness surveillance and rapid needs assessment among Hurricane Katrina evacuees--Colorado, September 1–23, 2005. MMWR Morb Mortal Wkly Rep. March 10 2006;55(9):244–7. [PubMed] [Google Scholar]
- 6.Division of Reproductive Health at National Center for Chronic Disease Prevention and Health Promotion. Safety messages for pregnant, postpartum, and breastfeeding women during natural disasters and severe weather. Centers for Disease Control and Prevention. Updated November 2, 2020. Accessed January 14, 2021. https://www.cdc.gov/reproductivehealth/emergency/safety-messages.htm [Google Scholar]
- 7.Cakmak B, Ribeiro AP, Inanir A. Postural balance and the risk of falling during pregnancy. J Matern Fetal Neonatal Med. 2016;29(10):1623–5. doi: 10.3109/14767058.2015.1057490 [DOI] [PubMed] [Google Scholar]
- 8.Ribeiro AP, João SM, Sacco IC. Static and dynamic biomechanical adaptations of the lower limbs and gait pattern changes during pregnancy. Women’s health (London, England). January 2013;9(1):99–108. doi: 10.2217/whe.12.59 [DOI] [PubMed] [Google Scholar]
- 9.Erickson TB, Brooks J, Nilles EJ, Pham PN, Vinck P. Environmental health effects attributed to toxic and infectious agents following hurricanes, cyclones, flash floods and major hydrometeorological events. J Toxicol Environ Health B Crit Rev. 2019;22(5–6):157–171. doi: 10.1080/10937404.2019.1654422 [DOI] [PubMed] [Google Scholar]
- 10.Baurick T, Mitchell D. Chemical fire in Lake Charles after Hurricane Laura’s landfall prompts shelter-in-place order. Times-Picayune/New Orleans Advocate. August 27, 2020. https://www.nola.com/news/hurricane/article_701d29c6-e87b-11ea-8de9-971e6dc5b55b.html [Google Scholar]
- 11.Public health response to Hurricanes Katrina and Rita--United States, 2005. MMWR Morb Mortal Wkly Rep. March 10 2006;55(9):229–31. [PubMed] [Google Scholar]
- 12.Barbeau DN, Grimsley LF, White LE, El-Dahr JM, Lichtveld M. Mold exposure and health effects following hurricanes Katrina and Rita. Annu Rev Public Health. 2010;31:165–78 1 p following 178. doi: 10.1146/annurev.publhealth.012809.103643 [DOI] [PubMed] [Google Scholar]
- 13.Nieuwenhuijsen MJ, Dadvand P, Grellier J, Martinez D, Vrijheid M. Environmental risk factors of pregnancy outcomes: a summary of recent meta-analyses of epidemiological studies. Environ Health. 2013;12:6. doi: 10.1186/1476-069x-12-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knap AH, Rusyn I. Environmental exposures due to natural disasters. Rev Environ Health. March 2016;31(1):89–92. doi: 10.1515/reveh-2016-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kihal-Talantikite W, Zmirou-Navier D, Padilla C, Deguen S. Systematic literature review of reproductive outcome associated with residential proximity to polluted sites. International journal of health geographics. May 30 2017;16(1):20. doi: 10.1186/s12942-017-0091-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harville EW, Rabito FA. Housing conditions and birth outcomes: The National Child Development Study. Environ Res. February 2018;161:153–157. doi: 10.1016/j.envres.2017.11.012 [DOI] [PubMed] [Google Scholar]
- 17.Wilson MJ, Aw TG, Sherchan S, Wickliffe J, Murphy SA. The Environmental Health and Emergency Preparedness Impacts of Hurricane Katrina. Am J Public Health. October 2020;110(10):1476–1477. doi: 10.2105/ajph.2020.305819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.NHC GIS Archive - Tropical Cyclone Best Track.
- 19.US Environmental Protection Agency. Geospatial Data Download Service. 2018. Accessed September 24, 2020. https://www.epa.gov/frs/geospatial-data-download-service
- 20.Florida Resources and Environmental Analysis Center. Data. Accessed September 24, 2020. https://freac.fsu.edu/data.html
- 21.Florida Fish and Wildlife Conservation Commission. Recent Harmful Algal Bloom (HAB) Events. Accessed September 24, 2020. https://geodata.myfwc.com/datasets/recent-harmful-algal-bloom-hab-events
- 22.Phlips EJ, Badylak S, Nelson NG, Havens KE. Hurricanes, El Niño and harmful algal blooms in two sub-tropical Florida estuaries: Direct and indirect impacts. Sci Rep. February 5 2020;10(1):1910. doi: 10.1038/s41598-020-58771-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman MA, Levin BE. Neurobehavioral effects of harmful algal bloom (HAB) toxins: a critical review. J Int Neuropsychol Soc. May 2005;11(3):331–8. doi: 10.1017/s1355617705050381 [DOI] [PubMed] [Google Scholar]
- 24.Levin ED, Pizarro K, Pang WG, Harrison J, Ramsdell JS. Persisting behavioral consequences of prenatal domoic acid exposure in rats. Neurotoxicol Teratol. Sep-Oct 2005;27(5):719–25. doi: 10.1016/j.ntt.2005.06.017 [DOI] [PubMed] [Google Scholar]
- 25.Maucher JM, Ramsdell JS. Maternal-fetal transfer of domoic acid in rats at two gestational time points. Environ Health Perspect. December 2007;115(12):1743–6. doi: 10.1289/ehp.10446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shiotani M, Cole TB, Hong S, et al. Neurobehavioral assessment of mice following repeated oral exposures to domoic acid during prenatal development. Neurotoxicol Teratol. November 2017;64:8–19. doi: 10.1016/j.ntt.2017.09.002 [DOI] [PubMed] [Google Scholar]
- 27.Grant KS, Burbacher TM, Faustman EM, Gratttan L. Domoic acid: neurobehavioral consequences of exposure to a prevalent marine biotoxin. Neurotoxicol Teratol. Mar-Apr 2010;32(2):132–41. doi: 10.1016/j.ntt.2009.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.He S, Kosatsky T, Smargiassi A, Bilodeau-Bertrand M, Auger N. Heat and pregnancy-related emergencies: Risk of placental abruption during hot weather. Environ Int. February 2018;111:295–300. doi: 10.1016/j.envint.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 29.Vicedo-Cabrera AM, Olsson D, Forsberg B. Exposure to seasonal temperatures during the last month of gestation and the risk of preterm birth in Stockholm. Int J Environ Res Public Health. April 10 2015;12(4):3962–78. doi: 10.3390/ijerph120403962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ward A, Clark J, McLeod J, Woodul R, Moser H, Konrad C. The impact of heat exposure on reduced gestational age in pregnant women in North Carolina, 2011–2015. Int J Biometeorol. December 2019;63(12):1611–1620. doi: 10.1007/s00484-019-01773-3 [DOI] [PubMed] [Google Scholar]
- 31.Zhang W, Spero TL, Nolte CG, et al. Projected Changes in Maternal Heat Exposure During Early Pregnancy and the Associated Congenital Heart Defect Burden in the United States. Journal of the American Heart Association. February 5 2019;8(3):e010995. doi: 10.1161/jaha.118.010995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soim A, Lin S, Sheridan SC, et al. Population-based case-control study of the association between weather-related extreme heat events and neural tube defects. Birth defects research. November 1 2017;109(18):1482–1493. doi: 10.1002/bdr2.1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bekkar B, Pacheco S, Basu R, DeNicola N. Association of Air Pollution and Heat Exposure With Preterm Birth, Low Birth Weight, and Stillbirth in the US: A Systematic Review. JAMA network open. June 1 2020;3(6):e208243. doi: 10.1001/jamanetworkopen.2020.8243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gronlund CJ, Berrocal VJ. Modeling and comparing central and room air conditioning ownership and cold-season in-home thermal comfort using the American Housing Survey. J Expo Sci Environ Epidemiol. September 2020;30(5):814–823. doi: 10.1038/s41370-020-0220-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hayden MH, Wilhelmi OV, Banerjee D, et al. Adaptive Capacity to Extreme Heat: Results from a Household Survey in Houston, Texas. Weather Climate and Society. October 2017;9(4):787–799. doi: 10.1175/wcas-d-16-0125.1 [DOI] [Google Scholar]
- 36.Call DA. A Survey of County Emergency Managers’ Response to Ice Storms. Journal of Homeland Security and Emergency Management. 2010;7(1)32. [Google Scholar]
- 37.Zhang Y, Yu C, Wang L. Temperature exposure during pregnancy and birth outcomes: An updated systematic review of epidemiological evidence. Environ Pollut. June 2017;225:700–712. doi: 10.1016/j.envpol.2017.02.066 [DOI] [PubMed] [Google Scholar]
- 38.Bruckner TA, Modin B, Vågerö D. Cold ambient temperature in utero and birth outcomes in Uppsala, Sweden, 1915–1929. Ann Epidemiol. February 2014;24(2):116–21. doi: 10.1016/j.annepidem.2013.11.005 [DOI] [PubMed] [Google Scholar]
- 39.Liang Z, Wang P, Zhao Q, et al. Effect of the 2008 cold spell on preterm births in two subtropical cities of Guangdong Province, Southern China. Sci Total Environ. November 15 2018;642:307–313. doi: 10.1016/j.scitotenv.2018.06.026 [DOI] [PubMed] [Google Scholar]
- 40.Van Zutphen AR, Hsu WH, Lin S. Extreme winter temperature and birth defects: a population-based case-control study. Environ Res. January 2014;128:1–8. doi: 10.1016/j.envres.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 41.Barrera R, Amador M, Acevedo V, Beltran M, Muñoz JL. A comparison of mosquito densities, weather and infection rates of Aedes aegypti during the first epidemics of Chikungunya (2014) and Zika (2016) in areas with and without vector control in Puerto Rico. Med Vet Entomol. March 2019;33(1):68–77. doi: 10.1111/mve.12338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boyce R, Reyes R, Matte M, et al. Severe Flooding and Malaria Transmission in the Western Ugandan Highlands: Implications for Disease Control in an Era of Global Climate Change. J Infect Dis. November 1 2016;214(9):1403–1410. doi: 10.1093/infdis/jiw363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ribeiro AC, Sarquis O, Lima MM, Abad-Franch F. Enduring extreme climate: Effects of severe drought on Triatoma brasiliensis populations in wild and man-made habitats of the Caatinga. PLoS Negl Trop Dis. October 2019;13(10):e0007766. doi: 10.1371/journal.pntd.0007766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chowell G, Mizumoto K, Banda JM, Poccia S, Perrings C. Assessing the potential impact of vector-borne disease transmission following heavy rainfall events: a mathematical framework. Philos Trans R Soc Lond B Biol Sci. June 24 2019;374(1775):20180272. doi: 10.1098/rstb.2018.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paixao ES, Barreto F, da Gloria Teixeira M, da Conceicao NCM, Rodrigues LC. History, Epidemiology, and Clinical Manifestations of Zika: A Systematic Review. Am J Public Health. April 2016;106(4):606–12. doi: 10.2105/ajph.2016.303112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pouliot SH, Xiong X, Harville E, et al. Maternal dengue and pregnancy outcomes: a systematic review. Obstet Gynecol Surv. February 2010;65(2):107–18. doi: 10.1097/OGX.0b013e3181cb8fbc [DOI] [PubMed] [Google Scholar]
- 47.Carlier Y, Sosa-Estani S, Luquetti AO, Buekens P. Congenital Chagas disease: an update. Mem Inst Oswaldo Cruz. May 2015;110(3):363–8. doi: 10.1590/0074-02760140405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chakalian PM, Kurtz LC, Hondula DM. After the Lights Go Out: Household Resilience to Electrical Grid Failure Following Hurricane Irma. Natural Hazards Review. November 2019;20(4)05019001. doi: 10.1061/(asce)nh.1527-6996.0000335 [DOI] [Google Scholar]
- 49.Iqbal S, Clower JH, Hernandez SA, Damon SA, Yip FY. A review of disaster-related carbon monoxide poisoning: surveillance, epidemiology, and opportunities for prevention. Am J Public Health. October 2012;102(10):1957–63. doi: 10.2105/ajph.2012.300674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Levy RJ. Carbon monoxide pollution and neurodevelopment: A public health concern. Neurotoxicol Teratol. May-Jun 2015;49:31–40. doi: 10.1016/j.ntt.2015.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bernard M, Mathews PR. Evacuation of a maternal-newborn area during Hurricane Katrina. MCN: The American Journal of Maternal Child Nursing. 2008;33(4):213–223. [DOI] [PubMed] [Google Scholar]
- 52.Hernandez-Diaz S, Boeke CE, Romans AT, et al. Triggers of spontaneous preterm delivery--why today? Paediatr Perinat Epidemiol. March 2014;28(2):79–87. doi: 10.1111/ppe.12105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Najarian LM, Goenjian AK, Pelcovitz D, Mandel F, Najarian B. The effect of relocation after a natural disaster. J Trauma Stress. July 2001;14(3):511–26. [DOI] [PubMed] [Google Scholar]
- 54.Hasegawa A, Ohira T, Maeda M, Yasumura S, Tanigawa K. Emergency Responses and Health Consequences after the Fukushima Accident; Evacuation and Relocation. Clin Oncol (R Coll Radiol). April 2016;28(4):237–44. doi: 10.1016/j.clon.2016.01.002 [DOI] [PubMed] [Google Scholar]
- 55.Haque MR, Parr N, Muhidin S. The effects of household’s climate-related displacement on delivery and postnatal care service utilization in rural Bangladesh. Soc Sci Med. January 28 2020;247:112819. doi: 10.1016/j.socscimed.2020.112819 [DOI] [PubMed] [Google Scholar]
- 56.Fellmeth G, Fazel M, Plugge E. Migration and perinatal mental health in women from low- and middle-income countries: a systematic review and meta-analysis. BJOG. April 2017;124(5):742–752. doi: 10.1111/1471-0528.14184 [DOI] [PubMed] [Google Scholar]
- 57.Heslehurst N, Brown H, Pemu A, Coleman H, Rankin J. Perinatal health outcomes and care among asylum seekers and refugees: a systematic review of systematic reviews. BMC Med. June 12 2018;16(1):89. doi: 10.1186/s12916-018-1064-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cohan CL, Cole SW. Life course transitions and natural disaster: marriage, birth, and divorce following Hurricane Hugo. J Fam Psychol. March 2002;16(1):14–25. [DOI] [PubMed] [Google Scholar]
- 59.Chen X, Dai K, Parnell A. Disaster tradition and change: Remarriage and family reconstruction in a post-earthquake community in the People’s Republic of China. Journal of Comparative Family Studies. Spr 1992 1992;23(1):115–132. [Google Scholar]
- 60.Luo ZC, Wilkins R, Kramer MS. Disparities in pregnancy outcomes according to marital and cohabitation status. Obstet Gynecol. June 2004;103(6):1300–7. doi: 10.1097/01.AOG.0000128070.44805.1f [DOI] [PubMed] [Google Scholar]
- 61.Boy A, Salihu HM. Intimate partner violence and birth outcomes: a systematic review. Int J Fertil Womens Med. Jul-Aug 2004;49(4):159–64. [PubMed] [Google Scholar]
- 62.Norbeck JS, Anderson NJ. Psychosocial predictors of pregnancy outcomes in low-income black, Hispanic, and white women. Nurs Res. Jul-Aug 1989;38(4):204–9. [PubMed] [Google Scholar]
- 63.Cerna-Turoff I, Fischer HT, Mayhew S, Devries K. Violence against children and natural disasters: A systematic review and meta-analysis of quantitative evidence. PLoS One. 2019;14(5):e0217719. doi: 10.1371/journal.pone.0217719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bell SA, Folkerth LA. Women’s Mental Health and Intimate Partner Violence Following Natural Disaster: A Scoping Review. Prehosp Disaster Med. December 2016;31(6):648–657. doi: 10.1017/s1049023x16000911 [DOI] [PubMed] [Google Scholar]
- 65.Sety M, James K, Breckenridge J. Understanding the risk of domestic violence during and post natural disasters: Literature review. In: Roeder LW Jr., ed. Issues of gender and sexual orientation in humanitarian emergencies: Risks and risk reduction. Springer International Publishing; 2014:99–111. Humanitarian solutions in the 21st century; ISSN: 2198–9958 (Print), 2198–9966 (Electronic). [Google Scholar]
- 66.Subedi S, Davison C, Bartels S. Analysis of the relationship between earthquake-related losses and the frequency of child-directed emotional, physical, and severe physical abuse in Haiti. Child Abuse Negl. August 2020;106:104509. doi: 10.1016/j.chiabu.2020.104509 [DOI] [PubMed] [Google Scholar]
- 67.Epstein A, Bendavid E, Nash D, Charlebois ED, Weiser SD. Drought and intimate partner violence towards women in 19 countries in sub-Saharan Africa during 2011–2018: A population-based study. PLoS Med. March 2020;17(3):e1003064. doi: 10.1371/journal.pmed.1003064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lahiri S, van Ommeren M, Roberts B. The influence of humanitarian crises on social functioning among civilians in low- and middle-income countries: A systematic review. Global public health. December 2017;12(12):1461–1478. doi: 10.1080/17441692.2016.1154585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Felix E, Afifi T, Kia-Keating M, Brown L, Afifi W, Reyes G. Family functioning and posttraumatic growth among parents and youth following wildfire disasters. Am J Orthopsychiatry. March 2015;85(2):191–200. doi: 10.1037/ort0000054 [DOI] [PubMed] [Google Scholar]
- 70.Chisholm CA, Bullock L, Ferguson JEJ 2nd. Intimate partner violence and pregnancy: epidemiology and impact. Am J Obstet Gynecol. August 2017;217(2):141–144. doi: 10.1016/j.ajog.2017.05.042 [DOI] [PubMed] [Google Scholar]
- 71.Kane JB, Harris KM, Siega-Riz AM. Intergenerational pathways linking maternal early life adversity to offspring birthweight. Soc Sci Med. June 2018;207:89–96. doi: 10.1016/j.socscimed.2018.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Margerison-Zilko CE, Strutz KL, Li Y, Holzman C. Stressors Across the Life-Course and Preterm Delivery: Evidence From a Pregnancy Cohort. Maternal and child health journal. March 2017;21(3):648–658. doi: 10.1007/s10995-016-2151-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Harville EW, Boynton-Jarrett R, Power C, Hypponen E. Childhood hardship, maternal smoking, and birth outcomes: a prospective cohort study. Arch Pediatr Adolesc Med. June 2010;164(6):533–9. doi:164/6/533 [pii] 10.1001/archpediatrics.2010.61 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Abell TD, Baker LC, Clover RD, Ramsey CN Jr. The effects of family functioning on infant birthweight. J Fam Pract. January 1991;32(1):37–44. [PubMed] [Google Scholar]
- 75.National Academies of Sciences E, and Medicine,. Introduction. Building and Measuring Community Resilience: Actions for Communities and the Gulf Research Program. National Academies Press; 2019. https://www.ncbi.nlm.nih.gov/books/NBK540795/ [PubMed] [Google Scholar]
- 76.Botzen WJW, Deschenes O, Sanders M. The Economic Impacts of Natural Disasters: A review of models and empirical studies. Review of Environmental Economics Policy. 2019;13(2):167–188. [Google Scholar]
- 77.Mitchell AM, Christian LM. Financial strain and birth weight: the mediating role of psychological distress. Archives of women’s mental health. February 2017;20(1):201–208. doi: 10.1007/s00737-016-0696-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Almeida J, Bécares L, Erbetta K, Bettegowda VR, Ahluwalia IB. Racial/Ethnic Inequities in Low Birth Weight and Preterm Birth: The Role of Multiple Forms of Stress. Matern Child Health J. August 2018;22(8):1154–1163. doi: 10.1007/s10995-018-2500-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Asgary R, Price JT. Socio-Cultural Challenges of Family Planning Initiatives for Displaced Populations in Conflict Situations and Humanitarian Settings. Disaster Med Public Health Prep. December 2018;12(6):670–674. doi: 10.1017/dmp.2017.146 [DOI] [PubMed] [Google Scholar]
- 80.Behrman JA, Weitzman A. Effects of the 2010 Haiti Earthquake on Women’s Reproductive Health. Stud Fam Plann. March 2016;47(1):3–17. doi: 10.1111/j.1728-4465.2016.00045.x [DOI] [PubMed] [Google Scholar]
- 81.Kissinger P, Schmidt N, Sanders C, Liddon N. The effect of the Hurricane Katrina disaster on sexual behavior and access to reproductive care for young women in New Orleans. Sex Transm Dis. 2007;34(11):883–886. [DOI] [PubMed] [Google Scholar]
- 82.Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32(1):152–74. doi: 10.1093/epirev/mxq012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Harville EW, Tran T, Xiong X, Buekens P. Population changes, racial/ethnic disparities, and birth outcomes in Louisiana after Hurricane Katrina. Disaster Med Public Health Prep. September 2010;4 Suppl 1:S39–45. doi: 10.1001/dmp.2010.15 [DOI] [PubMed] [Google Scholar]
- 84.Pan K, Beitsch L, Gonsoroski E, et al. Effects of Hurricane Michael on Access to Care for Pregnant Women and Associated Pregnancy Outcomes. Int J Environ Res Public Health. January 6 2021;18(2)doi: 10.3390/ijerph18020390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tong VT, Zotti ME, Hsia J. Impact of the Red River catastrophic flood on women giving birth in North Dakota, 1994–2000. Matern Child Health J. April 2011;15(3):281–8. doi: 10.1007/s10995-010-0576-9 [DOI] [PubMed] [Google Scholar]
- 86.Rosales-Rueda M The impact of early life shocks on human capital formation: evidence from El Nino floods in Ecuador. J Health Econ. November 2018;62:13–44. doi: 10.1016/j.jhealeco.2018.07.003 [DOI] [PubMed] [Google Scholar]
- 87.Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. The Cochrane database of systematic reviews. October 6 2010;(10):Cd000934. doi: 10.1002/14651858.CD000934.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fiscella K Does prenatal care improve birth outcomes? A critical review. Obstet Gynecol. March 1995;85(3):468–79. doi: 10.1016/0029-7844(94)00408-6 [DOI] [PubMed] [Google Scholar]
- 89.Kidd S, Bowen VB, Torrone EA, Bolan G. Use of National Syphilis Surveillance Data to Develop a Congenital Syphilis Prevention Cascade and Estimate the Number of Potential Congenital Syphilis Cases Averted. Sex Transm Dis. September 2018;45(9S Suppl 1):S23–s28. doi: 10.1097/olq.0000000000000838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schrag SJ, Arnold KE, Mohle-Boetani JC, et al. Prenatal screening for infectious diseases and opportunities for prevention. Obstet Gynecol. October 2003;102(4):753–60. doi: 10.1016/s0029-7844(03)00671-9 [DOI] [PubMed] [Google Scholar]
- 91.Medicaid and CHIP Learning Collaborative. Inventory of Medicaid and CHIP Flexibilities and Authorities in the Event of Disaster. 2018. https://www.medicaid.gov/state-resource-center/downloads/mac-learning-collaboratives/medicaid-chip-inventory.pdf
- 92.Lobel M, Dunkel Schetter C. Pregnancy and Prenatal Stress. In: Friedman HS, ed. Encyclopedia of Mental Health. Academic Press; 2016:318–329. [Google Scholar]
- 93.Hilmert CJ, Schetter CD, Dominguez TP, et al. Stress and blood pressure during pregnancy: racial differences and associations with birthweight. Psychosom Med. January 2008;70(1):57–64. doi: 10.1097/PSY.0b013e31815c6d96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Agrawal A, Wenger NK. Hypertension During Pregnancy. Curr Hypertens Rep. August 27 2020;22(9):64. doi: 10.1007/s11906-020-01070-0 [DOI] [PubMed] [Google Scholar]
- 95.Thomson M The physiological roles of placental corticotropin releasing hormone in pregnancy and childbirth. J Physiol Biochem. September 2013;69(3):559–73. doi: 10.1007/s13105-012-0227-2 [DOI] [PubMed] [Google Scholar]
- 96.Sandman CA. Prenatal CRH: An integrating signal of fetal distress. Dev Psychopathol. August 2018;30(3):941–952. doi: 10.1017/s0954579418000664 [DOI] [PubMed] [Google Scholar]
- 97.Bailey MT. Psychological Stress, Immunity, and the Effects on Indigenous Microflora. Adv Exp Med Biol. 2016;874:225–46. doi: 10.1007/978-3-319-20215-0_11 [DOI] [PubMed] [Google Scholar]
- 98.Jayaram PM, Mohan MK, Konje J. Bacterial vaginosis in pregnancy - a storm in the cup of tea. Eur J Obstet Gynecol Reprod Biol. October 2020;253:220–224. doi: 10.1016/j.ejogrb.2020.08.009 [DOI] [PubMed] [Google Scholar]
- 99.Steer PJ, Russell AB, Kochhar S, Cox P, Plumb J, Gopal Rao G. Group B streptococcal disease in the mother and newborn-A review. Eur J Obstet Gynecol Reprod Biol. September 2020;252:526–533. doi: 10.1016/j.ejogrb.2020.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lochner HJ 3rd, Maraqa NF. Sexually Transmitted Infections in Pregnant Women: Integrating Screening and Treatment into Prenatal Care. Paediatr Drugs. December 2018;20(6):501–509. doi: 10.1007/s40272-018-0310-4 [DOI] [PubMed] [Google Scholar]
- 101.Harville EW, Xiong X, Pridjian G, Elkind-Hirsch K, Buekens P. Postpartum mental health after Hurricane Katrina: A cohort study. BMC Pregnancy Childbirth. June 8 2009;9(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612 [DOI] [PubMed] [Google Scholar]
- 103.Osaki Y, Maesato H, Minobe R, et al. Changes in smoking behavior among victims after the great East Japan earthquake and tsunami. Environ Health Prev Med. June 11 2020;25(1):19. doi: 10.1186/s12199-020-00858-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vetter S, Rossegger A, Rossler W, Bisson JI, Endrass J. Exposure to the tsunami disaster, PTSD symptoms and increased substance use - an Internet based survey of male and female residents of Switzerland. BMC Public Health. 2008;8:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chemtob CM, Nomura Y, Josephson L, Adams RE, Sederer L. Substance use and functional impairment among adolescents directly exposed to the 2001 World Trade Center attacks. Disasters. July 2009;33(3):337–52. doi: 10.1111/j.1467-7717.2008.01077.x [DOI] [PubMed] [Google Scholar]
- 106.Duff EM, Cooper ES. Neural tube defects in Jamaica following Hurricane Gilbert. Am J Public Health. March 1994;84(3):473–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Clay LA, Papas MA, Gill KB, Abramson DM. Factors Associated with Continued Food Insecurity among Households Recovering from Hurricane Katrina. Int J Environ Res Public Health. August 3 2018;15(8)doi: 10.3390/ijerph15081647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ainehvand S, Raeissi P, Ravaghi H, Maleki M. The characteristic features of emergency food in national level natural disaster response programs: A qualitative study. Journal of education and health promotion. 2019;8:58. doi: 10.4103/jehp.jehp_266_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Aschbacher K, Kornfeld S, Picard M, et al. Chronic stress increases vulnerability to diet-related abdominal fat, oxidative stress, and metabolic risk. Psychoneuroendocrinology. August 2014;46:14–22. doi: 10.1016/j.psyneuen.2014.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Goldstein RF, Abell SK, Ranasinha S, et al. Gestational weight gain across continents and ethnicity: systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. August 31 2018;16(1):153. doi: 10.1186/s12916-018-1128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Doubleday A, Choe Y, Miles S, Errett NA. Daily Bicycle and Pedestrian Activity as an Indicator of Disaster Recovery: A Hurricane Harvey Case Study. Int J Environ Res Public Health. August 8 2019;16(16)doi: 10.3390/ijerph16162836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Davenport MH, Ruchat SM, Sobierajski F, et al. Impact of prenatal exercise on maternal harms, labour and delivery outcomes: a systematic review and meta-analysis. Br J Sports Med. January 2019;53(2):99–107. doi: 10.1136/bjsports-2018-099821 [DOI] [PubMed] [Google Scholar]
- 113.Louis-Jacques AF, Stuebe AM. Enabling Breastfeeding to Support Lifelong Health for Mother and Child. Obstet Gynecol Clin North Am. September 2020;47(3):363–381. doi: 10.1016/j.ogc.2020.04.001 [DOI] [PubMed] [Google Scholar]
- 114.Kyozuka H, Yasuda S, Kawamura M, et al. Impact of the Great East Japan Earthquake on feeding methods and newborn growth at 1 month postpartum: results from the Fukushima Health Management Survey. Radiat Environ Biophys. February 13 2016;doi: 10.1007/s00411-016-0636-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.DeYoung SE, Chase J, Branco MP, Park B. The Effect of Mass Evacuation on Infant Feeding: The Case of the 2016 Fort McMurray Wildfire. Matern Child Health J. December 2018;22(12):1826–1833. doi: 10.1007/s10995-018-2585-z [DOI] [PubMed] [Google Scholar]
- 116.Quinn D, Lavigne SV, Chambers C, et al. Addressing concerns of pregnant and lactating women after the 2005 hurricanes: the OTIS response. MCN Am J Matern Child Nurs. Jul-Aug 2008;33(4):235–41. [DOI] [PubMed] [Google Scholar]
- 117.Binns CW, Lee MK, Tang L, Yu C, Hokama T, Lee A. Ethical issues in infant feeding after disasters. Asia Pac J Public Health. July 2012;24(4):672–80. doi: 10.1177/1010539512453253 [DOI] [PubMed] [Google Scholar]
- 118.Zolala F Evaluation of the usefulness of maternal mortality ratio for monitoring long-term effects of a disaster: case study on the Bam earthquake. East Mediterr Health J. December 2011;17(12):976–80. doi: 10.26719/2011.17.12.976 [DOI] [PubMed] [Google Scholar]
- 119.Tennant E, Gilmore EA. Government effectiveness and institutions as determinants of tropical cyclone mortality. Proc Natl Acad Sci U S A. November 17 2020;117(46):28692–28699. doi: 10.1073/pnas.2006213117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.King S, Dancause K, Turcotte-Tremblay AM, Veru F, Laplante DP. Using natural disasters to study the effects of prenatal maternal stress on child health and development. Birth Defects Res C Embryo Today. December 2012;96(4):273–88. doi: 10.1002/bdrc.21026 [DOI] [PubMed] [Google Scholar]
- 121.Harville EW, Giarratano G, Savage J, Barcelona de Mendoza V, Zotkiewicz T. Birth Outcomes in a Disaster Recovery Environment: New Orleans Women After Katrina. Matern Child Health J. June 30 2015;doi: 10.1007/s10995-015-1772-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Simeonova E Out of Sight, Out of Mind? Natural Disasters and Pregnancy Outcomes in the USA. CESifo Economic Studies. 2011;57(3):403–431. [Google Scholar]
- 123.Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring Community Vulnerability to Natural and Anthropogenic Hazards: The Centers for Disease Control and Prevention’s Social Vulnerability Index. J Environ Health. June 2018;80(10):34–36. [PMC free article] [PubMed] [Google Scholar]
- 124.Olson DM, Bremault-Phillips S, King S, et al. Recent Canadian efforts to develop population-level pregnancy intervention studies to mitigate effects of natural disasters and other tragedies. J Dev Orig Health Dis. January 10 2019:1–7. doi: 10.1017/s2040174418001113 [DOI] [PubMed] [Google Scholar]
- 125.Paquin V, Bick J, Lipschutz R, et al. Unexpected effects of expressive writing on post-disaster distress in the Hurricane Harvey Study: a randomized controlled trial in perinatal women. Psychol Med. March 12 2021:1–9. doi: 10.1017/s003329172100074x [DOI] [PubMed] [Google Scholar]
- 126.Steinmetz SE, Benight CC, Bishop SL, James LE. My Disaster Recovery: a pilot randomized controlled trial of an Internet intervention. Anxiety, stress, and coping. 2012;25(5):593–600. doi: 10.1080/10615806.2011.604869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ruggiero KJ, Davidson TM, McCauley J, et al. Bounce Back Now! Protocol of a population-based randomized controlled trial to examine the efficacy of a Web-based intervention with disaster-affected families. Contemp Clin Trials. January 2015;40:138–49. doi: 10.1016/j.cct.2014.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Stasiak K, Merry SN, Frampton C, Moor S. Delivering solid treatments on shaky ground: Feasibility study of an online therapy for child anxiety in the aftermath of a natural disaster. Psychotherapy research : journal of the Society for Psychotherapy Research. July 2018;28(4):643–653. doi: 10.1080/10503307.2016.1244617 [DOI] [PubMed] [Google Scholar]
- 129.Abramson D Kids First: Children as bellwethers of recovery. Natural Hazards Center. Accessed July 24, 2020. https://hazards.colorado.edu/news/research-counts/kids-first-children-as-bellwethers-of-recovery [Google Scholar]
- 130.Nygaard E, Hussain A, Siqveland J, Heir T. General self-efficacy and posttraumatic stress after a natural disaster: a longitudinal study. BMC Psychol. April 06 2016;4:15. doi: 10.1186/s40359-016-0119-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Stanley E, Muntner P, Re RN, Frohlich ED, Holt E, Krousel-Wood MA. Quality of life in hypertensive clinic patients following hurricane katrina. The Ochsner journal. Fall 2011;11(3):226–31. [PMC free article] [PubMed] [Google Scholar]
- 132.Wheeler S, Maxson P, Truong T, Swamy G. Psychosocial Stress and Preterm Birth: The Impact of Parity and Race. Maternal and child health journal. October 2018;22(10):1430–1435. doi: 10.1007/s10995-018-2523-0 [DOI] [PubMed] [Google Scholar]
- 133.Sandifer PA, Knapp LC, Lichtveld MY, et al. Framework for a Community Health Observing System for the Gulf of Mexico Region: Preparing for Future Disasters Frontiers in Public Health. accepted;doi:doi: 10.3389/fpubh.2020.578463 [DOI] [PMC free article] [PubMed] [Google Scholar]


