Abstract
Aims
Heart failure (HF) is the most common primary inpatient diagnosis in Germany. We examined temporal trends of HF hospitalization within Germany focusing on regional differences.
Methods and results
We analysed aggregated data of more than 320 million hospitalizations in Germany from 2000 to 2017. Temporal trends of HF‐related parameters were analysed, focusing on regional differences between the federal states. The absolute number of HF‐related hospitalizations throughout Germany increased continuously and almost doubled (from 239 694 to 464 724 cases, +94%) with the relative increase being higher in East Germany compared with West Germany (119% vs. 88%). These regional differences persisted after age standardization with 609 and 490 cases per 100 000 population, respectively. The length of stay decreased continuously across Germany (from 14.3 to 10.2 days; −29%), while the total number of HF‐related hospital days increased by 51% in East Germany and 35% in West Germany. In 2017, HF remained the leading cause of in‐hospital death (8.9% of all cases), with a markedly higher rate in East vs. West Germany (65 vs. 43 deaths per 100 000 population).
Conclusions
Heart failure remains the most common cause of hospitalization and in‐hospital death throughout Germany. The increase in HF‐related morbidity and mortality was much higher in East Germany compared with West Germany during the observation period. A more detailed understanding of these striking disparities 30 years after the German reunification requires further investigations. There is an urgent need for action with regard to stronger control of risk factors and improvement of both chronic HF management and healthcare structures.
Keywords: Heart failure, Germany, Epidemiology, Regional disparities, Hospitalization, In‐hospital mortality
Introduction
Between the end of World War II and 1990, Germany was separated into two parts with different social, economic, and healthcare systems: the former German Democratic Republic (GDR) in the Eastern part of Germany and the Federal Republic of Germany (FRG) in the Western part. Since 1990, Germany is reunited, but there are still substantial differences between the former parts: the gross domestic product in the Eastern part (including Berlin) is actually 82% of that in the Western part but was 45% in the 1990s. The unemployment rate was 8.4% in the Eastern part and 5.8% in the Western part in 1997 and was 6.4% in the Eastern part and 4.7% in the Western part in 2019. 1
Until 1990, healthcare systems in former Eastern (East Germany) and Western (West Germany) regions of Germany differed markedly. The German Democratic Republic had a health system totally run by the state with no private insurance. Primary care was not provided by individual doctors but by 1650 ‘policlinics’, which were medical centres providing medical care in different specialties. Patients were treated there by the employed doctor on duty; a personal connection to one primary care physician was not foreseen. Medical doctors were paid the same amount of money, irrespective of how many patients they treated or how long they worked. The FRG had a system with physicians mostly working in their own practice and payment was a result of the number of patients and quantity of service provided. Most patients had a personal general practitioner. There was substantial shortage in technical equipment (e.g. one computer tomography per 600 000 inhabitants in East Germany compared with one per 100 000 in West Germany; one ultrasound device per 32 000 population in East Germany and one per 2500 in West Germany). 2 Since 1990, both parts have the same federal healthcare system with more physicians in private practice and an approximation in clinical care pathways. Differences between West and East Germany diminished partially but are still present. For instance, the mortality for acute myocardial infarction in East Germany is substantially higher than in West Germany. 3
Heart failure (HF) is the most common reason for hospitalization throughout the Western world. Between 2000 and 2013, the absolute number of HF‐related hospitalizations increased by 65% in Germany. 4 We aimed to analyse the impact of the change from two different social systems to a common social system from 1990 to 2017 on HF hospitalization in West and East Germany. We hypothesized that, in parallel to economic assimilation, HF hospitalization rates aligned from 2000 onwards with only small differences still present in 2017.
Methods
Data provenance and patient population
We retrospectively analysed aggregated administrative data obtained from the German Federal Health Monitoring (FHM), an annual complete census of inpatient routine data. 5 Contribution of standardized anonymized data to this database is obligatory for all German hospitals. Data are provided by the Federal Statistical Office and the Robert Koch Institute in an unchanged format since 2000 and have previously been used for research in cardiovascular epidemiology. 4 , 6 , 7 , 8 , 9
We used the most recent data available, covering the 18 year period from 2000 to 2017, in total including information on more than 320 million hospital admissions (see the Supporting Information for further details).
In the context of our research, data based on the primary diagnosis code I50 are referred to as ‘HF‐related’. Because all patient data in FHM database are anonymized routine clinical data, patient consent and approval by an independent local ethics committee was not required.
Study objectives, data analyses, and statistics
The TRENDS‐HF project aims to report on temporal trends in the epidemiology of HF in Germany to inform both the medical community and health policymakers. One principal objective is to analyse regional trends across Germany considering the individual federal states (n = 16). A specific focus is the comparison of former Eastern and Western regions in Germany, which are termed ‘old federal states’ and ‘new federal states’, respectively, within the FHM. For easier reading, we refer in this manuscript to ‘East Germany’ (Brandenburg, Mecklenburg‐Western Pomerania, Saxony, Saxony‐Anhalt, and Thuringia; Supporting Information, Figure S1 , green) and to ‘West Germany’ (remaining states, including Berlin; Supporting Information, Figure S1 , blue). With regard to the overall situation in Germany, we analysed the development of in‐hospital key metrics in HF patients as compared to the totality of the remaining patients. Data are presented as absolute numbers indexed to the year 2000 (value in 2000 is set to 100) for the respective event types: (i) hospitalizations, (ii) hospital days, and (iii) in‐hospital deaths. These analyses are paralleled by a respective comparison of long‐term temporal trends in East Germany compared with West Germany. On the level of the individual federal states, heat maps (created with EasyMap 11.2 SP1, Lutum+Tappert DV‐Beratung GmbH, Bonn, Germany) are provided as a colour‐coded graphical representation of data regarding hospitalizations and in‐hospital deaths per 100 000 population. In order to reflect increases in the burden of disease on the one hand and to control for changes in population composition on the other, HF hospitalizations per 100 000 population will be displayed as crude data as well as age standardized to the most recent standard population (‘Germany 2011’) that is provided by FHM. Because FHM does not offer respective age‐standardization, in‐hospital deaths per 100 000 population are presented as crude data only.
Temporal changes in the age composition of the German population and regional disparities were analysed based on data from the Federal Statistical Office, and the share of differing age groups as well as the median age by year‐end 2000 and 2017 are presented for East Germany as compared with West Germany.
Because the FHM database represents a complete census of all in‐hospital patients in Germany (and not a sample or a subgroup), data are presented as frequencies, and no formal statistical testing was deemed instrumental. Approximately 0.1–0.3% of the FMH I50 cases were attributable to patients with unknown or non‐German residence, resulting in a slight difference between the total number of cases captured in Germany (100%) and the number of cases in German residents (99.7–99.9%).
Results
Trend in hospitalizations for heart failure and other reasons
The absolute number of HF‐related hospitalizations throughout Germany increased continuously, from 239 694 in 2000 to 464 724 in 2017 (+93.9%). This temporal trend was much stronger in East vs. West Germany (+118.5% vs. +88.3%; Figure 1 ). During the same period, there was only a slight increase in the number of hospitalizations for other diagnoses all over Germany [from 16 947 833 in 2000 to 19 488 011 cases in 2017 (+15.0%); Supporting Information, Figure S2 ], with a higher increase in West Germany compared with East Germany (+15.9% vs. +10.1%). Accordingly, the proportion of HF‐related hospitalizations in relation to the total number of hospitalizations throughout Germany rose substantially from 1.4% to 2.3% (+67.0%). Thus, HF was the leading cause of disease‐related hospitalization in Germany in 2017. Again, HF hospitalization as a proportion of total hospitalization is higher in East Germany compared with West Germany [from 1.5% to 2.9% (+95.6%) vs. 1.4% to 2.2% (+61.0%)].
Figure 1.
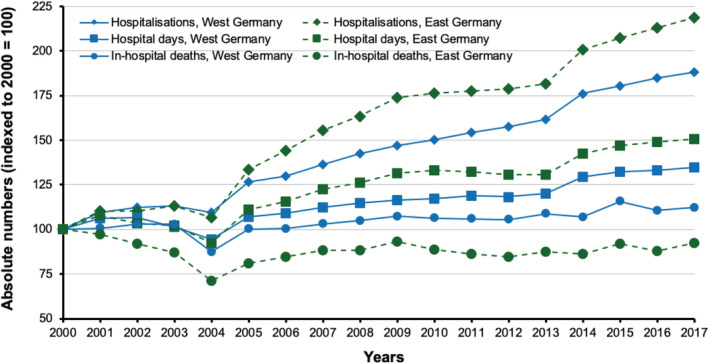
Heart failure‐related trends in hospital admissions, hospital days, and in‐hospital deaths in East and West Germany from 2000 to 2017. Graph shows absolute numbers indexed to the year 2000 (= 100) per respective event type.
In relation to the respective number of inhabitants, HF‐related hospitalizations increased from 321 to 776 per 100 000 population in East Germany and from 285 to 523 cases per 100 000 population in West Germany (+141.7% vs. +83.5%; Figure 2 A and Supporting Information, Figure S3 ). The relative and absolute increases were higher in each of the Eastern federal states than in every single state in West Germany, ranging from 134% in Brandenburg to 160% in Mecklenburg‐Western Pomerania, while the increase in West Germany ranged from 26% in Bremen to 112% in Baden‐Württemberg (Figure 2 A ).
Figure 2.
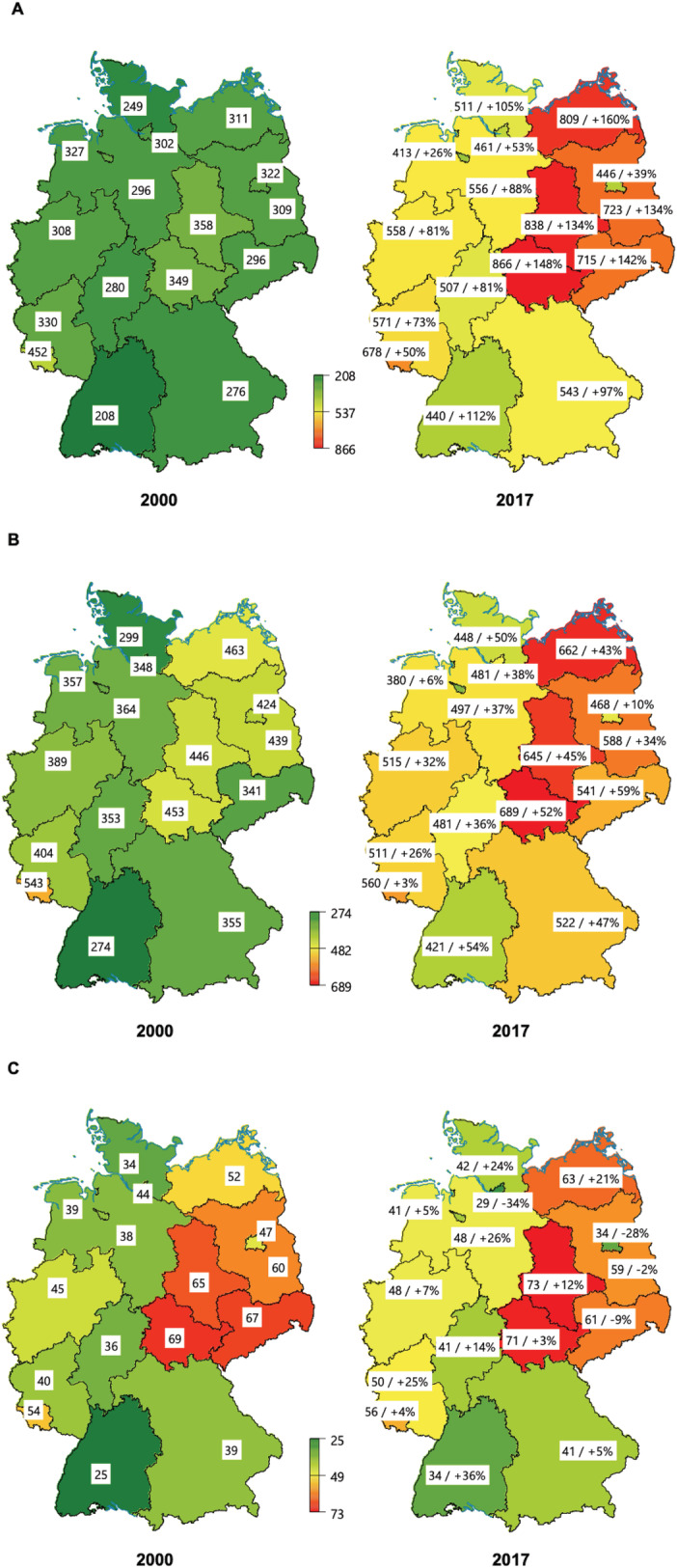
Numbers and changes of heart failure (HF)‐related key parameters for the German federal states in the years 2000 and 2017. (A) Crude numbers of and relative changes in HF‐related hospital admissions per 100 000 population; (B) age‐standardized numbers and relative changes of HF‐related hospitalizations per 100 000 population; and (C) crude numbers and relative changes of HF‐related in‐hospital deaths per 100 000 population.
Similar differences between East and West Germany were observed for age‐standardized hospitalization rates. In 2017, the rates of HF‐related hospitalizations were 609 per 100 000 population in East Germany and 490 per 100 000 population in West Germany. The relative increase was 48.5% and 36.1% compared with the numbers in 2000 (410 and 360 cases per 100 000 population). The relative and absolute increases were higher in most federal states in East Germany compared with West Germany (Figure 2 B ). Specifically, in East Germany, the age‐standardized increase of HF hospitalizations ranged from 34% in Brandenburg to 59% in Saxony. In West Germany, the lowest age‐standardized increase was seen in Saarland with 3%. Among the remaining 10 federal states in West Germany, five had relative increases that were higher than the lowest values observed in East Germany with the highest values seen in Schleswig‐Holstein with 50% and in Baden‐Württemberg with 54% (Figure 2 B ).
For all reported trends, we did not find any relevant differences between men and women for both the crude and age‐standardized number of cases per 100 000 population (Supporting Information, Figures S3 and S4 ). Likewise, there was a consistent and substantial increase in the population‐based number of HF‐related hospitalizations in East as well as West Germany across all age groups. Again, the absolute and relative changes were stronger in East Germany than in West Germany in each age group (Figure 3 ).
Figure 3.
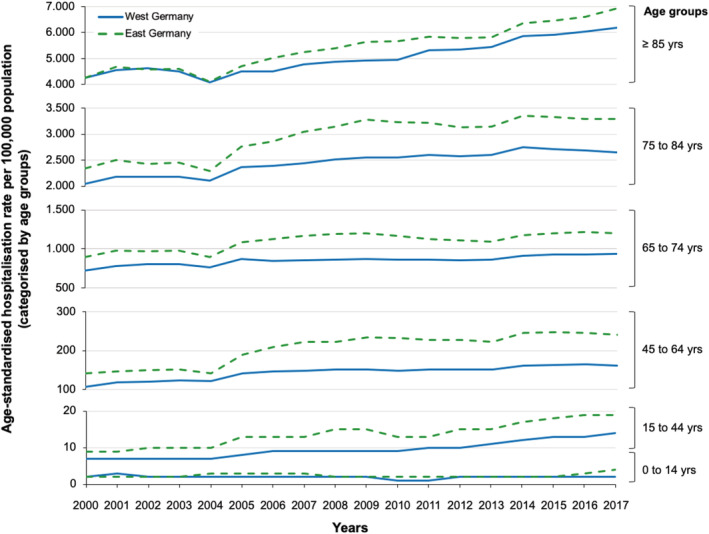
Heart failure‐related hospitalizations from 2000 to 2017 by age groups. Displayed is the age‐standardized rate of hospitalizations due to heart failure per 100 000 population in West and East Germany stratified by age groups. Solid lines denote values for West Germany and dotted lines for East Germany. Please note different scaling on the ordinates.
Changes in the age and gender distribution of the German population and of hospitalized heart failure patients
From 2000 to 2017, the number of inhabitants changed substantially within Germany comprising an increase of 1.8 million (+2.6%) in West Germany vs. a decrease of 1.3 million (−9.2%) in East Germany. Also, age distribution changed significantly: the number of inhabitants above 65 years increased by 29.3% throughout Germany, resulting in an increase in the proportion of this age group from 16.6% to 21.4% (East Germany from 17.1% to 25.2%; West Germany from 16.6% to 20.7%; Supporting Information, Figure S5 ). These demographic changes differed substantially between the two German regions and were seen in particular for the oldest age groups: in East Germany, people aged 75–84 doubled from 5.1% to 10.5% of inhabitants (+107.1%), while in West Germany, it increased from 5.3% to 8.3% (+56.1%). Likewise, the proportion of inhabitants aged ≥85 increased significantly (East Germany: from 1.8% to 3.1%, relative change +71.8%; West Germany: from 2.0% to 2.7%, relative change +34.1%). In 2017, the median age of the population was 45 years in West Germany and 49 years in East Germany (Supporting Information, Figure S5 ).
The age distribution of patients hospitalized for HF also underwent significant changes: throughout Germany, nearly three quarters of the affected patients were 75 years or older in 2017. HF‐related hospitalizations significantly increased across all age groups, most prominently among patients aged 75–84 years (+128.4%) and ≥85 years (+107.9%) (Supporting Information, Figure S6A ). These changes were more pronounced in East Germany than in West Germany with stronger increases in all age groups except for the lowest one. Thus, the number of HF‐related hospitalizations increased by 176.6% and 150.2% in those aged 75–84 and ≥85 years in East Germany compared with 117.9% and 100.2% in West Germany (Supporting Information, Figure S6B and S6C ). The average share of women among all HF hospitalizations decreased, whereas this trend could be observed in both regions. (Supporting Information, Table S1 ).
Heart failure‐related hospital days and in‐hospital death
From 2000 to 2017, the mean length of HF‐related hospitalizations decreased continuously throughout Germany (from 14.3 to 10.2 days; −29.1%), even exceeding the overall lowering of the mean length of hospitalizations for all diagnoses (from 9.7 to 7.3 days; −24.8%). These trends were comparable in East and West Germany (Supporting Information, Figure S7 ).
Despite the above‐average decrease in mean length of hospital stays and in contrast to a 12.8% decrease in hospital days related to all other diagnoses, the total number of HF‐related hospital days increased by 37.5% (2000: 3.44 million; 2017: 4.72 million hospital days) throughout Germany (Supporting Information, Figure S2 ), with an increase by 50.6% in East Germany (2000: 631 452; 2017: 951 145 hospital days) and by 34.6% in West Germany (2000: 2.78 million; 2017: 3.77 million hospital days) (Figure 1 ).
The absolute number of in‐hospital deaths in HF patients in whole Germany increased slightly (35 536 deaths in 2000 vs. 38 088 deaths in 2017; +7.2%) but less markedly compared with the overall number of HF cases (Supporting Information, Figure S2 ). In‐hospital deaths due to HF slightly rose in West Germany (26 608 deaths in 2000 vs. 29 870 deaths in 2017; +12.3%) compared with a slight decrease in East Germany (8850 deaths in 2000 vs. 8184 deaths in 2017; −7.5%) (Figure 1 ). These relative changes were due to an increase in the number of deaths in patients aged 75 years or older, while the numbers consistently decreased among younger patients (Supporting Information, Table S2 ).
In 2017, HF was by far the leading cause of in‐hospital death with a proportion of 8.9% among all cases. In East and West Germany, 10.8% and 8.5% of all in‐hospital deaths were due to HF, with substantially higher rates for East Germany (64 and 65 deaths per 100 000 population in 2000 and 2017, respectively; +1.6%) as compared with West Germany (39 and 43 deaths per 100 000 population in 2000 and 2017, respectively; +10.3%). Particularly high numbers of HF‐related in‐hospital deaths per 100 000 population were observed in Saxony‐Anhalt and Thuringia (Figure 2 C ).
Discussion
The comparison of HF hospitalization rates between West and East Germany revealed the following main results:
HF admissions throughout Germany almost doubled within 17 years, but the relative increase was higher in East Germany than in West Germany, even after age standardization.
The mean length of hospital stays decreased by 29%, similarly in West and East Germany, but the total number of HF‐related hospital days increased by 51% in East Germany and 35% in West Germany
The rate of HF‐related deaths in hospital was higher in East Germany than in West Germany.
Temporal trends in heart failure hospitalization
The previously reported increase in HF hospitalization rate of 4% per year from 2000 to 2013 continued uninterrupted throughout Germany until 2017 despite advances in HF treatment. 4 , 10 , 11 , 12
This temporal trend represents an enormous economic, social, and ethical challenge and deserves comprehensive consideration, especially as it is expected to increase further. The underlying causes are probably multifactorial. Because our findings were unchanged by age standardization, ageing of the population explains only a small part of the increase. Other reasons to be discussed are increasing prevalence rates of HF with preserved ejection fraction (an HF type for which still no evidence‐based treatment is available), improved survival of diseases that predispose towards HF (e.g. myocardial infarction), an increase in the prevalence of risk factors for HF (e.g. hypertension, diabetes, and obesity), and an enhanced awareness for HF among patients and physicians, which could potentially contribute to increased HF‐related hospital admissions. 3 , 13 , 14 , 15 , 16
Finally, the continuous increase in HF hospitalizations despite substantial advances in HF treatment and initiatives to implement interdisciplinary HF networks may represent a detrimental ‘latency effect’. 10 , 11 , 12 , 17 This refers to the phenomenon of delayed implementation of evidence‐based HF treatments into clinical practice, 18 , 19 which has also been linked to deficient improvement in HF survival in the community. 20 Thus, in line with current guidelines, we strongly advocate to undertake any effort to enhance chronic HF management in order to improve HF outcomes and hospitalization rate. 12
Differences in heart failure hospitalizations between East and West Germany
As East and West Germany came from different healthcare systems, we hypothesized that HF hospitalization patterns would align after German reunification. In contrary, we noticed a significant increase in hospital admissions in both East and West Germany. The relative (and absolute) increase in HF hospitalization rates was higher in all five federal states in East Germany (between 134% and 160%) than in any of the 11 Western German federal states (between 26% and 112%).
The reasons for these striking differences are poorly understood. The population in East Germany is on average 4 years older than its Western counterpart, but the results were consistent after age standardization and within age groups. We thus exclude differences in age distribution as a relevant explanation for the observed disparities.
One reason that may partly explain the observed disparities are regional differences in frequencies of cardiovascular risk factors contributing to HF, especially diabetes and obesity. 21 According to population‐based data, both prevalence and incidence of diabetes are substantially higher in East vs. West Germany. 14 , 15 Likewise, obesity is more prevalent with highest average values in Saxony‐Anhalt. 21 Finally, hypertension is still more prevalent in East Germany than in West Germany, despite improvements of treatment control in recent years. 13 Furthermore, it can be assumed that socio‐economic deprivation, a known strong predictor of HF development and poor outcomes, is another reason for this observation. In fact, relevant regional differences of income structure in Germany can be demonstrated. 22
Another putative explanation for the regional differences could be the ‘legacy effect’, which means that the risk factor burden in earlier years substantially impacts on the development of diseases later on, even if this burden has been reduced in the meantime. In line, a recent study in more than 30 000 participants from seven US cohort studies nicely demonstrated that higher baseline cardiovascular health at all ages in adulthood is associated with substantially lower lifetime risk for cardiovascular disease compared with moderate and low cardiovascular health. 23 Evidence for the ‘legacy hypothesis’ in HF is available from pooled analysis of data from four US cohort studies showing that prevention of hypertension, obesity, and diabetes in middle age may substantially prolong HF‐free survival and reduce HF‐related morbidity. 24 At the time of reunification, inhabitants of the former GDR (East Germany) displayed a clear disadvantage regarding health status and life expectancy compared with the inhabitants of the FRG (West Germany). For example, life expectancy was ~2.8 years shorter for women and 3.5 years shorter for men in the GDR than in the former FRG. 25
Furthermore, regional differences in the implementation of guideline‐directed HF therapy could also play a role, but recent data suggest higher guideline adherence in primary care in East Germany that is attenuated in patients also treated by a cardiologist. 26
Finally, persisting structural differences in healthcare supply may impact the disparities observed between East and West Germany. 27 In fact, there are significantly less cardiologists in private practice per inhabitants in the East than in the West German federal states. 3 Another example are the German Heart Failure Networks, an initiative that has been launched in 2016 by the German Cardiac Society aiming to improve the quality of care of HF patients in order to increase HF prognosis and reduce HF‐related hospitalizations. 17 Since the beginning of the initiative, three supraregional centres have been certified in East Germany (one per 4.2 million inhabitants), whereas in West Germany, already 27 centres have been established (one per 2.6 million inhabitants). 28
Mean duration of hospital stays and in‐hospital heart failure death
The German reimbursement system has been changed on 1 January 2004 from a rather fixed daily rate per occupied hospital bed to a disease‐related group system. This may have driven hospitals to optimize diagnostic and therapeutic intra‐hospital logistics and may be the main explanation for the reduced duration of the hospital stay that we observed across Germany.
The higher in‐hospital mortality of HF patients in East Germany compared with West Germany may be explained by either a higher burden of co‐morbidities or more advanced HF stages of hospitalized patients. A recent analysis identified older age, female sex, concomitant cancer, and adverse in‐hospital events as factors that were associated with in‐hospital death across Germany. 8 Unfortunately, available data are limited and do not allow us more detailed analyses regarding this topic.
Limitations
Some limitations merit discussion. First, the data are limited to inpatients. Therefore, we cannot provide information on the prevalence of HF for the overall community. Second, we cannot provide specific information on first vs. recurrent hospitalization, treatment patterns, left ventricular ejection fraction, type of HF (i.e. HF with preserved vs. reduced ejection fraction), and socio‐economic variables and therefore could not perform respective analyses. As the data set only comprises aggregated data, we were not able to adjust for risk factor control, which may be different between East and West Germany. Nevertheless, our analysis provides a large patient cohort over a long period of observation subsequently allowing valuable insights to be gathered. Third, we provide aggregated data on a federal state level that prevent accounting for differing settlement and infrastructure (e.g. possible association of rurality, shortage of physicians and more liberal referral of HF patients to hospitals, differences in first‐aid system, and primary care physician availability). Fourth, we are not able to control for relocations within Germany and immigration. Finally, data are derived from diagnostic codes that are routinely submitted by the hospitals and also are the basis for remunerations. Reimbursement for HF may have incentivized coding of ‘ICD 50’ cases, but payers are watchful, and the regulatory framework remains unchanged. Moreover, we cannot exclude that regional differences in coding may have affected our findings.
However, we are convinced that the previously mentioned limitations will hardly evoke the observed temporal trends and regional disparities and should be viewed in light of the strengths of the large and representative contemporary dataset.
Potential strategies for reducing heart failure hospitalizations in the future
In light of the increasing incidence of HF, we propose the following measurements: (i) better coordination between practices and medium‐level and high‐level care HF clinics as recently initiated by the German Cardiac Society 17 ; (ii) implementation of telemedicine for rural areas, which recently showed reduction in HF hospitalizations and improved survival in a large randomized trial 29 ; and (iii) better risk factor control, especially for hypertension and to prevent the development of HF.
Conclusions
Heart failure hospitalization rates are continuously rising throughout Germany. Moreover, detrimental initial measures and higher relative and absolute increases in East Germany than in West Germany demand specific attention and an improved understanding. Potential explanations for this disparity are the higher burden of cardiovascular risk factors, especially diabetes and obesity, as well as poorer healthcare structures. To fight the HF epidemic strategies for better risk factor control and HF prevention is just as urgently needed as further improvement of both chronic HF management and healthcare structures.
Conflict of interest
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.C., U.L., M.S., A.N., and S.S. report no conflicts of interest. M.D. reports honoraria for lectures and/or consulting from Bayer, Daiichi Sankyo, Hexal, and Novartis. U.R. is an employee of Novartis Germany. J.B. reports honoraria for lectures and/or consulting from Novartis, BMS, Pfizer, Vifor, Bayer, Servier, Daichii Sankyo, CVRx, MSD, Boehringer Ingelheim, AstraZeneca, Abiomed, Abbott, and Medtronic and research support from Zoll, CVRx, Vifor, and Abiomed. R.B. reports honoraria for lectures and/or consulting from Novartis, BMS, Pfizer, Bayer, Biotronik, and Medtronic and research support from BMS, Pfizer, Biotronik, and Abbott. U.L. has received honoraria for lectures and/or consulting from Novartis, Bayer, Servier, Daichii Sankyo, Boehringer Ingelheim, and Amgen. R.W. has been a consultant for or received speaker's bureau honoraria from Bayer, Berlin Chemie, Boehringer Ingelheim, Bristol Myers Squibb, CVRx, Daiichi, Johnson & Johnson, Medtronic, Novartis, Pfizer, Sanofi, and Servier.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Supporting information
Table S1. Distribution of HF hospitalisation cases. Displayed are distributions of HF‐related hospital admissions by 3‐year time periods and the whole study period according to age groups and gender. Colours of the lines have the following meaning: grey = whole Germany, blue = West Germany, green = East Germany.
Table S2. Relative changes in HF‐related hospital deaths from. Shown are relative changes of in‐hospital in HF patients in 2017 compared to 2000 for whole Germany, West Germany and East Germany by age groups.
Figure S1. Map of the German federal states. Federal states located in East Germany are shown in green (i.e. Brandenburg, Mecklenburg‐Western Pomerania, Saxony, Saxony‐Anhalt, and Thuringia), federal states in West Germany are shown in blue (i.e., remaining states, including Berlin).
Figure S2. Hospital admissions. Hospital days. and in‐hospital deaths for heart failure and all other diagnoses in whole Germany 2000 to 2017. Graph shows absolute numbers indexed to the year 2000 (=100) per respective event type due to heart failure and all other diagnoses.
Figure S3. Crude numbers of heart failure (HF)‐related hospitalisations in East and West Germany 2000 to 2017. Graph shows crude numbers of HF‐related hospital cases for both sexes, women and men.
Figure S4. Age‐standardised numbers of heart failure related hospitalisations per 100.000 population in East and West Germany 2000 to 2017. Graph shows crude numbers of hospitalisations due to heart failure for both sexes, women and men.
Figure S5. Age distribution of the population in East and West Germany in 2000 and 2017 by age groups. The graphs illustrate the percentages of different age groups in the total population in East Germany and West Germany. Of note, between 2000 and 2017, the median age increased from 39 to 45 years in West Germany and from 41 to 49 years in East Germany.
Figure S6. Heart failure‐related hospitalisations from 2000 to 2017 according to age groups. Displayed are HF‐related hospital admissions in predefined age groups for (A) whole Germany, (B) West Germany and (C) East Germany. Percentages on the right denominate increase from 2000 to 2017. Please note different scaling on the ordinates.
Figure S7. Temporal trends of mean length of in‐hospital stay due to heart failure and all diagnoses in East and West Germany 2000 to 2017. Graph shows mean values of hospital days related to heart failure and all diagnoses.
Acknowledgement
We thank Harald Brey (Novartis Pharma GmbH, Nuremberg, Germany) for the creation of heat maps.
Open Access funding enabled and organized by Projekt DEAL.
Dörr, M. , Riemer, U. , Christ, M. , Bauersachs, J. , Bosch, R. , Laufs, U. , Neumann, A. , Scherer, M. , Störk, S. , and Wachter, R. (2021) Hospitalizations for heart failure: still major differences between East and West Germany 30 years after reunification. ESC Heart Failure, 8: 2546–2555. 10.1002/ehf2.13407.
References
- 1. Statistisches Bundesamt . Registered unemployed, unemployment rate by territorial status 1997 [Registrierte Arbeitslose, Arbeitslosenquote nach Gebietsstatus 1997]. (Accessed July 30th 2020, at https://statistik.arbeitsagentur.de; access date: July 15th 2020.)
- 2. Deutz‐Schroeder M, Schroeder K. Soziales Paradies oder Stasi‐Staat? Das DDR‐Bild von Schülern—ein Ost‐West‐Vergleich. Stamsried: Druck & Verlag Ernst Vögel; 2008. [Google Scholar]
- 3. Zapf A, Bestehorn K. Mortalität und Morbidität der Herzerkrankungen—ein Überblick. Deutscher Herzbericht 2019: 11–31. https://www.herzstiftung.de/herzbericht (3 October 2020).
- 4. Christ M, Störk S, Dörr M, Heppner HJ, Müller C, Wachter R, Riemer U, for the Trend HF Germany Project . Heart failure epidemiology 2000–2013: insights from the German Federal Health Monitoring System. Eur J Heart Fail 2016; 18: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 5. Federal Statistical Office and Robert Koch Institute . The information system of the Federal Health Monitoring. http://www.gbe‐bund.de/gbe10/pkg_isgbe5.prc_isgbe?p_uid=gast%26p_aid=0%26p_sprache=E (3 October 2019)
- 6. Neumann T, Biermann J, Erbel R, Neumann A, Wasem J, Ertl G, Dietz R. Heart failure: the commonest reason for hospital admission in Germany: medical and economic perspectives. Dtsch Arztebl Int 2009; 106: 269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Freisinger E, Fuerstenberg T, Malyar NM, Wellmann J, Keil U, Breithardt G, Reinecke H. German nationwide data on current trends and management of acute myocardial infarction: discrepancies between trials and real‐life. Eur Heart J 2014; 35: 979–988. [DOI] [PubMed] [Google Scholar]
- 8. Keller K, Hobohm L, Ostad MA, Göbel S, Lankeit M, Konstantinides S, Münzel T, Wenzel P. Temporal trends and predictors of inhospital death in patients hospitalised for heart failure in Germany. Eur J Prev Cardiol 2020: 2047487320936020. [DOI] [PubMed] [Google Scholar]
- 9. Gobel S, Hobohm L, Ostad MA, Lavie CJ, Gori T, Münzel T, Wenzel P, Keller K. Sex‐specific differences drive temporal trends and outcomes of patients hospitalized for heart failure in Germany. Prog Cardiovasc Dis 2020; 63: 591–598. [DOI] [PubMed] [Google Scholar]
- 10. Berliner D, Hänselmann A, Bauersachs J. The treatment of heart failure with reduced ejection fraction. Dtsch Arztebl Int 2020; 117: 376–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seferovic PM, Ponikowski P, Anker SD, Bauersachs J, Chioncel O, Cleland JGF, Boer RA, Drexel H, Ben Gal T, Hill L, Jaarsma T, Jankowska EA, Anker MS, Lainscak M, Lewis BS, McDonagh T, Metra M, Milicic D, Mullens W, Piepoli MF, Rosano G, Ruschitzka F, Volterrani M, Voors AA, Filippatos G, Coats AJS. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2019; 21: 1169–1186. [DOI] [PubMed] [Google Scholar]
- 12. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group . 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 13. Neuhauser H, Diederichs C, Boeing H, Felix SB, Jünger C, Lorbeer R, Meisinger C, Peters A, Völzke H, Weikert C, Wild P, Dörr M. Hypertension in Germany. Dtsch Arztebl Int 2016; 113: 809–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schipf S, Ittermann T, Tamayo T, Holle R, Schunk M, Maier W, Meisinger C, Thorand B, Kluttig A, Greiser KH, Berger K, Müller G, Moebus S, Slomiany U, Icks A, Rathmann W, Völzke H. Regional differences in the incidence of self‐reported Type 2 diabetes in Germany: results from five population‐based studies in Germany (DIAB‐CORE Consortium). J Epidemiol Community Health 2014; 68: 1088–1095. [DOI] [PubMed] [Google Scholar]
- 15. Schipf S, Werner A, Tamayo T, Holle R, Schunk M, Maier W, Meisinger C, Thorand B, Berger K, Mueller G, Moebus S, Bokhof B, Kluttig A, Greiser KH, Neuhauser H, Ellert U, Icks A, Rathmann W, Völzke H. Regional differences in the prevalence of known type 2 diabetes mellitus in 45–74 years old individuals: results from six population‐based studies in Germany (DIAB‐CORE Consortium). Diabet Med 2012; 29: e88–e95. [DOI] [PubMed] [Google Scholar]
- 16. Dunlay SM, Roger VL, Redfield MM. Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 2017; 14: 591–602. [DOI] [PubMed] [Google Scholar]
- 17. Ertl G, Angermann CE, Bekeredjian R, Beyersdorf F, Güder G, Gummert J, Katus HA, Kindermann I, Pauschinger M, Perings S, Raake PW. Aufbau und Organisation von Herzinsuffizienz‐Netzwerken (HF‐NETs) und Herzinsuffizienz‐ Einheiten (“Heart Failure Units”, HFUs) zur Optimierung der Behandlung der akuten und chronischen Herzinsuffizienz—Gemeinsame Empfehlungen der DGK und der DGTHG zur Behandlung der Herzinsuffizienz. Der Kardiologe 2016; 10: 222–235. [Google Scholar]
- 18. Greene SJ, Butler J, Albert NM, DeVore AD, Sharma PP, Duffy CI, Hill CL, McCague K, Mi X, Patterson JH, Spertus JA, Thomas L, Williams FB, Hernandez AF, Fonarow GC. Medical therapy for heart failure with reduced ejection fraction: the CHAMP‐HF registry. J Am Coll Cardiol 2018; 72: 351–366. [DOI] [PubMed] [Google Scholar]
- 19. Luo N, Fonarow GC, Lippmann SJ, Mi X, Heidenreich PA, Yancy CW, Greiner MA, Hammill BG, Hardy NC, Turner SJ, Laskey WK, Curtis LH, Hernandez AF, Mentz RJ, O'Brien EC. Early adoption of sacubitril/valsartan for patients with heart failure with reduced ejection fraction: insights from Get With the Guidelines–Heart Failure (GWTG‐HF). JACC Heart Fail 2017; 5: 305–309. [DOI] [PubMed] [Google Scholar]
- 20. Jones NR, Roalfe AK, Adoki I, Hobbs FDR, Taylor CJ. Survival of patients with chronic heart failure in the community: a systematic review and meta‐analysis. Eur J Heart Fail 2019; 21: 1306–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Diederichs C, Neuhauser H, Kroll L, Lange C, Mensink G, Dornquast C, Heidemann C, Scheidt‐Nave C, Busch M. Regional differences in the prevalence of cardiovascular risk factors in men and women in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2017; 60: 151–162. [DOI] [PubMed] [Google Scholar]
- 22. Hawkins NM, Jhund PS, McMurray JJ, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail 2012; 14: 138–146. [DOI] [PubMed] [Google Scholar]
- 23. Bundy JD, Ning H, Zhong VW, Paluch AE, Lloyd‐Jones DM, Wilkins JT, Allen NB. Cardiovascular health score and lifetime risk of cardiovascular disease: the Cardiovascular Lifetime Risk Pooling Project. Circ Cardiovasc Qual Outcomes 2020; 13: e006450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ahmad FS, Ning H, Rich JD, Yancy CW, Lloyd‐Jones DM, Wilkins JT. Hypertension, obesity, diabetes, and heart failure‐free survival: the Cardiovascular Disease Lifetime Risk Pooling Project. JACC Heart Fail 2016; 4: 911–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nolte E, Shkolnikov V, McKee M. Changing mortality patterns in East and West Germany and Poland. I: long term trends (1960–1997). J Epidemiol Community Health 2000; 54: 890–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Guideline‐based therapy for heart failure [Leitliniengerechte Therapie bei Herzinsuffizienz]. 2014. https://www.versorgungsatlas.de (25 July 2020).
- 27. Dornquast C, Willich SN, Reinhold T. Prevalence, mortality, and indicators of health care supply—association analysis of cardiovascular diseases in Germany. s 2018; 5: 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. German Cardiac Society—Certified heart failure units [Deutsche Gesellschaft für Kardiologie (DGK)—Zertifizierte Heart Failure Units]. (Accessed July 15 th 2020, at https://hfu.dgk.org/zertifizierte‐hfus; access date: July 25th 2020.)
- 29. Koehler F, Koehler K, Deckwart O, Prescher S, Wegscheider K, Kirwan BA, Winkler S, Vettorazzi E, Bruch L, Oeff M, Zugck C, Doerr G, Naegele H, Störk S, Butter C, Sechtem U, Angermann C, Gola G, Prondzinsky R, Edelmann F, Spethmann S, Schellong SM, Schulze PC, Bauersachs J, Wellge B, Schoebel C, Tajsic M, Dreger H, Anker SD, Stangl K. Efficacy of telemedical interventional management in patients with heart failure (TIM‐HF2): a randomised, controlled, parallel‐group, unmasked trial. Lancet 2018; 392: 1047–1057. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Distribution of HF hospitalisation cases. Displayed are distributions of HF‐related hospital admissions by 3‐year time periods and the whole study period according to age groups and gender. Colours of the lines have the following meaning: grey = whole Germany, blue = West Germany, green = East Germany.
Table S2. Relative changes in HF‐related hospital deaths from. Shown are relative changes of in‐hospital in HF patients in 2017 compared to 2000 for whole Germany, West Germany and East Germany by age groups.
Figure S1. Map of the German federal states. Federal states located in East Germany are shown in green (i.e. Brandenburg, Mecklenburg‐Western Pomerania, Saxony, Saxony‐Anhalt, and Thuringia), federal states in West Germany are shown in blue (i.e., remaining states, including Berlin).
Figure S2. Hospital admissions. Hospital days. and in‐hospital deaths for heart failure and all other diagnoses in whole Germany 2000 to 2017. Graph shows absolute numbers indexed to the year 2000 (=100) per respective event type due to heart failure and all other diagnoses.
Figure S3. Crude numbers of heart failure (HF)‐related hospitalisations in East and West Germany 2000 to 2017. Graph shows crude numbers of HF‐related hospital cases for both sexes, women and men.
Figure S4. Age‐standardised numbers of heart failure related hospitalisations per 100.000 population in East and West Germany 2000 to 2017. Graph shows crude numbers of hospitalisations due to heart failure for both sexes, women and men.
Figure S5. Age distribution of the population in East and West Germany in 2000 and 2017 by age groups. The graphs illustrate the percentages of different age groups in the total population in East Germany and West Germany. Of note, between 2000 and 2017, the median age increased from 39 to 45 years in West Germany and from 41 to 49 years in East Germany.
Figure S6. Heart failure‐related hospitalisations from 2000 to 2017 according to age groups. Displayed are HF‐related hospital admissions in predefined age groups for (A) whole Germany, (B) West Germany and (C) East Germany. Percentages on the right denominate increase from 2000 to 2017. Please note different scaling on the ordinates.
Figure S7. Temporal trends of mean length of in‐hospital stay due to heart failure and all diagnoses in East and West Germany 2000 to 2017. Graph shows mean values of hospital days related to heart failure and all diagnoses.


