Abstract
Introduction
Overall, patients with Sars-cov-2 disease treated with mechanical ventilation, which is not the case in our study. This report presents our first successful experience of awake ECMO application in a critical patient with hypoxemic Respiratory Failure related to COVID-19 infection in Morocco.
Case management
We have reported a 52-year-old female patient who was diagnosed with COVID-19 infection and progressed to critical cases. She was a candidate for applying awake extracorporeal membrane oxygenation (ECMO) in the absence of invasive mechanical ventilation, under local anesthesia alone with good progress and ventilatory weaning.
Conclusion
This therapeutic attitude can be beneficial for certain critical and severe cases due to COVID-19 infection. Each ECMO program should develop goals, methods, protocols, and best practices while adapting appropriately to the personnel and equipment available.
Keywords: Extracorporeal membrane oxygenation, Venovenous ECMO, Acute respiratory distress syndrome, COVID-19, Awake, Case report
Highlights
-
•
Extracorporeal membrane oxygenation (ECMO) is extracorporeal life support used as salvage therapies in patients with acute cardiac, pulmonary or cardiopulmonary failure.
-
•
Early initiation of awake venovenous extracorporeal membrane oxygenation (ECMO) in critical cases of COVID-19 infection.
-
•
“Awake ECMO” support in patients with COVID-19 is feasible and has benefits in the absence of mechanical ventilation.
1. Introduction
Extracorporeal membrane oxygenation (ECMO) is extracorporeal life support used as salvage therapies in patients with acute cardiac, pulmonary or cardiopulmonary failure who have failed conventional treatment such as respiratory support [1].
Invasive mechanical ventilation (IMV) was used as the first therapeutic approach in patients with severe acute respiratory failure [2]. Its failure exposes patients to the risk of lung damage induced by mechanical ventilation, such as pneumonia acquired by mechanical ventilation (PAMV).
Veno-venous ECMO has anecdotally been applied as an alternative to IMV in the context of a COVID-19 infection in an awake and spontaneously-breathing patient with ARDS and presented a satisfactory result [3,4]. It is our first experience of early initiation of awake venovenous extracorporeal membrane oxygenation (ECMO) in critical cases.
The purpose of this study was to assess the feasibility and highlight the benefits of using “awake ECMO” support in the absence of mechanical ventilation.
2. Case presentation
In this article, we report a COVID-19 patient with severe ARDS who was unresponsive to high-flow nasal oxygen and non-invasive ventilation (NIV), and who was successfully treated with “fully awake ECMO” prolonged, thus avoiding endotracheal intubation and IMV.
On March 2021, a 52-year-old female patient (body mass index 31 kg/m2) was diagnosed with COVID-19 10 days before transferring to our hospital for further treatment. Her past medical history indicated that she had systemic hypertension, treated with calcic inhibitor. She presented with fever, chills, cough, and dyspnea on her admission to our intensive care unit. Physical examination showed a deterioration of general conditions, fever at 39 °C, normal hemodynamic state with tachycardia 126 pulse/minute, pulmonary crackles, and her saturation (SpO2) was 47 % on room air. She was not responding to oxygen via a facemask and high-flow nasal oxygen with a SpO2 of 50 %; oxygen inhalation immediately was given by noninvasive ventilation (NIV) as Initial therapy (minute ventilation 26 L/min, positive end-expiratory pressure [PEEP] 7 cm H2O, an inspiratory fraction of oxygen [FiO2] 100 %) then her SpO2 increased to 88 %. Blood gas values under NIV show PO2 41 mmHg, PCO2 45 mmHg, Lactate 1.9 mmol/L with FiO2 100 %.
The complete blood count showed: C-reactive protein and white blood cells high respectively (214 mg/L; 19440/mm3) with a positive procalcitonin at 1.44 ng/mL, high level of LDH, ferritin, D-dimer, and fibrinogen (1106 UI/L; 633.59 μg/L; 11.5 g/L; 8.1 g/L), Interleukin 6 was high also at 126 pg/ml, lymphopenia at 570/mm3, with normal hemostasis and kidney function.
The ECG 12-lead showed sinusal tachycardia with a heart rate of 86 bpm, normal axis without conduction or repolarization disturbances.
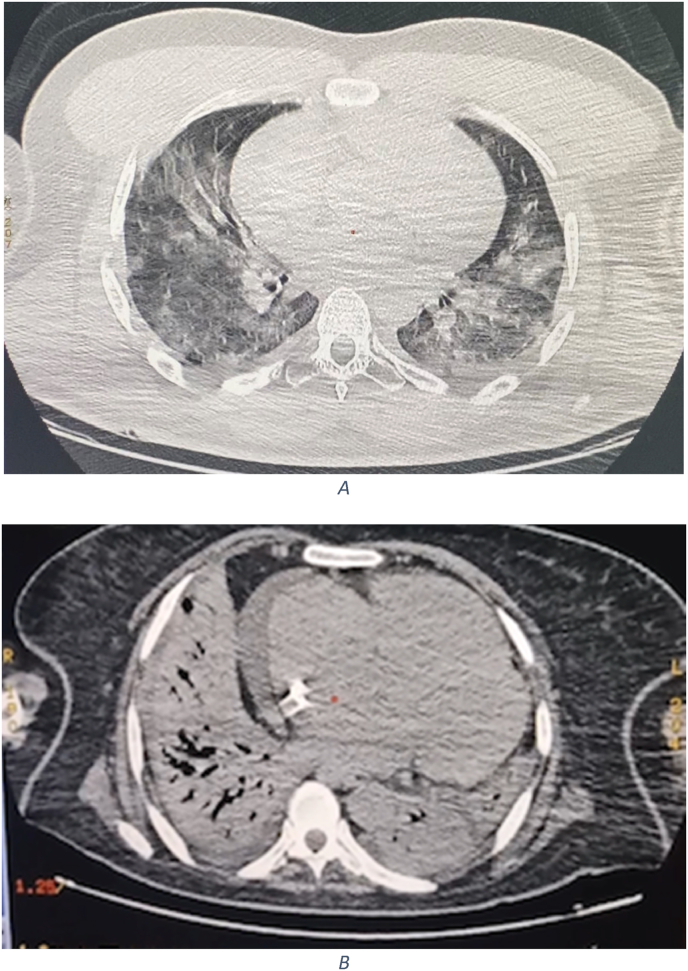
Chest CT indicated multifocal ground-glass opacities in both lungs presence triangular, peripheral and bilateral with crazy paving and foci of condensation with an estimated attack of more than 75 % related to viral pneumonia due to COVID-19 without associated pulmonary embolism (Fig. 1 A). Transthoracic echocardiogram (TTE) was normal.
Fig. 1.
A: Chest CT on the first day of admission; B: Chest CT on the 36 days of supports VV ECMO.
Antibiotics initiated the medical treatment, corticosteroids (Dexamethasone 6mg per day), and curative anticoagulation by Enoxaparine 100 UI/kg/12h.
On the 3rd day of his admission, she received a dose of Tacolizumab. Without improvement leading to initiating plasma exchange (PLEX) therapy on the 5th day of stay: for five sessions with the exchange of 3 L of plasma each session, a decrease in IL 6 was noted (48 pg/ml).
On day 15, after her admission to the ICU, the patient was anxious, and she presented a respiratory worsening with desaturation reaching 67 % under NIV with FiO2 100 %. Given the non-improvement, the VV ECMO was proposed to the patient and connected to VV ECMO. A 27F dual lumen cannula was inserted through the right internal jugular under NIV and local anesthesia.
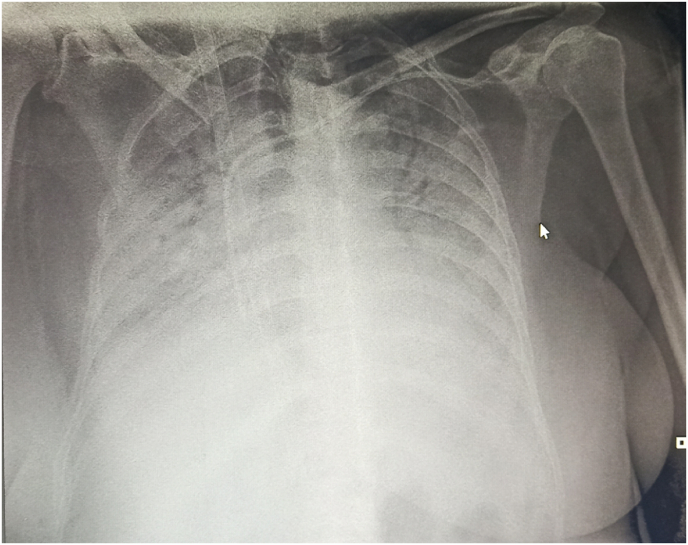
During the first week of support ECMO, ECMO jugular blood flow from 3.4 to 4.8 L/min, purge gas flow rate of 2–4 L/min, with a membrane O2 fraction (FmO2) set at 100 %. The patient was at ease with normocardia and less tachypnea under a high flow nasal cannula (30–50 L/min), with a Chest x-ray shows the cannula in place (Fig. 2).
Fig. 2.
Chest x-ray after setting up support VV ECMO.
Chest CT on day 36 of support VV ECMO showed extensive bilateral parenchymatous condensations with fibrosis features associated with the right lower pulmonary embolism with the presence of indirect signs of pulmonary embolism during routine bedside TTE (Fig. 1 B). Consequently, high-dose corticosteroids were initiated.
In particular, he had a single episode of nosocomial pneumonia on day 27 of support VV ECMO by multi-resistant Klebsiella sensitive to chloramphenicol.
Chest CT on day 52 of support VV ECMO does not show any improvement compared to the first CT scan done under ECMO, the presence of bilateral foci of condensation with Fibrosis noted (Fig. 3).
Fig. 3.
Chet CT on the 52 day of support VV ECMO.
She performed daily pulmonary and physical rehabilitation in bed with a physiotherapist. On day 22 of ECMO installation, she was able to get up with help. Throughout his stay in the intensive care unit, oral nutrition was maintained, as was social interaction face-to-face with loved ones. Indeed, she was informed daily of his health state. It is her 60 days of VV ECMO support in weaning.
This cases report follows scare guidelines [5].
3. Discussion
Veno-venous-extracorporeal membrane oxygenation (VV-ECMO) has been used as a rescue treatment for patients with severe acute respiratory distress syndrome (ARDS) due to COVID-19 infection with survival rates similar to those reported for ECMO support of ARDS of other causes [6,7].
The need for prolonged mechanical ventilation, sedation, and immobility may put patients at risk for ventilator-assisted pneumonia. Hence the interest of a “fully-awake” ECMO strategy in this patient [8]. Indeed, unlike the data reported for COVID-19 patients with an extended support ECMO [5], our patient had only one episode of nosocomial infection, as was noted in the paper of Schmidt and al [9].
As previously suggested and According to the literature review, wake up VV-ECMO for those with isolated non-intubated lung injury, breathing spontaneously with severe ARDS, seems more appropriate [9,10], As observed in our study.
Awake ECMO versus IMV to keep a patient awake is experimental and requires further studies in patients with ARDS associated with COVID-19. This strategy could theoretically be offered to many COVID-19 patients treated with high flow oxygen or even NIV and who refuse mechanical ventilation [11].
To avoid the complications of this VV ECMO management, routine bedside transthoracic echocardiography (TTE) and chest x-ray may be sensitive in the early detection of indirect signs of pulmonary embolism or even intra-cardiac thrombus and in order to improve the diagnostic and therapeutic process at the right time and to help better the management of patients positive for Covid-19 [12].
In addition, this awake ECMO strategy could become a promising alternative to IMV treatments. To limit the risk of infection, loss of muscle mass, myopathy, and polyneuropathy, while maintaining the psycho-social side of the patient with his relatives also the medical and paramedical staff [13].
Our patient was satisfied with our medical care.
However, careful monitoring of the risks associated with ECMO is required, and further studies in experienced ECMO centers are needed to assess the benefit of this strategy.
4. Conclusion
Our case reports the utility of awake VV ECMO in the treatment of critically ill COVID-19 patients without the use of invasive mechanical ventilation. However, clinical evidence was needed to verify whether awake ECMO could be widely used in treating these patients or even severe ARDS caused by other outbreaks.
Ethical approval
The ethical committee approval was not required give the article type (case report).However, the written consent to publish the clinical data of the patients was given and is available to check by the handling editor if needed.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
EL AIDOUNI Ghizlane: Corresponding author, study concept, Data collection, data analysis, writing review & editing.
MERBOUH Manal: Contributor.
BERRAJAA Sara: Contributor.
BAHOUH Choukri: Contributor.
BERRICHI Samia: Contributor.
EL KAOUINI Abderrahim: Contributor.
ZIANI Hamid: Contributor, data collection.
BOUABDALLAOUI Amine: Contributor.
BKIYAR Houssam: supervision and data validation.
HOUSNI Brahim: supervision and data validation.
Registration of research studies
This is not an original research project involving human participants in an interventional or an observational study but a case report. This registration is was not required.
Guarantor
EL AIDOUNI Ghizlane.
Consent
Obtained.
Declaration of competing interest
The authors state that they have no conflicts of interest for this report.
Contributor Information
El Aidouni Ghizlane, Email: elaidounighizlane@gmail.com.
Merbouh Manal, Email: manal.mrb@gmail.com.
Berrajaa Sara, Email: berrajaasara@gmail.com.
Bahouh Choukri, Email: choukribahouh17@gmail.com.
Berrichi Samia, Email: Sammia9@gmail.com.
El Kaouini Abderrahim, Email: abderrahimfmpo19@gmail.com.
Ziani Hamid, Email: hamid.ziani2018@gmail.com.
Bouabdallaoui Amine, Email: amine-bouabdallaoui1992@hotmail.com.
Bkiyar Houssam, Email: 7b.houssam@gmail.com.
Housni Brahim, Email: brahimhousni@yahoo.fr.
References
- 1.Tang 1 Junyi, Li 1 Wencan, Jiang 1 Fanli, Wang 2 Tao. Successfully treatment of application awake extracorporeal membrane oxygenation in critical COVID-19 patient: a case report. J. Cardiothorac. Surg. 2020 Dec 17;15(1):335. doi: 10.1186/s13019-020-01376-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajagopal K, Keller SP, Akkanti B, et al. Advanced pulmonary and cardiac support of COVID-19 patients: emerging recommendations from ASAIO—a living working document. Circ Heart Fail. 13: e0071752020. [DOI] [PMC free article] [PubMed]
- 3.Mohite Prashant N. 1, anton sabashnikov 1, anna reed 1, diana G saez 1, nikhil P patil 1, aron-frederik popov 1, fabio DeRobertis 1, toufan bahrami 1, mohamed amrani 1, martin carby 1, sundip kaul 1, andre R simon, extracorporeal life support in "awake" patients as a bridge to lung transplant. Thorac. Cardiovasc. Surg. 2015 Dec;63(8):699–705. doi: 10.1055/s-0035-1546429. [DOI] [PubMed] [Google Scholar]
- 4.Hoeper M.M., Wiesner O., Hadem J., Wahl O., Suhling H., Duesberg C., Sommer W., Warnecke G., Greer M., Boenisch O., Busch M., Kielstein J.T., Schneider A., Haverich A., Welte T., Kuhn C. Extracorporeal membrane oxygenation instead of invasive mechanical ventilation in patients with acute respiratory distress syndrome. Intensive Care Med. 2013;39:2056–2057. doi: 10.1007/s00134-013-3052-3. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines, Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt M., Hajage D., Lebreton G., Monsel A., Voiriot G., Levy D., Baron E., Beurton A., Chommeloux J., Meng P., Nemlaghi S., Bay P., Leprince P., Demoule A., Guidet B., Constantin J.M., Fartoukh M., Dres M., Combes A. Groupe de Recherche Clinique en REanimation et Soins intensifs du Patient en Insuffisance Respiratoire aiguE (GRCRESPIRE) Sorbonne Université, Paris-Sorbonne ECMO-COVID investigators. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30328-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barbaro R.P., MacLaren G., Boonstra P.S., Iwashyna T.J., Slutsky A.S., Fan E., Bartlett R.H., Tonna J.E., Hyslop R., Fanning J.J., Rycus P.T., Hyer S.J., Anders M.M., Agerstrand C.L., Hryniewicz K., Diaz R., Lorusso R., Combes A., Brodie D. Extracorporeal life support organization. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the extracorporeal life support organization registry. Lancet. 2020;396:1071–1078. doi: 10.1016/S0140-6736(20)32008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Covid-ICU Group on behalf of the REVA Network and the Covid-ICU Investigators Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intens. Care Med. 2020 doi: 10.1007/s00134-020-06294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt Matthieu, de Chambrun Marc Pineton, Lebreton Guillaume, Hékimian Guillaume, Chommeloux Juliette, Bréchot Nicolas, Barhoum Petra, Lefevre Lucie, Juvin Charles, Molle Julie, Luyt Charles-Edouard, Combes Alain. Extracorporeal membrane oxygenation instead of invasive mechanical ventilation in a patient with severe COVID-19-associated acute respiratory distress syndrome. AJRCCM. 2021;26 doi: 10.1164/rccm.202102-0259. April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoeper M.M., Wiesner O., Hadem J., Wahl O., Suhling H., Duesberg C., Sommer W., Warnecke G., Greer M., Boenisch O., Busch M., Kielstein J.T., Schneider A., Haverich A., Welte T., Kuhn C. Extracorporeal membrane oxygenation instead of invasive mechanical ventilation in patients with acute respiratory distress syndrome. Intensive Care Med. 2013;39:2056–2057. doi: 10.1007/s00134-013-3052-3. [DOI] [PubMed] [Google Scholar]
- 11.Grieco D.L., Menga L.S., Cesarano M., Rosà T., Spadaro S., Bitondo M.M., Montomoli J., Falò G., Tonetti T., Cutuli S.L., Pintaudi G., Tanzarella E.S., Piervincenzi E., Bongiovanni F., Dell'Anna A.M., Delle Cese L., Berardi C., Carelli S., Bocci M.G., Montini L., Bello G., Natalini D., De Pascale G., Velardo M., Volta C.A., Ranieri V.M., Conti G., Maggiore S.M., Antonelli M. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. J. Am. Med. Assoc. 2021 doi: 10.1001/jama.2021.4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El aidouni Ghizlane, Merbouh Manal, Aabdi Mohammed, Bouabdallaoui Amine, Bkiyar Houssam, Smaili Nabila, El ouafi Nouha, Housni Brahim. Intra cardiac thrombus in critically ill patient with coronavirus disease 2019: Case report. Ann. Med. Surg. 2021:102434. doi: 10.1016/j.amsu.2021.102434. 66 june. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langer T., Santini A., Bottino N., Crotti S., Batchinsky A.I., Pesenti A., Gattinoni L. “Awake” extracorporeal membrane oxygenation (ECMO): pathophysiology, technical considerations, and clinical pioneering. Crit. Care. 2016;20:150. doi: 10.1186/s13054-016-1329-y. [DOI] [PMC free article] [PubMed] [Google Scholar]