Acupuncture can be defined as the insertion of needles into the body at specific points (i.e., acupoints) for the purpose of treatment. Increasing evidence from large-scale effectiveness trials have shown that effectiveness of real and sham acupuncture did not differ significantly.1, 2, 3 However, considering the issues of blinding and physiological inertness of the sham needles, neither the Streitberger nor the Park sham device is an adequate control intervention. As sham needles do not constitute proper control in acupuncture research, we should not claim that acupuncture treatment is no more effective than a placebo control.4 To answer the controversy regarding sham acupuncture, neuroimaging techniques have been applied to investigate the effects of various components of acupuncture treatment on the central nervous system. In neuroimaging studies, the brain hemodynamic responses to acupunctural stimulation were shown to reflect sensory-discriminative as well as cognitive and affective dimensions of pain.5 Both the sensory-discriminative component and affective-social touch of acupuncture treatment are crucial for the therapeutic effect of acupuncture treatment in clinical practice.6
Based on the predictive coding paradigms, somatic sensations can be inferred by integrating afferent signals and high-level cognitive processes.7 For example, experiences and expectations prior to acupuncture stimulation also influence the perception of somatic sensations and therapeutic effects. Notably, similar to real acupuncture, sham acupuncture includes tactile stimulation, enhanced doctor-patient relationship, bodily sensation (de qi), and expectation regarding the treatment.8 Despite the reduced somatosensory inputs of sham acupuncture compared with real acupuncture, high-level cognitive components of sham acupuncture are very comparable with real acupuncture treatment and might explain why sham acupuncture can exert similar effects as real acupuncture. The power of mind (i.e., the non-specific effects of treatment) can be a crucial factor in pain modulation of acupuncture and other alternative medical practices.9 The brain contributes to reshaping how bottom-up information is processed through top-down regulation.
Herein, we introduce a series of studies on how top-down components of acupuncture affect the acupuncture action, especially bodily awareness, bodily attention, anticipation of stimulation, and medical context. First, acupuncture stimulation was delivered to the rubber hand, which participants experienced as their own hand using the rubber hand illusion, an experimental model to modify body ownership. Acupuncture stimulation on the rubber hand resulted in the de qi sensation as well as brain activation in the dorsolateral prefrontal cortex, insula, secondary somatosensory cortex, and visual area when the rubber hand was fully incorporated into the body.10 Second, acupuncture stimulation was administered to the embodied prosthetic hand or fake hand in an amputee patient. Brain activation responding to acupuncture stimulation in the prosthetic hand was observed in the contralateral insula, primary motor cortex, premotor cortex, and primary somatosensory cortex. Conversely, brain activation responding to acupuncture stimulation in the fake hand was observed only in the visual cortex.11 These results indicate that psychophysical and neurophysiological responses associated with acupuncture stimulation to the incorporated hand were influenced by an enhanced bodily awareness of the hand. Third, enhanced bodily awareness combined with acupuncture stimulation without afferent somatosensory inputs could evoke similar brain responses as real acupuncture. In addition, enhanced bodily attention triggered by genuine acupuncture stimulation can activate the salience network and deactivate the default mode network regardless of the actual stimulation12, which indicates that the component of enhanced attention to a certain part of the body is significant in the brain response to acupuncture stimulation. Fourth, expectation of electroacupuncture stimulation in the absence of an afferent somatosensory signal, induced significantly greater intensity of de qi sensation and brain activation in the right anterior insula, right inferior frontal gyrus, pre-supplementary motor area, and secondary somatosensory cortex.13 This result indicates that the sensory experience of electroacupuncture stimulation may be derived from expectation, which involves a function of the salience network in monitoring internal and external body states. Lastly, therapeutic effects of acupuncture can be modulated by the treatment context. Acupuncture yielded greater brain activation in reward-related brain areas (e.g., ventral striatum) in participants who received acupuncture stimulation as a treatment for pain relief compared with participants who received acupuncture as a painful stimulation. These findings indicate that inserting needles into the body in the context of treatment can activate reward circuitries in the brain and modulate brain response to experimental pain in the pain matrix.14
The cognitive component of acupuncture can influence the pain modulatory effect of the acupuncture treatment, as shown in previous studies. Phantom acupuncture, which is a visually presented acupuncture ritual to make participants believe they are receiving real acupuncture, evokes phasic autonomic responses to acupuncture and needling orienting response.15 Phantom acupuncture also results in significant pain reduction, with a significant correlation between the brain activation in the prefrontal cortex and the score assessing belief in acupuncture effectiveness.16 Recently, video-guided acupuncture imagery treatment (VGAIT) also successfully reduced pain in individuals when watching a video of acupuncture on the participant's own body and imagining its application. Both VGAIT and real acupuncture induce brain changes in brain regions involved in pain modulation, including the insula, cingulate, and prefrontal cortices.17 Functional connectivity showed that responses to real acupuncture were associated with brain activities in the basal ganglia, and responses to VGAIT were primarily associated with brain activities in the anterior insula.18 These results show that somatosensory components as well as visual components associated with needling can contribute to acupuncture analgesia by, ultimately, combining contextual meaning with verbal instruction.19 The clinical acupuncture setting includes a combination of the needling experiences and other contextual factors of a complex treatment situation.20 Taken together, acupuncture treatment not only involves simple needling but also includes complex healing processes.
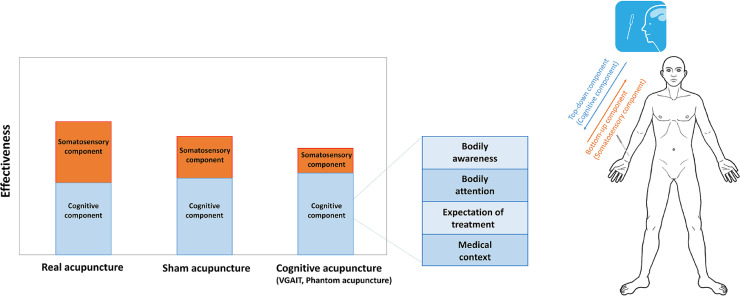
In summary, acupuncture is a complex treatment comprised of multimodal sensory stimulation that interacts with various cognitive factors. Acupuncture treatment involves touch, insertion, and healing ritual, consisting of multiple components including somatosensory stimulation, treatment context, and attention to needle-based procedures. Body ownership, enhanced bodily attention, anticipation of stimulation, and treatment context can be important factors that influence physiological responses during acupuncture stimulation. Understanding the top-down components of acupuncture treatment may be important for further scientific investigation on the effects and underlying mechanisms of acupuncture and lead to the development of a new sham acupuncture more suitable for clinical trials Fig. 1.
Fig. 1.
The role of cognitive components in acupuncture treatment
Acupuncture treatment involves touch, insertion, and healing ritual, consisting of multiple components including somatosensory stimulation, treatment context, and attention to needle-based procedures. Bottom-up components of acupuncture include somatosensory inputs, and top-down components include bodily awareness, bodily attention, anticipation of stimulation, and medical context. Because cognitive components of acupuncture contribute to acupuncture analgesia, sham acupuncture can achieve similar clinical improvements to real acupuncture.
Author contributions
Conceptualization: ISL and YC. Writing – Original Draft: ISL and YC. Writing – Review & Editing: YC.
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1A4A1018598, 2021R1F1A1046705).
Ethical statement
No ethical approval was required for this manuscript as this study did not include human subjects or laboratory animals.
Data availability
Not applicable.
Conflict of interest
The authors declare no conflict of interests.
References
- 1.Linde K, Streng A, Jurgens S, Hoppe A, Brinkhaus B, Witt C. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293(17):2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- 2.Zhang CS, Tan HY, Zhang GS, Zhang AL, Xue CC, Xie YM. Placebo devices as effective control methods in acupuncture clinical trials: a systematic review. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0140825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ee C, Xue C, Chondros P, Myers SP, French SD, Teede H. Acupuncture for menopausal hot flashes: a randomized trial. Ann Intern Med. 2016;164(3):146–154. doi: 10.7326/M15-1380. [DOI] [PubMed] [Google Scholar]
- 4.Chae Y. The dilemma of placebo needles in acupuncture research. Acupunct Med. 2017;35(5):382–383. doi: 10.1136/acupmed-2017-011394. [DOI] [PubMed] [Google Scholar]
- 5.Chae Y, Chang DS, Lee SH, Jung WM, Lee IS, Jackson S. Inserting needles into the body: a meta-analysis of brain activity associated with acupuncture needle stimulation. J Pain. 2013;14(3):215–222. doi: 10.1016/j.jpain.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Chae Y, Olausson H. The role of touch in acupuncture treatment. Acupunct Med. 2017;35(2):148–152. doi: 10.1136/acupmed-2016-011178. [DOI] [PubMed] [Google Scholar]
- 7.Friston K. The free-energy principle: a unified brain theory? Nat Rev Neurosci. 2010;11(2):127–138. doi: 10.1038/nrn2787. [DOI] [PubMed] [Google Scholar]
- 8.Lee YS, Chae Y. Powerful effects of placebo needles. Acupunct Med. 2018;36(3):197–198. doi: 10.1136/acupmed-2017-011516. [DOI] [PubMed] [Google Scholar]
- 9.Kong J, Eshel MN. Applying the power of the mind in acupuncture treatment of pain. Med Acupunct. 2020;32(6):367–372. doi: 10.1089/acu.2020.1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chae Y, Lee IS, Jung WM, Park K, Park HJ, Wallraven C. Psychophysical and neurophysiological responses to acupuncture stimulation to incorporated rubber hand. Neurosci Lett. 2015;591:48–52. doi: 10.1016/j.neulet.2015.02.025. [DOI] [PubMed] [Google Scholar]
- 11.Lee IS, Jung WM, Lee YS, Wallraven C, Chae Y. Brain responses to acupuncture stimulation in the prosthetic hand of an amputee patient. Acupunct Med. 2015;33(5):420–424. doi: 10.1136/acupmed-2015-010785. [DOI] [PubMed] [Google Scholar]
- 12.Jung WM, Lee IS, Wallraven C, Ryu YH, Park HJ, Chae Y. Cortical activation patterns of bodily attention triggered by acupuncture stimulation. Sci Rep. 2015;5:12455. doi: 10.1038/srep12455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung WM, Ryu Y, Park HJ, Lee H, Chae Y. Brain activation during the expectations of sensory experience for cutaneous electrical stimulation. Neuroimage Clin. 2018;19:982–989. doi: 10.1016/j.nicl.2018.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee IS, Wallraven C, Kong J, Chang DS, Lee H, Park HJ. When pain is not only pain: inserting needles into the body evokes distinct reward-related brain responses in the context of a treatment. Physiol Behav. 2015;140:148–155. doi: 10.1016/j.physbeh.2014.12.030. [DOI] [PubMed] [Google Scholar]
- 15.Lee J, Napadow V, Kim J, Lee S, Choi W, Kaptchuk TJ. Phantom acupuncture: dissociating somatosensory and cognitive/affective components of acupuncture stimulation with a novel form of placebo acupuncture. PLoS One. 2014;9(8) doi: 10.1371/journal.pone.0104582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makary MM, Lee J, Lee E, Eun S, Kim J, Jahng GH. Phantom acupuncture induces placebo credibility and vicarious sensations: a parallel fMRI study of low back pain patients. Sci Rep. 2018;8(1):930. doi: 10.1038/s41598-017-18870-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao J, Tu Y, Orr SP, Lang C, Park J, Vangel M. Analgesic effects evoked by real and imagined acupuncture: a neuroimaging study. Cereb Cortex. 2019;29(8):3220–3231. doi: 10.1093/cercor/bhy190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cao J, Tu Y, Wilson G, Orr SP, Kong J. Characterizing the analgesic effects of real and imagined acupuncture using functional and structure MRI. Neuroimage. 2020;221 doi: 10.1016/j.neuroimage.2020.117176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee J, Eun S, Kim J, Lee JH, Park K. Differential influence of acupuncture somatosensory and cognitive/affective components on functional brain connectivity and pain reduction during low back pain state. Front Neurosci. 2019;13:1062. doi: 10.3389/fnins.2019.01062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Musial F. Acupuncture for the treatment of pain - a mega-placebo? Front Neurosci. 2019;13:1110. doi: 10.3389/fnins.2019.01110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.