Abstract
Introduction:
Having higher purpose in life has been linked to favorable health outcomes. However, little research has examined whether the purpose–health association persists across different levels of SES. This study assesses whether the association between higher purpose in life and lower mortality is similar across levels of SES.
Methods:
A national sample of 13,159 U.S. adults aged >50 years from the Health and Retirement Study was analyzed. The baseline year was 2006/2008. Purpose in life was assessed at baseline using the Purpose in Life Subscale of the Ryff Psychological Well-being Scales. Risk of death during an 8-year follow-up was assessed. SES was measured using education, income, and wealth. Using multivariable Poisson regression, effect modification by SES was tested on both the additive and multiplicative scales. Analyses were done in 2020.
Results:
In analyses stratified by SES, people with the highest level of purpose (versus lowest) consistently tended to have lower mortality risk across levels of SES. However, people with mid-range purpose levels had lower mortality risk only if they also had mid-to-high education, income, and wealth. When formally testing the effect modification by SES, there was modest evidence that the associations between higher purpose and lower mortality were stronger among individuals with high education, income, and wealth.
Conclusions:
The highest level of purpose appeared protective against all-cause mortality regardless of levels of SES. On the other hand, when levels of purpose were more modest, people with lower SES may benefit less health-wise from having a purpose.
INTRODUCTION
Biomedical science and public health have almost exclusively focused on reducing risk factors. This deficit-focused approach has generated important preventive and therapeutic interventions. However, an emerging body of research suggests that also focusing on increasing health-promoting assets may be valuable, and emerging research suggests there are modifiable health assets that contribute to reduced risk of chronic disease and mortality.1,2 Purpose in life, the extent that people perceive their lives as having a sense of direction and goals, is a promising candidate health asset, and growing evidence suggests that it has salubrious effects.3–8 Studies suggest that higher purpose is associated with healthier biological function (e.g., reduced allostatic load, reduced inflammation),9–11 better physical function, reduced risk of chronic disease (e.g., lower risk of cardiovascular disease and declining cognitive function),10,12–17 and lower cause-specific mortality (e.g., lower mortality risk from heart, circulatory, and blood conditions—but not other causes),18 and lower all-cause mortality.13
Limited work has considered if the purpose–health relationship is moderated by key social structural factors such as SES.19 Specifically, individuals with higher versus lower SES might receive greater benefit from a sense of purpose because they are more likely to have infrastructural resources that facilitate the mechanisms through which purpose provides health benefits. For example, evidence suggests that purpose enhances health via increasing likelihood of engaging in healthy behavior.17,20 However, the intermediate pathway(s) through which purpose provides health benefits (i.e., promoting healthy behaviors) may be disrupted by a lack of resources (e.g., unable to afford a gym membership or live in a neighborhood without adequate walking or bike paths).
Understanding the potentially heterogeneous effects of purpose on health by SES can help identify subgroups where purpose interventions might be more, or less, health protective. For example, finding that purpose is associated with favorable health across the SES spectrum might suggest that the health benefits of purpose are realizable in multiple SES environments.21 Alternatively, results might suggest that potential purpose interventions have larger beneficial health effects in only specific subgroups, unless additional infrastructural resources are also available. However, little research has formally examined if the association between a sense of purpose and health (or mortality) is modified by SES. To address this research gap, this study examines whether the longitudinal association between purpose and all-cause mortality differs by levels of education, income, and wealth (i.e., effect modification by SES) among U.S. older adults.
METHODS
Study Population
Data were from the Health and Retirement Study (HRS), an ongoing nationally representative panel study of U.S. adults aged >50 years. It began in 1992 and surveys participants every 2 years; in 2006, study staff began visiting a randomly selected 50% of HRS study participants for an enhanced face-to-face interview. The remaining 50% of participants were assessed with the same protocol in 2008.22 After these interviews, respondents were given a self-administered psychosocial questionnaire that included an assessment of purpose.22 The questionnaires were completed and returned by mail; the response rate was 88% in 2006 and 84% in 2008.
Respondents were combined from both timepoints (N=13,770) and 2006/2008 was considered the baseline for the current study. Individuals with missing information on either purpose or death (n=611) were excluded, resulting in a final analytic sample of 13,159 participants. Because the study used de-identified, publicly available data, the Harvard T.H. Chan School of Public Health IRB exempted it from review. In addition, all HRS respondents provided written informed consent.
Measures
To keep the length of follow-up constant across all participants, information about death was obtained up to 2014 (for the 2006 subsample) and up 2016 (for the 2008 subsample). Thus, this study assessed death over an 8-year follow-up period in each subsample (2006–2014 and 2008–2016). Information about death was obtained first via an exit interview conducted with next of kin. When confirming the exit interviews with deaths reported by the National Death Index, there was a 95.5% match.23
Purpose in life was assessed at baseline (2006/2008) using the validated 7-item Purpose in Life Subscale of the Ryff Psychological Well-being Scales.24 Participants responded to each item on a 6-point Likert scale, and an overall score was derived using the mean of item responses such that higher scores reflect higher purpose (Cronbach’s α=0.74). Following HRS protocol, if respondents completed >5 of 7 items, a purpose score was derived (96.9%). To evaluate the possibility of a non-linear relationship between purpose and mortality, purpose was assessed as quartiles based on the baseline distribution of purpose scores in the analytic sample (Table 1 provides cut points).
Table 1.
Relative Risks for the Joint Exposure of Purpose in Life and Education (N=13,159)a
| Sense of purpose in lifeb | Additive and multiplicative effect modification | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Medium–low | Medium–high | High | Low | Medium–low | Medium–high | High | ||||||||
| Level of education | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | Additivec | Multiplicatived | Additive | Multiplicative | Additive | Multiplicative | |
| <High school | 421/591 | 1.0 | 222/394 | 0.97 (0.82, 1.14); p=0.72 | 164/340 | 0.96 (0.80, 1.15); p=0.64 | 75/308 | 0.68 (0.53, 0.87); p<0.01 | ref | ref | ref | ref | ref | ref | ref |
| High school | 667/1,196 | 1.04 (0.92, 1.18); p=0.55 | 441/1,365 | 0.90 (0.78, 1.04); p=0.15 | 402/1,526 | 0.86 (0.74, 0.99); p=0.03 | 257/1,369 | 0.77 (0.66, 0.91); p<0.01 | ref | −0.11 (−0.31, 0.09); p=0.30 | 0.89 (0.73, 1.10); p=0.28 | −0.14 (−0.36, 0.07); p=0.20 | 0.86 (0.69, 1.07); p=0.18 | 0.05 (−0.16, 0.27); p=0.63 | 1.09 (0.82, 1.45); p=0.54 |
| ≥College | 171/397 | 1.05 (0.88, 1.27); p=0.72 | 138/603 | 0.81 (0.67, 1.00); p=0.05 | 158/864 | 0.76 (0.62, 0.92); p<0.01 | 136/928 | 0.70 (0.57, 0.86); p<0.01 | ref | −0.21 (−0.48, 0.06); p=0.13 | 0.80 (0.60, 1.05); p=0.11 | −0.26 (−0.53, 0.02); p=0.07 | 0.75 (0.56, 0.99); p=0.04 | −0.03 (−0.30, 0.24); p=0.81 | 0.98 (0.70, 1.37); p=0.89 |
Notes: Boldface indicates statistical significance (p<0.05). The total number of cases in the table does not add up to the size of our analytic sample (N=13,159) because there was missing data in the education variable and the number of cases were derived from those study respondents who did not have missing data on this variable.
RRs were adjusted for age, gender, race/ethnicity, marital status, household income, wealth, health insurance, heart disease, stroke, cancer, diabetes, hypertension, lung disease, arthritis, and depression using Poisson regression.
Purpose in life was assessed using the purpose in life subscale of the Ryff Psychological Well-being Scales. Purpose in Life Quartiles: Low: 1.00–3.86; Medium–low: 3.87–4.57; Medium–high: 4.58–5.29; High: 5.30–6.00.
Effect modification on additive scale: relative excess risk due to interaction (RERI; SEs were calculated by using the delta method).
Effect modification on multiplicative scale: ratio of risk ratio (RRR).
RR, risk ratio.
As potential effect modifiers of the association between purpose in life and mortality, 3 separate measures of SES at baseline were examined, including: (1) education, (2) annual total household income, and (3) total wealth. These 3 factors were chosen because they are key SES indicators, capture different aspects of social exposure, and tap into different mechanisms that influence health.19 Missing income and total wealth values (but not educational attainment) were imputed by HRS as described in detail elsewhere.25 Respondents self-reported their educational attainment and were categorized according to the highest degree they attained: less than high school, high school or GED, and college or more. Annual total household income was assessed and calculated as the sum of the respondents’ and spouses’: earnings, pensions, annuities, supplemental security income, social security disability income, social security retirement income, unemployment and workers’ compensation, other government transfers, household capital income, and income from other sources.26 The aggregated continuous income variable was then categorized into quartiles: (Quartile 1: ≤$20,024, Quartile 2: $20,025–$38,321, Quartile 3: $38,322–$71,895, Quartile 4: ≥$71,896). Total wealth was calculated as the sum of the following: primary residence, real estate, vehicles, businesses, IRA/Keogh, stocks and mutual funds, checking, savings, money market accounts, CDs, government savings bonds, treasury bills, bonds or bond funds, mortgages, and debt. Net wealth was categorized into quintiles: Quintile 1: ≤$35,000, Quintile 2: $35,001–$140,000, Quintile 3: $140,001–$311,000, Quintile 4: $311,001–$652,500, Quintile 5: ≥$652,501.
All covariates were self-reported at baseline and selected a priori based on existing literature and theoretical grounds.17,27,28 They included sociodemographic characteristics, baseline physical health, and depression. Sociodemographic characteristics included: age (continuous), gender (man, woman), race/ethnicity (White, Black, Hispanic, other), marital status (married, not married), and health insurance (covered, not covered). Baseline physical health included self-reported presence/absence of having a doctor’s diagnosis for: heart disease, cancer, stroke, diabetes, hypertension, lung disease, and arthritis. Depression was assessed using the 8-item Center for Epidemiological Studies Depression Scale (Cronbach’s α=0.80; a score of ≥4 was categorized as depressed).29
Statistical Analysis
Because the outcome (death) was not rare (i.e., 24.7%), Poisson regression models30 were used to estimate the association between baseline purpose and risk of death over the 8-year follow-up period. To assess for potential effect modification by each of the 3 SES indicators, 3 separate models were fit. In each model, product terms between baseline purpose (quartile dummy variables) and the SES indicator of interest (dummy variables) were introduced. In each of the models, the other 2 SES indicators, age, gender, race/ethnicity, marital status, health insurance, baseline health status, and depression were adjusted as potential confounders. All 3 indicators of SES were included in each model because they can all be potential confounders of the purpose–mortality relationship. Because depression has been identified as a risk factor for mortality,31 depression was adjusted for to reduce concerns that purpose simply reflects the absence of depression.
Following the framework proposed by Knol and VanderWeele,32 a series of effect estimates and measures of effect modification were computed. First, using Poisson models, RRs were estimated to evaluate the association between purpose and mortality within each strata of SES. Second, RRs for the association of a joint exposure to purpose and SES with mortality over the 8-year follow-up period were estimated; the reference group in the second analysis was the group with the lowest purpose in life and lowest SES. Third, using the RRs for the joint purpose and SES exposure from the second analysis, measures of effect modification were estimated on both the additive (relative excess risk due to interaction [RERI]) and multiplicative (ratio of risk ratios [RRR]) scales. Additive effect modification has rarely been reported in epidemiology despite their public health relevance.32 Appendix Text 1 provides a more detailed description of how to estimate and interpret these measures of effect modification. Appendix Table 1 provides an example of how the regression coefficients from the Poisson model that assesses effect modification by education were combined. As many statistical tests for effect modification by each level of each SES indicator were performed, low power and multiple testing are both concerns. Thus, a sensitivity analysis in which purpose and each SES indicator were coded as continuous variables was conducted. An omnibus test for multiplicative effect modification using single product terms between continuous purpose and a continuously coded version of each SES indicator were then conducted.
Among the analytic sample of 13,159 individuals, some participants were missing data on education and other covariates. Complete case analyses that ignored missing data resulted in a loss of 2.9% (n=377) of the analytic sample. Missing data were thus imputed using multiple imputation by chained equation.33 All the variables used in the main analyses were included when creating 20 imputed data sets. The analyses were performed in each imputed data set, and combined estimates across the datasets via Rubin’s rule,34 using the R package “mice”. Additional information about covariates and missing can be found in the Appendix Text 2. All analyses were performed using R, version 3.6.0 in 2020.
RESULTS
Appendix Table 2 shows the descriptive statistics of the analytic sample. Among the 13,159 individuals in the study sample, 3,253 people (24.7%) died by the end of 8-year follow-up period. Individuals with higher baseline purpose were less likely to die during the follow-up period compared with those with lower purpose (e.g., 15.2% in the “high” baseline purpose group and 36.5% in the “low” baseline purpose group). Overall, those with higher baseline purpose (versus lower) tended to have higher SES, better baseline physical health, and a lower prevalence of depression.
Associations between purpose and 8-year mortality risk, stratified by SES, are shown in Figure 1 and Appendix Table 3. Overall, people with high (versus low) purpose consistently tended to have lower mortality risk, regardless of educational attainment, income, or wealth. However, when analyzing people with mid-range levels of purpose (i.e., “medium-high” and “medium-low”), there was an association with mortality only among people who also had higher SES.
Figure 1.
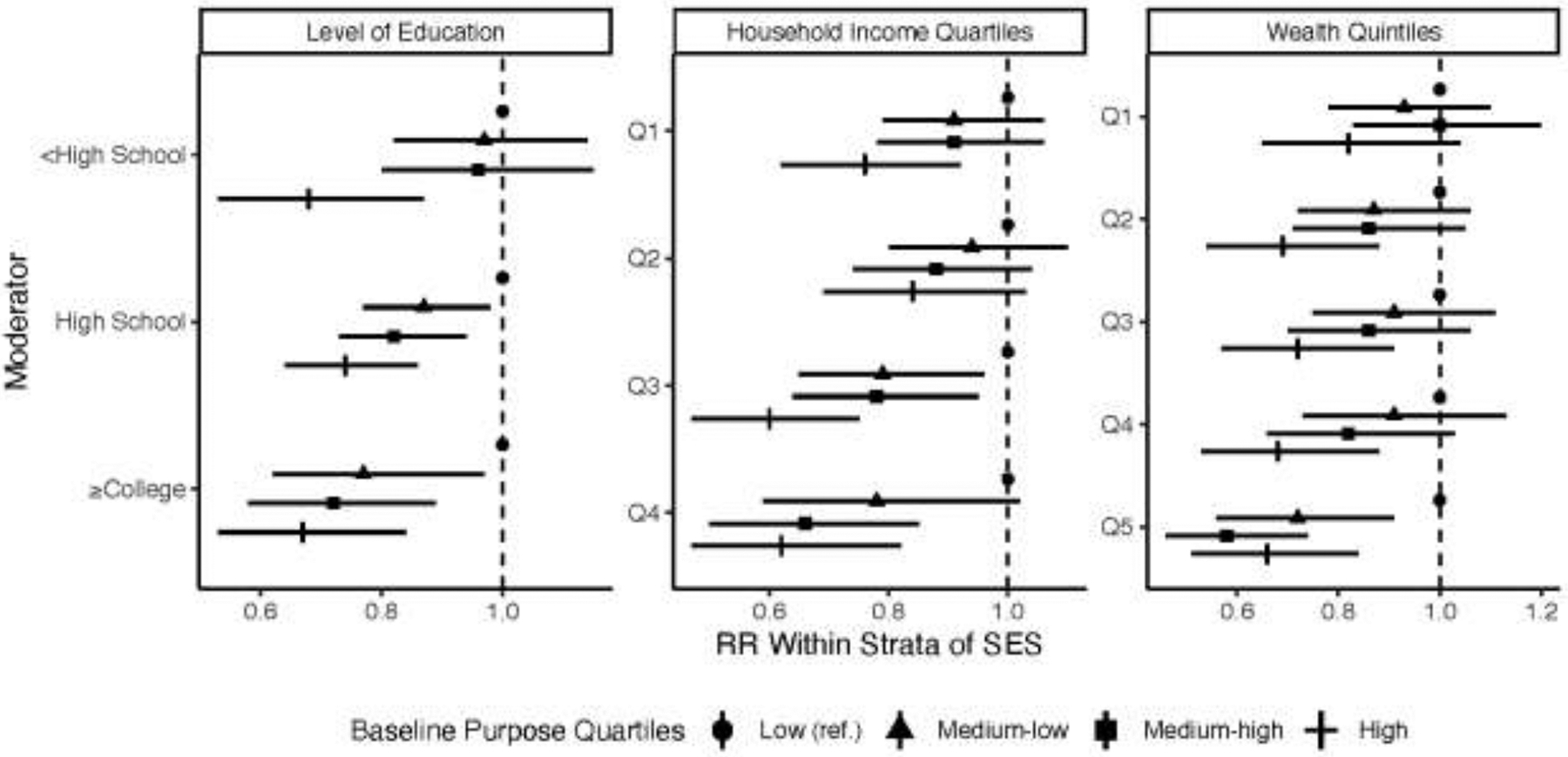
Associations between baseline purpose in life and 8-year mortality within strata of educational attainment, income quartiles, and wealth quintiles.a,b,c,d
aRRs were adjusted for: age, gender, race/ethnicity, marital status, health insurance, heart disease, stroke, cancer, diabetes, hypertension, lung disease, arthritis, and depression using Poisson regression. Each model was further adjusted for the other two SES indicators (e.g., income and wealth for the education model).
bPurpose in life was assessed using the purpose in life subscale of the Ryff Psychological Well-being Scales. Purpose in life quartiles: low: 1.00–3.86; medium–low: 3.87–4.57; medium–high: 4.58–5.29; high: 5.30–6.00.
cHousehold income quartiles: 1st quartile: ≤$20,024; 2nd quartile: $20,025–$38,321; 3rd quartile: $38,322–$71,895; 4th quartile: ≥$71,896.
dWealth quintiles: 1st quintile: ≤$35,000; 2nd quintile: $35,001–$140,000; 3rd quintile: $140,001–$311,000; 4th quintile: $311,001–$652,500; 5th quintile: ≥$652,501.
RR, risk ratio.
For example, within levels of education, people who had high (versus low) purpose consistently displayed lower mortality risk. However, there was strong evidence that people with medium-high purpose had lower mortality risk only among people who attained high school (RR=0.82, 95% CI=0.73, 0.94) or college degrees or higher (RR=0.72, 95% CI=0.58, 0.89), but not among people with less than high school degrees (RR=0.96, 95% CI=0.80, 1.15). Similarly, there was evidence that people with mid-range purpose levels (versus low purpose) had lower mortality only among those with higher income (Quartiles 3 and 4) or wealth (Quintile 5), and not among those with lower income (Quartiles 1 and 2) or wealth (Quartiles 1–4).
Tables 1–3 show associations between the joint exposure of purpose and SES with mortality, where there was some evidence of negative effect modification by SES on both the additive and multiplicative scales. For instance, the joint exposure of having medium-high purpose/being college educated or higher was more strongly associated with lower mortality risk than the simple sum of the 2 exposures alone (RERI= −0.26, 95% CI= −0.53, 0.02; RRR=0.75, 95% CI=0.56, 0.99) (Table 1). Similarly, modest evidence of negative effect modification was found for the joint exposure of medium-high purpose with either the highest income quartile (Quartile 4; RERI= −0.21, 95% CI= −0.47, 0.04; RRR=0.72, 95% CI=0.53, 0.98) (Table 2) or the highest quintile of wealth (Quintile 5; RERI= −0.40, 95% CI= −0.68, −0.13; RRR=0.58, 95% CI=0.43, 0.78) (Table 3).
Table 3.
Relative Risks for the Joint Exposure of Purpose in Life and Wealth (N=13,159)a
| Sense of purpose in lifeb | Additive and multiplicative effect modification | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Medium–low | Medium–high | High | Low | Medium–low | Medium–high | High | ||||||||
| Wealth quintilesc | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | Additived | Multiplicativee | Additive | Multiplicative | Additive | Multiplicative | |
| 1st quintile | 389/592 | 1.0 | 207/451 | 0.93 (0.78, 1.10); p=0.40 | 170/402 | 1.00 (0.83, 1.20); p=0.98 | 84/330 | 0.81 (0.64, 1.03); p=0.08 | ref | ref | ref | ref | ref | ref | ref |
| 2nd quintile | 2,990/504 | 0.94 (0.81, 1.10); p=0.45 | 166/483 | 0.82 (0.68, 0.99); p=0.04 | 156/470 | 0.82 (0.67, 0.99); p=0.04 | 900/422 | 0.66 (0.53, 0.84); p<0.01 | ref | −0.05 (−0.28, 0.18); p=0.68 | 0.94 (0.73, 1.21); p=0.63 | −0.12 (−0.378, 0.13); p=0.33 | 0.87 (0.67, 1.13); p=0.29 | −0.09 (−0.36, 0.18); p=0.52 | 0.87 (0.62, 1.22); p=0.42 |
| 3rd quintile | 234/430 | 0.89 (0.75, 1.05); p=0.18 | 164/456 | 0.81 (0.67, 0.98); p=0.03 | 142/555 | 0.77 (0.63, 0.94); p=0.01 | 88/539 | 0.66 (0.51, 0.80); p<0.01 | ref | −0.01 (−0.25, 0.22); p=0.90 | 0.97 (0.75, 1.26); p=0.84 | −0.12 (−0.37, 0.13); p=0.34 | 0.86 (0.66, 1.13); p=0.29 | −0.06 (−0.33, 0.20); p=0.63 | 0.88 (0.63, 1.23); p=0.46 |
| 4th quintile | 172/361 | 0.85 (0.70, 1.03); p=0.09 | 155/515 | 0.78 (0.64, 0.95); p=0.01 | 142/638 | 0.71 (0.57, 0.87); p<0.01 | 88/640 | 0.57 (0.45, 0.73); p<0.01 | ref | 0.00 (−0.24, 0.24); p=0.99 | 0.99 (0.75, 1.30); p=0.92 | −0.15 (−0.40, 0.11); p=0.27 | 0.83 (0.62, 1.11); p=0.21 | −0.09 (−0.36, 0.19); p=0.54 | 0.83 (0.59, 118); p=0.31 |
| 5th quintile | 165/299 | 0.95 (0.78, 1.16); p=0.64 | 109/461 | 0.68 (0.54, 0.86); p<0.01 | 108/676 | 0.55 (0.44, 0.69); p<0.01 | 108/682 | 0.63 (0.50, 0.80); p<0.01 | ref | −0.20 (−0.46, 0.06); p=0.13 | 0.77 (0.57, 1.03); p=0.08 | −0.40 (−0.68, −0.13); p<0.01 | 0.58 (0.43, 0.78); p<0.01 | −0.13 (−0.41, 0.15); p=0.36 | 0.82 (0.58, 116); p=0.24 |
Notes: Boldface indicates statistical significance (p<0.05).
Risk ratios were adjusted for age, gender, race/ethnicity, marital status, education, household income, health insurance, heart disease, stroke, cancer, diabetes, hypertension, lung disease, arthritis, and depression using Poisson regression.
Purpose in life was assessed using the purpose in life subscale of the Ryff Psychological Well`being Scales. Purpose in life quartiles: low: 1.00–3.86; medium–low: 3.87–4.57; medium–high: 4.58–5.29; high: 5.30–6.00.
Wealth quintiles: 1st quintile: ≤$35,000; 2nd quintile: $35,001–$140,000; 3rd quintile: $140,001–$311,000; 4th quintile: $311,001–$652,500; 5th quintile: ≥$652,501.
Effect modification on additive scale: relative excess risk due to interaction (RERI; SEs were calculated by using delta method).
Effect modification on multiplicative scale: ratio of risk ratios (RRR).
RR, risk ratio.
Table 2.
Relative Risks for the Joint Exposure of Purpose in Life and Income (N=13,159)a
| Sense of purpose in lifeb | Additive and multiplicative effect modification | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Medium–low | Medium–high | High | Low | Medium–low | Medium–high | High | ||||||||
| Household income quartile sc | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | n, died/alive | RR (95% CI) | Additived | Multiplicativee | Additive | Multiplicative | Additive | Multiplicative | |
| 1st quartile | 565/692 | 1.0 | 273/493 | 0.91 (0.79, 1.06); p=0.22 | 220/460 | 0.91 (0.78, 1.06); p=0.23 | 122/396 | 0.76 (0.62, 0.92); p=0.01 | ref | ref | ref | ref | ref | ref | ref |
| 2nd quartile | 353/591 | 0.93 (0.81, 1.07); p=0.33 | 252/627 | 0.87 (0.74, 1.02); p=0.09 | 205/609 | 0.81 (0.69, 0.97); p<0.01 | 140/526 | 0.78 (0.64, 0.95); p=0.01 | ref | 0.03 (−0.17, 0.22); p=0.80 | 1.02 (0.82, 1.27); p=0.83 | −0.03 (−0.23, 0.18); p=0.81 | 0.96 (0.76, 1.22); p=0.76 | 0.10 (−0.13, 0.32); p=0.40 | 1.11 (0.84, 1.47); p=0.46 |
| 3rd quartile | 234/519 | 0.98 (0.83, 1.16); p=0.83 | 176/637 | 0.78 (0.65, 0.93); p=0.01 | 187/770 | 0.76 (0.64, 0.92); p<0.01 | 105/684 | 0.58 (0.47, 0.73); p<0.01 | ref | −0.12 (−0.34, 0.11); p=0.30 | 0.87 (0.68, 1.11); p=0.25 | −0.13 (−0.35, 0.10); p=0.28 | 0.86 (0.67, 1.10); p=0.23 | −0.15 (−0.39, 0.08); p=0.21 | 0.79 (0.58, 1.07); p=0.12 |
| 4th quartile | 107/384 | 0.88 (0.70, 1.10); p=0.27 | 100/609 | 0.68 (0.54, 0.86); p=0.01 | 112/902 | 0.58 (0.46, 0.72); p<0.01 | 102/1007 | 0.55 (0.43, 0.69); p<0.01 | ref | −0.11 (−0.37, 0.15); p=0.41 | 0.85 (0.63, 1.16); p=0.31 | −0.21 (−0.47, 0.04); p=0.10 | 0.72 (0.53, 0.98); p=0.04 | −0.09 (−0.35, 0.17); p=0.50 | 0.82 (0.59, 1.15); p=0.25 |
Notes: Boldface indicates statistical significance (p<0.05).
RRs ratios were adjusted for age, gender, race/ethnicity, marital status, education, wealth, health insurance, heart disease, stroke, cancer, diabetes, hypertension, lung disease, arthritis, and depression using Poisson regression.
Purpose in life was assessed using the purpose in life subscale of the Ryff Psychological Well-being Scales. Purpose in Life Quartiles: Low: 1.00–3.86; Medium–low: 3.87–4.57; Medium–high: 4.58–5.29; High: 5.30–6.00
Household income quartiles: 1st Quartile: ≤$20,024; 2nd Quartile: $20,025–$38,321; 3rd Quartile: $38,322–$71,895; 4th Quartile: ≥$71,896
Effect modification on additive scale: relative excess risk due to interaction (RERI; SEs were calculated by using delta method).
Effect modification on multiplicative scale: ratio of risk ratio (RRR).
RR, risk ratio.
For other joint exposures of purpose and SES indicators, despite point estimates consistently indicating negative effect modification (i.e., the joint exposure of higher purpose and higher SES was more strongly associated with lower mortality than the simple sum of the 2 exposures alone), CIs were wide and evidence of effect modification was weak. However, the sensitivity analysis conducting an omnibus test (Appendix Table 4) indicated strong evidence of multiplicative effect modification by income and wealth but not educational attainment.
DISCUSSION
This study showed that, in a national sample of U.S. adults aged >50 years, people who had the highest level of purpose consistently had lower mortality risk across all levels of SES. However, for people who had mid-range levels of purpose (i.e., medium-high/medium-low versus low), the protective association against mortality was more strongly evident among people who also had higher SES, particularly income and wealth. Notably, when formally testing measures of effect modification, the evidence of negative effect modification by SES, albeit weak in magnitude, was present on both the additive and multiplicative scale, which is the strongest form of effect modification for 2 preventive exposures.35 Although the evidence is not definitive given that CIs were wide and power to detect effect modification is usually very low, it is notable that most (48/54) measures of effect modification indicated negative effect modification, on both the additive and the multiplicative scales. Moreover, the sensitivity analysis of an omnibus test indicated evidence of multiplicative effect modification by income and wealth, suggesting that the associations between higher purpose and lower mortality were stronger among individuals with higher income and wealth.
Overall, the findings suggest that, though having very high levels of purpose may be universally beneficial regardless of one’s SES, more moderate levels of purpose may confer less health-promoting benefits among individuals with fewer resources. A potential reason is that a lack of economic resources may make it harder for people in lower-SES circumstances to engage in healthy behaviors. Thus, the intermediate pathway(s) through which purpose provides health benefits (i.e., promoting healthy behaviors) may be disrupted by the lack of resources unless the level of purpose is sufficiently high to motivate people with low SES to overcome disadvantage and engage in healthy behaviors. Future research should identify these potential mechanisms, as making health-relevant behaviors or psychological strategies more available and accessible to diverse individuals via intervention and policy might help enhance the potential health-protective effects of future purpose interventions in low-SES individuals. Future research should also evaluate if differing mechanisms underlying the linkages between purpose and health outcomes are at work when considering people in different levels of SES.
The findings somewhat diverged from the only other existing study that evaluated the purpose–health association by SES. Using data from 1,275 adults in the Midlife in the U.S. Study, this study evaluated the association between purpose and several indicators of health in the context of differing levels of education. The authors observed that purpose was more protective against developing chronic conditions among study participants with lower versus higher education; however, this association was not observed when evaluating other health-related outcomes such as self-rated physical health or waist circumference.36 The findings and the findings from this earlier study might somewhat differ for several reasons including differences in the: study design (cross-sectional versus longitudinal), outcome(s) that were evaluated, age group of the sample, different analytic methods, and inclusion/exclusion of different covariates.
In addition to the differential effects of purpose on health by levels of SES, it is worth noting that distributions of purpose itself differ by SES. In the HRS data, purpose slightly decreases with declining SES along a gradient (Appendix Figure 1), which is likely attributable to the challenging circumstances that low-SES individuals often experience.37,38 However, the HRS data also indicate that a sizable number of people in lower SES levels display high purpose. A key question, especially as people age, is to identify the circumstances that enable individuals across the socioeconomic spectrum to achieve equity with regard to distributions of purpose.39,40 Studying individuals who are able to cultivate and maintain high purpose, in spite of low-SES conditions, might help researchers identify individual-level factors (e.g., patterns of thinking, types of coping, methods of navigating chronically difficult situations) and social structural factors (e.g., variations in contexts, access to various resources) that can then be considered when developing interventions and policies aimed at increasing purpose for all.
This study had a number of strengths. It was conducted in a large and national sample of U.S. older adults. The study design was prospective, which minimizes concerns that observed associations might be due to retrospective reporting bias or reverse causality. Adjustment was further made for a range of key sociodemographic characteristics and health conditions to help address potential bias from confounding. Additionally, the study used a validated and widely used measure of purpose.
Limitations
There are several study limitations. First, the analytic sample was composed of individuals aged >50 years and the findings may not generalize to younger populations. Second, the items that made up the measure of “purpose” were principally concerned with goals, rather than broader life aims, or a sense of mission or calling,5,41 and these other factors may be differently associated with mortality.
CONCLUSIONS
There was evidence that SES might modify the association between purpose in life and 8-year mortality risk among older U.S. adults. A growing body of research suggests that a sense of purpose might emerge as an important upstream target for interventions and policies aimed at enhancing health behaviors and physical health. As this idea is considered, further work is needed to evaluate how the purpose–health association is patterned across the socioeconomic spectrum.
Supplementary Material
ACKNOWLEDGMENTS
ESK was supported by NIH (K99AG055696) and the Michael Smith Foundation for Health Research.
This research was supported by John Templeton Foundation Grant 61075 and NIH Grant R01CA222147. Tyler VanderWeele reports receiving personal fees from Flerish Inc. and Flourishing Metrics.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Kubzansky LD, Huffman JC, Boehm JK, et al. Positive psychological well-being and cardiovascular health promotion: JACC health promotion series. J Am Coll Cardiol. 2018;72(12):1382–1396. 10.1016/j.jacc.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.VanderWeele TJ, Chen Y, Long K, Kim ES, Trudel-Fitzgerald C, Kubzansky LD. Positive epidemiology? Epidemiology. 2020;31(2):189–193. 10.1097/ede.0000000000001147. [DOI] [PubMed] [Google Scholar]
- 3.Ryff CD. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom. 2014;83(1):10–28. 10.1159/000353263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steger MF, Frazier P, Oishi S, Kaler M. The meaning in life questionnaire: assessing the presence of and search for meaning in life. J Couns Psychol. 2006;53:80–93. 10.1037/0022-0167.53.1.80. [DOI] [Google Scholar]
- 5.McKnight PE, Kashdan TB. Purpose in life as a system that creates and sustains health and well-being: an integrative, testable theory. Rev Gen Psychol. 2009;13:242–251. 10.1037/a0017152. [DOI] [Google Scholar]
- 6.Frankl VE. Man’s Search for Meaning. Boston, MA: Beacon Press; 2006. [Google Scholar]
- 7.George LS, Park CL. The Multidimensional Existential Meaning Scale: a tripartite approach to measuring meaning in life. J Posit Psychol. 2017;12(6):613–627. 10.1080/17439760.2016.1209546. [DOI] [Google Scholar]
- 8.Heintzelman SJ, King LA. Life is pretty meaningful. Am Psychol. 2014;69(6):561–574. 10.1037/a0035049. [DOI] [PubMed] [Google Scholar]
- 9.Zilioli S, Slatcher RB, Ong AD, Gruenewald TL. Purpose in life predicts allostatic load ten years later. J Psychosom Res. 2015;79(5):451–457. 10.1016/j.jpsychores.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steptoe A, Fancourt D. Leading a meaningful life at older ages and its relationship with social engagement, prosperity, health, biology, and time use. Proc Natl Acad Sci. 2019;116(4):1207–1212. 10.1073/pnas.1814723116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hafez D, Heisler M, Choi H, Ankuda CK, Winkelman T, Kullgren JT. Association between purpose in life and glucose control among older adults. Ann Behav Med. 2018;52(4):309–318. 10.1093/abm/kax012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim ES, Kawachi I, Chen Y, Kubzansky LD. Association between purpose in life and objective measures of physical function in older adults. JAMA Psychiatry. 2017;74(10):1039–1045. 10.1001/jamapsychiatry.2017.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2016;78:122–133. 10.1097/psy.0000000000000274. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y, Kim ES, Koh HK, Frazier AL, VanderWeele TJ. Sense of mission and subsequent health and well-being among young adults: an outcome-wide analysis. Am J Epidemiol. 2019;188(4):664–673. 10.1093/aje/kwz009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewis NA, Turiano NA, Payne BR, Hill PL. Purpose in life and cognitive functioning in adulthood. Aging Neuropsychol Cogn. 2016;24(6):662–671. 10.1080/13825585.2016.1251549. [DOI] [PubMed] [Google Scholar]
- 16.Yu L, Boyle PA, Wilson RS, Levine SR, Schneider JA, Bennett DA. Purpose in life and cerebral infarcts in community-dwelling older people. Stroke. 2015;46(4):1071–1076. 10.1161/strokeaha.114.008010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim ES, Delaney SW, Kubzansky LD. Sense of purpose in life and cardiovascular disease: underlying mechanisms and future directions. Curr Cardiol Rep. 2019;21(11):135. 10.1007/s11886-019-1222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alimujiang A, Wiensch A, Boss J, et al. Association between life purpose and mortality among U.S. adults older than 50 years. JAMA Netw Open. 2019;2(5):e194270. 10.1001/jamanetworkopen.2019.4270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krieger N, Williams DR, Moss NE. Measuring social class in U.S. public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 20.Kim ES, Shiba K, Boehm JK, Kubzansky LD. Sense of purpose in life and five health behaviors in older adults. Prev Med. 2020;139:106172. 10.1016/j.ypmed.2020.106172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen E, Miller GE. Socioeconomic status and health: mediating and moderating factors. Annu Rev Clin Psychol. 2013;9(1):723–749. 10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]
- 22.Smith J, Ryan L, Fisher G, Sonnega A, Weir D. HRS psychosocial and lifestyle questionnaire 2006–2016: documentation report. https://hrs.isr.umich.edu/sites/default/files/biblio/HRS%202006-2016%20SAQ%20Documentation_07.06.17_0.pdf. Published July 2017. Accessed January 2021.
- 23.Weir D. Validating mortality ascertainment in the Health and Retirement Study. https://hrs.isr.umich.edu/sites/default/files/biblio/Weir_mortality_ascertainment.pdf. Published November 3, 2016. Accessed January 2021.
- 24.Ryff CD, Keyes CLM. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–727. 10.1037/0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 25.Hurd MD, Meijer E, Moldoff M, Rohwedder S. Improved wealth measures in the Health and Retirement Study: asset reconciliation and cross-wave imputation. https://www.rand.org/content/dam/rand/pubs/working_papers/WR1100/WR1150/RAND_WR1150.pdf. Published April 2016. Accessed January 2021.
- 26.Pantoja P, Bugliari D, Campbell N, et al. RAND HRS Detailed Imputations File 2014 (V2) Documentation. https://www.rand.org/content/dam/rand/www/external/labor/aging/dataprod/randhrsimp1992_2014v2.pdf. Published February 2018. Accessed March 24, 2021.
- 27.Kubzansky LD, Huffman JC, Boehm JK, et al. Positive psychological well-being and cardiovascular health promotion. J Am Coll Cardiol. 2018;72(12):1382–1396. 10.1016/j.jacc.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.VanderWeele TJ. On the promotion of human flourishing. Proc Natl Acad Sci. 2017;114(31):8148–8156. 10.1073/pnas.1702996114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steffick DE. Documentation of affective functioning measures in the Health and Retirement Study. https://hrs.isr.umich.edu/sites/default/files/biblio/dr-005.pdf. Published 2000. Accessed January 2021.
- 30.Knol MJ, Le Cessie S, Algra A, Vandenbroucke JP, Groenwold RHH. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ Can Med Assoc J. 2012;184(8):895–899. 10.1503/cmaj.101715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry. 2014;171(4):453–462. 10.1176/appi.ajp.2013.13030325. [DOI] [PubMed] [Google Scholar]
- 32.Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514–520. 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by Chained equations in R. J Stat Softw. 2011;45(1):1–67. 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- 34.Little RJA, Rubin DB. Bayes and multiple imputation. In: Little RJA, Rubin DB, ed. Statistical Analysis With Missing Data. Hoboken, NJ: Wiley; 2014:200–220. 10.1002/9781119013563.ch10. [DOI] [Google Scholar]
- 35.VanderWeele TJ. The interaction continuum. Epidemiology. 2019;30(5):648–658. 10.1097/EDE.0000000000001054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kirsch JA, Ryff CD. Hardships of the Great Recession and health: understanding varieties of vulnerability. Health Psychol Open. 2016;3(1):2055102916652390. 10.1177/2055102916652390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186(1):5–23. 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- 38.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29(1):235–252. 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 39.Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry. 2006;14(1):6–20. 10.1097/01.jgp.0000192501.03069.bc. [DOI] [PubMed] [Google Scholar]
- 40.Netuveli G, Wiggins RD, Montgomery SM, Hildon Z, Blane D. Mental health and resilience at older ages: bouncing back after adversity in the British Household Panel Survey. J Epidemiol Community Health. 2008;62(11):987–991. 10.1136/jech.2007.069138. [DOI] [PubMed] [Google Scholar]
- 41.Hanson JA, VanderWeele TJ. The Comprehensive Measure of Meaning: psychological and philosophical foundations. In: Lee MT, Kubzansky LD, VanderWeele TJ, ed. Measuring Well-Being: Interdisciplinary Perspectives from the Social Sciences and the Humanities. 1st ed. Oxford, England: Oxford; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


