Abstract
Background
Hip pain during pregnancy is very common, but hip avascular necrosis represents a very rare entity.
Case report
We report a rare case of a healthy30-year-old female patient pregnant with twins, that suffered right hip avascular necrosis in the peripartum period, her symptoms were initially neglected as a benign cause of hip pain, this led to aggressive treatment at a young age.
Discussion
With less than 100 cases reported in the literature, pregnancy is not a well-known risk factor for femoral head avascular necrosis and it should be differentiated from one of the more common hip pathologies in pregnancy which is the so-called “Pelvic pain syndrome” and transient osteoporosis of the hip.
Conclusion
Having a high index of suspicion and low threshold for MRI imaging in a pregnant woman with hip pain is a must to prevent such complications.
Keywords: Avascular necrosis, Hip, Primary hip replacement, Pregnancy hip pain
Highlights
-
•
Corticosteroids and alcohol intake are the most common atraumatic cause of hip osteonecrosis
-
•
Hip and pelvic pain during pregnancy are very frequent and may hide a serious event such as hip avascular necrosis
-
•
Hip avascular necrosis can have disastrous complications if not diagnosed in young pregnant women.
-
•
Having a high index of suspicion in a pregnant woman with hip pain is a must to prevent such complications
1. Introduction
The pathophysiology for avascular necrosis is related to disruption of the blood flow to the affected femoral head with subsequent osteocyte and bone marrow cells death, which will eventually lead to necrosis and subsequent subchondral bone collapse [1].
There are several well-established causative factors of hip osteonecrosis as trauma, alcohol abuse, high dosage corticosteroid treatment, genetic predisposition, coagulation abnormalities and sickle cell disease [1]. With less than 100 cases reported in the literature, pregnancy is not a well-known risk factor for femoral head avascular necrosis and it should be differentiated from one of the more common hip pathologies in pregnancy which is the so-called “Pelvic pain syndrome” and transient osteoporosis of the hip [2], [3]. Due to the rare association of pregnancy and avascular necrosis of the femoral head, we had a case of neglected hip pain in a pregnant patient with twins that led to avascular necrosis of the femoral head with subchondral bone collapse, that if well investigated early on could have been treated more conservatively.
This case was reported in line with the SCARE criteria [4].
2. Case presentation
A healthy 30-year-old female patient Gravida 1 Para 1 presented with right hip pain that started immediately after pregnancy. This patient had an uneventful pregnancy that ended with delivery at 40 weeks of gestational age to a healthy non-identical twins by C-section.
Her pain started after delivery as a mechanical pain when ambulating associated with discomfort in her right hip, she has consulted her Obstetrician for these complaints and were neglected as a benign cause of hip pain without asking for imaging, eventually her symptoms worsened causing her a painful limp and incapacitating her daily functioning, so she consulted us 6 months after the onset of her symptoms in our orthopedic department.
Upon presentation she was wheelchair bound and unable to walk unassisted. She has no history of drug intake, alcohol abuse or trauma, she was nonsmoker and she never received any corticosteroid treatment.
On Physical exam she had a painful Range of motion of the hip, mainly with limitation of flexion and internal rotation of the hip. Standard X-rays of the pelvis and the hip (Fig. 1) showed crescent sign with subchondral bone collapse. MRI T-1 weighted images (Fig. 2) shows osteonecrosis of the femoral head with a subchondral collapse fracture of the necrotic bone located in the anterosuperior aspect of the femoral head corresponding to FICAT stage III.
Fig. 1.
Standard anteroposterior and lateral radiographs of the hip showing crescent sign with subchondral bone collapse of the right hip.
Fig. 2.
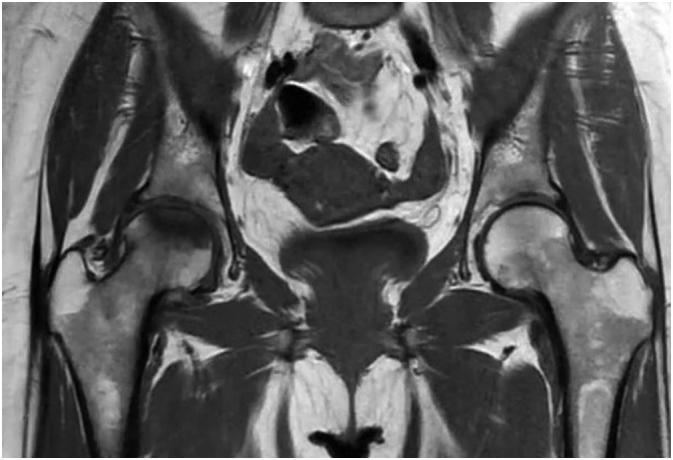
MRI T-1 weighted image shows osteonecrosis of the femoral head with a subchondral collapse fracture of the necrotic bone located in the anterosuperior aspect of the femoral head.
Her Lab tests Complete blood count, Prothrombin time, partial thromboplastin time, C-reactive protein, Erythrocyte sedimentation rate, TSH, Lipid panel, Liver function tests, Creatinine, Anti-nuclear antibody and Rheumatoid factor all came back within normal limits. Eventually she was diagnosed with idiopathic avascular necrosis of the femoral head related to pregnancy. The patient underwent an uneventful right ceramic on ceramic total hip arthroplasty (Fig. 3). Follow up at 3 weeks, 6 weeks, 3 months and 9 months post op reveal complete resolution of symptoms with a pain free gait without limping.
Fig. 3.

Post op X-ray of right ceramic on ceramic bearing total hip arthroplasty.
3. Discussion
Corticosteroids and alcohol intake are the most common atraumatic cause of hip osteonecrosis [3], [5]. Other risk factors include hypercoagulopathy, microemboli, vasculitis, genetics and cocaine use [6]. While idiopathic cause of hip avascular necrosis accounts for a large entity around 20% [3], [5], pregnancy as a risk factor for hip avascular necrosis has not yet been established well, it has been cited in the literature with several case reports and only small series, the largest one of 13 cases reported by Montella et al. in 1999 [7].
Multiple pathophysiologic mechanisms for hip avascular necrosis during pregnancy have been postulated but none of them were to be proven as a sole causative factor. Venous congestion and increased coagulability are common in pregnancy [7], [8], [9]. As well some endocrine alteration during pregnancy were also implied to increase the risk of hip avascular necrosis due to increase in plasma levels of unbound cortisol [7], [8], also parathyroid hyperplasia can occur during normal pregnancy with increased levels of parathyroid hormone [10], in addition placenta can destabilize endogenous lipoproteins which promotes fat embolism [11].
Also, a mechanical factor has been implied for increasing the risk of hip avascular necrosis in pregnancy, as the left common iliac vein passes under the right common iliac artery, hence the vein will be more prone to compression during pregnancy especially at left and with excessive weight gain [7], [8], [12], [13]. In the literature the left hip was most commonly involved and mainly in the 3rd trimester or shortly postpartum [7], [8], [13], [14] which is in support of the mechanical theory, adversely in our case the right hip was only involved, this can be related to pregnancy with twins and their position within the uterus or the fact that the pathophysiology is multifactorial. In addition, hip osteonecrosis tends to occur in primigravida [7], [15], and in relatively elderly women [7], [8], [14], [15] as in our case.
Hip or pelvic pain during pregnancy is a common complaint with incidence rate of 38–56% [16], [17], most of these complaints are benign and the result of strain in the ligaments of the pelvis and the lumbar spine [18], hence the physical examination is important to differentiate between hip and pelvic pathologies and can be useful, but it can be also erroneous and misleading [19]. For the reasons mentioned above hip osteonecrosis can be misdiagnosed as simple sciatica or sacroiliac strain [8].
One of the more common hip pathologies in pregnancy is the transient osteoporosis of the hip (TOH) and can be confused with hip osteonecrosis [7], [15], [19], [20], [21]. TOH is a rare cause of acute hip pain in pregnancy and as hip osteonecrosis appears most commonly in the 3rd trimester or shortly in the post-partum period [19], characterized by sudden onset of hip pain that can be severe with no limitation of movement, TOH is a self-limiting condition that gradually resolve within 6–8 months and treatment consists only of non-weight bearing [7], [18], [21]. Unlike TOH, AVN has an insidious onset with progressive increase in the pain and limitation of movement and will eventually need early surgical intervention [19], [20], [21]. AVN and TOH are distinct entities [21], their clinical features may initially overlap [13], [19], [20], [21], and its crucial to differentiate between those 2 entities as their approach for treatment and their prognosis differs greatly [7], [13], [19], [21].
For radiologic evaluation, standard X-ray of the hip will show diffuse osteopenia in the head and neck in TOH [20], [21], but will show localized area of sclerosis or the classic “crescent sign” in the superolateral femoral head representing subchondral bone collapse in the weightbearing region [8], [21]. Standard X-ray lacks sensitivity for differentiating TOH from AVN as osteopenia in TOH is only evident 4–8 week s after the onset of symptoms [20], [21].
MRI is the gold standard for diagnosing AVN in its early stages with more than 99% sensitivity and specificity [22], In TOH MRI will show diffuse edema of the head and neck, in contrast AVN MRI will show diffuse edema with focal defects and subchondral changes [8], [19], [20], [21].
The most effective treatment of AVN in pregnancy is still controversial and depends on the different stages of presentation. Many surgical treatments have been described, from core decompression with and without bone grafting or bone marrow aspirate concentration injection in the early stages of the disease passing by intertrochanteric osteotomy, Sugioka's rotational osteotomy and non-vascularized or vascularized fibular graft in more advanced stages. Most of those surgical treatment acts to delay osteoarthritis of the hip, but the end result is most hip osteoarthritis with the necessity of total hip arthroplasty. We believe ceramic on ceramic replacement is associated with better osteolysis profile having higher rate of survivorship [23]. This property is particularly important for young population like the case we discussed.
4. Conclusion
Hip and pelvic pain during pregnancy are very frequent and may hide a serious event such as hip avascular necrosis which can lead to disastrous complications and aggressive treatment in a young age if not diagnosed early, so one should have high index of suspicion for TOH and AVN in a pregnant women with hip pain, hence have a low threshold for ordering an MRI for a pregnant women with hip pain.
Patient perspective
The patient was satisfied with the result, and the patient returned to his regular activity 1 year post-operatively.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Ethical approval
This type of study is exempt from ethical approval.
Guarantor
Charbel D Moussallem
CRediT authorship contribution statement
Writing the paper: Mark E Mouchantaf, Kinan F Freih, Mohamad K Moussa
Data collection: Ali H Asfour, Christine Yahchouchi
Supervision: Charbel D Moussallem
Declaration of competing interest
We have no conflicts of interest.
Contributor Information
Mark E. Mouchantaf, Email: marc.mchantaf@hotmail.com.
Christine Yahchouchi, Email: Ce18@aub.edu.lb.
References
- 1.Jones L.C., Hungerford D.S. Osteonecrosis: etiology, diagnosis, and treatment. Curr. Opin. Rheumatol. 2004;16(4):443–449. doi: 10.1097/01.moo.0000127829.34643.fd. [DOI] [PubMed] [Google Scholar]
- 2.Lafforgue P. Pathophysiology and natural history of avascular necrosis of bone. Joint Bone Spine. 2006;73(5):500–507. doi: 10.1016/j.jbspin.2006.01.025. [DOI] [PubMed] [Google Scholar]
- 3.Lespasio M.J., Sodhi N., Mont M.A. Osteonecrosis of the hip: a primer. Perm J. 2019;23:18–100. doi: 10.7812/TPP/18-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020:84. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Hasegawa Y., Iwase T., Iwasada S., Kitamura S., Iwata H. Osteonecrosis of the femoral head associated with pregnancy. Arch. Orthop. Trauma Surg. 1999;119(1–2):112–114. doi: 10.1007/s004020050370. [DOI] [PubMed] [Google Scholar]
- 6.El-Yahchouchi C., Moussa M.K., Khalaf Z. Simultaneous bilateral avascular necrosis of the femoral heads associated with cocaine use. Cureus. August 19, 2020;12(8) doi: 10.7759/cureus.9865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montella B.J., Nunley J.A., Urbaniak J.R. Osteonecrosis of the femoral head associated with pregnancy. A preliminary report. J. Bone Joint Surg. Am. 1999;81(6):790–798. doi: 10.2106/00004623-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Cheng N., Burssens A., Mulier J.C. Pregnancy and post-pregnancy avascular necrosis of the femoral head. Arch. Orthop. Trauma Surg. 1982;100(3):199–210. doi: 10.1007/BF00442735. [DOI] [PubMed] [Google Scholar]
- 9.Vandenbussche E., Madhar M., Nich C., Zribi W., Abdallah T., Augereau B. Bilateral osteonecrosis of the femoral head after pregnancy. Arch. Orthop. Trauma Surg. 2005;125(3):201–203. doi: 10.1007/s00402-004-0750-x. [DOI] [PubMed] [Google Scholar]
- 10.Schnatz P.F., Curry S.L. Primary hyperparathyroidism in pregnancy: evidence-based management. Obstet. Gynecol. Surv. 2002;57(6):365–376. doi: 10.1097/00006254-200206000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Myllynen P., Mäkelä A., Kontula K. Aseptic necrosis of the femoral head during pregnancy. Obstet. Gynecol. 1988;71(3 Pt 2):495–498. [PubMed] [Google Scholar]
- 12.Cockett F.B., Thomas M.L. The iliac compression syndrome. Br. J. Surg. 1965;52(10):816–821. doi: 10.1002/bjs.1800521028. [DOI] [PubMed] [Google Scholar]
- 13.Hernigou P., Jammal S., Pariat J., Flouzat-Lachaniette C.H., Dubory A. Hip osteonecrosis and pregnancy in healthy women. Int. Orthop. 2018;42(6):1203–1211. doi: 10.1007/s00264-017-3736-3. [DOI] [PubMed] [Google Scholar]
- 14.Lausten G.S. Osteonecrosis of the femoral head during pregnancy. Arch. Orthop. Trauma Surg. 1991;110(4):214–215. doi: 10.1007/BF00571064. [DOI] [PubMed] [Google Scholar]
- 15.Gribble R. Idiopathic osteonecrosis of the hip during pregnancy: outcome in a subsequent gestation. Obstet. Gynecol. 2001;98(5):911–913. doi: 10.1016/S0029-7844(01)01558-7. [DOI] [PubMed] [Google Scholar]
- 16.Röst C.C.M., Jacqueline J., Kaiser A., Verhagen A.P., Koes B.W. Pelvic pain during pregnancy: a descriptive study of signs and symptoms of 870 patients in primary care. Spine. 2004;29(22):2567–2572. doi: 10.1097/01.brs.0000145416.22782.9f. [DOI] [PubMed] [Google Scholar]
- 17.Vullo V.J., Richardson J.K., Hurvitz E.A. Hip, knee, and foot pain during pregnancy and the postpartum period. J. Fam. Pract. 1996;43(1):63–68. [PubMed] [Google Scholar]
- 18.Mens J.M., Vleeming A., Stoeckart R., Stam H.J., Snijders C.J. Understanding peripartum pelvic pain. Implications of a patient survey. Spine (Phila Pa 1976) 1996;21(11):1363–1370. doi: 10.1097/00007632-199606010-00017. [DOI] [PubMed] [Google Scholar]
- 19.Steib-Furno S., Luc M., Pham T. Pregnancy-related hip diseases: incidence and diagnoses [published correction appears in Joint Bone Spine. 2007 Oct;74(5):520. Mathieu, Luc [corrected to Luc, Mathieu]] Joint Bone Spine. 2007;74(4):373–378. doi: 10.1016/j.jbspin.2006.12.0011. [DOI] [PubMed] [Google Scholar]
- 20.Guerra J.J., Steinberg M.E. Distinguishing transient osteoporosis from avascular necrosis of the hip. J. Bone Jt. Surg. 1995;77(4):616–624. doi: 10.2106/00004623-199504000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Balakrishnan A., Schemitsch E.H., Pearce D., McKee M.D. Distinguishing transient osteoporosis of the hip from avascular necrosis. Can. J. Surg. 2003;46(3):187–192. (6) [PMC free article] [PubMed] [Google Scholar]
- 22.Pierce T.P., Jauregui J.J., Cherian J.J., Elmallah R.K., Mont M.A. Imaging evaluation of patients with osteonecrosis of the femoral head. Curr. Rev. Musculoskelet. Med. 2015;8(3):221–227. doi: 10.1007/s12178-015-9279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang T., Sun J.Y., Zhao X.J., Liu Y., Yin H.B. Ceramic-on-ceramic bearings total hip arthroplasty in young patients. Arthroplast. Today. 2016;2(4):205–209. doi: 10.1016/j.artd.2016.04.004. (Published 2016 Aug 25) [DOI] [PMC free article] [PubMed] [Google Scholar]



