Abstract
Introduction
It remains controversial whether the direct anterior approach (DAA) or the posterior approach (PA) allows better restoration of hip biomechanics after total hip arthroplasty (THA). Besides, it is not certain which approach is best for a novice surgeon to avoid implant malposition, neither during the learning curve nor once the curve plateau has been reached.
Methods
We performed a retrospective cohort study of THAs operated on between 2014 and 2019 by a single novice surgeon (DAA, n = 187; PA, n = 184). The surgeon used both approaches, and thus went through parallel learning curves.
Results
While the DAA presented a greater number of acetabular cup implantations within Lewinnek's “safe zone” for inclination (84.5% vs. 79.3%; p = 0.003), the PA returned superior results for anteversion (77.7% vs. 68.4%; p = 0.000). The PA showed a tendency to verticalize acetabular cups, while the DAA tended to antevert them. The DAA resulted in fewer patients with leg length discrepancy (3.2% vs. 8.2%, p = 0.041). No differences were found in stem coronal alignment or femoral offset.
Conclusion
Both approaches are safe and reliable for restoring hip biomechanics through THA surgery during the learning curve of a novice hip surgeon. Similar radiological outcomes are also seen once the surgeon has reached the learning curve plateau.
Keywords: Total hip arthroplasty, Direct anterior approach, Posterior approach, Implant position, Learning curve, Hip biomechanics
1. Introduction
The primary goal in total hip arthroplasty (THA) is full restoration of original hip biomechanics.1,2 Correct implant positioning, orientation and alignment which reproduces native anatomy is linked to functional recovery, joint stability, low complication rate, and implant longevity.3, 4, 5, 6, 7, 8
The posterior approach (PA) is broadly used because of its history of yielding favorable results, its extensive surgical exposure, and the short learning curve for its performance.9,10 Nevertheless, it produces less favorable early function and pain outcomes than the DAA, and is associated with a higher dislocation rate.11, 12, 13, 14
In contrast, the direct anterior approach (DAA) is less popular, largely because of its narrow surgical exposure and its lengthy learning curve.10,12 Nevertheless, it is increasing in popularity among both surgeons and patients because it seems to offer superior early functional and pain outcomes, due to its muscle-sparing nature.9,11,15 Its dislocation rate is also favorable.12, 13, 14
It remains controversial whether the DAA or the PA results in better restoration of a patient's original hip biomechanics. Some authors assert that DAA better restores hip biomechanics11,13,16,17; others insist the PA is superior in this regard.18, 19, 20 Some studies have found no significant difference in outcomes between the two approaches.21,22 Concern also exists regarding reports of greater incidence of acetabular anteversion in DAA cases.16,23
To the best of our knowledge, no previous article has focused on comparing THA restoration of hip biomechanics between the DAA and the PA, in the hands of a novice hip surgeon. Thus, it is not known which approach should be recommended for novice surgeons to avoid implant malposition, neither during the learning curve nor once the curve plateau has been reached.
2. Material and methods
2.1. Study design
After institutional review board approval, we performed a retrospective cohort study. Using our prospective institutional database, we identified all patients who had undergone THA between January 2014 and December 2019 in our level-one healthcare center. All participants provided informed consent. Only patients operated upon by a specific surgeon (B. V.) were selected for the study. This surgeon began his practice in THA in 2014, in our hospital's hip unit. He used both the DAA and the PA indistinctly. As a novice surgeon, he acquired experience with both approaches simultaneously, and thus went through parallel learning curves. This circumstance afforded us the opportunity to investigate for differences in implant positioning between a novice's DAA and PA surgeries, throughout the course of his learning curve for each technique.
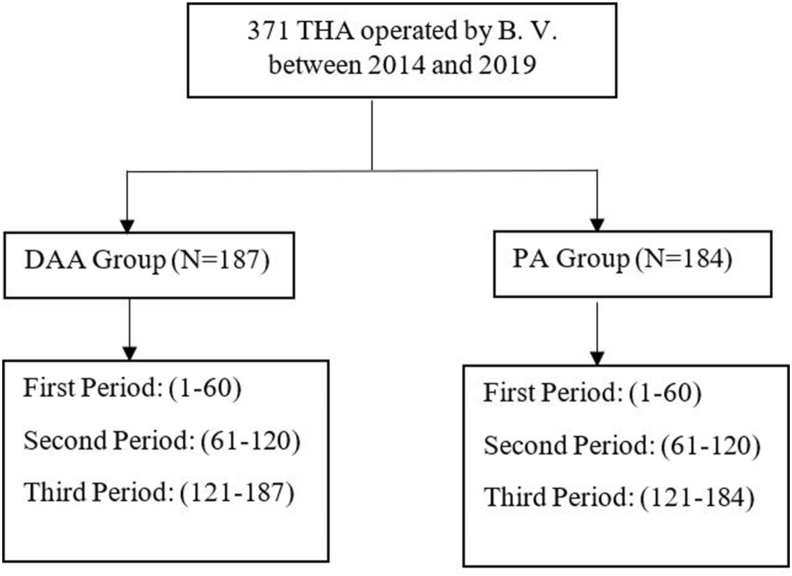
Patients were divided into two cohorts according to the approach used in THA: DAA or PA. Patients in each cohort were also classified into three consecutive chronological periods (Fig. 1). The third and final period began at the point where we considered the surgeon to have reached the learning curve plateau for a given approach: following completion of 120 cases using that approach.24,25
Fig. 1.
Patient flow diagram.
To determine whether outcome differences observed over the course of the surgeon's learning curve continued once he had reached the learning curve plateau for each approach, patient subgroups treated during the final period were compared separately.
2.2. Studied parameters
Data regarding demographics, surgical parameters and radiological outcomes were collected preoperatively, intraoperatively and during follow-up, using digital medical records.
Radiographic measurements were performed using the preoperative anteroposterior radiograph of the pelvis, and also the last strict anteroposterior radiograph available during follow-up. The digital templating program TraumaCad® version 2.0 (BrainLab, Feldkirchen, Germany) was used for the analysis. Radiological parameters were measured by three orthopedic surgeons.
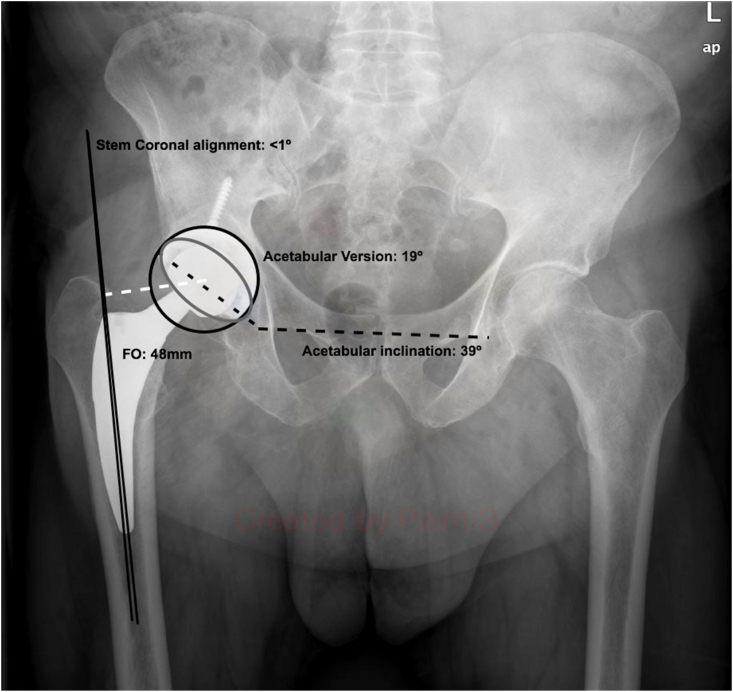
Radiological outcomes analyzed were acetabular cup inclination and anteversion, stem coronal alignment, femoral offset (FO) and lower limb discrepancy (LLD) (Fig. 2). We considered an implant to have been correctly implanted (restoring hip biomechanics) if the acetabular cup was implanted within Lewinnek's safe zone (inclination 40° ± 10°, anteversion 15° ± 10°),3,4 and with stem coronal alignment neutral (0°±3°).5,16,20,26 We also evaluated FO restoration compared to the contralateral hip (accepting ±5 mm as correctly implanted),6, 7, 8 and LLD (±10 mm).2
Fig. 2.
Postoperative radiographic evaluation. Stem coronal alignment is the angle formed by the solid black lines (<1°). Femoral offset (FO) measurement is denoted by the dashed white line (48 mm). Acetabular inclination corresponds to the angle formed by dashed black lines (39°). Acetabular version is measured through the grey ellipse (19°).
2.3. Statistical analysis
Demographic factors and clinical characteristics were summarized as counts and percentages for categorical variables. Means were calculated for continuous variables. Normality was tested using the Kolmogorov-Smirnov test. Groups were compared using the χ2 test or Fisher's exact test for categorical variables, depending on normality. Continuous variables were evaluated with the student's T test. A binary logistic regression analysis was conducted to look for a possible association between variables. All p values were two-tailed. A p-value < 0.05 was considered statistically significant. Statistical analysis was performed using SPSS® v.27.0 software (IBM, Armonk, NY, USA).
2.4. Surgical technique
The DAA was performed using the distal part of the Smith Petersen approach, through the intermuscular plane between the sartorius and the tensor fascia latae, in supine position and without traction table. The ilioinguinal ligament, iliopubic ligament and superior capsule were released in order to mobilize the femur. The transverse acetabular ligament was used as a guide for version. Femoral stem implantation was prepared with the hyperextended, adducted and externally rotated hip under the contralateral leg (“four-leg position”).
The PA was performed in the lateral position, requiring division of hip external rotators and posterior capsule. The transverse acetabular ligament was also used as a guide for version. The posterior capsule and external rotator muscles were sutured back together using a transosseus technique.
In both approaches the cup was implanted aiming for a 40° inclination angle and 15° anteversion angle, a 15° femoral anteversion angle and neutral coronal alignment. Acetabular cups were not cemented. The most frequently used implants were U-Motion II® (United Orthopedic Corporation, Taipei, Taiwan) and Delta® (Lima Corporate, San Daniele, Italy). 75.1% of the stems in this study were not cemented. The most frequently used implants were the UTF® (United Orthopedic Corporation, Taipei, Taiwan), Fitmore® (Zimmer Biomet, Warsaw, USA), and H-Max® (Lima Corporate, San Daniele, Italy).
After surgery, patients followed our post-operative rehabilitation protocol. Full, unrestricted weight bearing was allowed as tolerated. Patients were either discharged home or transferred to a rehabilitation ward, based on their functionality and home support.
3. Results
The DAA and PA approaches were used to implant a THA in 187 and 184 patients, respectively. In the DAA group 63/187 (33.7%) were women; mean patient age was 64.3 ± 0.9 years. In the PA group 107/184 (58.2%) were women; mean patient age was 65.9 ± 1.1 years. Patient demographic characteristics are shown in Table 1. Mean follow-up was 36.6 months in the DAA group and 42.5 months in the PA group.
Table 1.
Baseline characteristics of patients.
| Demographic variable | DAA Group | PA Group |
|---|---|---|
| Number of patients | 187 | 184 |
| Primary osteoarthritis as indication criteria (nº (%)) | 164 (87.7%) | 148 (80.4%) |
| Modified Harris Hip Score (mean ± standard deviation) | 45.1 ± 1.0 | 42.2 ± 1.2 |
| Age (years) (mean ± standard deviation) |
64.3 ± 0.9 | 65.9 ± 1.1 |
| Gender (Female:Male) | 63:124 (34%:66%) | 107:77 (58%:42%) |
| Laterality (Left:Right) | 88:99 (47.1%:52.9%) | 83:101 (45.1%:54.9%) |
| ASA Score (I:II:III:IV) | 12:115:58:2 (6.4%:61.5%:31%:1.1%) | 13:103:67:1 (7.1%:56%:36.4%:0.5%) |
| Body Mass Index (mean ± standard deviation) | 26.4 ± 0.3 | 30.4 ± 0.4 |
| Diabetes (nº (%)) | 20 (10.7%) | 38 (20.7%) |
| Smoking (nº (%)) | 44 (23.5%) | 33 (17.9%) |
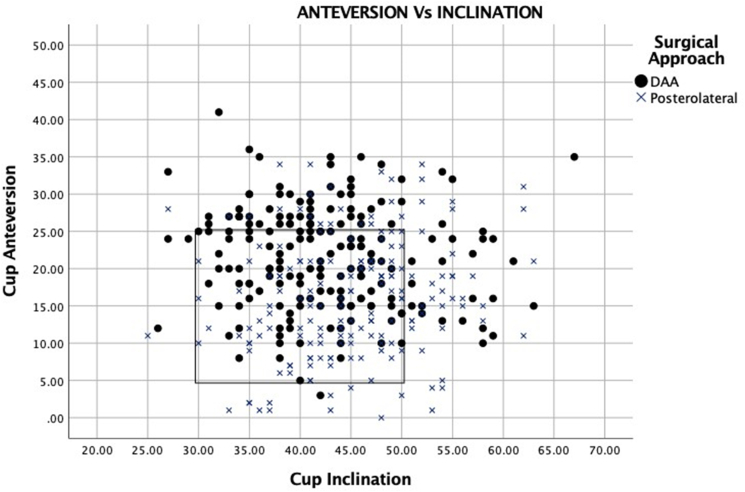
In studying postoperative radiological outcomes, we found acetabular cup inclination and anteversion showed statistically significant differences between groups (Fig. 3). While the DAA was associated with more acetabular cups implanted within Lewinnek's safe zone for inclination (84.5% vs.79.3%; p = 0.003), the PA produced better results with regard to the anteversion safe zone (77.7% vs.68.4%; p = 0.000). The PA showed a tendency to verticalize the acetabular cups (19.6% vs.13.5%), and the DAA to antevert them (31% vs.14.7%). Statistically significant differences in LLD were also found. Finally, the DAA resulted in fewer patients with LLD greater than 10 mm (3.2% vs.8.2%, p = 0.041).
Fig. 3.
Scatterplot depicting version and inclination of the acetabular cups in THA through the DAA and PA. The black rectangle delimits the outcomes inside Lewinnek's safe zone.
No statistically significant differences were seen between groups in terms of stem coronal alignment and FO. Neutral stem coronal alignment was found in 78.1% of implants in the DAA group, 80.4% in the PA group (p = 0.761). With regard to FO differences, in 52.4% of the DAA cases, the difference in offset between the operated and contralateral legs was ± 0 to 5 mm; in 26.7%, the difference was ± 6 to 10 mm. In PA cases, the percentages were 49.5% and 25.0%, respectively (p = 0.564).
Postoperative radiological outcomes are shown in Table 2. The radiological outcomes of both patient subgroups operated on during the final study period (67 DAA-THA and 64 PA-THA) are shown in Table 3. When comparing outcomes between the main groups and between the final period's groups, results were quite similar. Although in some cases statistical significance was lost (probably caused by the reduction of statistical power), distribution of results and tendency of the comparisons were similar. This suggests that the differences between approaches observed during the learning curve periods were maintained once the learning curve plateau was reached.
Table 2.
Postoperative radiological outcomes.
| Postoperative radiological outcomes | DAA Group (nº (%)) | PA Group (nº (%)) | P-value | |
|---|---|---|---|---|
| Acetabular cup inclination | ||||
| Safe (40° ± 10°) | 158 (84.5%) | 146 (79.3%) | 0.003* | |
| Horizontal (<30°) | 4 (2.1%) | 2 (1.1%) | ||
| Vertical (>50°) | 25 (13.4%) | 36 (19.6%) | ||
| Acetabular cup version | ||||
| Safe (15° ± 10°) | 128 (68.4%) | 143 (77.7%) | 0.000* | |
| Antevert (>25°) | 58 (31%) | 27 (14.7%) | ||
| Retrovert (<5°) | 1 (0.5%) | 14 (7.6%) | ||
| LLD | ||||
| <5 mm | 130 (69.5%) | 109 (59.2%) | 0.041* | |
| 5–10 mm | 51 (27.3%) | 60 (32.6%) | ||
| >10 mm | 6 (3,2%) | 15 (8,2%) | ||
| Stem coronal alignment | ||||
| Neutral (0°±3°) | 146 (78.1%) | 148 (80.4%) | 0.761 | |
| Valgus | 16 (8.6%) | 16 (8.7%) | ||
| Varus | 25 (13.4%) | 20 (10.9%) | ||
| Femoral offset discrepancy | ||||
| <5 mm | 98 (52.4%) | 91 (49.5%) | 0.564 | |
| 5–10 mm | 50 (26.7%) | 46 (25.0%) | ||
| >10 mm | 39 (20.9%) | 47 (25.5%) | ||
*: A p-value < 0.05 was considered statistically significant.
Table 3.
Postoperative radiological outcomes of both patient subgroups operated on during the last period.
| Postoperative radiological outcomes | DAA Group (n = 64) (last period) (nº (%)) |
PA Group (n = 60) (last period) (nº (%)) |
P value | |
|---|---|---|---|---|
| Acetabular cup inclination | ||||
| Safe (40° ± 10°) | 61 (95.3%) | 50 (83.3%) | 0.066 | |
| Horizontal (<30°) | 1 (1.6%) | 12 (1.7%) | ||
| Vertical (>50°) | 2 (3.1%) | 9 (15.0%) | ||
| Acetabular cup version | ||||
| Safe (15° ± 10°) | 35 (54.7%) | 43 (71.7%) | 0.002* | |
| Antevert (>25°) | 29 (45.3%) | 12 (20.0%) | ||
| Retrovert (<5°) | 0 (0.0%) | 5 (8.3%) | ||
| LLD | ||||
| <5 mm | 43 (67.2%) | 30 (50.0%) | 0.117 | |
| 5–10 mm | 19 (29.7%) | 25 (41.7%) | ||
| >10 mm | 2 (3.1%) | 5 (8.3%) | ||
| Stem coronal alignment | ||||
| Neutral (0°±3°) | 53 (82.8%) | 45 (75.0%) | 0.564 | |
| Valgus | 6 (9.4%) | 8 (13.3%) | ||
| Varus | 5 (7.8%) | 7 (11.7%) | ||
| Femoral offset discrepancy | ||||
| <5 mm | 32 (50.0%) | 31 (51.7%) | 0.783 | |
| 5–10 mm | 16 (25.0%) | 17 (28.3%) | ||
| >10 mm | 16 (25.0%) | 12 (20.0%) | ||
*: A p value < 0.05 was considered statistically significant.
4. Discussion
The results of our study support the idea that both approaches (DAA and PA) are safe and reliable in restoring hip biomechanics after THA surgery during the learning curve of a novice hip surgeon. They present similar postoperative radiological outcomes, though some peculiarities of each approach should be highlighted. While no differences were found in stem coronal alignment and FO, statistically significant differences were observed in acetabular cup inclination and version, and in LLD. The PA showed a tendency to verticalize acetabular cups, and the DAA to antevert them. Further, there were fewer patients with LLD higher than 10 mm following DAA.
4.1. Acetabular version
In our study, the PA was associated with more acetabular cups showing version within the Lewinnek safe zone (77.7% vs. 68.4%; p = 0.000). The DAA showed a tendency to antevert them (31% vs. 14.7%) (Fig. 3).
This propensity has previously been reported in the literature.27,28 Chen et al.23 reported that 10% of DAA hips were placed outside the safe zone for anteversion, and recommended being mindful of this tendency and adjust implant positioning accordingly when using this approach. Kobayashi et al.16 maintained that cups could be positioned with an anteversion angle greater than their target angle, by as much as 69.3%. Interference of the impactor with the femur forces the surgeon to raise his hands, placing the cup in anteversion.16 Consequently, sufficient soft tissue release, appropriate neck osteotomy level, use of a curved offset impactor and lowering the hands with the impactor are recommended. Use of anatomic landmarks such as the transverse acetabular ligament should not be forgotten. Furthermore, some studies15,16,29 have maintained that the target anteversion angle is often excessive, considering the risk of anterior instability in the DAA—so target anteversion should be intentionally decreased.
On the other hand, some articles report similar version outcomes with both approaches,13,21 or even lower acetabular anteversion with the DAA.11,22
4.2. Acetabular inclination
Although both approaches showed good results with regard to acetabular cup inclination, the DAA demonstrated superiority (84.5% vs.79.3%; p = 0.003). The PA showed a tendency to verticalize acetabular cups (19.6% vs.13.5%) (Fig. 3).
Acetabular inclination outcomes are mixed in published articles. Similar to our study, Kobayashi et al.16 found the PA associated with higher acetabular cup inclination. They reported that use of the lateral decubitus position during the PA allows the patient to shift in the coronal and axial planes, so acetabular orientation is changeable during implant insertion. In contrast, the supine position of the DAA offers more patient stability on the operating table, permitting easier manipulation of the acetabulum and leading to higher accuracy. Other studies have also maintained that the DAA improves acetabular inclination.30 While interference of the impactor with the femur forces a higher anteversion through the DAA, when using the PA this interference could partially explain increased inclination.
Some authors have reported no significant difference in acetabular inclination between the two approaches,9,13,21 while others have reported even worse outcomes with the DAA.19
4.3. Limb length discrepancy (LLD)
The DAA produced significantly fewer patients with LLD higher than 10 mm as compared to the PA (3.2% vs. 8.2%, p = 0.041).
Most of the articles we reviewed which compared LLD in the DAA vs. the PA reported no significant differences between the two.11,22 Other non-comparative studies reported favorable LLD results with the DAA.4,31 Hartford et al.24 reported that 97% of their DAA-THAs were within 10 mm of LLD.
Chen et al. and Lee et al. also reported superior LLD results with the DAA as compared to the PA.17,32 They attributed these results to the supine position. Nevertheless, neither the cut-off between acceptable and unacceptable LLD nor its clinical repercussions have been clearly determined.2
4.4. Stem coronal alignment
No statistically significant differences in stem coronal alignment were seen between our two groups. Neutral stem coronal alignment was found in 78.1% of implants in the DAA group, with 80.4% in the PA group (p = 0.761).
Similar outcomes in stem coronal alignment between the DAA and PA had previously been reported.16,19,20,22 Abe et al.20 specifically studied the difference in stem alignment between the two approaches; they concluded there was no difference in the incidence of varus or valgus implantation of more than 3°.
Other studies have reported that stems in DAA cases were significantly more likely to be placed in a neutral position.11 However, Haversath et al.33 maintained that the DAA provokes varus stem malalignment (9.7% of THAs in their study presented a varus deviation greater than 3°). They reported previous coxa vara with a long neck, and initial stages of the surgeon's learning curve as risk factors for varus positioning.
4.5. Femoral offset (FO)
FO values in our study indicated no significant difference between the two approaches. In 52.4% of the DAA cases, the FO difference between the operated and contralateral legs was ± 0 to 5 mm; in 26.7%, the difference was ± 6 to 10 mm. In PA cases, these percentages were 49.5% and 25.0%, respectively (p = 0.564).
There is a scarcity of literature comparing the DAA and PA in terms of ability to restore FO, which increases our article's value. Trevisan et al.26 reported an average FO reduction of −0.5 mm after DAA-THA, without significant contribution to the HHS. Hasegawa et al.31 also demonstrated good results in FO restoration with the DAA (3.5 ± 2.6 mm).
4.6. Restoring hip biomechanics during the learning curve
The DAA is associated with a steep learning curve, leading to long operative times, blood loss, and high rate of intraoperative complications.10, 11, 12,21 However, little information has been published regarding component positioning during the DAA learning curve. Foissey et al.34 reported 80% of cups implanted within the combined safe zones during their first 537 DAA-THAs. The authors warned that surgeons must beware of excess abduction early in their experience with the procedure, but they did not report having observed surgeons’ progressive learning curves in terms of other radiological parameters. Other articles have reported no difference in cup positioning or LLD as a surgeon advanced along the learning curve.25,35 On the other hand, Brun et al.36 observed a steady improvement in cup positioning until, somewhere between 200 and 300 patients, the surgeon reached a steady state.
However, to the best of our knowledge, no previous article has focused on comparing the ability to restore hip biomechanics between the DAA and PA, along a novice hip surgeon's learning curves. In our study, both approaches presented similar postoperative radiological outcomes.
Additionally, results with regard to acetabular version and inclination, LLD, stem coronal alignment and FO showed both approaches to be safe, avoiding component malpositioning.
4.7. Limitations
There are some limitations to the current study, including those inherent in any retrospective study without a randomized control group. Radiological parameters were not measured by an expert and independent radiologist, but rather by three orthopedic surgeons. Further, all radiologic morphology parameters were measured using an anteroposterior x-ray projection.
5. Conclusions
Both the DAA and the PA are safe and reliable in restoring hip biomechanics in THA surgery, during a novice hip surgeon's progress through the procedures' learning curves. The approaches yield similar postoperative radiological outcomes. Similar results also continue once the surgeon reaches the learning curve plateau. The PA showed a tendency to verticalize the cups, while the DAA tended to antevert them. The DAA offered better control of LLD. No significant differences were found in stem coronal alignment or FO.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or non-profit sectors.
Author's contributions
All authors contributed equally to this work. All authors contributed to the study conception and design, material preparation, data collection and analysis. The first draft of the manuscript was written by Oriol Pujol and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics approval
The study was approved by our Center's Ethics Committee (CEIC). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publication
Patients were informed that data concerning their cases might be submitted for publication, and they gave their consent.
Declaration of competing interest
None.
Acknowledgements
We thank Russell Williams of RoundlyWorded.com for his editorial recommendations.
This work has been done in the framework of the doctorate in Surgery of the Universitat Autònoma de Barcelona.
References
- 1.Colombi A., Schena D., Castelli C.C. Total hip arthroplasty planning. EFORT Open Rev. 2019;4:626–632. doi: 10.1302/2058-5241.4.180075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flecher X., Ollivier M., Argenson J.N. Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res OTSR. 2016;102:S9–S20. doi: 10.1016/j.otsr.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 4.Debi R., Slamowicz E., Cohen O. Acetabular cup orientation and postoperative leg length discrepancy in patients undergoing elective total hip arthroplasty via a direct anterior and anterolateral approaches. BMC Muscoskel Disord. 2018;19:188. doi: 10.1186/s12891-018-2097-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shishido T., Tateiwa T., Takahashi Y., Masaoka T., Ishida T., Yamamoto K. Effect of stem alignment on long-term outcomes of total hip arthroplasty with cementless Bi-Metric femoral components. J Orthop. 2018;15:134–137. doi: 10.1016/j.jor.2018.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Renkawitz T., Weber T., Dullien S. Leg length and offset differences above 5mm after total hip arthroplasty are associated with altered gait kinematics. Gait Posture. 2016;49:196–201. doi: 10.1016/j.gaitpost.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Mahmood S.S., Mukka S.S., Crnalic S., Wretenberg P., Sayed-Noor A.S. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta Orthop. 2016;87:36–41. doi: 10.3109/17453674.2015.1091955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cassidy K.A., Noticewala M.S., Macaulay W., Lee J.H., Geller J.A. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty. 2012;27:1863–1869. doi: 10.1016/j.arth.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Wang Z., Hou J.-Z., Wu C.-H. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg. 2018;13:229. doi: 10.1186/s13018-018-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng T.E., Wallis J.A., Taylor N.F. A prospective randomized clinical trial in total hip arthroplasty-comparing early results between the direct anterior approach and the posterior approach. J Arthroplasty. 2017;32:883–890. doi: 10.1016/j.arth.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 11.Barrett W.P., Turner S.E., Leopold J.P. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013;28:1634–1638. doi: 10.1016/j.arth.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 12.Bhandari Mohit, Matta Joel M., Dave Dodgin. Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin N Am. 2009;40:329–342. doi: 10.1016/j.ocl.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Yang X.-T., Huang H.-F., Sun L., Yang Z., Deng C.-Y., Tian X.-B. Direct anterior approach versus posterolateral approach in total hip arthroplasty: a systematic review and meta-analysis of randomized controlled studies. Orthop Surg. 2020;12(4):1065–1073. doi: 10.1111/os.12669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meermans G., Konan S., Das R., Volpin A., Haddad F.S. The direct anterior approach in total hip arthroplasty: a systematic review of the literature. Bone Jt J. 2017;99-B:732. doi: 10.1302/0301-620X.99B6.38053. 40. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez J.A., Deshmukh A.J., Rathod P.A. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res. 2014;472:455–463. doi: 10.1007/s11999-013-3231-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kobayashi H., Homma Y., Baba T. Surgeons changing the approach for total hip arthroplasty from posterior to direct anterior with fluoroscopy should consider potential excessive cup anteversion and flexion implantation of the stem in their early experience. Int Orthop. 2016;40:1813–1819. doi: 10.1007/s00264-015-3059-1. [DOI] [PubMed] [Google Scholar]
- 17.Lee S.H., Kang S.W., Jo S. Perioperative comparison of hip arthroplasty using the direct anterior approach with the posterolateral approach. Hip Pelvis. 2017;29:240–246. doi: 10.5371/hp.2017.29.4.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benson J.R., Govindarajan M., Muir J.M., Lamb I.R., Sculco P.K. Surgical approach and reaming depth influence the direction and magnitude of acetabular center of rotation changes during total hip arthroplasty. Arthroplasty Today. 2020;6:414–421. doi: 10.1016/j.artd.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Migliorini F., Eschweiler J., Trivellas A. Implant positioning among the surgical approaches for total hip arthroplasty: a Bayesian network meta-analysis. Arch Orthop Trauma Surg. 2020;140:1115–1124. doi: 10.1007/s00402-020-03448-w. [DOI] [PubMed] [Google Scholar]
- 20.Abe H., Sakai T., Takao M., Nishii T., Nakamura N., Sugano N. Difference in stem alignment between the direct anterior approach and the posterolateral approach in total hip arthroplasty. J Arthroplasty. 2015;30:1761–1766. doi: 10.1016/j.arth.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 21.Peng L., Zeng Y., Wu Y., Zeng J., Liu Y., Shen B. Clinical, functional and radiographic outcomes of primary total hip arthroplasty between direct anterior approach and posterior approach: a systematic review and meta-analysis. BMC Muscoskel Disord. 2020;21:338. doi: 10.1186/s12891-020-03318-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jia F., Guo B., Xu F., Hou Y., Tang X., Huang L. A comparison of clinical, radiographic and surgical outcomes of total hip arthroplasty between direct anterior and posterior approaches: a systematic review and meta-analysis. Hip Int J Clin Exp Res Hip Pathol Ther. 2019;29:584–596. doi: 10.1177/1120700018820652. [DOI] [PubMed] [Google Scholar]
- 23.Chen A.F., Chen C.-L., Low S. Higher acetabular anteversion in direct anterior total hip arthroplasty: a retrospective case-control study. HSS J Musculoskelet J Hosp Spec Surg. 2016;12:240–244. doi: 10.1007/s11420-016-9488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hartford J.M., Bellino M.J. The learning curve for the direct anterior approach for total hip arthroplasty: a single surgeon's first 500 cases. HIP Int. 2017;27:483–488. doi: 10.5301/hipint.5000488. [DOI] [PubMed] [Google Scholar]
- 25.Foissey C., Fauvernier M., Fary C., Servien E., Lustig S., Batailler C. Total hip arthroplasty performed by direct anterior approach - does experience influence the learning curve? SICOT-J. 2020;6:15. doi: 10.1051/sicotj/2020015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trevisan C., Klumpp R., Piscitello S., Compagnoni R., Grattieri R., Cazzaniga C. Biomechanical reconstruction parameters obtained after direct anterior approach total hip arthroplasty do not compromise clinical outcome. Eur J Orthop Surg Traumatol Orthop Traumatol. 2020;30:1463–1470. doi: 10.1007/s00590-020-02727-x. [DOI] [PubMed] [Google Scholar]
- 27.Watanabe K., Mitsui K., Usuda Y., Nemoto K. An increase in the risk of excessive femoral anteversion for relatively younger age and types of femoral morphology in total hip arthroplasty with direct anterior approach. J Orthop Surg Hong Kong. 2019;27:1–6. doi: 10.1177/2309499019836816. [DOI] [PubMed] [Google Scholar]
- 28.Barton C., Kim P.R. Complications of the direct anterior approach for total hip arthroplasty. Orthop Clin N Am. 2009;40:371–375. doi: 10.1016/j.ocl.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Murphy W.S., Yun H.H., Hayden B., Kowal J.H., Murphy S.B. The safe zone range for cup anteversion is narrower than for inclination in THA. Clin Orthop. 2018;476:325–335. doi: 10.1007/s11999.0000000000000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rathod P.A., Bhalla S., Deshmukh A.J., Rodriguez J.A. Does fluoroscopy with anterior hip arthoplasty decrease acetabular cup variability compared with a nonguided posterior approach? Clin Orthop Relat Res. 2014;472:1877–1885. doi: 10.1007/s11999-014-3512-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hasegawa I., Wright A.R., Andrews S.N., Unebasami E., Nakasone C.K. Hip offset and leg length equalization in direct anterior approach total hip arthroplasty without preoperative templating. Hawaii J Health Soc Welf. 2019;78:26–28. [PMC free article] [PubMed] [Google Scholar]
- 32.Chen W., Sun J.-N., Zhang Y., Zhang Y., Chen X.-Y., Feng S. Direct anterior versus posterolateral approaches for clinical outcomes after total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg. 2020;15:231. doi: 10.1186/s13018-020-01747-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haversath M., Lichetzki M., Serong S. The direct anterior approach provokes varus stem alignment when using a collarless straight tapered stem. Arch Orthop Trauma Surg. 2020 doi: 10.1007/s00402-020-03457-9. [DOI] [PubMed] [Google Scholar]
- 34.Foissey C., Batailler C., Fary C., Luceri F., Servien E., Lustig S. Transitioning the total hip arthroplasty technique from posterior approach in lateral position to direct anterior approach in supine position—risk factors for acetabular malpositioning and the learning curve. Int Orthop. 2020;44:1669–1676. doi: 10.1007/s00264-020-04583-0. [DOI] [PubMed] [Google Scholar]
- 35.Goytia R.N., Jones L.C., Hungerford M.W. Learning curve for the anterior approach total hip arthroplasty. J Surg Orthop Adv. 2012;21:78–83. doi: 10.3113/JSOA.2012.0078. [DOI] [PubMed] [Google Scholar]
- 36.Brun O.-C.L., Månsson L., Nordsletten L. The direct anterior minimal invasive approach in total hip replacement: a prospective departmental study on the learning curve. Hip Int J Clin Exp Res Hip Pathol Ther. 2018;28:156–160. doi: 10.5301/hipint.5000542. [DOI] [PubMed] [Google Scholar]