Abstract
Background
Community health workers (CHWs) are central to India's strategy for reaching the Sustainable Development Goals around maternal and child health. Despite India's significant investment in these programs, few studies have analyzed the effect of CHWs across India.
Objective
This study aims to analyze multiple types of CHWs and their impact on a broad range of antenatal and infant health outcomes across India.
Methods
In this population-based cross-sectional study, we analyzed data of women interviewed by the most recent 2015–2016 National Family Health Survey-4 (NFHS-4) in India. This study performed multiple variable regressions to examine the effect of receiving ANC during pregnancy from 1) any CHW and 2) by specific type of CHW - Accredited Social Health Activist (ASHA), Anganwadi Worker (AWW), and Community/Village Health Worker (defined in Table 1) on antenatal and infant health outcomes.
Results
Of 166,498 women, 14.2% received ANC from any CHW with specifically 5.9% receiving from ASHAs, 10.2% receiving from AWWs, and 0.5% receiving from Community/Village Health Workers. Women who received ANC from an ASHA had increased ANC utilization (OR 1.77; 95% CI 1.65, 1.91) as well as quality (IRR 1.06; 95% CI 1.05, 1.08), increased early initiation of breast feeding (OR 1.20; 95% CI 1.12, 1.29), and decreased one-year mortality (OR 0.75; 95% CI 0.63, 0.88). Women who received ANC from an AWW had increased ANC utilization (OR 2.24; 95% CI 2.12, 2.37) as well as quality (IRR 1.07, 95% CI 1.06, 1.08) and increased early initiation of breast feeding (OR 1.30; 95% CI 1.26, 1.40).
Conclusion
Receiving ANC from ASHAs and AWWs is associated with improved ANC utilization, ANC quality, early initiation of breastfeeding and the key outcome of reduced infant mortality.
Keywords: Global health, Community health workers, Prenatal care, Infant mortality, India
Highlights
-
•
14% of women received antenatal care from any community health worker.
-
•
ASHAs improve antenatal care utilization and quality, early initiation of breastfeeding, and infant mortality.
-
•
Anganwadi workers improve antenatal care utilization and quality as well as early initiation of breastfeeding.
1. Introduction
India accounts for a fifth of maternal deaths and a quarter of child deaths globally (UNICEF, 2007; UNICEF, 2009). Antenatal care (ANC) can help address this burden, as it has been associated with decreased maternal and neonatal mortality (Bauserman et al., 2015; Roy & Haque, 2018). According to India's Ministry of Health and Family Welfare, routine ANC in India includes at least 4 ANC visits, Tetanus Toxoid injections and Iron-Folic Acid supplementation, as well as measurements of blood hemoglobin, urine sugar and protein, blood pressure, and weight (Maternal Health Division - Ministry of Health and Family Welfare - Government of India, 2010). However, as of 2014, only 51% of Indian women had four or more ANC visits during their pregnancy (Antenatal Care.Gl).
India spends 3.7% of GDP on health, which is much lower than the global average of 10.0%. (The World Bank) Furthermore, 65% of Indian expenditures come out-of-pocket, which can financially cripple lower-income individuals (World Bank, 2016). Consequently, health outcomes vary widely by caste, education, wealth (Balarajan et al., 2011). Public expenditure is crucial for alleviating such health inequity.
Thus, over the past several decades, India has deployed community health workers (CHWs), namely the Accredited Social Health Activists (ASHA) and Anganwadi Worker (AWW) programs, to improve healthcare access. Table A.1 describes the roles and details of ASHAs and AWWs. In India, CHWs have shown the ability to acquire skills for conditions ranging from cardiovascular disease prevention to mental health (Armstrong et al., 2011; Khetan et al., 2018). ASHAs, India's frontline cadre of CHWs, have demonstrated mixed effects on maternal and child health across studies. An ecological analysis found that an increase in ASHAs had no effect on institutional deliveries or having a skilled attendant at birth (Wagner et al., 2018). On the other hand, a modelling study using the India Human Development Surveys (HDS) observed that receiving ASHA's services was associated with increased ANC visits, skilled birth attendance, and facility birth (Agarwal et al., 2019). Given the scale of investment into 857,000 ASHAs, 1.2 million AWWs, and countless local CHW programs across India, it is crucial to gain clear evidence as to their effectiveness (Perry et al., 2013). Data from the National Family Health Survey-4 (NFHS-4) is well-suited for this rigorous evaluation due to its widespread administration and robust questionnaires (Woman's Questionnaire, 2015).
This study aims to clarify and build upon prior research by investigating the impact of several cadres of community health workers on a broad range of antenatal and infant health variables. Because there are numerous outcomes that CHW-delivered ANC may affect, we investigate a subset of variables, spanning both healthcare process and outcome measures. Specifically, this study will investigate how ANC provided by CHWs, namely ASHAs, AWWs, and Community/Village Health Workers (defined in Table A.1), affect ANC utilization, ANC quality (defined in Table 1), early initiation of breast feeding, birthweight, and one-year mortality.
Table 1.
Definition of variables.
| Variable | Description |
|---|---|
| Demographic | |
| Age of Woman at Child's Birth |
|
| Age of Woman at Marriage |
|
| Rural or Urban Place of Residence |
|
| Parity |
|
| Religion |
|
| Socioeconomic | |
| Wealth Index |
|
| Woman's Educational Attainment |
|
| Caste or Tribe Membership |
|
| Exposure – Receiving Antenatal Care from a Community Health Worker | |
| Any Community Health Worker |
|
| ASHA |
|
| AWW |
|
| Other Community Health Worker |
|
| Outcomes – Antenatal and Infant Health | |
| Antenatal Care Utilization |
|
| Quality of Antenatal Care |
|
| Birthweight |
|
| Early Initiation of Breastfeeding |
|
| One-Year Mortality |
|
All variables were obtained from the Woman's Questionnaire of the National Family Health Survey 4 except for wealth index, which was obtained from the Household Questionnaire.
“Immediately” was a measure for time to initiation of breastfeeding in the data but does not represent a specific time interval.
2. Materials and methods
2.1. Cohort or case-control selection
This cross-sectional study used data from the most recent National Family Health Survey-4 (NFHS-4), a population-based survey (Woman's Questionnaire, 2015). NFHS-4 was administered from January 2015 to December 2016 across India (International Institute for Population Sciences, 2017). There were 699,686 women between ages 15–49 interviewed through two-stage stratified sampling at the village/Census Enumeration Block level and the household level. Women with a child born in the prior 5 years and complete sociodemographic data were analyzed. For women with multiple births, only their most recent was analyzed, as only this birth had the necessary data recorded.
2.2. Exposures and other socioeconomic and demographic variables
Exposures were receiving ANC from any CHW and specifically from ASHAs, AWWs, and Community/Village Health Workers, all of which are defined in Table 1. Unexposed women include those who received no ANC and those who received ANC from a doctor, auxiliary nurse midwife, dai/traditional birth attendant, or another provider but not a CHW. Thus, this study investigates the incremental effect of receiving ANC from a CHW on outcomes and in a sensitivity analysis, we adjust for the other providers a woman saw during ANC. Demographic variables were age of woman at child's birth, age of woman at marriage, rural or urban place of residence, parity, and religion. Socioeconomic variables were wealth index, women's educational attainment, and caste or tribe membership. These variables are further described in Table 1. While location of ANC is known to be associated with outcomes like ANC quality, this variable was not included as a confounder because it is a mediator in the relationship between CHW exposure and outcomes (Afulani et al., 2019). Multiple studies have found that CHWs can increase health facility attendance for ANC (Edmond et al., 2018; Wajid et al., 2013).
2.3. Outcomes
Outcomes were ANC utilization and quality, early initiation of breastfeeding, birthweight, and one-year mortality. These outcome variables are further defined in Table 1.
2.4. Statistical analyses
2.4.1. Descriptive statistics
Descriptive analyses of CHW exposure and outcome variables were conducted. Summary statistics for sociodemographic characteristics were reported for the cohort and by exposure status. Percentages were weighted as specified by NFHS-4.
2.4.2. Epidemiology of community health worker-delivered care
Associations with antenatal and infant health outcomes were initially assessed through unadjusted regressions. These were conducted among individuals with complete sociodemographic data, so that differences with the fully adjusted models would not be due to different analytic samples. Adjusted regressions examined the independent effect of CHWs on outcomes. These analyses were adjusted for all non-outcome variables listed in Table 1.
Analyses were conducted separately for each outcome: attended four ANC visits, ANC quality (defined in Table 1), early initiation of breast feeding, birthweight, and one-year mortality. The denominator for each analysis was infants with complete sociodemographic information and complete data for the relevant outcome. For each outcome, the regression was conducted with the exposure defined in two ways: 1) a single binary variable for whether or not a woman received ANC from any CHW and 2) three binary variables for whether or not a woman received ANC from an ASHA, AWW, or Community/Village Health Worker. By including all three variables in the same regression, the second form examined the independent effects of exposure to ASHAs, AWWs, and Community/Village Health Workers. According to the NFHS-4 survey, this ANC could have been provided at home or a health facility (International Institute for Population Sciences, 2017).
Logistic regressions were conducted for attended the recommended four ANC visits, early initiation of breast feeding, and one-year mortality (WHO, 2013). A Poisson regression was conducted for quality of ANC (defined in Table 1). A linear regression was conducted for birthweight. Stata's survey commands were utilized to incorporate the survey's clustering and stratification into analyses. Thus, these models were more robust to violations of autocorrelation. Variance inflation factors were computed for all regressions to assess the risk of multicollinearity and none of the predictor variables were highly collinear. All p-values were adjusted for multiple testing using the Holm method.
2.4.3. Missing data
Only 101 women were missing exposure data (Fig. 1), so this missingness was not further explored. Only the outcome of birthweight had greater than 6% of individuals missing data, so complete-case analyses were conducted. Individuals missing outcome data were explored descriptively by exposure status. Multiple variable logistic regressions were conducted to investigate the effect of CHW exposure on missingness.
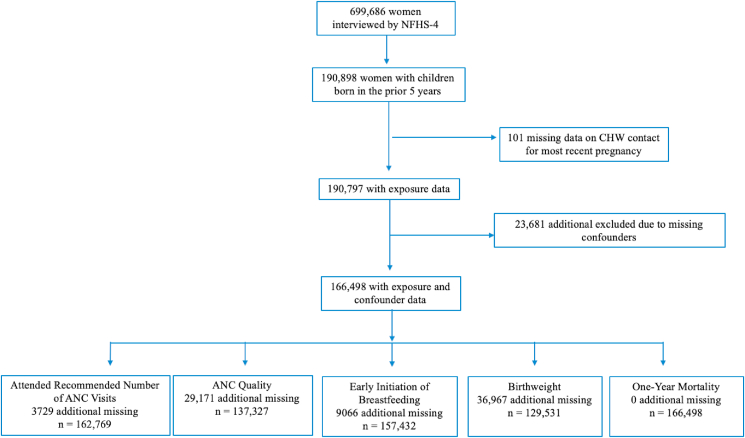
Fig. 1.
Flowchart of Inclusion/Exclusion Criteria. The numbers in this figure are the unweighted, sampled number of children. From top to bottom, the figure displays the number of individuals missing community health worker exposure data, confounder data, outcome data. Missingness for antenatal care quality is due to the fact that these women did not receive any antenatal care.
2.4.4. Sensitivity analysis
Sensitivity analyses were conducted to further examine associations. In one analysis, results were adjusted for the other providers women saw for ANC, including doctors, auxiliary nurse-midwives, nurses, mid-wives, lady health visitors, dai's, and traditional birth attendants. In another analysis, a fixed effect for each state and union territory was added to the models to account for potential residual confounding by region. Two sensitivity analyses were conducted with ANC utilization defined as: 1) whether or not a woman had eight or more ANC visits, as this became the new WHO recommendation in 2016 and 2) a Poisson regression with number of ANC visits as a count variable (WHO, 2013).
2.5. Ethics
The protocol for NFHS-4 was approved by the International Institute for Population Sciences Institutional Review Board (IRB) and the ICF IRB. It was reviewed by the U.S. Centers for Disease Control and Prevention (International Institute for Population Sciences, 2017).
3. Results
3.1. Participants
Of the 699,686 women interviewed, 190,898 had a pregnancy in the prior 5 years and 166,498 had complete data (Fig. 1).
3.2. Descriptive data
3.2.1. Study cohort
The majority of women were Hindu (80.8%; 95% CI 80.2%, 81.3%), lived in rural places (70.1%; 95% CI 69.6%, 70.6%), and were from a scheduled caste, scheduled tribe, or otherwise backwards class (78.6%; 95% CI 77.2%, 79.8%).
3.2.2. Exposure variables
The percentage of women who received ANC from any CHW was 14.2% (95% CI 13.9%, 14.5%), with specifically, 5.9% (95% CI 5.7%, 6.1%) from ASHAs, 10.2% (95% CI 10.0%, 10.5%) from AWWs, and 0.5% (95% CI 0.4%, 0.5%) from Community/Village Health Workers (defined in Table 1). The percentage of women who received ANC from any CHW ranged from 1.9% (95% CI 1.5%, 2.6%) in Nagaland to 38.6% (95% CI 36.8%, 40.4%) in Odisha (Table A.3).
Table 3.
Fully adjusted analysis of the impact of receiving antenatal care from community health workers on antenatal and infant health outcomes.
| Any CHW |
Specific CHW |
|||||||
|---|---|---|---|---|---|---|---|---|
| ASHA |
AWW |
Other |
||||||
| Estimate (95% CI)a | p-value b | Estimate (95% CI)a | p-value b | Estimate (95% CI)a | p-value b | Estimate (95% CI)a | p-value b | |
| Attended Four ANC Visits (OR) | 2.24 (2.13, 2.35) | <0.0001 | 1.77 (1.65, 1.91) | <0.0001 | 2.24 (2.12, 2.37) | <0.0001 | 1.15 (0.84, 1.57) | >0.99 |
| ANC Quality (IRR) | 1.07 (1.06, 1.08) | <0.0001 | 1.06 (1.05, 1.08) | 3.0E-16 | 1.07 (1.06, 1.08) | 3.2E-33 | 1.05 (1.01, 1.08) | 0.07 |
| Early Initiation of Breastfeeding (OR) | 1.29 (1.23, 1.35) | 6.3E-24 | 1.20 (1.12, 1.29) | 6.6E-06 | 1.3 (1.26, 1.40) | 1.5E-23 | 1.30 (1.06, 1.60) | 0.08 |
| Birthweight (grams) | −2.24 (−14.08, 9.60) | >0.99 | 2.54 (−15.47, 20.54) | >0.99 | −7.55 (−20.95, 5.85) | >0.99 | −14.54 (−76.29, 47.21) | >0.99 |
| One-Year Mortality (OR) | 0.79 (0.70, 0.88) | 4.2E-4 | 0.75 (0.63, 0.88) | 0.01 | 0.85 (0.74, 0.97) | 0.14 | 0.91 (0.51, 1.62) | >0.99 |
The estimates for Attended Recommended Number of ANC Visits, Early Initiation of Breastfeeding, and One-Year Mortality are Odds Ratios. The estimates for Antenatal Care Quality and Birthweight are incidence rate ratios and changes in grams respectively.
The 95% confidence interval presented is from the multiple regression associated with the outcome variable and does not correspond to the adjusted p-value.
p-values were adjusted using the Holm method.
3.2.3. Outcome variables
The percentage of women who attended four or more ANC visits was 48.9% (95% CI 47.0%, 51.1%). The mode of ANC quality scores was 11. There were 41.4% (95% CI 40.9%, 41.8%) of women who initiated breast feeding early, the mean birthweight of newborns was 2807 g (SD: 576), and 2.6% (95% CI 2.5, 2.7) of infants died within one year of birth.
3.2.4. Sociodemographic characteristics across exposure groups
As displayed in Table A.4, women who received ANC from a CHW were more likely to be in the lowest three wealth quintiles. The exposed group was also more likely to be Hindu (81.0% versus 78.5%), more likely to live in a rural place (83.5% versus 67.9%), and less likely to be in a non-scheduled caste/scheduled tribe/other backwards class (16.8% versus 21.0%).
3.3. Analyses
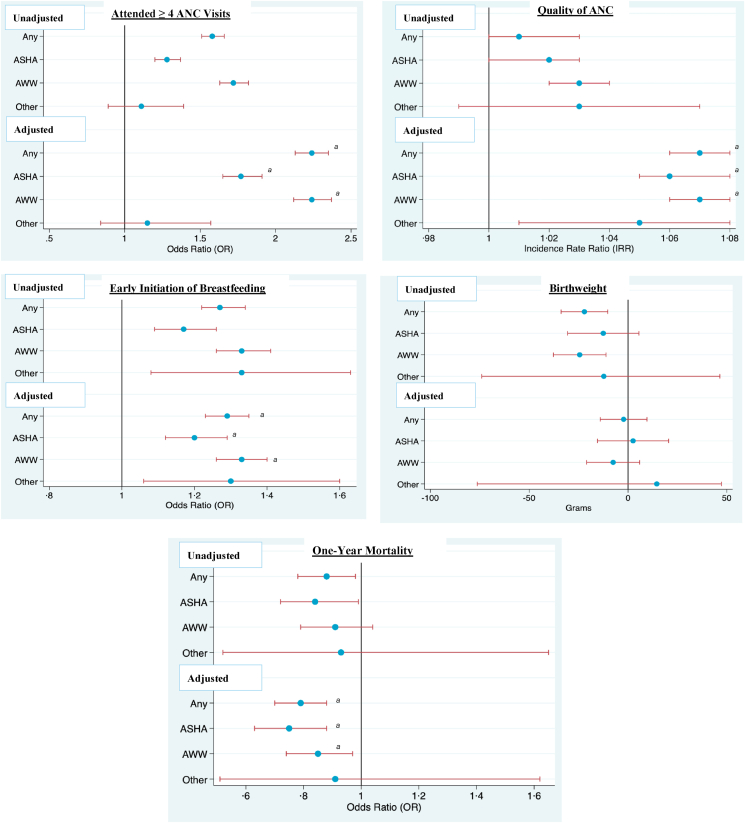
The analyses will be reported separately for: 1) receiving care from any CHW and 2) receiving care by type of CHW. Table 2, Table 3 provide the unadjusted and adjusted regression estimates and Fig. 2 displays them visually.
Table 2.
Unadjusted analysis of the impact of receiving antenatal care from community health workers on antenatal and infant health outcomes.
| Any CHW |
Specific CHW |
|||||||
|---|---|---|---|---|---|---|---|---|
| ASHA |
AWW |
Other |
||||||
| Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | |
| Attended Four ANC Visits (OR) | 1.58 (1.51, 1.66) | <0.001 | 1.28 (1.20, 1.37) | <0.001 | 1.72 (1.63, 1.82) | <0.001 | 1.11 (0.89, 1.39) | 0.36 |
| ANC Quality (IRR) | 1.01 (1.00, 1.03) | 0.005 | 1.02 (1.00, 1.03) | 0.04 | 1.03 (1.02, 1.04) | 1.2E-7 | 1.03 (0.99, 1.07) | 0.11 |
| Early Initiation of Breastfeeding (OR) | 1.27 (1.22, 1.34) | 9.7E-24 | 1.17 (1.09, 1.26) | 1.3E-05 | 1.33 (1.26, 1.41) | 5.7E-26 | 1.33 (1.08, 1.63) | 0.008 |
| Birthweight (grams) | −22.08 (−33.89, −10.26) | 2.5E-4 | −12.54 (−30.58, 5.51) | 0.17 | −24.46 (−37.77, −11.15) | 3.2E-4 | −12.27 (−74.00, 46.47) | 0.70 |
| One-Year Mortality (OR) | 0.88 (0.78, 0.98) | 0.02 | 0.84 (0.72, 0.99) | 0.05 | 0.91 (0.79, 1.04) | 0.16 | 0.93 (0.52, 1.65) | 0.80 |
The estimates for Attended Recommended Number of Antenatal Care Visits, Early Initiation of Breastfeeding, and One-Year Mortality are odds ratios. The estimates for Antenatal Care Quality and Birthweight are incidence rate ratios and changes in grams respectively.
Fig. 2.
Box Plot of Unadjusted and Fully Adjusted Effect Estimates for Receiving Antenatal Care from Community Health Workers on Antenatal and Infant Health Outcomes. Dot plots with confidence intervals of the associations between receiving antenatal care from any community health worker, Accredited Social Health Activists, Anganwadi Workers, as well as Other community health workers and antenatal as well as infant health outcomes. The results are depicted with the effect estimates from the unadjusted regression models on the top and the effect estimates from the fully adjusted regression models on the bottom. a Indicates which effect estimates were statistically significant after the adjustment of p-values for multiple testing. Adjustment for multiple testing was only done for the fully-adjusted regressions. Confidence intervals did not incorporate this adjustment, which is why some confidence intervals that do not cross 1 are not labeled with an asterisk.
3.3.1. Receiving ANC from with any community health worker
3.3.1.1. Process measures: ANC utilization, ANC quality, early initiation of breast feeding
In an unadjusted analysis, women who received ANC from any CHW had 1.58 (95% CI 1.51, 1.66) times the odds of attending four ANC visits. After adjustment, this OR increased to 2.24 (95% CI 2.13, 2.35). Receiving care from any CHW was positively associated with ANC quality in the unadjusted analysis (IRR: 1.01, 95% CI 1.00, 1.03) and after adjustment, was associated with a 1.07 (95% CI 1.06, 1.08) times increase in the score for quality of ANC. Women who received care from any CHW had 1.27 (95% CI 1.22, 1.34) times the odds of early initiation of breast feeding for their newborn in the unadjusted analysis and this effect increased after adjustment (OR: 1.29, 95% CI 1.23, 1.43).
3.3.1.2. Health outcomes: birthweight and one-year mortality of infant
In the unadjusted analysis, receiving care from any CHW was associated with a slight (Grams: 22.08, 95% CI 10.26, 33.89) decrease in birthweight and after adjustment, this association became null (Table 3). There was a statistically significant negative relationship between receiving ANC from any CHW and one-year mortality (OR: 0.88, 95% CI 0.78, 0.98). After adjustment, this association became stronger in magnitude, with women having 0.79 (95% CI 0.70, 0.88) times the odds of their child dying within one year of birth.
3.3.2. By specific community health worker: ASHA, AWW, Community/Village Health Worker
3.3.2.1. Process measures: ANC utilization, ANC quality, early initiation of breast feeding
In an unadjusted analysis, women who received ANC from ASHAs or AWWs were independently more likely to attend four ANC visits (Table 2). After adjustment, these associations grew in magnitude. Receiving ANC from ASHAs and AWWs were associated with 1.77 (95% CI 1.65, 1.91) and 2.24 (95% CI 2.12, 2.37) times the odds of attending four ANC visits respectively.
In an unadjusted analysis, women who received ANC from either ASHAs or AWWs were independently more likely to have better ANC quality (Table 2). After adjustment, these associations with ASHAs and AWWs grew in magnitude. Receiving care from ASHAs and AWWs were associated with a 1.06 (95% CI 1.05,1.08) times and 1.07 (95% CI 1.06, 1.08) times increase in the quality score for ANC respectively.
In an unadjusted analysis, women who received care from ASHAs, AWWs, and Community/Village Health Workers were independently more likely to initiate breast feeding early for their newborns (Table 2). After adjustment, only the associations with ASHAs and AWWs remained statistically significant. Women who received ANC from ASHAs and AWWs had 1.20 (95% CI 1.12, 1.29) times and 1.33 (95% CI 1.26, 1.40) times the odds of initiating breast feeding early respectively.
3.3.2.2. Outcome measures: birthweight and one-year mortality of infant
In an unadjusted analysis, only receiving ANC from AWWs was independently associated with a slight (Grams: 24.46; 95% CI -37.77, 11.15) decrease in newborn birthweight but after adjustment, no association remained.
Without adjustment, only receiving ANC from ASHAs was independently associated with decreased odds of one-year mortality for infants (Table 2). After adjustment, this effect size grew in magnitude to 0.75 (95% CI 0.63, 0.88) times the odds of one-year mortality.
3.4. Sensitivity analyses
After adjusting for the other providers women saw for ANC, the effect of CHW exposure on antenatal and infant health variables persisted (Table A.5). Incorporating a fixed effect for state or union territory also resulted in persisting associations of slightly decreased statistical significance (Table A.6).
When ANC utilization was redefined to attending eight ANC visits, the effect of receiving ANC from ASHAs decreased in statistically significance (OR: 1.17; 95% CI 1.04, 1.31). When ANC utilization was defined as a count variable for number of visits, receiving care from any CHW, ASHAs, AWWs, and Community/Village Health Workers were all associated with increased utilization (Table A.7).
Missingness for outcome data was explored with regards to its relationship with exposure status. Receiving ANC from any CHW was associated with missingness and thus, the values were not missing completely at random (Table A.8).
Because of the relatively limited amount of missing data (Fig. 1), imputation was not conducted.
4. Discussion
4.1. Principle findings
In this study of 166,498 Indian women, receiving ANC from any CHW was associated with greater ANC utilization, higher quality of ANC, and early initiation of breast feeding. This effect was not homogeneous across all types of CHWs. Receiving care from ASHAs and AWWs were each independently associated with improved ANC utilization and quality as well as early initiation of breast feeding. Only receiving ANC from ASHAs was independently associated with decreased one-year mortality. It is important to note, however, that fewer than 15% of women received ANC from either ASHAs or AWWs.
4.2. Strengths of the study
This is the first study to simultaneously analyze the effectiveness of multiple cadres of CHWs in India. Additionally, it is the first study globally to investigate the impact of receiving ANC from CHWs on birthweight or one-year mortality.
Another strength is the robust nature of the NFHS-4 sampling design. The survey is nationally representative. The two-stage stratified sampling design was established to produce reliable estimates of indicators at the district, state or union territory, and national level. Because of the large number of women interviewed, this analysis was well-powered. Due to the vast array of questions included in the survey, this study was able to adjust for many potential confounders.
4.3. Limitations of the data
One limitation of this study is exposure and outcome ascertainment. With regards to the exposure, the survey only indicates whether or not a CHW was seen but not the number of interactions and the quality of these interactions. The survey does not indicate what immunizations, counsel, and other services were provided during each ANC visit a woman had. This limitation is inherent to using the DHS survey which is comprehensive in coverage of topics and samples over a million Indians, but as a result, is not able to ask in depth questions about participant's multitude of healthcare experiences. The outcome variable quality of ANC was a composite variable created for this study and is not a validated instrument. For the outcome of early initiation of breast feeding, there could be measurement error, as the survey only includes two categorical values for breast feeding immediately or after 1 h or more birth. If breast feeding within an hour was rounded up to 1 h, the data would underestimate the proportion of women who initiated breast feeding early.
Residual confounding from distance to a healthcare facility, not available in NFHS-4 data, could confound observed relationships.
As with any cross-sectional study, recall bias could be present. For one-year mortality, women whose infants died could be more likely to recall receiving ANC from a CHW. Such a bias would skew the effect estimate towards the null. Reverse causality is possible, as the outcome of having more ANC visits could make it more likely to receive care from a CHW. Selection bias could be present, as the cohort only includes women with live births and thus, excludes women with the worst pregnancy outcomes: miscarriages, stillbirths, and maternal death. If these women were less likely to receive ANC from a CHW and more likely to experience adverse outcomes, effect estimates would be biased towards the null.
4.4. Interpretation
This study provides evidence for the value of CHWs for improving antenatal and infant health. Effects were seen independently for exposure to ASHAs and AWWs, indicating the effectiveness of both of India's largescale CHW programs.
As discussed before, prior literature contains mixed results as to the effectiveness of ASHAs for ANC. Nonetheless, ASHAs were hypothesized to have an impact on the investigated outcomes because part of their role is in maternal and child health (Fathima et al., 2015; Kohli et al., 2015; Perry et al., 2013; Scott et al., 2019). This study confirms prior research from Agarwal et al., which found, using the India HDS, that receiving services from ASHAs was associated with an increase in attending 4 or more ANC visits (Agarwal et al., 2019). In our study, this association held even after controlling for a variety of socioeconomic and demographic factors and even in sensitivity analyses that controlled for the other providers a woman received ANC from and the state or union territory a woman lived in. The long-term effect of ASHA-delivered ANC on infant mortality was not expected but could be explained by the fact that women who receive ANC from ASHAs are in the catchment area of an ASHA and thus, may be likely to receive infant care from an ASHA as well (Perry et al., 2013). For ASHAs, the effect on both process outcomes and health outcomes suggests a causal pathway by which receiving ANC from ASHAs can lead to improved infant health.
The effect of AWWs on antenatal health outcomes was not anticipated, as the primary aim of AWWs is to dispense nutritional supplementation not antenatal care (Perry et al., 2013). Thus, observing even larger effect sizes for receiving care from AWWs compared to ASHAs on attending the recommended number of ANC visits and ANC quality was surprising. Because AWWs are based in anganwadi centers while ASHAs are in the community, the greater effect observed from exposure to AWWs could be attributed to the unmeasured confounder of a woman being close to an anganwadi center and more generally, having better access to care (Perry et al., 2013). Still, the effects of receiving care from AWWs persists, even after controlling for the other providers a woman saw for ANC, so access to care may not fully explain the effect of AWWs. Because AWWs are also responsible for promoting healthy behavior and one of their target populations is pregnant women, it is plausible that they could improve care for pregnant women (Table 1).
5. Conclusion
This study provides both confirmatory and new evidence on the effectiveness of India's CHW programs for improving antenatal and infant health. This analysis was essential given the scope of and financial resources invested in India's 857,000 ASHAs and 1.2 million AWWs. Given the dearth of prior research on this topic, further work is needed to better understand these findings. Qualitative research must be conducted to better understand what activities ASHAs and AWWs, whose main role is in nutrition, conduct to affect antenatal and infant health. To more holistically evaluate CHWs, assessment should extend to maternal health outcomes. This study provides the first evidence globally on the effectiveness of CHW-delivered ANC on birthweight and one-year mortality. Further research should be conducted outside India to assess CHWs' influence on the same outcomes, so that better-performing CHW programs can be identified and lessons from them can be extracted and applied to new contexts. In this study, a small percentage of women received ANC from an ASHA. This may not be surprising as India needs to train 483,000 new ASHAs to fulfill the government mandate of 1 ASHA per 1000 people (Perry et al., 2013). This study's positive findings in tandem with nation-wide lack of access to ASHAs suggest that India's government should expand CHWs, in order to maximize their population-level impact for antenatal and infant health.
Funding
This work consisted of analysis of a pre-existing dataset, so it did not require any funding.
CRediT author statement
Pranay Vanella: Conceptualization, Methodology, Software, Data curation, Writing- Original draft preparation, Visualization, Investigation, Writing- Reviewing and Editing.
S V Subramanian: Conceptualization, Methodology, Software, Supervision, Writing- Reviewing and Editing.
Andres Roman-Urrestarazu: Conceptualization, Methodology, Software, Supervision, Writing- Reviewing and Editing.
Data availability statement
This data is from India's most recent round of its Demographic and Health Survey, DHS-IV. The data can be downloaded from here: https://dhsprogram.com/data/dataset/India_Standard-DHS_2015.cfm?flag=0.
Declaration of competing interest
No financial interest has arisen from this research.
Acknowledgments
The authors alone worked on this study.
Appendix.
Table A.1.
Outline of India's national community health worker programs
| Name | Role | Setting | Training | Compensation | Scale across India |
|---|---|---|---|---|---|
| Anganwadi Workers | Anganwadi workers work at the anganwadi centers in their own villages. They focus on nutritional supplementation for children, adolescent girls, pregnant women, and lactating mothers. They also interface with the community, by promoting healthy behaviors and mobilizing community members improved water sanitation, immunization, and other health activities. | Village | 3–4 weeks | Considered to be volunteers but paid around $27 to $29 per month. | 1,200,000 |
| Accredited Social Health Activists | ASHAs work solely in their village and focus on promoting maternal and child health, which includes immunizations, basic medicine provision, and facility-based deliveries. The aim is to have 1 ASHA for every 1000 people. | Village | 3–4 weeks | Receive $16 per month for completing day-to-day tasks. Performance-based compensation includes $10 for facilitating an institutional delivery and $2.50 for facilitating a child's complete immunization. | 857,000 |
Details about India's community health worker programs found in an international report (Perry et al., 2013).
Table A.2.
Descriptive Analysis of Sociodemographic Variables
| Characteristic | Total (n = 166,498) |
|---|---|
| Birth Parity | |
| Mean (SD) | 2.31 (2.25) |
| Woman's Age at Childbirth | |
| Median (IQR) | 24 (21–27) |
| Woman's Age at Marriage | |
| Median (IQR) | 18 (16–21) |
| Wealth Index | |
| Poorest | 23.4% (95% CI: 23.1%, 23.8%) |
| Poorer | 20.7% (95% CI: 20.4%, 21.0%) |
| Middle | 19.7% (95% CI: 19.4%, 20.1%) |
| Richer | 19.1% (95% CI: 18.7%, 19.5%) |
| Richest | 17.0% (95% CI: 16.6%, 17.4%) |
| Religion | |
| Hindu | 80.8% (95% CI: 80.2%, 81.3%) |
| Muslim | 14.0% (95% CI: 13.5%, 14.5%) |
| Christian | 2.1% (95% CI: 2.0%, 2.3%) |
| Sikh | 1.5% (95% CI: 1.4%, 1.5%) |
| Other | 1.7% (95% CI: 1.4%, 1.9%) |
| Type of Place of Residence | |
| Urban | 29.9% (95% CI: 29.4%, 30.4%) |
| Rural | 70.1% (95% CI: 69.6%, 70.6%) |
| Caste | |
| Scheduled Caste | 22.3% (95% CI: 21.8%, 22.7%) |
| Scheduled Tribe | 10.7% (95% CI: 10.4%, 11.0%) |
| Otherwise Backwards Caste | 45.6% (95% CI: 45.0%, 46.1%) |
| None of Them | 21.5% (95% CI: 21.0%, 22.0%) |
Because this table is for the study cohort, women missing data for any of the variables are already excluded, as displayed in Table A1. Percentages are weighted based on the sampling weights specified by National Family Health Survey 4. Weighting was not incorporated for the median and interquartile range for Woman's Age at Childbirth and Woman's Age at Marriage.
Table A.3.
Access to community health worker-delivered antenatal care by state and union territory
| State or Union Territory | Percentage of Women who Received Antenatal Care from any CHW (95% CI) |
|---|---|
| Andhra Pradesh | 10.4 (8.7, 12.3) |
| Arunachal Pradesh | 2.4 (1.8, 3.2) |
| Assam | 17.8 (16.3, 19.4) |
| Bihar | 10.5 (9.8, 11.2) |
| Chhattisgarh | 29.0 (27.1, 31.0) |
| Goa | 13.9 (9.8, 19.4) |
| Gujarat | 14.5 (13.2, 16.0) |
| Haryana | 12.5 (11.2., 14.0) |
| Himachal Pradesh | 2.3 (1.6, 3.2) |
| Jammu and Kashmir | 11.1 (9.6, 12.9) |
| Jharkhand | 16.8 (15.6, 18.1) |
| Karnataka | 6.0 (5.0, 7.1) |
| Kerala | 10.4 (8.5, 12.5) |
| Madhya Pradesh | 18.8 (17.9, 19.8) |
| Maharashtra | 6.0 (5.3, 6.9) |
| Manipur | 5.2 (4.3, 6.3) |
| Meghalaya | 5.1 (3.9, 6.5) |
| Mizoram | 4.9 (3.7, 6.5) |
| Nagaland | 1.9 (1.5, 2.6) |
| Odisha | 38.6 (36.8, 40.4) |
| Punjab | 10.8 (9.3, 12.5) |
| Rajasthan | 14.0 (13.0, 15.1) |
| Sikkim | 4.7 (3.4, 6.5) |
| Tamil Nadu | 15.2 (13.7, 16.9) |
| Telangana | 8.0 (6.6, 9.8) |
| Tripura | 10.0 (7.7, 13.0) |
| Uttar Pradesh | 11.7 (11.1, 12.4) |
| Uttarakhand | 7.0 (5.9, 8.2) |
| West Bengal | 28.7 (26.2, 31.4) |
| Andaman and Nicobar Islands | 0.6 (0.2, 1.8) |
| Chandisgarh | 2.0 (0.3, 12.7) |
| Dadra and Nagar Haveli | 6.7 (3.1, 13.6) |
| Daman and Diu | 10.5 (7.4, 14.9) |
| Delhi | 1.4 (0.8, 2.5) |
| Lakshadweep | 13.7 (8.5, 21.3) |
| Pondicherry | 7.8 (5.2, 11.5) |
Percentages were calculated based on the weighting specified by the survey.
Table A.4.
Descriptive analysis of sociodemographic variables by exposure to community health workers
| Characteristic | Total n = 166,498 |
|||||||
|---|---|---|---|---|---|---|---|---|
| No CHW Antenatal Care n = 142,529 | Any CHW Antenatal Care n = 23,969 | No ASHA Antenatal Care n = 156,595 | ASHA Antenatal Care n = 9903 | No Anganwadi Worker Antenatal Care n = 149,524 | Anganwadi Worker Antenatal Care n = 16,974 | No Community/Village Health Worker n = 165,647 | Community/Village Health Worker n = 851 | |
| Mother's Age at Childbirth | ||||||||
| Median (IQR) | 24 (22–28) | 24 (21–28) | 24 (22–28) | 24 (21–28) | 24 (22–28) | 24 (21–27) | 24 (22–28) | 25 (22–29) |
| Woman's Age at Marriage | ||||||||
| Median (IQR) | 19 (17–21) | 18 (16–20) | 19 (16–21) | 18 (16–21) | 19 (16–21) | 18 (16–20) | 19 (16–21) | 19 (17–21) |
| Wealth Index | ||||||||
| Poorest | 33,001 (22.3%) | 7790 (30.1%) | 37,630 (22.9%) | 3161 (32.2%) | 35,113 (22.8%) | 5678 (29.2%) | 40,596 (23.4%) | 195 (23.2%) |
| Poorer | 31,067 (19.8%) | 6362 (26.4%) | 34,504 (20.1%) | 2925 (30.1%) | 33,149 (20.2%) | 4280 (25.4%) | 37,241 (20.7%) | 188 (24.8%) |
| Middle | 28,640 (19.6%) | 4592 (20.4%) | 31,336 (19.8%) | 1896 (18.9%) | 30,021 (19.6%) | 3211 (20.9%) | 33,046 (19.7%) | 186 (20.5%) |
| Richer | 25,927 (19.8%) | 3241 (14.9%) | 28,016 (19.6%) | 1152 (11.6%) | 26,789 (19.5%) | 2379 (15.8%) | 29,001 (19.1%) | 167 (21.2%) |
| Richest | 23,894 (18.5%) | 1984 (8.3%) | 25,109 (17.6%) | 769 (7.3%) | 24,452 (18.0%) | 1426 (8.7%) | 25,763 (17.1%) | 115 (10.4%) |
| Religion | ||||||||
| Hindu | 104,348 (80.3%) | 19,737 (83.4%) | 116,460 (80.9%) | 7625 (78.8%) | 109,457 (80.3%) | 14,628 (85.0%) | 123,490 (80.8%) | 595 (83.9%) |
| Muslim | 18,841 (14.5%) | 2528 (11.4%) | 20,036 (14.0%) | 1333 (14.3%) | 19,906 (14.5%) | 1463 (9.6%) | 21,288 (14.0%) | 81 (10.8%) |
| Christian | 12,959 (2.2%) | 877 (1.8%) | 13,380 (2.2%) | 456 (1.6%) | 13,455 (2.2%) | 381 (1.8%) | 13,688 (2.1%) | 148 (3.6%) |
| Sikh | 2697 (1.5%) | 387 (1.2%) | 2821 (1.4%) | 263 (1.9%) | 2869 (1.5%) | 215 (0.9%) | 3076 (1.5%) | 8 (0.8%) |
| Other | 3684 (1.6%) | 440 (2.2%) | 3898 (1.5%) | 226 (3.4%) | 3837 (1.5%) | 287 (2.7%) | 4105 (1.7%) | 19 (1.0%) |
| Type of Place of Residence | ||||||||
| Urban | 38,769 (32.1%) | 3629 (16.7%) | 41,333 (31.0%) | 1065 (11.8%) | 39,598 (31.3%) | 2800 (18.2%) | 42,172 (29.9%) | 226 (24.7%) |
| Rural | 103,760 (67.9%) | 20,340 (83.3%) | 115,262 (69.0%) | 8838 (88.2%) | 109,926 (68.8%) | 14,174 (81.8%) | 123,475 (70.1%) | 625 (75.4%) |
| Caste | ||||||||
| Scheduled Caste | 27,130 (21.8%) | 5187 (24.9%) | 30,095 (22.0%) | 2222 (26.3%) | 28,650 (22.0%) | 3667 (24.4%) | 32,140 (22.2%) | 177 (28.7%) |
| Scheduled Tribe | 28,943 (9.9%) | 5501 (15.1%) | 32,194 (10.5%) | 2250 (13.7%) | 30,541 (10.0%) | 3903 (16.3%) | 34,218 (10.7%) | 226 (8.9%) |
| Otherwise Backwards Caste | 57,719 (46.0%) | 9888 (43.2%) | 63,998 (46.1%) | 3609 (37.4%) | 60,256 (45.7%) | 7351 (44.9%) | 67,265 (45.6%) | 342 (46.8%) |
| None of Them | 28,737 (22.3%) | 3393 (16.8%) | 30,308 (21.4%) | 1822 (22.6%) | 30,077 (22.3%) | 2053 (14.4%) | 32,024 (21.5%) | 106 (15.6%) |
Baseline sociodemographic characteristics of the cohort according to whether or not a woman received antenatal care from any CHW and specifically from ASHAs, anganwadi workers or Community/Village Health Workers. The frequencies are the actual counts from the cohort of 166,498 women, but the percentages are weighted based on the sampling weights specified by National Family Health Survey-4, so the percentages do not correspond perfectly to the frequencies. Weighting was not incorporated for the median and IQR for Woman's Age at Childbirth and Woman's Age at Marriage.
Table A.5.
Fully adjusted analysis of the impact of receiving antenatal care from community health workers on antenatal and infant health outcomes with additional adjustment for other providers seen for antenatal care
| Any CHW |
Specific CHW |
|||||||
|---|---|---|---|---|---|---|---|---|
| ASHA |
Anganwadi Worker |
Community/Village Health Worker |
||||||
| Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | |
| Attended Recommended Number of Antenatal Care Visits (OR) | 2.77 (2.62, 2.94) | <0.001 | 2.13 (1.95, 2.32) | <0.001 | 2.53 (2.37, 2.71) | <0.001 | 1.29 (0.83, 2.01) | 0.25 |
| Antenatal Care Quality (Score)* | 1.10 (1.09, 1.11) | <0.001 | 1.09 (1.07, 1.10) | <0.001 | 1.08 (1.07, 1.10) | <0.001 | 1.06 (1.03, 1.10) | <0.001 |
| Early Initiation of Breastfeeding (OR) | 1.30 (1.24, 1.36) | <0.001 | 1.21 (1.13, 1.31) | <0.001 | 1.33 (1.26, 1.40) | <0.001 | 1.28 (1.05, 1.56) | 0.02 |
| Birthweight (grams) | −0.84 (−12.70, 11.03) | 0.89 | 3.64 (−14.36, 21.65) | 0.69 | −6.76 (−20.17, 6.65) | 0.32 | −15.65 (−77.79, 46.49) | 0.62 |
| One-Year Mortality (OR) | 0.79 (0.70, 0.88) | <0.001 | 0.74 (0.63, 0.88) | 0.001 | 0.85 (0.75, 0.97) | 0.02 | 0.91 (0.51, 1.62) | 0.74 |
The effect estimates reported vary for outcome variable based on the regression used. As indicated in the first column, the estimates for Attended Recommended Number of Antenatal Care Visits, Early Initiation of Breastfeeding, and One-Year Mortality are Odds Ratios. The effect estimates for Antenatal Care Quality are incidence rate ratios and Birthweight are changes in grams. These results do not include any adjustment for multiple testing.
Table A.6.
Fully adjusted analysis of the impact of receiving antenatal care from community health workers on antenatal and infant health outcomes with additional fixed effect for state or union territory
| Any CHW |
Specific CHW |
|||||||
|---|---|---|---|---|---|---|---|---|
| ASHA |
Anganwadi Worker |
Community/Village Health Worker |
||||||
| Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | |
| Attended Recommended Number of Antenatal Care Visits (OR) | 2.05 (1.95, 2.15) | <0.001 | 1.64 (1.52, 1.77) | <0.001 | 2.06 (1.95, 2.19) | <0.001 | 1.00 (0.68, 1.45) | 0.98 |
| Antenatal Care Quality (IRR) | 1.03 (1.02, 1.04) | <0.001 | 1.06 (1.04,1.07) | <0.001 | 1.02 (1.01, 1.03) | <0.001 | 1.01 (0.98, 1.04) | 0.53 |
| Early Initiation of Breastfeeding (OR) | 1.18 (1.13, 1.24) | <0.001 | 1.17 (1.09, 1.26) | <0.001 | 1.21 (1.15, 1.28) | <0.001 | 1.17 (0.95, 1.45) | 0.14 |
| Birthweight (grams) | 1.85 (−9.99, 13.69) | 0.76 | 4.56 (−13.48, 22.63) | 0.62 | −2.61 (−16.14, 10.93) | 0.71 | −28.34 (−89.68, −33.01) | 0.37 |
| One-Year Mortality (OR) | 0.81 (0.72, 0.91) | <0.001 | 0.75 (0.64, 0.89) | 0.001 | 0.88 (0.77, 1.01) | 0.07 | 0.97 (0.54, 1.72) | 0.91 |
The effect estimates reported vary for outcome variable based on the regression used. As indicated in the first column, the estimates for Attended Recommended Number of Antenatal Care Visits, Early Initiation of Breastfeeding, and One-Year Mortality are Odds Ratios. The effect estimates for Antenatal Care Quality are incidence rate ratios and Birthweight are changes in grams. These results do not include any adjustment for multiple testing.
Table A.7.
Fully adjusted sensitivity analysis of the impact of receiving antenatal care from community health workers on antenatal care utilization
| Any CHW |
Specific CHW |
|||||||
|---|---|---|---|---|---|---|---|---|
| ASHA |
Anganwadi Worker |
Community/Village Health Worker |
||||||
| Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | Estimate (95% CI) | p-value | |
| Attended 8 or more Antenatal Care Visits (OR) | 1.32 (1.23, 1.43) | <0.001 | 1.17 (1.04, 1.31) | 0.008 | 1.45 (1.33, 1.57) | <0.001 | 1.28 (0.96, 1.70) | 0.60 |
| Number of Antenatal Care Visits (IRR) | 1.36 (0.29, 0.32) | <0.001 | 1.22 (1.19, 1.25) | <0.001 | 1.34 (1.31, 1.37) | <0.001 | 1.10 (1.01, 1.20) | 0.03 |
Antenatal care visits are defined as 1) meeting the current World Health Organization recommendation of 8 or more antenatal care visits and 2) number of antenatal care visits, as a count variable. These regressions were adjusted for all of sociodemographic confounders.
Table A.8.
Association between receiving antenatal care from any community health worker and missingness for each outcome variable
| Any CHW (n = 26,014) | No CHW (n = 158,524) | Odds Ratio (OR) | p-value | |
|---|---|---|---|---|
| Met Recommended Number of Antenatal Care Visits | ||||
| Missing | 811 (3.6%) | 3497 (2.5%) | 1.79 (1.55, 2.08) | <0.001 |
| Antenatal Care Quality | ||||
| Missing | 0 (0%) | 26,604 (19.3%) | N/A | N/A |
| Early Initiation of Breastfeeding | ||||
| Missing | 863 (3.8%) | 7452 (5.4%) | 0.70 (0.64, 0.77) | <0.001 |
| Birthweight | ||||
| Missing | 4003 (17.6%) | 26,986 (19.6%) | 0.69 (0.65, 0.74) | <0.001 |
This table reports the frequencies, percentages, and odds ratios of women with missing outcome data according to whether or not the women was seen for antenatal care by any community health worker. All of the frequencies and percentages are weighted based on the sampling weights specified by National Family Health Survey-4. Odds Ratios are adjusted for the sociodemographic variables adjusted for in all analyses.
References
- Afulani P.A., Buback L., Essandoh F., Kinyua J., Kirumbi L., Cohen C.R. Quality of antenatal care and associated factors in a rural county in Kenya: An assessment of service provision and experience dimensions. BMC Health Services Research. 2019 doi: 10.1186/s12913-019-4476-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal S., Curtis S.L., Angeles G., Speizer I.S., Singh K., Thomas J.C. The impact of India's accredited social health activist (ASHA) program on the utilization of maternity services: A nationally representative longitudinal modelling study. Human Resources for Health. 2019 doi: 10.1186/s12960-019-0402-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antenatal care. UNICEF Global Databases.
- Armstrong G., Kermode M., Raja S., Suja S., Chandra P., Jorm A.F. A mental health training program for community health workers in India: Impact on knowledge and attitudes. International Journal of Mental Health Systems. 2011 doi: 10.1186/1752-4458-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balarajan Y., Selvaraj S., Subramanian S.V. India: Towards universal health coverage 4 health care and equity in India. Lancet. 2011 doi: 10.1016/S0140-6736(10)61894-6. doi:10.1016/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauserman M., Lokangaka A., Thorsten V. Risk factors for maternal death and trends in maternal mortality in low- and middle-income countries: A prospective longitudinal cohort analysis. Reproductive Health. 2015 doi: 10.1186/1742-4755-12-S2-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmond K.M., Yousufi K., Anwari Z. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population-based intervention study. BMC Medicine. 2018 doi: 10.1186/s12916-018-1092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fathima F.N., Raju M., Varadharajan K.S., Krishnamurthy A., Ananthkumar S.R., Mony P.K. Assessment of ’Accredited Social Health Activists’-A national community health volunteer scheme in Karnataka state, India. Journal of Health, Population and Nutrition. 2015;33(1):137–145. [PMC free article] [PubMed] [Google Scholar]
- International Institute for Population Sciences National family health survey (NFHS-4) 2015-16 India. International Institute Population Science ICF. 2017 doi: 10.1093/aje/kwm120. kwm120 [pii] [DOI] [Google Scholar]
- Khetan A., Patel T., Hejjaji V. Role development of community health workers for cardiovascular disease prevention in India. Evaluation and Program Planning. 2018 doi: 10.1016/j.evalprogplan.2018.01.006. [DOI] [PubMed] [Google Scholar]
- Kohli C., Kishore J., Sharma S., Nayak H. Knowledge and practice of accredited social health Activists for maternal healthcare delivery in Delhi. Journal of Family Medicine and Primary Care. 2015 doi: 10.4103/2249-4863.161317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maternal Health Division - Ministry of Health and Family Welfare - Government of India . 2010. Guidelines for antenatal care and skilled attendance at birth by ANMs/LHVs/SNs. [Google Scholar]
- Perry H., Zulliger R., Scott K., Javadi D., Gergen J. Case studies of large-scale community health worker programs: Examples from Bangladesh, Brazil, Ethiopia, India, Iran, Nepal, and Pakistan. Matern Child Health Integration Program. 2013 [Google Scholar]
- Roy S., Haque M.A. Effect of antenatal care and social well-being on early neonatal mortality in Bangladesh. BMC Pregnancy and Childbirth. 2018;18(1):4–9. doi: 10.1186/s12884-018-2129-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott K., George A.S., Ved R.R. Taking stock of 10 years of published research on the ASHA programme: Examining India's national community health worker programme from a health systems perspective. Health Research Policy and Systems. 2019 doi: 10.1186/s12961-019-0427-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank. Current health expenditure (% of GDP). World health organisation global health expenditure database.
- UNICEF . Unicef.; 2007. The state OF the WORLD’S children 2008: Child survival. [DOI] [Google Scholar]
- UNICEF . Maternal and Newborn Health; 2009. The state of the world's children. 2009. [DOI] [Google Scholar]
- Wagner A.L., Porth J.M., Bettampadi D., Boulton M.L. Have community health workers increased the delivery of maternal and child healthcare in India? Journal of Public Health. 2018 doi: 10.1093/pubmed/fdx087. [DOI] [PubMed] [Google Scholar]
- Wajid A., White F., Karim M.S. Community health workers and health care delivery: Evaluation of a women's reproductive health care project in a developing country. PloS One. 2013 doi: 10.1371/journal.pone.0075476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO WHO recommendations on antenatal care for a positive pregnancy experience. Ultrasound in Obstetrics and Gynecology. 2013 doi: 10.1002/uog.12342. [DOI] [Google Scholar]
- Woman’s Questionnaire . 2015. National family health survey, India. [Google Scholar]
- World Bank Out-of-pocket health expenditure (% of private expenditure on health) World Dev Indic. 2016 doi: 10.5902/22364994/19339. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This data is from India's most recent round of its Demographic and Health Survey, DHS-IV. The data can be downloaded from here: https://dhsprogram.com/data/dataset/India_Standard-DHS_2015.cfm?flag=0.