Abstract
Because previous randomized clinical trials have failed to show any benefits of renal artery stenting (RAS), clinicians have been confused regarding the optimal management of patients with atherosclerotic renal artery stenosis (ARAS). Here, we report a notable case with ARAS whose clinical course could help clinicians identify patients suitable for RAS. A 66-year-old woman with ARAS and some parameter abnormalities on renal duplex ultrasound was admitted to our hospital with severe hypertension (>250 mmHg). After the initiation of antihypertensive intravenous treatment, the patient manifested acute worsening of renal function over 6 days and required dialysis. Because renal failure continued to deteriorate over more than 4 weeks, we performed stenting to the severe ostial stenosis of the right renal artery. As a result, the patient achieved dramatic improvement in renal function and successful withdrawal from dialysis and has maintained stable control of blood pressure without additional events for more than 2 years since discharge. This case suggests that careful analysis of the patient's profile, such as history of rapidly deteriorating renal failure, presence of bilateral ARAS, or a solitary functional kidney, in addition to various parameters of renal duplex ultrasound, may help predict the efficacy of RAS in patients with ARAS.
<Learning objective: Because several randomized studies have reported negative results for renal artery stenting (RAS), an individual-based approach is required for the treatment of atherosclerotic renal artery stenosis (ARAS). To determine whether RAS could be effective in patients with ARAS, it is important to assess patient-specific characteristics such as progression of renal failure (e.g. acute worsening), presence of bilateral ARAS, or the existence of a solitary functional kidney, as well as parameters of related examinations such as the renal arterial resistive index.>
Keywords: Atherosclerotic renal artery stenosis, Recovery from worsened renal failure, Renal artery stenting
Introduction
Because several randomized studies have not shown any benefits from adding renal artery stenting (RAS) to the optimal medical treatment [1, 2], clinicians have debated how to provide optimal management of patients with atherosclerotic renal artery stenosis (ARAS). We experienced a notable case with ARAS in which the patient had significant improvement in renal function and dialysis withdrawal after RAS treatment. The results of this study may help distinguish patients suitable for RAS.
Case report
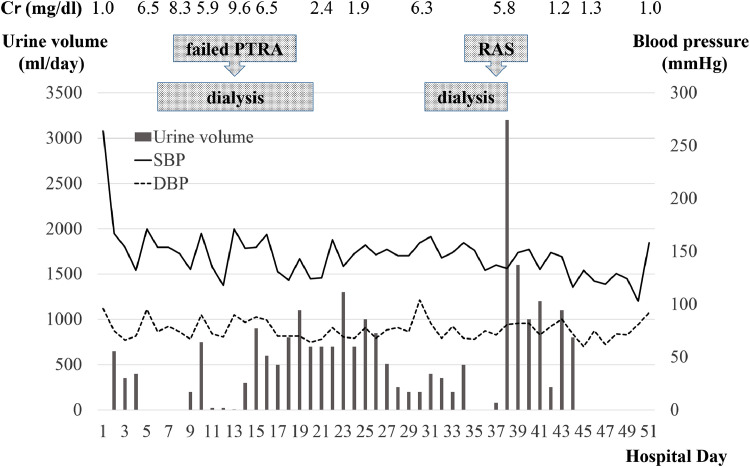
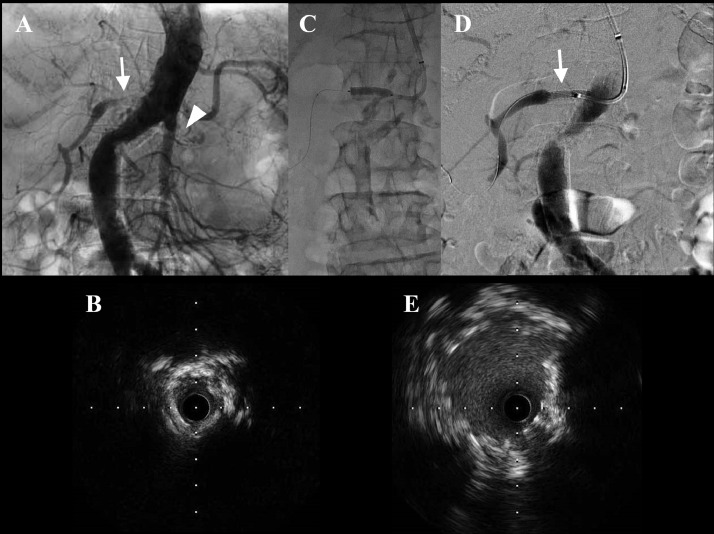
A 66-year-old woman who was taking six antihypertensive medications daily (nifedipine, 40 mg; azilsartan, 20 mg; carvedilol, 20 mg; furosemide, 20 mg; trichlormethiazide, 2 mg; spironolactone, 20 mg) presented at our hospital for assessment of refractory hypertension. Although her plasma renin activity and plasma concentrations of aldosterone, cortisol, and catecholamines were within the normal range, renal duplex ultrasound detected an atrophic left kidney (73 mm) with a peak systolic velocity of 90 cm/s and a normal-sized right kidney with an elevated peak systolic velocity of 239 cm/s. Bilateral renal arterial resistive index (right, 0.51; left, 0.45) was significantly low. Contrast-enhanced computed tomography (CT), which caused brief allergic symptoms in the patient, revealed equivalent enhancement and severely stenosed renal arteries with advanced calcified ostium of bilateral kidneys. After 10 months of medical treatment, she was transferred to our hospital due to palpitation with a markedly elevated blood pressure of 264/96 mmHg. CT and echocardiography did not reveal signs of aortic dissection or heart failure. After starting an intravenous injection of nicardipine to prevent fatal hemorrhagic events, the patient's blood pressure immediately decreased to about 150–170 mmHg; however, her urination and renal function worsened rapidly, with an elevation of serum creatinine level from 1.0 mg/dL at admission to 6.9 mg/dL at 5 days (Fig. 1). Because the patient reached anuria, hemodialysis was started on the sixth hospital day. Based on previous test results, we suspected that the acute renal failure was due to renal arterial stenosis. Aortography was performed under premedication of steroid for contrast media allergy and revealed 90% stenosis of the right renal artery and a suboccluded left renal artery (Fig. 2A). We attempted percutaneous transluminal renal artery angioplasty (PTRA) to the right renal artery stenosis, but this was unsuccessful due to an inability to insert intervention devices. After 2 weeks of dialysis three times weekly, the patient's urination improved, and she was able to temporarily suspend dialysis; however, anuria recurred after a few days with an increase in the serum creatinine level to 6.3 mg/dL. We again attempted PTRA to the right renal arterial stenosis by changing the strategy and using carbon dioxide (CO2) with an injection of a small test dose of contrast medium as allergy prevention measures. Intravascular ultrasound (IVUS) before stenting showed obstructive deposition of heterogeneous intimal plaques with marked calcification at the ostium of the right renal artery (Fig. 2B). A Palmaz Genesis renal stent was successfully deployed after several predilatations by plural balloons (Fig. 2C, D), and adequate gain of vessel lumen was confirmed on IVUS imaging (Fig. 2E). Renal duplex ultrasound a week later showed normalization of peak systolic velocity (162 cm/s) and renal arterial resistive index (0.60) in the right kidney. After the procedure, the patient's urinary volume increased dramatically to more than 3000 mL/day. Her serum creatinine level also improved to 1.2 mg/dL at 5 days, and dialysis was discontinued (Fig. 1). Furthermore, her blood pressure decreased to approximately 130 mmHg after the procedure and while taking fewer antihypertensive drugs than before admission. The patient did not experience any clinical events during the subsequent period and was discharged on the 51st hospital day with a serum creatinine level of 1.3 mg/dL. The patient's blood pressure was stabilized, and her serum creatinine level was maintained at approximately 1.0 mg/dL over 2 years of follow up, with no additional events.
Fig. 1.
Clinical course showing markedly increased urine volume and decreased serum creatinine level with mildly stabilized blood pressure control after RAS. Cr, creatinine; PTRA, percutaneous transluminal renal artery angioplasty; SBP, systolic blood pressure; DBP, diastolic blood pressure; RAS, renal artery stenting.
Fig. 2.
Aortography showed severe ostial stenosis of the right renal artery (arrow) and suboccluded left renal artery (arrowhead) (A). RAS was performed after predilatation of balloon (C), and the right renal artery was expanded well (arrow) (D). Intravascular ultrasound imaging revealed obstructive deposition of heterogeneous intimal plaques with marked calcification before RAS (B) and adequate vessel dilatation of a minimal luminal diameter of 4.6 mm after RAS (E) at the ostium of the right renal artery. RAS, renal artery stenting.
Discussion
We report a patient with ARAS with rapidly worsening renal failure who exhibited dramatic improvement after RAS treatment. Several observational studies and reports of clinical experience have indicated the beneficial effects of renal arterial revascularization on blood pressure control, renal function, and mortality in patients with ARAS [3, 4]. However previous randomized clinical trials failed to show any benefits from adding RAS to the optimal medical treatment as compared with medical treatment only in patients with ARAS [1, 2]. The discrepancy of these results has made it difficult to choose the most appropriate treatment for patients with ARAS and resulted in ongoing discussions about the use of RAS for the treatment of ARAS-associated diseases. Several studies have indicated that rapid deterioration of renal function with bilateral ARAS or a solitary functioning kidney, marked elevation of blood pressure with ARAS, hemodynamically significant ARAS, renal arterial resistive index < 0.8, and absence of high-grade proteinuria may be related to the beneficial effects of RAS on renal function [5], [6], [7]. A rapid decline in renal function and low renal arterial resistive index have been reported to reflect a viable kidney and functional reversibility after renal artery intervention [3, 8]. Our case included some of these factors. The patient's renal failure based on bilateral ARAS rapidly declined within 1 week from renal function close to biochemical normalcy to anuria that required dialysis. In particular, the nontreated atrophic left kidney with suboccluded renal artery was presumed to be nearly nonfunctional. In our case, a history of acute clinical progression, bilateral ARAS, renal dynamics indicating a solitary functional kidney and significantly depressed resistive index were all factors that may indicate that our patient was the best candidate for RAS. In addition to achieving improvement in renal function, our patient was able to achieve good blood pressure control after RAS. Despite conflicting opinions, most studies have suggested that patients with ARAS could receive some benefit in blood pressure control after RAS, and the J-RAS study group suggested that a high systolic blood pressure >160 mmHg was a predictor for a benign response [1]. In addition to the factors mentioned above in our case, the existence of markedly elevated blood pressure may be another important factor in determining a responder to RAS. On the other hand, renal denervation, which has been clinically applied recently, should be considered as an optional treatment for patients with refractory hypertension. However, having severe ostial stenosis of the bilateral renal arteries, our patient was considered unsuitable for this procedure because of the difficulty in access of devices. In addition, due to the patient's contrast allergy, we used CO2 gas as contrast medium along with a minimal dose of iodinated medium. Consequently, she did not experience any serious anaphylactic reaction and also achieved marked improvement in renal function. This supports the suggestion that the use of CO2 for renal artery intervention is effective because of its lack of renal toxicity in patients with progressive renal failure [9]. However, one problem encountered with CO2 angiograms is the difficulty of obtaining a valuable image because of its buoyancy, as experienced in our case. Thus, posture changes, such as elevation of the side of the target vessel, are recommended [10]. In conclusion, we have presented a patient with ARAS who achieved dramatic recovery from accelerated renal failure and successful withdrawal from dialysis after RAS treatment. Improvement of renal failure was thought to be due to the fact there were several beneficial prognostic factors after RAS such as rapid clinical progress, bilateral ARAS, a solitary functional kidney, and low resistive index. When making the difficult decision about how to best manage ARAS, it is important to identify patients who will benefit most from RAS through a careful assessment of the patient's clinical course and examinations and to keep the procedure in mind as an available option for patients with ARAS.
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
References
- 1.Cooper C.J., Murphy T.P., Cutlip D.E., Jamerson K., Henrich W., Reid D.M., Cohen D.J., Matsumoto A.H., Steffes M., Jaff M.R., Prince M.R., Lewis E.F., Tuttle K.R., Shapiro J.I., Rundback J.H. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370:13–22. doi: 10.1056/NEJMoa1310753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bax L., Woittiez A.J., Kouwenberg H.J., Mali W.P., Buskens E., Beek F.J., Braam B., Huysmans F.T., Schultze Kool L.J., Rutten M.J., Doorenbos C.J. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med. 2009;150:840–848. doi: 10.7326/0003-4819-150-12-200906160-00119. [DOI] [PubMed] [Google Scholar]
- 3.Fujihara M., Yokoi Y., Abe T., Soga Y., Yamashita T., Miyashita Y., Nakamura M., Yokoi H., Ito S., J-RAS Study Investigators Clinical outcome of renal artery stenting for hypertension and chronic kidney disease up to 12 months in the J-RAS study – prospective, single-arm, multicenter clinical study. Circ J. 2015;79:351–359. doi: 10.1253/circj.CJ-14-0908. [DOI] [PubMed] [Google Scholar]
- 4.Miyashita Y., Ikeda U., Soga Y., Yokoi H., Suzuki K., Inoue N. Results of the retrospective analysis of renal artery stenting for the salvage of renal function study. Angiology. 2014;65:620–623. doi: 10.1177/0003319713501069. [DOI] [PubMed] [Google Scholar]
- 5.Hirsh A.T., Haskal Z.J., Hertzer N.R., Bakal C.W., Creager M.A., Halperin J.L., Hiratzka L.F., Murphy W.R., Olin J.W., Puschett J.B., Rosenfield K.A. ACC/AHA 2005 practice guidelines for the management of the patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic) Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 6.Mousa A.Y., AbuRahma A.F., Bozzay J., Broce M., Bates M. Update on intervention versus medical therapy for atherosclerotic renal artery stenosis. J Vasc Surg. 2015;61:1613–1623. doi: 10.1016/j.jvs.2014.09.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanjay M., Ankaj K., Jake A., William S.H., Stephen C.T., Michael A.M. Mortality and renal replacement therapy after renal artery stenting for atherosclerotic renovascular disease. J Vasc Interv Radiol. 2016;27:1215–1224. doi: 10.1016/j.jvir.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muray S., Martin M., Amoedo M.L., Garcia C., Jornet A.R., Vera M., Oliveras A., Gómez X., Craver L., Real M.I., García L., Botey A., Montanyà X., Fernández E. Rapid decline in renal function reflects reversibility and predicts the outcome after angioplasty in renal artery stenosis. Am J Kidney Dis. 2002;39:60–66. doi: 10.1053/ajkd.2002.29881. [DOI] [PubMed] [Google Scholar]
- 9.Liss P., Eklöf H., Hellberg O., Hägg A., Boström-Ardin A., Löfberg A.M., Olsson U., Orndahl P., Nilsson H., Hansell P., Eriksson L.G., Bergqvist D., Nyman R. Renal effects of CO2 and iodinated contrast media in patients undergoing renovasular intervention: a prospective, randomized study. J Vasc Interv Radiol. 2005;16:57–65. doi: 10.1097/01.RVI.0000144807.81633.79. [DOI] [PubMed] [Google Scholar]
- 10.Kyung J.C. Carbon dioxide angiography: Scientific principals and practice. Vasc Spec Int. 2015;31:67–80. doi: 10.5758/vsi.2015.31.3.67. [DOI] [PMC free article] [PubMed] [Google Scholar]