Abstract
Background
Gaining vascular access in children is challenging. Ultrasound-guided central line insertion in adults became the standard of care; however, its role in children is not clear. Our objective was to evaluate the ultrasound-guided Port-A-Cath or totally implanted long-term venous access device insertion in pediatric patients compared to the traditional approach.
Methods
This single-institution retrospective cohort study included 169 children who had port-A-catheters between May 2016 and Oct 2019. The patients were divided into two groups; group A included patients who had Port-A-Cath insertion using the landmark method (n = 117), and Group B included patients who had ultrasound-guided Port-A-Cath insertion (n = 52). Preoperative, operative, and postoperative data were collected and compared between the two groups. The study outcomes were operative time and catheter insertion-related complications.
Results
There was no significant difference in age or gender between both groups (P = .33 and .71, respectively). Eleven cases in group A and two cases in group B were converted to cut down technique because of difficulty in inserting the guidewire. There was no difference in the indication of the need for the port-A-Cath between both groups. The mean operative time for group A was 47 min and for group B was 41.7 min (P < .042). Two patients had intraoperative bleeding and hemothorax and required blood transfusion and chest tube insertion in group A. No statistically significant difference was found in the reported complications between the groups. However, the insertion-related complications were higher in group A (P = .053). No procedure-related mortality was reported.
Conclusions
Ultrasound-guided insertion of Port-A-Cath is an effective and safe technique with a reduction of failure rate. It should be considered the standard technique for Port-A-Cath insertion in the pediatric population.
Keywords: Port-A-Cath insertion, Landmark technique, Ultrasound-guided insertion
1. Introduction
Port-A-Cath (M.R.I.® LOW-PROFILE IMPLANTABLE PORT-BARD) facilitated the delivery of chemotherapy to cancer patients [1] by providing safe and long-term subcutaneous venous access.[2] In addition to chemotherapy, these catheters have several other applications with a low risk of infection and higher patient comfort.[3].
Traditionally, the insertion of Port-A-Cath is a blinded-procedure that depends on anatomical landmarks; [4] however, this approach increased the complication rate.[5,6] Ultrasound-guided Port-A-Cath placement increased the accuracy and success of the procedure and decreased the number of complications.[7] It was considered a top patient safety practice by the Agency for Healthcare Quality and Research (AHRQ)[8] and the United Kingdom’s National Institution of Clinical Excellence (NICE).[9] The ultrasound-guided approach became the standard of care of adult patients with a reduction of cannulation time, cost, and complications.[[10], [11], [12]].
Studies on ultrasound-guided Port-A-Cath insertion in pediatrics are deficient [13,14], and the traditional method remains the preferred approach, although there is no consensus on the standard approach.[15,16] Our objective was to evaluate the ultrasound-guided central line insertion in pediatric patients compared to the traditional method.
2. Patients and methods
2.1. Design and patients
This is a retrospective cohort study performed from May 2016 to October 2019. The medical files of 169 pediatric patients who had Port-A-Cath insertion at our institution were reviewed. The Institutional Review Board approved the study, and the patients’ consent was waived. All patients had Port-A-Cath insertion for malignancy. Port-A-Cath1 insertion was performed using the landmark technique in 117 patients and ultrasound-guided technique in 52 patients. Patients were grouped according to the insertion method into group A (Landmark technique) and group B (ultrasound-guided technique). We used the left internal jugular vein as the standard catheter access site (Fig. 1). A portable Sonosite M-Turbo® ultrasound system was used for determining the proper site for implantation (Fig. 2).
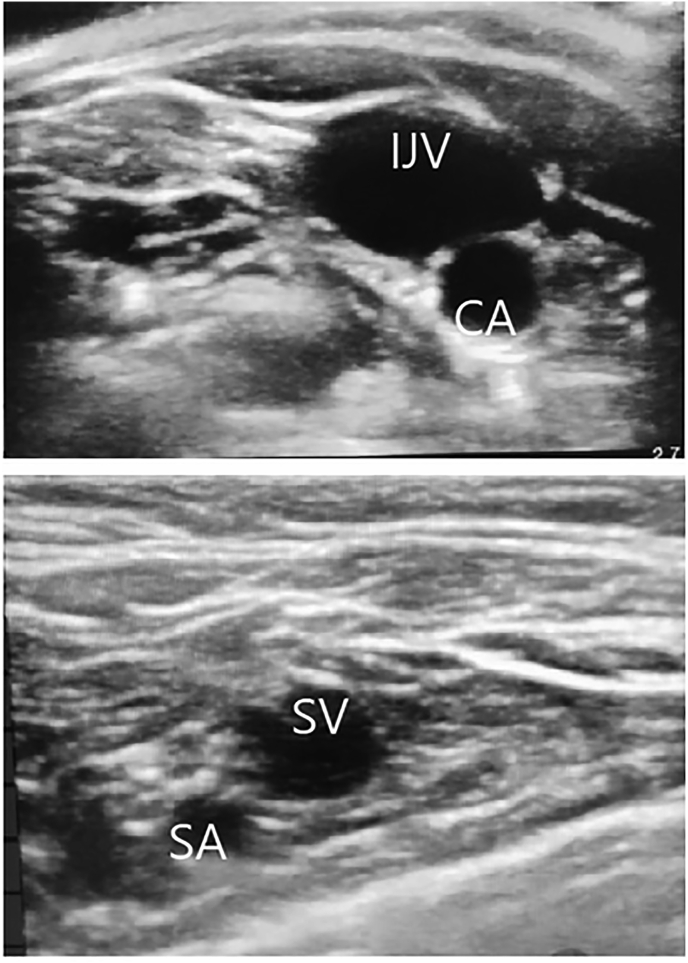
Fig. 1.
Ultrasound view of the internal jugular vein compared to the subclavian vein. (CA: carotid artery; IJV: internal jugular vein; SA: subclavian artery; SV: subclavian vein).
Fig. 2.
Ultrasound guided insertion of the a Port-A-Cath (CA: carotid artery; IJV: internal jugular vein; SCM: subcutaneous muscle). Arrow shows the tip of the needle in the vein.
2.2. Technique
General anesthesia was used in all patients. The head is turned away from the insertion site, and surgical draping for the neck and upper chest was done using chlorhexidine solution (ChloraPrep One-Step; Enturia, Leawood, Kansas). Then, the patients were placed in the Trendelenburg position. Local anesthesia was injected as an adjunctive to general anesthesia, and all patients received prophylactic antibiotics.
The choice of the vein depended on the surgeon’s preference, patient anatomy, and history of site use. In general, for the landmark insertion, we used the left subclavian vein (70%) as the first choice followed by the left internal jugular. For the ultrasound group, the left internal jugular was the first choice mainly because of easy accessibility followed by the left subclavian vein.
An ultrasound console (Sonosite) was used, and the probe was covered with a sterile bag containing gel. The probe was positioned at the apex of the sternomastoid triangle at the base of the neck, and the internal jugular vein and the common carotid artery were visualized. The vein is larger, more superficial, and compressible.
In the Landmark technique, we used the infra-clavicular approach; the needle entry was at the midclavicular point directed to supra-sternal notch. For the internal jugular vein, the needle entry was at the bifurcation of the sternocleidomastoid muscle directed to the nipple with a 30–45° angle.
The Seldinger technique was used to introduce the guidewire, and fluoroscopy was used to confirm the position of the wire and the extent of its distal end. The port was embedded in the subcutaneous tissue of the chest wall and tunneled under the skin. An introducer sheath was passed over the wire, the guidewire was then removed, and the catheter was introduced through the sheath.
The optimal position of the catheter tip is at the terminal part of the superior vena cava. A postoperative chest x-ray was not done routinely and was indicated if complications were suspected.
We used the left internal jugular vein more frequently because the risk of it coming out with the child’s growth is lower than the right side. Both techniques were performed by the same surgeons, and the first 30 cases were skipped for the learning curve. Additionally, all surgeons had training on manikins for five insertions before attempting insertion on patients.
2.3. Study outcomes and definitions
The study outcomes included complications of the insertion and include bleeding, pneumothorax, port infection and thrombus, and thrombosis of central veins.
The success in the use of Port-A-Cath was defined by the ability to infuse fluid and withdraw blood through it. The success rate was defined as the number of successful insertions with that technique divided by the total number of attempts for this method x100.
2.4. Statistical analysis
The data were analyzed using SPSS-25 statistical software (IBM Corp- Chicago- IL- USA), Chi-square or Fisher exact test was used to compare binary data, and independent T and Mann-Whitney U tests were used for numerical data. Description of continuous variables was done using average and standard deviation or median and (25th- 75th percentiles) binary variables with number and percent. A P-value of less than .05 was considered statistically significant.
3. Result
Male to female ratio was 1.48:1, the median age in group A was 5 (0.2–14) months versus 4.5 (0.2–13) months in group B, and there was no difference in age or sex ratio between groups (P = .33 and .71, respectively). There was no difference in the indication for catheter insertion characteristics between both groups (Table 1).
Table 1.
Preoperative and operative patients’ data.
| Variable | Anatomic Landmark Method (n = 117) | Ultrasound-Guidance method (n = 52) | P Value |
|---|---|---|---|
| Age (year) | 5.172 (3.49) | 4.62 (3.14) | .329 |
| Sex (female/male ratio) | 46/71 | 22/30 | .71 |
| Operative time (minutes) | 47 (16.3) | 41.7 (13.57) | .042 |
| Number of trials | 2.9 (1.8) | 2.2 (1.3) | .0125 |
| Indications: | |||
| Chemotherapy | (98) 83.8% | (44) 84.6% | .88 |
| Other | (19) 16.2% | (8) 15.4% | .88 |
| Malignancy: | |||
| Hematological | (77) 65.8% | (38) 73% | .34 |
| Solid organ tumor | (21) 17.9% | (14) 27% | .18 |
| Site of the insertion: | |||
| Left side | (106) 90.5% | (49) 94% | .43 |
| Left subclavian vein | (81) 76.4% | (8) 16.3% | <.001 |
| Left internal jugular | (25) 23.6% | (41) 83.6% | <.001 |
| Right side | (11) 9.4% | (3) 5.7% | .42 |
| First Port-A-Cath | (69) 58.9% | (33) 63.4% | .58 |
| 2nd Port-A-Cath | (37) 31.5% | (16) 30.8% | .91 |
| Third or more Port-A-Cath | (11) 9.4% | (3) 5.8% | .42 |
The majority of the patients (60.3%) had the first port-A-Cath insertion for the first time during this study period, and 39.7% had the first insertion outside our institution. Details of operative data are presented in Table 2. The mean operative time for group A was 47 min and for group B was 41.7 min. The operative time was significantly shorter in group B (P < .042).
Table 2.
Procedure complications.
| Variable | Anatomic Landmark Method (n = 117) | Ultrasound-Guidance method (n = 52) | P Value |
|---|---|---|---|
| Non | (90) 76.9% | (43) 82.6% | .39 |
| Bleedinga | (2) 0.8% | 0 | .34 |
| Pneumothorax (chest tube inserted) | (3) 2.6% | 0 | .24 |
| Arterial puncture | (2) 1.7% | 0 | .34 |
| Arterial insertion | (1) 0.85% | 0 | .5 |
| Conversion to cut down | (11) 9.4% | (2) 3.8% | .21 |
| Infection | (15) 12.8% | (7) 13.5% | .9 |
| Malfunction | (4) 3.4% | (2) 3.8% | .88 |
| Insertion-related complication | (8) 6.8% | 0 | .053 |
Bleeding require blood transfusion or chest tube insertion.
Two patients in group A had intraoperative bleeding and hemothorax and required blood transfusion and chest tube insertion. Eleven cases were converted to cut down technique in group A and two cases in group B because of difficulty in guidewire insertion. No statistically significant difference was found in the reported complications between groups. However, the insertion related complications were higher in group A (P value of .053). No procedure-related mortality was reported (Table 2).
4. Discussion
The administration of chemotherapeutic agents through a peripheral line is associated with various complications, [17] and Port-A-Cath provides vascular access for long-term use in those patients.[18] The use of the ultrasound-guided approach for cannulation of the center vein could be associated with reduced complication rates. [19] Repeated vein injection can lead to endothelial damage and increase the risk of thrombosis, [20] and the complication rate was found to be associated with the increased number of cannulations attempts, [21] with the highest complications occurred when three or more punctures were attempted. For this reason, we included the number of attempts as an outcome measure in our study. However, the use of ultrasound does not ensure successful cannulation from the first attempt as the veins in children are small and easily deformed. Additionally, the guidewire may not pass easily in the small veins, which warranted the use of a micropuncture introducer set.
In this study, the number of trials in group A was 2.9 (1.8) compare to 2.2 (1.3) in group B (P = .0125). The increased number of trials in group B may be related to early experience plus the difficult anatomy and small-caliber vein in young children and infants.
Ultrasound-guided central line insertion had demonstrated superior efficacy compared to the traditional method in several studies; [[22], [23], [24], [25], [26]] however, most studies were on adult patients, and studies on children are scarce. The study demonstrated a decrease in chest tube insertion and operative time when ultrasound was used (0 vs. 2.6%). These results are consistent with other studies that reported 0.4–2.8% chest tube insertion after central line placement.
In a study by Arul and coworkers on 500 pediatric patients, no pneumothoraces were reported [5]. Our results showed a higher insertion complication rate with the landmark technique (P = .052). Other studies demonstrated a reduction in insertion time, number of attempts, and failure rate when using ultrasound, [27] a finding that was confirmed in a randomized clinical trial.[28] In the current study, the operative time was lower (P = .042), and this reflects the efficiency of the technique. Additionally, the shorter operative time may indicate cost-effectiveness, as previously reported.[29].
We reported a success rate of 96.2% in the ultrasound-guided insertion group, which is comparable to what was reported in the literature (90–99.8%).[30,31] The success rate was lower in the landmark technique with accidental arterial puncture. The ultrasound-guided technique provides continuous visualization of the needle tip during insertion, which avoids arterial puncture and increases the safety of the procedure.
Ultrasound-guided insertion requires proper and sufficient training to achieve good results. We provided hands-on training to our physicians on manikins before using this technique. The learning curve for ultrasound-guided insertion in the pediatric population had not been evaluated, and the number of insertions to achieve a steady operative time has not been determined.[[32], [33], [34]] We have not evaluated the learning curve in our study, but the number of punctures has decreased over time, and all surgeons had five trials on manikins.
The internal jugular vein was the most commonly used because of the lower risk of pneumothorax and thrombosis [35,36]. The subclavian vein can be used, and it offers the advantages of fixed anatomy despite the increased risk of pneumothorax. In contrast, the use of the femoral vein is not recommended.[35] In this study, the left subclavian vein was used in 81 patients (76.4%) in the landmark group and in eight patients 1 (6.3%) in the ultrasound group. Visualization of the internal jugular vein was easier with the use of ultrasound. It could be useful to try using the external jugular vein followed by the internal jugular vein and then the subclavian vein; this is because the thrombosis of the subclavian vein renders the other two veins non-usable.
5. Study limitations
The major limitation is the retrospective nature of the study in which the outcomes can be affected by other variables than the technique itself. Another limitation is the single-center experience in which generalization of the findings may not be applicable. Additionally, the access site was different in both groups, which may have affected the results.
6. Conclusion
The ultrasound-guided central venous access is an efficient and safe technique to use in pediatric patients. It reduced the failure rate and the number of attempts when compared with the anatomic landmark technique. The technique is the recommended method of Port-A-Cath insertion in children.
Funding
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Biomedical Ethical Committee, Faculty of Medicine, Um Al Qura University (Institutional Review Number HAPO-02-K-012-2019-10-332).
Author statement
Osama Bawazir: Conceptualization, Methodology, Software. Abdullah Bawazir: Data curation, Writing- Original draft preparation, Visualization, Investigation. Osama Bawazir: Supervision, Software, Validation. Osama Bawazir: Writing- Reviewing and Editing.
Informed consent
Verbal consent was obtained from the parents of all patients included in the study.
Declaration of competing interest
Authors have no conflict of interests and the work was not supported or funded by any drug company and the authors declare that they have no competing interests.
Acknowledgements
I would like to express my deep gratitude to Miss Razan Bawazir for here valuable support on photo editing in this article.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
MRI Low-Profile Port-BARD
Supplementary data to this article can be found online at https://doi.org/10.1016/ijpam.2020.08.002.
Contributor Information
Osama A. Bawazir, Email: Oabawazir@uqu.edu.sa, obawazir@yahoo.com.
Abdullah Bawazir, Email: Abdoo.ksa.123@gmail.com.
Visual abstract
The following are the Supplementary data to this article:
Fig S1.
References
- 1.Poorter R.L., Lauw F.N., Bemelman W.A., Bakker P.J., Taat C.W., Veenhof C.H. Complications of an implantable venous access device (Port-a-Cath®) during intermittent continuous infusion of chemotherapy. Eur J Canc. 1996 Dec 1;32(13):2262–2266. doi: 10.1016/s0959-8049(96)00274-2. [DOI] [PubMed] [Google Scholar]
- 2.Ku Y.H., Kuo P.H., Tsai Y.F., Huang W.T., Lin M.H., Tsao C.J. Port-A-Cath implantation using percutaneous puncture without guidance. Ann Surg Oncol. 2009 Mar 1;16(3):729–734. doi: 10.1245/s10434-008-0224-4. [DOI] [PubMed] [Google Scholar]
- 3.Gross J.B. American society of anesthesiologists task force on perioperative management: practice guidelines for the perioperative management of patients with obstructive sleep apnea: a report by the American society of anesthesiologists task force on perioperative management of patients with obstructive sleep apnea. Anesthesiology. 2006;104:1081–1093. doi: 10.1097/00000542-200605000-00026. [DOI] [PubMed] [Google Scholar]
- 4.Palepu G.B., Deven J., Subrahmanyam M., Mohan S. Impact of ultrasonography on central venous catheter insertion in intensive care. Indian J Radiol Imag. 2009 Aug;19(3):191. doi: 10.4103/0971-3026.54877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arul G.S., Lewis N., Bromley P., Bennett J. Ultrasound-guided percutaneous insertion of Hickman lines in children. Prospective study of 500 consecutive procedures. J Pediatr Surg. 2009 Jul 1;44(7):1371–1376. doi: 10.1016/j.jpedsurg.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Chuan W.X., Wei W., Yu L. A randomized-controlled study of ultrasound prelocation vs anatomical landmark-guided cannulation of the internal jugular vein in infants and children. Pediatric Anesthesia. 2005 Sep;15(9):733–738. doi: 10.1111/j.1460-9592.2004.01547.x. [DOI] [PubMed] [Google Scholar]
- 7.Balls A., LoVecchio F., Kroeger A., Stapczynski J.S., Mulrow M., Drachman D. Ultrasound guidance for central venous catheter placement: results from the central line emergency access registry database. Am J Emerg Med. 2010 Jun 1;28(5):561–567. doi: 10.1016/j.ajem.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Shekelle P.G., Wachter R.M., Pronovost P.J., Schoelles K., McDonald K.M., Dy S.M. Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Evid Rep Technol Assess. 2013 Mar;(211):1. [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute for Clinical Excellence Guidance on the use of ultrasound locating devices for placing central venous catheters. Technology Appraisal Guidance No. September 2002;49 [Google Scholar]
- 10.Brass P., Hellmich M., Kolodziej L., Schick G., Smith A.F. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015;(1) doi: 10.1002/14651858.CD011447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bowen M.E., Mone M.C., Nelson E.W., Scaife C.L. Image-guided placement of long-term central venous catheters reduces complications and cost. Am J Surg. 2014 Dec 1;208(6):937–941. doi: 10.1016/j.amjsurg.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Mehta N., Valesky W.W., Guy A., Sinert R. Systematic review: is real-time ultrasonic-guided central line placement by ED physicians more successful than the traditional landmark approach? Emerg Med J. 2013 May 1;30(5):355–359. doi: 10.1136/emermed-2012-201230. [DOI] [PubMed] [Google Scholar]
- 13.Sigaut S., Skhiri A., Stany I., Golmar J., Nivoche Y., Constant I., Murat I., Dahmani S. Ultrasound guided internal jugular vein access in children and infant: a meta-analysis of published studies. Pediatric Anesthesia. 2009 Dec;19(12):1199–1206. doi: 10.1111/j.1460-9592.2009.03171.x. [DOI] [PubMed] [Google Scholar]
- 14.Lamperti M., Cortellazzi P., Caldiroli D. Ultrasound-guided cannulation of IJV in pediatric patients: are meta-analyses sufficient? Paediatr Anaesth. 2010;20(4):373–374. doi: 10.1111/j.1460-9592.2010.03276.x. [DOI] [PubMed] [Google Scholar]
- 15.Gurien L.A., Blakely M.L., Russell R.T. Real-time ultrasonography for placement of central venous catheters in children: a multi-institutional study. Surgery. 2016;160(6):1605–1611. doi: 10.1016/j.surg.2016.05.019. [DOI] [PubMed] [Google Scholar]
- 16.Sømme S., Bronsert M., Morrato E., Ziegler M. Frequency and variety of inpatient pediatric surgical procedures in the United States. Pediatrics. 2013 Dec 1;132(6):e1466–e1472. doi: 10.1542/peds.2013-1243. [DOI] [PubMed] [Google Scholar]
- 17.Nosher J.L., Bodner L.J., Ettinger L.J., Siegel R.L., Gribbin C., Asch J. Radiologic placement of a low profile implantable venous access port in a pediatric population. Cardiovasc Intervent Radiol. 2001 Dec 1;24(6):395–399. doi: 10.1007/s00270-001-0071-1. [DOI] [PubMed] [Google Scholar]
- 18.Vescia S., Baumgärtner A.K., Jacobs V.R., Kiechle-Bahat M., Rody A., Loibl S. Management of venous port systems in oncology: a review of current evidence. Ann Oncol. 2008 Jan 1;19(1):9–15. doi: 10.1093/annonc/mdm272. [DOI] [PubMed] [Google Scholar]
- 19.Yip D., Funaki B. Subcutaneous chest ports via the internal jugular vein. Acta Radiol. 2002;43:371–375. doi: 10.1080/j.1600-0455.2002.430405.x. [DOI] [PubMed] [Google Scholar]
- 20.Gebauer B., Teichgräber U.M., Werk M., Beck A., Wagner H.J. Sonographically guided venous puncture and fluoroscopically guided placement of tunneled, large-bore central venous catheters for bone marrow transplantation—high success rates and low complication rates. Support Care Canc. 2008 Aug 1;16(8):897–904. doi: 10.1007/s00520-007-0378-9. [DOI] [PubMed] [Google Scholar]
- 21.Hind D., Calvert N., McWilliams R., Davidson A., Paisley S., Beverley C. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003 Aug 14;327(7411):361. doi: 10.1136/bmj.327.7411.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson E.M., Saltzman D.A., Suh G., Dahms R.A., Leonard A.S. Complications and risks of central venous catheter placement in children. Surgery. 1998 Nov 1;124(5):911–916. [PubMed] [Google Scholar]
- 23.Fragou M., Gravvanis A., Dimitriou V., Papalois A., Kouraklis G., Karabinis A. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Read Online: Critical Care Medicine| Society of Critical Care Medicine. 2011 Jul 1;39(7):1607–1612. doi: 10.1097/CCM.0b013e318218a1ae. [DOI] [PubMed] [Google Scholar]
- 24.Hayashi H., Amano M. Does ultrasound imaging before puncture facilitate internal jugular vein cannulation? Prospective randomized comparison with landmark-guided puncture in ventilated patients. J Cardiothorac Vasc Anesth. 2002;16(5):572–575. doi: 10.1053/jcan.2002.126950. [DOI] [PubMed] [Google Scholar]
- 25.Denys B.G., Uretsky B.F., Reddy P.S. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmarkguided technique. Circulation. 1993;87(5):1557–1562. doi: 10.1161/01.cir.87.5.1557. [DOI] [PubMed] [Google Scholar]
- 26.Turker G., Kaya F.N., Gurbet A., Aksu H., Erdogan C., Atlas A. Internal jugular vein cannulation: an ultrasound-guided technique versus a landmark-guided technique. Clinics. 2009;64(10):989–992. doi: 10.1590/S1807-59322009001000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verghese S.T., McGill W.A., Patel R.I., Sell J.E., Midgley F.M., Ruttimann U.E. Ultrasound-guided internal jugular venous cannulation in infants A prospective comparison with the traditional palpation method. Anesthesiology. 1999 Jul 1;91(1):71–77. doi: 10.1097/00000542-199907000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Bruzoni M., Slater B.J., Wall J., St Peter S.D., Dutta S. A prospective randomized trial of ultrasound-vs landmark-guided central venous access in the pediatric population. J Am Coll Surg. 2013 May 1;216(5):939–943. doi: 10.1016/j.jamcollsurg.2013.01.054. [DOI] [PubMed] [Google Scholar]
- 29.Calvert N., Hind D., McWilliams R., Davidson A., Beverley C.A., Thomas S.M. Ultrasound for central venous cannulation: economic evaluation of cost-effectiveness. Anaesthesia. 2004 Nov;59(11):1116–1120. doi: 10.1111/j.1365-2044.2004.03906.x. [DOI] [PubMed] [Google Scholar]
- 30.Tercan F., Oguzkurt L., Ozkan U., Eker H.E. Comparison of ultrasonography-guided central venous catheterization between adult and pediatric populations. Cardiovasc Intervent Radiol. 2008;31(3):575–580. doi: 10.1007/s00270-008-9315-7. [DOI] [PubMed] [Google Scholar]
- 31.Froehlich C.D., Rigby M.R., Rosenberg E.S., Li R., Roerig P.L., Easley K.A. Ultrasound-guided central venous catheter placement decreases complications and decreases placement attempts compared with the landmark technique in patients in a pediatric intensive care unit. Crit Care Med. 2009;37(3):1090–1096. doi: 10.1097/CCM.0b013e31819b570e. [DOI] [PubMed] [Google Scholar]
- 32.Fosh B., Canepa M., Eaton M. Long-term venous access insertion: ’the learning curve. ANZ J Surg. 2016;86(12):1038–1041. doi: 10.1111/ans.13338. [DOI] [PubMed] [Google Scholar]
- 33.Omid M., Rafiei M.H., Hosseinpour M., Memarzade M., Riahinejad M. Ultrasound-guided percutaneous central venous catheterization in infants: learning curve and related complications. Adv Biomed Res. 2015;4 doi: 10.4103/2277-9175.166135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bayci A.W., Mangla J., Jenkins C.S., Ivascu F.A., Robbins J.M. Novel educational module for subclavian central venous catheter insertion using real-time ultrasound guidance. J Surg Educ. 2015 Nov 1;72(6):1217–1223. doi: 10.1016/j.jsurg.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 35.Gonda S.J., Li R. Principles of subcutaneous port placement. Tech Vasc Intervent Radiol. 2011;14(4):198–203. doi: 10.1053/j.tvir.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 36.Miccini M., Cassini D., Gregori M., Gazzanelli S., Cassibba S., Biacchi D. Ultrasound-guided placement of central venous port systems via the right internal jugular vein: are chest x-ray and/or fluoroscopy needed to confirm the correct placement of the device? World J Surg. 2016;40(10):2353–2358. doi: 10.1007/s00268-016-3574-2. [DOI] [PubMed] [Google Scholar]