Abstract
Objective
Extensive research has demonstrated high prevalences of post-traumatic stress disorder (PTSD) and major depression (MD) in war-surviving populations. However, absolute estimates are lacking, which may additionally inform policy making, research and healthcare. We aimed at estimating the absolute global prevalence and disease burden of adult survivors of recent wars (1989–2019) affected by PTSD and/or MD.
Methods
We conducted a systematic literature search and meta-analysis of interview-based epidemiological surveys assessing the prevalence of PTSD and/or MD in representative samples from countries with a recent war history (1989–2019). Drawing on the war definition and geo-referenced data of the Uppsala Conflict Database Programme and population estimates of the United Nations for 2019, we extrapolated the meta-analytic results to absolute global numbers of affected people. Drawing on disability-adjusted life years (DALYs) data of the Global Burden of Diseases Study 2019, we further calculated the PTSD-associated and MD-associated DALYs.
Results
Twenty-two surveys (N=15 420) for PTSD, 13 surveys for MD (N=9836) and six surveys on the comorbidity of PTSD and MD (N=1131) were included. Random effects meta-analyses yielded point prevalences of 26.51% for PTSD and 23.31% for MD. Of those affected by PTSD, 55.26% presented with comorbid MD. Prevalence rates were not significantly associated with war intensity and length, time since war, response rate or survey quality. The extrapolation yielded 316 million adult war-survivors globally who suffered from PTSD and/or MD in 2019. War-survivors were almost exclusively living in low/middle-income countries (LMICs) and carried a burden of 3 105 387 and 4 083 950 DALYs associated with PTSD and MD, respectively.
Conclusions
Since LMICs lack sufficient funding and qualified professionals to provide evidence-based psychological treatments for such large numbers of affected people, alternative and scalable strategies using existing resources in primary care and communities are required. Research is required to assist upscaling.
Keywords: epidemiology, mental health & psychiatry, public health, traumatology, treatment
Key questions.
What is already known?
Several meta-analyses of epidemiological surveys have demonstrated high prevalences of post-traumatic stress disorder (PTSD) and major depression (MD) in war-surviving populations.
However, absolute global estimates of prevalence and disease burden are lacking.
Estimates in absolute numbers may inform policy making, research and healthcare beyond percentages.
What are the new findings?
In this systematic review and meta-analysis that included 41 surveys, random effects meta-analyses yielded a point prevalence of 26.51% for PTSD and 23.31% for MD.
Of those affected by PTSD, 55.26% presented with comorbid MD.
The extrapolation yielded about 316 million adult war survivors who experienced PTSD and/or MD in 2019 residing in 43 war-ridden countries with a war history between 1989 and 2019 (almost exclusively low/middle-income countries (LMICs)).
PTSD and MD were associated with about 3 million and 4 million disability-adjusted life years, respectively.
What do the new findings imply?
The number of war survivors experiencing PTSD and/or MD creates a massive mental health burden, which is primarily borne by LMICs.
Tailored approaches for LMICs contexts are necessary to address the presented vast mental health burden.
Low-cost and scalable solutions that build on available resources are recommended as well as multidisciplinary research to guide evidence-based upscaling.
The findings generally illustrate the importance of peace-building and maintenance.
Introduction
Meta-analyses demonstrate high prevalence rates of post-traumatic stress disorder (PTSD) and major depression (MD) in war-affected populations with pooled estimates ranging from 15.3% to 30.6% for PTSD and 10.8% to 30.8% for MD.1–4 However, there is a lack of prevalence estimates and disease burden estimates in absolute numbers. Such absolute estimates are important for three major reasons. First, war affects large populations globally: between 1989 and 2019, about one-sixth of the global population have experienced war within their country of residence.5 6 Second, absolute numbers add clarity to the scope of war-related mental health burdens and, as such, inform policy making, healthcare and research beyond relative estimates. Third, countries with a recent history of war are almost exclusively low/middle-income countries (LMICs) with limited healthcare resources.7 Absolute estimates may reveal particular challenges for mental healthcare in LMICs settings and inform tailored approaches. All previous meta-analyses partly or exclusively involved specific populations precluding extrapolations to general war-surviving populations.
Against this background, we aimed to estimate the absolute global number of war survivors with PTSD and/or MD, as well as the absolute associated disease burden. For this, we conducted a systematic literature search and meta-analysis on high-quality epidemiological surveys conducted in countries with a history of war within their own territory between 1989 and 2019, and extrapolated results to absolute numbers and the associated disability-adjusted life years (DALYs) as a measure of disease burden.
Methods
Definition of war and war-afflicted country
We used the definition of war and geo-referenced war-data from the Uppsala Conflict Data Programme (UCDP) from the Department of Peace and Conflict Research of the Uppsala University.5 The UCDP supplies geo-referenced war data from 1989 to 2019. Based on the geo-referenced data, we classified war in four countries (ie, India, Israel, Russia and Ukraine) as regional rather than nationally distributed (see https://ucdp.uu.se/) which was relevant for the accuracy of extrapolations, which are described in more detail elsewhere.6
Systematic literature search
Up until September 2017, we relied on our previous systematic literature search with identical search strategy,2 which we pre-registered in the PROSPERO database (ID: CRD42016032720; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=32720). However, for the present report, we excluded surveys that were not representative of general populations. A new systematic literature search was conducted in Medline, PsycINFO and PTSDpubs between 1 August 2017 up until 15 January 2021 (see detailed search strategy in online supplemental eList 1). We conducted the systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.8 Two authors (THH, IV) independently conducted all search steps (eg, duplicate detection, title and abstract screen, full-text screen) as well as all following steps (eg, data extraction, risk of bias assessment); regular meetings between three authors (THH, IV and NM) were held to discuss disagreements. Inclusion and exclusion criteria were set to maximise representativeness of general war surviving populations and, therefore, to allow for extrapolations. Epidemiological surveys were eligible if they met all of the following inclusion criteria: (1) conducted after the first year of war in a country with a history of war between 1989 and 2019 as defined by the UCDP; (2) using a random sampling technique to draw a representative sample from the general population; (3) including at least 50 participants; (4) at least 80% of the participants were aged 18 years or older and (5) PTSD and/or MD were measured with a (semi-)structured interview based on the diagnostic criteria reported in any version of the Diagnostic and Statistical Manual for Mental Disorders (DSM) or the International Statistical Classification of Diseases (ICD). There were no restrictions in terms of language or population (other than the mentioned inclusion criteria). In line with the inclusion criterion 2, surveys were excluded if they were conducted in an area with particularly high or low war intensity as compared with the rest of the country, indicated by geo-referenced UCDP data, or if surveys involved help-seeking populations. We also reviewed relevant secondary literature (see PRISMA flow chart; figure 1)1 4 6 9 10 as well as reference lists of eligible articles. Since all relevant data were reported in the eligible surveys, no contact with authors of primary literature was necessary.
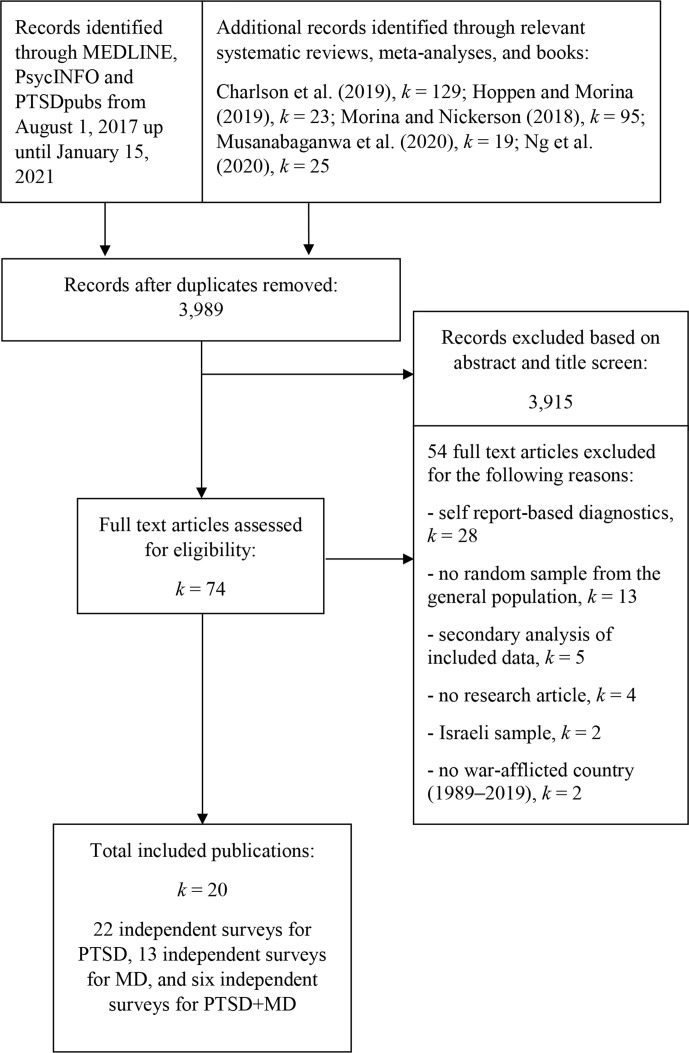
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of study selection. MD, major depression; PTSD, post-traumatic stress disorder.
bmjgh-2021-006303supp001.pdf (217.6KB, pdf)
Coding of survey information
The main outcome was the point prevalence of PTSD, MD and their comorbidity. We further extracted relevant data for the planned moderator analyses (see later).
Quality assessment
We assessed the quality of included surveys with a scale that we had developed previously.2 The scale is based on the recommendations reported in the Strengthening the Reporting of Observational Studies in Epidemiology guidelines and related meta-analyses,11–13 and consists of six quality items (see online supplemental eTable 1). Two authors (THH, IV) independently rated the quality of included trials on the applicable items with 73% agreement. All disagreements were solved through discussions between three authors (THH, IV and NM). A quality sum score of percentage of the possible sum score was created for each survey since they differed on the number of applicable quality items.
Meta-analysis
We conducted random effects meta-analyses on Freeman-Tukey double arcsine transformed prevalence proportions using the inverse variance method.14 We used the packages meta (V.4.16-2)15 and metafor (V.2.4-0)16 in R (V.3.6.1).17 To calculate 95% CIs for individual studies in the forest plots, we used the Agresti-Coull interval.18 Q-statistics and the I²-statistics were calculated to get an estimate of homogeneity in effect sizes. The latter indicates the degree of heterogeneity in percentages. We estimated the between-study variance by calculating τ²-statistics via the restricted maximum likelihood method.19 To analyse the potential effects of outliers, we defined outliers as prevalence proportions that were at least 3.3 SD above or below the pooled prevalence proportion and aimed to supply outlier-adjusted results.20 To analyse potential publication bias, we visually inspected funnel plots and performed Egger’s test of asymmetry.21 As recommended,22 we did this only in the presence of at least 10 independent estimates. In case of detected asymmetry, we used the trim and fill method, which supplies asymmetry-adjusted results by introducing additional hypothetical studies.23 To statistically control for effects of potentially moderating variables (ie, total war deaths, war deaths per 100.000 population, total conflict-related deaths, conflict-related deaths per 100.000, war lengths in years, years since end of war and conduct of survey, response rate, quality of survey, mean age, % females, % in a relationship, % in employment and continent) on prevalence proportions, we planned to perform univariate mixed-method meta-regressions if enough independent surveys reported on the given information (ie, k≥10).19 Data on country-specific war intensity, conflict intensity and war length (accumulative for 1989–2019) was retrieved from the UCDP (https://ucdp.uu.se/). Since there was more than one survey for some countries which experienced multiple wars (Rwanda, Kosovo, Democratic Republic of the Congo, and Palestine for PTSD; Rwanda and Kosovo for MD), we merged cases and non-cases per country for these specific moderator analyses. Some planned moderator analyses (intervention utilisation, non-war-related trauma history) were precluded since these variables were either not assessed or assessed too heterogeneously (differences in defining and assessing mean number of traumatic events per trauma type, breadth of assessed trauma history) to allow for the planned moderator analyses.
Population estimates, extrapolation and income groups
For all nationally distributed wars, we relied on population estimates of the Population Division of the Department of Economic and Social Affairs (DESA) of the United Nations.24 Since people who were very young during war might not be able to remember exposure to war-related events,25 we only extrapolated data on adults who were at least 6 years old at the time of the war. Countries where only specific regions were affected by war were: India (Punjab, Nagaland, Kashmir, Assam and Manipur), Ukraine (Donetsk People’s Republik, Kharkiv Oblast, Luhansk People’s Republic, Zaporizhzhia Oblast and Dnipropetrovsk Oblast), Israel (Gaza strip and West Bank) and Russia (Chechnya). For regional wars, we relied on national consensus data and World Bank population data since DESA does not supply age-grouped regional population estimates. Definitions of LMICs were based on the World Bank classifications (ie, gross national income per capita of less than US$12 536).26
Disease burden estimate
To estimate the associated disease burden of the global number of war survivors with PTSD and MD, we replied on country-specific DALYs estimates published in the last iteration of the Global Burden of Diseases (GBD) study; the GBD 2019.27 Since the GBD 2019 does not report on PTSD data separately, the estimate for all anxiety disorders was used. Total country DALYs for PTSD and all anxiety disorders were retrieved, divided by the total country population and subsequently multiplied by the retrieved number of adult war survivors.
Results
Article synthesis
The PRISMA flowchart in figure 1 shows an overview of the survey synthesis. Of the initial 3989 records identified, 74 full texts remained after the title and abstract screen for eligibility. After thorough screening of the 74 full texts, a total of 20 eligible publications were included in the present meta-analysis reporting on 22 independent surveys (N=15 420) for PTSD from 12 countries and 3 continents, 13 independent surveys (N=9836) for MD from 9 countries and 3 continents, and 6 independent surveys (N=1131) for PTSD and comorbid MD from 6 countries and 2 continents.
Characteristics of included studies
An overview of the characteristics of included surveys is provided in table 1. On average, surveys assessed PTSD and/or MD 6.88 years (weighted mean; SD=5.88) after the end of warfare. War intensity and lengths varied considerably across countries. Survey response rates were high with a weighted mean of 88.91% (SD=11.10). Most surveys used mental health professionals as interviewers who were trained for the purpose of the survey. The most frequently used interview measure was the Mini International Neuropsychiatric Interview28 for both PTSD and MD. Quality of surveys was moderate overall with a weighted mean of 34.92% (SD=10.94) of the maximum attainable quality sum scores. None of the included surveys involved a formal psychometric validation of translated measures.
Table 1.
Characteristics of eligible epidemiological surveys included in the meta-analysis
| Publication | Country | Years since war* | War-related deaths 1989–2019† (per 100.000) | Conflict-related deaths 1989–2019 ‡ | Lengths of war(s) in years 1989–2019 | N | Random sampling technique used | Response rate in % | PTSD assessment | MD assessment | Expertise and training of interviewers | Quality of survey in %§ |
| Ayazi et al53 | Sudan | 5 | 51 837 (118.22) | 93 133 | 20 | 1200 | Multistage random cluster sampling | 95 | NA | MINI | Local health personnel, 9 days of training | 41.67 |
| Canetti et al54 | Palestine | 0 | 1708 (33.48) | 1710 | 1 | 1196 | Stratified 3-stage cluster random sampling | 62.9 | PSS-I | NA | Trained interviewers not otherwise specified | 25.00 |
| de Jong et al55 | Algeria | 6 | 18 920 (43.15) | 21 153 | 6 | 653 | Random sample of population based on governmental registries | 76.7 | CIDI | NA | n.r. | 25.00 |
| Palestine | 0 | s.a. | s.a. | s.a. | 585 | 4-stage random sampling strategy | 98 | CIDI | NA | n.r. | 33.33 | |
| Eytan et al56 | Kosovo | 2 | 1898 (106.10) | 2847 | 2 | 996 | Random sampling from eight municipalities | 93 | MINI | NA | Local psychosocial counsellors, trained by authors | 41.67 |
| Fodor et al57 | Rwanda | 17 | 6749 (52.11) | 516 805 | 1 | 465 | Probability proportional to size sampling based on census data | 96 | NA | MINI | Experienced Rwandan college graduates, 1 week of training | 50.00 |
| Johnson et al58 | Liberia | 4 | 3048 (60.26) | 23 245 | 1 | 1661 | Combination of systematic random sampling and 40×40 cluster sampling | 98.2 | PSS-I | NA | Liberian public health graduates and community health workers, several days of training | 41.67 |
| Johnson et al59 | DRC | 0 | 28 637 (31.97) | 114 888 | 7 | 989 | Systematic cluster sampling strategy | 98.9 | PSS-I | NA | Experienced Congolese interviewers, several days of training | 58.33 |
| Madianos et al60 | Palestine | 0 | s.a. | s.a. | s.a. | 916 | Multistage sample in four areas of West Bank | 92 | SCID | SCID | Second author (native to West Bank), training through pilot interviews | 50.00 |
| Morina and Ford61 | Kosovo | 6 | s.a. | s.a. | s.a. | 102 | Random sample of civilians, random walk technique | 81 | MINI | MINI | Psychology students trained by the first author | 25.00 |
| Morina et al62 | Kosovo | 6 | s.a. | s.a. | s.a. | 84 | Random walk technique in the region of Drenica | 90 | MINI | NA | Psychology students trained by the first author | 41.67 |
| Morina et al63 | Kosovo | 8 | s.a. | s.a. | s.a. | 163 | Random walk technique in different regions | 90.1 | MINI | MINI | Psychology students trained by the first author | 31.25 |
| Mugisha et al64 | Uganda | 7 | 9970 (21.80) | 17 034 | 3 | 2361 | Multistage sampling, random selection of parishes from selected subcounties | n.r. | MINI | MINI | Psychiatric nurses trained for this study | 18.75 |
| Munyandamutsa et al65 | Rwanda | 14 | s.a. | s.a. | s.a. | 962 | Multistage random sampling procedure | n.r. | MINI | MINI | Psychologists, social workers and physicians, 20 hours of training | 18.75 |
| Priebe et al66 | Croatia | 13 | 3091 (31.98) | 1478 | 1 | 727 | Multistage probabilistic sampling frame and random-walk technique | 70 | MINI | MINI | Trained mental health professionals or trainees | 31.25 |
| Kosovo | 8 | s.a. | s.a. | s.a. | 648 | Multistage probabilistic sampling frame and random-walk technique | 91 | MINI | MINI | Trained mental health professionals or trainees | 43.75 | |
| Serbia | 13 | 5806 (66.45) | 7267 | 3 | 637 | Multistage probabilistic sampling frame and random-walk technique | 70.1 | MINI | MINI | Trained mental health professionals or trainees | 31.25 | |
| Bosnia and Herze-govina | 13 | 13 440 (409.65) | 26 333 | 4 | 640 | Multistage probabilistic sampling frame and random-walk technique | 85 | MINI | MINI | Trained mental health professionals or trainees | 43.75 | |
| Rieder et al67 | Rwanda | 16 | s.a. | s.a. | s.a. | 172 | Random sampling in Muhanga district | n.r. | PSS-I | NA | Experienced local bachelor-level psychologists | 16.67 |
| Rugema et al68 | Rwanda | 17 | s.a. | s.a. | s.a. | 917 | Two-stage random sampling | 99.8 | MINI | MINI | Experienced clinical psychologists, several days of training | 31.25 |
| Schaal et al69 ** | Rwanda | 15 | s.a. | s.a. | s.a. | 112 | Random community sample of Butare and Kigali | 97 | PSS-I | NA | Masters-level and clinical psychologists, extensive previous training | 41.67 |
| Somasundaram and Sivayokan70 | Sri Lanka | 4 | 61 265 (286.11) | 65 628 | 15 | 98 | Random sampling procedure in a suburb of Jaffna | 97 | SIQ | SIQ | Trained medical students | 31.25 |
| Veling et al71 | DRC | 0 | s.a. | s.a. | s.a. | 93 | Balanced sampling to 12 quarters of Bunia | n.r. | CIDI | NA | Trained local interviewers | 25.00 |
| Yasan et al72 | Turkey | 9.8 | 26 981 (31.99) | 28 611 | 9 | 708 | Random sampling of regions in Diyarbakir, proportionate sample of residents | 98.3 | CAPS | NA | Final-year psychology students trained by psychiatry professors | 41.67 |
| Summary (ie, sum or weighted/unweighted mean (SD) or most prevalent option) | 12 countries+Palestine from 3 continents | 6.88 (5.88) | Total: 17 813 (18 807)¶ Per 100.000: 99.48 (112.16) |
70 779 (133,300)¶ | 3.92 (4.83)¶ | 17 085 | (Multistage) random sampling procedure | 88.91 (11.10) | MINI | MINI | Mental health professionals with specific training for the used interview | 34.92 (10.94) |
*Timespan in years between the end of war and the time the respective survey was conducted.
†Number of war-related death (ie, state-based violence) in the respective country with a history of war between 1989 and 2019 as defined by Uppsala Conflict Data Programme (UCDP).5 Retrieved from: https://ucdp.uu.se/.
‡Number of all conflict-related death (ie, state-based violence+non-state violence+one-sided violence) in the respective country with a history of war between 1989 and 2019 as defined by the UCDP.
§As assessed with Strengthening the Reporting of Observational Studies in Epidemiology criteria.11
¶To calculate these unweighted means and SDs, country-specific data were considered once per country.
**Only representative sample included.
CAPS, Clinician-Administered PTSD Scale; CIDI, Composite International Diagnostic Interview; DRC, Democratic Republic of Congo; MD assessment, used (semi-)structured interview based on Diagnostic and Statistical Manual of Mental Disorders (DSM) or International Statistical Classification of Diseases (ICD) diagnostic criteria to assess major depression; MINI, Mini International Neuropsychiatric Interview; n, included amount of subjects in the given survey; NA, not applicable; n.r., not reported; PSS-I, Post-traumatic Symptom Scale Interview; PTSD assessment, used (semi-)structured interview based on Diagnostic and Statistical Manual of Mental Disorders (DSM) or International Statistical Classification of Diseases (ICD) diagnostic criteria to assess post-traumatic stress disorder; s.a., see intensity/lengths of war for the respective country above; SCID, Structured Clinical Interview for DSM-IV; SIQ, Stress Impact Questionnaire.
Meta-analytic results
Prevalence of PTSD and MD
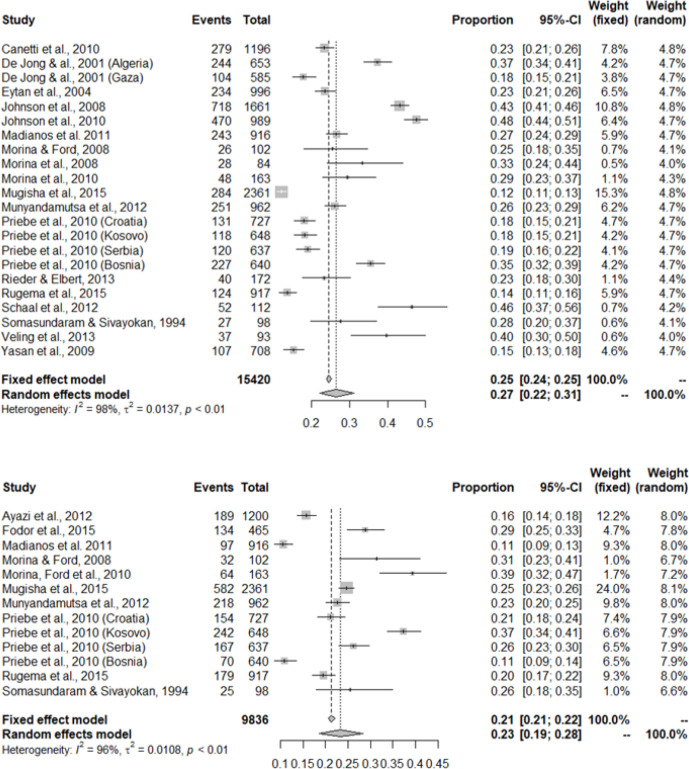
Figure 2 shows forest plots of prevalence of PTSD and MD in the included surveys. Random effects models yielded a pooled point prevalence of 26.51% (k=22, 95% CI 22.17 to 31.10) for PTSD. Heterogeneity was large (I2=98%, Q=1057.13, p<0.001). No statistical outliers were observed. The funnel plot (see online supplemental eFigure 1) and Egger’s test of asymmetry (t=0.77, p=0.453) did not indicate publication bias. For MD, the random effects model yielded a pooled point prevalence of 23.31% (k=13, 95% CI 18.55 to 28.42) with large heterogeneity (I2=96.1%, Q=310.72, p<0.001). No statistical outliers were observed. Again, the funnel plot (see online supplemental eFigure 2) and Egger’s test of asymmetry (t=0.77, p=0.457) did not indicate publication bias. For the comorbidity between PTSD and MD, the random effects model yielded a pooled point prevalence of 55.26% (k=6, 95% CI 42.11 to 68.05) with large heterogeneity (I2=95.6%, Q=113.39, p<0.001; see the corresponding forest plot in online supplemental eFigure 3). No statistical outliers were observed. We used pooled point prevalence in the extrapolation to absolute numbers.
Figure 2.
Forest plots for point prevalence of post-traumatic stress disorder (top) and major depression (bottom).
Moderator results
In the meta-regressions on prevalence of PTSD and MD, none of the analysed potential moderators was found to be significantly related (see online supplemental eTable 2). Meta-regressions for comorbidity point prevalence were precluded (k<10).
Extrapolation to absolute numbers and DALYs
Table 2 shows point prevalence estimates for PTSD, MD and their comorbidity per country as well as globally. We estimate that a total of 854 653 860 adult war survivors were alive in 2019 and resided in one of 43 countries which experienced at least one war between 1989 and 2019. Of these, 849 754 461 were residing in LMICs. Based on the meta-analytic summary of epidemiological surveys, the extrapolation yielded that, in 2019, about 227 million adult war survivors globally experienced PTSD (95% CI 189 476 761 to 265 797 350) and about 199 million experienced MD (95% CI 158 538 291 to 242 892 627). Based on the meta-analytic results on comorbidity point prevalence, about 110 million (95% CI 83 891 464 to 135 569 084) adult war survivors globally experienced comorbid PTSD and MD. Consequently, about 315 699 683 adult war survivors globally experienced PTSD and/or MD in 2019 in 43 war-afflicted countries. Of these, 313 889 900 were residing in LMICs. Only two countries affected by war (Kuwait and Croatia) were considered high-income. Extrapolations to disease burden are also provided in table 2. When the GBD 2019 results are taken as a reference, the extrapolations yielded 3 127 089 PTSD-associated DALYs and 4 114 663 MD-associated DALYs across 43 war-affected countries, of which 3 105 387 (PTSD) and 4 083 950 (MD) were located in LMICs.
Table 2.
Extrapolation to absolute prevalence and associated disease burden, as measured by DALYs
| Country | Last war-affected year for the given country (1989–2019) | Total population of adult war survivors (2019) | Absolute prevalence of war survivors with PTSD (95% CI) | PTSD-associated DALYs | Absolute prevalence of war survivors with MD (95% CI) | MD-associated DALYs | Absolute prevalence of war survivors with PTSD+MD |
| El Salvador | 1989 | 2 483 500 | 658 376 (550 592 to 772 369) | 10,262 | 578 904 (460 689 to 705 811) | 12 636 | 319 902 (243 776 to 393 944) |
| Mozambique | 1991 | 6 686 071 | 1 772 477 (1 482 302 to 2 079 368) | 20 387 | 1 558 523 (1 240 266 to 1 900 181) | 30 377 | 861 240 (656 294 to 1 060 575) |
| Kuwait | 1991 | 2 317 732 | 614 431 (513 841 to 720 815) | 11 450 | 540 263 (429 939 to 658 699) | 16 877 | 298 550 (227 505 to 367 649) |
| Croatia | 1991 | 2 581 667 | 684 400 (572 356 to 802 898) | 10 251 | 601 787 (478 899 to 733 710) | 13 836 | 332 547 (253 412 to 409 516) |
| Myanmar | 1992 | 22 181 071 | 5 880 202 (4 917 543 to 6 898 313) | 86 017 | 5 170 408 (4 114 589 to 6 303 860) | 36 527 | 2 857 167 (2 177 259 to 3 518 462) |
| Peru | 1992 | 14 322 678 | 3 796 942 (3 175 338 to 4 454 353) | 80 362 | 3 338 616 (2 656 857 to 4 070 505) | 39 573 | 1 844 919 (1 405 891 to 2 271 928) |
| Georgia | 1993 | 2 464 257 | 653 275 (546 326 to 766 384) | 5 733 | 574 418 (457 120 to 700 342) | 12 726 | 317 424 (241 888 to 390 892) |
| Azerbaijan | 1994 | 5 508 694 | 1 460 355 (1 221 277 to 1 713 204) | 13 963 | 1 284 077 (1 021 863 to 1 565 571) | 19 722 | 709 581 (540 725 to 873 814) |
| Bosnia-Herzegovina | 1995 | 2 236 056 | 592 778 (495 734 to 695 413) | 8 519 | 521 225 (414 788 to 635 487) | 9 678 | 288 029 (219 488 to 354 693) |
| Tajikistan | 1996 | 3 523 143 | 933 985 (781 081 to 1 095 697) | 7757 | 821 245 (653 543 to 1 001 277) | 10 380 | 453 820 (345 826 to 558 857) |
| Congo | 1998 | 2 191 526 | 580 974 (485 861 to 681 565) | 7030 | 510 845 (406 528 to 622 832) | 15,489 | 282 293 (215 117 to 347 630) |
| Serbia | 1999 | 6 352 650 | 1 684 088 (1 408 383 to 1 975 674) | 22 395 | 1 480 803 (1 178 417 to 1 805 423) | 28 139 | 818 292 (623 566 to 1 007 686) |
| Algeria | 1999 | 24 441 969 | 6 479 566 (5 418 785 to 7 601 452) | 108 133 | 5 697 423 (4 533 985 to 6 946 408) | 147 708 | 3 148 396 (2 399 185 to 3 877 096) |
| Sierra Leone | 1999 | 3 129 883 | 829 732 (693 895 to 973 394) | 10 829 | 729 576 (580 593 to 889 513) | 15 341 | 403 164 (307 224 to 496 476) |
| Kosovo | 1999 | 915 361 | 242 662 (202 936 to 284 677) | NA | 213 371 (169 799 to 260 146) | NA | 117 909 (89 850 to 145 199) |
| Ethiopia | 2000 | 44 350 185 | 11 757 234 (9 832 436 to 13 792 908) | 121 905 | 10 338 028 (8 226 959 to 12,604,323) | 194 816 | 5 712 794 (4 353 344 to 7 035 028) |
| Eritrea | 2000 | 1 428 785 | 378 771 (316 763 to 444 352) | 8 864 | 333 050 (265 040 to 406 061) | 14 143 | 184 043 (140 247 to 226 640) |
| Angola | 2001 | 11 202 755 | 2 969 850 (2 483 651 to 3 484 057) | 33 302 | 2 611 362 (2 078 111 to 3 183 823) | 68 513 | 1 443 039 (1 099 645 to 1 777 032) |
| Burundi | 2002 | 5 293 042 | 1 403 185 (1 173 467 to 1 646 136) | 15 802 | 1 233 808 (981 859 to 1 504 283) | 24 527 | 681 802 (519 557 to 839 606) |
| Liberia | 2003 | 2 463 836 | 653 163 (546 232 to 766 253) | 7550 | 574 320 (457 042 to 700 222) | 11 837 | 317 369 (241 846 to 390 825) |
| Uganda | 2004 | 19 435 624 | 5 152 384 (4 308 878 to 6 044 479) | 57 787 | 4 530 444 (3 605 308 to 5 523 604) | 122 373 | 2 503 523 (1 907 770 to 3 082 967) |
| Russia (regional) | 2004 | 959 727 | 254 424 (212 771 to 298 475) | 3091 | 223 712 (178 029 to 272 754) | 4,676 | 123 623 (94 205 to 152 236) |
| India (regional) | 2005 | 53 366 769 | 14 147 530 (11 831 413 to 16 597 065) | 152 752 | 12 439 794 (9 899 536 to 15 166 836) | 265 286 | 6 874 230 (5 238 397 to 8 465 280) |
| Colombia | 2005 | 35 348 853 | 9 370 981 (7 836 841 to 10 993 493) | 156 309 | 8 239 818 (6 557 212 to 10 046 144) | 102 122 | 4 553 323 (3 469 787 to 5 607 196) |
| Nepal | 2005 | 17 553 695 | 4 653 485 (3 891 654 to 5 459 199) | 55 365 | 4 091 766 (3 256 210 to 4 988 760) | 125 913 | 2 261 110 (1 723 043 to 2 784 447) |
| Chad | 2006 | 6 934 582 | 1 838 358 (1 537 397 to 2 156 655) | 19 251 | 1 616 451 (1 286 365 to 1 970 808) | 33 647 | 893 251 (680 688 to 1 099 995) |
| Rwanda | 2009 | 7 004 398 | 1 856 866 (1 552 875 to 2 178 368) | 22 281 | 1 632 725 (1 299 316 to 1 990 650) | 40 235 | 902 244 (687 541 to 1 111 069) |
| Sri Lanka | 2009 | 15 326 238 | 4 062 986 (3 397 827 to 4 766 460) | 63 630 | 3 572 546 (2 843 017 to 4 355 717) | 50 174 | 1 974 189 (1 504 399 to 2 431 118) |
| Israel (regional) | 2014 | 5 840 055 | 1 548 199 (1 294 740 to 1 816 257) | 22 332 | 1 361 317 (1 083 330 to 1 659 744) | 39 874 | 752 264 (573 251 to 926,376) |
| South Sudan | 2014 | 5 828 199 | 1 545 056 (1 292 112 to 1 812 570) | 19 525 | 1 358 553 (1 081 131 to 1 656 374) | 22 909 | 750 736 (572 087 to 924 495) |
| Pakistan | 2015 | 130 645 594 | 34 634 147 (28 964 128 to 40 630 780) | 382 665 | 30 453 488 (24 234 758 to 37 129 478) | 581 982 | 16 828 597 (12 823 964 to 20 723 599) |
| Ukraine (regional) | 2015 | 9 172 307 | 2 431 579 (2 033 500 to 2 852 587) | 30 410 | 2 138 065 (1 701 463 to 2 606 770) | 68 580 | 1 181 495 (900 339 to 1 454 953) |
| Sudan | 2016 | 23 446 328 | 6 215 622 (5 198 051 to 7 291 808) | 98 386 | 5 465 339 (4 349 294 6 663 446) | 132 072 | 3 020 146 (2 301 454 to 3 719 163) |
| Turkey | 2016 | 60 057 715 | 15 921 300 (13 314 795 to 18 677 949) | 267 749 | 13 999 453 (11 140 706 to 17 068 403) | 378 125 | 7 736 098 (5 895 170 to 9 526 628) |
| Iraq | 2017 | 70 339 201 | 18 646 922 (15 594 201 to 21 875 492) | 384 721 | 16 396 068 (13 047 922 to 19 990 401) | 409 203 | 9 060 467 (6 904 384 to 11 157 524) |
| Philippines | 2017 | 42 632 563 | 11 301 892 (9 451 639 to 13 258 727) | 184 410 | 9 937 650 (7 908 340 to 12 116 174) | 121 384 | 5 491 546 (4 184 745 to 6 762 571) |
| DR Congo | 2018 | 22 520 461 | 5 970 174 (4 992 786 to 7 003 863) | 71 413 | 5 249 519 (4 177 546 to 6 400 315) | 144 335 | 2 900 884 (2 210 573 to 3 572 298) |
| Afghanistan | 2019 | 19 791 367 | 5 246 691 (4 387 746 to 6 155 115) | 83 888 | 4 613 368 (3 671 299 to 5 624 707) | 119 476 | 2 549 347 (1 942 689 to 3 139 397) |
| Somalia | 2019 | 7 433 691 | 1 970 671 (1 648 049 to 2 311 878) | 24 977 | 1 732 793 (1 378 950 to 2 112 655) | 43 406 | 957 542 (729 679 to 1 179 166) |
| Yemen | 2019 | 16 284 148 | 4 316 928 (3 610 196 to 5 064 370) | 76 436 | 3 795 835 (3 020 709 to 4 627 955) | 113 562 | 2 097 578 (1 598 426 to 2 583 066) |
| Libya | 2019 | 4 619 825 | 1 224 716 (1 024 215 to 1 436 766) | 24 878 | 1 076 881 (856 978 to 1 312 954) | 34 089 | 595 085 (453 475 to 732 818) |
| Syria | 2019 | 11 163 348 | 2 959 404 (2 474 914 to 3 471 801) | 51 859 | 2 602 176 (2 070 801 to 3 172 624) | 58 620 | 1 437 963 (1 095 776 to 1 770 781) |
| Nigeria | 2019 | 102 874 311 | 27 271 980 (22 807 235 to 31 993 911) | 282 463 | 23 980 002 (19 083 185 to 29 236 879) | 379 778 | 13 251 349 (10 097 979 to 16 318 391) |
| Total | n.a. | 854 653 860 | 226 568 738 (189 476 761 to 265 797 350) | 3 127 089 | 199 219 815(158 538 291 to 242 892 627) | 4 114 663 | 110 088 870 (83 891 464 to 135 569 084) |
| LMICs only total | n.a. | 849 754 461 | 225 269 908 (188 390 564 to 264 273 637) | 3 105 387 | 198 077 765 (157 629 453 to 241 500 218) | 4 083 950 | 109 457 773 (83 410 547 to 134 791 919) |
Bold indicates that the respective war-affected country is a high-income country.
DALYs, disability-adjusted life years; LB, lower bound; MD, major depression; NA, data on Kosovo not available; n.a., not applicable; PTSD, post-traumatic stress disorder; UB, upper bound.
Discussion
Main findings
We aimed to estimate the absolute global number of war survivors with PTSD and/or MD and the associated disease burden in countries that experienced warfare within their own territory between 1989 and 2019. Extrapolation informed by meta-analysis yielded about 316 million adult survivors of war experiencing PTSD and/or MD globally. Almost all war survivors of recent wars reside in LMICs carrying a global accumulated burden of 3 million PTSD-associated DALYs and 4 million MD-associated DALYs.
Strengths and limitation
We estimated the absolute global number of war survivors with PTSD and/or MD by conducting an up-to-date and comprehensive systematic literature search. We maximised validity of extrapolations by only including interview-based epidemiological data from random general population samples. The extrapolations to absolute numbers may enable professionals from various disciplines to better grasp the burden of PTSD and MD on survivors of war and guide decision making to ultimately improve mental health of survivors.
Our study also has several limitations. The meta-analyses relied on only 41 surveys. This primarily reflects the current state of literature on war survivors that has mostly focused on refugees or other special war-surviving populations rather than general populations.29 In fact, the current literature base on interview-based randomly sampled surveys covers only 12 countries (and Palestine) and for the remaining 30 war-affected countries such samples are currently lacking. Therefore, our summary of the available literature might not be generalisable to countries with lacking data. On the notion of generalisability to countries with lacking data, it is worthwhile to check whether countries with available data may differ from countries without such data in terms of war-intensity. As can be seen in table 1, countries with available data bewailed on average 17 813 war-related deaths from 1989 to 2019 (SD=18 807) which translates into 99.48 war-related deaths per 100.000 population (SD=112.16). Whereas countries with missing data on average bewailed 40 042 (SD=71 980) or 183.17 per 100.000 population (SD=339.65). Across all 43 war-afflicted countries, an average of 33 322 (SD=61 593) individuals or 155.97 per 100.000 (SD=288.95) died due to war events. This demonstrates that the war-afflicted countries with available data are somewhat below average in terms of war-intensity. The performed moderator analyses did not yield significant differences in prevalence rates across 12 war-affected countries (plus Palestine) despite varying degrees of war-intensity and war-length (see online supplemental eTable 2). This finding may be unexpected, since higher intensity of trauma has been shown to relate to higher risk and prevalences of PTSD generally30 and also in the context of war trauma31 and genocide such as the Holocaust.32 Therefore, the results of this moderator analysis should be interpreted with caution as a dose–response relationship between war intensity and prevalences of trauma-related disorders appears plausible.31
Also related to the issue of limited data and generalisability, extrapolative accuracy is naturally restrained. Due to the general scarcity of data, we had to rely on pooled prevalences of PTSD and MD for extrapolations. In the light of varying degrees of war intensity and lengths as well as more general country-specific differences, such an approach is limited. However, the CIs for the pooled PTSD and MD prevalences were fairly narrow (22.17% to 31.10% and 18.55% to 28.42%, respectively) indicating fairly similar prevalences of PTSD and MD across the included surveys from 12 war-affected countries (plus Palestine) from three continents. Similarly, the moderator analysis on pooled prevalences by continent did not yield significant differences in PTSD prevalences across the three war-afflicted continents (ie, Africa, Asia and Europe). Surveys on MD were too scarce to allow for this moderator analysis. As more data accumulates, more fine-grained meta-analyses and, consequently, more fine-grained extrapolations will become possible.
Another potential limitation is that the current literature base exclusively covers cross-sectional surveys and lacks longitudinal data on remission from PTSD and MD. In their summary of the World Mental Health (WMH) Surveys, Kessler et al reported that remission of war-related PTSD would steeply increase about 6 years after exposure. The remission rate was reported to rise from about 20% at 5 years after war to about 70% at 6 years after war.33 In our review, the mean time between war and the assessment of disorders across all included surveys was 6.88 years. In our moderator analyses (see online supplemental eTable 2), the number of years between the end of the (last) war and the conduct of the survey was not found to be related to prevalence rates. This finding is at odds with previous research as illustrated by the above-mentioned summary of the WMH surveys. Yet, several factors might explain why remission rates may be dampened in post-war settings. Besides war-trauma, non-war-related traumatic experiences and difficult socioeconomic conditions may also influence the development and maintenance of PTSD and MD.34 35 Socioeconomic risk factors are more prevalent in LMICs with a history of war as compared with the countries included in the WHM surveys which were mostly high-income countries. Furthermore, individuals with mental disorders in LMICs are less likely to receive appropriate healthcare,36–38 and PTSD as well as MD, if left untreated, may follow a chronic course.39 40 However, while remission rates post-conflict might be dampened in war-ridden LMICs for various reasons, a degree of remission is still to be expected particularly over several decades as illustrated by long-term epidemiological data on WWII survivors.41–43 Therefore, null findings more probably boil down to a lack of longer-term data rather than lacking remissions per se.
Another potential limitation concerns heterogeneity in outcomes based on different nosology. We included surveys that conducted diagnostic interviews based on any ICD or DSM iteration, which use different criteria for defining PTSD and MD. Finally, this study estimates the disease burden for PTSD. Since the GBD 2019 does not report on PTSD DALYs separately, all anxiety disorder DALYs had to be used. The presented estimate, therefore, may overestimate or underestimate the PTSD-associated DALYs. The GBD study has already announced that it will report data on PTSD separately in coming iterations, which will allow for more accurate extrapolations.
Comparison with the literature
The pooled PTSD and MD prevalences are slightly lower than reported prevalences in most meta-analyses on these conditions in war-surviving populations (ie, ≥30%).3 4 29 In our previous meta-analyses, we found similarly high prevalences (ie, 24%–26% for PTSD and 23%–27% for MD).2 6 However, recent estimates by the WHO are considerably lower with 15.3% for PTSD and 10.8% for MD.1 As mentioned before, all previous meta-analyses partly or exclusively involved specific populations (eg, refugees, bereaved individuals) and precluded extrapolations to general war-surviving. Furthermore, related meta-analyses included self-report-based data.1 Self-report-based measures of PTSD (eg, PTSD CheckList – Civilian Version) and MD (eg, Patient Health Questionnaire – 9) either are not validated for LMICs or have poor psychometric properties in LMICs.44 To our knowledge, we performed the first meta-analysis that exclusively included representative interview-based data and, therefore, allowed for more valid extrapolations. We aimed at estimating the absolute prevalence and disease burden of PTSD and MD in war-afflicted countries, irrespective of assumptions about their aetiology. The elevated prevalences of PTSD and MD in war-surviving populations are not to be mistaken as solely caused by war-related trauma. The aetiologies of PTSD and MD are complex and, besides war experiences, non-war-related traumatic experiences, psychological stressors and aversive social conditions can play a role in the development and maintenance of PTSD and MD. However, independently of the precise aetiology of the disorders, the reported prevalences reflect the extent of the total burden and the need for help due to PTSD and MD in war-surviving populations.
Clinical, policy and research implications
In theory, effective psychological interventions for both youth and adult survivors of mass conflict do exist.38 45 However, most LMICs lack the resources in terms of both funding and qualified staff to provide evidence-based psychological treatments for all affected war survivors.36 37 46 While the allocation of financial and human resources for mental healthcare should surely increase,36 47 other approaches than specialised treatments are needed to address the mental health needs of survivors of war. For this, mental healthcare should be as much as possible integrated into the overall response to healthcare following wars. This may include strengthening of primary care to address mental disorders in primary care, task-sharing of psychosocial interventions with trained non-professional individuals, involving families and informal carers, using digital platforms to facilitate the delivery of interventions, and the development and implementation of community-based interventions.48–52 All these options may benefit from more systematic research to inform public health policies and practice.
Conclusions
The effects of exposure to war place a large mental health burden on the affected countries. An extrapolation from relative prevalence of PTSD and MD to absolute numbers suggests that hundreds of millions adult war survivors globally are affected. Countries with a recent history of war are almost exclusively LMICs. These countries lack the resources to provide specialised treatments for most of the affected war survivors. Therefore, alternative strategies—such as low-cost and technology-based interventions that build on existing resources—should be brought forward to meet the high burden of war-related mental disorders. The presented results generally illustrate the importance of peace-building and maintenance.
Footnotes
Handling editor: Seye Abimbola
Twitter: @HoppenDr
Contributors: THH and NM designed the study. THH and IV conducted the systematic literature search and data extraction. THH conducted the statistical analyses. THH wrote the manuscript. NM, SP and IV commented on and contributed to the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data analysed in this meta-analysis and in the extrapolations is published and publically available.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Charlson F, van Ommeren M, Flaxman A, et al. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet 2019;394:240–8. 10.1016/S0140-6736(19)30934-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morina N, Stam K, Pollet TV, et al. Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. J Affect Disord 2018;239:328–38. 10.1016/j.jad.2018.07.027 [DOI] [PubMed] [Google Scholar]
- 3.Steel Z, Chey T, Silove D, et al. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA 2009;302:537–49. 10.1001/jama.2009.1132 [DOI] [PubMed] [Google Scholar]
- 4.Ng LC, Stevenson A, Kalapurakkel SS, et al. National and regional prevalence of posttraumatic stress disorder in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med 2020;17:e1003090. 10.1371/journal.pmed.1003090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UCDP . Uppsala conflict data program (UCDP) conflict encyclopedia. Uppsala University, 2020. [Google Scholar]
- 6.Hoppen TH, Morina N. The prevalence of PTSD and major depression in the global population of adult war survivors: a meta-analytically informed estimate in absolute numbers. Eur J Psychotraumatol 2019;10:1578637. 10.1080/20008198.2019.1578637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morina N. Mental health among adult survivors of war in low-and middle-income countries: epidemiology and treatment outcome. In: Morina N, Nickerson A, eds. Mental health of refugee and Conflict-Affected populations: theory, research and clinical practice. Cham: Springer Nature, 2018: 3–14. [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morina N, Nickerson A, eds. Mental health of refugee and conflict-affected populations: theory, research and clinical practice. Cham: Springer Nature, 2018. [Google Scholar]
- 10.Musanabaganwa C, Jansen S, Fatumo S, et al. Burden of post-traumatic stress disorder in postgenocide Rwandan population following exposure to 1994 genocide against the Tutsi: a meta-analysis. J Affect Disord 2020;275:7-13. 10.1016/j.jad.2020.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495–9. 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- 12.Sanderson S, Tatt ID, Higgins JPT. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol 2007;36:666–76. 10.1093/ije/dym018 [DOI] [PubMed] [Google Scholar]
- 13.Wang W, Fan J, Huang G, et al. Meta-analysis of prevalence of erectile dysfunction in mainland China: evidence based on epidemiological surveys. Sex Med 2017;5:e19–30. 10.1016/j.esxm.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barendregt JJ, Doi SA, Lee YY, et al. Meta-analysis of prevalence. J Epidemiol Community Health 2013;67:974–8. 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 15.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019;22:153–60. 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Viechtbauer W. Conducting meta-analyses in R with the metafor package. Comput Softw 2010;36:313–20. 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 17.R Core Team . R: a language and environment for statistical computing. Vienna, Austria, 2015. [Google Scholar]
- 18.Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat 1998;52:119–26. 10.1080/00031305.1998.10480550 [DOI] [Google Scholar]
- 19.Schwarzer G, Carpenter JR, Rücker G. Meta-analysis with R. Springer, 2015. [Google Scholar]
- 20.Tabaschnick BG, Fidell LS. Using multivariate statistics. 6th edn. Boston: Pearson, 2013. [Google Scholar]
- 21.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterne JAC, Sutton AJ, Ioannidis JPA, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 23.Duval S. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc 2000;95:89–98. 10.1080/01621459.2000.10473905 [DOI] [Google Scholar]
- 24.United Nations . World population prospects 2019: department of economic and social Affairs, 2020. Available: https://population.un.org/wpp/Download/Standard/Population/
- 25.Morina N, von Lersner U, Prigerson HG. War and bereavement: consequences for mental and physical distress. PLoS One 2011;6:e22140. 10.1371/journal.pone.0022140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fantom N, Serajuddin U. The World Bank’s classification of countries by income. The World Bank, 2016. [Google Scholar]
- 27.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020;396:1204–22. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheehan DV, Lecrubier Y, Harnett Sheehan K, et al. The validity of the mini international neuropsychiatric interview (mini) according to the SCID-P and its reliability. Eur Psychiatry 1997;12:232–41. 10.1016/S0924-9338(97)83297-X [DOI] [Google Scholar]
- 29.Blackmore R, Boyle JA, Fazel M, et al. The prevalence of mental illness in refugees and asylum seekers: a systematic review and meta-analysis. PLoS Med 2020;17:e1003337. 10.1371/journal.pmed.1003337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 2000;68:748. 10.1037//0022-006x.68.5.748 [DOI] [PubMed] [Google Scholar]
- 31.Buydens-Branchey L, Noumair D, Branchey M. Duration and intensity of combat exposure and posttraumatic stress disorder in Vietnam veterans. J Nerv Ment Dis 1990;178:582–7. 10.1097/00005053-199009000-00005 [DOI] [PubMed] [Google Scholar]
- 32.Kuch K, Cox BJ. Symptoms of PTSD in 124 survivors of the holocaust. Am J Psychiatry 1992;149:337–40. 10.1176/ajp.149.3.337 [DOI] [PubMed] [Google Scholar]
- 33.Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. Trauma and PTSD in the who world mental health surveys. Eur J Psychotraumatol 2017;8:1353383. 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benjet C. Childhood adversities of populations living in low-income countries: prevalence, characteristics, and mental health consequences. Curr Opin Psychiatry 2010;23:356–62. 10.1097/YCO.0b013e32833ad79b [DOI] [PubMed] [Google Scholar]
- 35.Benjet C, Bromet E, Karam EG, et al. The epidemiology of traumatic event exposure worldwide: results from the world mental health survey Consortium. Psychol Med 2016;46:327–43. 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patel V, Saxena S, Lund C, et al. The lancet commission on global mental health and sustainable development. Lancet 2018;392:1553–98. 10.1016/S0140-6736(18)31612-X [DOI] [PubMed] [Google Scholar]
- 37.Patel V, Maj M, Flisher AJ, et al. Reducing the treatment gap for mental disorders: a WPA survey. World Psychiatry 2010;9:169–76. 10.1002/j.2051-5545.2010.tb00305.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morina N, Malek M, Nickerson A, et al. Psychological interventions for post-traumatic stress disorder and depression in young survivors of mass violence in low- and middle-income countries: meta-analysis. Br J Psychiatry 2017;210:247–54. 10.1192/bjp.bp.115.180265 [DOI] [PubMed] [Google Scholar]
- 39.Morina N, Wicherts JM, Lobbrecht J, et al. Remission from post-traumatic stress disorder in adults: a systematic review and meta-analysis of long term outcome studies. Clin Psychol Rev 2014;34:249–55. 10.1016/j.cpr.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 40.Richards D. Prevalence and clinical course of depression: a review. Clin Psychol Rev 2011;31:1117–25. 10.1016/j.cpr.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 41.Lis-Turlejska M, Szumiał S, Drapała I. Posttraumatic stress symptoms among Polish World war II survivors: the role of social acknowledgement. Eur J Psychotraumatol 2018;9:1423831. 10.1080/20008198.2018.1423831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bramsen I, van der Ploeg HM. Fifty years later: the long-term psychological adjustment of ageing World war II survivors. Acta Psychiatr Scand 1999;100:350–8. 10.1111/j.1600-0447.1999.tb10878.x [DOI] [PubMed] [Google Scholar]
- 43.Frounfelker R, Gilman SE, Betancourt TS, et al. Civilians in world war II and DSM-IV mental disorders: results from the world mental health survey initiative. Soc Psychiatry Psychiatr Epidemiol 2018;53:207–19. 10.1007/s00127-017-1452-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ali G-C, Ryan G, De Silva MJ. Validated screening tools for common mental disorders in low and middle income countries: a systematic review. PLoS One 2016;11:e0156939. 10.1371/journal.pone.0156939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morina N, Malek M, Nickerson A, et al. Meta-analysis of interventions for posttraumatic stress disorder and depression in adult survivors of mass violence in low- and middle-income countries. Depress Anxiety 2017;34:679–91. 10.1002/da.22618 [DOI] [PubMed] [Google Scholar]
- 46.Osborn TL, Wasil AR, Weisz JR, et al. Where is the global in global mental health? A call for inclusive multicultural collaboration. Gen Psychiatr 2020;33:e100351. 10.1136/gpsych-2020-100351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jakovljevic MB. Resource allocation strategies in southeastern European health policy. Eur J Health Econ 2013;14:153–9. 10.1007/s10198-012-0439-y [DOI] [PubMed] [Google Scholar]
- 48.Dawson KS, Rahman A. Low intensity interventions for psychological symptoms following mass trauma. In: Morina N, Nickerson A, eds. Mental health of refugee and Conflict-Affected populations: theory, research and clinical practice. Cham: Springer Nature, 2018: 341–56. [Google Scholar]
- 49.Naslund JA, Aschbrenner KA, Araya R, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry 2017;4:486–500. 10.1016/S2215-0366(17)30096-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patel V, Simon G, Chowdhary N, et al. Packages of care for depression in low- and middle-income countries. PLoS Med 2009;6:e1000159. 10.1371/journal.pmed.1000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rahman A, Hamdani SU, Awan NR, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. JAMA 2016;316:2609–17. 10.1001/jama.2016.17165 [DOI] [PubMed] [Google Scholar]
- 52.Singla DR, Kohrt BA, Murray LK, et al. Psychological treatments for the world: lessons from low- and middle-income countries. Annu Rev Clin Psychol 2017;13:149–81. 10.1146/annurev-clinpsy-032816-045217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ayazi T, Lien L, Eide AH, et al. What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war-affected population? A cross-sectional community study in South Sudan. BMC Psychiatry 2012;12:175. 10.1186/1471-244X-12-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Canetti D, Galea S, Hall BJ, et al. Exposure to prolonged socio-political conflict and the risk of PTSD and depression among Palestinians. Psychiatry 2010;73:219–31. 10.1521/psyc.2010.73.3.219 [DOI] [PubMed] [Google Scholar]
- 55.de Jong JT, Komproe IH, Van Ommeren M, et al. Lifetime events and posttraumatic stress disorder in 4 postconflict settings. JAMA 2001;286:555–62. 10.1001/jama.286.5.555 [DOI] [PubMed] [Google Scholar]
- 56.Eytan A, Guthmiller A, Durieux-Paillard S, et al. Mental and physical health of Kosovar Albanians in their place of origin: a post-war 6-year follow-up study. Soc Psychiatry Psychiatr Epidemiol 2011;46:953–63. 10.1007/s00127-010-0269-0 [DOI] [PubMed] [Google Scholar]
- 57.Fodor KE, Pozen J, Ntaganira J, et al. The factor structure of posttraumatic stress disorder symptoms among Rwandans exposed to the 1994 genocide: a confirmatory factor analytic study using the PCL-C. J Anxiety Disord 2015;32:8–16. 10.1016/j.janxdis.2015.03.001 [DOI] [PubMed] [Google Scholar]
- 58.Johnson K, Asher J, Rosborough S, et al. Association of combatant status and sexual violence with health and mental health outcomes in postconflict Liberia. JAMA 2008;300:676–90. 10.1001/jama.300.6.676 [DOI] [PubMed] [Google Scholar]
- 59.Johnson K, Scott J, Rughita B, et al. Association of sexual violence and human rights violations with physical and mental health in territories of the eastern Democratic Republic of the Congo. JAMA 2010;304:553–62. 10.1001/jama.2010.1086 [DOI] [PubMed] [Google Scholar]
- 60.Madianos MG, Sarhan AL, Koukia E. Posttraumatic stress disorders comorbid with major depression in West bank, Palestine: a general population cross sectional study. Eur. J. Psychiat. 2011;25:19–31. 10.4321/S0213-61632011000100003 [DOI] [Google Scholar]
- 61.Morina N, Ford JD. Complex sequelae of psychological trauma among Kosovar civilian war victims. Int J Soc Psychiatry 2008;54:425–36. 10.1177/0020764008090505 [DOI] [PubMed] [Google Scholar]
- 62.Morina N, Stangier U, Risch AK. Experiential avoidance in civilian war survivors with current versus recovered posttraumatic stress disorder: a pilot study. Behav Change 2008;25:15–22. 10.1375/bech.25.1.15 [DOI] [Google Scholar]
- 63.Morina N, Ford JD, Risch AK, et al. Somatic distress among Kosovar civilian war survivors: relationship to trauma exposure and the mediating role of experiential avoidance. Soc Psychiatry Psychiatr Epidemiol 2010;45:1167–77. 10.1007/s00127-009-0160-z [DOI] [PubMed] [Google Scholar]
- 64.Mugisha J, Muyinda H, Wandiembe P, et al. Prevalence and factors associated with posttraumatic stress disorder seven years after the conflict in three districts in northern Uganda (the Wayo-Nero study). BMC Psychiatry 2015;15:170. 10.1186/s12888-015-0551-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Munyandamutsa N, Mahoro Nkubamugisha P, Gex-Fabry M, et al. Mental and physical health in Rwanda 14 years after the genocide. Soc Psychiatry Psychiatr Epidemiol 2012;47:1753–61. 10.1007/s00127-012-0494-9 [DOI] [PubMed] [Google Scholar]
- 66.Priebe S, Bogic M, Ajdukovic D. Mental disorders following war in the Balkans: a study in 5 countries. Arch Gen Psychiatry 2010;67:518–28. 10.1001/archgenpsychiatry.2010.37 [DOI] [PubMed] [Google Scholar]
- 67.Rieder H, Elbert T. Rwanda - lasting imprints of a genocide: trauma, mental health and psychosocial conditions in survivors, former prisoners and their children. Confl Health 2013;7:6. 10.1186/1752-1505-7-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rugema L, Mogren I, Ntaganira J, et al. Traumatic episodes and mental health effects in young men and women in Rwanda, 17 years after the genocide. BMJ Open 2015;5:e006778. 10.1136/bmjopen-2014-006778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schaal S, Weierstall R, Dusingizemungu J-P, et al. Mental health 15 years after the killings in Rwanda: imprisoned perpetrators of the genocide against the Tutsi versus a community sample of survivors. J Trauma Stress 2012;25:446–53. 10.1002/jts.21728 [DOI] [PubMed] [Google Scholar]
- 70.Somasundaram DJ, Sivayokan S. War trauma in a civilian population. Br J Psychiatry 1994;165:524–7. 10.1192/bjp.165.4.524 [DOI] [PubMed] [Google Scholar]
- 71.Veling W, Hall BJ, Joosse P. The association between posttraumatic stress symptoms and functional impairment during ongoing conflict in the Democratic Republic of Congo. J Anxiety Disord 2013;27:225–30. 10.1016/j.janxdis.2013.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yasan A, Saka G, Ozkan M, et al. Trauma type, gender, and risk of PTSD in a region within an area of conflict. J Trauma Stress 2009;22:663–6. 10.1002/jts.20459 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-006303supp001.pdf (217.6KB, pdf)
Data Availability Statement
All data analysed in this meta-analysis and in the extrapolations is published and publically available.