Abstract
Introduction and importance
Foreign body aspiration (FBA) in adults may be asymptomatic or symptomatic. Fever and cough are the most common symptoms of Coronavirus infection and other causes of pneumonia. Regardless of the etiology of pneumonia, the first step in the treatment of FBA-associated pneumonia is to remove the foreign body from the airway.
Case presentation
A 32-year-old man was referred to our emergency department on October 26, 2020 with shortness of breath (SOB) and a cough. He was referred to the medical center with clinical suspicion of Coronavirus disease-19 (COVID-19), and his disease was treated considering COVID-19. Based on the persistence of his symptoms after discharge, he was referred to the hospital again, and the presence of a foreign body was confirmed by a rigid bronchoscopy, which was then removed.
Clinical discussion
Our patient did not remember any history of aspirating solid particles, choking, or any other high-risk conditions associated with aspiration. Also, he had no symptoms with the exception of cough and SOB before the first admission. It means that asymptomatic FBA can be tolerated and go undiagnosed, particularly in adults, and manifests as a secondary complication, such as pneumonia.
Conclusion
The FBA and other causal agents may mimic COVID-19 pneumonia. Consequently, FBA should be included in the COVID-19 differential diagnosis.
Keywords: COVID-19, Pneumonia, Foreign body aspiration, Rigid bronchoscopy
Highlights
-
•
The over diagnosed COVID-19 infection in an adult patient with foreign body aspiration.
-
•
FBA and other causal agents may mimic COVID-19 pneumonia. Consequently, FBA should be included in the COVID-19 differential diagnosis.
-
•
The taking comprehensive history, physical examination and purposeful paraclinical assessments helps to make the best decision for management of the patients.
1. Introduction
In December 2019, the world health organization (WHO) declared a pandemic caused by a novel Coronavirus that could cause severe acute respiratory syndrome (SARS-Cov2). This syndrome has the same etiology as the SARS and MERS outbreaks, which occurred in 2002 and 2012, respectively. This novel disease is primarily presented by respiratory symptoms such as cough, dyspnea, fever, fatigue, nausea, vomiting, diarrhea, headache, etc. These may differ depending on the geographical setting and individual characteristics, which, in some cases, lead to critical conditions necessitating admission to the intensive care unit (ICU). The mortality rate was announced at 11–15% in China, the first place where SARS-Cov2 was discovered [[1], [2], [3], [4]].
Foreign body aspiration (FBA) is an emergency medical condition demanding immediate attention to diagnose and set a treatment plan. FBA has a high risk of mortality in the Case of total obstruction. However, it can be tolerated and subsequently undetectable, especially in adults with partial obstruction. The symptoms may include choking, coughing, vomiting, and they may be asymptomatic. A patient with FBA may possibly have experience of recurrent pneumonia, bronchiectasis, recurrent hemoptysis, and some other complications. Studies show that it is more common to happen on the right side of the airway. The extraction of the foreign body should be performed as soon as possible [[5], [6], [7], [8]]. In this regard, differential diagnosis of Coronavirus disease-19 (COVID-19) from other respiratory disorders that mimic similar clinical patterns, especially during pandemics, should be strongly considered.
2. Case presentation
A 32-year-old man was referred to our emergency department on October 26, 2020 with shortness of breath (SOB) and a cough. The O2 saturation (O2 sat) value was 96% on admission. He had a past history of admission to the local hospital for 5 days on referral. On that admission, the patient was hospitalized with dyspnea, fever, and on-arrival laboratory data revealed leukopenia with a WBC count of 2.5 × 103/mm3 and increased levels of CRP at a level of 61 mg/dL. Other lab parameters were in the normal range. The patient was admitted to the infection ward based on the COVID-19 diagnosis. The treatment started with remdesivir, interferon β, doxycycline, hydroxychloroquine, naproxen, pantoprazole, and enoxaparin.
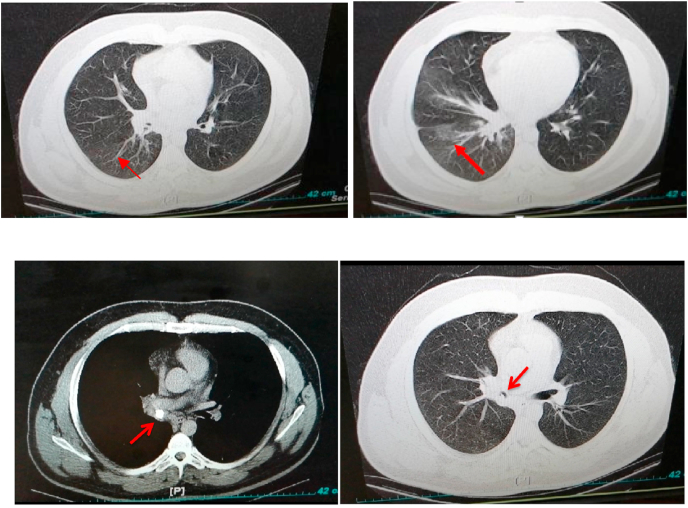
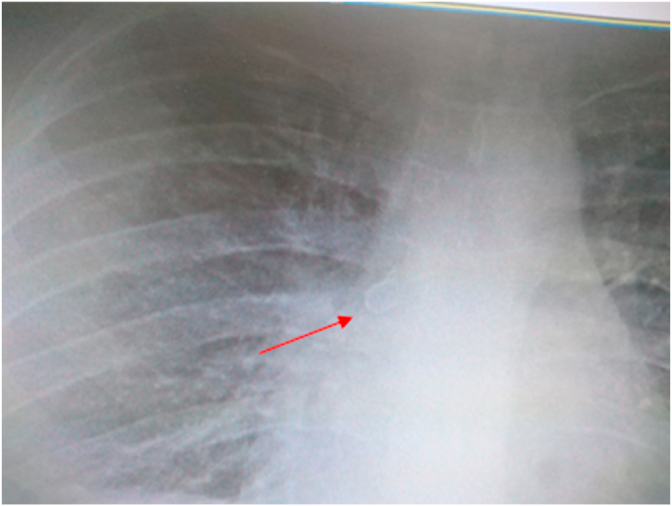
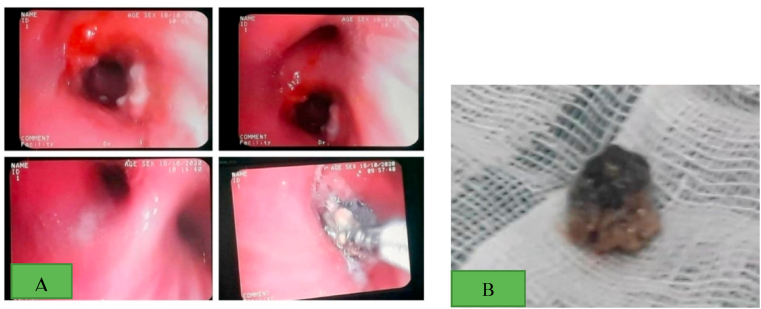
After 5 days, the patient's general condition improved and he was discharged to his own personal satisfaction. However, he was referred to our hospital 24 hours later due to the persistence of his cough and SOB. He was admitted under the supervision of a pulmonologist, and HRCT and RT-PCR were ordered. The result of the lung HRCT showed mosaic attenuation in the right middle and lower lobes due to air trapping (Fig. 1). In addition, the RT-PCR for COVID-19 was negative. Moreover, the results of the chest X-ray (CXR) revealed a round opacity in the right main bronchus (Fig. 2). Clinical suspicion was placed on the FBA based on the radiologist's comment (Fig. 1, Fig. 2). Rigid bronchoscopy was performed to further investigate and diagnose the patient, and an olive kernel was discovered in the right main bronchus (Fig. 3 A, B).
Fig. 1.
The result of lung HRCT showing mosaic attenuation in the right middle and lower lobes (arrow head) due to air trapping.
Fig. 2.
A round opacity showing in the right main bronchus (arrow head) on chest X-ray.
Fig. 3.
The rigid bronchoscopy view of the aspirated olive kernel (A), removal of the olive kernel (B).
Due to the pandemic prevalence of COVID-19 and the large number of patients referred to medical centers with clinical suspicion of COVID-19, the patient was admitted to the infectious service, where his disease was missed due to a lack of an accurate history and attention to the x-ray. Due to the persistence of his symptoms after discharge, a rigid bronchoscopy was performed to rule out the presence of a foreign body, which was then removed. This study was conducted according to the declaration of Helsinki principles. Also, CARE guidelines and methodology were followed in this study. The work has been reported in line with the SCARE 2020 criteria [9]. This study is registered with the research registry, and the UIN is research registry 6928 https://www.researchregistry.com/register-now#home/addregistration/register-research-study-please-note-it-costs-99-to-register-payment/60d95493051a1e001fe5e028/
3. Discussion
Cough and dyspnea are the two symptoms which are common in COVID-19 and FBA. Since cough is the most frequent early symptom of COVID19, a chest CT scan is performed on all suspicious patients. Interstitial pneumonia with predominantly bilateral involvement and multiple patchy, flocculent, or stripped ground glass shadows are the most frequent pulmonary changes seen on imaging. The marginal areas of the lesions were poorly defined. There was little pleural effusion, and consolidation of the lungs occurred when the disease was serious [[1], [2], [3], [4], [5], [6],10]. FBA is a serious medical problem associated with significant morbidity and mortality. However, it is not a routine condition in adults, but situations including altered mental status, trauma with decreased level of consciousness, dental procedures, and impaired airway reflexes associated with neurological disease could increase the incidence risk [5,11].
Cough is a very common symptom in patients with an aspirated foreign body. Infective complications secondary to foreign body aspiration may cause associated symptoms such as fever, hemoptysis, foul-smelling sputum, pain in the chest, etc., [11].
Silent FBA is uncommon in adults. The migration of a silent foreign body from one main stem bronchus to the other within the tracheobronchial tree is rarer still. Food particles such as bone chips, nut shells, and food boluses are the most common foreign body aspirations in a healthy adult. Broken teeth and dentures may be aspirated under anesthesia during a difficult laryngoscopy, with medicolegal implications. Organic aspirated materials induce intense inflammatory tissue responses and, thus, identification of such foreign bodies occurs much sooner. Complications of organic aspirated materials are secondary to these inflammatory responses and may result in stenosis. Alternatively, organic materials may absorb moisture and present an acute emergency such as airway obstruction [11].
Our patient did not remember any history of aspirating solid particles, choking, or any other high risk conditions associated with aspiration. Also, he had no symptoms except for a cough and SOB before the first admission. It means that asymptomatic FBA can be tolerated and misdiagnosed, particularly in adults, and manifests as a secondary complication, such as pneumonia [5,7,11].
Our patient was feverish on his first admission. Fever, dry cough, fatigue, and muscle pain are the most common symptoms of COVID-19; less common symptoms include sore throat, runny nose, diarrhea, hemoptysis, and chills [12]. On the other hand, a diagnosis of pneumonia as a complication of FBA should be considered in patients with an acute onset of fever or chills and cough. The cough may be described as productive. Additional symptoms frequently seen include fatigue, anorexia, and pleuritic chest pain. Important components of history include recent travel, the history of underlying lung disease, and smoking history [13].
Actually, fever and cough are two common symptoms of COVID-19 pneumonia and non-COVID-19 pneumonia. The lung CT involvement in COVID-19 pneumonia is usually bilateral ground glass opacities and consolidation, but it can vary in different patients and stages. In comparison, multiple mottling, centrilobular nodules, unilateral segmental or lobar consolidation, and mucoid impaction reveal bacterial etiology as the origin or a bacterial super-infection. It should be noted that in the current pandemic of COVID-19, RT-PCR result may be helpful for confirmation of diagnosis [14,15].
4. Conclusion
Considering differential diagnosis regarding the complaints of the patient at the time of admission, it's necessary to make an exact diagnosis. Despite suitable treatment, in hospitalized patients with similar symptoms, other differential diagnosis should also be considered. To avoid misdiagnosis or over diagnosis, physicians should be aware of the differential diagnosis of pneumonia. As a whole, FBA should be included in the COVID-19 differential diagnosis. Accordingly, taking a comprehensive history, physical examination and purposeful para-clinical assessments help to make the best decision for management of the patients.
Ethics approval and consent to participate
The study was approved by our local ethics committee.
Funding
None.
Authors’ contributions
As, zz involved in the interpretation and collecting of data and editing of the manuscript. Zn, esb involved in drafting the first version of the manuscript and editing it. Mrn, ah and kr involved in writing, editing, and preparing the final version of the manuscript. Mf is involved in critically revising the whole manuscript. Ms is responsible for collecting data and submitting the manuscript. All authors reviewed the paper and approved the final version of the manuscript.
Registration of research studies
6928.
Guarantor
Zakaria zakariaei.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Pascarella G., Strumia A., Piliego C., Bruno F., Del Buono R., Costa F., Scarlata S., Agrò F.E. COVID-19 diagnosis and management: a comprehensive review. J. Intern. Med. 2020;288(2):192–206. doi: 10.1111/joim.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naserghandi A., Allameh S.F., Saffarpour R. All about COVID-19 in brief. New Microbes New Infect. 2020 13;35:100678. doi: 10.1016/j.nmni.2020.100678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pourbagheri-Sigaroodi A., Bashash D., Fateh F., Abolghasemi H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin. Chim. Acta. 2020;510:475–482. doi: 10.1016/j.cca.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harapan H., Itoh N., Yufika A., Winardi W., Keam S., Te H., Megawati D., Hayati Z., Wagner A.L., Mudatsir M. Coronavirus disease 2019 (COVID-19): a literature review. J Infect Public Health. 2020;13(5):667–673. doi: 10.1016/j.jiph.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyd M., Chatterjee A., Chiles C., Chin R., Jr. Tracheobronchial foreign body aspiration in adults. South. Med. J. 2009;102(2):171–174. doi: 10.1097/SMJ.0b013e318193c9c8. [DOI] [PubMed] [Google Scholar]
- 6.Hewlett J.C., Rickman O.B., Lentz R.J., Prakash U.B., Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J. Thorac. Dis. 2017;9(9):3398–3409. doi: 10.21037/jtd.2017.06.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qureshi A., Behzadi A. Foreign-body aspiration in an adult. Can. J. Surg. 2008;51(3):69–70. [PMC free article] [PubMed] [Google Scholar]
- 8.Tatsanakanjanakorn W., Suetrong S. Do times until treatment for foreign body aspiration relate to complications? Int J Otolaryngol. 2016;2016:2831614. doi: 10.1155/2016/2831614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE Group. The SCARE 2020 guideline: updating consensus surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Wan S., Xiang Y., Fang W., Zheng Y., Li B., Hu Y., Lang C., Huang D., Sun Q., Xiong Y., Huang X., Lv J., Luo Y., Shen L., Yang H., Huang G., Yang R. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J. Med. Virol. 2020;92(7):797–806. doi: 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panigrahi B., Sahay N., Samaddar D.P., Chatterjee A. Migrating foreign body in an adult bronchus: an aspirated denture. J Dent Anesth Pain Med. 2018;18(4):267–270. doi: 10.17245/jdapm.2018.18.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wujtewicz M., Dylczyk-Sommer A., Aszkiełowicz A., Zdanowski S., Piwowarczyk S., Owczuk R. COVID-19 - what should anaethesiologists and intensivists know about it? Anaesthesiol. Intensive Ther. 2020;52(1):34–41. doi: 10.5114/ait.2020.93756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grief S.N., Loza J.K. Guidelines for the evaluation and treatment of pneumonia. Prim Care. 2018;45(3):485–503. doi: 10.1016/j.pop.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye Z., Zhang Y., Wang Y., Huang Z., Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur. Radiol. 2020;30(8):4381–4389. doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hani C., Trieu N.H., Saab I., Dangeard S., Bennani S., Chassagnon G., Revel M.P. COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn Interv Imaging. 2020;101(5):263–268. doi: 10.1016/j.diii.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]