Abstract
Objective
To systematically investigate the relationship between cardiac biomarkers and COVID-19 severity and mortality.
Methods
We performed a literature search using PubMed, Web of Science, and Google Scholar. The standardized mean difference (SMD) and 95% confidence interval (CI) were applied to estimate the combined results of 67 studies. A meta-analysis of cardiac biomarkers was used to evaluate disease mortality and severity in COVID-19 patients.
Results
A meta-analysis of 7812 patients revealed that patients with high levels of cardiac troponin I (SMD = 0.81 U/L, 95% CI = 0.14–1.48, P = 0.017), cardiac troponin T (SMD = 0.78 U/L, 95% CI = 0.07–1.49, P = 0.032), high-sensitive cardiac troponin I (SMD = 0.66 pg/mL, 95% CI = 0.51–0.81, P < 0.001), high-sensitive cardiac troponin T (SMD = 0.93 U/L, 95% CI = 0.21–1.65, P = 0.012), creatine kinase-MB (SMD = 0.54 U/L, 95% CI = 0.39−0.69, P < 0.001), and myoglobin (SMD = 0.80 U/L, 95% CI = 0.57–1.03, P < 0.001) were associated with prominent disease severity in COVID-19 infection. Moreover, 9532 patients with a higher serum level of cardiac troponin I (SMD = 0.51 U/L, 95% CI = 0.37–0.64, P < 0.001), high-sensitive cardiac troponin (SMD = 0.51 ng/L, 95% CI = 0.29–0.73, P < 0.001), high-sensitive cardiac troponin I (SMD = 0.51 pg/mL, 95% CI = 0.38–0.63, P < 0.001), high-sensitive cardiac troponin T (SMD = 0.85 U/L, 95% CI = 0.63–1.07, P < 0.001), creatine kinase-MB (SMD = 0.48 U/L, 95% CI = 0.32–0.65, P < 0.001), and myoglobin (SMD = 0.55 U/L, 95% CI = 0.45−0.65, P < 0.001) exhibited a prominent level of mortality from COVID-19 infection.
Conclusion
Cardiac biomarkers (cardiac troponin I, cardiac troponin T, high-sensitive cardiac troponin, high-sensitive cardiac troponin I, high-sensitive cardiac troponin T, creatine kinase-MB, and myoglobin) should be more frequently applied in identifying high-risk COVID-19 patients so that timely treatment can be implemented to reduce severity and mortality in COVID-19 patients.
Abbreviations: hs-cTnI, high-sensitive cardiac troponin I; hs-cTnT, high-sensitive cardiac troponin T; hs-cTn, high-sensitive cardiac troponin; cTnI, cardiac troponin I; cTnT, cardiac troponin T; Mb, myoglobin; CK-MB, creatine kinase-MB
Keywords: COVID-19, Cardiac biomarkers, Meta-analysis, Severity, Mortality
Introduction
In December 2019, a novel coronavirus pneumonia (coronavirus disease 2019, COVID-19) outbreak was reported in Wuhan, China, and developed into a global pandemic. SARS-CoV-2 infection is induced by a combination of the spike protein of the virus and an angiotensin-converting enzyme 2 (ACE2), which is strongly expressed in the heart and lungs [1]; it primarily invades alveolar epithelial cells and causes respiratory symptoms. ACE2 is not only expressed in the lung, but also in the heart and blood vessels. Therefore, SARS-CoV-2 may cause acute myocardial injury and chronic cardiovascular injury [2]. Myocardial injury, as shown by increased cardiac biomarkers, was identified among the first 41 patients with COVID-19 in Wuhan [3].
Increases in lactose dehydrogenase (LDH), creatine kinase (CK), and aspartate aminotransferase (AST) can serve as markers of myocardial damage, as well as damage to the lungs, liver, kidneys, or other organs. In contrast, myoglobin (Mb), an oxygen binding protein, is mainly distributed in the cytoplasm of skeletal muscle and in the myocardium. Mb is a marker that can be detected early after myocardial injury. Creatine kinase-MB (CK-MB), cardiac troponin I (cTnI), and cardiac troponin T (cTnT) are also myocardial-specific isoenzymes and proteins. Increases in CK-MB, cTnI, cTnT, and hs-cTnT have high specificity in the diagnosis of myocardial injury. High-sensitive cardiac troponin I (hs-cTnI) has high sensitivity as a marker of early myocardial injury [4]. Some studies in patients with COVID-19 reported that levels of specific myocardial biomarkers including CK-MB, Mb, and cTnI were higher in patients treated in an intensive care unit (ICU) than in patients who did not require ICU care [[5], [6], [7]]. In this regard, identification of cardiac-specific biomarkers may reflect the severity of COVID-19 and improve outcomes by assisting with the management of COVID-19 patients.
The purpose of the present research was to investigate the relationships between cardiac-specific biomarkers (cTnI, cTnT, hs-cTn, hs-cTnI, hs-cTnT, CK-MB, and Mb) and COVID-19 severity and mortality through a meta-analysis.
Methods
Search strategy
This meta-analysis and systematic review is reported in accordance with the Preferred Reporting Items and Meta-Analyses (PRISMA) guidelines. Two researchers (An, Wang) screened the literature and chose the relevant studies using the Web of Science, PubMed, and Google Scholar for publications as of May 9, 2021, published in either English or Chinese. The following terms were used for the study search: (“SARS-CoV-2” or “COVID-19” or “Novel coronavirus 2019” or “coronavirus disease 2019”) and (“Cardiac injury” or “Cardiac biomarkers” or “Heart” or “Myoglobin” or “Cardiac troponin I” or “cTnI” or “Cardiac troponin T” or “cTnT” or “Creatine Kinase-MB” or “Ck-MB” or “High-sensitive cardiac troponin I” or “hs-cTnI” or “High-sensitive cardiac troponin T” or “hs-cTnT” or “High-sensitive cardiac troponin” or “hs-cTn”). Studies in the reference list of related papers were also included in the study. IRB approval was not required.
Selection criteria
The inclusion criteria were as follows: (a) types of studies: observational, retrospective, prospective, case‐control, or descriptive studies of cardiac biomarkers including cTnI, cTnT, hs-cTn, hs-cTnI, hs-cTnT, CK-MB, and Mb in COVID-19 patients at admission; (b) subjects: patients diagnosed with COVID-19; (c) exposure/intervention: including at least one outcome of ICU vs. non-ICU, severe vs. non-severe, or survived vs. deceased; and (d) outcome measurements: mean and standard deviation or IQR for each laboratory experiment and total sample size for events. Editorial materials, reviews, summaries of discussions, and conference abstracts were excluded.
Definition of endpoints
The end point of the severity of this study was the diagnosis of severe or critical cases at admission (including other cases requiring ICU care). Severe cases meet any of the following criteria: (1) increased respiratory rate (≥30 beats/min), dyspnea or cyanosis of lips; (2) decreased blood oxygen saturation ≤ 93% after inhalation; (3) Arterial partial pressure of oxygen (PaO2) / oxygen concentration (FiO2) ≤300 mmHg (1 mmHg = 0.133 kPa). Critical cases meet one of the following conditions: (1) respiratory failure requiring mechanical ventilation; (2) shock; or (3) complicated with organ failure requiring ICU monitoring and treatment. Or the severity in accordance with the cap guidelines of the American Thoracic Society (ATS). The mortality rate was determined by death regardless of other causes.
Data abstraction
Data were extracted using a pre-designed excel worksheet. Any differences were resolved by a third investigator. The following data were extracted from the studies: first author; sample size; study design; age of patients; serum levels of cTnI, cTnT, hs-cTn, hs-cTnI, hs-cTnT, CK-MB, and Mb at admission; mortality; and severity.
Statistical analysis
Standardized mean difference (SMD) and 95% confidence interval (CI) for serum levels of cTnI, cTnT, hs-cTn, hs-cTnI, hs-cTnT, CK-MB, and Mb at admission were used to estimate the pooled results. We used fixed effects to evaluate the studies. Publication bias was estimated using a funnel plot. Sensitivity analyses were conducted to assess the impact of each study on the pooled effect. A P value <0.05 was considered statistically significant. All statistical analyses were carried out using Stata version 15.1 (StataCorp, USA).
Results
Study selection and characteristics
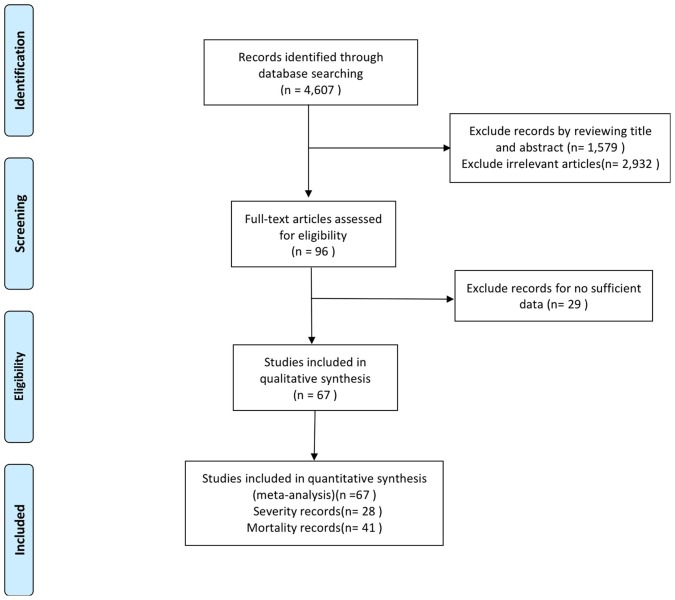
A total of 4607 articles were retrieved based on the keywords. After screening the abstracts and titles of the studies, 96 were selected for full-text evaluation. Among them, 29 were excluded owing to the lack of sufficient data such as median (IQR) or mean (SD). The final 67 studies were included in the meta-analysis and comprised 28 articles comparing the performance of severe vs. non-severe patients, and forty-one studies conducted to compare the performance of survivors vs. non-survivors (Fig. 1 ). The characteristics of the included studies are listed in Table 1 .
Fig. 1.
Flow chart of the study selection process.
Table 1.
Characteristics of the studies in the meta-analysis.
| Study (years) | Country | Mean age, year | Sample size |
Reported biomarkers | |
|---|---|---|---|---|---|
| Severity (%) | Mortality (%) | ||||
| Du et al. [8] | China | 57.6 | – | 179 (12) | cTnI |
| Shi et al. [9] | China | 63 | – | 671 (9) | cTnI |
| Lanza et al. [10] | China | 65.9 | – | 324 (14) | cTnI |
| Pan et al. [11] | China | 65 | – | 124 (72) | cTnI |
| Zhao et al. [12] | China | 64 | – | 83 (59) | cTnI |
| Ozdemir et al. [13] | Turkey | 76 | – | 350 (16) | cTnI |
| Chen et al. [14] | China | 65 | – | 681 (15) | cTnI |
| Tuo et al. [15] | China | 67 | – | 146 (34) | cTnI, Mb |
| Peiro et al. [16] | China | 67.5 | – | 196 (19) | cTnI |
| Guo et al. [17] | China | 61 | – | 74 (62) | cTnI, CK-MB, Mb |
| Zhang et al. [18] | Turkey | 54 | – | 432 (95) | cTnI, CK-MB, Mb |
| Zhu et al. [19] | China | 68 | – | 64 (63) | cTnI, CK-MB, Mb |
| Rodriguez-Nava et al. [20] | USA | 68 | – | 313 (32) | hs-cTn |
| Bennouar et al. [21] | Algeria | 62.3 | – | 120 (31) | hs-cTn |
| Kocayigit et al. [22] | Turkey | 69.6 | – | 103 (50) | hs-cTn, CK-MB |
| Barman et al. [23] | Turkey | 68.5 | – | 607 (17) | hs-cTn, hs-cTnI, CK-MB |
| Luo et al. [24] | China | 56 | – | 403 (25) | hs-cTnI |
| Chen et al. [25] | China | 62 | – | 274 (41) | hs-cTnI |
| Ghio et al. [26] | Italy | 68.6 | – | 405 (31) | hs-cTnI |
| Zhang et al. [27] | China | 64.03 | – | 48 (35) | hs-cTnI |
| Li et al. [28] | China | 57 | – | 102 (15) | hs-cTnI |
| Viana-Llamas et al. [29] | Spain | 71 | – | 609 (21) | hs-cTnI |
| Sit et al. [30] | Turkey | 57.4 | – | 205 (31) | hs-cTnI, CK-MB |
| Wang et al. [31] | China | 64 | – | 344 (39) | hs-cTnI, CK-MB |
| Zhou et al. [32] | China | 56 | – | 191 (28) | hs-cTnI |
| Hu et al. [33] | China | 62 | – | 50 (32) | hs-cTnI |
| Cao et al. [34] | China | 56.6 | – | 101 (35) | hs-cTnI, Mb |
| Primmaz et al. [35] | Switzerland | 64 | – | 129 (19) | hs-cTnT |
| Zhou et al. [36] | China | 59.5 | – | 220 (24) | hs-cTnT |
| Larcher et al. [37] | France | 67 | – | 32 (29) | Hs-cTnT |
| Li et al. [38] | China | 66 | – | 74 (19) | CK-MB |
| Wu et al. [39] | China | 51 | – | 84 (52) | CK-MB |
| Vassiliou et al. [40] | Greece | 62 | – | 38 (26) | CK-MB |
| Cortes-Telles et al. [41] | Mexico | 55 | – | 200 (39) | CK-MB |
| Aladag et al. [42] | Turkey | 68 | – | 50 (30) | CK-MB |
| Ruan et al. [43] | China | – | – | 150 (45) | Mb |
| Wang et al. [44] | China | 63 | – | 202 (16) | Mb |
| Deng et al. [45] | China | 64.5 | – | 262 (20) | Mb |
| Wang et al. [46] | China | 59.2 | – | 293 (40) | Mb |
| Zhao et al. [7] | China | 52 | 77 (26) | 77 (53) | CK-MB, Mb |
| Li et al. [47] | China | 63 | 2068 (23) | 476 (38) | hs-cTnI |
| 1539 (20) | 305 (33) | CK-MB | |||
| – | 311 (33) | Mb | |||
| Cao et al. [48] | China | 50.1 | 175 (10) | – | cTnI |
| Li et al. [49] | China | 50.1 | 299 (8) | – | cTnI |
| Chen et al. [50] | China | – | 126 (16) | – | cTnI |
| Liaqat et al. [51] | Pakistan | 44.6 | 144 (28) | – | cTnI |
| Lano et al. [52] | France | 73.5 | 122 (37) | – | cTnT |
| Vial et al. [53] | Chile | 37 | 88 (20) | – | cTnT |
| Han et al. [54] | China | 63 | 59 (45) | – | cTnI, CK-MB |
| Deng et al. [55] | China | 65 | 45 (60) | – | cTnI, CK-MB |
| Peng et al. [56] | China | 61 | 208 (15) | – | cTnI, CK-MB |
| Peng et al. [57] | China | 62 | 96 (14) | – | cTnI, CK-MB |
| He et al. [58] | China | 63 | 1031 (49) | – | hs-cTnI |
| Taghiloo et al. [59] | Iran | 62 | 61 (36) | – | hs-cTnI |
| Wang et al. [6] | China | 56 | 138 (26) | – | hs-cTnI, CK-MB |
| Zhang et al. [60] | China | 55 | 221 (25) | – | hs-cTnI, CK-MB |
| Rivinius et al. [61] | Germany | 58.6 | 21 (38) | – | hs-cTnT |
| Xiong et al. [62] | China | 58.5 | 116 (47) | – | hs-cTnT, CK-MB, Mb |
| Ma et al. [63] | China | 48 | 84 (24) | – | CK-MB |
| Wang et al. [64] | China | 45 | 242 (15) | – | CK-MB |
| Gong et al. [65] | China | 49 | 177 (15) | – | CK-MB |
| Wu et al. [66] | China | 43.12 | 280 (30) | – | CK-MB |
| Abohamr et al. [67] | Saudi Arabia | 46.36 | 768 (46) | – | CK-MB |
| Saleh et al. [68] | Germany | 67 | 40 (33) | – | CK-MB |
| Zeng et al. [69] | China | 64 | 416 (8) | – | CK-MB, Mb |
| Zheng et al. [70] | China | 49.4 | 88 (35) | – | Mb |
| Li et al. [71] | China | 57 | 193 (34) | – | Mb |
| Yang et al. [72] | China | 56 | 136 (24) | – | Mb |
*Disease severity based on the guidelines for diagnosis and management of COVID-19 by the National Health Commission of China and the World Health Organization interim guidance for COVID-19. cTnI: cardiac troponin I; cTnT: cardiac troponin T; hs-cTn: high-sensitive cardiac troponin; hs-cTnI: high-sensitive cardiac troponin I; hs-cTnT: high-sensitive cardiac troponin T; CK-MB:creatine kinase-MB; Mb: myoglobin.
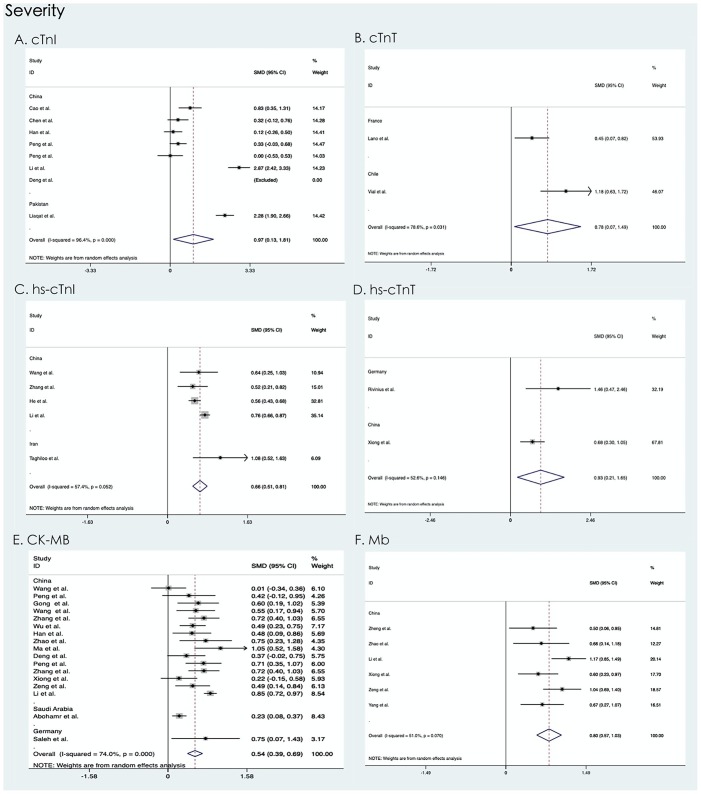
Serum levels of cardiac troponin I, cardiac troponin T, high-sensitive cardiac troponin I, high-sensitive cardiac troponin T, creatine kinase-MB, and myoglobin and severity of COVID-19 infection.
In the 28 (cTnI:8; cTnT:2; hs-cTnI:5; hs-cTnT:2; CK-MB:17; Mb:6) studies comprising 7812 COVID-19-infected patients (severe = 2225 non-severe = 5587) with severity information, increased cTnI (SMD = 0.81 U/L, 95% CI = 0.14–1.48, P = 0.017), cTnT (SMD = 0.78 U/L, 95% CI = 0.07–1.49, P = 0.032), hs-cTnI (SMD = 0.66 pg/mL, 95% CI = 0.51–0.81, P < 0.001), hs-cTnT (SMD = 0.93 U/L, 95% CI = 0.21–1.65, P = 0.012), CK-MB (SMD = 0.54 U/L, 95% CI = 0.39–0.69, P < 0.001), and Mb (SMD = 0.80 U/L, 95% CI = 0.57–1.03, P < 0.001) levels were significantly associated with severe COVID-19 infection. Forest plots of the severity are listed in Fig. 2 .
Fig. 2.
Severity of (a) cTnI, (b) cTnT, (c) hs-cTnI, (d) hs-cTnT, (e) CK-MB, and (f) Mb. SMD: standardized mean difference; CI: confidence interval; cTnI: cardiac troponin I; cTnT: cardiac troponin T; hs-cTnI: high-sensitive cardiac troponin I; hs-cTnT: high-sensitive cardiac troponin T; CK-MB:creatine kinase-MB; Mb: myoglobin.
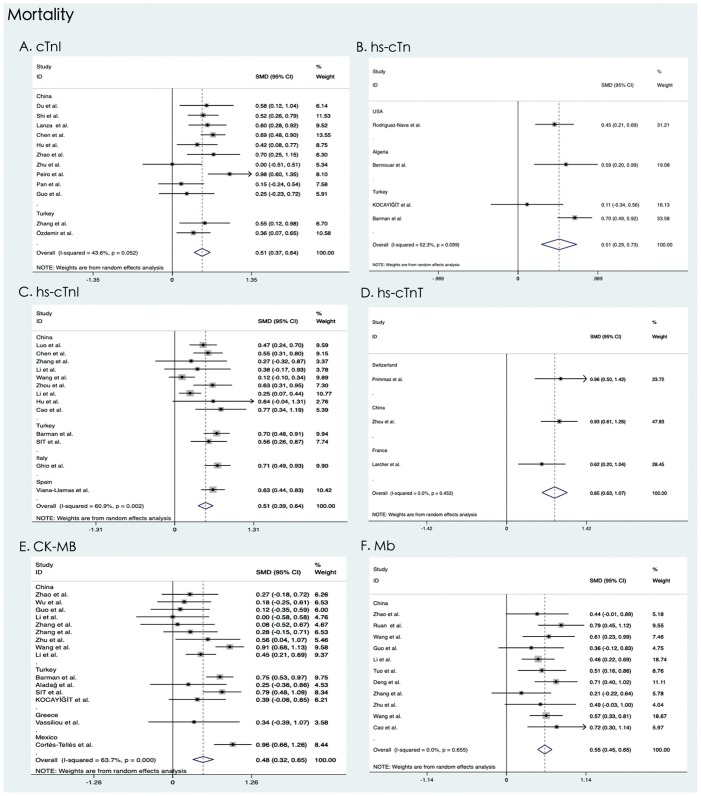
Serum levels of cardiac troponin I, high-sensitive cardiac troponin, high-sensitive cardiac troponin I, high-sensitive cardiac troponin T, creatine kinase-MB, myoglobin, and mortality of COVID-19 infection.
In forty-one (cTnI:12; hs-cTn:4; hs-cTnI:13; hs-cTnT:3; CK-MB:15; Mb:11) studies with mortality information, 9532 patients with COVID-19 infection (deceased = 2858, survived = 6674) were analyzed. High levels of cTnI (SMD = 0.51 U/L, 95% CI = 0.37–0.64, P < 0.001), hs-cTn (SMD = 0.51 ng/L, 95% CI = 0.29–0.73, P < 0.001), hs-cTnI (SMD = 0.51 pg/mL, 95% CI = 0.38–0.63, P < 0.001), hs-cTnT (SMD = 0.85 U/L, 95% CI = 0.63–1.07, P < 0.001), CK-MB (SMD = 0.48 U/L, 95% CI = 0.32–0.65, P < 0.001), and Mb (SMD = 0.55 U/L, 95% CI = 0.45–0.65, P < 0.001) were associated with a remarkable increase in mortality from COVID-19 infection. The forest plots of the mortality are listed in Fig. 3 .
Fig. 3.
The mortality of (a) cTnI, (b) hs-cTn, (c) hs-cTnI, (d) hs-cTnT, (e) CK-MB, (f) Mb. SMD: standardized mean difference; CI: confidence interval; cTnI: cardiac troponin I; hs-cTn: high-sensitive cardiac troponin; hs-cTnI: high-sensitive cardiac troponin I; hs-cTnT: high-sensitive cardiac troponin T; CK-MB: creatine kinase-MB; Mb: myoglobin.
Publication bias and sensitivity analysis
The results of the sensitivity analysis (I2 > 50%) and publication bias (n ≥ 10) showed that overall estimates were not dependent on a single publication (Supplement Figs. S1–S15). The source of heterogeneity and publication bias were mainly due to the different measurement methods within the group.
Discussion
Based on a comprehensive analysis of a large number of studies, this meta-analysis identified cardiac biomarkers at admission (cTnI, cTnT, hs-cTn, hs-cTnI, hs-cTnT, CK-MB, and Mb) related to COVID-19 and analyzed their impact on the disease. One study showed that elevated serum myoglobin was associated with increased hospitalization mortality in patients, while elevated creatine kinase-MB and cardiac troponin I were not [73]. However, this study suggests that an increase in serum cTnI, hs-cTn, hs-cTnI, hs-cTnT, CK-MB, and Mb except for cTnT is directly related to COVID-19 mortality, while a raise in serum cTnI, cTnT, hs-cTnI, hs-cTnT, CK-MB, or Mb except for hs-cTn is directly related to the severity of COVID-19. Our meta-analysis of 16,791 samples suggests that increased cardiac biomarkers at admission in patients with COVID-19 infection are related to increased risk of disease and death. The present study’s findings of increase in mortality and severity risk among COVID-19 patients with cardiac abnormality biomarkers test are consistent with previous narrative reviews [9,[74], [75], [76]].
In COVID-19 infection patients, in addition to the typical clinical manifestations of the respiratory system, there is also a certain proportion of patients with cardiac involvement in whom myocardial injury is more common [77]. Published studies showed that 7.2–19.7% of COVID-19 patients [6,9,78,32] had acute heart injury, defined as cardiac troponin I above the 99th percentile. Studies also revealed that patients with heart injuries had a higher mortality rate [9,79].
There are several possible mechanisms of COVID-19-induced myocardial injury: 1. Myocardial injury that is caused by an imbalance of oxygen supply and demand. Severe clinical symptoms such as arrhythmia, severe tachycardia, anaemia, and respiratory failure in patients with COVID-19 are related to increased cTnI due to myocardial injury [80]; 2. Myocardial injury that is directly caused by viral invasion. The SARS-CoV-2 virus enters human cells by binding with angiotensin-converting enzyme 2 (ACE2) receptors, which is expressed in the heart and lungs. The binding of the SARS-CoV-2 virus to ACE2 receptors may be the cause of acute myocardial and lung injury [1]; 3. Excessive immune response further damages the heart, leading to ischemia and hypoxia of the heart tissue, and this overload of the heart maintains a high output and low resistance state. This leads to further ischemic injury and changes in laboratory cardiac markers, such as CK-MB, troponin I, and N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) increases [5]. Myocardial injury resulting in an excessive immune response mechanism can increase the severity of the disease and mortality.
Evidence suggested that five (12%) of 41 COVID-19 cases had virus-related myocardial injury that mainly manifested as increased high-sensitive cardiac troponin I (hs-cTnI) (>28 pg/mL) [3] and changes in laboratory cardiac biomarkers, such as increased creatine kinase-MB and cardiac troponin I, which can reflect ischemic damage of the heart [5]. There can also be progressive myocardial injury in COVID-19 patients. Clinical evidence from Wuhan showed that most of the 112 COVID-19 patients had normal troponin level at admission but then showed a gradual increase with clinical deterioration and systemic inflammation. The data displayed an increase in 42 (37.5%) patients during hospitalization and a significant increase in cardiac troponin I level in the week before death [55]. Another study reported that, four days after the onset of symptoms, the high-sensitive cardiac troponin I (hs-cTnI) level was 8.8 pg/mL in non-survivors and 2.5 pg/mL in survivors [81]. An elevated level of serum myoglobin (≥306.5 μg/L) was related to greater in-hospital mortality among non-survivors [73]. Elevated hs-cTnI is also associated with increased utilization of non-invasive and invasive mechanical ventilation as well as acute respiratory distress syndrome (ARDS) [82]. However, cardiac biomarker levels at admission are also related to the mortality of COVID-19 patients. High levels of high-sensitive cardiac troponin I (hs-cTnI) (≥6.126 pg/mL) and creatine kinase-MB at admission were associated with increased mortality [83]. Furthermore, creatine kinase-MB and cardiac troponin I have prognostic value in the prognosis of COVID-19 [84]. Elevated cTnT levels are common in patients with ARDS without electrocardiographic evidence of myocardial ischemia. Therefore, potential myocardial injury can be detected earlier by observing these biomarker levels at admission and comparing them to those during hospitalization. Once abnormal changes in myocardial markers are detected in COVID-19 patients at admission, the attending doctor can administer timely treatment to reduce the risk of serious disease and improve the prognosis of patients.
Limitations
A limitation of this study could be the source region of the sample. Although samples from different countries were included, Chinese samples were predominant in this study. Some cardiac biomarkers (hs-cTn, hs-cTnT, and cTnT) were involved in only a limited number of studies, which may have led to some bias in the results. For the comparison of cardiac markers and ECG, there was no valid meta-analysis due to the lack of original study data. Despite these limitations, we believe that the large sample from various publications can somewhat attenuate the limitations.
Conclusion
The meta-analysis showed a clinically meaningful relationship between serum levels of cardiac markers and the severity and mortality of COVID-19 infection. The results suggest that the cardiac biomarkers of cTnI, cTnT, hs-cTn, hs-cTnI, hs-cTnT, CK-MB, and Mb have the potential to predict poor prognosis of COVID-19, especially in critically ill patients. In conclusion, detection of elevated serum cardiac biomarkers at admission and during hospitalization is invaluable for reducing mortality and severity in COVID-19 patients.
Contributorship statement
Wen An and Qiuyang Wang designed the model and the computational framework, and analyzed the data. Ju-seop Kang was involved in planning and supervised the work. Tae-Eun Kim discussed the results and commented on the manuscript.
Funding
No funding sources.
Competing interests
None declared.
Ethical approval
Not required.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jiph.2021.07.016.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Turner A.J., Hiscox J.A., Hooper N.M. ACE2: from vasopeptidase to SARS virus receptor. Trends Pharmacol Sci. 2004;25(6):291–294. doi: 10.1016/j.tips.2004.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boeddinghaus J., Nestelberger T., Koechlin L., Wussler D., Lopez-Ayala P., Walter J.E., et al. Early diagnosis of myocardial infarction with point-of-care high-sensitivity cardiac troponin I. J Am Coll Cardiol. 2020;75(10):1111–1124. doi: 10.1016/j.jacc.2019.12.065. [DOI] [PubMed] [Google Scholar]
- 5.Li L., Zhou Q., Xu J. Changes of laboratory cardiac markers and mechanisms of cardiac injury in coronavirus disease 2019. Biomed Res Int. 2020;2020 doi: 10.1155/2020/7413673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao W., Zha X., Wang N., Li D., Li A., Yu S. Clinical characteristics and durations of hospitalized patients with COVID-19 in Beijing: a retrospective cohort study. medRxiv. 2021 2020.2003.2013.20035436. [Google Scholar]
- 8.Du R.H., Liang L.R., Yang C.Q., Wang W., Cao T.Z., Li M., et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5) doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lanza G.A., De Vita A., Ravenna S.E., D’Aiello A., Covino M., Franceschi F., et al. Electrocardiographic findings at presentation and clinical outcome in patients with SARS-CoV-2 infection. Europace. 2021;23(1):123–129. doi: 10.1093/europace/euaa245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan F., Yang L., Li Y., Liang B., Li L., Ye T., et al. Factors associated with death outcome in patients with severe coronavirus disease-19 (COVID-19): a case-control study. Int J Med Sci. 2020;17(9):1281–1292. doi: 10.7150/ijms.46614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao S., Lin Y., Zhou C., Wang L., Chen X., Clifford S.P., et al. Short-term outcomes of patients with COVID-19 undergoing invasive mechanical ventilation: a retrospective observational study from Wuhan, China. Front Med (Lausanne) 2020;7 doi: 10.3389/fmed.2020.571542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ozdemir I.H., Ozlek B., Cetin N. Permanent atrial fibrillation portends poor outcomes in hospitalized patients with COVID-19: a retrospective observational study. J Electrocardiol. 2021;65:113–120. doi: 10.1016/j.jelectrocard.2021.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen F.F., Zhong M., Liu Y., Zhang Y., Zhang K., Su D.Z., et al. The characteristics and outcomes of 681 severe cases with COVID-19 in China. J Crit Care. 2020;60:32–37. doi: 10.1016/j.jcrc.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tuo H., Li W., Tang L., He B., Yao B., Mao P., et al. Cardiac biomarker abnormalities are closely related to prognosis in patients with COVID-19. Int Heart J. 2021;62(1):148–152. doi: 10.1536/ihj.20-180. [DOI] [PubMed] [Google Scholar]
- 16.Peiro O.M., Carrasquer A., Sanchez-Gimenez R., Lal-Trehan N., Del-Moral-Ronda V., Bonet G., et al. Biomarkers and short-term prognosis in COVID-19. Biomarkers. 2021;26(2):119–126. doi: 10.1080/1354750X.2021.1874052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guo H., Shen Y., Wu N., Sun X. Myocardial injury in severe and critical coronavirus disease 2019 patients. J Card Surg. 2021;36(1):82–88. doi: 10.1111/jocs.15164. [DOI] [PubMed] [Google Scholar]
- 18.Zhang X.B., Hu L., Ming Q., Wei X.J., Zhang Z.Y., Chen L.D., et al. Risk factors for mortality of coronavirus disease-2019 (COVID-19) patients in two centers of Hubei province, China: a retrospective analysis. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0246030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu Q., Zhang W., Wang Q., Liu J.H., Wu C.H., Luo T., et al. Clinical characteristics and outcome of 64 patients with severe COVID-19. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(8):659–664. doi: 10.3760/cma.j.cn112147-20200308-00275. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez-Nava G., Yanez-Bello M.A., Trelles-Garcia D.P., Chung C.W., Chaudry S., Khan A.S., et al. Clinical characteristics and risk factors for death of hospitalized patients with COVID-19 in a community hospital: a retrospective cohort study. Mayo Clin Proc Innov Qual Outcomes. 2021;5(1):1–10. doi: 10.1016/j.mayocpiqo.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bennouar S., Cherif A.B., Kessira A., Bennouar D.E., Abdi S. Vitamin D deficiency and low serum calcium as predictors of poor prognosis in patients with severe COVID-19. J Am Coll Nutr. 2021;40(2):104–110. doi: 10.1080/07315724.2020.1856013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kocayigit H., Ozmen Suner K., Tomak Y., Demir G., Kocayigit I., Yaylaci S., et al. Characteristics and outcomes of critically ill patients with covid-19 in Sakarya, Turkey: a single centre cohort study. Turk J Med Sci. 2021;51(2):440–447. doi: 10.3906/sag-2005-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barman H.A., Atici A., Sahin I., Alici G., Aktas Teki E., Baycan O.F., et al. Prognostic significance of cardiac injury in COVID-19 patients with and without coronary artery disease. Coron Artery Dis. 2020 doi: 10.1097/MCA.0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luo X., Xia H., Yang W., Wang B., Guo T., Xiong J., et al. Characteristics of patients with COVID-19 during epidemic ongoing outbreak in Wuhan, China. medRxiv. 2020 2020.2003.2019.20033175. [Google Scholar]
- 25.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghio S., Baldi E., Vicentini A., Lenti M.V., Di Sabatino A., Di Matteo A., et al. Cardiac involvement at presentation in patients hospitalized with COVID-19 and their outcome in a tertiary referral hospital in Northern Italy. Intern Emerg Med. 2020;15(8):1457–1465. doi: 10.1007/s11739-020-02493-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang F., Yang D., Li J., Gao P., Chen T., Cheng Z., et al. Myocardial injury is associated with in-hospital mortality of confirmed or suspected COVID-19 in Wuhan, China: a single center retrospective cohort study. medRxiv. 2020 2020.2003.2021.20040121. [Google Scholar]
- 28.Li K., Chen D., Chen S., Feng Y., Chang C., Wang Z., et al. Radiographic findings and other predictors in adults with Covid-19. medRxiv. 2020 doi: 10.1186/s12931-020-01411-2. 2020.2003.2023.20041673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Viana-Llamas M.C., Arroyo-Espliguero R., Silva-Obregon J.A., Uribe-Heredia G., Nunez-Gil I., Garcia-Magallon B., et al. Hypoalbuminemia on admission in COVID-19 infection: an early predictor of mortality and adverse events. A retrospective observational study. Med Clin (Barc) 2021;156(9):428–436. doi: 10.1016/j.medcli.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sit O., Oksen D., Atici A., Barman H.A., Alici G., Pala A.S., et al. Prognostic significance of Tp-e interval and Tp-e/QTc ratio in patients with COVID-19. Eur Rev Med Pharmacol Sci. 2021;25(8):3272–3278. doi: 10.26355/eurrev_202104_25736. [DOI] [PubMed] [Google Scholar]
- 31.Wang Y., Lu X., Li Y., Chen H., Chen T., Su N., et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201(11):1430–1434. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu B., Wang D., Hu C., Hu M., Zhu F., Xiang H., et al. Clinical features of critically ill patients with COVID-19 infection in China. Res Square. 2020 [Google Scholar]
- 34.Cao Y., Han X., Gu J., Li Y., Liu J., Alwalid O., et al. Prognostic value of baseline clinical and HRCT findings in 101 patients with severe COVID-19 in Wuhan, China. Sci Rep. 2020;10(1):17543. doi: 10.1038/s41598-020-74497-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Primmaz S., Le Terrier C., Suh N., Ventura F., Boroli F., Bendjelid K., et al. Preparedness and reorganization of care for coronavirus disease 2019 patients in a Swiss ICU: characteristics and outcomes of 129 patients. Crit Care Explor. 2020;2(8):e0173. doi: 10.1097/CCE.0000000000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou S., Mi S., Luo S., Wang Y., Ren B., Cai L., et al. Risk factors for mortality in 220 patients with COVID-19 in Wuhan, China: a single-center, retrospective study. Ear Nose Throat J. 2021;100(2_suppl):140S–147S. doi: 10.1177/0145561320972608. [DOI] [PubMed] [Google Scholar]
- 37.Larcher R., Besnard N., Akouz A., Rabier E., Teule L., Vandercamere T., et al. Admission high-sensitive cardiac troponin t level increase is independently associated with higher mortality in critically ill patients with COVID-19: a multicenter study. J Clin Med. 2021;10(8) doi: 10.3390/jcm10081656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li J., Xu G., Yu H., Peng X., Luo Y., Cao C. Clinical characteristics and outcomes of 74 patients with severe or critical COVID-19. Am J Med Sci. 2020;360(3):229–235. doi: 10.1016/j.amjms.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vassiliou A.G., Keskinidou C., Jahaj E., Gallos P., Dimopoulou I., Kotanidou A., et al. ICU admission levels of endothelial biomarkers as predictors of mortality in critically ill COVID-19 patients. Cells. 2021;10(1) doi: 10.3390/cells10010186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cortes-Telles A., Lopez-Romero S., Mancilla-Ceballos R., Ortiz-Farias D.L., Nunez-Caamal N., Figueroa-Hurtado E. Risk factors for mortality in hospitalized patients with COVID-19: an overview in a mexican population. Tuberc Respir Dis (Seoul) 2020;83(Suppl. 1):S46–S54. doi: 10.4046/trd.2020.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aladag N., Atabey R.D. The role of concomitant cardiovascular diseases and cardiac biomarkers for predicting mortality in critical COVID-19 patients. Acta Cardiol. 2021;76(2):132–139. doi: 10.1080/00015385.2020.1810914. [DOI] [PubMed] [Google Scholar]
- 43.Ruan Q., Yang K., Wang W., Jiang L., Song J. Correction to: clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(6):1294–1297. doi: 10.1007/s00134-020-06028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang L., He W.B., Yu X.M., Liu H.F., Zhou W.J., Jiang H. Prognostic value of myocardial injury in patients with COVID-19. Zhonghua Yan Ke Za Zhi. 2020;56(0):E009. doi: 10.3760/cma.j.cn112148-20200313-00202. [DOI] [PubMed] [Google Scholar]
- 45.Deng P., Ke Z., Ying B., Qiao B., Yuan L. The diagnostic and prognostic role of myocardial injury biomarkers in hospitalized patients with COVID-19. Clin Chim Acta. 2020;510:186–190. doi: 10.1016/j.cca.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Z., Ye D., Wang M., Zhao M., Li D., Ye J., et al. Clinical features of COVID-19 patients with different outcomes in Wuhan: a retrospective observational study. Biomed Res Int. 2020;2020 doi: 10.1155/2020/2138387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li C., Jiang J., Wang F., Zhou N., Veronese G., Moslehi J.J., et al. Longitudinal correlation of biomarkers of cardiac injury, inflammation, and coagulation to outcome in hospitalized COVID-19 patients. J Mol Cell Cardiol. 2020;147:74–87. doi: 10.1016/j.yjmcc.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cao M., Zhang D., Wang Y., Lu Y., Zhu X., Li Y., et al. Clinical features of patients infected with the 2019 novel coronavirus (COVID-19) in Shanghai, China. medRxiv. 2020 [Google Scholar]
- 49.Ling Y., Zhang J., Li W., Zhang X., Jin Y., et al. Clinical characteristics of SARS-CoV-2 infections involving 325 hospitalized patients outside Wuhan. Res Square. 2020 [Google Scholar]
- 50.Chen C., Chen C., Yan J.T., Zhou N., Zhao J.P., Wang D.W. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(7):567–571. doi: 10.3760/cma.j.cn112148-20200225-00123. [DOI] [PubMed] [Google Scholar]
- 51.Liaqat A., Ali-Khan R.S., Asad M., Rafique Z. Evaluation of myocardial injury patterns and ST changes among critical and non-critical patients with coronavirus-19 disease. Sci Rep. 2021;11(1):4828. doi: 10.1038/s41598-021-84467-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lano G., Braconnier A., Bataille S., Cavaille G., Moussi-Frances J., Gondouin B., et al. Risk factors for severity of COVID-19 in chronic dialysis patients from a multicentre French cohort. Clin Kidney J. 2020;13(5):878–888. doi: 10.1093/ckj/sfaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vial M.R., Peters A., Perez I., Spencer-Sandino M., Barbe M., Porte L., et al. Covid-19 in South America: clinical and epidemiological characteristics among 381 patients during the early phase of the pandemic in Santiago, Chile. BMC Infect Dis. 2020;20(1):955. doi: 10.1186/s12879-020-05665-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Han Y., Zhang H., Mu S., Wei W., Jin C., Tong C., et al. Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: a retrospective and observational study. Aging (Albany NY) 2020;12(12):11245–11258. doi: 10.18632/aging.103372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Deng Q., Hu B., Zhang Y., Wang H., Zhou X., Hu W., et al. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int J Cardiol. 2020;311:116–121. doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peng Y., Meng K., He M., Zhu R., Guan H., Ke Z., et al. Clinical characteristics and prognosis of 244 cardiovascular patients suffering from coronavirus disease in Wuhan, China. J Am Heart Assoc. 2020;9(19) doi: 10.1161/JAHA.120.016796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peng Y., M K.K., Guan H., Leng L., Zhu R., Wang B., et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Chin J Cardiol. 2020;48:450–455. doi: 10.3760/cma.j.cn112148-20200220-00105. [DOI] [PubMed] [Google Scholar]
- 58.He X., Wang L., Wang H., Xie Y., Yu Y., Sun J., et al. Factors associated with acute cardiac injury and their effects on mortality in patients with COVID-19. Sci Rep. 2020;10(1):20452. doi: 10.1038/s41598-020-77172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Taghiloo S., Aliyali M., Abedi S., Mehravaran H., Sharifpour A., Zaboli E., et al. Apoptosis and immunophenotyping of peripheral blood lymphocytes in Iranian COVID-19 patients: clinical and laboratory characteristics. J Med Virol. 2021;93(3):1589–1598. doi: 10.1002/jmv.26505. [DOI] [PubMed] [Google Scholar]
- 60.Zhang G., Hu C., Luo L., Fang F., Chen Y., Li J., et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rivinius R., Kaya Z., Schramm R., Boeken U., Provaznik Z., Heim C., et al. COVID-19 among heart transplant recipients in Germany: a multicenter survey. Clin Res Cardiol. 2020;109(12):1531–1539. doi: 10.1007/s00392-020-01722-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xiong S., Liu L., Lin F., Shi J., Han L., Liu H., et al. Clinical characteristics of 116 hospitalized patients with COVID-19 in Wuhan, China: a single-centered, retrospective, observational study. BMC Infect Dis. 2020;20(1):787. doi: 10.1186/s12879-020-05452-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ma K.-L., Liu Z.-H., Cao C.-F., Liu M.-K., Liao J., Zou J.-B., et al. COVID-19 myocarditis and severity factors: an adult cohort study. medRxiv. 2020 2020.2003.2019.20034124. [Google Scholar]
- 64.Wang G., Wu C., Zhang Q., Wu F., Yu B., Lv J., et al. Epidemiological and clinical features of corona virus disease 2019 (COVID-19) in Changsha, China. Lancet. 2020 [Google Scholar]
- 65.Gong J., Ou J., Qiu X., Jie Y., Chen Y., Yuan L., et al. Multicenter development and validation of a novel risk nomogram for early prediction of severe 2019-novel coronavirus pneumonia. Lancet. 2020 [Google Scholar]
- 66.Wu J., Li W., Shi X., Chen Z., Jiang B., Liu J., et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19) J Intern Med. 2020;288(1):128–138. doi: 10.1111/joim.13063. [DOI] [PubMed] [Google Scholar]
- 67.Abohamr S.I., Abazid R.M., Aldossari M.A., Amer H.A., Badhawi O.S., Aljunaidi O.M., et al. Clinical characteristics and in-hospital mortality of COVID-19 adult patients in Saudi Arabia. Saudi Med J. 2020;41(11):1217–1226. doi: 10.15537/smj.2020.11.25495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Saleh A., Matsumori A., Abdelrazek S., Eltaweel S., Salous A., Neumann F.J., et al. Myocardial involvement in coronavirus disease 19. Herz. 2020;45(8):719–725. doi: 10.1007/s00059-020-05001-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zeng J.H., Wu W.B., Qu J.X., Wang Y., Dong C.F., Luo Y.F., et al. Cardiac manifestations of COVID-19 in Shenzhen, China. Infection. 2020;48(6):861–870. doi: 10.1007/s15010-020-01473-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zheng Y., Xu H., Yang M., Zeng Y., Chen H., Liu R., et al. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li Z., Wu M., Yao J., Guo J., Liao X., Song S., et al. Caution on kidney dysfunctions of COVID-19 patients. medRxiv. 2020 2020.2002.2008.20021212. [Google Scholar]
- 72.Yang Q., Xie L., Zhang W., Zhao L., Wu H., Jiang J., et al. Analysis of the clinical characteristics, drug treatments and prognoses of 136 patients with coronavirus disease 2019. J Clin Pharm Ther. 2020;45(4):609–616. doi: 10.1111/jcpt.13170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Su M., Wang Y., Peng J., Wu M.J., Deng W., Yang Y.S. Elevated cardiac biomarkers are associated with increased mortality for inpatients with COVID-19: a retrospective case-control study. J Clin Anesth. 2020;65 doi: 10.1016/j.jclinane.2020.109894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shi S., Qin M., Cai Y., Liu T., Shen B., Yang F., et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Qiang Z., Wang B., Garrett B.C., Rainey R.P., Superko H.R. Coronavirus disease 2019: a comprehensive review and meta-analysis on cardiovascular biomarkers. Curr Opin Cardiol. 2021;36(3):367–373. doi: 10.1097/HCO.0000000000000851. [DOI] [PubMed] [Google Scholar]
- 76.Dy L.F., Lintao R.C.V., Cordero C.P., Cabaluna I.T.G., Dans L.F. Prevalence and prognostic associations of cardiac abnormalities among hospitalized patients with COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11(1):8449. doi: 10.1038/s41598-021-87961-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Madjid M., Solomon S., Vardeny O. ACC clinical bulletin cardiac implications of novel coronavirus (COVID-19) Am Coll Cardiol Extended Learn Suppl Tape. 2020 [Google Scholar]
- 78.Wan S., Xiang Y., Fang W., Zheng Y., Li B., Hu Y., et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020;92(7):797–806. doi: 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li L., Zhang S., He B., Chen X., Zhao Q. Retrospective study of risk factors for myocardial damage in patients with critical coronavirus disease 2019 in Wuhan. J Am Heart Assoc. 2020;9(15) doi: 10.1161/JAHA.120.016706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sarkisian L., Saaby L., Poulsen T.S., Gerke O., Hosbond S., Jangaard N., et al. Prognostic impact of myocardial injury related to various cardiac and noncardiac conditions. Am J Med. 2016;129(5) doi: 10.1016/j.amjmed.2015.12.009. 506–514 e501. [DOI] [PubMed] [Google Scholar]
- 81.B K.A., Chaudhuri D. A review of acute myocardial injury in coronavirus disease 2019. Cureus. 2020;12(6):e8426. doi: 10.7759/cureus.8426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gordon J.S., Drazner M.H. Biomarkers of cardiac stress and cytokine release syndrome in COVID-19: a review. Curr Heart Fail Rep. 2021:1–6. doi: 10.1007/s11897-021-00505-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wu C., Hu X., Song J., Du C., Xu J., Yang D., et al. Heart injury signs are associated with higher and earlier mortality in coronavirus disease 2019 (COVID-19) medRxiv. 2020 2020.2002.2026.20028589. [Google Scholar]
- 84.Aboughdir M., Kirwin T., Abdul Khader A., Wang B. Prognostic value of cardiovascular biomarkers in COVID-19: a review. Viruses. 2020;12(5) doi: 10.3390/v12050527. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.