Abstract
Study Objectives:
Sleep is an essential normal function for children’s growth and development, but over the years, lifestyle changes have resulted in insufficient sleep, a factor that may be associated with increased childhood obesity. The aim of this study was to evaluate the association between sleep duration and sleep patterns separately on weekdays and weekends regarding children’s weight status.
Methods:
This study was conducted among Greek students (55.1% girls) in 2014–2016. Children’s weight status was classified according to the International Obesity Task Force tables and guidelines. Sleep duration was determined based on the sleep and wake time that children reported, separately for weekdays and weekends. Classification and regression tree analysis was used to derive sleep patterns and evaluate their relation to children’s weight status.
Results:
Multiadjusted analysis revealed an inverse association between average duration of sleep on weekdays and weekends with the likelihood of being overweight/obese (odds ratio per 1 hour 0.82; 95% confidence interval, 0.73–0.92). This was more prominent on weekends than on weekdays. Children who had lower duration on weekdays, but catch-up sleep duration on weekends, were 2% (95% confidence interval, 0.97–0.99) less likely to be overweight/obese compared to those children having both less or increased sleep duration on weekdays and weekends.
Conclusions:
Sleep duration and sleep patterns seem to be associated with childhood weight status. Interventions should be developed to educate parents on the importance of an adequate sleep duration and healthy sleep patterns for their children’s healthy development.
Citation:
Kanellopoulou A, Notara V, Magriplis E, et al. Sleeping patterns and childhood obesity: an epidemiological study in 1,728 children in Greece. J Clin Sleep Med. 2021;17(5):1093–1101.
Keywords: sleep patterns, sleep duration, overweight and obesity, children, CART analysis
BRIEF SUMMARY
Current Knowledge/Study Rationale: In recent years, sleep duration has begun to be studied. However, the aim of this study was to investigate the effect of sleep duration and sleep patterns during weekdays and weekends, separately, on the likelihood of overweight/obesity in pre-adolescents in Greece.
Study Impact: Nowadays, there are still uncertainties about sufficient sleep patterns. Parents need to understand their role in ensuring a healthy sleep pattern in their children.
INTRODUCTION
Sleep is a normal, necessary biological process, which affects the human body in multiple ways.1 Proper and adequate sleep enhances the immune function2 and may reduce the likelihood of developing a number of diseases, such as cardiovascular disease,3 diabetes,4 and stroke.5 It has also been found to improve memory and to help learning6 and to regulate the secretion of growth hormone,7 which is responsible for the physical development of children and adolescents. It has been proposed that the body’s ability to regulate its endocrine function is affected by sleep duration and patterns.8 Sleep deprivation leads to the deregulation of 2 appetite-related hormones, ghrelin9 and leptin.10 Ghrelin is a hormone that increases the feeling of hunger, and leptin regulates the feeling of satiety. Disturbed sleep may result in an increased feeling of hunger and food consumption through this deregulation.11 Moreover, insulin, which is associated with sleep duration12 and responsible for blood sugar levels, may also be deregulated, resulting in increased blood levels, which leads to increased fat deposition—ie, it increases the risk of being overweight and of obesity.13 Children, however, often have habits that affect sleep, such as the time they spend in front of screens.14 It has been found that many hours of use of electronic devices during a day are connected with symptoms of insomnia in children.15 Sleep-specific guidelines have been developed by the American Academy of Sleep Medicine to enhance the healthy growth of children. Specifically, it is recommended that children should sleep 9–12 hours on a daily basis.16 In recent years, it has been observed that children adopt patterns of restricted sleep17 as they transition toward adolescence. Also, children have different schedules on weekdays compared to weekends, since they spend most of their time at school on weekdays and have homework and other school-related activities. This may lead to adopting different sleep duration and patterns on weekends compared to weekdays.18
In the GRECO study, in which researchers assessed average sleep durations for weekdays and weekends, longer sleep duration decreased the likelihood of overweight/obesity.19 Another cross-sectional study with more than 5,000 children revealed that the shorter the sleep duration the higher the body mass index (BMI) was, while the more hours children slept during weekends/holidays may improve the risk of childhood overweight/obesity.20 A systematic review of 103 papers revealed a significant inverse association between sleep duration and children’s weight status.21 Another recent cross-sectional study on children and adolescents indicated that shorter duration of sleep on weekdays and greater duration on weekends is associated with eating in the absence of hunger, which may lead to excess weight gain.22
Although the association between sleep duration and obesity status has been well-studied, there is not sufficient evidence on the association between children’s sleep patterns separately on weekdays and weekends and their weight status. Therefore, the main aim of the present study was to investigate the result of sleep duration and patterns during weekdays and weekends, separately, on the likelihood of overweight/obesity in children aged 10–12 years in Greece. Moreover, and since different lifestyles have been reported in the literature between people living in the greater Athens metropolitan area and other provincial cities of Greece,19 the role of residence in the aforementioned hypothesis was also examined.
METHODS
Design and setting
This is a cross-sectional, school-based survey, conducted in the school years 2014–2015 and 2015–2016. A total of 47 schools was randomly selected, through a stratified sampling, from various Greek areas, including the greater Athens metropolitan area, the Peloponnese peninsula (Sparta, Kalamata, and Pyrgos), and Heraklion in Crete. In particular, based on the school listings of each regional Primary Education Office of the Greek Ministry of Education, a predefined number of schools (according to the population density) was selected, using a special function of MS Excel software (ie, RAND). The sampling areas were proportionally obtained, covering approximately 75% of the total population and representing large urban and rural municipalities.
Participants and sampling procedure
All children aged 10–12 years attending the fifth and sixth grade of the selected primary schools were invited to participate voluntarily in the study. The participation rate within schools ranged from 95% to 100%, without any significant differences between the studied areas. A total of 1,728 children (933 girls) were enrolled. Trained investigators (ie, dietitians, registered nurses, and physicians) recorded the anthropometric characteristics of the children and performed a face-to-face interview in which several other characteristics, behaviors (including sleep patterns), and attitudes were recorded. For the present analysis, only children with recorded sleep patterns were analyzed; hence, the working sample was 1,482 children (55.1% girls). No differences in their basic characteristics were found between children who answered about their sleep patterns and those who did not answer.
Statistical power analysis
An a priori statistical power analysis showed that the sample was adequate for the evaluation of minimum detectable standardized, 2-sided differences of 20% between obesity groups and various exposure factors (including sleep pattern categories), with 85% statistical power at a 5% significance level.
Ethical approval
This study received approval from the Institute of Educational Policy of the Greek Ministry of Education (F15/396/72005/C1), and it was carried out in accordance with the Declaration of Helsinki (1989). The school directors, teachers, parents, and students were informed about the aims and procedures of the study. Before children’s participation, parents signed a consent form.
Measurements
Children completed anonymously, in the school setting, without the presence of their parents and through face-to-face interviews with the study’s investigators, a special questionnaire that recorded various demographic characteristics of children (age, sex, region of residence) and daily activities (ie, physical activity, dietary habits, and other behaviors, including sleep duration on a daily and weekend basis). A validated semiquantitative food frequency questionnaire23 was used to evaluate children’s dietary habits recalling from a “typical” week. Information on frequency consumption of various foods, food groups, and beverages, as well as information on the number of meals per day, including snacks, was gathered. To assist children and strengthen the accuracy of their responses, they were provided with practical examples by specially trained investigators.
Children’s height (in m) and weight (in kg) were measured using a tape measure and a scale, with children wearing skin-tight clothes and without shoes. Anthropometric data were used to calculate children’s BMI (kg/m2). Children’s specific age (by 0.5 years) and sex were taken into consideration for the evaluation of weight status in relation to the derived BMI. The International Obesity Task Force BMI cut-offs that link BMI values at the age of 18 years (ie, 18.5, 25, and 30 kg/m2) in child centiles were used to assess the prevalence of childhood underweight, normal weight, overweight, and obesity.24
Adherence to the Mediterranean diet was assessed through a Mediterranean diet quality scale for children and adolescents (the KIDMED score). This index ranges from 0 to 12 and was divided into 3 categories (≤ 3, very low-quality diet; 4–7, diet that needs improvement to conform to Mediterranean patterns; ≥ 8, optimal Mediterranean diet).25 Children’s physical and sedentary activities were recorded using the validated Physical Activity and Lifestyle Questionnaire (PALQ).26 Involvement in usual activities, such as participation in sports clubs, jogging, and swimming, was recorded on a weekly basis and was coded as a binary variable (yes/no) based on whether children achieved at least 60 minutes of physical activity daily according to World Health Organization recommendations. Sedentary activities were evaluated through total screen time exposure, including the total hours that children watched television (TV) or used any electronic device.
Sleep patterns were assessed through the time children went to bed (bedtime) and the time they woke up. Sleep duration (in hours, minutes) was calculated as the interval between the reported bedtime and the reported hour children usually woke up. Given that children usually have different sleep habits throughout the week, sleep duration was calculated separately for weekdays and weekends. Here it should be pointed out that given that sleep duration was based on a self-reported bedtime and wake-up time, it was actually a self-reported sleep duration.
Statistical methods
Continuous variables are presented as mean value ± standard deviation, while categorical variables are presented as absolute and relative (%) frequencies. Between-mean group differences were evaluated through the independent samples t test, while associations between categorical variables were evaluated through the Pearson chi-square test. Multiple binary logistic regression was used to estimate adjusted odds ratios and their 95% confidence intervals between sleep duration and children’s weight status. Multicollinearity among the independent variables was evaluated through the variance inflation factor and tolerance. The classification and regression tree (CART) analysis,27 a simple and powerful analytic tool for determining the most significant factors, identifying interactions, and crafting a potent explanatory model, was used to assess the relationship between children’s weight status and several contributing factors, including sex, sleep duration, and sleep patterns. All analyses were conducted using Stata 15.0 (M. Psarros & Assoc., Sparti, Greece) at the 5% significance level.
RESULTS
Sleep duration and patterns
Data analysis regarding sleep time revealed that children had different sleep patterns on the weekends than on weekdays. Specifically, 25% of children went to bed before 21:00 on weekdays, 42% of children went to bed between 21:00 and 22:00, and the rest (33%) went to bed after 22:00 (P for sex differences = .60). The vast majority of children, ie, 95%, woke up between 07:00 and 07:55 on weekdays (P for sex differences = .58). The mean duration of sleep on weekdays was 9.05 (± 0.9) hours (P for sex differences = .10). Regarding weekends, the mean duration of sleep was 10.3 (± 1.4) hours (girls slept 0.5 hour more than boys; P < .001). Only 20% of children woke up before 08:00, whereas 55% woke up between 08:00 and 10:00, and the remaining 14% woke up between 10:00 and 11:00; girls woke up earlier than boys on weekends (P < .001). In addition, 52% of children went to bed before 22:00, and 10% went to bed after 23:00. Girls tended to go earlier to bed than boys on weekends (P < .001). Moreover, children slept approximately 1.5 hours more on weekends compared to weekdays (10.30 ± 1.48 vs 9.08 ± 0.95; P < .001); 45.3% of children had insufficient sleep duration (ie, less than 9 hours) on weekdays, while only 22.3% slept for less than 9 hours on weekends. Furthermore, 2 out of 3 children (ie, 67%) who went to bed before 23:00 on weekdays did so after 23:00 on weekends.
Sleep duration, patterns, and overweight/obesity
Overall, the prevalence of overweight was 21.7% and obesity was 5.0% among the school-aged children enrolled. Significant sex differences were found, with more boys (32.4%) compared to girls (23.3%) being categorized as children with overweight/obesity (P < .001 for sex difference). In Table 1, the distribution of children’s sleep patterns and other characteristics by weight status is presented. Children with normal weight were sleeping on average more time compared to children who were overweight or obese, both on weekdays (P = .044) and on weekends (P = .002). Moreover, a large proportion of children with overweight or obesity went to sleep after 23:00, whereas a large proportion of children with normal weight went to sleep before 23:00 (P = .003).
Table 1.
Characteristics stratified by body weight status.
| Characteristics | Overall (n = 1,482) | Normal Weight* (n = 1,068) | Overweight and Obese (n = 414) | P† |
|---|---|---|---|---|
| Sex | ||||
| Boys | 665 (44.9%) | 443 (41.5%) | 222 (53.6%) | < .001 |
| Girls | 817 (55.1%) | 625 (58.5%) | 192 (46.4%) | |
| Age (y) | 11.20 (0.78) | 11.22 (0.79) | 11.17 (0.78) | .259 |
| Sleep duration (h/d) | ||||
| Weekdays | 9.08 (0.95) | 9.11 (0.93) | 9.00 (1.02) | .044 |
| Weekend | 10.30 (1.48) | 10.37 (1.44) | 10.11 (1.57) | .002 |
| Bedtime (weekdays) | ||||
| Before 23:00 | 1128 (76.1%) | 835 (78.2%) | 293 (70.8%) | .003 |
| After 23:00 | 354 (23.9%) | 233 (21.8%) | 121 (29.2%) | |
| Wake time (weekdays) | ||||
| Before 07:00 | 779 (52.6%) | 552 (51.7%) | 227 (54.8%) | .277 |
| After 07:00 | 703 (47.4%) | 516 (48.3%) | 187 (45.2%) | |
| Bedtime (weekends) | ||||
| Before 23:00 | 400 (27.0%) | 300 (28.1%) | 100 (24.2%) | .126 |
| After 23:00 | 1082 (73.0%) | 768 (71.9%) | 314 (75.8%) | |
| Wake time (weekends) | ||||
| Before 09:30 | 757 (51.1%) | 538 (50.4%) | 219 (52.9%) | .383 |
| After 09:30 | 725 (48.9%) | 530 (49.6%) | 195 (47.1%) | |
| KIDMED score (–4 to 12) | 4.54 (2.28) | 4.65 (2.26) | 4.28 (2.31) | .005 |
| Physical activity (yes) | 1170 (78.9%) | 871 (81.6%) | 299 (72.2%) | < .001 |
| Present in their room | ||||
| TV | 435 (29.6%) | 287 (27.0%) | 149 (36.5%) | < .001 |
| Computer | 436 (29.7%) | 282 (26.6%) | 153 (37.4%) | < .001 |
| Family structure | ||||
| Married | 872 (89.1%) | 653 (89.6%) | 219 (87.6%) | .388 |
| Nonmarried | 107 (10.9%) | 76 (10.4%) | 31 (12.4%) | |
| Father’s educational level | ||||
| Primary | 159 (16.3%) | 120 (16.5%) | 39 (15.7%) | .111 |
| Secondary | 429 (44.0%) | 301 (41.4%) | 128 (51.4%) | |
| Tertiary | 388 (39.8%) | 306 (42.1%) | 82 (32.9%) | |
| Mother’s educational level | ||||
| Primary | 101 (10.3%) | 74 (10.2%) | 27 (10.9%) | .036 |
| Secondary | 433 (44.3%) | 307 (42.1%) | 126 (508%) | |
| Tertiary | 443 (45.3%) | 348 (47.7%) | 95 (38.3%) | |
| Income (euros) | ||||
| ≤ 18,000 | 466 (49,9%) | 343 (49.2%) | 123 (52.1%) | .440 |
| > 18,000 | 467 (50,1%) | 354 (50.8%) | 113 (47.9%) | |
| Area of residence | ||||
| Athens | 945 (65.5%) | 699 (67.2%) | 246 (61.0%) | .027 |
| Other area | 498 (34.5%) | 341 (32.8%) | 157 (39.0%) |
Age, KIDMED score, and sleep duration are presented as mean (standard deviation) and categorical variables as n (%). *Weight status is defined based on International Obesity Task Force cutoff criteria for children. †Level of significance set at P < .05; tested via t test for sleeping duration and chi-square test for all other categorical variables.
Unadjusted analyses between children’s overweight/obesity status, other characteristics, and sleep duration on weekdays and on weekends are presented in Table 2. The prevalence of overweight/obesity was progressively reduced with sleep duration, both on weekdays (P = .016) and on weekends (P < .001). However, although an inverse association was observed between sleep duration and overweight/obesity status of children, residual confounding may exist. To account for such confounding, multiadjusted models were estimated (Table 3). In the basic model (model 1), it was observed that for each additional 1 hour of sleep on weekdays, the odds of being overweight/obese decreased by 11%. This association remained significant even when adjusted for age and sex (model 2) but lost its significance when dietary habits (ie, through the KIDMED score), physical activity status, and having a TV or personal computer (PC) or tablet in the bedroom were inserted in the model (see models 3–6). Moreover, when sex was taken into account, the significant association of weekday sleep duration with the likelihood of being overweight/obese was revealed only in boys (ie, for 1 more hour of sleep on weekdays, boys had 14% lower odds of being overweight/obese; P < .001), but not in girls (P = .67).
Table 2.
Characteristics stratified by sleep duration on weekdays and weekends.
| Characteristics | Sleep Duration on Weekdays | Sleep Duration on Weekends | ||||||
|---|---|---|---|---|---|---|---|---|
| < 8 h/d (n = 106) | 8–9 h/d (n = 713) | > 9 h/d (n = 663) | P* | < 8 h/d (n = 63) | 8–9 h/d (n = 267) | > 9 h/d (n = 1,152) | P* | |
| Weight status | ||||||||
| Normal weight | 64 (60.4%) | 513 (71.9%) | 491 (74.1%) | .016 | 34 (54.0%) | 183 (68.5%) | 851 (73.9%) | < .001 |
| Overweight or obese | 42 (39.6%) | 200 (28.1%) | 172 (25.9%) | 29 (46.0%) | 84 (31.5%) | 301 (26.1%) | ||
| Age (y) | 11.45 (0.70) | 11.29 (0.77) | 11.07 (0.79) | < .001 | 11.36 (0.78) | 11.19 (0.74) | 11.20 (0.79) | .275 |
| Bedtime (weekdays) | ||||||||
| Before 23:00 | 3 (2.8%) | 462 (64.8%) | 663 (100.0%) | < .001 | 30 (47.6%) | 181 (67.8%) | 917 (79.6%) | < .001 |
| After 23:00 | 103 (97.2%) | 251 (35.2%) | 0 (0.0%) | 33 (52.4%) | 86 (32.2%) | 235 (20.4%) | ||
| Wake time (weekdays) | ||||||||
| Before 07:00 | 63 (59.4%) | 461 (64.7%) | 255 (38.5%) | < .001 | 46 (73.0%) | 158 (59.2%) | 575 (49.9%) | < .001 |
| After 07:00 | 43 (40.6%) | 252 (35.3%) | 408 (61.5%) | 17 (27.0%) | 109 (40.8%) | 577 (50.1%) | ||
| Bedtime (weekends) | ||||||||
| Before 23:00 | 9 (8.5%) | 117 (16.4%) | 274 (41.3%) | < .001 | 3 (4.8%) | 41 (15.4%) | 356 (30.9%) | < .001 |
| After 23:00 | 97 (91.5%) | 596 (83.6%) | 389 (58.7%) | 60 (95.2%) | 226 (84.6%) | 796 (69.1%) | ||
| Wake time (weekends) | ||||||||
| Before 09:00 | 40 (37.7%) | 363 (50.9%) | 354 (53.4%) | .013 | 61 (96.8%) | 226 (84.6%) | 470 (40.8%) | < .001 |
| After 09:00 | 66 (62.3%) | 350 (49.1%) | 309 (46.6%) | 2 (3.2%) | 41 (15.4%) | 682 (59.2%) | ||
| Sex | ||||||||
| Boys | 56 (52.8%) | 327 (45.9%) | 282 (42.5%) | .042 | 36 (57.1%) | 159 (59.6%) | 470 (40.8%) | < .001 |
| Girls | 50 (47.2%) | 386 (54.1%) | 381 (57.5%) | 27 (42.9%) | 108 (40.4%) | 682 (59.2%) | ||
| KIDMED score (–4 to 12) | 3.74 (2.32) | 4.39 (2.24) | 4.84 (2.27) | < .001 | 4.21 (2.38) | 4.28 (2.09) | 4.62 (0.07) | .045 |
| Physical activity (yes) | 81 (76.4%) | 558 (78.3%) | 531 (80.1%) | .287 | 51 (81.0%) | 218 (81.6%) | 901 (78.2%) | .241 |
| Present in their room | ||||||||
| TV | 53 (50.9%) | 232 (32.8%) | 151 (23.0%) | < .001 | 14 (22.2%) | 84 (31.7%) | 338 (29.6%) | .663 |
| Computer | 55 (51.9%) | 239 (33.8%) | 141 (21.5%) | < .001 | 22 (34.9%) | 82 (30.9%) | 331 (29.0%) | .264 |
| Family structure | ||||||||
| Married | 48 (85.7%) | 458 (90.7%) | 366 (87.6%) | .441 | 21 (84.0%) | 161 (90.4%) | 690 (88.9%) | .986 |
| Nonmarried | 8 (14.3%) | 47 (9.3%) | 52 (12.4%) | 4 (16.0%) | 17 (9.6%) | 86 (11.1%) | ||
| Father’s educational level | ||||||||
| Primary | 12 (22.2%) | 76 (15.3%) | 71 (16.7%) | .636 | 7 (29.2%) | 32 (17.9%) | 120 (15.5%) | .022 |
| Secondary | 20 (37.1%) | 230 (46.1%) | 179 (42.3%) | 8 (33.3%) | 90 (50.3%) | 33 (42.8%) | ||
| Tertiary | 22 (40.7%) | 192 (38.6%) | 174 (41.0%) | 9 (37.5%) | 57 (31.8%) | 322 (41.7%) | ||
| Mother’s educational level | ||||||||
| Primary | 8 (14.5%) | 52 (10.4%) | 41 (9.7%) | .191 | 8 (32.0%) | 22 (12.2%) | 71 (9.2%) | .010 |
| Secondary | 24 (43.6%) | 229 (45.7%) | 180 (42.8%) | 10 (40.0%) | 79 (43.9%) | 344 (44.6%) | ||
| Tertiary | 23 (41.8%) | 220 (43.9%) | 200 (47.5%) | 7 (28.0%) | 79 (43.9%) | 357 (46.2%) | ||
| Area of residence | ||||||||
| Athens | 71 (68.3%) | 501 (72.2%) | 373 (57.8%) | < .001 | 19 (67.8%) | 170 (65.6%) | 756 (67.2%) | < .001 |
| Other area | 33 (31.7%) | 193 (27.8%) | 272 (42.2%) | 40 (32.2%) | 89 (34.4%) | 369 (32.8%) | ||
Data presented as n (%) except age and KIDMED score, which are presented as mean (standard deviation). *Level of significance set at P < .05; tested via t test for KIDMED score and chi-square test for all other categorical variables.
Table 3.
Results of nested multiple logistic regressions that evaluate the association between children’s sleep characteristics (weekdays or weekends) and body weight status.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Sleep duration (weekdays) (h/day) | 0.89 (0.79–0.99)* | 0.88 (0.78–0.99)* | 0.90 (0.80–1.02) | 0.91 (0.80–1.02) | 0.92 (0.81–1.04) | 0.94 (0.83–1.07) |
| Sleep duration (weekends) (h/day) | 0.89 (0.82–0.96)* | 0.91 (0.84–0.98)* | 0.91 (0.84–0.99)* | 0.91 (0.84–0.98)* | 0.91 (0.84–0.98)* | 0.91 (0.84–0.98)* |
| Wake time < 07:00 (weekdays), yes/no | 1.14 (0.90–1.43) | 1.13 (0.90–1.42) | 1.13 (0.89–1.42) | 1.10 (0.87–1.39) | 1.10 (0.87–1.39) | 1.08 (0.86–1.37) |
| Bedtime < 22:00 (weekdays), yes/no | 0.79 (0.63–1.01) | 0.77 (0.61–0.99)* | 0.77 (0.62–0.98)* | 0.77 (0.62–0.98)* | 0.76 (0.62–0.97)* | 0.79 (0.62–1.00)* |
| Bedtime > 23:00 (weekdays), yes/no | 1.48 (1.15–1.91)* | 1.50 (1.16–1.96)* | 1.44 (1.11–1.88)* | 1.41 (1.08–1.85)* | 1.38 (1.05–1.81)* | 1.36 (1.04–1.78)* |
| Wake time < 07:00 (weekends), yes/no | 1.97 (1.30–2.98)* | 1.87 (1.22–2.84)* | 1.85 (1.22–2.82)* | 1.91 (1.25–2.91)* | 1.94 (1.27–2.97)* | 2.00 (1.30–3.06)* |
| Bedtime < 22:00 (weekends), yes/no | 0.84 (0.75–1.41) | 0.89 (0.77–1.49) | 0.91 (0.79–1.52) | 0.90 (0.78-1.41) | 0.95 (0.85–1.71) | 1.01 (0.75–1.39) |
| Bedtime > 23:00 (weekends), yes/no | 1.23 (0.94–1.59) | 1.22 (0.94–1.59) | 1.19 (0.91–1.55) | 1.19 (0.92–1.55) | 1.17 (0.89–1.53) | 1.14 (0.87–1.50) |
Data presented as odds ratio (95% confidence interval). Model 1 = crude model, Model 2 = adjusted for age and sex, Model 3 = adjusted for variables in model 2 plus KIDMED score, Model 4 = adjusted for variables in model 3 plus physical activity status, Model 5 = adjusted for variables in model 4 plus having television in the room. Model 6 = adjusted for variables in model 5 plus having personal computer or tablet in the room. *P value < .05.
When the analysis was split between weekdays and weekends, sleep duration on weekends was also inversely associated with overweight/obesity status (Table 3). In particular, it was observed that for each additional hour of sleep on weekends, the odds of being overweight/obese decreased by 11% (model 1); this association remained significant even after various adjustments were made (see models 2–6). No significant interaction between sleep duration on weekends and dietary habits, playing video games, having a PC or TV in their room, or sex regarding children’s overweight/obesity status was observed (all P values > .5).
Concerning sleep patterns, children who reported bedtime after 23:00 on weekdays had up to 50% higher odds of being overweight/obese (Table 3). Moreover, children who woke up before 07:00 on weekends had up to 100% higher odds of being overweight/obese (all P values < .05). On the contrary, children who reported bedtime before 22:00 on weekdays had a 21% lower likelihood of being overweight/obese, whereas no significant association was observed regarding weekend bedtime before 22:00 and the likelihood of being overweight/obese. However, a highly significant interaction between sleep duration on weekdays and sleep duration on weekends on the overweight/obesity status of children was revealed. Specifically, in children who had 1-hour longer duration on weekends and 1-hour lower duration on weekdays, the likelihood of being overweight/obese was 2% lower compared to children having both 1-hour lower or 1-hour higher sleep duration (odds ratio per 1 hour = 0.98; 95% confidence interval, 0.97–0.99).
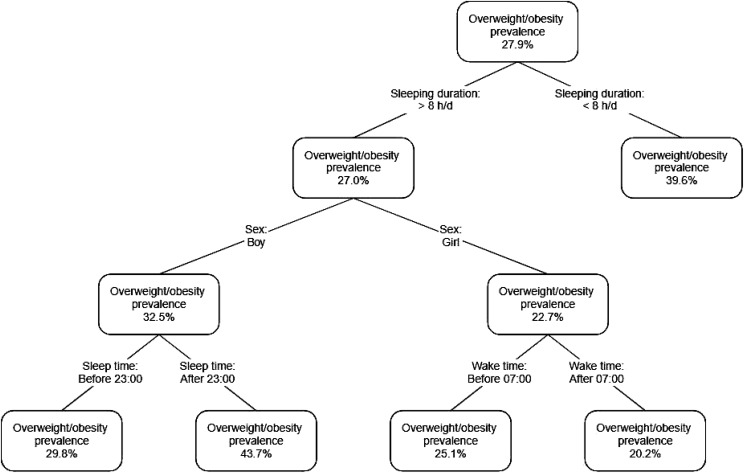
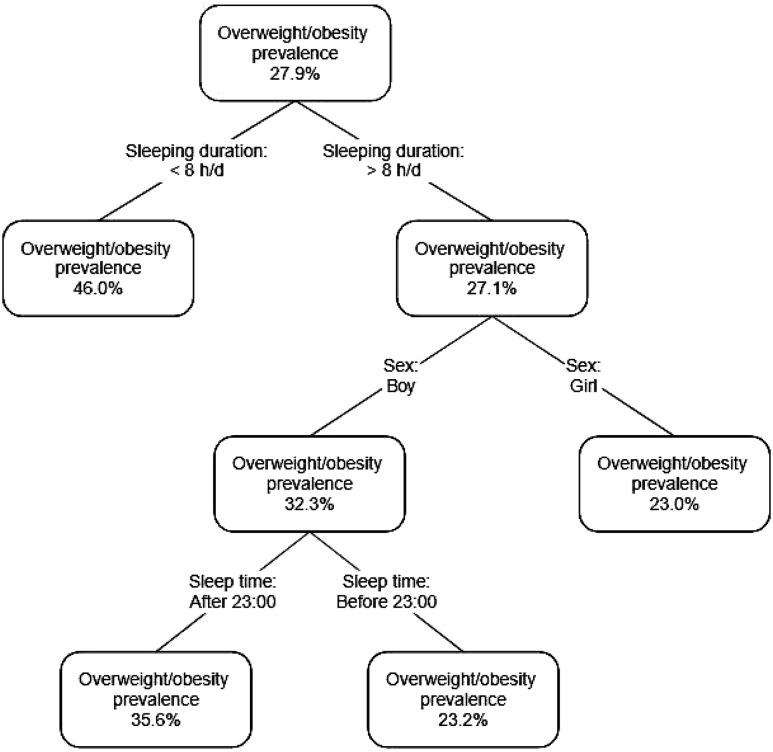
The CART analysis concerning sleep duration on weekdays and overweight/obesity status led to a 3-level tree solution. As can be seen from the paths illustrated in Figure 1, the prevalence of overweight/obesity increased from 27.9% (baseline level) to 39.6% among both boys and girls reporting < 8 hours of sleep during weekdays (first level). Moreover, the prevalence of overweight/obesity increased from the baseline level to 43.7% among boys reporting sleep duration > 8 hours but bedtime after 23:00 (third level). On the contrary, the prevalence of overweight/obesity decreased from the 27.9% baseline level to 20.2% for girls reporting sleep duration > 8 hours but wake-up time after 07:00 on weekdays (third level). Regarding sleep patterns on the weekends, a 3-level CART solution was revealed (Figure 2). The prevalence of overweight/obesity increased from the baseline level (ie, 27.9%) to 46.0% among children reporting < 8 hours of sleep during weekdays (first level). In another path, the prevalence was also increased from the baseline level to 35.6% in boys who reported sleep duration > 8 hours but also bedtime after 23:00.
Figure 1. Classification tree for overweight/obesity based on weekday sleep duration.
Figure 2. Classification tree for overweight/obesity based on weekend sleep duration.
DISCUSSION
The aim of the present study was to investigate the association of sleep duration and sleep patterns on the likelihood of overweight/obesity among children aged 10–12 years and also to test whether there was a weekday effect. It was revealed that increased sleep duration was associated with decreased odds of overweight/obesity among children, and this was more prominent for weekends than for weekdays. However, children who had lower sleep duration on weekdays but caught up with the lack of sleep on weekends were less likely to be overweight/obese compared to those children having both less or increased sleep duration on weekdays and weekends. To our knowledge, this is one of the few studies that investigated not only the duration of sleep but also sleep patterns on weekdays and weekends of school children in association with overweight and obesity.
It has been reported that insufficient sleep duration in children is associated with an increased risk of obesity, ranging from 58–89%, with each additional hour of sleep per day reducing the risk of obesity by 9%.28 In recent years, the observed association between short sleep and obesity has been explained through several mechanisms. A review of the laboratory evidence has come to the conclusion that sleep deprivation leads to the downregulation of leptin and upregulation of ghrelin, leading to the enhancement of overeating and weight gain risk.11,12 The study of Miller et al29 showed that children who go to bed late or do not have a regular sleep schedule are exposed to a higher risk of developing obesity. Similarly, Ogden et al30 and Knutson and Van Cauter31 reported an inverse association between sleep duration and risk of childhood obesity. Moreover, in a recent systematic review and meta-analysis of Fatima et al,32 it was highlighted that children and adolescents who sleep less had approximately twice higher odds of being overweight/obese compared to those who sleep for more time. Similar to these observations, the present study also revealed an inverse association between sleep duration and the likelihood of a child aged 10–12 years being overweight/obese. However, the previous studies did not distinguish the association of sleep duration on overweight/obesity risk between weekdays and weekends, although it has been reported that children follow different sleep patterns on weekends than on weekdays.33–35 According to our findings, children slept about 90 minutes more on weekends compared to weekdays, and this seemed to have a detrimental role in the likelihood of being overweight/obese. In particular, the association between sleep duration and overweight/obesity was stronger on weekends, but less prominent and more influenced to confounding when weekdays were studied. This probably can be attributed to the fact that on weekdays children had to wake up earlier and thus had less sleep duration,18 whereas those who caught up the “lost” sleep hours seemed to benefit more than the others.
Regarding the weekend sleeping pattern, this seemed to have a more prominent role for children who reported bedtime early (ie, before 22:00) and for children who woke up early even on weekends. These results highlight the usefulness, but also the need, for children to sleep and wake up early; the earlier children sleep, the easier it is to complete the necessary hours of sleep without having to wake up late.
The association between having a TV in the children’s room or using small screens (ie, smartphones or tablets) to relax with shorter sleep duration has already been reported.36,37 Although in the present study sleep duration was positively associated with better dietary habits and inversely associated with the presence of a TV and or a PC/tablet in the children’s room, no significant interaction between sleep duration and dietary habits, playing video games, or having a PC or TV in their room on children’s overweight/obesity status was observed. This could be explained by the fact that few children reported having a PC or TV in their room in our sample. Moreover, sleep duration, especially at weekends, was positively associated with both parents’ educational levels. This is in line with the results of Padez et al38: Children whose parents have a lower level of education sleep fewer hours than those whose parents have a higher level of education. This is probably because parents with low education do not understand the importance of sleep for their children’s proper growth. Moreover, the more adherent to the Mediterranean diet children were, the greater their sleep duration. This result is in line with the results of Rosi et al,39 who studied 690 primary school children attending the fifth grade (ie, ages 9–11 years) in Parma, Italy, and found a positive association between dietary quality and sleep duration.
The American Academy of Sleep Medicine recommends that the nightly duration of healthy sleep for children ages 6–12 years should be 9–12 hours.16 If children sleep the recommended hours regularly, they will have better health outcomes, such as improved attention, better memory, emotional regulation, better quality of life, and better mental and physical health. The National Sleep Foundation40 has stated that approximately 35% of U.S. children and adolescents had insufficient sleep duration on weekdays, while a study conducted in 10 European cities revealed that about 34% of adolescents had insufficient sleep time.41 Our study revealed that 45.3% of children had insufficient sleep duration (ie, less than 9 hours) on weekdays. This percentage is similar to the one reported by Tambalis et al35 in a nationwide study of the Greek population, in which approximately 40% of the 177,091 studied children aged 8–17 years in Greece reported insufficient sleeping hours. The National Sleep Foundation recommends parents to teach school-aged children about healthy sleep habits, to emphasize the need for a regular and consistent sleep schedule and bedtime routine, and to keep children’s bedrooms conducive to sleep, ie, dark, cool, and quiet without TV and PC inside.38
Limitations
This study has some limitations due to its cross-sectional design. First of all, no temporal relationship and causal inference can be established. Moreover, the findings cannot be generalized to all Greek children, but only to children aged 10–12 years. Regarding the accuracy of the children’s answers, this would always be a “question” as in all observational studies that use questionnaires. However, to limit this bias, trained investigators were present throughout the whole study’s procedure to address any possible misunderstanding, increasing in this way the validity of the responses and measurements. Another limitation of the study is that it did not evaluate sleep quality. The calculation of sleep duration was based only on the information about sleep and wake time, which was self-reported; thus, reporting bias may also be an additional limitation. The pubertal stage of the participating children was not taken into account. This age is a borderline time where some children have already begun their puberty, and may have less sleep duration, whereas others have not. This lack of information may have confounded the strength of the relationships with body weight status.
CONCLUSIONS
Despite the aforementioned limitations, the findings of this study deserve special attention to the promotion of effective strategies and policies toward the reduction of childhood overweight/obesity. Sleep is a natural need, the quantity and quality of which are important for the healthy development of children. Although the literature has dealt extensively with the study of sleep and its aspects, there are still uncertainties about adequate sleep patterns. The present study revealed that sleep patterns on weekends are different from those on weekdays and they seem to play a different role in overweight/obesity risk; nevertheless, enough sleep hours during the entire week seems to be a key player in reducing the prevalence of childhood overweight/obesity. Actions should be taken for parents to realize and understand that a sufficient sleep duration, especially on weekends when children’s schedules are not so heavy, has a protective role in their children’s weight status.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank all the students for their participation, their parents for their consent, all the teachers and school principals who contributed to the sampling process and data collection, and, moreover, all the field investigators of the study for their support and assistance with the data collection.
ABBREVIATIONS
- BMI
body mass index
- CART
Classification and Regression Tree
- PC
personal computer
- TV
television
REFERENCES
- 1.Chaput JP, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S266–S282. 10.1139/apnm-2015-0627 [DOI] [PubMed] [Google Scholar]
- 2.Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012;463(1):121–137. 10.1007/s00424-011-1044-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cappuccio FP, Cooper D, Delia L, et al. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–1492. 10.1093/eurheartj/ehr007 [DOI] [PubMed] [Google Scholar]
- 4.Shan Z, Ma H, Xie M, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–537. 10.2337/dc14-2073 [DOI] [PubMed] [Google Scholar]
- 5.Leng Y, Cappuccio FP, Wainwright NW, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. 2015;84(11):1072–1079. 10.1212/WNL.0000000000001371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dotto L. Sleep stages, memory and learning. CMAJ. 1996;154(8):1193–1196. [PMC free article] [PubMed] [Google Scholar]
- 7.Brandenberger G, Gronfier C, Chapotot F, Simon C, Piquard F. Effect of sleep deprivation on overall 24 h growth-hormone secretion. Lancet. 2000;356(9239):1408. 10.1016/S0140-6736(00)02847-6 [DOI] [PubMed] [Google Scholar]
- 8.Morgan D, Tsai SC. Sleep and the endocrine system. Crit Care Clin. 2015;31(3):403–418. 10.1016/j.ccc.2015.03.004 [DOI] [PubMed] [Google Scholar]
- 9.van der Lely AJ, Tschöp M, Heiman ML, Ghigo E. Biological, physiological, pathophysiological, and pharmacological aspects of ghrelin. Endocr Rev. 2004;25(3):426–457. 10.1210/er.2002-0029 [DOI] [PubMed] [Google Scholar]
- 10.Chin-Chance C, Polonsky KS, Schoeller DA. Twenty-four-hour leptin levels respond to cumulative short-term energy imbalance and predict subsequent intake. J Clin Endocrinol Metab. 2000;85(8):2685–2691. 10.1210/jc.85.8.2685 [DOI] [PubMed] [Google Scholar]
- 11.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62. 10.1371/journal.pmed.0010062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep duration and insulin resistance in healthy black and white adolescents. Sleep. 2012;35(10):1353–1358. 10.5665/sleep.2112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018;84:56–66. 10.1016/j.metabol.2018.02.010 [DOI] [PubMed] [Google Scholar]
- 14.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–58. 10.1016/j.smrv.2014.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maras D, Flament MF, Murray M, et al. Screen time is associated with depression and anxiety in Canadian youth. Prev Med. 2015;73:133–138. 10.1016/j.ypmed.2015.01.029 [DOI] [PubMed] [Google Scholar]
- 16.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: methodology and discussion. J Clin Sleep Med. 2016;12(11):1549–1561. 10.5664/jcsm.6288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12(2):110–118. 10.1016/j.sleep.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 18.Carissimi A, Dresch F, Martins AC, et al. The influence of school time on sleep patterns of children and adolescents. Sleep Med. 2016;19:33–39. 10.1016/j.sleep.2015.09.024 [DOI] [PubMed] [Google Scholar]
- 19.Magriplis E, Farajian P, Panagiotakos DB, Risvas G, Zampelas A. The relationship between behavioral factors, weight status and a dietary pattern in primary school aged children: the GRECO study. Clin Nutr. 2019;38(1):310–316. 10.1016/j.clnu.2018.01.015 [DOI] [PubMed] [Google Scholar]
- 20.Wing YK, Li SX, Li AM, Zhang J, Kong APS. The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics. 2009;124(5):e994–e1000. 10.1542/peds.2008-3602 [DOI] [PubMed] [Google Scholar]
- 21.Morrissey B, Taveras E, Allender S, Strugnell C. Sleep and obesity among children: a systematic review of multiple sleep dimensions. Pediatr Obes. 2020;15(4):e12619. 10.1111/ijpo.12619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.LeMay-Russell S, Tanofsky-Kraff M, Schvey NA, et al. Associations of weekday and weekend sleep with children’s reported eating in the absence of hunger. Nutrients. 2019;11(7):1658. 10.3390/nu11071658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antonogeorgos G, Grigoropoulou D, Papadimitriou A, et al. Validation of a food frequency questionnaire designed for children 10-12 years: the PANACEA-FFQ. Perioperative Nursing. 2013;2(1):40–54. 10.1038/pr.2011.1003 [DOI] [Google Scholar]
- 24.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000; 320(7244):1240–1243. 10.1136/bmj.320.7244.1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Serra-Majem L, Ribas L, Ngo J, et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004;7(7):931–935. 10.1079/PHN2004556 [DOI] [PubMed] [Google Scholar]
- 26.Argiropoulou EC, Michalopoulou M, Aggeloussis N, Avgerinos A. Validity and reliability of physical activity measures in Greek high school age children. J Sports Sci Med. 2004;3(3):147–159. [PMC free article] [PubMed] [Google Scholar]
- 27.Breiman L, Friedman J, Stone CJ, Olshen RA. Classification and Regression Trees. Monterey, CA: CRC Press; 1984. [Google Scholar]
- 28.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. 10.1093/sleep/31.5.619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller AL, Lumeng JC, LeBourgeois MK. Sleep patterns and obesity in childhood. Curr Opin Endocrinol Diabetes Obes. 2015;22(1):41–47. 10.1097/MED.0000000000000125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288(14):1728–1732. 10.1001/jama.288.14.1728 [DOI] [PubMed] [Google Scholar]
- 31.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129(1):287–304. 10.1196/annals.1417.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16(2):137–149. 10.1111/obr.12245 [DOI] [PubMed] [Google Scholar]
- 33.Li A, Chen S, Quan SF, et al. Sleep patterns and sleep deprivation recorded by actigraphy in 4th-grade and 5th-grade students. Sleep Med. 2020;67:191–199. 10.1016/j.sleep.2019.12.001 [DOI] [PubMed] [Google Scholar]
- 34.Chaput JP, Janssen I. Sleep duration estimates of Canadian children and adolescents. J Sleep Res. 2016;25(5):541–548. 10.1111/jsr.12410 [DOI] [PubMed] [Google Scholar]
- 35.Tambalis KD, Panagiotakos DB, Psarra G, Sidossis LS. Insufficient sleep duration is associated with dietary habits, screen time, and obesity in children. J Clin Sleep Med. 2018;14(10):1689–1696. 10.5664/jcsm.7374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arora T, Hussain S, Hubert Lam KB, Lily Yao G, Neil Thomas G, Taheri S. Exploring the complex pathways among specific types of technology, self-reported sleep duration and body mass index in UK adolescents. Int J Obes Lond. 2013;37(9):1254–1260. 10.1038/ijo.2012.209 [DOI] [PubMed] [Google Scholar]
- 37.Falbe J, Davison KK, Franckle RL, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015;135(2):e367–e375. 10.1542/peds.2014-2306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Padez C, Mourao I, Moreira P, Rosado V. Long sleep duration and childhood overweight/obesity and body fat. Am J Hum Biol. 2009;21(3):371–376. 10.1002/ajhb.20884 [DOI] [PubMed] [Google Scholar]
- 39.Rosi A, Calestani MV, Parrino L, et al. Weight status is related with gender and sleep duration but not with dietary habits and physical activity in primary school Italian children. Nutrients. 2017;9(6):579. 10.3390/nu9060579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Sleep Foundation . Children and Sleep. https://www.sleepfoundation.org/children-and-sleep. Accessed August 25, 2020.
- 41.Garaulet M, Ortega FB, Ruiz JR, et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes Lond. 2011;35(10):1308–1317. 10.1038/ijo.2011.149 [DOI] [PubMed] [Google Scholar]