Abstract
Objective:
Following disasters, perinatal women are vulnerable to developing post-traumatic stress disorder (PTSD)-like symptoms. Little is known about protective factors. We hypothesized that peritraumatic stress would predict PTSD-like symptoms in pregnant and postpartum women and would be moderated by social support and resilience.
Method:
Women (n = 200) who experienced the 2016 Fort McMurray Wood Buffalo wildfire during or shortly before pregnancy completed the Peritraumatic Distress Inventory (PDI), Peritraumatic Dissociative Experiences Questionnaire, and the Impact of Event Scale-Revised for current PTSD-like symptoms. They also completed scales of social support (Social Support Questionnaire-Short Form) and resilience (Connor-Davidson Resilience Scale).
Results:
Greater peritraumatic distress (r = 0.56) and dissociative experiences (r = 0.56) correlated with more severe PTSD-like symptoms. Greater social support satisfaction was associated with less severe post-traumatic stress symptoms but only when peritraumatic distress was below average; at more severe levels of PDI, this psychosocial variable was not protective.
Conclusions:
Maternal PTSD-like symptoms after a wildfire depend on peritraumatic distress and dissociation. Higher social support satisfaction buffers the association with peritraumatic distress, although not when peritraumatic reactions are severe. Early psychosocial interventions may protect perinatal women from PTSD-like symptoms after a wildfire.
Keywords: prenatal maternal stress, maternal mental health, natural disaster, subjective distress, post-traumatic stress, social support, resilience
Introduction
Women and children are thought to be more susceptible to the range of negative consequences resulting from disasters and stress in general, such as mental health issues. 1,2 Experiencing a natural disaster during gestation or postpartum may complicate the potential aftermath of these traumatic events, although the rates of psychopathology after disaster in postpartum women are not necessarily higher than in women who were not recently pregnant. 3 However, it is well known that pregnancy and the perinatal period are inherently associated with extensive psychological and physiological changes, which confer an increased vulnerability to psychopathology for pregnant and postpartum women. 4,5
Although the evidence is at times equivocal, the association between preconception and prenatal maternal psychosocial stress, maternal perinatal mental health, and adverse offspring outcomes is generally accepted. 6,7 Indeed, prenatal maternal psychopathology and stress have been associated with suboptimal infant development 8 such as obesity, 9 difficult temperament, 7,10 poorer cognition, 11 and dysregulation of socioemotional development. 12 Prenatal stress from natural disasters also predicts autism-like symptoms 13 and eating disorders. 14 In turn, these are associated with neurodevelopmental disorders (e.g., autism, schizophrenia) and future psychological problems. 10,15
When it comes to daily life or pregnancy-associated stressors, it is challenging to objectively quantify the amount of stress a mother experiences. In that context, natural disasters offer the opportunity to study exposure to a severe stressor with a sudden onset that impacted a sizable community in a quasi-random manner, more or less independent of individual influences. 16 Objective hardship, the degree to which one is exposed to the disaster, subjective distress, the intensity of the emotional response, and cognitive appraisal are thought to determine the psychological outcomes of disaster. 17,18 These characteristics were demonstrated to be predictive factors with regard to negative maternal mental health outcomes of a disaster during pregnancy. 19,20 Other studies have shown post-disaster maternal mental health to be more influential when it comes to the deleterious effects on child development than the experience of the disaster itself. 21,22
Subjective disaster-related stress can be assessed by measuring peritraumatic distress and peritraumatic dissociative experiences. 23 –25 These responses at the time of the event are often measured retrospectively. 25,26 Peritraumatic dissociation is considered a mechanism intended to cope with severe trauma, shielding the individual from overwhelming emotions during and/or after the traumatic event through derealization and altered awareness. 27 Both peritraumatic distress and dissociation were found to be robust contributing factors toward the development of post-traumatic stress disorder (PTSD)-like symptoms and depression, two psychopathologies with extensive overlap in symptomatology, risk factors, and comorbidities. 23,25,28
Psychological resilience is thought to be a major moderator of the relationship between the experience of trauma and the development of post-traumatic psychopathology. 29,30 In this context, resilience is thought of as a dynamic process, the capacity to bounce back, cope with, and recover from adverse events. 31 Specific coping styles and social support have been associated with resilience, with perceived social support being of particular importance. 32 –34 In turn, inadequate social support and social withdrawal are recognized as vulnerability factors in developing negative effects of trauma exposure. 32
Fortunately, not all mothers who face high levels of stress during pregnancy will experience adverse pregnancy and child health and developmental outcomes or have maternal mental health issues. Similarly, not all who experience traumatic events develop PTSD, post-traumatic stress (PTS) symptoms, or depression. Therefore, it is important to determine which personal and trauma-associated characteristics are protective against the development of mental health issues that are associated with subsequent adverse outcomes for mother and child. A greater understanding of personal factors that moderate the effects of stress may help to develop interventions to strengthen mothers experiencing high levels of stress and potentially short-circuit the transgenerational transmission of its effects. 35
This study evaluated the moderating influence of social support and resilience on the effects of two measures of peritraumatic responses (distress and dissociation) regarding the development of PTS symptoms in women who were preconception or pregnant at the time of the May 2016 Fort McMurray Wood Buffalo wildfire. This natural disaster resulted in major destruction of the city and the evacuation of upward of 88,000 people, approximately 1,850 of whom were women who were either pregnant or preconception. 36 We hypothesized that more severe peritraumatic experiences during the disaster would predict more severe PTSD-like symptoms in pregnant and postpartum women but that social support and resilience would moderate this association. The moderators assessed here include two measures of social support (number of people and satisfaction) and a self-reported measure of resilience.
Method
Study Design, Setting, and Participants
The Fort McMurray Mommy Baby Study is a longitudinal study established in the wake of the Fort McMurray Wood Buffalo wildfire in May 2016. It aimed to look at the resilience of pregnant women during and after this natural disaster and to improve the health of these women and their infants using an expressive writing intervention. 36 Our goal for this study was to determine the extent to which peritraumatic reactions to the disaster would predict the mental health of pregnant women. English-speaking women who (1) were evacuated from Fort McMurray due to the May 2016 wildfire and (2) were either within 6 months of conception or pregnant with a single baby during the evacuation were eligible. Enrollment started on November 7, 2016, and continued until October 29, 2018. Recruitment (62.2% within 1 year of the fire) occurred through word of mouth, media reports, social media (Facebook ads ran on and off from January 2017 until August 2018), the study website (www.mommybabyfmm.ca), and flyers distributed in community centers. After providing informed consent, eligible women were asked to complete a range of self-report questionnaires. Participants received a CAD$50 Amazon certificate. Informed consent and all questionnaires were administered through the secure web-based application REDCap, hosted by the Women and Children’s Health Research Institute at the University of Alberta, AB, Canada. 37 The study was approved by the University of Alberta Health Research Ethics Board.
Of the 309 women who responded, 300 were eligible. Women were excluded for the following reasons: pregnancy loss prior to 12 weeks of gestation (n = 3), twin pregnancy with loss of 1 fetus (n = 2), 1 termination of pregnancy followed by a new pregnancy, and one multivariate outlier. The sample included all women with complete data about their subjective stress (Impact of Event Scale–Revised [IES-R], Peritraumatic Distress Inventory [PDI], and Peritraumatic Dissociative Experiences Questionnaire [PDEQ]) at recruitment (n = 222), thus removing 71 participants. For 22 of these 222 participants, the timing of exposure to the wildfire (in pregnancy or preconception) was not available, leaving n = 200 participants eligible for analyses.
Instruments
PTSD-like symptoms
The self-administered 22-item IES-R was used to assess current and ongoing PTSD-like symptoms with respect to the fire as experienced during the preceding 7 days. 38 Items are scored on a 5-point Likert-type scale anchored at not at all (0) to extremely (4). Previous studies have suggested cutoff levels between 22 and 35 to screen for potential PTSD. 39,40
Peritraumatic experiences
The 13-item PDI and the 10-item PDEQ 41,42 were administered as per our previous studies. 43 The PDI evaluates the individual’s recollection of panic-like reactions and emotional distress, whereas the PDEQ estimates the severity of dissociative-like experiences, during and immediately after the fire. These peritraumatic measures, scored on a similar 5-point Likert-type scale, allow the quantification of the “exposure to trauma” criterion A of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition diagnostic criteria for PTSD. 44
Social support
The Social Support Questionnaire–Short Form asks for a list of people available for help or support in various situations and the level of satisfaction with the support received, scored from very dissatisfied (1) to very satisfied (6). 45
Resilience
The Connor-Davidson Resilience Scale (CD-RISC) was developed to quantify and identify characteristics of resilience and for use as a clinical measure assessing treatment response. It consists of 25 items describing how the respondent may have felt over the preceding month, such as “I am able to adapt when changes occur” and “I feel in control of my life.” Participants respond on a 5-point rating scale from not true at all (0) to true nearly all of the time (4). Scoring is based on the sum of all items, with a full range of 0 to 100; higher scores reflect a greater level of resilience. The CD-RISC has high test–retest reliability and internal consistency. 31
Demographic variables
Data were collected at recruitment (maternal age, information about the eligible pregnancy and newborn, parity, obstetric history, marital status, education, job status of both parents, and 2015 household income). Additional information was acquired from the obstetric complications checklist as used by Jacobsen and Kinney. 46 The timing of exposure to the fire preconception or during pregnancy was defined as the number of days between May 1, 2016 – the start of the fire – and the best estimated due date. The latter was calculated using a combination of estimated date of delivery as indicated by the mother, gestational age at birth, last menstrual period, and written comments made by the mother when available. The best estimated gestational age at birth and on May 1, 2016, was then calculated. First-trimester exposure corresponds to due dates falling 187 to 279 days following May 1; second trimester, 94 to 186 days; and third trimester, 0 to 93 days. Preconception exposure was defined as having a due date more than 280 days after the fire and evacuation.
Statistical Methods
All analyses were performed using IBM SPSS Statistics, Version 26.0 (IBM Corp, Armonk, NY). Descriptive statistics and correlations were conducted after thorough data checking. The reports on gestational age at birth for 3 participants were found to be inconsistent and biologically implausible. Therefore, these values were imputed using the expectation–maximization method to estimate the best model coefficient based on all available data. The imputation model included maternal age at birth, birthweight and length, obstetrical complications, parity, maternal education, and income. Demographic data are reported as means ± standard deviation.
To determine the extent to which maternal factors influenced the association between PDI or PDEQ and PTS symptoms, multiple linear regressions with interaction terms were used. Scores on the social support and CD-RISC questionnaires were evaluated as potential moderators. Covariates included the time between the fire and recruitment, timing of fire exposure before or during pregnancy, whether delivery had occurred before recruitment, and parity. To probe the significant interactions, the PROCESS macro Version 3.4 for SPSS was used, 47 which first tests whether the interaction term is significant. Given a significant result, it probes the interaction, indicating the magnitude and significance of conditional (or simple) effects of the main predictor at different levels of the moderator. Using the Johnson–Neyman procedure, it indicates the moderator level at which the conditional effects of the predictor become significant (or vice versa), delimiting the region of significance. PROCESS then provides coordinates to graph interaction figures in Microsoft Excel. All tests were 2-sided with P < 0.05 considered significant.
Results
Recruitment scales were completed, on average, 45.79 ± 18.1 weeks (range: 27.3 to 120.7) or 10.53 ± 4.2 months (range: 6.3 to 23.6) after the fire. There were no differences with regard to sample characteristics between those who were pregnant at the time of recruitment or had already gone through childbirth. The demographic and obstetric characteristics are presented in Table 1. The mean score for PTS symptoms at recruitment was 21.98 ± 15.4 such that 23.5% ranked as possible PTSD (IES-R = 22 to 32), whereas 26% qualified for probable PTSD (>32). Peritraumatic distress scores (PDI) were on average 23.95 ± 11.7, with 41.5% of mothers scoring above 28, whereas 49.5% had a score between 7 and 28. The mean score for peritraumatic dissociative experiences (PDEQ) was 14.58 ± 9.4.
Table 1.
Demographic and Obstetric Characteristics.
| Variable | N | Mean (SD) |
|---|---|---|
| Maternal age at delivery (years) | 192 | 30.90 (3.83) |
| Gestational age at birth (weeks) | 190 | 39.30 (1.59) |
| Birthweight (grams) | 164 | 3,449.11 (565.01) |
| Maternal age at evacuation (years) | 200 | 29.71 (3.98) |
| Time since fire (weeks) | 200 | 45.79 (18.13) |
| Gestational age at fire (days) | 200 | 65.59 (158.83) |
| N | % | |
| Recruitment status | ||
| Pregnant | 54 | 27.0 |
| Postpartum | 146 | 73.0 |
| Trimester of exposure | ||
| Preconception | 65 | 32.5 |
| First trimester | 36 | 18.0 |
| Second trimester | 45 | 22.5 |
| Third trimester | 52 | 26.0 |
| Postpartum | 2 | 1.0 |
| Parity | ||
| 0 | 102 | 51.5 |
| 1 | 62 | 31.3 |
| 2 | 27 | 13.6 |
| 3+ | 7 | 3.5 |
| Marital status | ||
| Single | 4 | 2.0 |
| Married | 153 | 77.3 |
| Common law | 37 | 18.7 |
| Separated, divorced, widowed | 4 | 2.0 |
| Education mother | ||
| Less than high school | 3 | 1.5 |
| High school diploma or equivalent | 23 | 11.6 |
| Technical, associate’s | 30 | 10.1 |
| Some college, bachelor’s | 132 | 66.7 |
| Master’s, doctorate | 20 | 10.1 |
| Income | ||
| <CAD$25,000 | 3 | 1.5 |
| CAD$25,000 to CAD$100,000 | 26 | 13.1 |
| CAD$100,000 to CAD$175,000 | 65 | 32.8 |
| >CAD$175,000 | 104 | 52.5 |
Correlations are shown in Table 2. Both peritraumatic distress and dissociative experiences were positively correlated with PTS symptoms, as evaluated by the IES-R, and with each other. The CD-RISC scores were weakly negatively related to PTS symptomatology and peritraumatic distress scores, but not with the dissociative experiences scores. This suggests that more resilient women had less severe PTSD-like symptoms and experienced less peritraumatic distress. Social support number and satisfaction marginally associated with peritraumatic distress as well, with higher distress levels associated with less social support received (P < 0.100). Conversely, both social support measures showed a weak negative correlation with PTSD-like symptoms.
Table 2.
Correlation Analyses with n = 200 Unless Otherwise Indicated, Cronbach’s α for the Scales Used Is shown.
| Measure | Mean (SD) | α | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | PTSD-like symptoms | 21.98 (15.35) | 0.93 | — | 0.556 | 0.561 | −0.207 | −0.211 | −0.170 |
| P-value | <0.001 | <0.001 | 0.003 | 0.003 | 0.016 | ||||
| 2 | Peritraumatic dissociation | 14.58 (9.36) | 0.88 | — | 0.685 | −0.086 | −0.048 | −0.057 | |
| P-value | <0.001 | 0.226 | 0.497 | 0.421 | |||||
| 3 | Peritraumatic distress | 23.95 (11.74) | 0.89 | — | −0.229 | −0.135 | −0.134 | ||
| P-value | 0.001 | 0.057 | 0.058 | ||||||
| 4 | CD-RISC Resiliencea | 69.15 (13.02) | 0.92 | — | 0.111 | 0.282 | |||
| P-value | 0.118 | <0.001 | |||||||
| 5 | Social support number | 2.24 (1.35) | — | 0.312 | |||||
| P-value | <0.001 | ||||||||
| 6 | Social support satisfaction | 5.27 (0.88) | 0.96b | — | |||||
Note. Mean scores on the recruitment questionnaires are indicated. PTSD-like symptoms at recruitment were significantly correlated with peritraumatic dissociation and distress, as well as the psychosocial variables resilience and social support. CD-RISC = Connor-Davidson Resilience Scale; PTSD = post-traumatic stress disorder.
a N = 199.
b N = 161 for Cronbach’s α.
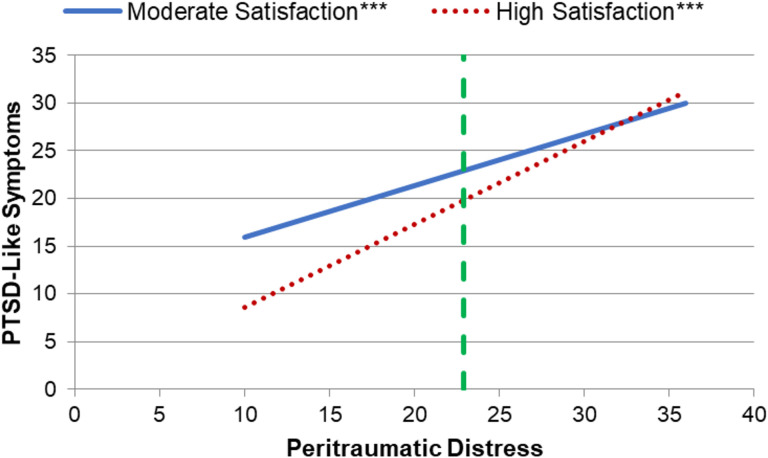
Results of the moderation analyses are presented in Table 3. Only social support satisfaction had a moderating effect on the relationship between peritraumatic distress (PDI) and current PTS symptoms (IES-R). Considering the covariates, the full model explained 34.3% of the variance in PTSD-like symptoms. The interaction between peritraumatic distress and social support satisfaction contributed a statistically significant change of R 2 = 2.3% with F(1, 190) = 6.459, P = 0.012. Regardless of the level of satisfaction, higher peritraumatic distress scores were significantly associated with increased PTS symptoms (Figure 1). At peritraumatic distress levels below 22.9, greater satisfaction was related to lower PTS symptoms. Contrarily, at higher levels, social support satisfaction no longer had a significant effect, and PTS symptoms were at levels indicative of possible or probable PTSD when the covariates were held at their average. At levels of satisfaction below 3.53 (n = 6), peritraumatic distress scores did not correlate with PTS symptoms. None of the control variables contributed significantly to explaining variance in PTSD-like symptoms.
Table 3.
Social Support Satisfaction Moderates the Relationship between Peritraumatic Distress and PTSD-Like Symptoms, as Evident from the Significant Interaction between PDI and SSS.
| Variable | B | SE B | t | P-value | Lower Level CI | Upper Level CI |
|---|---|---|---|---|---|---|
| Peritraumatic distress (PDI) | −0.436 | 0.456 | −0.957 | 0.340 | −1.334 | 0.463 |
| Social support satisfaction (SSS) | −7.078 | 2.427 | −2.913 | 0.004 | −11.865 | −2.291 |
| PDI × SSS | 0.217 | 0.085 | 2.541 | 0.012 | 0.049 | 0.386 |
| Time since fire | 0.051 | 0.060 | 0.844 | 0.400 | −0.068 | 0.169 |
| Delivered at recruitment | −2.527 | 1.609 | −1.240 | 0.118 | −2.700 | 0.647 |
| Parity | −0.394 | 1.086 | −0.363 | 0.717 | −2.536 | 1.747 |
| Exposure (days of pregnancy) | 0.011 | 0.009 | 1.120 | 0.264 | −0.008 | 0.029 |
Note. n = 198. CI = confidence interval; PDI = Peritraumatic Distress Inventory; SSS = social support satisfaction.
Figure 1.
Moderating effect of social support satisfaction on the relationship between peritraumatic distress levels and post-traumatic stress disorder–like symptoms (n = 198). The region of significance is indicated with the vertical dashed line, showing the level of peritraumatic distress below which social support satisfaction was shown to have a significant effect. Moderate satisfaction represents the 10th percentile score, whereas the 90th percentile corresponds to high levels of satisfaction. Asterisks indicate the level of statistical significance of the slopes for the respective percentiles: ***P < 0.001.
Discussion
The May 2016 Fort McMurray Wood Buffalo wildfire was the largest natural disaster and mass evacuation in Canadian history. 48 It touched a population that was already vulnerable due to the oil recession, affecting the community mental health. 49 The present data are part of an intervention study to evaluate the effectiveness of using expressive writing to improve maternal and infant outcomes in the aftermath of the wildfire. 36 However, it should be noted that the intervention was not found to have any effect on women’s mental health. 50 Here, we investigated whether a mother’s social support and resilience at recruitment, that is, prior to the writing intervention, were able to moderate the association between peritraumatic subjective distress or dissociation and PTSD-like symptoms at recruitment.
High levels of social support satisfaction, but not the number of people, had a significant moderating effect on the relationship between peritraumatic distress and PTSD-like symptoms. In our significant interaction result, we show that social support satisfaction only protects against the development of PTS symptoms in those whose peritraumatic distress was relatively low. It seems that social support satisfaction loses its power to protect against PTS symptoms when the individual’s subjective distress at the time of the disaster was more extreme. These data reinforce the importance of one’s satisfaction with their perceived social support, as compared to the reported number of people available to lean on, in influencing the development of PTS symptoms. 33,51,52
In the current sample, we were not able to detect a moderating effect of resilience. Resilience has been demonstrated to have a protective effect, although conflicting evidence exists. 29,53,54 According to Connor and Davidson, it can be seen as “a measure of stress coping ability.” 31 Resilient individuals utilize more social support-seeking behaviors and other active coping strategies, for example, positive reframing. 32 Indeed, social support is considered a buffer toward the development of PTSD, potentially by having an effect on how coping occurs. 31,54,55 Research in trauma victims also indicates that lower levels of resilience correspond with increased social withdrawal as an avoidance strategy. 32
In previous disaster studies, we have demonstrated that different types of social support have protective effects against the deleterious consequences of severe stress exposure during pregnancy. This includes support from partners and midwifery care in a continuous care model, spanning from the prenatal to the postpartum period. 56,57 This support was shown to provide a barrier between objective and subjective distress and postpartum anxiety and depression, which may occur together with PTSD. 21,58 In this study, we did not systematically ask about partner support and only inquired about prenatal care to a limited extent; thus, we could not evaluate whether a similar effect existed.
One limitation of the current study was our inability to account for previous levels of trauma in childhood or adulthood. Abundant research shows that prior history of stressful events and PTSD are key factors in predicting the development of post-traumatic response. 59 As such, if one is to draw conclusions about the psychological burden of a recent traumatic experience, one needs to account for other traumatic events in a mother’s life, ranging from adverse childhood experiences to other life events and difficult environmental circumstances, for example, racism, violence, unemployment, (substance) abuse, and socioeconomic struggles, across her lifetime and potentially even previous generations. 60,61 Unfortunately, we did not have these data available for this study.
Post-disaster research studies face considerable methodological challenges. Mounting a large-scale study in the aftermath of a disaster is a feat that is not easily accomplished, especially when it pertains to a pregnant or postpartum population. It often takes more than a year to procure the necessary funding, while pregnancy only lasts for 9 months. All data were collected between 6 and 23 months after the fire, inducing the possibility of recall bias. While conflicting evidence exists regarding the reliability of retrospective reporting of PTS symptoms (for an overview, see David et al. 26 ), in this study, we looked at symptomatology regarding the fire as experienced over the last 7 days. Therefore, using the IES-R eliminates the possibility of recall bias for this construct. 38 However, it has been demonstrated that reports of peritraumatic responses may change with time, especially in those who develop chronic PTSD, such that the scales evaluating peritraumatic distress and dissociative experiences (PDI and PDEQ) are best administered closely after exposure to a traumatic event. 25,26 Similarly, Thomas et al. noted that the effects of peritraumatic distress are likely to reduce over time since PTSD is a state condition and not a trait. Other factors such as additional life stressors, inadequate social support, and avoidance may then maintain the psychopathology. 25 Remarkably, it was also shown that depending on the specific PTSD symptoms, that is, intrusions versus avoidance and numbing, over- and underreporting of traumatic experiences may occur. In a sample of former prisoners of war, Dekel et al. found that hyperarousal as a PTSD symptom modified the memory of the experience over time, increasing negative recollections. 62 Recall bias has also been associated with worse mental health in that depression may negatively distort recollections (see Oni et al. 63 for review).
Our study population may also be subject to selection bias. It is understandable that advertisements asking for participation in a research study may be easily overlooked or ignored by evacuees when struggling to get their life back together. Participating in disaster-related studies requires remembering the traumatic event, facing one’s fears, which may be exactly what individuals with PTSD are avoiding. 26 This aspect of PTSD is also what may perpetuate symptoms as avoidance prevents the adequate processing of the trauma and fear associated with the disaster. 64 It may also be an explanation for the high attrition rates in disaster studies. In addition, the participants in this study were highly educated, rather affluent women who are mostly in committed relationships, which is a vastly different population than, for instance, single women with limited financial means. The average level of satisfaction reported was already high (above 5 on a scale of 6). This may indicate that the results in a different population could point toward a beneficial effect of bolstering social support in all post-disaster perinatal women, regardless of the level of PTSD-like symptoms or peritraumatic distress. Finally, since high levels of maternal stress and psychopathology are widely accepted to have potentially deleterious consequences, perhaps it is time to focus more on early screening and developing interventions to increase resilience and support the development of adequate coping strategies. Given the importance of social support satisfaction, specific attention for personal relationships, at home and with care providers, is of importance for this at-risk population.
Conclusion
Social support satisfaction may moderate the effect of peritraumatic distress on the development of PTSD-like symptoms in pregnant and postpartum women after a wildfire, supporting conclusions from previous research. Given the established long-term effects of prenatal maternal stress on fetal and early life programming, specific attention to interventions geared toward women of reproductive age, either pregnant, postpartum or with plans of becoming pregnant during and after a disaster, is warranted. This population should be targeted for early screening and interventions in the immediate aftermath of traumatic experiences with the aim of improving long-term maternal and child outcomes.
Acknowledgments
The authors would like to thank the Fort McMurray mothers who participated in the study for their contribution. We also gratefully acknowledge Alain Brunet for his advice on the manuscript.
Authors’ Note: The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Declaration of Conflicting Interests: The author declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclose receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Canadian Institutes of Health Research Project Grant 151029 and Alberta Innovates Grant 201500871.
ORCID iD: Barbara S. E. Verstraeten, MD, PhD  https://orcid.org/0000-0002-0539-8877
https://orcid.org/0000-0002-0539-8877
References
- 1. Corrarino J. Disaster-related mental health needs of women and children. MCN Am J Matern Child Nurs. 2008;33(4):242–248. [DOI] [PubMed] [Google Scholar]
- 2. Tang B, Deng Q, Glik D, Dong J, Zhang L. A meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. Int J Environ Res Public Health. 2017;14(12):1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med. 2010;5(3):181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brunton PJ, Russell JA. The expectant brain: adapting for motherhood. Nat Rev Neurosci. 2008;9(1):11–25. [DOI] [PubMed] [Google Scholar]
- 5. Schaffir J. Biological changes during pregnancy and the postpartum period. In: Wenzel A, editor. The Oxford handbook of perinatal psychology. New York (NY): Oxford Library of Psychology. Oxford University Press; 2016. p. 26–37. [Google Scholar]
- 6. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18–31. [DOI] [PubMed] [Google Scholar]
- 7. Gustafsson HC, Sullivan EL, Nousen EK, et al. Maternal prenatal depression predicts infant negative affect via maternal inflammatory cytokine levels. Brain Behav Immun. 2018;73:470–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Van den Bergh BRH, van den Heuvel MI, Lahti M, et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehav Rev. 2017;S0149-7634(16):30734–30735. [DOI] [PubMed] [Google Scholar]
- 9. Lamichhane N, Olsen NJ, Mortensen EL. Associations between maternal stress during pregnancy and offspring obesity risk later in life—a systematic literature review. Obes Rev. 2020;21(2):e12951. [DOI] [PubMed] [Google Scholar]
- 10. McLean MA, Cobham VE, Simcock G, Kildea S, King S. Toddler temperament mediates the effect of prenatal maternal stress on childhood anxiety symptomatology: the QF2011 Queensland Flood Study. Int J Environ Res Public Health. 2019;16(11):1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kingston D, McDonald S, Austin MP, Tough S. Association between prenatal and postnatal psychological distress and toddler cognitive development: a systematic review. PLoS One. 2015;10(5):e0126929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Madigan S, Oatley H, Racine N, et al. A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J Am Acad Child Adolesc Psychiatry. 2018;57(9):645–657.e648. [DOI] [PubMed] [Google Scholar]
- 13. Walder DJ, Laplante DP, Sousa-Pires A, Veru F, Brunet A, King S. Prenatal maternal stress predicts autism traits in 6(1/2) year-old children: Project Ice Storm. Psychiatry Res. 2014;219(2):353–360. [DOI] [PubMed] [Google Scholar]
- 14. St-Hilaire A, Steiger H, Liu A, et al. A prospective study of effects of prenatal maternal stress on later eating-disorder manifestations in affected offspring: preliminary indications based on the Project Ice Storm cohort. Int J Eat Disord. 2015;48(5):512–516. [DOI] [PubMed] [Google Scholar]
- 15. Pugliese V, Bruni A, Carbone EA, et al. Maternal stress, prenatal medical illnesses and obstetric complications: risk factors for schizophrenia spectrum disorder, bipolar disorder and major depressive disorder. Psychiatry Res. 2019;271:23–30. [DOI] [PubMed] [Google Scholar]
- 16. Lechat MF. Disasters and public health. Bull World Health Organ. 1979;57(1):11–17. [PMC free article] [PubMed] [Google Scholar]
- 17. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York (NY): Springer Publishing Company; 1984. [Google Scholar]
- 18. Olff M, Langeland W, Gersons BP. Effects of appraisal and coping on the neuroendocrine response to extreme stress. Neurosci Biobehav Rev. 2005;29(3):457–467. [DOI] [PubMed] [Google Scholar]
- 19. Harville E, Xiong X, Buekens P. Disasters and perinatal health: a systematic review. Obstet Gynecol Surv. 2010;65(11):713–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brock RL, O’Hara MW, Hart KJ, et al. Peritraumatic distress mediates the effect of severity of disaster exposure on perinatal depression: the Iowa Flood Study. J Trauma Stress. 2015;28(6):515–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tees MT, Harville EW, Xiong X, Buekens P, Pridjian G, Elkind-Hirsch K. Hurricane Katrina-related maternal stress, maternal mental health, and early infant temperament. Matern Child Health J. 2010;14(4):511–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Buthmann J, Finik J, Ventura G, Zhang W, Shereen AD, Nomura Y. The children of Superstorm Sandy: maternal prenatal depression blunts offspring electrodermal activity. Biol Psychol. 2019;146:107716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Canan F, North CS. Dissociation and disasters: a systematic review. World J Psychiatry. 2019;9(6):83–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52–73. [DOI] [PubMed] [Google Scholar]
- 25. Thomas E, Saumier D, Brunet A. Peritraumatic distress and the course of posttraumatic stress disorder symptoms: a meta-analysis. Can J Psychiatry. 2012;57(2):122–129. [DOI] [PubMed] [Google Scholar]
- 26. David AC, Akerib V, Gaston L, et al. Consistency of retrospective reports of peritraumatic responses and their relation to PTSD diagnostic status. J Trauma Stress. 2010;23(5):599–605. [DOI] [PubMed] [Google Scholar]
- 27. Marmar CR, Weiss DS, Metzler T. Peritraumatic dissociation and posttraumatic stress disorder. In: Bremner TJD, Marmar CR, editors. Trauma, memory and dissociation. Washington (DC): American Psychiatric Press; 1998. p. 229–252. [Google Scholar]
- 28. McCanlies EC, Sarkisian K, Andrew ME, Burchfiel EM, Violanti JM. Association of peritraumatic dissociation with symptoms of depression and posttraumatic stress disorder. Psychol Trauma. 2017;9(4):479–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Powers MB, Warren AM, Rosenfield D, et al. Predictors of PTSD symptoms in adults admitted to a level I trauma center: a prospective analysis. J Anxiety Disord. 2014;28(3):301–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pietrzak RH, Johnson DC, Goldstein MB, et al. Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: the role of resilience, unit support, and postdeployment social support. J Affect Disord. 2010;120(1-3):188–192. [DOI] [PubMed] [Google Scholar]
- 31. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. [DOI] [PubMed] [Google Scholar]
- 32. Thompson NJ, Fiorillo D, Rothbaum BO, Ressler KJ, Michopoulos V. Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J Affect Disord. 2018;225:153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee JS. Perceived social support functions as a resilience in buffering the impact of trauma exposure on PTSD symptoms via intrusive rumination and entrapment in firefighters. PLoS One. 2019;14(8):e0220454–e0220454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bakic H, Ajdukovic D. Stability and change post-disaster: dynamic relations between individual, interpersonal and community resources and psychosocial functioning. Eur J Psychotraumatol. 2019;10(1):1614821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Braga LL, Mello MF, Fiks JP. Transgenerational transmission of trauma and resilience: a qualitative study with Brazilian offspring of Holocaust survivors. BMC Psychiatry. 2012;12(1):134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Olson DM, Brémault-Phillips S, King S, et al. Recent Canadian efforts to develop population-level pregnancy intervention studies to mitigate effects of natural disasters and other tragedies. J Dev Orig Health Dis. 2019;10(1):108–114. [DOI] [PubMed] [Google Scholar]
- 37. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Weiss DS, Marmar CR. The Impact of Event Scale—Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York (NY): Guilford Press; 1997. p. 399–411. [Google Scholar]
- 39. Rash CJ, Coffey SF, Baschnagel JS, et al. Psychometric properties of the IES-R in traumatized substance dependent individuals with and without PTSD. Addict Behav. 2008;33(8):1039–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Boudou M, Sejourne N, Chabrol H. Douleur de l’accouchement, dissociation et détresse périnatales comme variables prédictives de symptômes de stress post-traumatique en post-partum [Childbirth pain, perinatal dissociation and perinatal distress as predictors of posttraumatic stress symptoms]. Gynecol Obstet Fertil. 2007;35(11):1136–1142. [DOI] [PubMed] [Google Scholar]
- 41. Brunet A, Weiss DS, Metzler TJ, et al. The Peritraumatic Distress Inventory: a proposed measure of PTSD criterion A2. Am J Psychiatry. 2001;158(9):1480–1485. [DOI] [PubMed] [Google Scholar]
- 42. Marmar CR, Weiss DS, Metzler TJ. The Peritraumatic Dissociative Experiences Questionnaire. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York (NY): Guilford Press; 1997. p. 412–428. [Google Scholar]
- 43. King S, Kildea S, Austin MP, et al. QF2011: a protocol to study the effects of the Queensland flood on pregnant women, their pregnancies, and their children’s early development. BMC Pregnancy Childbirth. 2015;15:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. doi: 10.1176/appi.books.9780890425596.dsm18; 2013. [Google Scholar]
- 45. Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: practical and theoretical implications. J Soc Pers Relat. 1987;4(4):497–510. [Google Scholar]
- 46. Jacobsen B, Kinney DK. Perinatal complications in adopted and non-adopted schizophrenics and their controls: preliminary results. Acta Psychiatr Scand. 1980;62(S285):337–346. [Google Scholar]
- 47. Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: observations, recommendations, and implementation. Behav Res Ther. 2017;98:39–57. [DOI] [PubMed] [Google Scholar]
- 48. Alam R, Islam S, Mosely E, et al. Rapid impact assessment of the Fort McMurray wildfire. Edmonton, Canada: MacEwan University; 2017. [Google Scholar]
- 49. Ritchie A, Hrabok M, Igwe O, et al. Impact of oil recession on community mental health service utilization in an oil sands mining region in Canada. Int J Soc Psychiatry. 2018;64(6):563–569. [DOI] [PubMed] [Google Scholar]
- 50. Brémault-Phillips S, Pike A, Olson J, et al. Expressive writing for wildfire-affected pregnant women: themes of challenge and resilience. Int J Disaster Risk Reduct. 2020;50:101730. [Google Scholar]
- 51. Sarason BR, Shearin EN, Pierce GR, Sarason IG. Interrelations of social support measures: theoretical and practical implications. J Pers Soc Psychol. 1987;52(4):813–832. [Google Scholar]
- 52. Goletzke J, Kocalevent RD, Hansen G, et al. Prenatal stress perception and coping strategies: insights from a longitudinal prospective pregnancy cohort. J Psychosom Res. 2017;102:8–14. [DOI] [PubMed] [Google Scholar]
- 53. Hooberman J, Rosenfeld B, Rasmussen A, Keller A. Resilience in trauma-exposed refugees: the moderating effect of coping style on resilience variables. Am J Orthopsychiatry. 2010;80(4):557–563. [DOI] [PubMed] [Google Scholar]
- 54. Forbes CN, Tull MT, Xie H, et al. Emotional avoidance and social support interact to predict depression symptom severity one year after traumatic exposure. Psychiatry Res. 2020;284:112746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Agyapong VIO, Juhas M, Omege J, et al. Prevalence rates and correlates of likely post-traumatic stress disorder in residents of Fort McMurray 6 months after a wildfire. Int J Ment Health Addict. 2019; 17:120–136. [Google Scholar]
- 56. Brock RL, O’Hara MW, Hart KJ, et al. Partner support and maternal depression in the context of the Iowa floods. J Fam Psychol. 2014;28(6):832–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kildea S, Simcock G, Liu A, et al. Continuity of midwifery carer moderates the effects of prenatal maternal stress on postnatal maternal wellbeing: the Queensland Flood Study. Arch Womens Ment Health. 2018;21(2):203–214. [DOI] [PubMed] [Google Scholar]
- 58. Simcock G, Kildea S, Kruske S, et al. Disaster in pregnancy: midwifery continuity positively impacts infant neurodevelopment, QF2011 study. BMC Pregnancy Childbirth. 2018;18(1):309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Youngner CG, Burton MS, Price M, et al. The contributions of prior trauma and peritraumatic dissociation to predicting post-traumatic stress disorder outcome in individuals assessed in the immediate aftermath of a trauma. West J Emerg Med. 2012;13(3):220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Christiaens I, Hegadoren K, Olson DM. Adverse childhood experiences are associated with spontaneous preterm birth: a case-control study. BMC Med. 2015;13:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Yehuda R, Bierer LM. Transgenerational transmission of cortisol and PTSD risk. Prog Brain Res. 2008;167:121–135. [DOI] [PubMed] [Google Scholar]
- 62. Dekel S, Solomon Z, Ein-Dor T. PTSD symptoms lead to modification in the memory of the trauma: a prospective study of former prisoners of war. J Clin Psychiatry. 2016;77(3):e290–e296. [DOI] [PubMed] [Google Scholar]
- 63. Schraedley P, Turner R, Gotlib I. Stability of retrospective reports in depression: traumatic events, past depressive episodes, and parental psychopathology. J Health Soc Behav. 2002;43(3):307–316. [PubMed] [Google Scholar]
- 64. Oni O, Harville EW, Xiong X, Buekens P. Impact of coping styles on post-traumatic stress disorder and depressive symptoms among pregnant women exposed to Hurricane Katrina. Am J Disaster Med. 2012;7(3):199–209. [DOI] [PubMed] [Google Scholar]