Abstract
Background:
Medial ulnar collateral ligament (MUCL) repair has been proven to be effective in nonprofessional overhead-throwing athletes, with faster and higher rates of return to play (RTP) than the more traditional Tommy John reconstruction. Biomechanical studies and clinical data suggest that MUCL repair augmented with a collagen-coated internal brace may be an effective treatment option in this patient population.
Purpose:
To evaluate the functional outcomes of young nonprofessional athletes who underwent MUCL repair with internal brace augmentation for medial elbow instability. The hypothesis was that these patients will have high rates of RTP and improved functional outcomes.
Study Design:
Case series; Level of evidence, 4.
Methods:
Nonprofessional overhead athletes treated with MUCL repair with internal brace augmentation between 2015 and 2017 were prospectively evaluated for a minimum of 1 year. Preoperatively, all patients had evidence of medial elbow pain caused by MUCL insufficiency, as confirmed by signal changes on magnetic resonance imaging and valgus instability on arthroscopic examination. These findings did not allow them to participate in their chosen sport or profession, and each patient had failed nonoperative treatment. Postoperative outcomes were evaluated using the Overhead Athlete Shoulder and Elbow Score of the Kerlan-Jobe Orthopaedic Clinic. Complications were recorded and detailed.
Results:
A total of 40 nonprofessional overhead athletes were included in this study (35 men and 5 women; mean age, 17.8 years [range, 14-28 years]). The mean follow-up time was 23.8 months (range, 12-44 months). The mean postoperative Kerlan-Jobe Orthopaedic Clinic score was 92.6 (range, 64-100). Overall, 37 athletes (92.5%) returned to play or profession at the same level or higher at a mean time of 6.9 months (range, 2-12 months). Three patients did not RTP: 1 was limited by a concomitant medical diagnosis, and the other 2 chose not to resume athletics after the procedure but remained symptom free.
Conclusion:
In the nonprofessional athlete, primary MUCL repair with internal brace augmentation is a viable alternative to traditional repair techniques or reconstruction, allowing for a rapid RTP and promising functional outcomes.
Keywords: medial elbow instability, MUCL, internal brace, MUCL repair
The anterior oblique ligament of the medial ulnar collateral ligament (MUCL) complex is the primary stabilizer of valgus stress of the elbow. 1,2,13,21,23,24,29,32 Injuries to this ligament most commonly occur among overhead-throwing athletes from excessive and repetitive stress on the medial side of the elbow. 15,19
As our understanding of these injuries improved, focus turned to nonoperative management. Rapid initiation of nonoperative management after the onset of symptoms has been shown to be effective in allowing some athletes to return to play (RTP). 5,7 Early surgical interventions focused primarily on autograft reconstructions in professional overhead-throwing athletes with chronic ligament damage and attenuation. 9,16,28
Since the early 1990s, there has been a rapid increase in MUCL injuries in younger nonprofessional athletes. 27 In these patients, the injury more commonly involves the proximal and/or distal portion of the ligament in comparison with the diffuse damage seen in professional overhead-throwing athletes. 18,31 Within this population, direct suture repair of the MUCL complex can restore valgus stability, decrease soft tissue dissection, and preserve bone as compared with reconstruction, enabling reliable and rapid recovery. 3,30,31 Furthermore, there is no need to wait for graft incorporation, which accelerates the recovery timetable. More recently, a technique for augmented MUCL repair with a collagen-dipped tape anchored on each end (InternalBrace; Arthrex) has shown promising results. 11 A biomechanical study by Dugas et al 11 indicate increased resistance to gapping at low cyclic loads in comparison with traditional reconstruction.
The purpose of this study was to evaluate the functional outcomes of young nonprofessional athletes undergoing MUCL repair with internal brace augmentation for medial elbow instability. Additionally, we sought to compare the proportion of those who were able to RTP, the mean Kerlan-Jobe Orthopaedic Clinic (KJOC) score, and the mean time to RTP according to location of tear, level of play, sport, and use of intraoperative platelet-rich plasma (PRP) and ulnar nerve transposition.
Methods
Institutional review board approval for this study was obtained before data collection. Between 2015 and 2017, nonprofessional athletes treated with MUCL repair with internal brace augmentation were prospectively followed as part of an elbow database for a minimum of 1 year. The operations were performed by 2 fellowship-trained surgeons at 2 facilities. No patients were lost to follow-up. Preoperatively, all patients were active in competitive athletics, coaching, or military duties and wished to continue their activities, which were limited by medial elbow pain and MUCL insufficiency. Our indications for repair were a focal area of ligament injury identified on magnetic resonance imaging (MRI; an injury of the proximal end, distal end, or both, with or without a small fragment of bone) and direct inspection in a patient who is at the college level or below and desires to continue throwing or other activities limited by their pain (Figure 1). Patients first completed a course of nonoperative management, which included a combination of rest and rehabilitation that varied by individual circumstance and typically lasted 3 months. In our practice, professional athletes or patients with diffuse ligament injury or degeneration on MRI or direct intraoperative inspection are treated with reconstruction. Patients were counseled on alternative treatment options, such as MUCL reconstruction, and signed informed consent for the procedure. Patients were excluded from the study if they had previous MUCL surgery or if intraoperative evaluation necessitated for reconstruction.
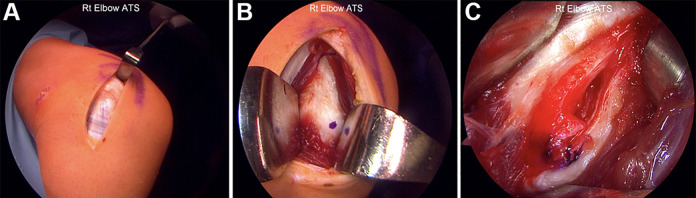
Figure 1.
Coronal T2-weighted magnetic resonance images of a left elbow showing a proximal medial ulnar collateral ligament injury (white and blue arrows) on sequential cuts. In panel A, the distal insertion is intact, and the midsubstance of the ligament has no degenerative signal.
Patient data included age, sex, handedness, type of sport or activity, level of competition, onset of symptoms, and follow-up. Preoperative data were recorded as follows: physical examination findings of generalized laxity, presence of MUCL tenderness, presence of paresthesia in the ulnar nerve distribution upon percussion at the level of the cubital tunnel, range of motion, and instability tests (eg, valgus stress, moving valgus stress). The valgus stress test was performed by placing the elbow in 20° of flexion while supinating the forearm and applying a valgus stress. A positive result elicited pain about the area of the medial elbow ligaments or widening of the medial joint line. A moving valgus stress test was similarly performed, moving the elbow from flexion to extension with the shoulder in full external rotation. The test result was considered positive when there was medial elbow pain between 120° and 70° of flexion.
Preoperative evaluations included anteroposterior and lateral radiographs, MRI, or computed tomography arthrograms. The images were read by orthopaedic board–certified sports surgeons (F.S. and M.O.) and classified as diffuse, partial, or complete tears with location identified as proximal, distal, or midsubstance. In select cases, an electromyograph was performed if symptoms of ulnar neuropathy were present. Examination under anesthesia and arthroscopic examination were performed to evaluate the elbow for medial, lateral, and posterolateral rotatory instability. Intraoperative findings were recorded for type of MUCL tear, location of tear, and any concomitant elbow pathology. Direct inspection of the MUCL is critical for decision-making, as any significant midsubstance degenerative changes or chronic attenuation of the ligament that precludes anatomic reduction is an indication for reconstruction. Clinical and functional outcomes were evaluated postoperatively using the KJOC Overhead Athlete Shoulder and Elbow Score and RTP data. Complications were recorded and detailed.
Surgical Technique
Before positioning, an examination under anesthesia was performed testing for valgus instability and any associated loss in terminal extension from olecranon osteophytes. The patient was then placed in the standard prone arthroscopy position with the arm flexed over a padded block on a standard arm board. A standard diagnostic elbow arthroscopy was completed, with any instability noted and concomitant pathology addressed.
The arm was then moved to full internal rotation of the shoulder, with the hinge of the arm board rotated toward the head and the dorsum of the hand rested on the board. This position ensured constant varus stress on the elbow while the medial side was repaired or reconstructed. A small incision was made from the tip of the medial epicondyle distally toward the sublime tubercle following a path anterior to the ulnar nerve. The dissection was continued while protecting the medial antebrachial cutaneous nerve, and the flexor pronator fascia was identified. The ulnar nerve was identified by palpation just posterior to the medial epicondyle and protected throughout the case. When necessary (typically only with distal injury patterns or in the setting of ulnar nerve symptoms), the nerve was decompressed by releasing the overlying fascia and dissecting distally between the 2 heads of the flexor carpi ulnaris; however, no transposition was performed unless there was instability during range of motion. The flexor-pronator fascia was then split longitudinally along the raphe of the anterior two-thirds and posterior one-third of the muscle. Using a Cobb for blunt dissection, the ulnar collateral ligament (UCL) was identified. 33 The MUCL tear was identified and characterized as proximal, distal, both, or midsubstance. If no intrasubstance degeneration or attenuation was noted within the MUCL, we proceeded with an augmented repair. The ligament and capsule were then split longitudinally at the location of the tear (Figure 2).
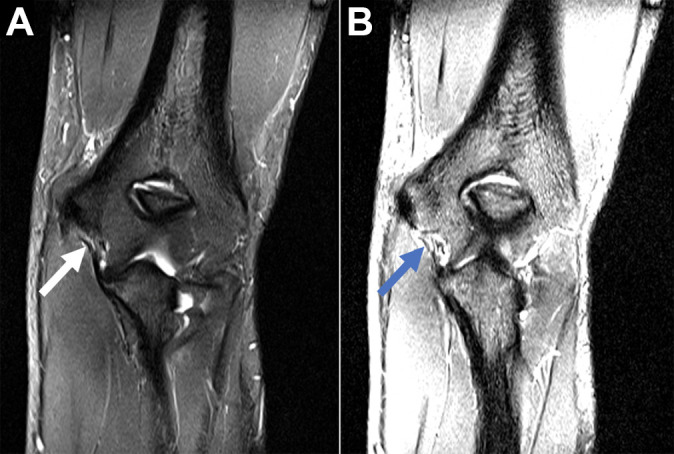
Figure 2.
(A) A right elbow is shown with the incision going from the medial epicondyle (superior on image) to the sublime tubercle (inferior). (B) The medial ulnar collateral ligament is visualized, and the joint line is marked with the blue dot. (C) The medial ulnar collateral ligament is then split, and the underlying tear can be visualized.
The tear in the ligament was identified (proximal or distal), and the first 3.5-mm SwiveLock anchor from the InternalBrace implant system was inserted at this location. Before anchor insertion, the bone was drilled with a 2.7-mm drill bit to a depth of 23 mm and tapped with a 3.8-mm tap. The preloaded FiberTape was 2 mm wide and had a type I bovine collagen coating. The No. 0 FiberWire stitch that ran through the eyelet of the anchor was passed as an inverted mattress stitch and tied down to repair the ligament (Figure 3).
Figure 3.
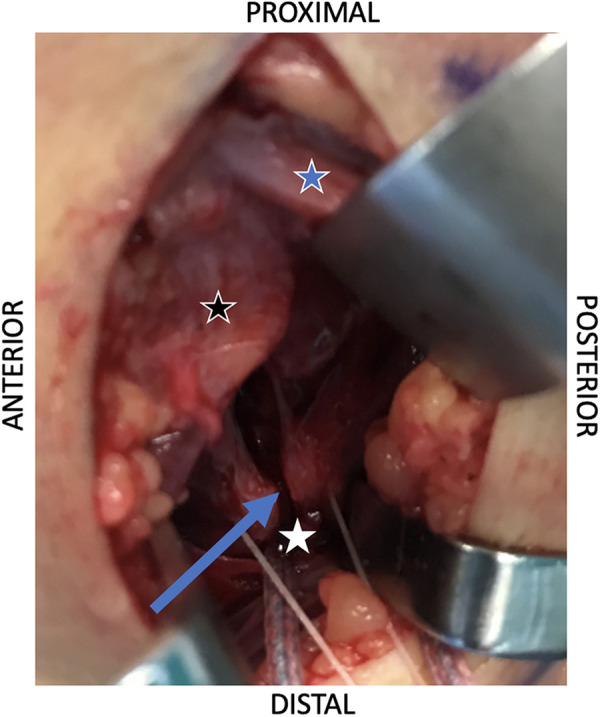
A right elbow is shown with the medial epicondyle at the top of the image and the sublime tubercle at the bottom. As this patient had an ulnar-sided injury, the first 3.0-mm SwiveLock anchor is placed at the sublime tubercle (white star). The ulnar nerve (blue star) is protected, and the flexor mass is depicted by the black star. The white FiberWire stitch is then placed in an inverted-mattress fashion around the torn ligament (blue arrow).
With the joint reduced, the FiberTape was tensioned to the unanchored side. The elbow was taken through a full arc of motion, and the isometry point was marked on the bone and drilled. The origin and insertion isometry points were described by Frangiamore et al 8 as being 8.5 mm distal and 7.8 mm anterior to the medial epicondyle of the humerus and medial ulnar ridge. The process was repeated, and the FiberTape was tensioned to the tunnel and marked 15.5 mm from the tunnel (to account for the length of the anchor seated in the bone); the second 3.5-mm anchor was then loaded to this mark. This ensured that the FiberTape was appropriately tensioned throughout a full arc of motion when the anchor was secured, and it prevented stress shielding of the MUCL (Figure 4).
Figure 4.
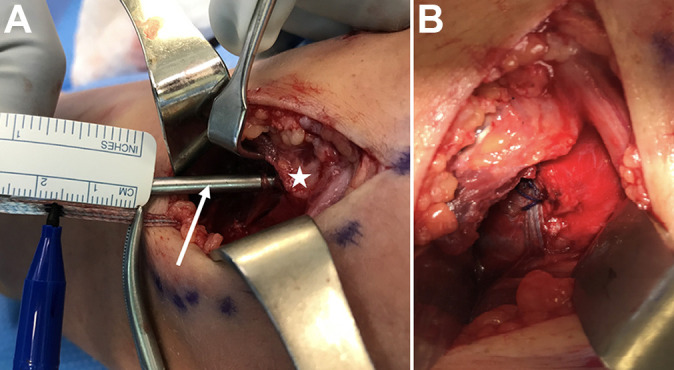
A right elbow is shown in both images. (A) The first anchor has already been inserted into the sublime tubercle (left side), and the white star marks the medial epicondyle. After drilling and tapping (white arrow) for the second suture anchor, the internal brace is pulled to its desired tension and marked with a hemostat at the level of the bone. The tape is marked 15.5 mm away from the hemostat. The anchor is loaded to this mark and inserted. This compensates for the length of the anchor and avoids overtensioning the internal brace. (B) The final construct after backup suture fixation with a 2-0 braided suture.
Next, a 2-0 braided suture (Orthocord; Johnson & Johnson) was used to tack the internal brace to the remaining ligament to prevent sliding. Frequently, a leukocyte-rich PRP blood clot (Harvest Technologies) was placed on top of the construct. PRP was used by 1 surgeon (F.S.) when the patient consented, although it was not used by the other surgeon (M.O.). In the case of proximal and distal injuries, a separate single-loaded 1.8-mm Q-Fix anchor with No. 2 suture (Smith & Nephew) was placed proximally at the most lateral aspect of the base of the medial epicondyle and used to repair the proximal aspect of the ligament. The first anchor for the internal brace was placed distally and the technique followed as stated with the second anchor being placed slightly more medial than the Q-Fix placement.
The flexor pronator fascia was then closed with 2-0 Vicryl, and the superficial tissue was closed with 2-0 braided absorbable suture, 4-0 monofilament suture, and surgical glue. Once the procedure was completed, the motion was checked 1 last time and a well-padded posterior splint was applied.
Postoperative Protocol
The posterior splint was switched to a hinged elbow brace at 1 week, and physical therapy initially focused on leg, core, and scapular strengthening. Shoulder and wrist exercises were allowed as long as there was no elbow pain. The brace was worn full-time and set in a pain-free arc, typically between 60° and 90°. This was increased as pain and swelling resolved, with the goal to have the brace unlocked by 4 weeks. At this time, more aggressive elbow and wrist exercises were incorporated into the process. By 6 to 8 weeks postoperatively, the goal was to begin a “return to hit and throw” program started in the brace. At 12 weeks, the program was continued without the brace, and the patient could resume sporting activities when the RTP program was completed.
Results
During the study period, 45 patients consented to UCL repair. However, 1 patient underwent conversion to UCL reconstruction intraoperatively. Another patient was a professional athlete and thus excluded, as were 3 patients who had concomitant procedures during MUCL repair: a triceps repair, an endoscopic excision of a triceps traction spur with tendon repair, and an open flexor pronator repair and ulnar nerve transposition.
Therefore, 40 patients met the inclusion criteria for this study (Table 1). The mean age of 35 male and 5 female patients was 17.8 years (range, 14-28 years). The mean follow-up was 23.8 months (range, 12-44 months). All overhead athletes had the dominant arm affected. Thirty-five (87.5%) patients were baseball players, although specific positional data were not recorded. The other 5 patients (12.5%) were involved in other activities, such as competitive tumbling sports (n = 2), and volleyball coaching (n = 1). No patients were lost to follow-up. Preoperatively, all patients reported medial elbow tenderness, but only 27.5% noted acute pain or an audible “pop.” Additionally, 39 (97.5%) had a positive valgus stress test finding, and 34 (85.0%) had tenderness over the MUCL; however, it was not recorded if the tenderness was proximal or distal, and 3 (5.0%) had paresthesia in the ulnar distribution upon palpation of the ulnar nerve at the level of the cubital tunnel. The mean time from onset of the symptoms to the date of surgery was 8.8 months (range, 0.3-62.3 months). One patient had previous open reduction of the elbow but continued to have persistent medial elbow pain and instability that necessitated repair of the MUCL. Otherwise, no other patients had prior elbow surgery. The dominant arm of the tumbling athletes was not recorded.
Table 1.
Patient Characteristics and Preoperative Treatment
| Variable | No. of Patients |
|---|---|
| Sex | |
| Male | 35 |
| Female | 5 |
| Dominant arm | |
| Left | 10 |
| Right | 30 |
| Sport or activity | |
| Baseball | 35 |
| Tumblers | 4 |
| Volleyball | 1 |
| Level of play | |
| High school | 22 |
| College | 17 |
| Employment (coach) | 1 |
| Preoperative treatment | |
| Physical therapy | 26 |
| Activity modification | 32 |
| Sling/brace | 11 |
| Over-the-counter medication | 20 |
| Platelet-rich plasma injection | 8 |
| Steroids | 2 |
All patients had MRI testing with or without contrast that revealed damage to the MUCL. Two patients had MRI results indicating isolated proximal tears, with “damage to the UCL” in another, and all 3 patients had proximal and distal tears upon intraoperative examination. Upon examination, 39 patients (97.5%) had a positive result on the valgus stress test; 34 (85.0%) had tenderness to palpation over the MUCL; and 3 (7.5%) had paresthesia in the ulnar nerve distribution upon palpation of the nerve at the level of the cubital tunnel (Table 2). Upon intraoperative evaluation, 32 patients demonstrated valgus laxity during the arthroscopic portion of the operation. Intraoperative assessment revealed that 6 patients had distal MUCL tears, 28 proximal, 5 proximal and distal, and 1 an acute midsubstance (Table 2). For the patient with the midsubstance tear, there was no degeneration of the ligament, so the decision was made to proceed with repair using a free repair stitch, as opposed to the stitch loaded in the eyelet of the first anchor. Two patients had concomitant ulnar nerve transposition and were able to RTP.
Table 2.
Preoperative and Intraoperative Findings a
| Finding | No. of Patients |
|---|---|
| Physical examination | |
| Valgus stress test | 39 |
| Tenderness to palpation over medial UCL | 34 |
| Paresthesia in the ulnar distribution on palpation | 3 |
| Magnetic resonance imaging | |
| Distal tear | 6 |
| Proximal tear | 30 |
| Distal and proximal tears | 2 |
| Midsubstance tear | 1 |
| Damage to UCL | 1 |
| Arthroscopy | |
| Valgus laxity | 32 |
| Synovitis | 3 |
| Intraoperative diagnosis | |
| Distal tear | 6 |
| Proximal tear | 28 |
| Distal and proximal tears | 5 |
| Midsubstance tear | 1 |
a UCL, ulnar collateral ligament.
Return to Play
Thirty-seven patients (92.5%) returned to play or coaching at their full preinjury levels at a mean 6.9 months (range, 2-12 months). Three patients did not RTP. One had a concomitant cancer diagnosis that prevented physical participation in athletic activity. Another had evidence of full healing of the MUCL on ultrasound postsurgery without symptoms but did not return to sport owing to fear of reinjury. The third patient had a concomitant cancer diagnosis that hindered the ability to return to full competition. No patients reported failure of the repair.
Functional Outcomes
The mean KJOC Overhead Athlete Shoulder and Elbow Score was 92.6 (range, 64-100). Overall, 95% of patients were satisfied with the results of their surgery. Both of those who were not satisfied with their surgery results cited being unable to RTP as the reason.
Comparative Subgroup Analysis
At the high school level, 95.4% of athletes (21/22) were able to return to the previous level of competition or higher, with a mean KJOC score of 95.3 (range, 64-100). At the college level, 88.2% of athletes (15/17) returned to play at the previous level of competition or higher, with a mean KJOC score of 93.9 (range, 71-100). The 1 coach was able to return to duty, with a KJOC score of 87 (Table 3). There was no statistical difference in RTP by location of tear, level of play, use of intraoperative PRP injection, or concomitant ulnar nerve transposition. Of the 40 patients, 26 (65%) received an intraoperative PRP injection, and 92.3% (n = 24) were able to RTP. Of the 14 who did not receive an injection, 92.8% (n = 13) were able to RTP.
Table 3.
Comparative Subgroup Analysis a
| No. of Patients | RTP, No. (% of Subgroup) | Time to RTP, mo | Mean KJOC Score | |
|---|---|---|---|---|
| Tear location | ||||
| Distal | 6 | 5 (83.3) | 7.00 | 96.14 |
| Proximal | 28 | 27 (96.4) | 7.15 | 92.86 |
| Distal and proximal | 5 | 4 (80.0) | 7.83 | 95.17 |
| Midsubstance | 1 | 1 (100.0) | 5.00 | 100.00 |
| Level of play | ||||
| High school | 22 | 21 (95.4) | 7.37 | 95.33 |
| College | 17 | 15 (88.2) | 7.22 | 93.39 |
| Employment (coach) | 1 | 1 (100.0) | 5.67 | 87.00 |
| Sport or activity | ||||
| Baseball | 35 | 33 (94.4) | 4.05 | 95.13 |
| Tumblers | 4 | 3 (75.0) | 5.13 | 89.5 |
| Employment | 1 | 1 (100.0) | 2.50 | 87.00 |
a KJOC, Kerlan-Jobe Orthopaedic Clinic; RTP, return to play.
Complications
There was 1 complication (2.5%) noted at most recent follow-up. One patient reported ulnar nerve paresthesia that presented after surgery but resolved within 6 weeks postoperation.
Discussion
This study presents a case series of patients who underwent primary repair of the MUCL with a collagen-dipped fiber tape internal brace augmentation. This is one of the first reports of the clinical and functional outcomes of this procedure, which was introduced by Dugas et al 11 after initial biomechanical studies indicated similar strength with increased resistance to gap formation as compared with reconstruction.
MUCL repair is not a new concept and was first reported with success in 4 patients by Norwood et al 26 in 1981. However, when Conway et al 9 studied Dr Jobe’s original cohort, which included repair and reconstruction, there was only a 50% rate of return after repair. This rate dropped to 29% (2/7) in professional baseball players undergoing repair. This finding was reproduced in subsequent research by Azar et al, 4 with an RTP rate of 63% versus 81% in repair versus reconstruction in the professional athlete. Given the lower RTP rates in professionals, it was largely abandoned as part of the treatment algorithm.
Increasing evidence suggests that MUCL repair after failure of nonoperative management may produce favorable outcomes and a more rapid RTP in carefully selected nonprofessional athletes. 31 It has been proposed that younger overhead athletes lack the chronic attritional damage and secondary pathologic changes involving the nonligamentous parts of the elbow that are common among professional athletes, which may allow an elbow to be more amenable to repair. 31 Furthermore, it has been shown that the MUCL has sufficient vascularization to allow for adequate healing in the setting of more acute or discrete trauma. 14 Additionally, the young nonprofessional population likely places lower stress on the repaired ligament as compared with its professional counterparts.
In an early study on repair in younger athletes, Argo et al 3 reported on 19 female patients with a mean age of 22 years who underwent repair utilizing various techniques, including plication, anchor-based repair, and drill holes. The authors reported excellent overall results in 16 patients and good results in 2 patients. Of the 18 patients, 17 (94.4%) who played sports were able to RTP at a mean 2.5 months. However, 1 patient did require graft reconstruction after intraoperative evaluation of the ligament. In 2008, Richard et al 30 treated 11 athletes with repair rather than reconstruction. Of the 11 patients, 9 (82%) were able to return to sport within 6 months of surgery. Similarly, Savoie et al 31 reported a case series of 60 patients who underwent direct anchor-based repair of MUCL avulsion injuries. Forty-seven male and 13 female patients with a mean age of 17.2 years underwent the primary repair. Results indicated that the mean Andrews-Carson outcomes score improved from 132 to 188 postoperation with good to excellent outcomes in 93% of patients and 58 (97%) who were able to RTP at the same level or higher than before the injury. These results indicated significant improvement in comparison with past UCL repair studies 3,4,9,26 that primarily focused on professional athletes.
Dugas et al 34 introduced a new technique of augmented MUCL repair utilizing a collagen-dipped fiber tape internal brace. They treated 22 high school–level athletes with this technique and reported an RTP rate of 95.5%, with only 1 pitcher (out of 13) unable to return. Subsequently, an initial biomechanical study by Dugas et al 11 compared the characteristics of 9 matched pairs undergoing traditional MUCL reconstruction and primary repair with internal brace augmentation. The results indicated that the repair group showed significantly more resistance to gapping than the reconstruction group and a similar time zero strength. Mazzocca et al 22 examined the healing response to collagen-coated sutures versus standard commercial sutures. The authors concluded that at the 24- and 48-hour periods, the addition of type 1 collagen to polyester/polyethylene sutures may stimulate the adhesion, proliferation, and differentiation of primary osteoblasts and tenocytes in comparison with standard commercial sutures. Murray et al 17 conducted a comparison of ACL repair with suture and suture with collagen-platelet composite augmentation in immature pigs. The authors indicated that the addition of the collagen-platelet composite yielded improved linear stiffness, with a significant increase in cellularity within the healing ligament as compared with the control. Furthermore, the internal brace can protect the ligament through stress shielding while healing is taking place. This has been shown in the ACL literature where a suture brace construct was added to small hamstring grafts (<8 mm) to add protection during the weak remodeling phase of graft incorporation. Bedi et al 25 showed that the addition of the suture tape significantly decreased total graft elongation by 56% and increased dynamic stiffness.
In 2019, Dugas et al 10 reported initial results in a larger cohort undergoing MUCL repair with internal brace augmentation (111 overhead-throwing athletes; mean age, 18.3 years). A majority of the patients were high school and college athletes (95%) and baseball players (92%). The results indicated that 102 (92%) athletes were able to RTP at the same level or higher versus preoperation in a mean 6.7 months. An additional case study cited the RTP of a college football player 4 months postoperation. 35 We found high RTP rates (92.5%) at a mean 6.9 months, which is similar to results recently published by Dugas et al. 10,34 Comparatively, in a large study on reconstructions, Cain et al 6 stated that 83% of patients returned to play at a mean 11.6 months.
The mean KJOC score at final follow-up in our study was 92.6. This is significant in that it approaches that of the study by Kraeutler et al, 20 who cited a mean KJOC score of 94.8 in 44 asymptomatic baseball players.
There were minimal differences in subgroup analysis in level of play (high school vs college), use of PRP, concomitant ulnar nerve transposition, and location of injury (proximal, distal, or both) with regard to RTP, KJOC scores, or time to RTP. However, the study was underpowered to make any significant conclusions. The use of PRP and bracing has had some success in nonoperative treatment of acute MUCL injuries, so its inconsistent use in this study may confound the effects of the repair with the internal brace. There was minimal difference in outcomes based on the addition of PRP, although again the study was underpowered to make this conclusion. We do recommend, when possible, the addition of PRP to the repair construct given the results previously demonstrated with nonoperative treatment.
The limitations of this study first include the short-term follow-up (mean, 24 months; range, 12-44 months) and the lack of a comparison group against the more traditional reconstruction procedure. Second, the addition of PRP to the repair construct was inconsistent, although in subgroup analysis (Table 1) there was minimal difference in outcomes based on the addition of PRP. Positional data for baseball players were not available, which would have been informative as MUCL strain is variable by position. Given the number of patients in our series, although we would not have been able to perform a subgroup statistical analysis among positions, we acknowledge that it still is important when making surgical decisions. Additionally, our study comprised 40 patients, which may not allow for definitive conclusions based on our results. Furthermore, the functional outcomes of this study were gathered by follow-up in office and over the phone, potentially introducing bias. However, Erickson et al 12 reported that the KJOC questionnaire can be administered over the phone with results not being significantly different versus those in person. Last, follow-up examination and imaging results were not included in our study.
Conclusion
Medial elbow instability within the young nonprofessional athlete population is an increasing problem attributed to an increased incidence of injury. Primary repair in this population has been indicated as a useful technique in the event of failure of nonoperative treatment. The augmentation of the primary repair utilizing a collagen-dipped fiber tape internal brace has shown promising functional results and should be considered a viable alternative to the traditional repair technique.
Footnotes
Final revision submitted December 13, 2020; accepted February 3, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.O. has received education payments from Arthrex, Smith & Nephew, and Alon Medical Technology and grant support from Arthrex. J.H. has received honoraria from Horizon Therapeutics. M.O. has received consulting fees from Smith & Nephew, Arthrex, DePuy Mitek, Stryker, and Wright Medical. F.S. has received nonconsulting fees from Smith & Nephew; royalties and speaking fees from Linvatec; and consulting fees from Exactech, DePuy, and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Tulane University (2019-786).
References
- 1. An KN, Morrey BF, Chao EY. The effect of partial removal of proximal ulna on elbow constraint. Clin Orthop Relat Res. 1986;209:270–279. [PubMed] [Google Scholar]
- 2. Andrews JR, Heggland EJ, Fleisig GS, Zheng N. Relationship of ulnar collateral ligament strain to amount of medial olecranon osteotomy. Am J Sports Med. 2001;29(6):716–721. [DOI] [PubMed] [Google Scholar]
- 3. Argo D, Trenhaile SW, Savoie FH, 3rd, Field LD. Operative treatment of ulnar collateral ligament insufficiency of the elbow in female athletes. Am J Sports Med. 2006;34(3):431–437. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23. [DOI] [PubMed] [Google Scholar]
- 5. Barnes DA, Tullos HS. An analysis of 100 symptomatic baseball players. Am J Sports Med. 1978;6(2):62–67. [DOI] [PubMed] [Google Scholar]
- 6. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 7. Chauhan A, McQueen P, Chalmers PN, et al. Nonoperative treatment of elbow ulnar collateral ligament injuries with and without platelet-rich plasma in professional baseball players: a comparative and matched cohort analysis. Am J Sports Med. 2019;47(13):3107–3119. [DOI] [PubMed] [Google Scholar]
- 8. Cinque ME, Schickendantz M, Frangiamore S. Review of anatomy of the medial ulnar collateral ligament complex of the elbow. Curr Rev Musculoskelet Med. 2020;13(1):96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67–83. [PubMed] [Google Scholar]
- 10. Dugas JR, Looze CA, Capogna B, et al. Ulnar collateral ligament repair with collagen-dipped FiberTape augmentation in overhead-throwing athletes. Am J Sports Med. 2019;47(5):1096–1102. [DOI] [PubMed] [Google Scholar]
- 11. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–741. [DOI] [PubMed] [Google Scholar]
- 12. Erickson BJ, Chalmers PN, Newgren J, et al. Can the Kerlan-Jobe Orthopaedic Clinic shoulder and elbow score be reliably administered over the phone? A randomized study. Orthop J Sports Med. 2018;6(8):2325967118791510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233–239. [DOI] [PubMed] [Google Scholar]
- 14. Frangiamore SJ, Morris ER, Scibetta AC, et al. Evaluation of endothelial and vascular-derived progenitor cell populations in the proximal and distal UCL of the elbow: a comparative study. Orthop J Sports Med. 2018;6(6):2325967118777825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gainor BJ, Piotrowski G, Puhl J, Allen WC, Hagen R. The throw: biomechanics and acute injury. Am J Sports Med. 1980;8(2):114–118. [DOI] [PubMed] [Google Scholar]
- 16. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68(8):1158–1163. [PubMed] [Google Scholar]
- 17. Joshi SM, Mastrangelo AN, Magarian EM, Fleming BC, Murray MM. Collagen-platelet composite enhances biomechanical and histologic healing of the porcine anterior cruciate ligament. Am J Sports Med. 2009;37(12):2401–2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Joyner PW, Bruce J, Hess R, Mates A, Mills FBT, Andrews JR. Magnetic resonance imaging–based classification for ulnar collateral ligament injuries of the elbow. J Shoulder Elbow Surg. 2016;25(10):1710–1716. [DOI] [PubMed] [Google Scholar]
- 19. Kenter K, Behr CT, Warren RF, O’Brien SJ, Barnes R. Acute elbow injuries in the National Football League. J Shoulder Elbow Surg. 2000;9(1):1–5. [DOI] [PubMed] [Google Scholar]
- 20. Kraeutler MJ, Ciccotti MG, Dodson CC, Frederick RW, Cammarota B, Cohen SB. Kerlan-Jobe Orthopaedic Clinic overhead athlete scores in asymptomatic professional baseball pitchers. J Shoulder Elbow Surg. 2013;22(3):329–332. [DOI] [PubMed] [Google Scholar]
- 21. Loftice J, Fleisig GS, Zheng N, Andrews JR. Biomechanics of the elbow in sports. Clin Sports Med. 2004;23(4):519–530. [DOI] [PubMed] [Google Scholar]
- 22. Mazzocca AD, McCarthy MB, Arciero C, et al. Tendon and bone responses to a collagen-coated suture material. J Shoulder Elbow Surg. 2007;16(5):S222–S230. [DOI] [PubMed] [Google Scholar]
- 23. Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985;201:84–90. [PubMed] [Google Scholar]
- 24. Morrey BF, Tanaka S, An KN. Valgus stability of the elbow: a definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;265:187–195. [PubMed] [Google Scholar]
- 25. Noonan BC, Bachmaier S, Wijdicks CA, Bedi A. Independent suture tape reinforcement of tripled smaller-diameter and quadrupled grafts for anterior cruciate ligament reconstruction with tibial screw fixation: a biomechanical full construct model. Arthroscopy. 2020;36(2):481–489. [DOI] [PubMed] [Google Scholar]
- 26. Norwood LA, Shook JA, Andrews JR. Acute medial elbow ruptures. Am J Sports Med. 1981;9(1):16–19. [DOI] [PubMed] [Google Scholar]
- 27. Olsen SJ, 2nd, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34(6):905–912. [DOI] [PubMed] [Google Scholar]
- 28. Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32(5):1158–1164. [DOI] [PubMed] [Google Scholar]
- 29. Regan WD, Korinek SL, Morrey BF, An KN. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. 1991;271:170–179. [PubMed] [Google Scholar]
- 30. Richard MJ, Aldridge JM, 3rd, Wiesler ER, Ruch DS. Traumatic valgus instability of the elbow: pathoanatomy and results of direct repair. J Bone Joint Surg Am. 2008;90(11):2416–2422. [DOI] [PubMed] [Google Scholar]
- 31. Savoie FH, 3rd, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36(6):1066–1072. [DOI] [PubMed] [Google Scholar]
- 32. Schwab GH, Bennett JB, Woods GW, Tullos HS. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop Relat Res. 1980;146:42–52. [PubMed] [Google Scholar]
- 33. Smith GR, Altchek DW, Pagnani MJ, Keeley JR. A muscle-splitting approach to the ulnar collateral ligament of the elbow: neuroanatomy and operative technique. Am J Sports Med. 1996;24(5):575–580. [DOI] [PubMed] [Google Scholar]
- 34. Walters BL, Cain EL, Emblom BA, Frantz JT, Dugas JR. Ulnar collateral ligament repair with internal brace augmentation: a novel UCL repair technique in the young adolescent athlete. Orthop J Sports Med. 2016;4(3_suppl_3):2325967116S00071. [Google Scholar]
- 35. Wilson WT, Hopper GP, Byrne PA, MacKay GM. Repair of the ulnar collateral ligament of the elbow with internal brace augmentation: a 5-year follow-up. BMJ Case Rep. 2018;11(1):e227113. [DOI] [PMC free article] [PubMed] [Google Scholar]