Abstract
Background:
Return to sport (RTS) commonly serves as a measure for assessment of clinical outcomes in orthopaedic sports medicine surgery. Unfortunately, while RTS is commonly utilized in research for this purpose, currently there is no widely accepted or standardized definition for when an athlete has officially returned to his or her sport.
Purpose:
To conduct a systematic review to evaluate and report the differences in specific definitions of RTS utilized in the orthopaedic surgery literature.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was performed using PubMed, EMBASE, and Cochrane Trials databases per PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Search terms consisted of variations of “RTS” combined with variations of “orthopedic surgery” and “define” to capture as many relevant articles as possible. The definition of RTS was recorded and analyzed.
Results:
A total of 718 articles were identified in the initial search, 29 of which met eligibility criteria, providing a clear definition of RTS. Of the 29 studies included, 20 (69.0%) defined RTS as an athlete competing in a game or other competitive play. Three (10.3%) defined this as the athlete competing in a game or other competitive play but with an explicitly stated competition-level modifier of the athlete returning to his or her preinjury level of competition. Two articles (6.9%) included returning to training or practice, and the remaining 4 articles (13.8%) used terminology other than the standard RTS.
Conclusion:
There is variability in the definition of RTS used in orthopaedic sports medicine literature. Most studies refer to the athlete competing in a game or other competitive play. Other variants include returning to practice/training and explicitly defined competition levels and objectives. Future studies should aim to standardize the definition of RTS to facilitate more precise assessment of outcome after sports medicine surgery. Using terminology that describes components of the recovery and rehabilitation process, such as “return to participation” and “return to performance,” in addition to RTS will allow us to more clearly understand the athlete’s recovery and associated level of competition or performance.
Keywords: athletic training, medical aspect of sports, physical therapy/rehabilitation, return to play, return to sport
A desire to return to sport (RTS) participation after orthopaedic surgery is a powerful motivating factor and, oftentimes, the primary measure of success from the athlete’s standpoint. Therefore, RTS, also referred to as return to play (RTP), has become an often-cited surrogate for clinical outcomes in orthopaedic sports medicine surgery. Unfortunately, while it is commonly utilized in research for this purpose, currently there is no standardized or widely accepted definition for when an athlete has officially returned to his or her sport. This lack of standardization can result in inaccurate comparisons, difficulty managing patient expectations, and patient disappointment.
Many potential variables exist in reporting RTS, including the type of activity to which the athlete returns (regular season or preseason game vs practice), the volume (1 game vs a season), the level of competition (high school, college, professional), and type of sport (throwing, contact, noncontact). Because of the variations in reporting, many authors have called for a more standardized approach to reporting RTS. 1,25 For instance, a 2018 meta-analysis of RTS after surgical treatment of femoroacetabular impingement (FAI) syndrome found an overall RTS at any level of 91% but an RTS at the same level of competition of 74%. 24 Additionally, Wörner et al 34 reported an 89% RTS after hip arthroscopy for FAI when patients were asked in a general way (return to participation in some sort of sport or exercise) but reported only a 28% RTS in the same preinjury sport at a lower competition level and a 21% RTS in the same sport at the same or higher competition level. These studies demonstrate the disparity that can occur between reported RTS levels when the definition for RTS is not clearly established.
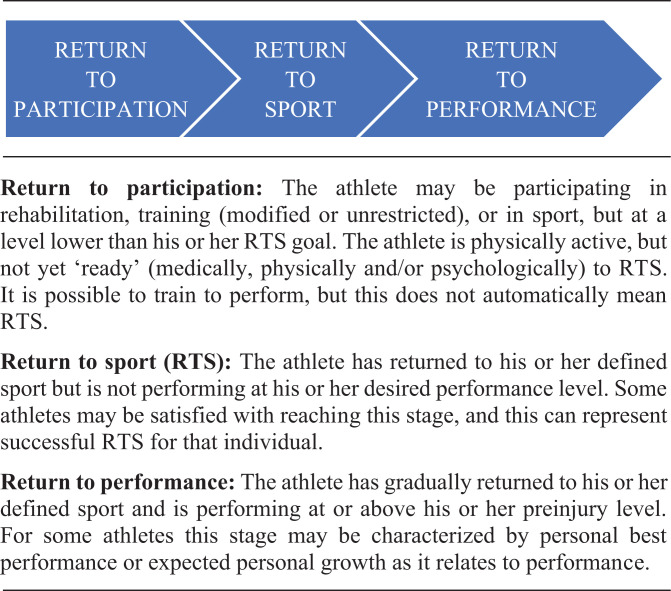
Most RTS outcomes are reported as binary (returned to sport or did not), while an athlete’s postinjury clinical course is more complex and best viewed as a spectrum of recovery. 1 In a 2016 consensus statement on RTS, Ardern et al 1 proposed a model that defines 3 elements of RTS: return to participation, RTS, and return to performance. 1 Combining these elements in the reporting of RTS will result in a more complete picture of an athlete’s recovery. The purpose of this study was to conduct a systematic review to evaluate and report the differences in specific definitions of RTS utilized in the orthopaedic surgery literature. We hypothesized that there would be substantial variability in the reported definitions of RTS.
Methods
Study Design
A systematic search was performed using PubMed, EMBASE, and Cochrane Trials databases and according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (April 2020) to identify and collect articles defining RTS/RTP.
Search Strategy
The search strategy aimed to capture articles that defined RTS and involved athletes who had undergone orthopaedic surgery. The search terms consisted of the following phrases and their synonyms: “return to sport” (“return to play,” “RTS,” “RTP,” “Return to Sporting Activities,” “Return to Sporting Activity,” “Resumption of Sporting Activity,” and “Resumption of Sporting Activities”), “orthopedic procedures” (“orthopedic procedure,” “orthopedic surgery,” “orthopedic surgeries,” post op*, surger*, “surgical,” “reconstruction,” arthroscop*, and “orthopedic”) and “define” (“defines,” “definition,” “defined,” and “defining”). Synonyms were linked using the Boolean command “OR,” and the three phrases were combined using the Boolean command “AND”. A variety of word combinations were used, “/exp” term “explosions” were used in Embase, and Medical Subject Headings terms were used in PubMed when appropriate in order to capture as many definitions as possible. Because of the large volume of articles involving RTS combined with orthopaedic surgery, the term “define” was included to capture articles that defined RTS in the abstract. Accordingly, while this search strategy resulted in a manageable number of full texts to review, it also likely missed numerous articles, which may have defined RTS in the body of the text but not in the abstract.
Eligibility Criteria
This review included articles written in English with abstracts that provided a definition of RTS or referred to a definition being given in the full text of the paper. Inclusion criteria aimed to capture articles studying athletes who had undergone orthopaedic surgery for a sport-related injury. To capture as many relevant articles as possible, the search was not limited to a specific injury or sport. Articles that solely used medical or rehabilitation guidelines/criteria (eg, strength or range of motion testing, pain scale) to determine when an athlete was cleared to RTS were excluded, as these did not provide a definition of when an athlete actually returned to his or her sport. Concussion studies, case reports, systematic reviews, narratives, commentaries, editorials, cadaveric studies, animal studies, and published abstracts that did not have a full-text article were excluded.
Data Extraction
The systematic review was conducted per PRISMA guidelines, as noted, and interreviewer agreement of the studies to be included was determined as follows: 2 authors (J.D. and J.M.A.) independently performed the search, removed duplicates, and screened titles and abstracts for relevance and a clear definition of RTS. Three authors (J.D., J.M.A, and M.J.M.) then screened the remaining full-text articles against the eligibility criteria. Any relevant studies referenced by the remaining articles were also identified and screened against the eligibility criteria. Interreviewer disagreement about an article’s eligibility for inclusion was resolved by a majority ruling among the 3 reviewers.
Results
Search Results
As shown in the PRISMA flow diagram (Figure 1), a total of 718 articles were originally identified across the 3 databases (238 from PubMed, 461 from EMBASE, and 19 from Cochrane Trials). Of these, 228 duplicates were excluded, leaving 490 articles. After screening titles and then abstracts for relevance, 455 articles were excluded, leaving 35 articles. Of these, 7 were excluded based on the eligibility criteria, and 1 article that was referenced by an included article was identified as being relevant and meeting eligibility criteria. This resulted in a total of 29 articles, which are summarized in Appendix Table A1. Given that this study did not analyze any of the data or conclusions from the articles, we did not believe it was necessary to determine and report on the quality of the included studies.
Figure 1.
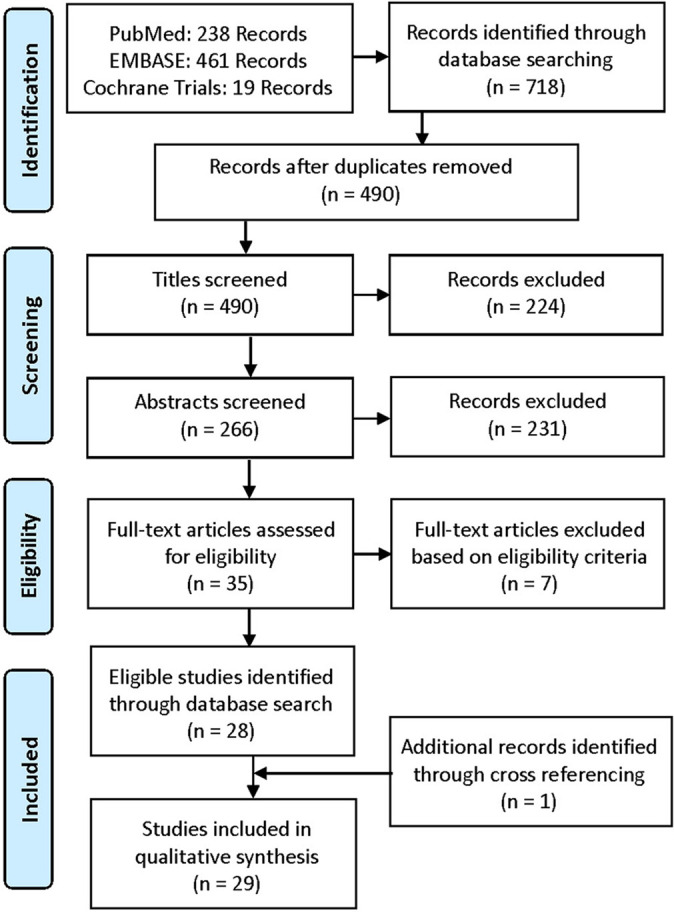
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
Types of Publications and Their Contents
The articles included in this systematic review evaluated athletes in professional hockey (2 articles 23,28 ), professional football (9 articles § ), professional baseball (4 articles 9,12 –14 ), professional basketball (2 articles 4,15 ), professional soccer (1 article 30 ), across >1 professional sport (3 articles 7,16,19 ), collegiate football (1 article 32 ), baseball athletes across several levels of competition (1 article 6 ), high school athletes across several sports (1 article 3 ), and overhead-throwing athletes of many ages (1 article 22 ). Some articles focused on injuries across multiple age groups and sports (4 articles 11,21,26,27 ). The surgeries reported in the studies included arthroscopic labral repair in FAI (hip arthroscopy) (11 articles ∥ ), anterior cruciate ligament reconstruction (3 articles 3,8,19 ), Achilles tendon repair (2 articles 30,35 ), hindfoot arthroscopy (1 article 27 ), arthroscopic treatment of internal impingement of the shoulder (1 article 22 ), ligament reconstruction of the Lisfranc joint (1 article 21 ), clavicle open reduction and internal fixation (1 article 17 ), forearm open reduction and internal fixation (1 article 29 ), thumb ulnar collateral ligament repair (3 articles 14,31,32 ), Tommy John surgery (ulnar collateral ligament reconstruction) (1 article 13 ), repair of acute superficial deltoid complex avulsion during ankle fracture fixation (1 article 10 ), hook of hamate excision (1 article 6 ), partial lateral meniscectomy (1 article 2 ), and operative Jones fracture treatment (1 article 18 ). In addition, 25 of the 29 included studies ¶ (86.2%) reported data on time to RTS, 7 studies 11,21 -23,26,27,32 (24.1%) reported on patient-reported outcomes, and 15 studies 4,7-9,12 -17,19,28 -31 (51.7%) utilized sport-specific metrics in the data and evaluation of RTS.
Definition of RTS/RTP
Of the 29 articles that met inclusion criteria, 14 articles 8,11 -17,23,26,28 -31 (48.3%) used the terminology “return to sport,” 11 articles # (37.9%) used “return to play,” 1 article 3 (3.4%) used “return to competitive play,” 1 article 21 (3.4%) used “return to athletic activity,” 1 article 27 (3.4%) used “return to sporting activities,” and 1 article 22 (3.4%) used “favorable return to sport outcome (RTS +).” The most common definitions of RTS and RTP are summarized in Table 1. The less commonly used terminologies are individually described below, and all are listed in Appendix Table A1.
Table 1.
Definitions of RTS and RTP in the 29 Included Studies a
| Definition | Studies |
|---|---|
| Playing in at least 1 game of the athletes’ respective sport or the first game played after surgery | 12 studies 4,8,12 –17,28 –31 |
| The first regular season game played after surgery | 3 studies 10,18,19 |
| The first preseason or regular season game played after surgery | 3 studies 2,9,20 |
| The first regular or postseason game played after surgery | 2 studies 7,35 |
| Specification of competition level | 3 studies 6,11,26 |
| Return to training or practice | 2 studies 23,32 |
| Articles that did not use RTS or RTP | 4 studies 3,21,22,27 |
a RTP, return to play; RTS, return to sport.
Twelve articles (41.4%), 6 by Jack et al, 12 –17 4 by Sochacki et al, 28 –31 1 by Begly et al, 4 and 1 by Cinque et al, 8 defined RTS as playing in at least 1 game of the athletes’ respective sport or the first game played after surgery. All of these articles used the terminology “RTS” and explicitly stated this definition except Begly et al, 4 who used “RTP” and defined RTP as competing in a professional basketball game of equal competition level after surgery.
Three articles 10,18,19 (10.3%) specified that RTS is defined as the first regular season game played after surgery. Two of these articles, Hsu et al 10 and Lareau et al, 18 explicitly stated this definition of RTP. Mai et al 19 defined RTP as successful return to the active roster for at least 1 regular season game after surgery. Three articles 2,9,20 (10.3%) defined RTS as the first preseason or regular season game played after surgery. Menge et al 20 explicitly stated this definition of RTP in professional football players. Frangiamore et al 9 defined RTP in Major League Baseball players as playing in a preseason or regular season major or minor league game after surgery. Aune et al 2 included the first preseason game in their definition of RTP in National Football League players, provided that the athlete played in a subsequent regular season game. Two articles (6.9%), Yang et al 35 and Christian et al, 7 defined RTS as the first regular season or postseason game played after surgery. Three articles 6,11,26 (10.3%) included a specification of competition level in their definition of RTS. Rosinsky et al 26 defined RTP as a patient’s return to competitive participation in his or her sport at the same or higher level of competition than that of presurgery, regardless of time elapsed after surgery. Burleson and Shin 6 defined RTP in baseball players as reaching the athlete’s preinjury level of competition and being able to perform full sports activities. Ishoi et al 11 defined RTS as the athlete being engaged in one’s preinjury sport at preinjury level of competition at follow-up with a mean follow-up of 33.1 ± 16.3 months.
Two articles (6.9%), Philippon et al 23 and Werner et al, 32 included returning to training in their definitions of RTS and RTP. Philippon et al defined RTS in professional hockey players as the player resuming skating for training or participation in the sport of ice hockey. Werner et al defined RTP in collegiate athletes as when both the senior author and athletic trainer released the patient to return to game play (when in season) or practice (when out of season).
Four studies 3,21,22,27 (13.8%) used terminology other than the standard RTS or RTP and each study included a specification of competition level in their definition. Bauer et al 3 defined “return to competitive play” in high school athletes as return to the same sport that was played preinjury within 1 year of surgery and specified that the sport had to be organized---that is, collegiate, interscholastic, “travel” or club teams, organized intramural sports, or tournaments. Smyth et al 27 defined “return to sporting activities” as being calculated as the time period from the date of surgery until the patient was able to participate at one’s previous level of competition. Miyamoto et al 21 defined “return to athletic activity” as return to near preinjury performance level, although the authors did not state how this was determined. Peduzzi et al 22 distinguished between RTS + and RTS – in overhead-throwing athletes, defining a “favorable RTS outcome (RTS +)” as returning to the previous sport at a same or higher level of competition and defining “RTS –” as returning to the previous sport at a lower level of competition, a switch to another sport, or an inability to engage in any sport. The article analyzed the level of competition by determining whether the athletes competed recreationally, in regional competitions, in national competitions, or in international competitions both pre- and postoperatively. 22
Discussion
Although a majority of the studies included in our analysis defined RTS as competing in a game or competitive play after surgery, significant variability exists among the definitions in the literature. Future studies should seek to standardize the definition and use more specific terminology to better describe the recovery and rehabilitation of the athlete. While we are not aware of any other studies that have analyzed the definitions of RTS used in the literature, the inconsistency of RTS definitions has been discussed in several studies and editorial commentaries, some with concern about patient satisfaction and safety as a result of the ill-defined parameter. 5,25,33
Of the 25 studies 2,4,6-20,23,26,28 -32,35 which used standard RTS or RTP terminology, 20 studies 2,4,7-10,12-20,28 -31,35 (69.0% overall) defined RTS as an athlete competing in a game or other competitive play, while 3 studies 6,11,26 (10.3% overall) defined RTS as the athlete competing in a game or other competitive play but with an explicitly stated competition-level modifier of the athlete returning to one’s preinjury level of competition. Philippon et al 23 and Werner et al 32 alternatively defined RTS as the athlete returning to practice or training. The difference between returning to training versus competition is important to consider, and unfortunately, current definitions of RTS do not allow for this distinction.
Although many of the included studies discussed professional athletes, studies that discuss athletes in high school sports or amateur sports may give way to even greater variability if RTS is not defined explicitly. As mentioned, Bauer et al 3 defined “return to competitive play” in high school athletes as return to the same sport that was played preinjury within 1 year of surgery and indicated the sport had to be organized (ie, collegiate, interscholastic, “travel” or club teams, organized intramural sports, or tournaments). Although Bauer et al offered a very strict definition of RTS relative to similar articles, the general requirement for the sport to be organized is an important consideration. Absent this criterion, an athlete may be determined to have returned to sport even if that athlete returns to noncompetitive and nonorganized sports in which the degree of intensity may be significantly decreased from the athlete’s preinjury level of competition. That said, it is equally important to analyze RTS for recreational athletes in noncompetitive and nonorganized sports such as golf, skiing, and running. For reasons of health maintenance, socialization, and personal enjoyment, a patient may wish to return to his or her preinjury noncompetitive and nonorganized sport. Therefore, it is important for physicians to be able to share relevant data with these patients.
Finally, RTS in adolescent and high school sports may be biased because an athlete’s age, graduation from high school/college, or both may lead to his or her cessation from playing sports. For example, while a professional athlete’s RTP or retirement can be tracked, the same is not necessarily possible for a high school athlete who may not continue to play his or her sport after graduation.
In their study of professional basketball players, Begly et al 4 defined RTP as competing in a game of “equal level” after surgery. This is in contrast to Frangiamore et al, 9 who defined RTP in Major League Baseball players as playing in a preseason or regular season major or minor league game after surgery. However, this would not qualify as competing in a game of “equal level.” These 2 definitions are further contrasted by Mai et al, 19 who defined RTP as successful return to the active roster for at least 1 regular season game after surgery. Being on the active roster, however, does not give any indication of the athlete’s level of competition or frequency of play.
As mentioned in the eligibility criteria for this study, articles that solely used medical or rehabilitation guidelines/criteria (eg, strength or range of motion testing, pain scale) to determine when an athlete was cleared to RTS were excluded, as these did not provide a clear definition of when an athlete actually returned to his or her sport. This is significant because it is possible for an athlete to meet established criteria for being physically able to RTS but not actually RTS, which may be related to the athlete’s psychological response to injury and recovery. 36
Developing a more standardized definition of RTS would benefit sports medicine physicians, coaches, athletic trainers, researchers, and patients. Analysis of RTS on a spectrum, such as that presented by Ardern et al 1 in a 2016 consensus statement, may be advantageous compared with a binary definition, given that an athlete’s recovery is a complex process involving multiple stages and benchmarks. 1 Whereas the definition of RTS varied in the studies included in this systematic review, all definitions were binary (ie, an athlete was determined to either have returned to sport/play or not). Although Philippon et al 23 and Werner et al 32 were unique in including return to training in their definitions of RTS, the definitions were still a yes or no question of whether the athlete had returned to sport/play. We endorse the use of a spectrum of RTS that more explicitly states the athlete’s recovery status, such as that presented by Ardern et al (summarized in Figure 2). As the consensus statement states, “A clear definition of RTS is important, and researchers should consider using the RTS continuum as a basis for their definition.” 1
Figure 2.
Return-to-sport continuum. Image adapted from Ardern et al 1 with permission from BMJ Publishing Group Limited.
It may be difficult to determine an athlete’s return to performance as it is stated in Figure 2 because that is largely a subjective and personal determination by the athlete, particularly for noncompetitive and nonorganized sports. In addition, in reporting levels of RTS in a study according to the RTS continuum in Figure 2, the percentage of athletes returning to sport will certainly be much higher than will the percentage of athletes returning to performance. However, the continuum offers more specificity and more uniformity. Those 2 objectives provide for greater clarity and reliability of the metric of RTS.
Limitations
There are several limitations to this study. First, a small group of authors wrote the majority of studies identified in the systematic review. We identify this as a limitation because one would assume that an author or institution would use the same definition across all of their studies, which could make the definitions in the literature appear very uniform even if every author or institution defined RTS differently. However, we identified at least 1 example of authors from the same institution using 2 different definitions in their respective studies. 4,9,20,23 Thus, while an author may wish to use the same definition across all of his or her studies, it may not even be standardized at the level of the individual institution. In addition, we found that in the 20 studies (69.0%) that defined RTS as an athlete competing in a game or other competitive play, the authors represented 7 unique institutions, indicating a level of convergence on a common definition.
Second, there was undoubtedly a wide variety of injuries and treatment modalities, as well as type and competition level of sports in the studies analyzed in this review. Accordingly, there may have been opportunities to create or agree on unique definitions of RTS for specific subsets of athletes. However, given the inherent challenges posed by a lack of consistency in defining RTS, it was the intention of this review to evaluate and analyze a broad definition of RTS as it is used across the sports medicine literature.
Third, as a systematic review, only abstracts could be searched for the defined terms, as opposed to evaluating the full texts. There may have been other studies that defined RTS in the full text of the paper but not in the abstract. The word “define” was included in our search terms to limit the findings to those studies that specifically define RTS. It is possible that a definition could be provided, perhaps parenthetically, without using the word “define.” That said, we identified several studies in our search results that provided the definition parenthetically without the use of the word “define.” These studies most likely appeared in the search results because the word “define” was present in other sentences in the abstract. Fourth, many studies that use RTS as an outcome measure never define those terms likely because it is not seen as needing a definition given its prominence in the literature and simplicity of terminology.
Conclusion
There is variability in the definition of RTS used in orthopaedic sports medicine literature. Most studies refer to the athlete competing in a game or other competitive play. Other variants include returning to practice/training and explicitly defined competition levels and objectives. Future studies should aim to standardize the definition of RTS to facilitate more precise assessment of outcome after sports medicine surgery. Using terminology that describes components of the recovery and rehabilitation process, such as “return to participation” and “return to performance,” in addition to RTS will allow us to more clearly understand the athlete’s recovery and associated level of competition or performance.
APPENDIX
Table A1.
Summary of Included Articles a
| Lead Author (Year) | Injury/Surgery | Sports/Athletes | LOE | Terminology Used and Definition |
|---|---|---|---|---|
| Jack (2017) 17 | Clavicle ORIF | Pro football | 3 | RTS, defined as playing in 1 NFL game after surgery |
| Jack (2018) 14 | Thumb UCL repair | Pro baseball | 3 | RTS, defined as playing in at least 1 MLB game after surgery |
| Jack (2018) 13 | Tommy John surgery | Pro baseball | 3 | RTS, defined as playing in at least 1 MLB game after UCL reconstruction |
| Jack (2019) 12 | Hip arthroscopy | Pro baseball | 3 | RTS, defined as playing in at least 1 MLB game after surgery |
| Jack (2019) 16 | Hip arthroscopy for FAI | Pro football, basketball, baseball, and hockey | 3 | RTS, defined as playing in at least 1 game after surgery |
| Jack (2020) 15 | Hip arthroscopy | Pro basketball | 3 | RTS, defined as playing in at least 1 game after surgery |
| Sochacki (2018) 29 | Forearm fracture ORIF | Pro football | 3 | RTS, defined as playing in a single NFL game after surgery |
| Sochacki (2019) 28 | Hip arthroscopy for FAI syndrome | Pro hockey | 3 | RTS, defined as playing in at least 1 NHL game after surgery |
| Sochacki (2019) 31 | Thumb UCL surgery | Pro football | 3 | RTS, defined as playing in at least 1 NFL game after thumb UCL surgery |
| Sochacki (2019) 30 | Achilles tendon repair | Pro soccer | 3 | RTS, defined as playing in any MLS game after surgery |
| Begly (2018) 4 | Hip arthroscopy | Pro basketball | 3 | RTP, defined as competing in a single professional game of equal level after surgery |
| Cinque (2017) 8 | ACL reconstruction | Pro football linemen | 3 | RTS, defined as an athlete playing in at least 1 NFL game after ACL reconstruction |
| Hsu (2015) 10 | Repair of acute superficial deltoid complex avulsion during ankle fracture fixation | Pro football | 4 | RTP, defined as the ability to successfully participate in at least 1 full regular season NFL game after surgery |
| Lareau (2016) 18 | Operative Jones fracture treatment | Pro football | 4 | RTP, defined as the ability to play in a single regular season NFL game after surgery |
| Mai (2017) 19 | ACL reconstruction | Pro football, basketball, hockey, and baseball | 3 | RTP, defined as a successful return to the active roster for at least 1 regular season game after ACL reconstruction |
| Menge (2017) 20 | Hip arthroscopy | Pro football | 4 | RTP, defined as competing in a preseason or regular season professional football game after surgery |
| Frangiamore (2018) 9 | Hip arthroscopy | Pro baseball | 4 | RTP, defined as playing in a preseason or regular season major or minor league game after arthroscopy |
| Aune (2014) 2 | Partial lateral meniscectomy | Pro football | 4 | RTP, defined as the first time a player played in a regular season NFL game after partial lateral meniscectomy; preseason game play was accepted as successful RTP, provided that the athlete played in a subsequent regular season game |
| Yang (2019) 35 | Primary Achilles tendon tear | Pro football | 3 | RTP, defined as playing in a regular season or postseason game after injury |
| Christian (2019) 7 | Hip arthroscopy | Pro football, baseball, basketball, and hockey | 3 | RTP date, defined as the date of the first regular or postseason game played in the respective professional league after each arthroscopic hip procedure |
| Rosinsky (2019) 26 | Bilateral hip arthroscopy | High school, collegiate, and pro athletes across many sports | 4 | RTS, defined as a patient’s return to competitive participation in his or her sport at the same level as or higher than that of presurgery, regardless of time elapsed after surgery |
| Burleson (2018) 6 | Hook of hamate excision | High school, collegiate, and pro baseball | 4 | RTP, defined as reaching the athlete’s preinjury level and being able to perform full sports activities |
| Ishoi (2018) 11 | Hip arthroscopy for FAI | 18- to 30-y-old athletes across many sports | 3 | RTS, defined as the proportion of athletes who were engaged in their preinjury sport at preinjury level at follow-up |
| Philippon (2010) 23 | Arthroscopic labral repair and treatment of FAI | Pro hockey | 4 | RTS, defined as the player’s resuming skating for training or participation in the sport of ice hockey |
| Werner (2014) 32 | Thumb ulnar collateral suture anchor repair | Collegiate football | 4 | RTP, defined as when both the senior author and athletic trainer released the patient to return to game play (when in season) or practice (when out of season) |
| Bauer (2019) 3 | ACL reconstruction | High school athletes across many sports | 3 | Return to competitive play, defined as return to the same sport that was played preinjury within 1 y of surgery, and the sport had to be organized (ie, collegiate, interscholastic, “travel” or club teams, organized intramural sports, or tournaments) |
| Smyth (2013) 27 | Hindfoot arthroscopy | No specific sport or age group | 4 | Return to sporting activities, “calculated as the time period from the date of surgery until the patient was able to participate at one’s previous level of activity” |
| Miyamoto (2015) 21 | Ligament reconstruction using single bone tunnel technique for chronic symptomatic subtle injury of the Lisfranc joint | Rugby, football, and judo | 4 | Return to athletic activity, defined as return to near preinjury performance level |
| Peduzzi (2019) 22 | Arthroscopic treatment of internal impingement of the shoulder | Overhead athletes including handball, tennis, volleyball, and swimming | 4 | RTS +, defined as returning to the previous sport at the same or a higher level, or RTS –, defined as a return to the previous sport at a lower level, a switch to another sport, or an inability to engage in any sport |
a ACL, anterior cruciate ligament; FAI, femoroacetabular impingement; LOE, level of evidence; MLB, Major League Baseball; MLS, Major League Soccer; NFL, National Football League; NHL, National Hockey League; ORIF, open reduction and internal fixation; pro, professional; RTP, return to play; RTS, return to sport; UCL, ulnar collateral ligament.
Footnotes
Final revision submitted November 29, 2020; accepted January 5, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: B.G.V. has received consulting fees from DePuy, research support from Stryker, education payments from Titan Surgical Group, and hospitality payments from Smith & Nephew. M.K.M. has received speaking fees from Arthrex; education payments from Arthrex, Alon Medical Technology, and Quest Medical; and hospitality payments from Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ardern CL, Glasgow P, Schneiders A, et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50(14):853–864. [DOI] [PubMed] [Google Scholar]
- 2. Aune KT, Andrews JR, Dugas JR, Cain EL, Jr. Return to play after partial lateral meniscectomy in National Football League athletes. Am J Sports Med. 2014;42(8):1865–1872. [DOI] [PubMed] [Google Scholar]
- 3. Bauer M, Feeley BT, Gallo RA. Effect of academic grade level on return to athletic competition after anterior cruciate ligament reconstruction. J Pediatr Orthop. 2019;39(4):198–201. [DOI] [PubMed] [Google Scholar]
- 4. Begly JP, Buckley PS, Utsunomiya H, Briggs KK, Philippon MJ. Femoroacetabular impingement in professional basketball players: return to play, career length, and performance after hip arthroscopy. Am J Sports Med. 2018;46(13):3090–3096. [DOI] [PubMed] [Google Scholar]
- 5. Bizzini M, Silvers HJ. Return to competitive football after major knee surgery: more questions than answers? J Sports Sci. 2014;32(13):1209–1216. [DOI] [PubMed] [Google Scholar]
- 6. Burleson A, Shin S. Return to play after hook of hamate excision in baseball players. Orthop J Sports Med. 2018;6(10):2325967118803090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Christian RA, Lubbe RJ, Chun DS, Selley RS, Terry MA, Hsu WK. Prognosis following hip arthroscopy varies in professional athletes based on sport. Arthroscopy. 2019;35(3):837–842.e831. [DOI] [PubMed] [Google Scholar]
- 8. Cinque ME, Hannon CP, Bohl DD, et al. Return to sport and performance after anterior cruciate ligament reconstruction in National Football League linemen. Orthop J Sports Med. 2017;5(6):2325967117711681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Frangiamore SJ, Mannava S, Briggs KK, McNamara S, Philippon MJ. Career length and performance among professional baseball players returning to play after hip arthroscopy. Am J Sports Med. 2018;46(11):2588–2593. [DOI] [PubMed] [Google Scholar]
- 10. Hsu AR, Lareau CR, Anderson RB. Repair of acute superficial deltoid complex avulsion during ankle fracture fixation in National Football League players. Foot Ankle Int. 2015;36(11):1272–1278. [DOI] [PubMed] [Google Scholar]
- 11. Ishoi L, Thorborg K, Kraemer O, Holmich P. Return to sport and performance after hip arthroscopy for femoroacetabular impingement in 18- to 30-year-old athletes: a cross-sectional cohort study of 189 athletes. Am J Sports Med. 2018;46(11):2578–2587. [DOI] [PubMed] [Google Scholar]
- 12. Jack RA, Sochacki KR, Hirase T, et al. Performance and return to sport after hip arthroscopic surgery in Major League Baseball players. Orthop J Sports Med. 2019;7(2):2325967119825835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jack RA, II, Burn MB, Sochacki KR, McCulloch PC, Lintner DM, Harris JD. Performance and return to sport after Tommy John surgery among Major League Baseball position players. Am J Sports Med. 2018;46(7):1720–1726. [DOI] [PubMed] [Google Scholar]
- 14. Jack RA II, Sochacki KR, Gagliano B, Lintner DM, Harris JD, McCulloch PC. Performance and return to sport after thumb ulnar collateral ligament repair in Major League Baseball players. Orthop J Sports Med. 2018;6(1):2325967117747268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jack RA II, Sochacki KR, Hirase T, et al. Performance and return to sport after hip arthroscopy in the National Basketball Association. Arthroscopy. 2020;36(2):473–478. [DOI] [PubMed] [Google Scholar]
- 16. Jack RA II, Sochacki KR, Hirase T, Vickery JW, Harris JD. Performance and return to sport after hip arthroscopy for femoroacetabular impingement in professional athletes differs between sports. Arthroscopy. 2019;35(5):1422–1428. [DOI] [PubMed] [Google Scholar]
- 17. Jack RA II, Sochacki KR, Navarro SM, McCulloch PC, Lintner DM, Harris JD. Performance and return to sport after clavicle open reduction and internal fixation in National Football League players. Orthop J Sports Med. 2017;5(8):2325967117720677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lareau CR, Hsu AR, Anderson RB. Return to play in National Football League players after operative Jones fracture treatment. Foot Ankle Int. 2016;37(1):8–16. [DOI] [PubMed] [Google Scholar]
- 19. Mai HT, Chun DS, Schneider AD, et al. Performance-based outcomes after anterior cruciate ligament reconstruction in professional athletes differ between sports. Am J Sports Med. 2017;45(10):2226–2232. [DOI] [PubMed] [Google Scholar]
- 20. Menge TJ, Bhatia S, McNamara SC, Briggs KK, Philippon MJ. Femoroacetabular impingement in professional football players: return to play and predictors of career length after hip arthroscopy. Am J Sports Med. 2017;45(8):1740–1744. [DOI] [PubMed] [Google Scholar]
- 21. Miyamoto W, Takao M, Innami K, Miki S, Matsushita T. Ligament reconstruction with single bone tunnel technique for chronic symptomatic subtle injury of the Lisfranc joint in athletes. Arch Orthop Trauma Surg. 2015;135(8):1063–1070. [DOI] [PubMed] [Google Scholar]
- 22. Peduzzi L, Grimberg J, Chelli M, et al. Internal impingement of the shoulder in overhead athletes: retrospective multicentre study in 135 arthroscopically-treated patients. Orthop Traumatol Surg Res. 2019;105(8)(suppl):S201–S206. [DOI] [PubMed] [Google Scholar]
- 23. Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99–104. [DOI] [PubMed] [Google Scholar]
- 24. Reiman MP, Peters S, Sylvain J, Hagymasi S, Mather RC, Goode AP. Femoroacetabular impingement surgery allows 74% of athletes to return to the same competitive level of sports participation but their level of performance remains unreported: a systematic review with meta-analysis. Br J Sports Med. 2018;52(15):972–981. [DOI] [PubMed] [Google Scholar]
- 25. Robinson J, Casartelli NC, Leunig M. Editorial commentary: return to sport. An ill-defined parameter. Arthroscopy. 2020;36(2):450–452. [DOI] [PubMed] [Google Scholar]
- 26. Rosinsky PJ, Kyin C, Lall AC, Shapira J, Maldonado DR, Domb BG. Rate of return to sport and functional outcomes after bilateral hip arthroscopy in high-level athletes. Am J Sports Med. 2019;47(14):3444–3454. [DOI] [PubMed] [Google Scholar]
- 27. Smyth NA, Murawski CD, Levine DS, Kennedy JG. Hindfoot arthroscopic surgery for posterior ankle impingement: a systematic surgical approach and case series. Am J Sports Med. 2013;41(8):1869–1876. [DOI] [PubMed] [Google Scholar]
- 28. Sochacki KR, Jack RA, Hirase T, Vickery J, Harris JD. Performance and return to sport after hip arthroscopy for femoracetabular impingement syndrome in National Hockey League players. J Hip Preserv Surg 2019;6(3):234–240. [Google Scholar]
- 29. Sochacki KR, Jack RA II, Hirase T, et al. Performance and return to sport after forearm fracture open reduction and internal fixation in National Football League players. Hand (N Y). 2018;13(6):682–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sochacki KR, Jack RA II, Hirase T, et al. There is a high return to sport rate but with reduced career lengths after Achilles tendon repair in Major League Soccer players. J ISAKOS. 2019;4(1):15–20. [Google Scholar]
- 31. Sochacki KR, Jack RA II, Nauert R, et al. Performance and return to sport after thumb ulnar collateral ligament surgery in National Football League players. Hand (N Y). 2019;14(4):487–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Werner BC, Hadeed MM, Lyons ML, Gluck JS, Diduch DR, Chhabra AB. Return to football and long-term clinical outcomes after thumb ulnar collateral ligament suture anchor repair in collegiate athletes. J Hand Surg Am. 2014;39(10):1992–1998. [DOI] [PubMed] [Google Scholar]
- 33. Williams RJ III. Editorial commentary: reviewing the science of our unscientific criteria for return to sports after shoulder stabilization. Arthroscopy. 2018;34(3):914–916. [DOI] [PubMed] [Google Scholar]
- 34. Wörner T, Thorborg K, Stalman A, Webster KE, Momatz Olsson H, Eek F. High or low return to sport rates following hip arthroscopy is a matter of definition? Br J Sports Med. 2018;52(22):1475–1476. [DOI] [PubMed] [Google Scholar]
- 35. Yang J, Hodax JD, Machan JT, et al. Factors affecting return to play after primary Achilles tendon tear: a cohort of NFL players. Orthop J Sports Med. 2019;7(3):2325967119830139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zarzycki R, Failla M, Arundale AJH, Capin JJ, Snyder-Mackler L. Athletes with a positive psychological response to return to sport training have better outcomes one and two years after ACL reconstruction. Orthop J Sports Med. 2017;5(7)(suppl 6):2325967117S00324. [Google Scholar]