Abstract
Background:
Previous studies have attempted to determine whether certain risk factors can predict the occurrence of inversion ankle sprains in male collegiate soccer players. However, no consensus has been reached on the predictive risk factors of inversion ankle sprain in this population.
Purpose:
To identify risk factors for inversion ankle sprains among male collegiate soccer players.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Included were 145 male collegiate soccer players in Japan who were assessed during a preseason medical checkup for potential risk factors of inversion ankle sprain. The preseason assessment included anthropometric measurements, joint laxity and flexibility, muscle flexibility, muscle strength, and balance ability, with a total of 33 variables. The participants were monitored during the 2019 season for inversion ankle sprains as diagnosed by physicians.
Results:
A total of 31 inversion ankle sprains in 31 players (21.4%) occurred during the season. Only the measured isometric hip abductor strength was significantly lower in injured players as compared with uninjured players. Logistic regression analysis revealed measured hip abductor muscle strength deficit as a significant risk factor for inversion ankle sprain (odds ratio, 0.978 [95% CI, 0.976-0.999]; P = .05).
Conclusion:
Hip abductor strength deficit was a risk factor for inversion ankle sprain in the study population. This finding could be useful for the prevention of inversion ankle sprains in male collegiate soccer players.
Keywords: inversion ankle sprain, hip abductor, risk factor, collegiate soccer player, injury prevention
Ankle sprains are among the most common musculoskeletal injuries observed in competitive athletes, and inversion (or lateral) ankle sprains are observed most frequently. 9,18 Soccer is the most popular sport in the world and is characterized by rapid speed changes, pivoting, jumping, kicking, and cutting movements; therefore, ankle sprains represent one of the most common injuries in this sport. 6,32,42 In addition, men aged 15 to 24 years have substantially higher ankle sprain rates than women. 41 Surprisingly, ankle sprains accounted for approximately 30% to 40% of all injuries in young male soccer players. 22 Additionally, long-term symptoms occur in up to 79% of players, and some players become frustrated with chronic ankle instability. 1 Approximately 70% to 85% of ankle sprains are inversion-type (lateral-type) sprains. 46 Therefore, from an injury-prevention standpoint, inversion ankle sprains in young male soccer players are of particular interest. To prevent inversion ankle sprains, we should recognize the risk factors in young male soccer players.
Several risk factors have been proposed to predict the occurrence of ankle injury. Previous injury history, especially with poor rehabilitation, 1,8,10,15,21,30 has been proposed as the greatest contributor to future ankle injury. Extrinsic risk factors, such as exposure hours, 34 weather, and competition level, 33 have also been investigated as potential contributors. However, potential intrinsic risk factors, including age, 2 lower limb range of motion, 13 balance, 44 body mass index, 29 and muscular strength, 4 are more clinically relevant, as they represent possible opportunities for intervention. Beynnon et al, 6 though, found little consensus in the literature with regard to whether such variables are always risk factors for ankle sprains. Additionally, previous studies on intrinsic risk factors of ankle sprain focused on deficits in muscle strength and flexibility and injury history independently and derived the risk factor from few possible factors. The most relevant risk factor for ankle sprain remains controversial, indicating the need for a prospective cohort study of multiple possible risk factors in the lower leg.
The aim of this study was to clarify risk factors of ankle inversion sprain prospectively in a relatively large, young male soccer population.
Methods
A prospective cohort study was conducted on collegiate male soccer players in the 2019 season, with data on potential risk factors collected during a preseason medical assessment and participants monitored for injury during the season. This study was a part of a sports injury prevention project titled The Prospective Study of Predictors of Sports Injuries: UTokyo Sports Science Initiative. Players’ injury registration continued from the start of the study until the competition of the season. Medical assessment was performed before the start of the season for each player. This study was approved by the ethics committee of our institution, and consent was obtained from all participants.
A total of 145 male collegiate soccer players from 2 regional first-division collegiate soccer teams in Japan were enrolled in this study. None of the players were injured at the start of the study, and none reported any lower limb musculoskeletal injury in the prior 3 months. All participants received a preseason medical checkup and completed a questionnaire to identify their age, years of soccer experience, injury history, and medication. In this study, preseason data from 5 physical screening tests were used: anthropometric measurements, joint laxity and flexibility tests, muscle flexibility test, muscle strength test, and balance test.
Anthropometric Measurements
Each player's body weight (BW) and height were measured at the preseason medical checkup, and body mass index was calculated for each player. Each body-composition parameter was measured using the InBody 270 (Biospace), which is a multifrequency impedance analyzer that can record each player’s lean soft tissue mass (skeletal muscle mass), body fat mass, and percentage body fat. Additionally, as a flat-foot index, the height of the navicular tubercle in each player’s foot was measured.
Joint Laxity and Flexibility
General Joint Laxity Testing
Each player underwent general joint laxity testing using the methods of the University of Tokyo as described by Watanabe et al. 41 The test consisted of 7 conditions: thumb-to-forearm position, elbow hyperextension ≥15°, shoulder hyperrotation, hip hyper–external rotation ≥90° in the standing position, knee hyperextension ≥10°, ankle hyperdorsiflexion ≥45° of knee flexion, and trunk flexion with both palms touching the floor and knees fully extended. Shoulder hyperrotation was considered positive when participants could clasp their hands from the cranial and caudal sections of their back, and hip hyper–external rotation was considered positive when participants could maintain their hips at 90° of external rotation with both their lower legs in a neutral position. All tests except for trunk flexion and hip external rotation were performed bilaterally. A point value of 0.5 was given each time that a player surpassed the designated laxity measure at each side of the 5 joints tested (wrists, elbows, shoulders, knees, and ankles), and 1 point each was given for the trunk and hip, for a maximum possible score of 7.
Joint Flexibility
Joint-flexibility tests were performed for internal rotation of hip, ankle dorsiflexion, and knee extension based on previous studies. 2,3 For internal rotation of hip, passive hip internal rotation angle in the prone position was measured. For ankle dorsiflexion, the weightbearing angle with knee flexion was measured. For knee extension, the knee hyperextension angle was measured in a standing position with involvement of the quadriceps.
Muscle Flexibility
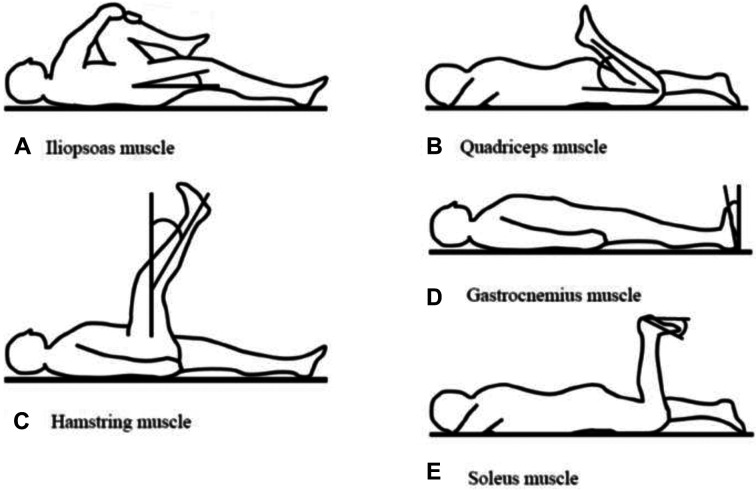
Muscle flexibility tests were performed bilaterally on the iliopsoas, quadriceps femoris, hamstrings, gastrocnemius, and soleus muscles (Figure 1). 38 Flexibility of all muscles were measured by a skilled sports physician (Y.M.). Excellent intrarater reliability has been reported on all muscle flexibility measures (intraclass correlation coefficient, 0.89-0.96). 41
Figure 1.
Muscle-flexibility tests performed bilaterally. (A) Iliopsoas muscle flexibility was measured by obtaining the angle of the hip joint when the participant passively bent the opposite hip joint to the maximum in a supine position. (B) For the quadriceps, the participant grasped the lower leg just proximal to the ankle in a prone position and pulled it toward the buttocks. The bending angle of the knee joint represented quadriceps muscle flexibility. The physician tried not to lift the participant’s buttocks by muscle tension during the measurement. (C) Hamstring muscle flexibility was measured with the hip at 90° of flexion in a supine position. The angle between the vertical line to the floor and the long axis of the tibia after the knee joint was maximally extended. (D) To measure gastrocnemius muscle flexibility, the ankle joint passive dorsiflexion angle was measured with maximal dorsiflexion in the supine position and the knee extended and maintained in a neutral position relative to the varus-valgus angle of the ankle. (E) To measure soleus muscle flexibility, the ankle joint passive dorsiflexion angle was measured during maximal dorsiflexion in the prone position with the knee at 90° of flexion.
Muscle Strength Tests
Isometric Knee Extension and Flexion
Cybex Humac Norm (CSMi) was used for the measurement of knee flexion and extension muscle isometric strength. Before the measurement, the participant performed a 5-minute warm-up routine consisting of cycling on a stationary exercise bicycle. The order of which side was measured first was randomized, and each player was positioned on the dynamometer so that the hip was flexed to 90°, ensuring that the dynamometer and knee joint axes were aligned. Testing consisted of isometric contraction at knee flexion and extension at 70°, and the highest peak torque value was recorded. Strength measures were recorded as measured and normalized to BW.
Isometric Hip Abduction
The strength of the hip abductors was measured isometrically using a handheld dynamometer (μTAS F-1; Anima Industry). To allow for a standardized testing procedure, all participants lay supine with the hips in a neutral position beside the wall, both knees extended, and arms crossed over the chest. As the participants were instructed to abduct the leg as much as possible over 5 seconds, with 1 minute of rest between contractions, the peak force was retained for further analysis. The dynamometer was placed on the lateral epicondyle of the femur, and the distance between the lateral epicondyle and hip center was measured (Figure 2). Previous isometric hip abductor strength assessed with a handheld dynamometer has had good to excellent intra- and intertester reliability. 27,37 The highest peak torque value was recorded. Strength measures were recorded as measured and normalized to BW.
Figure 2.

Strength measurement during isometric hip abduction using a portable handheld dynamometer.
Balance Tests
We measured double- and single-leg stance balance with a 1-m Footscan pressure plate with 8192 resistive sensors and a pixel resolution of 5.08 × 7.62 mm (RSscan International), with a sampling frequency of 250 Hz. The procedures used were based on methods previously described. 19 The participant performed a 30-second trial of double-leg standing balance barefooted with arms crossed over the chest and eyes opened. After a 30-second interval, each participant then performed a 30-second trial of single-leg standing balance of each leg, similar to the double-leg test. The total distance of the center of pressure during the 30 seconds in both tests was measured as the balance parameter. 26
Diagnosis of Inversion Ankle Sprain
Inversion ankle sprains were diagnosed and monitored by the team’s medical staff under the supervision of an orthopaedic team physician or directly by the team physician (K.Kawaguchi). For every injury, the date, type (eg, sprain), diagnosis (eg, inversion ankle sprain), and site (eg, left ankle) were documented, including the time of return to play and playing time lost. An injury was defined as a physical complaint that required restricted activity for at least 1 day and was considered only when it occurred during soccer practice or a game. 23 Injury data were collected every 2 months from the medical staff in both teams.
Statistical Analysis
All statistical analyses were performed using SPSS Version 22.0 (IBM). Parameters except for those of the lower limb were compared between injured and uninjured players. Lower limb parameters were compared between the injured and uninjured contralateral limbs among the injured players as well as between the injured limb of injured players and the uninjured limbs of the uninjured players; each uninjured side was considered separately. The unpaired 2-tailed Student t test, Mann-Whitney U test, and Fisher exact test were used to assess continuous variables, nonparametric variables, and ordered variables, respectively. Of these examined factors, those showing a significant difference (P < .05) were further analyzed using multivariate logistic regression models to determine which could predict inversion ankle sprain. Two-tailed P values <.05 were deemed statistically significant.
Results
Inversion ankle sprain occurred in a total of 31 ankles of 31 players (21.4%). No participants were lost to follow-up during the injury-registration period. Table 1 shows the characteristics of the players in the injured and uninjured groups, and Table 2 shows the comparison of injured and uninjured players in terms of anthropometric measurements, joint laxity tests, and balance test with double-leg stance. There were no statistically significant differences between the groups on any of the variables.
TABLE 1.
Player Characteristics for the Injured and Uninjured Study Groups a
| Injured Players (n = 31) | Uninjured Players (n = 114) | P Value | |
|---|---|---|---|
| Age, y | 19.9 ± 1.0 | 19.8 ± 1.2 | .36 |
| Playing experience, y | 13.4 ± 2.4 | 13.5 ± 2.4 | .85 |
| Previous history of ankle sprain | 15 (48.4) | 40 (35.1) | .21 |
| Weight, kg | 66.3 ± 6.2 | 67.6 ± 6.4 | .54 |
| Height, cm | 173.0 ± 5.0 | 173.7 ± 6.2 | .60 |
| Body mass index, kg/m2 | 22.1 ± 1.7 | 22.4 ± 1.4 | .77 |
a Data are presented as mean ± SD or No. (%) of players.
TABLE 2.
Anthropomorphic, Joint Laxity, and Double-Leg Balance Measurements Between the Injured and Uninjured Groups a
| Injured Players (n = 31) | Uninjured Players (n = 114) | P Value | |
|---|---|---|---|
| Anthropometric measurement | |||
| Body muscle mass, kg (lean soft tissue mass) | 54.0 ± 5.0 | 54.9 ± 5.4 | .67 |
| Body fat mass, kg | 8.9 ± 2.3 | 9.1 ± 2.2 | .74 |
| Percentage body fat, % | 13.4 ± 3.0 | 13.5 ± 2.9 | .83 |
| General joint laxity test score (out of 7) | 1.5 (0-4.0) | 1.0 (0-5.0) | .49 |
| Balance test for double-leg stance, center of pressure, mm | 42.0 ± 27.1 | 41.6 ± 20.9 | .53 |
a Data are presented as mean ± SD or median (range).
Table 3 shows the comparison between the injured and contralateral uninjured limbs of the injured players. No significant differences were noted between the groups. Also shown are results of the lower limb parameters between the injured limbs of the injured players and the limbs of uninjured players. Only the measured value of hip abductor strength was significantly different between these groups (P = .03).
TABLE 3.
Lower Limb Parameters in the Injured Limb vs the Uninjured Limb of Injured and Uninjured Players a
| Injured Players | Uninjured Players | ||||
|---|---|---|---|---|---|
| Injured Limb (n = 31) | Uninjured Limb (n = 31) | P Value | Uninjured Limb (n = 228) | P Value | |
| Anthropometric measurement | |||||
| Height of navicular tubercle, cm | 4.9 ± 0.6 | 5.0 ± 0.6 | .41 | 4.8 ± 0.7 | .30 |
| Joint range of motion, deg | |||||
| Knee extension angle | 3.8 ± 5.2 | 3.2 ± 5.0 | .62 | 2.8 ± 4.5 | .25 |
| Ankle dorsal flex angle | 40.4 ± 7.1 | 40.4 ± 5.7 | .85 | 39.6 ± 6.3 | .50 |
| Hip internal rotation angle | 36.4 ± 6.6 | 36.1 ± 5.7 | .85 | 35.4 ± 8.5 | .54 |
| Muscle flexibility tests results | |||||
| Iliopsoas | 5.9 ± 4.0 | 5.7 ± 3.4 | .78 | 5.2 ± 2.9 | .26 |
| Quadriceps | 26.7 ± 6.7 | 28.0 ± 7.1 | .46 | 25.8 ± 4.8 | .39 |
| Hamstring | 20.1 ± 9.1 | 19.6 ± 8.4 | .85 | 17.7 ± 8.3 | .40 |
| Gastrocnemius | 13.0 ± 3.9 | 12.4 ± 4.7 | .62 | 12.5 ± 4.2 | .58 |
| Soleus | 22.2 ± 5.3 | 21.1 ± 5.9 | .55 | 21.4 ± 5.6 | .47 |
| Muscle strength tests | |||||
| Knee extension | |||||
| Isometric, N·m | 222.7 ± 36.5 | 223.6 ± 50.9 | .92 | 237.7 ± 52.3 | .12 |
| Normalized isometric, N·m/kg | 3.3 ± 0.4 | 3.3 ± 0.5 | .84 | 3.5 ± 0.7 | .22 |
| Knee flexion | |||||
| Isometric, N·m | 114.9 ± 22.9 | 115.4 ± 24.9 | .96 | 115.3 ± 24.5 | .92 |
| Normalized isometric, N·m/kg | 1.7 ± 0.3 | 1.7 ± 0.3 | .97 | 1.7 ± 0.3 | .71 |
| Hip abduction | |||||
| Isometric, N·m | 153.2 ± 32.2 | 158.8 ± 37.3 | .62 | 167.4 ± 34.0 | .03 |
| Normalized isometric, N·m/kg | 2.3 ± 0.5 | 2.4 ± 0.5 | .63 | 2.5 ± 0.4 | .05 |
| Balance test | |||||
| Center of pressure in single-leg balance, mm | 461.6 ± 93.9 | 479.4 ± 148.9 | .58 | 463.3 ± 144.8 | .93 |
a Data are presented as mean ± SD. Bold P value indicates a statistically significant difference vs the injured limb (P < .05).
Table 4 presents the results of the multivariable logistic regression analysis for inversion ankle sprain between the injured limbs of injured players and the uninjured limbs of uninjured players. Results indicated that inversion ankle sprain was significantly associated with hip abductor strength (measured value; odds ratio, 0.978 [95% CI, 0.976-0.999]; P = .05). In other words, the odds of a male collegiate soccer player sustaining an inversion ankle sprain were increased by approximately 2% for each 1-N·m decrease in hip abductor strength.
TABLE 4.
Results of the Multivariable Regression Analysis a
| Regression Coefficient | SE | Odds Ratio (95% CI) | P Value | |
|---|---|---|---|---|
| Age | 0.045 | 0.159 | 1.046 (0.775-1.429) | .777 |
| Body mass index | –0.036 | 0.141 | 0.967 (0.733-1.275) | .812 |
| Isometric hip abduction | –0.012 | 0.001 | 0.978 (0.976-0.999) | .047 |
a Bold P value indicates statistical significance (P < .05).
Discussion
The most important finding in this study was that the hip abductor muscle strength deficit (measured value) was the significant risk factor of inversion ankle sprains in male collegiate soccer players.
Regarding abductor muscle strength, Powers et al 35 reported that reduced isometric hip abductor muscle strength was a predictor of ankle sprain in 185 male soccer players including adolescents and adults, and their conclusion was consistent with our result. However, they did not consider many possible risk factors, such as knee muscle strength, balance, and range of motion; as such, their results represent only a small aspect of a complex interaction among anthropometric measurements, muscle strength, balance, anatomic morphology, and other factors. In contrast, our results were derived from many possible risk factors, including a complex interaction, and we revealed that reduced abductor muscle strength was the most important risk factor of inversion ankle sprain for young collegiate soccer players. In our study, post hoc analysis showed that our power was 0.61, which we thought was moderate to support our result. However, our results contrasted with those of McHugh et al, 30 who reported that hip abduction strength had no influence on future lateral ankle sprain among 169 athletes. Their rate of ankle sprain in high school athletes was 5.9%, as calculated from in 1 season, and was relatively low. Therefore, it might be too low an injury rate to extract risk factors of ankle sprain, such as deficiency of abductor muscle strength.
Given that the deficiency of abductor muscle strength was the risk factor of ankle sprain, one possible mechanism could be related to the role of the hip abductors in maintaining pelvic and trunk stability during sports activities. Ford et al 11 reported that frontal pelvis obliquity was negatively correlated with hip abductor strength during running in collegiate cross-country runners. Additionally, hip abduction strength was shown to be correlated with pelvic drop and hip adduction moment during single-leg squat, 45 and Cerny 7 found that weakness in a stabilizing muscle, such as the gluteus medius, may produce deviations in joint motion and subsequent loss of stability. Hence, according to these previous studies, hip abductor strength deficit could lead to a more frontal pelvic and trunk tilt during soccer, which could then induce insufficient control of the center of gravity at a cutting or landing maneuver. With regard to the relationship between the center of gravity and ankle sprain, Wilkerson et al 43 stated that, during changes in balance, uncontrollable excessive lateral displacement of the center of gravity results in increased lateral sway, which causes the lateral border of the foot to act as a fulcrum, with subsequent inversion of the ankle. The shifting center of gravity could not be smoothly or sufficiently performed in a cutting or landing leg, and the leg could be unbalanced and likely injured. Therefore, inversion ankle sprain is likely to occur in soccer players with abductor strength deficit.
As another possible mechanism for abductor muscle strength deficit as the risk factor of ankle sprain, foot placement error could not be corrected because of it. 12 Inversion ankle sprains seem to be related to either unanticipated foot placement on a sloped surface or inappropriate positioning of the foot in space before contact with a surface. 36 MacKinnon and Winter 28 reported that errors in foot placement are corrected at the hip joint or subtalar joint, which work in synergy, and large errors in foot placement are corrected at the hip. Interactions between the supporting foot and hip musculature permit various strategies to be used to maintain balance; in particular, control of pelvic motion by the abductor strength is critical to maintaining total body balance. Additionally, these interactions could be the cause of functional ankle instability without mechanical ankle instability. Tropp et al 40 found that the ability to maintain postural stability was reduced with functional ankle instability but was not affected by mechanical ankle instability. Therefore, the hip abductor muscle strength deficit could negatively cause an unexpected foot placement situation in a soccer game, and it could be one of the causes of ankle functional instability.
Regarding previous speculation about ankle sprain and center of gravity, postural stability was considered related to an ankle sprain. Previous studies revealed a significant correlation between poor static postural control and inversion ankle sprain. 14,44 Additionally, Powers et al 35 demonstrated a relationship between ankle sprain and hip abductors in terms of postural stability. Persons with hip abductor strength deficit showed decreased medial-lateral postural stability, increased activation, and earlier onset of the ankle evertors in an effort to prevent excessive ankle inversion. 24,25 Thus, abductor hip muscle strength deficit could reduce postural stability. However, in this study, we could not find any difference between the ankle sprain limb and the uninjured limb in postural balance, which was based on the displacement of the center of pressure during the 30-second single-leg stance. This possibly occurs because this task was relatively easy for athletes and may not have been sufficiently discriminative in this population. Additionally, this task was popularly used to assess postural stability in nonathletes. 5 Therefore, it is necessary to evaluate postural stability in athletes under less stable conditions, such as a single stance blindfolded or single stance with a balance board. 16
Previous studies reported that a history of ankle sprain was one of the obvious risk factors of ankle inversion sprain, 8,10 because previous injury could alter the lower limb kinetic chain for long periods after symptom dissipation, thereby increasing future injury risk. 31 However, in the present study, 48.3% of injured limbs and 35.5% of uninjured limbs had a history of ankle sprain, but no significant difference was found. This may be due to a relatively young sample population that is yet to incur any significant injury, 8,21 or it could be attributed to the level of competition 8,17,39 or play conditions. 47 Although chronic ankle instability could be a risk factor, this study did not include mechanical or functional ankle instability evaluation after ankle sprain. Therefore, further investigation with a functional or mechanical evaluation is necessary.
This study has several limitations. First, it focused on inversion ankle sprains in male collegiate soccer players at a high competition level. Thus, our findings may not be applicable to other sports or female athletes. Moreover, the International Olympic Committee online meeting in 2019 suggested defining an injury as any condition that affects an athlete’s normal state of full health, regardless of its consequences on his or her sports participation or performance or whether the athlete sought medical attention; however, our study defines an injury as a physical complaint that requires restricted activity for at least 1 day. Therefore, our findings may not be applicable to minor ankle injuries without resting sports activity. Second, this study followed a relatively large cohort of collegiate soccer players; nevertheless, 200 injury cases might be needed to detect small to moderate associations in a prospective cohort study. 3 However, our prospective study of predictors for sports injuries including ankle sprains is ongoing; accordingly, we could reveal other weak to moderate risk factors of ankle sprain in the future with more players and injuries. Third, we collected the incidence of ankle sprain for 1 year, and further investigation might reveal risk factors other than abductor muscle strength. Fourth, we assessed only knee and hip muscle isometric strength, such as knee extension, knee flexion, and hip abductor muscle strength, and did not evaluate muscle strength around the ankle. Thus, regarding whether other muscle strength could be a risk factor, a meta-analysis showed that decreased slow eccentric ankle inversion strength and increased fast concentric plantar flexion strength significantly correlated with lateral ankle sprain. 20 We are now prospectively assessing toe-grasping strength as a new strength factor around the foot and can reveal the results in the near future. Additionally, Baumhauer et al 4 demonstrated that players with a muscle strength imbalance, as measured by an elevated eversion-to-inversion ratio, exhibited a higher incidence of inversion ankle sprains and that ankles with greater plantar flexion strength and a smaller dorsiflexion-to-plantar flexion ratio had a higher incidence of inversion ankle sprains. Therefore, abduction-to-adduction ratio could be worth investigating in future studies. Fifth, despite the dynamic balance needed for complex maneuvers in soccer, we evaluated only static isometric muscle strength and static balance. As such, dynamic muscle strength and dynamic balance ability are expected to be evaluated in future study. Additionally, functional and mechanical ankle instability was not included in this study and should be evaluated in future work. Sixth, we did not distinguish contact injury or noncontact injury. Finally, as this is an analysis of limited teams, the results may be influenced by the specific background of each team. It is thus not clear whether the results of this study are applicable to soccer players in general.
Conclusion
Hip abductor muscle strength deficit was an important risk factor for inversion ankle sprain in the study population. This finding could be useful for the prevention of inversion ankle sprain in male collegiate soccer players.
Acknowledgment
The authors gratefully acknowledge the cooperation of physicians, physical therapists, and athletic trainers as volunteer staff in our prospective study of predictors for sports injuries.
Footnotes
Final revision submitted January 6, 2021; accepted February 18, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by scholarships from the East Japan Railway Company and Shimamura-Syoukai and by grants from Nakatomi Foundation. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Tokyo.
References
- 1. Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(1, suppl):5–16. [DOI] [PubMed] [Google Scholar]
- 3. Bahr R, Holme I. Risk factors for sports injuries—a methodological approach. Br J Sports Med. 2003;37(5):384–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baumhauer JF, Alosa DM, Renström AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23(5):564–570. [DOI] [PubMed] [Google Scholar]
- 5. Bazett-Jones DM, Cobb SC, Joshi MN, Cashin SE, Earl JE. Normalizing hip muscle strength: establishing body-size-independent measurements. Arch Phys Med Rehabil. 2011;92(1):76–82. [DOI] [PubMed] [Google Scholar]
- 6. Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376–380. [PMC free article] [PubMed] [Google Scholar]
- 7. Cerny K. Pathomechanics of stance: clinical concepts for analysis. Phys Ther. 1984;64(12):1851–1859. [DOI] [PubMed] [Google Scholar]
- 8. Chomiak J, Junge A, Peterson L, Dvorak J. Severe injuries in football players: influencing factors. Am J Sports Med. 2000;28(5):S58–S68. [DOI] [PubMed] [Google Scholar]
- 9. Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. [DOI] [PubMed] [Google Scholar]
- 10. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for acute ankle injuries among male soccer players: a prospective cohort study. Scand J Med Sci Sports. 2010;20(3):403–410. [DOI] [PubMed] [Google Scholar]
- 11. Ford KR, Taylor-Haas JA, Genthe K, Hugentobler J. Relationship between hip strength and trunk motion in college cross-country runners. Med Sci Sports Exerc. 2013;45(6):1125–1130. [DOI] [PubMed] [Google Scholar]
- 12. Friel K, McLean N, Myers C, Caceres M. Ipsilateral hip abductor weakness after inversion ankle sprain. J Athl Train. 2006;41(1):74–78. [PMC free article] [PubMed] [Google Scholar]
- 13. Gabbe BJ, Finch CF, Wajswelner H, Bennell KL. Predictors of lower extremity injuries at the community level of Australian football. Clin J Sport Med. 2004;14(2):56–63. [DOI] [PubMed] [Google Scholar]
- 14. Grassi A, Alexiou K, Amendola A, et al. Postural stability deficit could predict ankle sprains: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):3140–3155. [DOI] [PubMed] [Google Scholar]
- 15. Hägglund M, Waldén M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Henry T, Evans K, Snodgrass SJ, Miller A, Callister R. Risk factors for noncontact ankle injuries in amateur male soccer players: a prospective cohort study. Clin J Sport Med. 2016;26(3):251–258. [DOI] [PubMed] [Google Scholar]
- 17. Hrysomallis C. Relationship between balance ability, training and sports injury risk. Sports Med. 2007;37(6):547–556. [DOI] [PubMed] [Google Scholar]
- 18. Kaminski TW, Hertel J, Amendola N, et al. National Athletic Trainers’ Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kilroy EA, Crabtree OM, Crosby B, Parker A, Barfield WR. The effect of single-leg stance on dancer and control group static balance. Int J Exerc Sci. 2016;9(2):110–120. [PMC free article] [PubMed] [Google Scholar]
- 20. Kobayashi T, Tanaka M, Shida M. Intrinsic risk factors of lateral ankle sprain: a systematic review and meta-analysis. Sports Health. 2016;8(2):190–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kofotolis ND, Kellis E, Vlachopoulos SP. Ankle sprain injuries and risk factors in amateur soccer players during a 2-year period. Am J Sports Med. 2007;35(3):458–466. [DOI] [PubMed] [Google Scholar]
- 22. Kucera KL, Marshall SW, Kirkendall DT, Marchak PM, Garrett WE, Jr. Injury history as a risk factor for incident injury in youth soccer. Br J Sports Med. 2005;39(7):462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Le Gall F, Carling C, Reilly T, Vandewalle H, Church J, Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. Am J Sports Med. 2006;34(6):928–938. [DOI] [PubMed] [Google Scholar]
- 24. Lee SP, Powers C. Fatigue of the hip abductors results in increased medial-lateral center of pressure excursion and altered peroneus longus activation during a unipedal landing task. Clin Biomech (Bristol, Avon). 2013;28(5):524–529. [DOI] [PubMed] [Google Scholar]
- 25. Lee SP, Powers CM. Individuals with diminished hip abductor muscle strength exhibit altered ankle biomechanics and neuromuscular activation during unipedal balance tasks. Gait Posture. 2014;39(3):933–938. [DOI] [PubMed] [Google Scholar]
- 26. Li Z, Liang YY, Wang L, Sheng J, Ma SJ. Reliability and validity of center of pressure measures for balance assessment in older adults. J Phys Ther Sci. 2016;28(4):1364–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lu YM, Lin JH, Hsiao SF, Liu MF, Chen SM, Lue YJ. The relative and absolute reliability of leg muscle strength testing by a handheld dynamometer. J Strength Cond Res. 2011;25(4):1065–1071. [DOI] [PubMed] [Google Scholar]
- 28. MacKinnon CD, Winter DA. Control of whole body balance in the frontal plane during human walking. J Biomech. 1993;26(6):633–644. [DOI] [PubMed] [Google Scholar]
- 29. McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10(4):239–244. [DOI] [PubMed] [Google Scholar]
- 30. McHugh MP, Tyler TF, Tetro DT, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006;34(3):464–470. [DOI] [PubMed] [Google Scholar]
- 31. Nadler SF, Malanga GA, Feinberg JH, Rubanni M, Moley P, Foye P. Functional performance deficits in athletes with previous lower extremity injury. Clin J Sport Med. 2002;12(2):73–78. [DOI] [PubMed] [Google Scholar]
- 32. Nielsen AB, Yde J. Epidemiology and traumatology of injuries in soccer. Am J Sports Med. 1989;17(6):803–807. [DOI] [PubMed] [Google Scholar]
- 33. Peterson L, Junge A, Chomiak J, Graf-Baumann T, Dvorak J. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28(5):S51–S57. [DOI] [PubMed] [Google Scholar]
- 34. Poulsen TD, Freund KG, Madsen F, Sandvej K. Injuries in high-skilled and low-skilled soccer: a prospective study. Br J Sports Med. 1991;25(3):151–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Powers CM, Ghoddosi N, Straub RK, Khayambashi K. Hip strength as a predictor of ankle sprains in male soccer players: a prospective study. J Athl Train. 2017;52(11):1048–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Robbins S, Waked E. Factors associated with ankle injuries: preventive measures. Sports Med. 1998;25(1):63–72. [DOI] [PubMed] [Google Scholar]
- 37. Scott DA, Bond EQ, Sisto SA, Nadler SF. The intra- and interrater reliability of hip muscle strength assessments using a handheld versus a portable dynamometer anchoring station. Arch Phys Med Rehabil. 2004;85(4):598–603. [DOI] [PubMed] [Google Scholar]
- 38. Tojima M, Noma K, Torii S. Changes in serum creatine kinase, leg muscle tightness, and delayed onset muscle soreness after a full marathon race. J Sports Med Phys Fitness. 2016;56(6):782–788. [PubMed] [Google Scholar]
- 39. Trojian TH, McKeag DB. Single leg balance test to identify risk of ankle sprains. Br J Sports Med. 2006;40(7):610–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16(1):64–66. [PubMed] [Google Scholar]
- 41. Watanabe H, Fujii M, Yoshimoto M, et al. Pathogenic factors associated with Osgood-Schlatter disease in adolescent male soccer players: a prospective cohort study. Orthop J Sports Med. 2018;6(8):2325967118792192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ, Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. [DOI] [PubMed] [Google Scholar]
- 43. Wilkerson GB, Pinerola JJ, Caturano RW. Invertor vs evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J Orthop Sports Phys Ther. 1997;26(2):78–86. [DOI] [PubMed] [Google Scholar]
- 44. Willems TM, Witvrouw E, Delbaere K, Mahieu N, Bourdeaudhuij ID, Dirk De Clercq DD. Intrinsic risk factors for inversion ankle sprains in male subjects: a prospective study. Am J Sports Med. 2005;33(3):415–423. [DOI] [PubMed] [Google Scholar]
- 45. Willson JD, Ireland ML, Davis I. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. 2006;38(5):945–952. [DOI] [PubMed] [Google Scholar]
- 46. Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician. 2001;63(1):93–104. [PubMed] [Google Scholar]
- 47. Yde J, Nielsen AB. Sports injuries in adolescents’ ball games: soccer, handball and basketball. Br J Sports Med. 1990;24(1):51–54. [DOI] [PMC free article] [PubMed] [Google Scholar]