Abstract
Health care services for children with Autism Spectrum Disorder (ASD) are often expensive and frequently not covered under private health insurance. The 2008 Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA) was viewed as a possible means of improving access by eliminating differences between behavioral health and medical/surgical benefits. We examined whether the MHPAEA was associated with increased use of and spending on mental health care and functional services for children with ASD compared to the period prior to implementation of the law. We used national health insurance commercial group claims data to examine trends in service use and spending among children with ASD before and after implementation. For children with ASD, MHPAEA implementation was associated with increased use of both mental health and non-mental health services. On a positive note, these increases in use were not associated with higher out-of-pocket spending, suggesting that the law improved financial protection for families.
INTRODUCTION
The Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008, also referred to in this paper as the (federal) parity law, went into effect in 2010. The legislation aimed at eliminating the long-standing differences in the generosity of private health insurance coverage for mental health and substance use disorder (MH/SUD) services relative to other medical care services. Before the law, insurance coverage for MH/SUD services often required higher cost sharing (e.g., coinsurance of 50 percent compared with 20 percent for outpatient medical services) and placed limits on special services (e.g., 20 outpatient visits and 30 inpatient days per year).1 The MHPAEA requires group commercial insurance policies offering MH/SUD benefits to ensure that all financial requirements (deductibles, copayments, and coinsurance) and treatment limits (number of inpatient days and outpatient visits) for MH/SUD benefits are at least as generous as those for medical/surgical benefits, and prohibits the use of special annual and lifetime dollar limits on MH/SUD services. It also requires, under the final regulations2, equivalence in so-called non-quantitative treatment limitations (NQTLs) such as prior authorization and other utilization management requirements, medical necessity determinations, and network adequacy standards.
A controversial provision of the law relates to which diagnoses it covers. The law does not require that specific conditions be covered; rather it specifies that services are covered for those MH/SUDs as defined “under the terms of a health plan”. It is left to the discretion of the insurer as to decide which diagnoses the parity law applies.3 An important unanswered question is whether the federal parity law was associated with changes in services provided under private insurance for children with Autism Spectrum Disorder (ASD).
ASD is a neurobehavioral syndrome that is defined by the presence of repetitive/stereotypic behaviors and disruption in the development of social and language abilities.4 Over the last several decades, prevalence estimates of ASD have risen precipitously. In the 1980s, ASD was believed to occur in 5 out of every 10,000 (.05%) children.5,6 Today, ASD is estimated to affect 1 in 68 youths (1.5%).5,6
Individuals with ASD require chronic management throughout their lifespan. Services include behavioral, speech-language, occupational, and physical therapies to treat a range of behavioral, language, sensory, and adaptive deficits intrinsic to the disorder.7 Health care costs for children with ASD can be substantial8–10 because of the substantial need for these services, and families of children with ASD consistently report challenges paying for services.11–13
Historically, commercial health insurance has excluded or provided minimal coverage for the treatment of ASD.14 In most cases, these treatments involve traditional outpatient mental health services (e.g., pharmacology, psychotherapy) since most children with ASD suffer from a co-occurring psychiatric disorder.15,16 Behavioral therapies specific to the treatment of ASD, such as applied behavioral analysis, are often also recommended to treat behavioral challenges. Behavioral health services to treat children with ASD may be delivered for as many as 40 hours per week (or more) for several years17. The intensity of services often recommended for behavioral therapies typically far exceeds the level that traditionally most policies covered17 for mental health services.
Advocates for children with ASD viewed the passage of the MHPAEA as an opportunity to expand access to mental health services to this population and to lower the out-of-pocket (OOP) financial burden on families. An increase in mental health services could also increase use of functional services (such as speech/language services and occupational or physical therapy (OT/PT)) and total health care spending due to increased contacts and referrals. However, the provision of the federal parity law that gives insurers discretion over which diagnoses are covered could also result in a minimal or no change in service use and spending for children with ASD. If the law leads some employers to drop coverage of ASD, a decrease in service use and spending could be observed. For example, a recent study found that litigation challenges to federal parity involved multiple cases where denials of services to treat ASD were at issue, suggesting controversy exists around application of the law to ASD.18
Only one prior study has examined the relationship between insurance parity and access to care or financial protection among children with ASD; that study focused on earlier state parity laws.19 Using data from the 2005–2006 wave of the National Survey of Children with Special Health Care Needs, Lucy Bilaver and Neil Jordan examined the effects of state mental health parity laws on family financial burden, satisfaction with health insurance, and receipt of mental health services for privately insured children and did not find state parity laws to be associated with improved outcomes.19 However, that study was based on retrospective report and may be subject to recall bias. That study also could not distinguish which children were enrolled in commercial health insurance through self-insured firms versus fully-insured firms. This is a critical limitation in estimating the effects of state parity laws since only individuals with commercial insurance through fully-insured firms in states with parity laws were actually subject to those laws due to the Employee Retirement Income Security Act (ERISA) of 1974. The ERISA law exempts self-insured firms, those contracting with health plans to administer employee health benefits only and not to manage their insurance risk pool, from state insurance regulations. About half of all commercially insured individuals are enrolled through self-insured firms that are exempt from state mandates.3,20
In this study, we used an interrupted time series research design to examine if federal parity was associated with changes in the probability of using mental health services, the intensity of services used, and spending on mental health services among children with ASD paid by private insurance. In addition, we assessed whether the law had secondary associations through changes in use of functional therapies including speech/language therapies and OT/PT services, and whether the law was associated with a change in total health care spending among children with ASD.
METHODS
Data and Sample.
We used the Truven Health MarketScan Database from 2007 to 2012. The MarketScan database includes health insurance claims and encounters for employees and their dependents from approximately 100 large employers and health plans in the US, covering approximately 15 to 22 million enrollees per year. These employers nearly all self-insure and thus are not subject to state insurance mandates. The data includes inpatient, outpatient, and pharmacy claims with information on diagnoses, procedures, and payments.
The study population consisted of all children ages 0–18 with at least two inpatient or outpatient claims with a primary diagnosis of autism (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 299.xx) anytime during the six-year study period from 2007 through 2012 (N=38,928); this approach to identification of ASD was validated by James Burke and colleagues.21 A child’s data for a given year was utilized if they were enrolled continuously during all 12 months of the year. Because of the many differences in the types of services used across children’s ages, we did not require continuous enrollment throughout the entire 6-year study period as this would have resulted in the same sample being included in every calendar year, leading to a cohort that aged 6 years over the study period, as well as a much smaller sample overall. Sensitivity analyses considered whether effects differed for younger (0–12) vs. older (13–18) youth as well as for the sub-sample of youth with at least 2 primary diagnoses of Autistic Disorder (299.00) during the study period; see the appendix.22 To ensure we have all information on mental health service use, we omitted plans that carved-out mental health benefits.
Outcomes.
We examined use of mental health care, speech/language therapy, and OT/PT within four categories of outcomes: (1) any service use; (2) the quantity of services utilized among service users; (3) total spending (insurer plus out-of-pocket) among service users, and (4) out-of-pocket spending among service users. We also examined total health care spending (all inpatient, outpatient, and pharmaceutical spending for all medical, mental health, and pharmaceutical care) for children with ASD. Use of inpatient or outpatient mental health services and psychotropic medications were identified using well-established algorithms23–25 based on ICD-9 diagnosis codes 295–309 (except 303, 304, and 305) and 311–314 and mental health specific procedure codes. Inpatient hospitalizations were identified as mental health-related if 50% or more of the claims associated with that hospitalization had a primary mental health diagnostic or procedure code and a primary discharge diagnosis of mental illness. Outpatient speech/language services were identified based on the following procedure codes: 92506–92508, 92526, G0153, S9128, S9152, T1013. Outpatient OT/PT services were identified based on the following procedure codes: 97001–97004, 97039, 97100, 97110, 97112, 97113, 97116, 97140, 97533, 97760, 98960, 99091, G0151, G0152, G0283, H2033, S8990, S9129, S9131. Given that providers may not always be precise about the exact billing codes used, we also consider a combined outcome for mental health, speech/language, and OT/PT. Outcomes examining the quantities of specific services used were measured among the subset of children using a specific service in a given calendar year. Spending outcomes are reported in real 2012 dollars. Note that the use of insurance claims data means that out-of-pocket costs include only co-pays and deductibles associated with claims processed through the insurance system and do not include costs associated with services that were entirely self-paid.
Statistical approach.
To evaluate how the federal parity law was related to outcomes, we used an interrupted time series model to compare trends observed in the post-parity time period with what would have been expected given trends observed pre-parity. The model included a linear monthly time variable, a parity indicator (0 from 2007–2009 and 1 from 2010–2012), the interaction between time and parity, and 11 binary variables for the calendar months. (The calendar month variables were included to account for seasonality, in particular due to deductibles that restart in January of each calendar year). The parameters of interest are the coefficient on parity, which captures any change in the outcome that happened at the time of parity implementation, and the coefficient on the time by parity interaction, which reflects any change in the time trend due to parity. A statistically significant coefficient on either or both of these terms is indicative of an association between the parity law and the outcome. We also present summary measures regarding the associations between the federal parity law and service use and spending outcomes during the first year following implementation. See the work of Anthony Biglan and colleagues (2000) or work by Anita Wagner and colleagues (2002) for details on these models.26,27
The models were fit with 72 monthly observations, aggregated across individuals; thus no individual-level covariates were included. Variances were calculated using Yule-Walker first order autoregressive parameters to control for correlation between consecutive months, fit using the SAS autoreg command (SAS Institute, Inc.).28 The model specification was chosen based on the Akaike Information Criterion (AIC),29 although results were similar across models that included other predictor sets, including a model with no month indicators and another with only those monthly indicators that were statistically significant.
Limitations and Strengths.
This study has a number of limitations. First, our analysis lacks a comparison group not affected by the parity law; identifying such a group is challenging for national policy changes such as the parity law. This means that the results could be sensitive to other changes or unmeasured factors that may be affecting service use and spending (unrelated to parity) occurring at the same time point. For example, from 2008 to 2010, 18 states enacted state autism insurance mandates that aimed to increase coverage of autism services among the commercially insured population. In practice, however, these laws would not be expected to affect enrollees in the Truven MarketScan data, which, as noted above, are comprised of employees and dependents of large firms that self-insure; state autism mandates only apply to enrollees of firms that are fully insured due to the ERISA law mentioned above. And, a recent published study of the effects of state autism mandate laws suggested little change in access to autism treatment services among self-insured enrollees in states with autism mandate laws, suggesting spillover effects are not a major concern.30 Related to this, many states enacted their own, typically narrower, parity laws in the years prior to passage of the federal parity law. Similar to state autism mandates, these state parity laws only applied to enrollees of firms that are fully insured. These enrollees are not included in these Truven data, thereby minimizing our concern about spillover. And very few state parity laws applied to children with ASD. However, in practice, if any spillover is occurring, the combined effects of both the federal and state parity laws are perhaps most relevant to understanding how this specific policy lever affects relevant outcomes among children with ASD.
Second, the MarketScan data captures plans with disproportionately generous coverage and thus may not be representative of all employer-sponsored plans. Third, while state indicators are available in Marketscan, our analysis is aggregated to the month level prohibiting us from controlling for state level characteristics. Fourth, we do not have details on specific benefits offered within enrollees’ health plans to understand which services were covered and at what levels, and how benefits changed before and after the parity law. Fifth, children with ASD receive many services in schools31,32 and parents have traditionally paid for much of ASD care on a self-pay basis. We do not capture any services received in school settings or any paid completely out-of-pocket, therefore we cannot observe how the changes we have identified in commercial coverage are connected to utilization or spending changes in the school sectors or family financial burden outside of insurance.
Offsetting strengths of this study include the very large sample size, inclusion of all claims paid for through private insurance, and examination of a variety of important outcomes.
RESULTS
Unadjusted demographic and clinical characteristics of the full sample with ASD diagnoses at the child-year level are presented in Exhibit 1. Across study years, only about 18% of children in each year were female and about 33% were between 12 and 18 years old. In each year, approximately two-thirds of the children had a co-morbid mental health diagnosis, the most common of which was conduct disorder/oppositional defiant disorder. There was a slight increase over time in the treated prevalence of ASD, measured as the share of enrollees ages 0–18 with a primary diagnosis of ASD on a service claim, from 0.30% in 2007–2009 to 0.40% in 2010–2012.
Exhibit 1.
Unadjusted descriptive statistics of children with autism spectrum disorder (ASD), Ages 0–18, and their annual service utilization: three years pre-parity and three years post-parity 1
| Pre-Parity (2007–2009) | Post-Parity (2010–2012) | |
|---|---|---|
| N | 20,155 | 28,009 |
| Treated prevalence (of all children 0–18)2 | 0.30 | 0.40 |
| Female gender, % | 17.4 | 18.2 |
| Age, % | ||
| 0–3 | 8.0 | 6.7 |
| 4–7 | 31.3 | 28.5 |
| 8–11 | 27.8 | 30.2 |
| 12–15 | 22.4 | 22.6 |
| 16–18 | 10.6 | 12.0 |
| Any co-morbid mental health diagnosis, %3 | ||
| Any depression diagnosis, % | 2.9 | 3.3 |
| Any anxiety diagnosis, % | 8.2 | 10.3 |
| Any ADHD diagnosis, % | 19.3 | 21.2 |
| Any conduct disorder or oppositional defiance disorder diagnosis, % | 61.7 | 63.8 |
| Any other mental health diagnosis | 16.7 | 17.1 |
| Annual use of specific types of services among children with ASD | ||
| Any inpatient mental health service use, % | 2.5 | 2.4 |
| Any outpatient mental health service use, % | 67.4 | 69.7 |
| Any outpatient psychotropic medication management service use, % | 18.5 | 17.5 |
| Any outpatient psychotherapy service use, % | 45.6 | 46.5 |
| Any speech/language therapy service use, % | 8.8 | 11.3 |
| Any OT/PT therapy service use, % | 5.4 | 6.3 |
| Any psychotropic drug use, % | 53.9 | 54.0 |
| Annual quantity of specific types of services used among children with ASD using that type of service | ||
| Average # outpatient visits per year | 11.1 | 15.1 |
| Average # psychotropic medication management visits per year | 3.9 | 3.9 |
| Average # outpatient psychotherapy visits per year | 11.0 | 12.6 |
| Average # speech/language therapy visits per year | 19.9 | 22.6 |
| Average # OT/PT visits per year | 12.1 | 14.6 |
| Annual total spending on specific types of services among children with ASD using that type of service4 | ||
| Total health care spending per year (mean $)5 | 8759.24 | 10819.5 |
| Total mental health spending per year (mean $) 6 | 3044.97 | 3524.35 |
| Total outpatient mental health spending per year (mean $) | 995.40 | 1529.50 |
| Total speech/language therapy spending per year (mean $) | 190.65 | 284.39 |
| Total OT/PT spending per year (mean $) | 59.71 | 131.53 |
| Total psychotropic drug spending per year (mean $) | 1647.28 | 1582.61 |
| Annual Out-of-Pocket (OOP) spending on specific types of services among children with ASD using that type of service | ||
| Total OOP health care spending per year (mean $) | 1245.60 | 1468.17 |
| Total OOP mental health care spending per year (mean $) | 454.91 | 505.40 |
| Total OOP outpatient mental health care spending per year (mean $) | 214.04 | 270.96 |
| Total OOP speech/language therapy spending per year (mean $) | 39.00 | 59.72 |
| Total OOP OT/PT spending per year (mean $) | 13.37 | 15.99 |
| Total OOP psychotropic drug spending per year (mean $) | 214.84 | 204.92 |
Each observation is at the child-year level, and one child may appear in multiple years. Each cell represents the average of 3 years of annual data.
Treated prevalence of autism is defined as the proportion of child enrollees ages 0–18 with at least one claim with an ASD diagnosis.
Children with an ASD diagnosis in the sample could have multiple co-morbid mental health diagnoses.
Total spending includes both the health insurer and the family out-of-pocket payment for services paid for through insurance.
Health care spending among children with ASD includes all types of services paid for by insurance including medical care, mental health care, functional therapies and prescription drugs.
Mental health care spending among children with ASD includes inpatient mental health care, outpatient mental health services and psychotropic drug use.
ADHD – Attention-deficit/hyperactivity disorder
OT/PT: Occupational or Physical Therapy
Source: Authors’ analysis of data from the Truven Health MarketScan Database, 2007 to 2012.
Descriptive information on service utilization paid for through private insurance by calendar year is presented in Exhibit 1. Approximately two-thirds of the sample used outpatient mental health services while only about 2 percent used inpatient mental health services in a given year. Use of outpatient psychotherapy services was more common than use of outpatient psychotropic medication management services. Fewer children with ASD used functional therapies in a given year with only 8.8–11.3% using speech/language therapy and 5.4–6.3% using OT/PT during the study period. Approximately 54% used psychotropic prescription drugs in a given year. Total health care spending averaged from close to $8,800–$10,800 and total mental health care spending averaged $3,000–$3,500 per year per child. Total out-of-pocket mental health care spending averaged $450–500 per year per child.
Exhibit 2 shows the associations between the federal parity law and use of services among children with ASD. There were generally no statistically significant increases in service utilization at the time of the federal parity law’s implementation, but there were increases in the trends in service utilization over time attributable to the federal parity law. For example, while the probability of mental health service use among children with ASD did not increase at the time of implementation of the parity law (p=0.75; 95% CI: −0.0078, 0.0056), the rate of change in the use of mental health services over time did increase after parity (p=<.001; CI: 0.0010, 0.0017). A similar pattern was seen for speech/language therapies (p for trend<.001; CI: 0.0005, 0.0008) and OT/PT therapies (p for trend<.001; CI: 0.0003, 0.0004). Conditional on use of specific types of services, the quantity of most categories of services used by children with ASD also increased after parity (Exhibit 2). Specifically, among children with ASD using outpatient mental health services, there was a small but significant increase in the number of visits per month (p=0.05; CI: −0.0002, 0.1012) both at the time of parity implementation and as an increase in the trend in the number of outpatient mental health visits per month (p<.001; CI: 0.0110, 0.0156) after parity. A similar pattern was seen among children with ASD using speech/language and OT/PT therapies (speech/language: p<.001; CI: 0.0084, 0.0172; OT/PT: p<.001; CI: 0.0076, 0.0137). For example, over the first year following parity, this translated into 1.6 additional mental health visits per user of mental health services, 0.4 additional speech therapy visits per user of speech therapy, and 0.7 additional OT/PT visits per user of OT/PT. These results are summarized in Exhibit 3, which shows the increase in mental health, speech/language, and OT/PT visits associated with the federal parity law’s implementation.
Exhibit 2.
Associations between parity and service utilization among children with autism spectrum disorders before and after federal parity, 2007–20121 (N=38,928)
| Parity | Parity by Month Interaction | |
|---|---|---|
| Change in probability of any mental health or functional therapy outpatient service use, per month | 0.0029 | 0.0015** |
| Change in probability of any mental health service use, per month | −0.0011 | 0.0014** |
| Change in probability of any speech therapy service use, per month | −0.0001 | 0.0006** |
| Change in probability of any OT/PT service use, per month | −0.0001 | 0.00035** |
| Change in number of mental health or functional therapy outpatient visits, per month per user | 0.0450* | 0.0178** |
| Change in number of outpatient mental health visits, per month per user | 0.0505* | 0.0133** |
| Change in number of speech therapy visits, per month per user | 0.0516 | 0.0129** |
| Change in number of OT/PT therapy visits per month, per user | −0.0086 | 0.0108** |
Results were estimated using Yule-Walker interrupted time series regression models with first-order autocorrelation parameters. Model covariates included 12 month indicator variables to adjust for month-specific trends in outcomes. Note: mental health services includes both inpatient and outpatient mental health services. Restricted to children with 2 or more primary diagnoses of ASD. The parameters of interest are the coefficient on parity (“parity” column in Exhibit), which captures any change in the outcome that happened at the time of parity implementation, and the coefficient on the time by parity interaction (“Parity by Month” column in the Exhibit), which reflects any change in the time trend due to parity. A statistically significant coefficient on either or both of these terms is indicative of an association between the parity law and the outcome. Full results in appendix.22
OT/PT: Occupational or Physical Therapy
: 0.05 < p-value < 0.1;
: p-value < 0.05
Source: Authors’ analysis of data from the Truven Health MarketScan Database, 2007 to 2012.
EXHIBIT 3 (Figure).
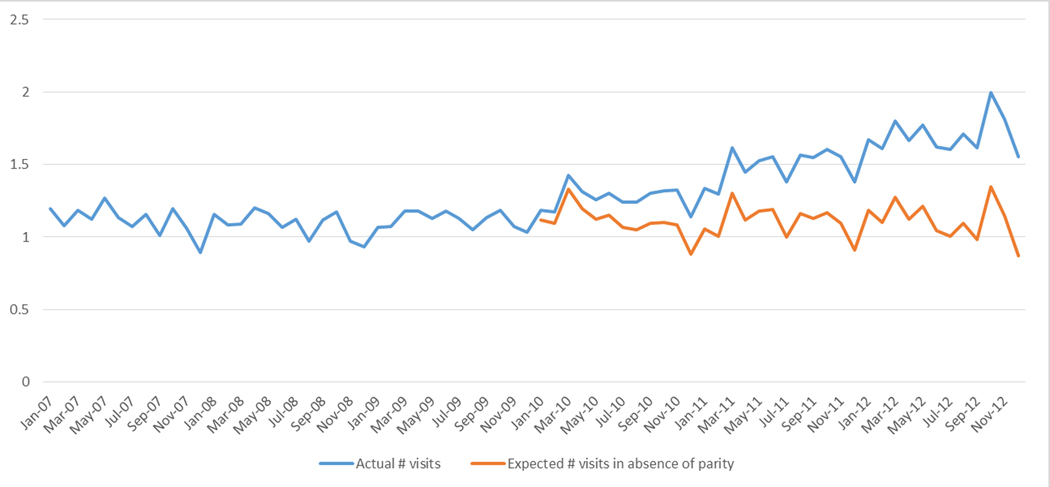
Associations between federal parity law and outpatient mental health and functional therapy visits, among youth using those services.
Source: Authors’ analysis of data from the Truven Health MarketScan Database, 2007 to 2012
Exhibit 4 shows the associations between the federal parity law and total and out-of-pocket spending. For all total spending outcomes, we found no evidence of a jump in spending at the time of parity implementation. However, we found small but significant increases in the post-parity trends for total health care spending and each of the components examined. During the first year following implementation of the parity law, for example, this corresponds to an average increase in total spending of $73 per child. As indicated by the lower panel of Exhibit 4, the increase in total spending was not accompanied by an increase in out-of-pocket spending by families. We found no significant associations between the federal parity law and out-of-pocket spending, with one exception: a slight increase in the trend in out-of-pocket spending on OT/PT services (p<.001; CI: 0.0165, 0.0382).
Exhibit 4.
Associations between parity and total and out-of-pocket spending among children with autism spectrum disorders before and after federal parity, 2007–20121 (N=38,928)
| Parity | Parity by Month Interaction | |
|---|---|---|
| Change in total health care spending, per month | −5.8204 | 1.8358** |
| Change in total mental health or functional therapy outpatient spending, per month | 2.2714 | 2.0622** |
| Change in total mental health spending,1 per month | 6.4507 | 1.5739** |
| Change in total speech/language therapy spending, per month | −0.6493 | 0.3115** |
| Change in total OT/PT spending, per month | −0.097 | 0.3266** |
| Change in total OOP health care spending, per month | 3.1919 | 0.3310 |
| Change in OOP mental health or functional therapy outpatient spending, per month | 1.0039 | 0.0360 |
| Change in OOP mental health spending, per month | 1.6322 | 0.0296 |
| Change in OOP speech/language therapy spending, per month | −0.1581 | 0.0363 |
| Change in OOP OT/PT spending, per month | −0.0791 | 0.0273** |
Results were estimated using Yule-Walker interrupted time series regression models with first-order autocorrelation parameters. Model covariates included 12 month indicator variables to adjust for month-specific trends in outcomes. Total spending includes inpatient and outpatient spending on medical, mental health, functional services, and drug costs, and includes both insurer and out-of-pocket spending. Note: mental health spending includes inpatient and outpatient mental health service spending and psychotropic drug spending. Restricted to children with 2 or more primary diagnoses of ASD. The parameters of interest are the coefficient on parity (“parity” column in Exhibit), which captures any change in the outcome that happened at the time of parity implementation, and the coefficient on the time by parity interaction (“Parity by Month” column in the Exhibit), which reflects any change in the time trend due to parity. A statistically significant coefficient on either or both of these terms is indicative of an association between the parity law and the outcome. Full results in appendix.22
OT/PT: Occupational or Physical Therapy
: 0.05 < p-value < 0.1;
: p-value < 0.05
Source: Authors’ analysis of data from the Truven Health MarketScan Database, 2007 to 2012.
There is evidence that the associations observed are concentrated in youth ages 0–12 (compared to 13–18 year olds). Full results are presented in the appendix22; in brief, the parity law was associated with 4.6 additional mental health or functional therapy (speech/therapy or OT/PT) visits per 0–12 year old child using those services during the first year following implementation. Sensitivity analyses restricting attention to youth with 2 diagnoses of Autistic Disorder found results nearly identical to those presented here; full results are in the appendix22.
DISCUSSION
The federal parity law was associated with increases in the probability of children with ASD receiving mental health and functional therapies, and increases in the quantity of these services used. MHPAEA’s implementation was also associated with increases in expenditures for mental health services and functional therapies. However, the law was not associated with significant changes in OOP spending among families of children with ASD except for a slight increase in OOP spending for OT/PT services. These differences in findings between outcomes reduces the likelihood that our findings were due to a general secular increase in autism treatment under commercial insurance; if that was the case we would have expected to see an accompanying increase in family OOP spending. The fact that we did not observe such an increase suggests that the federal parity law may have conferred financial protection to families seeking to avail themselves of treatments now covered more generously under the law – a central intent of its architects.
Changes in outcomes associated with the federal parity law were larger in magnitude among younger children with ASD than older children. This finding makes sense for a few reasons. First, as children move into school settings, schools tend to provide more services that might have been paid by commercial insurance prior to the school years. Second, as children age they have less time for intensive treatment due to the increasing demands of school and other activities. And finally, many providers only work with younger children with ASD so even among children with private insurance coverage, it becomes increasingly difficult to find providers as children age.
Our findings regarding the federal parity law differ substantially from prior work indicating no effects of state parity laws on access to services or financial protection for children with ASD.19 The results also differ from some previous work showing limited effects of state autism mandates on out-of-pocket costs and financial burden among families of children with ASD. However, both Bilaver and Jordan (2013) and Pinka Chatterji et al. (2015) used data from the National Survey of Children with Special Health Care Needs and relied on families’ self-report of out-of-pocket expenditures, which may be subject to recall bias.19,33 In addition, these data did not allow researchers to determine whether a child was enrolled in an insurance plan subject to the mandate; typically only about half of privately insured individuals would have been affected,20 due to the fact that the Employee Retirement Income Security Act (ERISA) exempts “self-insured” firms—those that contract with health plans only to administer employee health benefits and not to pool risk—from state insurance regulations.
CONCLUSIONS
This study provides evidence that the federal parity law was associated with greater use of services paid for through insurance for children with ASD without driving up the out-of-pocket spending paid by families through their insurance policies. However, the higher rates of use after MHPAEA implementation are still well below what one might expect in the context of increasing levels of impairment and service needs over the last few years with the most recent Centers for Disease Control and Prevention’s estimate of the community prevalence of ASD now at 15 per 1000 children. Monitoring and enforcement of the federal parity law has been a persistent concern.34 Our findings suggest that more stringent parity enforcement, additional policy approaches, or both, may be needed to ensure that children with ASD are connected to evidence-based services and supports.
Supplementary Material
References
- 1.Barry CL, Gabel JR, Frank RG, Whitmore HH, Hawkins S, Pickreign JD. Design of mental health benefits: still unequal after all these years. Health Aff (Millwood). 2003; 22(5):127–37. [DOI] [PubMed] [Google Scholar]
- 2.Internal Revenue Service, Department of the Treasury; Employee Benefits Security Administration, Department of Labor; Centers for Medicare & Medicaid Services, Department of Health and Human Services. Interim final rules under the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008. Interim final rules with request for comments. Fed Regist. 2010; 75(21): 5409–51. [PubMed] [Google Scholar]
- 3.Barry CL, Huskamp HA, Goldman HH. A political history of federal mental health and addiction insurance parity. Milbank Q. 2010; 88(3):404–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 5.King M, Bearman P. Diagnostic change and the increased prevalence of autism. Int J Epidemiol. 2009; 38(5):1224–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christensen DL, Baio J, Braun KV, Bilder D, Charles J, Constantino JN, et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveill Summ. 2016;65(No. SS-3): 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Myers SM, Johnson CP, American Academy of Pediatrics Council on Children with Disabilities. Management of children with autism spectrum disorders. Pediatrics. 2007; 120(5):1162–82. [DOI] [PubMed] [Google Scholar]
- 8.Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014; 168(8):721–8. [DOI] [PubMed] [Google Scholar]
- 9.Leslie D. Health care service use and costs among patients with autism. In: American Public Health Association 133rd Annual Meeting & Exposition; December 2005; Philadelphia, PA. [Google Scholar]
- 10.Mandell DS, Cao J, Ittenbach R, Pinto-Martin J. Medicaid expenditures for children with autistic spectrum disorders: 1994 to 1999. J Autism Dev Disord. 2006;36(4):475–85. [DOI] [PubMed] [Google Scholar]
- 11.Brookman-Frazee L, Baker-Ericzén M, Stadnick N, Taylor R. Parent perspectives on community mental health services for children with autism spectrum disorders. J Child Fam Stud. 2012; 21(4):533–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zablotsky B, Anderson C, Law P. The association between child autism symptomatology, maternal quality of life, and risk for depression. J Autism Dev Disord. 2013; 43(8):1946–55. [DOI] [PubMed] [Google Scholar]
- 13.Chiri G, Warfield ME. Unmet need and problems accessing core health care services for children with autism spectrum disorder. Matern Child Health J. 2012; 16(5): 1081–91. [DOI] [PubMed] [Google Scholar]
- 14.Peele PB, Lave JR, Kelleher KJ. Exclusions and limitations in children’s behavioral health care coverage. Psychiatr Serv. 2002; 53(5):591–4. [DOI] [PubMed] [Google Scholar]
- 15.Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord. 2006; 36(7):849–61. [DOI] [PubMed] [Google Scholar]
- 16.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–9. [DOI] [PubMed] [Google Scholar]
- 17.Behavior Analyst Certification Board. Applied Behavior Analysis Treatment of Autism Spectrum Disorder: Practice Guidelines for Healthcare Funders and Managers. 2nd ed. Littleton, CO: Behavior Analyst Certification Board; 2014. [Google Scholar]
- 18.Berry KN, Huskamp HA, Goldman HG, Rutkow L, Barry CL . Litigation Provides Clues to Ongoing Challenges in Implementing Insurance Parity. Under Review. [DOI] [PubMed] [Google Scholar]
- 19.Bilaver LA, Jordan N. Impact of state mental health parity laws on access to autism services. Psychiatr Serv. 2013; 64(10):967–73. [DOI] [PubMed] [Google Scholar]
- 20.Buchmueller TC, Cooper PF, Jacobson M, Zuvekas SH . Parity for whom? Exemptions and the extent of state mental health parity legislation. Health Aff (Millwood). 2007; 26(4):w483–7. [DOI] [PubMed] [Google Scholar]
- 21.Burke JP, Jain A, Yang W, Kelly JP, Kaiser M, Becker L, et al. Does a claims diagnosis of autism mean a true case? Autism. 2014; 18(3):321–30. [DOI] [PubMed] [Google Scholar]
- 22.To access the appendix, click on the Appendix link in the box to the right of the article online.
- 23.Goldman HH, Frank RG, Burnam MA, Huskamp HA, Ridgely MS, Normand SL, et al. Behavioral health insurance parity for federal employees. N Engl J Med. 2006;354(13):1378–86. [DOI] [PubMed] [Google Scholar]
- 24.Busch AB, Yoon F, Barry CL, Azzone V, Normand SL, Goldman HH, et al. The effects of mental health parity on spending and utilization for bipolar, major depression, and adjustment disorders. Am J Psychiatry. 2013;170(2):180–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barry CL, Chien AT, Normand SL, Busch AB, Azzone V, Goldman HH, et al. Parity and out-of-pocket spending for children with high mental health or substance abuse expenditures. Pediatrics. 2013; 131(3): e903–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Biglan A, Ary D, Wagenaar AC. The value of interrupted time-series experiments for community intervention research. Prev Sci. 2000; 1(1): 31–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002; 27(4): 299–309. [DOI] [PubMed] [Google Scholar]
- 28.SAS Institute Inc. SAS/ETS® 13.2 User’s Guide. Cary, NC: SAS Institute Inc; 2014. [Google Scholar]
- 29.Akaike H. Information theory and an extension of the maximum likelihood principle. In: Petrov BN, Csáki F. 2nd International Symposium on Information Theory.Budapest: Akadémiai Kiadó; 1973. pp. 267–281. [Google Scholar]
- 30.Mandell DS, Barry CL, Marcus SC, Xie M, Shea K, Mullan K, et al. The Effects of Autism Insurance Mandates on the Treated Prevalence of Autism. JAMA Pediatr. 2016; 170(9): 887–93 [DOI] [PubMed] [Google Scholar]
- 31.Levy SE, Mandell DS, Schultz RT. Autism. Lancet. 2009; 374(9701):1627–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Narendorf SC, Shattuck PT, Sterzing PR. Mental health service use among adolescents with an autism spectrum disorder. Psychiatr Serv. 2011; 62(8):975–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chatterji P, Decker SL, Markowitz S. The effects of mandated health insurance benefits for autism on out-of-pocket costs and access to treatment. J Policy Anal Manage. 2015; 34(2): 328–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barry CL, Goldman HH, Huskamp HA. Federal Parity in the Evolving Mental Health and Addiction Care Landscape. Health Aff (Millwood) 2016; 35(6): 1009–16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


