Abstract
Although best practice recommendations exist regarding school-based healthy eating and physical activity policies, practices, and programs, research indicates that implementation is poor. As the field of implementation science is rapidly evolving, an update of the recent review of strategies to improve the implementation of healthy eating and physical activity interventions in schools published in the Cochrane Library in 2017 was required. The primary aim of this review was to examine the effectiveness of strategies that aim to improve the implementation of school‐based policies, practices, or programs to address child diet, physical activity, or obesity. A systematic review of articles published between August 31, 2016 and April 10, 2019 utilizing Cochrane methodology was conducted. In addition to the 22 studies included in the original review, eight further studies were identified as eligible. The 30 studies sought to improve the implementation of healthy eating (n = 16), physical activity (n = 11), or both healthy eating and physical activity (n = 3). The narrative synthesis indicated that effect sizes of strategies to improve implementation were highly variable across studies. For example, among 10 studies reporting the proportion of schools implementing a targeted policy, practice, or program versus a minimal or usual practice control, the median unadjusted effect size was 16.2%, ranging from –0.2% to 66.6%. Findings provide some evidence to support the effectiveness of strategies in enhancing the nutritional quality of foods served at schools, the implementation of canteen policies, and the time scheduled for physical education.
Keywords: School, Implementation, Nutrition, Physical activity, Policy
Implications.
Practice: Findings of the review provide guidance for health promotion practitioners and jurisdictions working within school-based settings to implement World Health Organization obesity-prevention recommendations
Policy: The review identified that the implementation of several policies have facilitated improvements in the availability of healthy foods in schools, of magnitudes that could lead to substantial improvements in public health nutrition.
Research: The review builds on current literature to provide greater clarity on the effect of strategies to support the implementation of evidence-based healthy eating, physical activity, and obesity-prevention policies and practices, a critical component to achieve the public health benefits of such policies and practices.
INTRODUCTION
An unhealthy diet, inadequate physical activity, and excessive weight gain are independent risk factors for the leading causes of death and disability globally, including cancer and cardiovascular disease [1]. In childhood and adolescents, a healthy diet [2, 3], physical activity [4–6], and healthy weight [7] have also been found to be independently associated with immediate positive health outcomes, including improved mental health and academic performance. Additionally, as health behaviors developed during childhood have been found to track into adulthood [8], interventions to address these risk factors are recommended by the World Health Organization (WHO) and governments internationally as part of population health and chronic disease prevention strategies [9].
Schools represent an attractive and important setting for health promotion initiatives as they provide continual access to children during a critical period of their development [10, 11]. Systematic reviews have identified well over 100 randomized trials of school-based interventions targeting student diet, physical activity, or obesity and have demonstrated that such interventions can be effective in reducing associated health risks [12–14]. On the basis of such evidence, national and international best-practice guidelines have been established acknowledging the potential for school-based settings to influence the development of children’s healthy eating and physical activity behaviors [15–18]. These evidence-based guidelines recommend schools adopt a range of policies, practices, and programs, such as the scheduling and provision of physical activity and active play opportunities, reducing the availability of unhealthy foods for sale at schools and alignment of foods services with national dietary guidelines [15, 18, 19].
Despite the existence of these best-practice guidelines, research suggests that schools fail to routinely implement evidence-based policies, practices, and programs. For example, the 2014 report card of physical activity in Ireland found that only 17% of primary schools were providing the mandated 2 hr of compulsory physical education per week [20]. Similarly, studies of Australian primary schools have found that only 5%–35% of Australian schools comply with mandated school canteen policies regarding the availability of unhealthy foods and beverages [21], whilst just 10% of middle and high schools within the USA prohibit the sale of sugar-sweetened beverages other than soda [22]. Without routine implementation, the public health benefits of such policies and practices promoting healthy eating and physical activity will not be fully achieved.
The field of implementation science seeks to address this issue through the generation of evidence to facilitate the use of evidence-based policies, practices, and programs [23]. Implementation science research seeks to identify effective strategies, such as educational outreach visits, reminders, or audit and feedback, which best support the integration of evidence-based practices into a specific setting [23, 24]. Implementation trials seek to assess the impact of such implementation strategies on the measures of the implementation of an evidence-based policy, practice, or program [23, 24]. Relative to trials testing the efficacy of behavioral interventions, few implementation trials have been conducted examining strategies to best implement evidence-based healthy eating, physical activity, or obesity-prevention interventions in the school setting [25].
We conducted a comprehensive Cochrane review on the topic in 2017, which included studies (randomized and nonrandomized) published until August 2016 [25]. The review identified 27 studies, 15 of which aimed to improve the implementation of healthy eating practices, and 6 studies targeted physical activity (the remaining studies pertained to alcohol and tobacco prevention) [25]. Findings of the review was mixed, with inconsistent improvements in the implementation of policies, practices, or programs reported across studies. Additionally, considerable clinical heterogeneity in the type of implementation strategies tested, policies, practices, and programs targeted, and outcomes assessed across the included studies was evident within the review [25]. Overall, the impact of strategies on the implementation of physical activity and healthy eating policies, practices, and programs was unclear, and the certainty of the evidence was low [25].
We are not aware of any review of school-based implementation interventions undertaken since that review. The field of implementation science, however, is rapidly evolving and a number of implementation studies targeting healthy eating and physical activity policies, practices, and programs have been published in recent years [26–28]. The addition of new studies may provide greater clarity regarding the effect of such strategies on the implementation of evidence-based policies, programs, and practices in schools given variable and inconclusive findings from the previous review. The aim of this review, therefore, was to update our previous review by Wolfenden et al. to reflect the current state of the evidence.
OBJECTIVES
The primary aim of this review was to examine the effectiveness of strategies that aim to improve the implementation of school‐based policies, practices, or programs to address child diet, physical activity, or obesity.
METHODS
This review aligns with the reporting guidelines specified within the 2009 PRISMA checklist for systematic reviews [29] (Supplementary File I) and utilized Cochrane methodology to replicate the previous review by Wolfenden et al. [25].
Selection criteria
Types of studies
“Implementation” was defined as the use of strategies to adopt and integrate evidence‐based health interventions and to change practice patterns within specific settings [30]. Any study (randomized or nonrandomized) conducted at any scale with a parallel control group that compared a strategy to implement school-based policies, practices, or programs to address child diet, physical activity, overweight, or obesity by school staff to “no intervention,” “usual” practice, or a different implementation strategy was eligible for inclusion. Unlike the original review, we excluded studies solely targeting the implementation of tobacco or alcohol use prevention policies, practices, or programs as these were not the focus of this review update.
Types of interventions
Studies employing any strategy with the primary aim of improving implementation of healthy eating, physical activity, or obesity prevention policies, practices, or programs in schools were eligible. Strategies must have aimed to improve the implementation of policies, practices, or programs by usual school staff. Strategies could include quality improvement initiatives, education and training, performance feedback, prompts and reminders, implementation resources (e.g., manuals), financial incentives, penalties, communication and social marketing strategies, professional networking, the use of opinion leaders, implementation consensus processes, or other strategies [25].
Types of participants
Eligible studies were set in schools (e.g., primary, elementary, middle, and secondary) where the age of students is predominately between 5 and 18 years [31]. Study participants could be any stakeholders who may influence the uptake, implementation, or sustainability of the target health promoting policy, practice, or program in schools, including teachers, managers, cooks/catering staff, or other staff of schools and education departments.
Types of outcome measures
Studies with any objectively or subjectively (self‐reported) assessed measure of school policy, practice, or program implementation—including uptake, partial/complete uptake (e.g., consistent with protocol/design), or routine use—were included. Implementation could have occurred at any scale (e.g., local, national, or international). Implementation outcomes (e.g., frequency of practice implementation by teachers) must have been undertaken by a school or routine school personnel and not those undertaken by paid research personnel. Child-level outcomes (e.g., child diet and physical activity) were not considered as implementation outcomes. Studies collecting outcome data at follow-up only for an implementation outcome were included for randomized trial designs only (i.e., equivalent baseline values assumed or differ only by chance) or if baseline values were assumed to be zero (i.e., a school policy did not exist at baseline). Implementation outcome data may have been obtained from audits of school records, questionnaires or surveys of staff, direct observation or recordings, examination of routinely collected information from government departments (such as compliance with food standards or breaches of department regulations), or other sources.
Search strategy
The original search by Wolfenden et al. was undertaken for studies published up to August 31, 2016 [25]. Small amendments were made to the original search strategy to improve the sensitivity of the search, which was conducted by an experienced research librarian. This updated review included eligible studies published up until April 10, 2019, from a search of the following electronic databases: Cochrane Library, including the Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE; MEDLINE InProcess & Other Non‐Indexed Citations; Embase Classic and Embase; PsycINFO; Education Resource Information Center; Cumulative Index to Nursing and Allied Health Literature; Dissertations and Theses; and SCOPUS (Appendix II Medline search strategy). Additionally, a search of the World Health Organization International Clinical Trials Registry Platform (www.who.int/ictrp/) and ClinicalTrials.gov (www.clinicaltrials.gov) conducted by Wolfenden et al. was replicated for this review. The “Characteristics of Ongoing Studies” section of the original review was also searched for potentially eligible studies that were unpublished at the time of the first review [25].
Data collection and analysis
Selection of studies
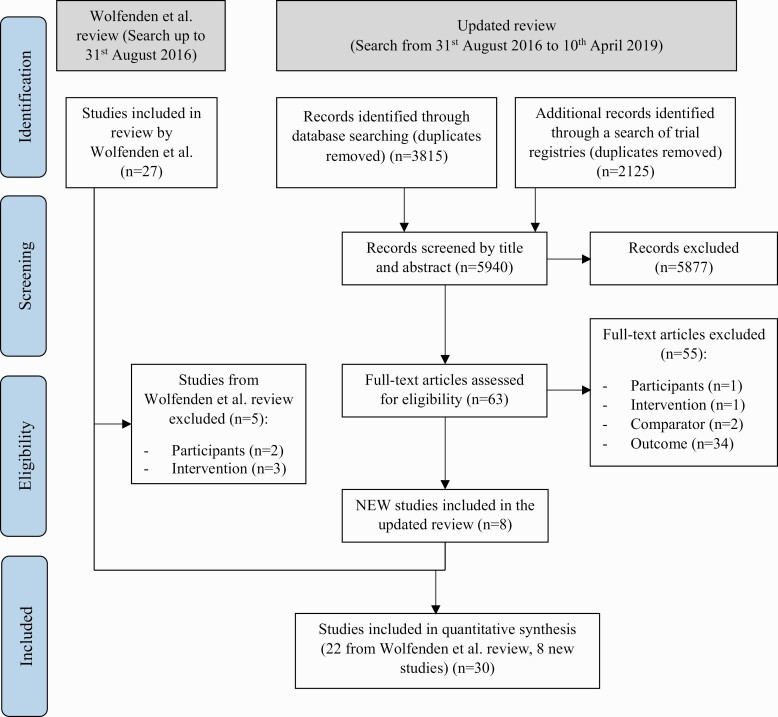
Title and abstract screening for eligible studies was performed independently by review authors in pairs. Authors were not blind to author or journal information. For potentially eligible studies, full texts of manuscripts were examined for eligibility by a pair of review authors independently. Reasons for exclusion were documented for all studies and recorded in Fig. 1. Disagreements between review authors were resolved via consensus or, when required, by a third author.
Fig 1.
Study flow diagram.
Data extraction and management
Data extraction was completed independently by two authors unblinded to author and journal information. Discrepancies between review authors were resolved via consensus or by a third author when required. Information extracted from eligible studies included: study eligibility and design; date of publication; country and demographic characteristics of participants; number of experimental conditions; characteristics of employed implementation strategies; study outcomes of interest and information to allow the assessment of risk of bias. Implementation strategies were classified according to the Effective Practice and Organization of Care (EPOC) taxonomy [32] (Appendix III).
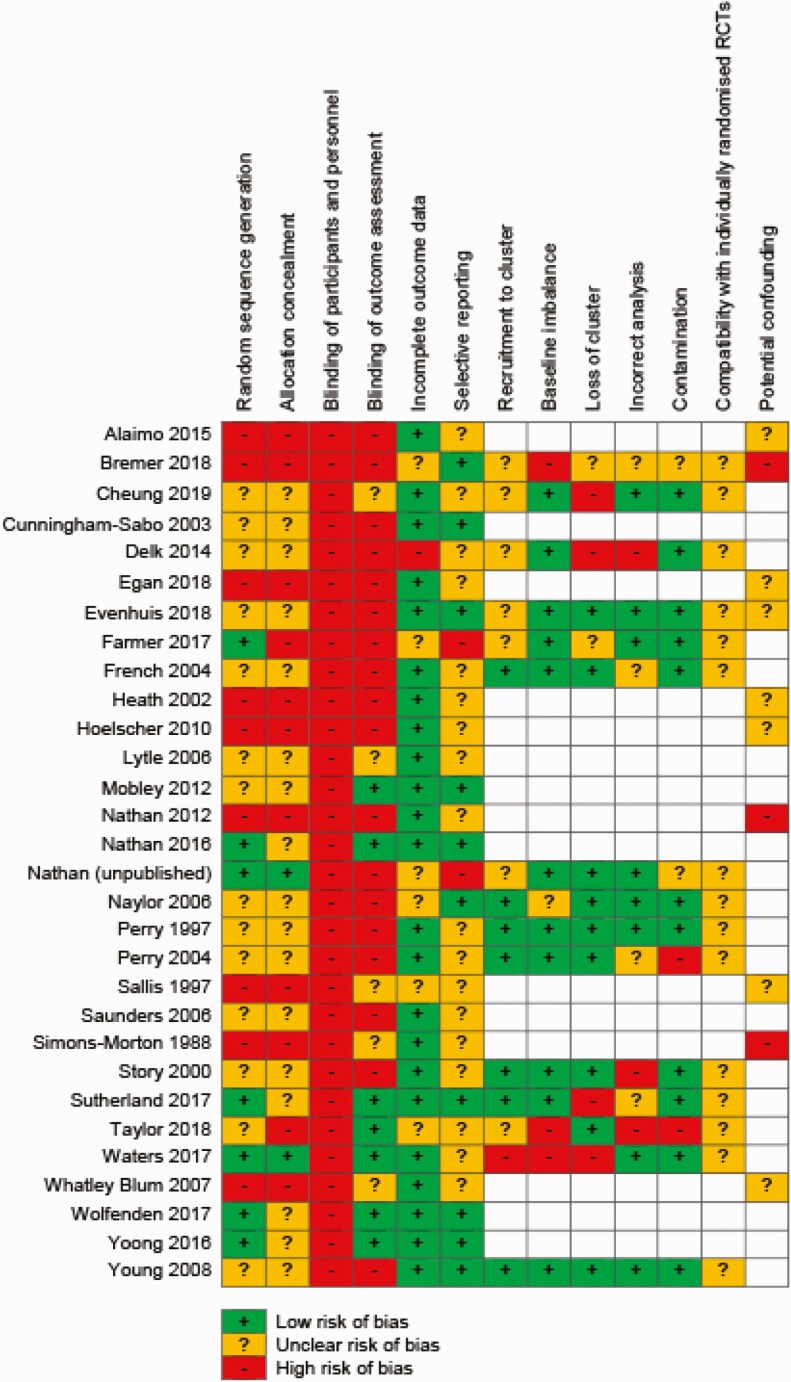
Assessment of risk of bias in included studies
Two authors independently assessed risk of bias within each included study using the “Risk of Bias” tool described within the Cochrane Handbook for Systematic Reviews of Interventions [33]. The following domains were assessed for individual studies and outcomes to determine an overall risk of bias: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and “other” potential sources of bias. For nonrandomized trials, an additional “potential confounding” domain was also assessed, defined as the risk that an unmeasured characteristic shared by those allocated to receive the implementation intervention (or strategy), rather than the intervention itself, was responsible for reported outcomes [34]. Additional domains were also used to assess cluster-randomized controlled trials, including: recruitment to cluster, baseline imbalance, loss of clusters, incorrect analysis, and compatibility with individually randomized controlled trials [33]. Disagreements between review authors were resolved via consensus or, when required, by a third author.
Measurement of treatment effect
Substantial study heterogeneity in outcomes and measures used to assess implementation precluded meta‐analysis and presented considerable synthesis challenges. As such, a narrative synthesis was conducted collectively with studies from the original and updated review. First, we summarized the characteristics of included studies based on population, and “intervention” (implementation strategy categorized based on EPOC taxonomy [32]) characteristics. Second, to provide a high-level summary of findings, we described the effect size of the primary policy, practice, or program implementation outcome measure for each study and summarized this across studies for each broad category of implementation outcomes (e.g., score-based measures, proportion of time implementing a practice, or frequency of implementation) [25, 35]. Effect sizes were calculated by subtracting the change from baseline on the primary implementation outcome for the control (or comparison) group from the change from baseline in the experimental or intervention group. We reverse-scored implementation measures that did not represent an improvement (e.g., proportion of schools serving unhealthy food items) [25, 35]. For studies with multiple follow‐up periods, data from the final follow‐up period reported was extracted and subtracted from baseline [25, 35, 36]. If data to enable the calculation of change from baseline were unavailable, the differences between groups postintervention were used. Where there were two or more primary implementation outcome measures, standardized measures of effect size were calculated for each outcome, measures were ranked based on their size of effect, and the median measure was used (and range reported) [35, 36].
Where the primary outcome measure was not identified by the study authors in the published manuscripts, the implementation outcome on which the study sample size calculation was based was used or, in its absence, the median effect size of all measures judged to be implementation outcomes reported in a manuscript was calculated and the range reported [25, 35, 36]. The inclusion of such effect sizes is for descriptive purposes and should not be considered as pooled estimates of effect as they do not weigh study effects by the inverse of their variance, nor do they consider study issues of study quality or design. Finally, we present a narrative synthesis of all studies, followed by a narrative synthesis of individual studies by the risk factor (physical activity or diet) targeted by the intervention.
RESULTS
The updated search (August 31, 2016 to April 10, 2019) identified 3,815 unique records of which 62 full-text records and one unpublished study (identified via the trial registry search, findings have since been published [37]) were assessed for eligibility (see Fig. 1). Fifty-five records were excluded following full-text screening for the following reasons: wrong participants (n = 1); wrong intervention (n = 1); no comparator (n = 2); and inappropriate outcomes (n = 34). Studies were excluded based on “inappropriate outcomes” if it did not measure implementation of a policy, practice, or program.
In this review update, seven new published studies [26–28, 38–42] and one unpublished study were identified for inclusion (see Fig. 1). Of the 27 studies included in the original Cochrane review covering multiple health risks, 22 studies [43–64] examining healthy eating, physical activity, or obesity prevention policy or practice implemented were included in this review update (see Fig. 1 for reasons for exclusion). In total, 30 studies were included in this review update. See Appendix I for characteristics of included studies.
Types of studies
Collectively from the 30 studies included from the original and updated review, 19 were conducted in the USA, 7 in Australia, 2 in Canada, and 1 each in New Zealand and the Netherlands. Nineteen included studies employed randomized designs (including 15 cluster randomized) and the remaining 11 studies were nonrandomized with a parallel control group. Studies were conducted between 1985 [59] and 2018 [65], with the duration of the studies varying from 20 weeks [26] to 4 years [49]. Twenty-six of the 30 included studies compared an implementation strategy to a control group or usual practice, whilst the remaining four studies directly compared different implementation strategies [39, 40, 46, 49].
Participants
The number of schools participating in the studies included in the review varied. The largest study recruited 828 schools [52], whilst the smallest study recruited two schools. The majority of studies (n = 22) were conducted within primary (or elementary) schools, which cater for children aged 5–12 years. The remaining studies were conducted in middle schools (n = 5) catering for children aged 11–14 years and secondary schools (n = 3) catering for children aged 13–18 years. All included studies were conducted within high-income countries.
Interventions
Sixteen studies tested strategies to implement healthy eating policies, practices, or programs, 11 tested strategies targeting physical activity policies or practices, and 3 tested strategies targeting both healthy eating and physical activity. A comprehensive description of the existing studies in the Cochrane Review are available in the “Characteristics of Included Studies” table of the manuscript [25], whilst a summary of all included 30 studies is provided in Appendix I.
All studies examined multistrategy implementation interventions. The number of implementation strategies, as characterized by the EPOC Taxonomy [32] (see Appendix III), ranged from two to nine (mean number of strategies = 6.5). While there was considerable heterogeneity in the strategies tested, 21 studies tested educational materials and educational meetings in combination with other strategies. Of those other strategies tested, educational outreach visits or academic detailing (n = 10) and audit with feedback (n = 4) were the most common. No study tested the effectiveness of just one implementation strategy and only two studies [26, 38] tested the same combination of strategies. A summary of the implementation strategies and effects of all included studies is provided in Appendix I.
Assessment of risk of bias of included studies
The “Risk of Bias” assessment for the included studies for each domain is presented in Fig. 2 and described below.
Fig 2.
Risk of bias summary.
Allocation
Risk of bias varied across studies. Nine studies, including eight with nonrandomized designs, were assessed as high risk of selection bias [26, 39, 43, 48, 49, 51, 52, 57, 61]. Thirteen studies, including four RCTs were assessed as unclear risk of selection bias as methods of sequence generation and allocation were not reported [44, 46, 47, 50, 51, 54–56, 58, 64, 66, 67]. While four studies were assessed as low risk of bias for random sequence generation, the method of allocation concealment was unclear [53, 60, 62, 63]. Two studies were assessed as low risk for both sequence generation and allocation concealment [27, 37].
Blinding
All studies were assessed as high risk of performance bias as study participants and personnel (e.g., school staff) were not blinded to group allocation. Detection bias varied across studies depending on whether implementation was assessed via self-report (high risk) or objective measures (low risk). Seventeen of the included studies were assessed as high risk [26, 28, 37, 41, 43, 44, 46–49, 52, 54–56, 58, 66, 67] and seven studies were assessed as low risk of detection bias [27, 42, 51, 53, 60, 62, 63]. The remaining five studies were assessed as unclear risk of detection bias due to insufficient information regarding the blinding of data collection staff provided [38, 50, 57, 59, 61].
Incomplete outcome data
The majority of studies (n = 23) were assessed as low risk of bias as either all or most participating schools were present at follow-up and/or sensitivity analyses were conducted to assess the impact of missing data. The risk of attrition was assessed as unclear in six studies, as insufficient information regarding the loss of schools and treatment of missing data were provided [26, 37, 41, 42, 54, 57]. One study was assessed as high risk of attrition due to untreated missing data at follow-up [46].
Selective reporting
Ten studies were assessed as low risk of selective reporting as a trial registration or a published protocol paper was identified and all a priori determined outcomes were reported [26, 44, 51, 53, 54, 60, 62–64, 67]. Two studies were classified as high risk for selective reporting as the implementation outcome was not previously registered in the available protocol or trial registration [37, 41]. For the remaining studies (n = 18), the risk of reporting bias was deemed unclear as a published protocol or trial registration was not identified.
Other potential sources of bias
For studies using a cluster-RCT design (n = 15), additional risk of bias domains were assessed. Potential risk of recruitment (to cluster) was assessed as low for seven studies as randomization occurred either postrecruitment or postbaseline data collection [47, 54–56, 58, 60, 64]. Seven studies were assessed as unclear [26, 37, 38, 41, 42, 46, 67], whilst the remaining study [27] was assessed as high risk of bias due to randomization occurring prior to recruitment and a lack of blinding of recruiters. For risk of bias due to baseline imbalances, the majority of studies (n = 11) were assessed as low risk as studies accounted for imbalances by making adjustments for baseline differences during analyses, stratifying by school characteristics or through random allocation of schools to experimental groups [37, 38, 41, 46, 47, 55, 56, 58, 60, 64, 67]. Three studies were assessed as high risk [26, 27, 42], while the remaining study [54] was at unclear risk of bias due to baseline imbalance. Four studies were assessed as high risk for loss of clusters [27, 38, 46, 60]. Three studies were high risk of bias due to incorrect analysis [42, 46, 58], while eight studies were assessed as low risk [27, 37, 38, 41, 54, 56, 64, 67] and the remaining studies (n = 4) at unclear risk [26, 47, 55, 60]. Risk of contamination was assessed as low for the majority of clustered studies (n = 11), with only two studies assessed as high [42, 55] and the remaining two studies unclear [26, 37].
The potential of confounding factors was assessed as an additional risk of bias domain for nonrandomized trial designs. Of the seven nonrandomized studies, three were considered as high risk of confounding [26, 52, 59], while it was unclear in the remaining five studies whether confounders had been sufficiently adjusted for [39, 43, 57, 61, 67].
Overall effect of implementation support on policy, practice, or program implementation
Of the 30 included studies, 19 reported significant improvements in at least one implementation outcome (including the one unpublished study) [44, 46–50, 52–58, 60–62, 64, 68]; 3 studies did not report any significant improvements in implementation [26, 43, 63] and 8 did not report any significance tests on such outcomes [27, 38, 39, 42, 51, 59, 66, 67].
Among 10 studies reporting dichotomous implementation strategy outcomes—the proportion of schools or school staff (e.g., classes) implementing a targeted policy, practice, or program—versus a minimal or usual practice control, the median unadjusted (improvement) effect size was 16.2% and ranged from –0.2% to 66.6% [27, 41, 50–53, 60, 62–64].
Six studies reported the percentage of an intervention program or program content that had been implemented, the effects of which were mixed [47, 55, 56, 58, 60, 61]. The unadjusted median effect, relative to the control in the proportion of program or program content implemented, was 23.65% (range –8% to 43%) [47, 55, 56, 58, 60, 61].
Four studies reported the impact of implementation strategies on the time per week that teachers spent implementing physical activity or physical education (PE) lessons, with improvements, relative to control ranging from 5.7 to 54.9 min per week (median = 36.6 min per week; including the one unpublished study) [38, 54, 57].
Among studies reporting other continuous implementation outcomes (e.g., quantity of physical activity lessons), findings were mixed [43, 44, 46, 48, 49, 59, 64, 66]. For example, across the three studies assessing the availability of fruit and vegetables within schools, the median effect size was 1.15 and ranged from 0.64 to 1.23 [42, 55, 58].
Substantial variability in the type of implementation strategies employed in the included studies prevented the impact of specific implementation support strategies, or combinations thereof, from being examined. However, most studies included educational meetings, educational materials in addition to other strategies. The effectiveness of such strategies to achieve improvements in measures of implementation were mixed.
Implementation of healthy eating policies, practices, and programs
Nineteen of the 30 included studies targeted the implementation of healthy eating practices (13 studies in primary, 4 in middle, and 2 in secondary schools). Studies to improve the implementation of healthy eating policies and practices were dominated by studies to improve the nutritional content or availability of healthy foods as part of U.S. school food services (n = 13). In general, such studies reported small improvements in food provision. For example, Cunningham et al. reported reductions in the percentage of energy from fat provided at school breakfast and lunch from –3.3% to –2.7% [44]. Percentage of fat in school meals was reported as reduced by up to 4% in the study by Heath and Coleman [48]. Similarly, in the study by Perry et al., modest although significant reductions were reported in the percentage of kilocalories from fat (–4.3%) and milligrams of sodium (–100.5) in school lunches [56].
Significant improvements were also reported across a range of measures of the percentage of food and beverage items meeting nutrient and portion criteria in a study by Whatley Blum et al. [61]. U.S. studies targeting improvements in the availability of fruits and vegetables in à la carte lines typically significantly increased the mean number of fruit and vegetables options available by between 0.5 to 1.37 [58] or the proportion of schools selling such foods by between 4% and 12% [50]. There was consistent evidence of large effects from Australian randomized trials demonstrating improvement in the availability of healthy foods at school canteens [53, 62, 63]. Three trials demonstrated a dose–response relationship between the intensity of implementation support and school compliance with canteen policies. In the trial by Wolfenden et al., assessing the most intensive implementation strategy—comprised of nine implementation strategies—more than 70% of schools that received multicomponent implementation support (vs. 3% in the control) did not regularly sell foods that were restricted or banned from sale by healthy canteen guidelines, and more than 80% (versus 27% in the control) had more than half of all foods for sale as healthy (“green”) products [62]. An Australian study also reported significant improvement relative to control (16%) in the implementation of fruit and vegetable breaks during class time [52]. Large changes were also reported in a small randomized trial (12 schools per group), in the presence of a written school nutrition or policy, but not canteen policy, in a trial by Waters et al. [27].
Implementation of physical activity policies, practices, and programs
Fourteen of the 30 included studies targeted the implementation of physical activity policies and practices (nine studies in primary, four in middle, and one in secondary school). Studies testing strategies to improve the implementation of physical activity policies and practices focused on measures of time that classroom teachers spent delivering PE or structured physical activity each week, the quality of PE lessons (e.g., lesson time allocated to children engaging in physical activity), or the implementation of specific elements of physical activity interventions [26, 27, 38, 39, 41, 46, 49, 54, 56, 57, 60, 64, 66]. Studies targeting the time spent on PE typically saw significant improvements following multistrategy implementation support [38, 54, 57]. For example, in their Canadian study, Naylor et al. reported significant improvements in classroom time spent on PE relative to control of up to 1 hr per week [54]. Similarly, one study by Nathan et al. found significant improvements in the minutes per day that teachers scheduled physical activity relative to control [37]. Sallis et al. found significant increases in the duration per week of PE lessons relative to control of 26.6 min and significant increases in the frequency of PE lessons a week [57]. However, Cheung et al. found far smaller changes in the mean minutes of physical activity offered per week, ranging from −2.4 to 13 min (significance not reported) [38].
Three studies compared implementation strategies to a usual care or minimal support control on measures of lesson quality [26, 56, 60]. Perry et al. reported a significant increase of 14% relative to control, in the proportion of quality activities observed, relative to control in PE lessons following implementation support [56]. Significant improvements were also reported in physical activity program quality score in an Australian randomized trial by Sutherland et al. [60] but not in measures of quality of PE lessons in a more recent study by Bremer et al. [26] among schools receiving implementation support. Among studies that assessed changes in the implementation of a physical activity policy, practice, or program [27, 41, 60, 64], effects were modest with median effect sizes ranging from no change (–0.2%) in the study by Farmer et al. [41] to a change of almost 20% in the Australian randomized trial by Sutherland et al. [60].
DISCUSSION
This review aimed to examine the impact of strategies to improve the implementation of policies, practices, and programs to promote healthy eating, physical activity, or prevent obesity within school-based settings. Despite the substantial number of efficacious school-based behavioral interventions published in the last 10 years [13, 69], and the increase in implementation science research during the same period, this review only identified an additional eight studies since the publication of the original review in 2017 [25]. Collectively, from the newly included studies and the 22 studies included in the original review by Wolfenden et al. [25], most studies employed randomized controlled trial designs to test multicomponent implementation support strategies. Despite considerable heterogeneity in the effects of implementation strategies, the findings provide some evidence to support the effectiveness of strategies in enhancing the nutritional quality of foods served at schools [61], implementation of canteen nutrition policies [62], improvements in the time scheduled for PE [57], and the quality of PE lessons [54]. Such evidence could provide some guidance for school-based settings and jurisdictions seeking to implement recommendations within the WHO Commission on Ending Childhood Obesity Report [11] and the WHO Health Promoting Schools Framework [70].
The median effect size of the primary implementation outcomes reported in this review (16.5%, range 0.2% to 66.6%) are comparable with implementation efforts in other community settings. For example, in a recent review of implementation strategies to improve healthy eating and physical activity promoting policies and practices in childcare, the median effect size in the proportion of staff implementing a policy or practice was 11% (range 2.5 to 33%) [35]. Similarly, in a review of strategies to improve healthy eating and physical activity policies and practices in workplaces, the median effect size in the proportion of workplaces implementing a policy or practice was 13.4% (range 10.9%–39.6%) [36]. Effect sizes and range of effects reported across these reviews suggests that implementation strategies typically yield modest but highly variable improvements in implementation. Such findings indicate that while it is possible to result in large improvements (up to 66.6% in this instance) in the implementation of policies and practices, the effects of implementation strategies are likely dependent on context, the factors impeding implementation, and the extent to which the selected implementation strategies adequately address these. Research to better identify the most potent mix of implementation supports given barriers and context, therefore, should be a priority for future research in the field.
While limited, there is an accumulating body of evidence to suggest that implementation strategies have resulted in small improvements in the availability and provision of healthy foods in schools [40, 44, 52]. Given that food consumed at school contributes to an estimated 40% of a child’s daily energy intake [71], small improvements in consumption could lead to important improvement in public health nutrition. For example, studies modeling the impact of reductions in energy intake have found a small decrease in energy intake of 290 kJ per day could be sufficient in preventing excessive weight gain in children [72]. Several studies within the review found significant reductions in energy from fat [44, 48, 56] and total energy [59] provided by lunch meals, in magnitudes exceeding 200 kJ, that could make a meaningful contribution to such reductions. The potential benefit of such improvements, however, is maximized when implementation occurs at scale. Disappointingly, just 5 of the 30 studies included in this review (including three targeting implementation of nutrition interventions) examined the impact of implementation occurring “at scale,” defined as 50 or more schools [37, 43, 52, 56, 73]. Effects were mixed among these studies, with three reporting significant improvements in the majority of implementation outcomes [37, 52, 56], whilst the remaining two studies reporting no improvement [38, 43]. As the effects of interventions may attenuate when delivered on a larger scale, the potential benefit of strategies to improve population-wide implementation of school health initiatives remains uncertain.
LIMITATIONS
Substantial variation across included studies in the implementation strategies employed, policies, practices, and programs targeted and measures used to assess implementation resulted in considerable challenges during data synthesis and interpretation of findings. Studies tested a range of multicomponent implementation strategies, with only two studies testing the same combination [26, 38]. As such, the impact of specific implementation support strategies or combinations thereof were unable to be examined. In contrast to a similar review conducted within the childcare setting [35] where a number of studies used similar score-based measures of implementation, enabling the pooling of studies for meta-analysis, such homogeneity in outcomes and measures was not evident within this review. Due to this, synthesizing the data and drawing comparisons between outcomes within this review was difficult. Additionally, with 18 studies recruiting a sample of less than 30 schools, 19 studies using nonvalidated self-reported measures of implementation, and all but 2 studies assessed as high risk of bias in multiple domains, the true improvements in policy and practice implementation may be unable to be detected. Finally, a lack of consistent terminology and inadequate reporting of employed implementation strategies across studies is an important limitation of this review.
Despite best efforts from the authors, the review process was not without its limitations. A search of international implementation journals and a hand search of reference lists of included studies was not conducted, which may have identified additional eligible studies to contribute to the findings of this review. Finally, the review extracted a limited range of the many trial characteristics, outcomes, and other structural or contextual factors that may influence implementation. Greater extraction and reporting of a broader range of such characteristics would improve the external validity and utility of the findings by the end user. As such, future reviews should consider coding and reporting studies using the Reach, Effectiveness, Adoption, Implementation and Maintenance (RE-AIM) framework [74, 75].
CONCLUSION
Despite the field of implementation science rapidly evolving and a considerable amount of research being conducted in the schools setting, a lack of strong and consistent evidence remains to support the selection of strategies to improve the implementation of healthy eating, physical activity, and obesity-prevention policies, practices, and programs. In the absence of clear evidence from empirical studies, researchers, and practitioners responsible for health promotion in school-based settings may have to rely on considerable formative research (e.g., consultation with schools to identify barriers and enablers) and theory to guide implementation. Future research calls for studies of high methodological quality using validated and consistent measures of implementation whilst adequately reporting employed implementation strategies using taxonomies, such as the EPOC [32] or Expert Recommendations for Implementing Change [76] taxonomies.
Supplementary Material
Acknowledgments
We would like to acknowledge the contributions made by Debbie Booth in refining the search strategy and conducting the search. Additionally, we would like to acknowledge the coauthors of the original review, Rebecca Wyse, Tessa Delaney, Alison Fielding, Flora Tzelepis, Tara Clinton-McHarg, Benjamin Parmenter, Peter Butler, John Wiggers, Adrian Bauman, Andrew Milat, and Christopher Williams.
Appendix A1
Summary of intervention, measures, and absolute intervention effect size in included studies
| Study | Targeted risk factor | Implementation strategies | Comparison | Primary implementation outcome and measures |
Effect size | Number of measures with significant result (p < .05) favoring the intervention |
|---|---|---|---|---|---|---|
| Alaimo et al. [43] | N | Clinical practice guidelines, educational materials, educational outreach visits or academic detailing, external funding, local consensus processes, tailored interventions | Usual practice or waitlist control |
Continuous: Nutrition policy score and nutrition education and/or practice score (two measures) |
Median (range): 0.65 (0.2 to 1.1) |
0/2 |
| Cunningham- Sabo et al. [44] |
N | Clinical practice guidelines, educational materials, educational meetings, educational outreach visits or academic detailing | Usual practice | Continuous: Nutrient content of school meals % of calories from fat breakfast/lunch (two measures) |
Median (range): −3% (−3.3% to −2.7%) |
1/2 |
| Delk et al. [46] | PA | Local consensus process, educational meetings, clinical practice guidelines, educational outreach visits or academic detailing, tailored interventions, other | Different implementation strategy |
Continuous: % of teachers that conducted activity breaks weekly (one measure, two comparisons) Dichotomous: % implementing a variety of policies and practices (two measures, four comparisons) |
Median (range): 13.3% (11.1% to 15.4%) Median (range): 26.5% (19.4% to 31.9%) |
6/6 |
| French et al. [47] | N | Local consensus processes, tailored intervention, educational meetings, pay for performance |
Usual practice or waitlist control |
Continuous % of program implementation (five measures) |
Median (range): 33% (11% to 41%) |
5/5 |
| Heath and Coleman [48] | N | Educational materials, educational meetings, educational outreach visits or academic detailing | Usual practice | Continuous: % fat in school meal (two measures) Sodium of school meals (two measures) |
Median (range): −1.7% (−4.4% to 1%) Median (range): −29.5 (−48 to −11) |
1/4 |
| Hoelscher et al. [49] |
N/PA | Educational materials, educational meetings, educational outreach visits or academic detailing, pay for performance, other, the use of information and communication technology, local consensus process | Different implementation strategy |
Continuous: Mean number of lessons/or activities (five measures) Dichotomous: % implementing a variety of policies and practices (two measures) |
Median (range): 0.8 (−0.4 to 1. 2) Median (range): 4.4% (3.6% to 5.2%) |
4/7 |
| Lytle et al. [50] | N | Educational materials, educational meetings, local opinion leaders, local consensus processes | Usual practice or waitlist control |
Dichotomous: % of schools offering or selling targeted foods (four measures) |
Median (range): 8.5% (4% to 12%) |
2/4 |
| Mobley et al. [51] | N | Educational games, educational meetings, external funding, tailored intervention, educational materials, educational outreach or academic detailing, other, the use of information and communication technology |
Usual practice or waitlist control |
Dichotomous: % schools meeting various nutrition goals (12 measures) |
Median (range): 15.5% (0% to 88%) |
NR |
| Nathan et al. [52] | N | Educational materials, educational meetings, local consensus processes, local opinion leaders, other, monitoring the performance of the delivery of the healthcare, tailored interventions | Minimal support control |
Dichotomous: % Schools implementing a vegetable and fruit break (one measure) |
Mean difference (95% CI): 16.2% (5.6% to 26.8%) |
1/1 |
| Nathan et al. [53] | N | Audit and feedback, continuous quality improvement, education materials, education meeting, local consensus process, local opinion leader, tailored intervention, other | Usual practice | Dichotomous: % implementing a variety of policies and practices (two measures) |
Median (range): 35.5% (30.0% to 41.1%) |
2/2 |
| Naylor et al. [54] | PA | Educational materials, educational meetings, educational outreach meetings or academic detailing, local consensus process, other, tailored interventions | Usual practice or waitlist control |
Continuous: Minutes per week of physical activity implemented in the classroom (one measure, two comparisons) |
Median (range): 54.9 min (46.4 to 63.4) |
2/2 |
| Perry et al. [56] | N/PA | Educational materials, educational meetings, educational outreach visits or academic detailing, other | Usual practice or waitlist control |
Continuous: % of kilocalories from fat in school lunch (one measure) Mean milligrams of sodium in lunches (one measure) Cholesterol milligrams in lunches (one measure) Quality of PE lesson % of seven activities observed (one measure) |
Mean difference (95%CI): −4.3% (−5.8% to −2.8%) Mean difference (95% CI): −100.5 (−167.6 to −33.4) Mean difference (95% CI): −8.3 (−16.7 to 0.1) Mean difference (95% CI): 14.3% (11.6% to 17.0%) |
3/4 |
| Perry et al. [55] | N | Educational meetings, educational outreach visits or academic detailing, educational materials, local consensus processes, other | Usual practice or waitlist control |
Continuous: % of program implementation (two measures) Mean number of fruit and vegetables available (two measures) |
Median (range): 14% (−2% to 30%) Median (range): 0.64 (0.48 to 0.80) |
2/4 |
| Sallis et al. [57] | PA | Educational materials, educational meetings, educational outreach visits or academic detailing, length of consultation, other | Usual practice or waitlist control |
Continuous: Duration (minutes) per week of physical education lessons (one measure) Frequency (per week) of physical education lessons (one measures) |
Mean difference (95% CI): 26.6 (15.3 to 37.9) Mean difference (95% CI): 0.8 (0.3 to 1.3) |
2/2 |
| Saunders et al. [66] | PA | Educational materials, educational meetings, educational outreach visits or academic detailing, local consensus processes, local opinion leaders, other | Usual practice or waitlist control |
Continuous: School level policy and practice related to physical activity (nine measures) |
N/A | NR |
| Simons- Morton et al. [59] |
N | Educational materials, educational outreach visits or academic detailing, local consensus processes, local opinion leaders, managerial supervision, monitoring of performance, other | Usual practice | Continuous: Macronutrient content of school meals (two measures) |
N/A | NR |
| Story et al. [58] | N | Educational meetings, other | Usual practice | Continuous: Mean number of fruit and vegetables available (two measures) % of guidelines implemented and % of promotions held (four measures) |
Median (range): 1.15 (1 to 1.3) Median (range): 38.4% (28.5% to 43.8%) |
6/6 |
| Sutherland et al. [60] | PA | Audit and feedback, education materials, education meeting, education outreach visits or academic detailing, local opinion leader, other | Usual practice or waitlist control |
Dichotomous: % implementing a variety of policies and practices (two measures) Continuous: Physical education lesson quality score (one measures) % of program implementation (four measures) |
Median (range): 19% (16% to 22%) Mean difference: 21.5 Median (range): −8% (−18% to 2%) |
0/2 1/1 0/4 |
| Whatley Blum et al. [61] | N | Clinical practice guidelines, educational materials, educational meetings, educational outreach visits or academic detailing, external funding, distribution of supplies, local consensus process, other | Usual practice or waitlist control |
Continuous: % of food and beverage items meeting guideline nutrient and portion criteria (six measures) |
Median (range): 42.95% (15.7% to 60.6%) |
5/6 |
| Wolfenden et al. [62] | N | Audit and feedback, continuous quality improvement, external funding, education materials, education meeting, education outreach visits or academic detailing, local consensus process, local opinion leader, tailored intervention | Usual practice | Dichotomous: % implementing a variety of policies and practices (two measures) |
Median (range): 66.6% (60.5% to 72.6%) |
2/2 |
| Yoong et al. [63] | N | Audit and feedback, continuous quality improvement, education materials, tailored intervention | Usual practice | Dichotomous: % implementing a variety of policies and practices (two measures) |
Median (range): 21.6% (15.6% to 27.5%) |
0/2 |
| Young et al. [64] | PA | Education materials, education meetings, educational outreach visits or academic detailing, interprofessional education, local consensus processes, local opinion leaders | Usual practice | Dichotomous: % implementing a variety of policies and practices (seven measures) Continuous: Average number of physical activity programs taught (one measure) |
Median (range): 9.3% (−6.8% to 55.5%) Effect size (95% CI): 5.1 (−0.4 to 10.6) |
1/8 |
| New studies identified in this review | ||||||
| Bremer et al. [26] | PA | Educational meetings, educational materials | Usual practice | Continuous: Quantity of physical education lessons (one measure) |
Mean difference: t(27) = −0.23, |
0/1 |
| Cheung et al. [38] | PA | Educational meeting, educational materials | Usual practice | Continuous: Mean minutes of physical activity offered per week (three measures) |
Median (range): 5.7 (−2.4 to 13) |
NR |
| Egan et al. [39] |
PA | Educational materials; educational outreach visit or academic detailing, tailored intervention, audit, and feedback | Alternate intervention or usual practice | Continuous:Mean implementation score for components of movement integration (five measures) | Median (range): −2.79 (−4.92 to 3.66) |
NR |
| Evenhuis et al. [40] | N | Educational materials, educational meeting, audit with feedback, educational outreach visit or academic detailing | Educational materials | Continuous: Availability of healthier food products on display (one measure) Healthier product accessibility (one measure) |
Mean difference: 16.79 Mean difference: 9 |
NR |
| Farmer et al. [41] | PA | Incentives, local consensus approach, tailored interventions | Usual practice | Dichotomous: % implementing a variety of policies and practices (one measure) Continuous: Provision of play opportunities (one measure) |
Mean difference (95% CI): −0.20 (−11.46 to 11.06) Mean difference (95% CI): 4.50 (1.82 to 7.18) |
0/1 1/1 |
| Nathan, unpublished data | PA | Educational outreach visits, centralized technical support, mandate change, identify and prepare champions, provide ongoing consultation, educational material | Usual practice | Continuous: Mean minutes of teacher’s scheduled PA per day |
Mean difference (95% CI): 36.60 (2.68 to 70.51) | 1/1 |
| Taylor et al. [42] | N | Incentives, educational materials, educational outreach visits, or academic detailing | Usual practice or waitlist control |
Continuous: Quantity of fruit and vegetables available (two measures) |
Median (range): 1.23 (−0.79 to 3.26) |
NR |
| Waters et al. [27] | N/PA | Educational materials, educational outreach visits or academic detailing; local consensus approach, tailored interventions | Usual practice | Dichotomous: % implementing a variety of policies and practices (three measures) |
Median (range): 7% (−11.7% to 15%) |
NR |
CI confidence interval; N nutrition; NR not reported; PA physical activity.
Appendix A2
Search StrategyDatabase(s): Ovid MEDLINE(R) and Epub ahead of print, in-process and other nonindexed citations and daily 1946 to April 10, 2019 Search strategy:
| # | Searches | Results |
|---|---|---|
| 1 | schools/ | 34,641 |
| 2 | ((primary or elementary or middle or junior or high or secondary) adj (school* or student*)).mp. | 61,499 |
| 3 | kinder*.mp. | 22,544 |
| 4 | 1 or 2 or 3 | 106,292 |
| 5 | implement*.tw. | 427,155 |
| 6 | Health Promotion/mt [Methods] | 19,229 |
| 7 | “Outcome and Process Assessment (Health Care)”/ | 25,691 |
| 8 | “Process Assessment (Health Care)”/ | 4,389 |
| 9 | “Outcome Assessment (Health Care)”/ | 67,208 |
| 10 | Program Evaluation/ | 59,115 |
| 11 | Interrupted Time Series Analysis/ | 553 |
| 12 | dissemin*.tw. | 115,236 |
| 13 | adopt*.tw. | 220,568 |
| 14 | practice.tw. | 634,669 |
| 15 | organi?ational change*.tw. | 2,613 |
| 16 | diffus*.tw. | 353,856 |
| 17 | (system* adj2 change*).tw. | 15,325 |
| 18 | quality improvement*.tw. | 30,437 |
| 19 | transform*.tw. | 452,648 |
| 20 | translat*.tw. | 283,791 |
| 21 | transfer*.tw. | 594,534 |
| 22 | uptake*.tw. | 335,586 |
| 23 | sustainab*.tw. | 55,964 |
| 24 | institutionali*.tw. | 14,726 |
| 25 | routin*.tw. | 355,436 |
| 26 | maintenance.tw. | 254,465 |
| 27 | capacity.tw. | 460,913 |
| 28 | incorporat*.tw. | 395,520 |
| 29 | adher*.tw. | 172,945 |
| 30 | ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).tw. | 103,076 |
| 31 | integrat*.tw. | 460,724 |
| 32 | scal* up.tw. | 16,615 |
| 33 | 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 | 4,833,658 |
| 34 | exp Obesity/ | 195,8011 |
| 35 | Weight Gain/ | 29,698 |
| 36 | exp Weight Loss/ | 38,540 |
| 37 | obes*.tw. | 269,101 |
| 38 | (weight gain or weight loss).tw. | 130,488 |
| 39 | (overweight or over weight or overeat* or over eat*).tw. | 64,358 |
| 40 | weight change*.tw. | 10,275 |
| 41 | ((bmi or body mass index) adj2 (gain or loss or change)).tw. | 4,130 |
| 42 | exp Primary Prevention/ | 143,568 |
| 43 | (primary prevention or secondary prevention).tw. | 30,738 |
| 44 | (preventive measure* or preventative measure*).tw. | 22,909 |
| 45 | (preventive care or preventative care).tw. | 5,038 |
| 46 | (obes* adj2 (prevent* or treat*)).tw. | 19,978 |
| 47 | 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 | 633,369 |
| 48 | exp Exercise/ | 176,978 |
| 49 | physical activity.tw. | 94,644 |
| 50 | physical inactivity.tw. | 6,883 |
| 51 | Motor Activity/ | 94,188 |
| 52 | (“physical education” or “physical training”).tw. | 9,495 |
| 53 | “Physical Education and Training”/ | 13,213 |
| 54 | Physical Fitness/ | 26,208 |
| 55 | sedentary.tw. | 27,694 |
| 56 | exp Life Style/ | 85,835 |
| 57 | exp Leisure Activities/ | 220,470 |
| 58 | Dancing/ | 2,669 |
| 59 | dancing.tw. | 1,576 |
| 60 | (exercise* adj aerobic*).tw. | 186 |
| 61 | sport*.tw. | 66,644 |
| 62 | ((lifestyle* or life style*) adj5 activ*).tw. | 6,082 |
| 63 | 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 | 547,175 |
| 64 | exp Diet/ | 261,598 |
| 65 | nutrition*.tw. | 248,427 |
| 66 | healthy eating.tw. | 5,898 |
| 67 | Child Nutrition Sciences/ | 1,075 |
| 68 | fruit*.tw. | 95,658 |
| 69 | vegetable*.tw. | 49,588 |
| 70 | “Fruit and Vegetable Juices”/ | 1,248 |
| 71 | canteen*.tw. | 589 |
| 72 | food service*.tw. | 1,810 |
| 73 | menu*.tw. | 4,561 |
| 74 | calorie*.tw. | 24,033 |
| 75 | Energy Intake/ | 38,728 |
| 76 | energy density.tw. | 8,494 |
| 77 | Eating/ | 50,500 |
| 78 | Feeding Behavior/ or feeding behavio?r*.tw. | 81,927 |
| 79 | dietary intake.tw. | 21,918 |
| 80 | Food Habits/ | 77,114 |
| 81 | Food/ | 31,390 |
| 82 | Carbonated Beverages/ or soft drink*.mp. | 5,116 |
| 83 | soda.tw. | 3,799 |
| 84 | sweetened drink*.tw. | 262 |
| 85 | Dietary Fats, Unsaturated/ or Dietary Fats/ | 51,350 |
| 86 | confectionar*.tw. | 240 |
| 87 | (school adj (lunch* or meal*)).tw. | 1,439 |
| 88 | menu plan*.tw. | 184 |
| 89 | ((feeding or food or nutrition*) adj program*).tw. | 4,133 |
| 90 | cafeteria*.tw. | 1,848 |
| 91 | Nutritional Status/ | 40,791 |
| 92 | 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 | 741,173 |
| 93 | exp Smoking/ | 140,042 |
| 94 | exp “Tobacco Use Cessation”/ | 1,064 |
| 95 | smok*.tw. | 258,516 |
| 96 | Nicotine/ | 24,526 |
| 97 | Tobacco/ or “Tobacco Use”/ | 30,560 |
| 98 | ((ceas* or cess* or prevent* or stop* or quit* or abstin* or abstain* or reduc*) adj5 (smok* or tobacco or nicotine)).tw. | 51,511 |
| 99 | “Tobacco Use Disorder”/ | 10,617 |
| 100 | ex-smoker*.tw. | 3,769 |
| 101 | anti-smok*.tw. | 1,225 |
| 102 | 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 | 335,144 |
| 103 | alcohol drinking/ or binge drinking/ | 64,411 |
| 104 | alcohol*.tw. | 308,065 |
| 105 | Alcoholic Intoxication/ or Alcoholism/ | 82,939 |
| 106 | drink*.tw. | 128,749 |
| 107 | liquor*.tw. | 7,780 |
| 108 | beer*.tw. | 9,611 |
| 109 | wine*.tw. | 18,647 |
| 110 | spirit*.tw. | 24,880 |
| 111 | drunk*.tw. | 4,203 |
| 112 | intoxicat*.tw. | 44,075 |
| 113 | binge.tw. | 11,829 |
| 114 | 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 | 508,479 |
| 115 | 47 or 63 or 92 or 102 or 114 | 2,374,155 |
| 116 | Randomized Controlled Trial/ | 479,844 |
| 117 | clinical trial/ or controlled clinical trial/ | 537,645 |
| 118 | random allocation/ | 98,475 |
| 119 | Double-Blind Method/ | 150,664 |
| 120 | Single-Blind Method/ | 26,573 |
| 121 | placebos/ | 34,301 |
| 122 | Research Design/ | 100,656 |
| 123 | Evaluation Studies/ | 242,326 |
| 124 | Comparative Study/ | 1,826,707 |
| 125 | exp Longitudinal Studies/ | 1,22,430 |
| 126 | Cross-Over Studies/ | 45,007 |
| 127 | exp Cohort studies/ | 1,844,224 |
| 128 | Controlled Before-After Studies/ | 383 |
| 129 | Interrupted Time Series Analysis/ | 553 |
| 130 | comparative study.pt. | 1,826,707 |
| 131 | clinical trial.tw. | 125,184 |
| 132 | latin square.tw. | 4,495 |
| 133 | (time adj series).tw. | 26,782 |
| 134 | (before adj2 after adj3 (stud* or trial* or design*)).tw. | 12,708 |
| 135 | ((singl* or doubl* or trebl* or tripl*) adj5 (blind* or mark)).tw. | 160,930 |
| 136 | placebo*.tw. | 202,959 |
| 137 | random*.tw. | 1,038,274 |
| 138 | (matched adj (communit* or school* or population*)).tw. | 2,305 |
| 139 | control*.tw. | 3,546,542 |
| 140 | (comparison group* or control group*).tw. | 434,335 |
| 141 | matched pairs.tw. | 5,809 |
| 142 | outcome stud*.tw. | 7,564 |
| 143 | (qua?iexperimental or qua?i experimental or pseudo experimental).tw. | 11,696 |
| 144 | (nonrandomi?ed or non randomi?ed or psuedo randomi?ed or quasi randomi?ed).tw. | 26,473 |
| 145 | prospectiv*.tw. | 638,036 |
| 146 | volunteer*.tw. | 182,708 |
| 147 | 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 or 137 or 138 or 139 or 140 or 141 or 142 or 143 or 144 or 145 or 146 | 7,432,338 |
| 148 | exp adolescent/ or child/ | 2,671,427 |
| 149 | (child or children or adolescen* or teen*).tw. | 1,276,835 |
| 150 | 148 or 149 | 3,119,058 |
| 151 | 4 and 33 and 115 and 147 and 150 | 4,111 |
| 152 | limit 151 to ed=20160901-20190412 | 823 |
DATABASE(S): EMBASE 1947 TO PRESENT SEARCH STRATEGY:
| # | Searches | Results |
|---|---|---|
| 1 | schools/ | 63,598 |
| 2 | ((primary or elementary or middle or junior or high or secondary) adj (school* or student*)).mp. | 83,026 |
| 3 | kinder*.mp. | 32,382 |
| 4 | 1 or 2 or 3 | 166,381 |
| 5 | implement*.tw. | 557,138 |
| 6 | dissemin*.tw. | 158,810 |
| 7 | adopt*.tw. | 281,184 |
| 8 | practice.tw. | 870,432 |
| 9 | organi?ational change*.tw. | 3,193 |
| 10 | diffus*.tw. | 478,311 |
| 11 | system* change*.tw. | 8,902 |
| 12 | quality improvement*.tw. | 46,116 |
| 13 | transform*.tw. | 535,815 |
| 14 | translat*.tw. | 350,917 |
| 15 | transfer*.tw. | 714,912 |
| 16 | uptake*.tw. | 442,073 |
| 17 | sustainab*.tw. | 67,481 |
| 18 | institutionali*.tw. | 19,660 |
| 19 | routin*.tw. | 539,589 |
| 20 | maintenance.tw. | 351,213 |
| 21 | capacity.tw. | 602,641 |
| 22 | incorporat*.tw. | 494,048 |
| 23 | adher*.tw. | 252,374 |
| 24 | ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).tw. | 141,527 |
| 25 | integrat*.tw. | 561,121 |
| 26 | scal* up.tw. | 20,866 |
| 27 | health care quality/ | 231,534 |
| 28 | quality control/ | 170,122 |
| 29 | program evaluation/ | 12,357 |
| 30 | total quality management/ | 55,032 |
| 31 | 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 | 6,381,792 |
| 32 | exp Obesity/ | 482,160 |
| 33 | Weight Gain/ | 91,702 |
| 34 | Weight Loss.tw. or exp weight reduction/ | 135,406 |
| 35 | obes*.tw. | 406,493 |
| 36 | (weight gain or weight loss).tw. | 200,827 |
| 37 | (overweight or over weight or overeat* or over eat*).tw. | 97,808 |
| 38 | weight change*.tw. | 15,239 |
| 39 | ((bmi or body mass index) adj2 (gain or loss or change)).tw. | 6,986 |
| 40 | exp Primary Prevention/ | 37,972 |
| 41 | (primary prevention or secondary prevention).tw. | 46,930 |
| 42 | (preventive measure* or preventative measure*).tw. | 32,787 |
| 43 | (preventive care or preventative care).tw. | 6,298 |
| 44 | (obes* adj2 (prevent* or treat*)).tw. | 28,499 |
| 45 | 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 | 850,700 |
| 46 | exp Exercise/ | 336,319 |
| 47 | physical activity.tw. or exp physical activity/ | 433,582 |
| 48 | physical inactivity.tw. | 9,388 |
| 49 | exp Motor Activity/ | 536,018 |
| 50 | (“physical education” or “physical training”).tw. | 13,789 |
| 51 | physical education/ | 13,316 |
| 52 | physical fitness.tw. or fitness/ | 41,592 |
| 53 | sedentary.tw. | 37,170 |
| 54 | lifestyle/ | 104,759 |
| 55 | Leisure Activit*.tw. or leisure/ | 34,038 |
| 56 | exp Sports/ | 157,505 |
| 57 | Dancing/ | 4,479 |
| 58 | (dance* or dancing).tw. | 8,367 |
| 59 | (exercise* adj2 aerobic*).tw. | 12,926 |
| 60 | sport*.tw. | 91,539 |
| 61 | ((lifestyle* or life style*) adj5 activ*).tw. | 8,789 |
| 62 | 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 | 1,385,883 |
| 63 | exp Diet/ | 340,795 |
| 64 | nutrition*.tw. or nutrition/ | 386,929 |
| 65 | (health* adj2 eat*).tw. | 10,407 |
| 66 | nutritional science/ | 5,719 |
| 67 | fruit*.mp. or fruit/ or “fruit and vegetable juice”/ | 143,342 |
| 68 | vegetable*.tw. or vegetable/ | 76,624 |
| 69 | canteen*.tw. | 978 |
| 70 | Food Services.tw. or catering service/ | 18,558 |
| 71 | menu*.tw. | 5,961 |
| 72 | (calorie or calories or kilojoule*).tw. | 36,880 |
| 73 | Energy Intake.tw. or caloric intake/ | 64,139 |
| 74 | energy density.tw. | 6,365 |
| 75 | Eating/ | 35,119 |
| 76 | Feeding Behavior/ or feeding behavio?r*.tw. | 86,486 |
| 77 | dietary intake.tw. or dietary intake/ | 86,822 |
| 78 | Food Habits/ | 67,209 |
| 79 | Food/ | 91,993 |
| 80 | Carbonated Beverages/ or soft drink*.mp. | 6,974 |
| 81 | soda.tw. | 5,149 |
| 82 | sweetened drink*.tw. | 360 |
| 83 | Dietary Fats, Unsaturated/ or Dietary Fats/ | 48,641 |
| 84 | confectionar*.tw. | 341 |
| 85 | (school adj (lunch* or meal*)).tw. | 1,836 |
| 86 | ((feeding or food or nutrition*) adj program*).tw. | 5,015 |
| 87 | cafeteria*.tw. | 2,308 |
| 88 | Nutritional Status/ | 62,601 |
| 89 | 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 | 1,089,562 |
| 90 | exp Smoking/ | 368,685 |
| 91 | exp “Tobacco Use Cessation”/ | 54,469 |
| 92 | smok*.tw. | 382,866 |
| 93 | Nicotine/ | 47,085 |
| 94 | Tobacco/ or “Tobacco Use”/ | 54,004 |
| 95 | ((ceas* or cess* or prevent* or stop* or quit* or abstin* or abstain* or reduc*) adj5 (smok* or tobacco or nicotine)).tw. | 66,147 |
| 96 | “Tobacco Use Disorder”/ | 7,394 |
| 97 | ex-smoker*.tw. | 6,694 |
| 98 | anti-smok*.tw. | 1,588 |
| 99 | 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 | 545,883 |
| 100 | alcohol drinking/ or binge drinking/ | 40,705 |
| 101 | alcohol*.tw. | 442,943 |
| 102 | Alcoholic Intoxication/ or Alcoholism/ | 133,150 |
| 103 | drink*.tw. | 178,445 |
| 104 | liquor*.tw. | 12,281 |
| 105 | beer*.tw. | 13,964 |
| 106 | wine*.tw. | 23,346 |
| 107 | spirit*.tw. | 32,568 |
| 108 | drunk*.tw. | 6,026 |
| 109 | intoxicat*.tw. | 66,687 |
| 110 | binge.tw. | 16,608 |
| 111 | 100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 | 716,291 |
| 112 | 45 or 62 or 89 or 99 or 111 | 3,879,229 |
| 113 | Randomized Controlled Trial/ | 544,426 |
| 114 | clinical trial/ or controlled clinical trial/ | 1,037,260 |
| 115 | random allocation/ | 78,229 |
| 116 | Double-Blind Method/ | 126,778 |
| 117 | Single-Blind Method/ | 32,642 |
| 118 | placebos/ | 285,441 |
| 119 | Research Design/ | 1,626,031 |
| 120 | Intervention Studies/ | 31,912 |
| 121 | Evaluation Studies/ | 38,259 |
| 122 | Comparative Study/ | 835,481 |
| 123 | exp Longitudinal Studies/ | 124,566 |
| 124 | Cross-Over Studies/ | 48,369 |
| 125 | clinical trial.tw. | 183,772 |
| 126 | latin square.tw. | 4,848 |
| 127 | (time adj series).tw. | 30,180 |
| 128 | (before adj2 after adj3 (stud* or trial* or design*)).tw. | 17,774 |
| 129 | ((singl* or doubl* or trebl* or tripl*) adj5 (blind* or mark)).tw. | 226,356 |
| 130 | placebo*.tw. | 291,972 |
| 131 | random*.tw. | 1,404,881 |
| 132 | (matched adj (communit* or school* or population*)).tw. | 3,301 |
| 133 | control*.tw. | 4,744,140 |
| 134 | (qua?iexperimental or qua?i experimental or pseudo experimental).tw. | 14,109 |
| 135 | (nonrandomi?ed or non randomi?ed or psuedo randomi?ed or quasi randomi?ed).tw. | 35,465 |
| 136 | prospectiv*.tw. | 970,850 |
| 137 | volunteer*.tw. | 248,636 |
| 138 | cohort analysis/ or cohort studies/ | 452,474 |
| 139 | 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 or 137 or 138 | 9,238,197 |
| 140 | school child/ | 343,648 |
| 141 | adolescent/ | 1,559,797 |
| 142 | (child or children or adolescen* or teen*).tw. | 1,768,364 |
| 143 | 140 or 141 or 142 | 2,887,338 |
| 144 | 4 and 31 and 112 and 139 and 143 | 4,962 |
| 145 | limit 144 to dd=20160901-20190412 | 688 |
DATABASE(S): PSYCINFO 1806 TO APRIL WEEK 2 2019 SEARCH STRATEGY:
| # | Searches | Results |
|---|---|---|
| 1 | schools/ | 28,501 |
| 2 | ((primary or elementary or middle or junior or high or secondary) adj (school* or student*)).mp. | 187,658 |
| 3 | kinder*.mp. | 25,418 |
| 4 | 1 or 2 or 3 | 229,493 |
| 5 | implement*.tw. | 162,915 |
| 6 | Dissemin*.tw. | 10,234 |
| 7 | adopt*.tw. | 87,104 |
| 8 | practice.tw. | 316,893 |
| 9 | organi?ational change*.tw. | 7,087 |
| 10 | diffus*.tw. | 28,195 |
| 11 | system* change*.tw. | 3,736 |
| 12 | quality improvement*.tw. | 4,661 |
| 13 | transform*.tw. | 73,504 |
| 14 | translat*.tw. | 53,620 |
| 15 | transfer*.tw. | 69,749 |
| 16 | uptake*.tw. | 14,796 |
| 17 | sustainab*.tw. | 18,291 |
| 18 | institutionali*.tw. | 16,494 |
| 19 | routin*.tw. | 44,817 |
| 20 | maintenance.tw. | 57,427 |
| 21 | capacity.tw. | 77,478 |
| 22 | incorporat*.tw. | 78,384 |
| 23 | adher*.tw. | 34,556 |
| 24 | ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).tw. | 87,456 |
| 25 | integrat*.tw. | 216,469 |
| 26 | scal* up.tw. | 1,994 |
| 27 | Quality Control/ | 1,438 |
| 28 | quality of services/ | 6,031 |
| 29 | program evaluation/ | 12,201 |
| 30 | 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 | 1,137,067 |
| 31 | exp Obesity/ | 22,903 |
| 32 | Weight Gain/ | 2,925 |
| 33 | exp Weight Loss/ | 3,426 |
| 34 | obes*.tw. | 38,244 |
| 35 | (weight gain or weight loss).tw. | 19,875 |
| 36 | (overweight or over weight or overeat* or over eat*).tw. | 16,413 |
| 37 | weight change*.tw. | 2,122 |
| 38 | ((bmi or body mass index) adj2 (gain or loss or change)).tw. | 764 |
| 39 | (primary prevention or secondary prevention).tw. | 5,844 |
| 40 | (preventive measure* or preventative measure*).tw. | 2,815 |
| 41 | (preventive care or preventative care).tw. | 1,198 |
| 42 | (obes* adj2 (prevent* or treat*)).tw. | 4,884 |
| 43 | 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 | 65,396 |
| 44 | exp Exercise/ | 24,563 |
| 45 | physical activity.tw. | 31,222 |
| 46 | physical inactivity.tw. | 1,843 |
| 47 | (“physical education” or “physical training”).tw. | 6,220 |
| 48 | Physical Fitness/ | 4,077 |
| 49 | sedentary.tw. | 6,296 |
| 50 | exp Sports/ | 24,756 |
| 51 | Dance/ | 2,120 |
| 52 | (dance* or dancing).tw. | 7,867 |
| 53 | (exercise* adj2 aerobic*).tw. | 2,033 |
| 54 | sport*.tw. | 33,287 |
| 55 | ((lifestyle* or life style*) adj5 activ*).tw. | 2,255 |
| 56 | 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 | 98,946 |
| 57 | nutrition*.tw. | 24,725 |
| 58 | (health* adj2 eat*).tw. | 3,701 |
| 59 | fruit*.tw. | 17,266 |
| 60 | vegetable*.tw. | 5,508 |
| 61 | canteen*.tw. | 132 |
| 62 | food service*.tw. | 521 |
| 63 | (diet* or food habits or fat or menu*).tw. | 51,336 |
| 64 | (calorie or calories or kilojoule*).tw. | 3,936 |
| 65 | Food Intake/ | 14,041 |
| 66 | energy density.tw. | 300 |
| 67 | Eating/ | 11,764 |
| 68 | Feeding Behavior/ or feeding behavio?r*.mp. | 11,191 |
| 69 | dietary intake.tw. | 2,104 |
| 70 | Food/ | 13,443 |
| 71 | Carbonated Beverages/ or soft drink*.mp. | 684 |
| 72 | soda.tw. | 418 |
| 73 | sweetened drink*.tw. | 52 |
| 74 | confectionar*.tw. | 40 |
| 75 | (school adj (lunch* or meal*)).tw. | 538 |
| 76 | ((feeding or food or nutrition*) adj program*).tw. | 988 |
| 77 | cafeteria*.tw. | 720 |
| 78 | 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 | 114,688 |
| 79 | smok*.tw. | 52,934 |
| 80 | Nicotine/ | 10,600 |
| 81 | Tobacco smoking/ | 29,571 |
| 82 | ((ceas* or cess* or prevent* or stop* or quit* or abstin* or abstain* or reduc*) adj5 (smok* or tobacco or nicotine)).tw. | 22,093 |
| 83 | “Tobacco Use Disorder”/ | 198 |
| 84 | ex-smoker*.tw. | 712 |
| 85 | anti-smok*.tw. | 540 |
| 86 | 79 or 80 or 81 or 82 or 83 or 84 or 85 | 60,113 |
| 87 | alcohol drinking/ or binge drinking/ | 2,226 |
| 88 | alcohol*.tw. | 125,592 |
| 89 | Alcoholic Intoxication/ or Alcoholism/ | 29,153 |
| 90 | drink*.tw. | 50,966 |
| 91 | liquor*.tw. | 890 |
| 92 | beer*.tw. | 2,708 |
| 93 | wine*.tw. | 2,634 |
| 94 | spirit*.tw. | 47,011 |
| 95 | drunk*.tw. | 3,653 |
| 96 | intoxicat*.tw. | 9,133 |
| 97 | binge.tw. | 11,559 |
| 98 | 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 | 200,599 |
| 99 | 43 or 56 or 78 or 86 or 98 | 458,108 |
| 100 | clinical trial/ or controlled clinical trial/ | 11,288 |
| 101 | placebo/ | 5,228 |
| 102 | Research Design/ | 10,996 |
| 103 | Intervention/ | 58,664 |
| 104 | exp Longitudinal Studies/ | 16,128 |
| 105 | ((Cross-Over or evaluation or comparative) adj Stud*).tw. | 17,808 |
| 106 | clinical trial.tw. | 13,637 |
| 107 | latin square.tw. | 493 |
| 108 | (time adj series).tw. | 7,680 |
| 109 | (before adj2 after adj3 (stud* or trial* or design*)).tw. | 2,286 |
| 110 | ((singl* or doubl* or trebl* or tripl*) adj5 (blind* or mark)).tw. | 24,988 |
| 111 | placebo*.tw. | 38,937 |
| 112 | random*.tw. | 187,356 |
| 113 | (matched adj (communit* or school* or population*)).tw. | 424 |
| 114 | control*.tw. | 658,383 |
| 115 | comparison group*.tw. | 12,778 |
| 116 | matched pairs.tw. | 1,272 |
| 117 | outcome stud*.tw. | 4,759 |
| 118 | (qua?iexperimental or qua?i experimental or pseudo experimental).tw. | 10,839 |
| 119 | (nonrandomi?ed or non randomi?ed or psuedo randomi?ed or quasi randomi?ed).tw. | 2,226 |
| 120 | prospectiv*.tw. | 64,156 |
| 121 | volunteer*.tw. | 37,238 |
| 122 | 100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 | 945,144 |
| 123 | (child or children or adolescen* or teen*).tw. | 754,758 |
| 124 | 4 and 30 and 99 and 122 and 123 | 1,049 |
| 125 | limit 124 to up=20160901-20190412 | 184 |
CUMULATIVE INDEX TO NURSING AND ALLIED HEALTH LITERATURE
| # | Query | Results |
|---|---|---|
| S1 | (MH “Schools”) OR (MH “Schools, Elementary”) OR (MH “Schools, Middle”) OR (MH “Schools, Secondary”) | 20,192 |
| S2 | ((primary or elementary or middle or junior or high or secondary) n1 (school* or student*)) | 42,756 |
| S3 | kinder* | 3,121 |
| S4 | S1 OR S2 OR S3 | 54,176 |
| S5 | implement* | 163,174 |
| S6 | dissemin* | 19,963 |
| S7 | adopt* | 54,029 |
| S8 | ((polic* or practice* or program* or innovation*) n5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or “social market*” or “professional development” or network* or leadership or “opinion leader*” or “consensus process*” or “change manage*” or train* or audit*)) | 60,829 |
| S9 | “organi?ational change*” | 12,260 |
| S10 | diffus* | 40,947 |
| S11 | “system* change*” | 2,038 |
| S12 | “quality improvement*” | 52,948 |
| S13 | transform* | 37,570 |
| S14 | translat* | 47,031 |
| S15 | transfer* | 68,493 |
| S16 | uptake* | 33,290 |
| S17 | sustainab* | 15,336 |
| S18 | institutionali* | 7,551 |
| S19 | routin* | 77,827 |
| S20 | maintenance | 45,478 |
| S21 | capacity | 61,690 |
| S22 | incorporat* | 52,472 |
| S23 | adher* | 55,246 |
| S24 | practice | 565,324 |
| S25 | integrat* | 108,963 |
| S26 | “scal* up” | 3,043 |
| S27 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 | 1,209,243 |
| S28 | (MH “Obesity+”) | 84,796 |
| S29 | (MH “Weight Gain”) | 10,596 |
| S30 | (MH “Weight Loss”) | 18,829 |
| S31 | obes* | 113,508 |
| S32 | (“weight gain” or “weight loss”) | 45,507 |
| S33 | (overweight or “over weight” or overeat* or “over eat*”) | 26,427 |
| S34 | “weight change*” | 3,356 |
| S35 | ((bmi or body mass index) n2 (gain or loss or change)) | 2,901 |
| S36 | “Primary Prevention” | 5,678 |
| S37 | “secondary prevention” | 5,003 |
| S38 | “preventive measure*” | 4,270 |
| S39 | “preventative measure*” | 753 |
| S40 | “preventive care” or “preventative care” | 2,585 |
| S41 | (obes* n2 (prevent* or treat*)) | 18,976 |
| S42 | S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 | 162,511 |
| S43 | (MH “Exercise+”) | 98,166 |
| S44 | (MH “Physical Activity”) | 34,052 |
| S45 | “physical inactivity” | 2,862 |
| S46 | (MH “Motor Activity+”) | 11,331 |
| S47 | (MH “Physical Education and Training”) OR “physical education” or “physical training” | 5,789 |
| S48 | (MH “Physical Fitness”) | 15,398 |
| S49 | “sedentary” | 12,921 |
| S50 | (MH “Life Style+”) OR (MH “Life Style, Sedentary”) | 191,970 |
| S51 | (MH “Leisure Activities+”) | 59,776 |
| S52 | (MH “Sports+”) | 70,276 |
| S53 | (MH “Dancing+”) OR “Dance*” | 5,011 |
| S54 | (exercise* n1 aerobic*) | 8,133 |
| S55 | sport* | 60,320 |
| S56 | ((lifestyle* or “life style*”) n5 activ*) | 3,102 |
| S57 | S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 | 422,446 |
| S58 | (MH “Diet+”) | 99,721 |
| S59 | nutrition* | 132,059 |
| S60 | health* n2 eat* | 6,335 |
| S61 | “Child Nutrition Sciences” OR (MH “Child Nutrition”) | 6,615 |
| S62 | (MH “Fruit+”) | 22,055 |
| S63 | (MH “Vegetables”) OR “vegetable*” | 19,045 |
| S64 | fruit* | 23,015 |
| S65 | canteen* | 222 |
| S66 | (MH “Food Services”) OR “food service*” | 7,038 |
| S67 | “menu*” | 3,133 |
| S68 | “calorie” or calories or kilojoule* | 6,393 |
| S69 | (MH “Energy Intake”) | 15,666 |
| S70 | (MH “Energy Density”) | 768 |
| S71 | (MH “Eating”) | 5,602 |
| S72 | (MH “Eating Behavior”) OR “feeding behavio?r*” | 13,107 |
| S73 | (MH “Food Intake”) OR “dietary intake” | 15,815 |
| S74 | (MH “Food Habits”) | 11,568 |
| S75 | (MH “Food”) | 12,475 |
| S76 | (MH “Carbonated Beverages”) OR “soft drink*” | 2,878 |
| S77 | “soda” | 932 |
| S78 | “sweetened drink*” | 157 |
| S79 | (MH “Dietary Fats”) | 11,637 |
| S80 | “confectionar*” | 64 |
| S81 | (MH “Candy”) | 550 |
| S82 | (school n1 (lunch* or meal*)) | 997 |
| S83 | ((feeding or food or nutrition*) n1 program*) | 3,598 |
| S84 | “cafeteria*” | 553 |
| S85 | (MH “Nutritional Status”) | 12,624 |
| S86 | S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 OR S85 | 254,598 |
| S87 | (MH “Smoking+”) | 61,753 |
| S88 | (MH “Smoking Cessation Programs”) OR (MH “Tobacco Abuse Control (Saba CCC)”) OR (MH “Tobacco Abuse (Saba CCC)”) OR “Tobacco Use Cessation” | 2,476 |
| S89 | smok* | 102,107 |
| S90 | (MH “Nicotine”) | 3,843 |
| S91 | (MH “Tobacco”) | 6,806 |
| S92 | ((ceas* or cess* or prevent* or stop* or quit* or abstin* or abstain* or reduc*) n5 (smok* or tobacco or nicotine)) | 34,452 |
| S93 | (MH “Substance Use Disorders”) | 30,133 |
| S94 | “ex-smoker*” | 865 |
| S95 | “anti-smok*” | 507 |
| S96 | S87 OR S88 OR S89 OR S90 OR S91 OR S92 OR S93 OR S94 OR S95 | 131,288 |
| S97 | (MH “Binge Drinking”) OR (MH “Drinking Behavior”) | 2,983 |
| S98 | alcohol* | 88,324 |
| S99 | (MH “Alcoholism”) OR (MH “Alcoholic Intoxication”) | 17,169 |
| S100 | drink* | 49,157 |
| S101 | liquor* | 648 |
| S102 | beer* | 1,813 |
| S103 | wine* | 2,861 |
| S104 | spirit* | 26,997 |
| S105 | drunk* | 1,346 |
| S106 | intoxicat* | 6,974 |
| S107 | binge | 6,400 |
| S108 | S97 OR S98 OR S99 OR S100 OR S101 OR S102 OR S103 OR S104 OR S105 OR S106 OR S107 | 136,966 |
| S109 | S42 OR S57 OR S86 OR S96 OR S108 | 917,121 |
| S110 | (MH “Randomized Controlled Trials”) OR (MH “Clinical Trials+”) | 257,461 |
| S111 | (MH “Random Assignment”) | 54,198 |
| S112 | (MH “Double-Blind Studies”) | 40,941 |
| S113 | (MH “Single-Blind Studies”) | 12,411 |
| S114 | (MH “Placebos”) | 11,197 |
| S115 | (MH “Study Design”) | 28,853 |
| S116 | (MH “Experimental Studies”) OR “Intervention Studies” | 26,918 |
| S117 | (MH “Evaluation Research”) OR “Evaluation Studies” | 112,449 |
| S118 | (MH “Comparative Studies”) | 186,640 |
| S119 | (MH “Prospective Studies”) OR “Longitudinal Studies” | 383,320 |
| S120 | (MH “Crossover Design”) OR “Cross-Over Studies” | 17,483 |
| S121 | “clinical trial*” | 207,810 |
| S122 | “latin square” | 191 |
| S123 | (MH “Time Series”) | 2,468 |
| S124 | (before n2 after n3 (stud* or trial* or design*)) | 5,063 |
| S125 | ((singl* or doubl* or trebl* or tripl*) n5 (blind* or mark)) | 65,046 |
| S126 | placebo* | 54,518 |
| S127 | random* | 343,356 |
| S128 | (matched n1 (communit* or school* or population*)) | 1,484 |
| S129 | control* | 1,068,659 |
| S130 | “comparison group*” | 6,675 |
| S131 | “matched pairs” | 1,481 |
| S132 | “outcome stud*” | 2,824 |
| S133 | qua?iexperimental or “qua?i experimental” or “pseudo experimental” | 13,804 |
| S134 | nonrandomi?ed or “non randomi?ed” or “psuedo randomi?ed” or “qua?i randomi?ed” | 8,381 |
| S135 | prospectiv* | 449,494 |
| S136 | volunteer* | 44,312 |
| S137 | S110 OR S111 OR S112 OR S113 OR S114 OR S115 OR S116 OR S117 OR S118 OR S119 OR S120 OR S121 OR S122 OR S123 OR S124 OR S125 OR S126 OR S127 OR S128 OR S129 OR S130 OR S131 OR S132 OR S133 OR S134 OR S135 OR S136 | 1,733,188 |
| S138 | (MH “Child”) OR (MH “Adolescence”) | 667,718 |
| S139 | (child or children or adolescen* or teen*) | 876,565 |
| S140 | S138 OR S139 | 876,565 |
| S141 | S4 AND S27 AND S109 AND S137 AND S140 (limited to September 2016-April 2019) | 656 |
EDUCATION RESOURCE INFORMATION CENTER
noft((School* OR ((primary OR elementary OR middle OR junior OR high OR secondary) AND student*) OR kinder*)) AND noft((Implement* OR dissemin* OR adopt* OR practice* OR “organisational change*” OR “organizational change*” OR diffuse* OR “system* change*” OR “quality improvement*” OR transform* OR translat* OR transfer* OR uptake* OR sustainab* OR institutionali* OR routin* OR maintenance OR capacity OR incorporate* OR adher* OR program* OR integrat* OR “scal* up”)) AND noft((Obes* OR “Weight Gain” OR “Weight Loss” OR overweight OR “over weight” OR overeat* OR “over eat*” OR “weight change*” OR ((bmi OR body mass index) AND (gain OR loss OR change)) OR “Primary Prevention” OR “secondary prevention” OR “preventive measure*” OR “preventative measure” OR “preventive care” OR “preventative care” OR Exercise OR “physical activity” OR “physical inactivity” OR “Motor Activity” OR “physical education” or “physical training” OR “Physical Fitness” OR sedentary OR “Life Style” OR lifestyle OR “Leisure Activit*” OR sport* OR Dancing OR dance* OR aerobic* OR diet OR nutrition* OR “Child Nutrition Sciences” OR fruit* OR vegetable* OR canteen* OR “food service*” OR menu* OR calorie* OR kilojoule* OR “Energy Intake” OR “energy density” OR eating OR “Feeding Behavio*” OR “dietary intake” OR food OR “Carbonated Beverage*” OR “soft drink*” OR soda OR “sweetened drink*” OR “Dietary Fats” OR confectionar* OR “school lunch*” OR “school meal*” OR ((feeding OR food OR nutrition*) AND program*) OR cafeteria* OR smok* OR Tobacco OR Nicotine OR alcohol* OR drink* OR liquor* OR beer* OR wine* OR spirit* OR drunk* OR intoxicat* OR binge)) AND noft((“clinical trial*” OR random* OR placebo* OR “Research Design” OR “Intervention Stud*” OR “Evaluation Stud*” OR “Comparative Stud*” OR “Longitudinal Stud*” OR “Cross-Over Stud*” OR “latin square” OR “time series” OR ((before AND after) AND (stud* OR trial* OR design*)) OR ((singl* OR doubl* OR trebl* OR tripl*) AND (blind* OR mark)) OR (matched AND (communit* OR school* OR population*)) OR control* OR “comparison group*” OR “control group*” OR “matched pairs” OR “outcome stud*” OR qu?siexperimental OR “qua?i experimental” OR “pseudo experimental” OR nonrandomized OR nonrandomised OR prospective* OR volunteer*)) AND noft(Child or children or teen* or adolescen*)
DISSERTATIONS AND THESES
Ab/ti/su((School* OR ((primary OR elementary OR middle OR junior OR high OR secondary) AND student*) OR kinder*)) AND Ab/ti/su ((Implement* OR dissemin* OR adopt* OR practice* OR “organisational change*” OR “organizational change*” OR diffuse* OR “system* change*” OR “quality improvement*” OR transform* OR translat* OR transfer* OR uptake* OR sustainab* OR institutionali* OR routin* OR maintenance OR capacity OR incorporate* OR adher* OR program* OR integrat* OR “scal* up”)) AND Ab/ti/su ((Obes* OR “Weight Gain” OR “Weight Loss” OR overweight OR “over weight” OR overeat* OR “over eat*” OR “weight change*” OR ((bmi OR body mass index) AND (gain OR loss OR change)) OR “Primary Prevention” OR “secondary prevention” OR “preventive measure*” OR “preventative measure” OR “preventive care” OR “preventative care” OR Exercise OR “physical activity” OR “physical inactivity” OR “Motor Activity” OR “physical education” OR “physical training” OR “Physical Fitness” OR sedentary OR “Life Style” OR lifestyle OR “Leisure Activit*” OR sport* OR Dancing OR dance* OR aerobic* OR diet OR nutrition* OR “Child Nutrition Sciences” OR fruit* OR vegetable* OR canteen* OR “food service*” OR menu* OR calorie* OR kilojoule* OR “Energy Intake” OR “energy density” OR eating OR “Feeding Behavio*” OR “dietary intake” OR food OR “Carbonated Beverage*” OR “soft drink*” OR soda OR “sweetened drink*” OR “Dietary Fats” OR confectionar* OR “school lunch*” OR “school meal*” OR ((feeding OR food OR nutrition*) AND program*) OR cafeteria* OR smok* OR Tobacco OR Nicotine OR alcohol* OR drink* OR liquor* OR beer* OR wine* OR spirit* OR drunk* OR intoxicat* OR binge)) AND Ab/ti/su ((“clinical trial*” OR random* OR placebo* OR “Research Design” OR “Intervention Stud*” OR “Evaluation Stud*” OR “Comparative Stud*” OR “Longitudinal Stud*” OR “Cross-Over Stud*” OR “latin square” OR “time series” OR ((before AND after) AND (stud* OR trial* OR design*)) OR ((singl* OR doubl* OR trebl* OR tripl*) AND (blind* OR mark)) OR (matched AND (communit* OR school* OR population*)) OR control* OR “comparison group*” OR “control group*” OR “matched pairs” OR “outcome stud*” OR qu?siexperimental OR “qua?i experimental” OR “pseudo experimental” OR nonrandomized OR nonrandomised OR prospective* OR volunteer*)) AND Ab/ti/su ((Child OR children OR teen* OR adolescen*))
SCOPUS
TITLE (school* OR ((primary OR elementary OR middle OR junior OR high OR secondary) AND student*) OR kinder*) AND ABS (implement* OR dissemin* OR adopt* OR practice* OR “organisational change*” OR “organizational change*” OR diffuse* OR “system* change*” OR “quality improvement*” OR transform* OR translat* OR transfer* OR uptake* OR sustainab* OR institutionali* OR routin* OR maintenance OR capacity OR incorporate* OR adher* OR program* OR integrat* OR “scal* up”) AND TITLE (obes* OR “Weight Gain” OR “Weight Loss” OR overweight OR “over weight” OR overeat* OR “over eat*” OR “weight change*” OR ((bmi OR body AND mass AND index) AND (gain OR loss OR change)) OR “Primary Prevention” OR “secondary prevention” OR “preventive measure*” OR “preventative measure” OR “preventive care” OR “preventative care” OR exercise OR “physical activity” OR “physical inactivity” OR “Motor Activity” OR “physical education” OR “physical training” OR “Physical Fitness” OR sedentary OR “Life Style” OR lifestyle OR “Leisure Activit*” OR sport* OR dancing OR dance* OR aerobic* OR diet OR nutrition* OR “Child Nutrition Sciences” OR fruit* OR vegetable* OR canteen* OR “food service*” OR menu* OR calorie* OR kilojoule* OR “Energy Intake” OR “energy density” OR eating OR “Feeding Behavio*” OR “dietary intake” OR food OR “Carbonated Beverage*” OR “soft drink*” OR soda OR “sweetened drink*” OR “Dietary Fats” OR confectionar* OR “school lunch*” OR “school meal*” OR ((feeding OR food OR nutrition*) AND program*) OR cafeteria* OR smok* OR tobacco OR nicotine OR alcohol* OR drink* OR liquor* OR beer* OR wine* OR spirit* OR drunk* OR intoxicat* OR binge) AND ABS ((“clinical trial*” OR random* OR placebo* OR “Research Design” OR “Intervention Stud*” OR “Evaluation Stud*” OR “Comparative Stud*” OR “Longitudinal Stud*” OR “Cross-Over Stud*” OR “latin square” OR “time series” OR ((before AND after) AND (stud* OR trial* OR design*)) OR ((singl* OR doubl* OR trebl* OR tripl*) AND (blind* OR mark)) OR (matched AND (communit* OR school* OR population*)) OR control* OR “comparison group*” OR “control group*” OR “matched pairs” OR “outcome stud*” OR qu?siexperimental OR “qua?i experimental” OR “pseudo experimental” OR nonrandomized OR nonrandomised OR prospective* OR volunteer*)) AND TITLE (child OR children OR teen* OR adolescen*) AND (LIMIT-TO (PUBYEAR, 2019) OR LIMIT-TO (PUBYEAR, 2018) OR LIMIT-TO (PUBYEAR, 2017) OR LIMIT-TO (PUBYEAR, 2016))
COCHRANE LIBRARY
(School* OR kinder* OR ((primary OR elementary OR middle OR junior OR high OR secondary) AND student*)) in Title Abstract Keyword AND (Implement* OR dissemin* OR adopt* OR practice* OR “organisational change*” OR “organizational change*” OR diffuse* OR “system* change*” OR “quality improvement*” OR transform* OR translat* OR transfer* OR uptake* OR sustainab* OR institutionali* OR routin* OR maintenance OR capacity OR incorporate* OR adher* OR program* OR integrat* OR “scal* up”) in Title Abstract Keyword AND (Obes* OR “Weight Gain” OR “Weight Loss” OR overweight OR “over weight” OR overeat* OR “over eat*” OR “weight change*” OR ((bmi OR body mass index) AND (gain OR loss OR change)) OR “Primary Prevention” OR “secondary prevention” OR “preventive measure*” OR “preventative measure” OR “preventive care” OR “preventative care” OR Exercise OR “physical activity” OR “physical inactivity” OR “Motor Activity” OR “physical education” or “physical training” OR “Physical Fitness” OR sedentary OR “Life Style” OR lifestyle OR “Leisure Activit*” OR sport* OR Dancing OR dance* OR aerobic* OR diet OR nutrition* OR “Child Nutrition Sciences” OR fruit* OR vegetable* OR canteen* OR “food service*” OR menu* OR calorie* OR kilojoule* OR “Energy Intake” OR “energy density” OR eating OR “Feeding Behavio*” OR “dietary intake” OR food OR “Carbonated Beverage*” OR “soft drink*” OR soda OR “sweetened drink*” OR “Dietary Fats” OR confectionar* OR “school lunch*” OR “school meal*” OR ((feeding OR food OR nutrition*) AND program*) OR cafeteria* OR smok* OR Tobacco OR Nicotine OR alcohol* OR drink* OR liquor* OR beer* OR wine* OR spirit* OR drunk* OR intoxicat* OR binge) in Title Abstract Keyword AND Child or children or teen* or adolescen* in Title Abstract Keyword - with Cochrane Library publication date Between Sep 2016 and Apr 2019, in Cochrane Reviews, Cochrane Protocols, Trials (Word variations have been searched)
Appendix A3
Implementation strategies as characterized by effective practice and organization of care (EPOC) taxonomy list
| Category | Subcategory | Definition |
|---|---|---|
| Interventions targeted at health care organizations | Organizational culture | Strategies to change organizational culture |
| Interventions targeted at health care workers | Audit and feedback | A summary of health workers’ performance over a specified period of time, given to them in a written electronic or verbal format. The summary may include recommendations for clinical action. |
| Clinical incident reporting | System for reporting critical incidents | |
| Monitoring the performance of the delivery of healthcare | Monitoring of health services by individuals or health care organizations, for example, by comparing with an external standard | |
| Communities of practice | Groups of people with a common interest who deepen their knowledge and expertise in this area by interacting on an ongoing basis | |
| Continuous quality improvement | An iterative process to review and improve care that includes involvement of health care teams, analysis of a process or system, a structured process improvement method or problem solving approach, and use of data analysis to assess changes | |
| Educational games | The use of games as an educational strategy to improve standards of care | |
| Educational materials | Distribution to individuals, or groups, of educational materials to support clinical care, that is, any intervention in which knowledge is distributed. For example, this may be facilitated by the internet, learning critical appraisal skills; skills for electronic retrieval of information, diagnostic formulation; question formulation | |
| Educational meetings | Courses, workshops, conferences, or other educational meetings | |
| Educational outreach visits, or academic detailing | Personal visits by a trained person to health workers in their own settings to provide information with the aim of changing practice. | |
| Clinical practice guidelines | Clinical guidelines are systematically developed statements to assist health care providers and patients to decide on appropriate health care for specific clinical circumstances (U.S. IOM). Within schools, this may include the development of best-practice nutrition or physical activity guidelines, which are then provided to school staff as instructional material to support the implementation of policies, practices, or programs. |
|
| Interprofessional education | Continuing education for health professionals that involves more than one profession in joint, interactive learning | |
| Local consensus processes | Formal or informal local consensus processes, for example, agreeing a clinical protocol to manage a patient group, adapting a guideline for a local health system or promoting the implementation of guidelines | |
| Local opinion leaders | The identification and use of identifiable local opinion leaders to promote good clinical practice | |
| Managerial supervision | Routine supervision visits by health staff | |
| Patient-mediated interventions | The use of patients, for example, by providing patient outcomes, to change professional practice | |
| Public release of performance data | Informing the public about health care providers by the release of performance data in written or electronic form | |
| Reminders | Manual or computerized interventions that prompt health workers to perform an action during a consultation with a patient, for example, computer decision support systems | |
| Routine patient-reported outcome measures | Routine administration and reporting of patient-reported outcome measures to providers and/or patients | |
| Tailored interventions | Interventions to change practice that are selected based on an assessment of barriers to change, for example, through interviews or surveys |
Appendix A4
Data extraction table for included studies
| Alaimo et al. [43] | ||
|---|---|---|
| Study characteristics | Design: nonrandomized trial | |
| Setting: Middle school | ||
| Population: Michigan, USA | ||
| n (number of participants) | Baseline: HSAT: 24 (schools); HSAT + SNAK: 5 (schools); HSAT + MSBE: 25 (schools);Control: 21 (schools) |
Follow-up: HSAT: 18 (schools); HSAT + SNAK: 5 (schools); HSAT + MSBE: 22 (schools);Control: 20 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Healthy School Actions Tools (HSAT) included questions on the following topics: school nutrition policies, school nutrition environment, school health education programs including nutrition education, and food service programs. - At the end of each module, schools were to brainstorm several “bright ideas” they could implement. Schools identified bright ideas for each section were shown together to facilitate the development of an action plan with goals (tailored interventions). - Schools were asked to prioritize goals and received funding to implement nutrition education or nutrition activities in their action plans and compensate for any loss in canteen revenue (external funding). - Schools were provided with a facilitator meeting to assess nutrition environments and policies (educational outreach visits). - Guidance documents were provided to school staff (educational materials). - Schools established a coordinated school health team (local consensus approach). - Implementation of policy in cafeteria à la carte lines (clinical practice guidelines). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: mean nutrition policy score (range 0–6) and mean nutrition education and/or practice change score (range 0–14) | |
| Measure: The Middle-School School Environment and Policy Survey was completed either online or by paper. There were two versions of the survey: one for administrators and one for food service directors. | ||
| Results: Median (range) nutrition policy score: 0.65 (0.2–1.1) | ||
| Cunningham-Sabo et al. [44] | ||
| Study characteristics | Design: RCT | |
| Setting: Elementary school | ||
| Population: New Mexico and South Dakota, USA | ||
| n (number of participants) | Baseline: Intervention: 19 (schools); Control: 20 (schools) | Follow-up: Intervention: 19 (schools); Control: 20 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Components included a classroom curriculum, new skills and activities for the school physical education classes, activities and events with the families, and skill building with school food service - The intervention included the development of nutrient guidelines operationalized as behavioral guidelines (clinical practice guidelines). Training sessions were conducted twice each school year with food service staff. Schools also received at least five kitchen visits in the first year and eight or more visits to each school in the second and third years (educational outreach visits). - Materials and activities for the training sessions and kitchen visits were developed (educational materials). - The food service working group met annually and held monthly conference calls to establish and carry out the intervention (educational meetings). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: percentage calories total fat breakfast (%) and percentage energy from total fat Lunch (%) | |
| Measure: All schools had a Pathways notebook with forms to be completed for each meal per day. On the form each food item was listed with a complete description of the food, the serving size, and the number of students served the food. Separate forms were completed for breakfast and lunch. | ||
| Results: Median (range) nutrient content of school meals % of calories from fat breakfast/ lunch: −3% (−3.3% to −2.7%) | ||
| Delk et al. [46] | ||
| Study characteristics | Design: Cluster-RCT | |
| Setting: Middle schools | ||
| Population: Central Texas, USA | ||
| n (number of participants) | Baseline: Basic: 10 (schools); Basic Plus: 10 (schools); Basic Plus SM: 10 (schools) | Follow-up: 10 (schools); Basic Plus: 10 (schools); Basic Plus SM: 10 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Promote the adoption of active breaks (ABs) by teachers. - In promoting ABs, we developed a CATCH Middle School ABs guide. Each school received 10 hard copies of the ABs and an electronic version. ABs stated the amount of time required, contained instructional content, identified equipment needed (clinical practice guidelines). - A CATCH Team was developed at each school, consisting of staff members, parents and community members (local consensus approach) - Schools were required to send representatives from their CATCH Team to 8 trainings and were assigned a CATCH facilitator to conduct visits at these schools (educational meetings). - A CATCH facilitator was assigned and conducted monthly visits at these schools. During these visits strategies to help CATCH Teams promote ABs on their campus were developed (educational outreach visits and tailored interventions). - Social marketing campaigns to promote physical activity (other) |
|
| Comparator description | Different implementation strategy | |
| Implementation outcomes | Outcome: Teacher reported frequency of AB implementation including: Have you conducted at least one AB this year; Percentage of teachers that conducted activity breaks weekly (%, N); Last week, did you conduct an activity break on at least 1 day? (%, N) | |
| Measure: The survey is a 15-item, self-administered questionnaire that includes items on teacher implementation of ABs, encouragement of specific health behaviors, and other process evaluation measures for the CATCH program | ||
| Results: Median (range) % of teachers that conducted activity breaks weekly: 13.3% (11.1% to 15.4%); Median (range) % implementing a variety of policies and practices: 26.5% (19.4% to 31.9%) | ||
| French et al. [47] | ||
| Study characteristics | Design: Cluster-RCT | |
| Setting: High school | ||
| Population: Minneapolis, USA | ||
| n (number of participants) | Baseline: Intervention: 10 (schools); Control: 10 (schools) | Follow-up: Intervention: 10 (schools); Control: 10 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Increasing the availability of lower-fat foods in cafeteria à la carte areas and implementing school-wide, student-based promotions of these lower-fat foods. The goal was to increase lower-fat à la carte food availability by 30% relative to baseline. The ultimate goal was to have 50% of products be lower fat. - Quarterly meetings between researchers and staff were held to review progress toward goals (local consensus approach). - Development of tailored lists of high and low fat foods for schools (tailored interventions) - Staff worked with the student groups and their faculty advisors to train the students for specific promotional activities (educational meetings) - Student groups were offered financial incentives for completing each promotion (pay for performance) |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: Students seen any posters in school about cafeteria food choices; Students heard any messages over public address system, in school; Students heard about any contests or events at school about cafeteria food choices; Students took part in any taste tests, food samplings, or contests in the school cafeteria; Percentage low-fat à la carte foods | |
| Measure: Complete à la carte inventories in intervention and control schools were conducted by trained research staff at baseline and after the second intervention year | ||
| Results: Median (range) % of program implementation: 33% (11% to 41%) | ||
| Heath and Coleman [48] | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: West Texas and East New Mexico, USA | ||
| n (number of participants) | Baseline: Intervention: 20 (schools); Control: 4 (schools) | Follow-up: Intervention: 20 (schools); Control: 4 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: CATCH intervention was delivered at school level to: reduce the total fat content of food served to 30% and reduce the total sodium content to 600 mg ‐ 1000 mg per serving. - Staff received training sessions (educational meetings). - Staff received ongoing support visits to implement EATSMART/ CATCH PE (educational outreach visits). Educational materials were provided to staff/schools. Smart choices manual was provided to all schools (educational materials). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: % fat in breakfast; Sodium (mg) in breakfast; % fat in lunch; Sodium (mg) in lunch | |
| Measure: Menus and recipes were collected for 5 consecutive days during each semester in every year of the study. Recipes for these menus were obtained by interviewing cooks and kitchen managers in school cafeterias and by reviewing the cafeteria production sheets for each meal. Foods from the menus, production sheets, and recipes were entered into a nutritional database that is especially useful for ethnic foods. Once the nutrient content of the meals was analyzed, averages of breakfast and lunch values across the 5 days of data collection were obtained. | ||
| Results: % fat in school meal: −1.7% (−4.4% to 1%); Sodium of school meals: −29.5 (−48 to −11) | ||
| Hoelscher et al. [49] | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: Texas, USA | ||
| n (number of participants) | Baseline: Intervention: 15 (schools); Control: 15 (schools) | Follow-up: Intervention: 15 (schools); Control: 15 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Target multiple aspects of the school environment, including the classroom, nutrition services and the cafeteria environment, physical education activities, family and home environment, and, via school health promotion messages and events, the broader school community. - Coordinated school health CATCH training and booster training sessions and community workshops (educational meetings). - Program materials, CATCH component coordination kit and health promotion resources (educational materials). - CATCH committee meetings (local consensus approach) - Recognition and funds for CATCH through rewards program (pay for performance) - School social marketing efforts (use of information and communication technology) - Family fun night activities (other) - Community member required on CATCH committee and CATCH community workshops (local consensus approach) - CATCH facilitator support visits (2–3 visits/4–6 weeks) (educational outreach visit). |
|
| Comparator description | Different implementation strategy | |
| Implementation outcomes | Outcome: Continuous: CATCH parent and extracurricular activities, CATCH coordinated healthy eating–related activities, CATCH coordinated physical activity–related activities, Number of CATCH lessons taught, Number health lessons taught Dichotomous: % Reporting CATCH lessons in schoolroom, % Reporting that fruit usually served at lunch |
|
| Measure: Structured interview with CATCH Champion and self‐administered questionnaire for classroom teachers | ||
| Results: Mean number of lessons/or activities: 0.8 (−0.4 to 1. 2) % implementing a variety of policies and practices: 4.4% (3.6% to 5.2%) |
||
| Lytle et al. [50] | ||
| Study characteristics | Design: RCT | |
| Setting: Middle schools | ||
| Population: Minneapolis. USA | ||
| n (number of participants) | Baseline: 8 (schools); Control: 8 (schools) | Follow-up: 8 (schools); Control: 8 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Teens Eating for Energy and Nutrition at School (TEENS) was a school‐based intervention trial with a goal of developing and evaluating school and family‐linked intervention strategies to promote students’ consumption of fruit, vegetable, and lower fat snacks. TEENS intervention included classroom, family, school policy, and food service components. - School Nutrition Advisory Councils were established to convene school and parental stakeholders to discuss and propose school-level policy to improve the school food environment (local opinion leaders and local consensus approach). - District food service directors and workers from intervention schools attended training that emphasized the importance of offering more fruit and vegetables, gave them new tools for promoting fruit, vegetable, and lower fat snacks (educational materials and educational meetings). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: Food offered: Foods to limit and foods to promote. Foods sold: Foods to limit and foods to promote | |
| Measure: Data collected included the total number of students served the meal pattern lunch, the types and amounts of fruit and vegetable choices offered and sold, and the number of vegetable salads sold. With a few exceptions, these data were extracted from schools’ food production records. | ||
| Results: % of schools offering or selling targeted foods: 8.5% (4% to 12%) | ||
| Mobley et al. [51] | ||
| Study characteristics | Design: RCT | |
| Setting: Middle schools | ||
| Population: 10 districts across USA | ||
| n (number of participants) | Baseline: Intervention: 21 (schools); Control: 21 (schools) | Follow-up: Intervention: 21 (schools); Control: 21 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Lower the average fat content of food served in schools; serve at least 2 servings of fruit and/or vegetables per student and at least 1 serving per student each day; serve all dessert and snack foods with ≤ 200 kcal per single size serving and/or package; eliminate milk >1% fat, all other added sugar beverages, and 100% fruit juice; serve at least 2 servings of high fiber grain‐based foods and/or legumes per student and at least 1 serving per student each day. - Provision of staff training and educational events (educational meetings). - “Taste tests” of new products and unfamiliar foods, including conducting comparison of available items (educational games). - Intervention schools received funding to defray expenses and potential loss of income, cafeteria enhancements and to attend training (external funding). - Research staff worked with food service managers to identify barriers and develop solutions for schools to achieve selected goals (tailored interventions). - Curricula, posters, brief messages displayed near serving lines (educational materials). - Research staff met weekly with food service staff to observe the food environment and to plan and support goal achievement (educational outreach visits) - Engagement with social marketing experts to generate content (use of information and communication in technology) - Meetings with district level staff and buyers who procure food and with food distributors, to solicit support for change (other) |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: 12 scores across the following variables: Lower than average fat content; serve two servings of fruit and vegetables; serve all desert and snack foods with <200 kcal; eliminate milk >1% fat; serve at least two servings of high fiber | |
| Measure: Data collected by trained staff not involved in the intervention. Nutrition data were extracted from food service management source documents maintained by school food service personnel. | ||
| Results: % schools meeting various nutrition goals: 15.5% (0% to 88%) | ||
| Nathan et al. [52] | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: NSW, Australia | ||
| n (number of participants) | Baseline: Intervention: 407 (schools); Control: 316 (schools) | Follow-up: Intervention: 388 (schools); Control: 258 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Structured multi-strategy intervention was developed based on theoretical frameworks of practice change and recommendations from reviews and implementation studies conducted in schools and other settings - Program materials, including curriculum resources and information to parents (educational materials) - Staff training and professional development (educational meetings). - School consensus approach, as well as leadership support and enhancement (local consensus approach and local opinion leaders). - School-specific follow-up support (tailored interventions) - Incentives in the form of material goods (other) - Implementation feedback, including performance monitoring (monitoring the performance of the delivery of the health care). |
|
| Comparator description | Minimal support control | |
| Implementation outcomes | Outcome: The prevalence of vegetable and fruit breaks. | |
| Measure: Principal reported computer‐assisted telephone interviewing (CATI). | ||
| Results: % Schools implementing a vegetable and fruit break: 16.2% (5.6% to 26.8%) | ||
| Nathan et al. [53] | ||
| Study characteristics | Design: RCT | |
| Setting: Elementary schools | ||
| Population: NSW, Australia | ||
| n (number of participants) | Baseline: Intervention: 28 (schools); Control: 25 (schools) | Follow-up: Intervention: 27 (schools); Control: 24 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: State government had introduced a healthy school canteen policy. Utilizing a “traffic light” food classification system, the policy classifies foods and beverages sold in school canteens as either “red,” “amber” or “green” based on their nutritional content. For all foods sold in the canteen at recess and lunch the policy requires schools to remove all red foods from regular sale and to fill the menu with green foods and to not let amber foods dominate the menu. - Schools were provided with a written feedback report on their previously supplied canteen menu (audit and feedback). - Canteen managers were asked to send an updated version of the menu for review and a second feedback report was generated (continuous quality improvement). - Canteen managers were provided with a “Canteen Resource Kit” containing various printed and electronic instructional materials, including electronic menu and pricing templates (educational materials) - 1 day (5 hr) group-training workshop was offered to canteen - managers and parent representatives providing education and skill development in the Fresh Tastes@ School policy, label reading, canteen stock and financial management, pricing and promotion, and change management (educational meeting) - The workshop provided opportunities for canteen managers to participate in consensus processes through the development of a canteen action plan (local consensus approach). - School principals were asked to demonstrate their support for implementation of the Fresh Tastes @ School policy (local opinion leader) - The feedback report included a sample “compliant” menu, individually tailored to the schools (tailored interventions) - Canteen managers received two support contacts per school term via text messages. These contacts provided targeted advice to overcome common barriers to policy implementation and encouraged canteen managers to review progress against their action plan (other). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Proportion of schools with a menu that did not include red or banned foods and beverages and the proportion of schools where green items make up the majority of the menu (more than 50 % of menu items). | |
| Measure: Audits of canteen menus faxed or emailed to the project team by the school. | ||
| Results: % implementing a variety of policies and practices: 35.5% (30.0% to 41.1%) | ||
| Naylor et al. [54] | ||
| Study characteristics | Design: cluster-RCT | |
| Setting: Elementary schools | ||
| Population: British Columbia, Canada | ||
| n (number of participants): | Baseline: Intervention: 7 (schools); Control: 3 (schools) | Follow-up: Intervention: 7 (schools); Control: 3 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: - The AS! BC model provided tools for schools and teachers to create individualized Action Plans that increased PA opportunities across Six Action Zones: School Environment, Scheduled physical education (PE), Classroom Action, Family and Community, Extra‐curricular, Spirit (tailored interventions). - Teachers received teacher-on-call support to attend a Classroom Action training session (half-day) from the AS! BC Support Team and School Facilitators (educational meetings) - A committee of school stakeholders, including grade teachers, administrators, parents, health, sport/recreation practitioners, was developed (local consensus approach). Teachers had weekly contact with the School Facilitator who would come to the classroom to provide mentorship and demonstrate activities (educational outreach visits). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: Minutes per week of physical activity | |
| Measure: Teachers at Intervention schools were asked to complete weekly activity Logs during Phases I and II. Teachers recorded daily, the type, frequency and duration (minutes) of PA implemented in the classroom, in PE or in the other Action Zones. Activity Logs were collected monthly by the School Facilitators. | ||
| Results: Minutes per week of physical activity implemented in the classroom: 54.9 min (46.4–63.4) | ||
| Perry et al. [56] | ||
| Study characteristics | Design: cluster-RCT | |
| Setting: Elementary schools | ||
| Population: California, Louisiana, Minneapolis and Texas, USA | ||
| n (number of participants) | Baseline: CATCH 1: 28 (schools); CATCH 2: 28 (schools); Control: 40 (schools) | Follow-up: CATCH 1: 28 (schools); CATCH 2: 28 (schools); Control: 40 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: EATSMART: to reduce the total fat content of food served to 30%, to reduce the total sodium content to 600‐1000 mg per serving, recommendations to lower the total cholesterol in foods offered. CATCH PE: increase the amount of PE time that students spent in MVPA to 40% of class time. - Staff received training sessions to deliver EATSMART and CATCH PE (educational meetings). - Staff received ongoing support visits to implement EATSMART/CATCH PE (educational outreach visits). - Educational materials were provided to staff for EATSMART and CATCH PE (educational materials). Families were engaged by Family Fun Nights and home curricula (other). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: Mean % of kilocalories from fat in lunches, Mean mg of sodium in lunches, cholesterol mg in lunches (mean), quality of PE lesson % of seven activities observed | |
| Measure: Quality of PE lesson: Direct observation. Nutrient content: School menu information were collected from schools. Staff conducted in‐person interviews with the cooks about the menus and recipes using standardized probes for ingredients and preparation methods. | ||
| Results: % of kilocalories from fat in school lunch: −4.3% (−5.8% to −2.8%) Mean mg of sodium in lunches: −100.5 (−167.6 to −33.4) Cholesterol mg in lunches: −8.3 (−16.7 to 0.1) Quality of PE lesson % of seven activities observed: 14.3% (11.6% to 17.0%) |
||
| Perry et al. [55] | ||
| Study characteristics | Design: cluster-RCT | |
| Setting: Elementary schools | ||
| Population: Minnesota, USA | ||
| n (number of participants) | Baseline: Intervention: 13 (schools); Control: 13 (schools) | Follow-up: Intervention: 13 (schools); Control: 13 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Increasing the availability, appeal, and encouragement of fruits and vegetables in the school lunch program; emphasizing changes in the lunch line; and the school snack cart; increase the quality and quantity of fruits and vegetables served; increase the choices of fruits and vegetables in the lunch line, and to vary the type and preparation methods daily; special events to promote fruits and vegetables. - Monthly meetings were held with the cook managers to discuss and share implementation issues and new ideas during the 1st school year (educational meetings and local consensus approach). - Intervention staff visited schools weekly, on average, and supported the activities (educational outreach visits). - The “High 5 Flyers” that were hung in posters around the school cafeteria (educational materials). Sampling of fruit and vegetables, class challenges (other). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: Verbal encouragement by food staff (mean % of observations), number of fruits and vegetables on the snack cart (mean), number of fruits and vegetables students can choose (mean), fruit and vegetables rated as appealing (mean %). | |
| Measure: Direct observations of the lunchroom, lunch line, food cart, and food service staff behavior. | ||
| Results: % of program implementation: 14% (−2% to 30%) Mean number of fruit and vegetables available: 0.64 (0.48–0.80) |
||
| Sallis, 1997 | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: California, USA | ||
| n (number of participants) | Baseline: Intervention: 2 (schools); Control: 3 (schools) | Follow-up: Intervention: 2 (schools); Control: 3 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Sports, Play and Active Recreation for Kids (SPARK) PE was designed to be a comprehensive program for upper elementary students to increase physical activity. Designed to influence the quantity and quality of elementary PE lessons and the amount of PE through: # Lessons per week and minutes of PE per week. - Written curriculum guide identified the program philosophy and goals and included a yearly plan which was divided into instruction units with activity progressions within each unit (educational materials). - An additional 30 min per week was allocated for classroom instruction and practices in self-management activities and skills (length of consultation). - Equivalent types of equipment were provided to all seven schools, including control schools, and replacement equipment was added each year (other). - On-site support which was provided during the 3 years ensured the curriculum was followed. A PE specialist provided feedback, encouragement and direct assistance during schools visits (educational outreach visits). - Classroom teachers were trained to implement SPARK PE (educational meetings). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: Duration (minutes) per week of physical education lessons and frequency (per week) of physical education lessons | |
| Measure: Direct observation by trained assessors for one full week twice a year in each school year. | ||
| Results: Duration (minutes) per week of physical education lessons: 26.6 (15.3–37.9) Frequency (per week) of physical education lessons: 0.8 (0.3–1.3) |
||
| Saunders, 2006 | ||
| Study characteristics | Design: RCT | |
| Setting: High school | ||
| Population: South Carolina, USA | ||
| n (number of participants) | Baseline: Intervention: 12 (schools); Control: 12 (schools) | Follow-up: Intervention: 12 (schools); Control: 12 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Focused on changing personal, social, and environmental factors related to physical activity and involved changes to the school environment and instructional programs. Instructional program components included changes in physical education and health instruction to enhance physical activity self‐efficacy and enjoyment. Schools were not required to implement a specific LEAP curriculum. Rather, to change instructional practice. The environmental strategy involved changing school practices that encouraged and supported physical activity and included changes to school health services, faculty staff health promotion, school environment, and school community linkages. - Two full-time program support staff provided (educational outreach visits). - Each LEAP team was headed by a LEAP champion who was usually the teacher responsible for girls PE (local opinion leaders). - Staff training consisted of formal workshops and one-on-one technical assistance for school personnel (educational meetings). - LEAP staff maintained a wide range of resources (educational materials). - LEAP staff worked with the LEAP champion and the LEAP team in each school to identify opportunities to enhance the environment or change school policy in support of physical activity (local consensus approach). - Equipment, such as hand weights, exercise bands, pedometers, for intervention schools (other). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: School physical activity team, School administrator supports physical activity promotion, Emphasizes lifelong physical activity, Includes cooperative activities, School nurse counseling for physical activity, Adult modeling of physical activity through faculty/staff health promotion, Health education reinforces messages and skills taught in physical education, Community agency involvement, Family involvement. | |
| Measure: The organizational assessment interview was a 22‐item interview (10–15 min) conducted by the independent process evaluator in all intervention and control schools with a school administrator, to assess organizational‐level components. | ||
| Results: School level policy and practice related to physical activity from the school administrators perspective | ||
| Simons-Morton, 1988 | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: Texas, USA | ||
| n (number of participants) | Baseline: Intervention: 2 (schools); Control: 2 (schools) | Follow-up: Intervention: 2 (schools); Control: 2 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Innovations introduced into the schools included: 1) the new school lunch,) and 2) health education for healthful diet. Implementation of each of the program components required organizational changes in school programs and in the roles and practices of school personnel. - Project staff examined existing menu planning, food purchasing and recipe selection practices (monitoring of performance). - Practice changes in four areas purchasing, menu planning, recipes, and food preparation were identified and negotiated with the food service director and with intervention school cafeteria managers (local consensus processes). - Food handlers received six hours of summer in-service training conducted by the project staff in cooperation with cafeteria managers (educational outreach visits). - The staff dietitian served as consultant and was present in the treatment schools on a regular basis (managerial supervision). - Six health education modules on diet were provided, which included visual aids and teaching materials ready to be handed out to the children (educational materials). - Classroom modules were developed by project staff with the aid of a classroom teacher who had recently retired from the school district (local opinion leaders). - Children were eligible to receive token incentives, such as stickers and sweat bands, upon completion of the major learning activities (other). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Sodium content of school meals mg by schools, Fat content of school lunches (g). | |
| Measure: Recipe analyses, based on detailed interviews with each were conducted by trained staff nutritionists and analyzed by the Nutrition Coding Center (NCC). | ||
| Results: Macronutrient content of school meals | ||
| Story, 2000 | ||
| Study characteristics | Design: Cluster-RCT | |
| Setting: Elementary schools | ||
| Population: Minnesota, USA | ||
| n (number of participants) | Baseline: Intervention: 10 (schools); Control: 10 (schools) | Follow-up: Intervention: 10 (schools); Control: 10 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | Intervention description: Intervention strategies were (a) point‐of‐purchase promotion of fruit and vegetable using characters and messages, (b) increasing the appeal of fruit and vegetable, (c) increasing the variety and choice of fruit and vegetable served, and (d) offering an additional fruit choice on days when baked or frozen desserts were served. - Centralized training sessions were held for food service staff from the intervention schools. It was held during a regularly scheduled school day and was conducted by the 5-a-Day Power Plus staff. Food service staff attended the teacher training for 2 hr and also attended 2 hr training after school each of the 2 intervention years (educational meetings). - A local producer provided some fruit and vegetable for use in classroom taste testing, home snack packs, and to expand choice in school lunch. They also provided a 30 min presentation on fruit and vegetable to each classroom (other). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Mean number of fruit and vegetable choices available, Mean number of fruit and vegetable choices available, Mean % of 8 guidelines on how to offer appealing fruit and vegetable, Mean % of 8 guidelines on how to offer appealing fruit and vegetable, Mean % of 4 fruit and vegetable promotions, Mean % of 4 fruit and vegetable promotions. | |
| Measure: Direct observations using trained observers and standardized protocols and instruments. | ||
| Results: Mean number fruit and vegetables available: 1.15 (1–1.3) % of guidelines implemented and % of promotions held: 38.4% (28.5% to 43.8%) |
||
| Sutherland, 2017 | ||
| Study characteristics | Design: Cluster-RCT | |
| Setting: Elementary schools | ||
| Population: NSW, Australia | ||
| n (number of participants) | Baseline: Intervention: 25 (schools); Control: 21 (schools) | Follow-up: Intervention: 25 (schools); Control: 21 (schools) |
| Intervention description (implementation strategy categorized by EPOC) | The evidence‐based school physical activity program known as SCORES (Supporting Children’s Outcomes using Rewards, Exercise and Skills) was rolled out in primary schools and the implementation intervention strategies facilitated its roll out. - Schools were provided feedback on the implementation of the intervention on three occasions via email (audit and feedback). - Teachers were provided with resources, including lesson booklets, posters, whistles, lanyards and fundamental motor skills cards (educational materials). - Teachers were offered a 90 min professional learning workshop including theory and practical sessions. The workshop focused on delivery of fundamental motor skills to students, strategies to improve lesson quality through student engagement and increase students’ MVPA (educational meeting), - Teaching with experienced Health Promotion staff with a PE background was offered to classroom teachers in intervention schools (educational outreach visits). - A meeting with school executive was held at the commencement of intervention and a school champion nominated for each school (local opinion leader). - Additional support was provided to classroom teachers via five short video clips viewed in staff meetings, reinforcing the quality PE teaching principles (other). |
|
| Comparator description: | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: school PA policy or plan (% of schools), overall lesson quality score, recess PA (mean % of days offered), lunch PA (mean % of days offered), provision of sports equipment at recess (mean % of days offered), provision of sports equipment at lunch (mean % of days offered), provision of parent newsletters regarding PA. | |
| Measure: Survey and observation | ||
| Results: % implementing a variety of policies and practices: 19% (16% to 22%) Physical education lesson quality score: 21.5 % of program implementation: −8% (−18% to 2%) |
||
| Whatley Blum, 2007 | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: High school | ||
| Population: Maine, USA | ||
| n (number of participants) | Baseline: Intervention: 4 (schools); Control: 3 (schools) | Follow-up: Intervention: 4 (schools); Control: 3 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: Implementing low‐fat, low‐sugar and portion controlled guidelines in à la carte and vending (snack and beverage) programs. - Visits by research staff to each schools food and beverage supplier to identify items that met the guidelines (educational outreach visits). - Suppliers who stocked vending machines were given lists of the available items and letters sent home to parents and students informing them of changes incentives. Banners were also displayed to promote healthier foods and taste testing was conducted (educational materials). - Modification of recipes and preparation techniques by research and food service personnel (clinical practice guidelines). - Food service directors were given lists of available products/vendors that met guidelines (procurement and distribution of supplies). - Presentations describing guidelines made to school staff (educational meeting). - Funding allocated to school liaison personnel (external funding). - A committee at each school site was created. A liaison identified at each school was responsible for establishing a committee to promote the healthy changes at the school (local consensus approach). - Communication between the project team and schools began in 2004 to obtain the cooperation of school administration and meet food service personnel (other). |
|
| Comparator description: | Usual practice or waitlist control | |
| Implementation outcomes: | Outcome: % items meeting nutrient criteria in à la carte, % items meeting nutrient criteria in snack vending, % items meeting nutrient criteria in beverage vending, % items meeting nutrient and proportion criteria in à la carte, % items meeting nutrient and proportion criteria in snack vending, % items meeting nutrient and proportion criteria in beverage vending. | |
| Measure: Observation and recording of items sold was taken at breakfast and lunch at cafeterias | ||
| Results: % of food and beverage items meeting guideline nutrient and portion criteria: 42.95% (15.7% to 60.6%) | ||
| Wolfenden, 2017 | ||
| Study characteristics | Design: RCT | |
| Setting: Elementary schools | ||
| Population: NSW, Australia | ||
| n (number of participants) | Baseline: Intervention 35 (schools); Control: 35 (schools) | Follow-up: Intervention: 27 (schools); Control: 30 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: Sought to increase implementation of a healthy canteen policy. Specifically, the intervention assisted schools to remove “red” and “banned” menu items from regular sale and increase the availability of “green” items to more than 50% of menu items. - Feedback menu reviews were conducted quarterly and the results were used to compile written feedback reports to the canteen manager and school principal (audit and feedback). - Support officers contacted canteen managers every 2 months throughout the intervention and used a continuous quality improvement framework of repeated goal setting, action planning, self-monitoring and problem-solving with canteen managers (continuous quality improvement). - Schools were also offered a small reimbursement to cover the costs associated with canteen manager attendance at training (external funding). - Printed instructional materials, sample policies/menus, planning templates and pricing guides were provided to all school canteen managers (educational materials). - Canteen managers, canteen staff and parent representatives were invited to attend a training workshop (5 hr) with the aim of providing education and skill development in the policy, nutrition and food label reading (educational meeting). - Canteen visits were conducted 1 and 3 months post-canteen manager training (educational outreach visits). - Meetings between support officers and canteen staff were held to discuss and reach consensus regarding the policy (local consensus process). - Executive support school principals were asked to communicate support for policy implementation and maintenance to teachers, parents, students and canteen managers (local opinion leader). - Individualized goal setting, action planning with canteen managers at different schools (tailored interventions). - Quarterly project newsletters communicated key messages, provided information and case studies of successful implementation approaches to common barriers (other). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Proportion of schools with a menu that did not contain foods or beverages restricted for sale under the policy, proportion of schools where healthy canteen items represented more than 50% of menu items. | |
| Measure: Canteen menus were collected and audited by two dietitians independently. | ||
| Results: % implementing a variety of policies and practices: 66.6% (60.5% to 72.6%) | ||
| Yoong, 2016 | ||
| Study characteristics | Design: RCT | |
| Setting: Elementary schools | ||
| Population: NSW, Australia | ||
| n (number of participants) | Baseline: Intervention 36 (schools); Control: 36 (schools) | Follow-up: Intervention: 29 (schools); Control: 24 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: - Consisting of up to four menu audits together with verbal and/or written feedback delivered by Health Promotion Officers as part of routine service delivery in the study region (audit with feedback). - During feedback calls the Health Promotion Officer tailored the discussion to the needs of the Canteen Manager based on previous contact; and monitored their actions and progress toward their goals, set new goals where required, or monitored compliance (continuous quality improvement). - Schools were provided with “Fresh Tastes @ School” resources, healthy food guidelines, a menu planning template, sample policies and menus, pricing guides and a local suppliers buyer’s guide (educational materials). - The specific number of menu audits, feedback reports and calls provided was tailored depending on each school’s compliance with the guidelines and whether menu changes had occurred (tailored interventions). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Proportion of schools having a canteen menu that did not contain any “red” foods or “banned” drinks, proportion of schools having a canteen menu that contained > 50% “green” items. | |
| Measure: Menu audits by trained dietitians | ||
| Results: % implementing a variety of policies and practices: 21.6% (15.6% to 27.5%) | ||
| Young, 2008 | ||
| Study characteristics | Design: RCT | |
| Setting: Middle schools | ||
| Population: Six districts across USA | ||
| n (number of participants) | Baseline: Intervention: 18 (schools); Control: 18 (schools) | Follow-up: Intervention: 18 (schools); Control: 18 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: Health education, PE, science or homeroom teachers attended workshops to teach a series of six lessons that promoted development of behavioral skills associated with physical activity. - PE teachers received instructional materials for PE lessons (educational materials). - PE teachers received regular on-site support to conduct lessons that encouraged active participation of girls during PE classes and to promote out-of-class physical activity (educational outreach visits). - Health education, PE, science or homeroom teachers attended workshops to teach a series of six lessons that promoted development of behavioral skills associated with physical activity (educational meetings). - Collaborations were created between schools, community agencies and staff to increase girl‐focused physical activity programs outside of PE classes (interprofessional education). - Program champions were directed the intervention to enhance its sustainability in the third year (local opinion leaders). - Intervention goals were identified for optimal intervention implementation (local consensus processes). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: average number of physical activity programs, students encouraged for out‐of‐PE‐class physical activity (% of classes), teacher strategies to minimize management time (% classes), students provided with choices (% of classes), students encouraged for in‐class physical activity (% classes), student equipment ratio was appropriate for activity (% classes), group sizes appropriate for activity (% of classes), % of school reporting collaborations. | |
| Measure: Surveys of physical activity program leaders | ||
| Results: % implementing a variety of policies and practices: 9.3% (−6.8% to 55.5%) Average number of physical activity programs taught: 5.1 (−0.4 to 10.6) |
||
| Bremer, 2018 | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Middle schools | ||
| Population: Ontario, Canada | ||
| n (number of participants) | Baseline: Intervention: 19 (classes); Control: 11 (classes) | Follow-up: Intervention: 19 (classes); Control: 11 (classes) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: The intervention consisted of a physical activity (PA) program designed by a national organization with expertise in school-based physical activity programming and delivered in school by teachers. The program was offered to students in grades 4 through 8 and consisted of 20 min of structured PA in school for 20 consecutive weeks. - School teachers and student leaders attended a one-day workshop on how to deliver the program as part of regular school activities and were provided with instructional materials to take back to their school for program delivery (educational meetings). - This workshop was intended to increase teachers’ confidence to implement daily physical activity through the use of the manual and supporting resources (educational materials). |
|
| Comparator description | The remaining teachers were however still expected to provide DPA to their students, as per the Ontario education curriculum. | |
| Implementation outcomes | Outcome: Adherence to the program, student behavior, and physical activity opportunities. | |
| Measure: A 21-item questionnaire was developed for this study. Completed by the homeroom teacher at the last measurement point, it included 3 sections: adherence to the program, student behavior, and physical activity opportunities. | ||
| Results: Quantity physical education lessons: t(27) = −0.23, p = .82 | ||
| Cheung, 2019 | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: Georgia, USA | ||
| n (number of participants) | Baseline: Intervention: 71 (schools); Control: 62 (schools) | Follow-up: Intervention: 71 (schools); Control: 62 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: Power Up for 30 (PU30) is a state-wide initiative to increase PA in school which allows tailoring of the initiative at the school level to encourage 30 min of PA outside physical education each day. - A tailored full-day training based on evidence-based strategies for increasing PA before, during (recess, in-class PA), and after school. PU30 recommended at least one administrator, one PE teacher, and one grade level chair from each school attend the training at an area school (educational meetings).Schools received low- and no-cost resources including exercise DVDs, PowerPoint files, and an online resource guide containing links to web-based PA videos, PA curricula, and integrated PA-academic lessons (educational materials). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Crude mean (standard deviation) minutes of physical activity (PA) offered per week for trained and untrained schools at baseline and follow-up. | |
| Measure: School PA survey adapted from widely used school PA survey tools. PE teachers provided data regarding PE, before school and after schools PA opportunities, while grade teachers provided data regarding recess and in-class PA breaks. | ||
| Results: Crude mean (standard deviation) minutes of physical activity (PA) offered per week:During PE: Baseline: intervention 107.7 (4.4), control 105.6 (5.3)Follow-up: intervention 104.9 (4.3), control 105.5 (5.5)During recess: Baseline: intervention 89.8 (4.2), control 100.3 (3.9)Follow-up: intervention 98.7 (3.6), control 96.2 (3.6)In-class PA: Baseline: intervention 40.5 (2.6), control 30.4 (2.3)Follow-up: intervention 51.9 (2.5), control 36.1 (2.6) | ||
| Egan, 2018 | ||
| Study characteristics: | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: South Eastern state, USA | ||
| n (number of participants): | Baseline: Group 1: 3 (classes); Group 2: 3 (classes); Group 3: 3 (classes); Control: 3 (classes) | Follow-up: Group 1: 3 (classes); Group 2: 3 (classes); Group 3: 3 (classes); Control: 3 (classes) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: PACES is a pilot intervention program focused on increasing children’s PA during regular school hours. It specifically targets two components: (a) physical education and (b) PA during school (i.e. opportunities to be active beyond physical education). We employed three partnership approaches (communities of practice, community-based participatory research, and service learning) based on Webster, Beets et al.’s (2015) partnership model with the aim of providing external support for the participating classroom teachers in the intervention classrooms and, subsequently, increasing the extent of MI in these classrooms. - Community-based participatory research involved a member of the research team meeting with each teacher individually to share baseline PA and MI results (educational outreach visits). - During the meeting, the research team identified current MI strengths and areas for improvement, collaboratively set personalized MI goals, and consider suitable resources, including those posted on the community of practice (audit with feedback). - The community-based participatory research strategy also included identifying each teacher’s specific MI requests and preferences (tailored interventions). - Schools had access to the Move for Thought website, which included educational materials, videos and links (educational materials). |
|
| Comparator description | Group 1: Received the first PACES partnership approach (community of practice); Group 2: Received the first two approaches (community of practice and community-based participatory research); Group 3: Received all three approaches; Control: Usual practice | |
| Implementation outcomes | Outcome: Implementation of teacher directed transition, implementation of other movement - nonacademic, Other movement academic, Non-teacher directed transition | |
| Measure: Twelve research assistants coded video records (n = 57) using the System for Observing Student Movement in Academic Routines and Transitions (SOSMART). | ||
| Results: Total implementation: Group 1: baseline 44.0, follow-up 39.13, change −4.87; Group 2: baseline 50.9, follow-up 54.27, change 3.37; Group 3: baseline 49.63, follow-up 50.73, change 1.10; Control: baseline 36.30, follow-up 35.37, change −0.93Implementation of teacher directed transition: Group 1: baseline 17.83, follow-up 14.87, change −2.97; Group 2: baseline 17.03, follow-up 20.60, change 3.57; Group 3: baseline 24.40, follow-up 21.07, change −3.33; Control: baseline 18.24, follow-up 20.20, change 1.95Implementation of other movement - nonacademic: Group 1: baseline 3.23, follow-up 2.20, change −1.00; Group 2: baseline 1.83, follow-up 4.90, change 3.07; Group 3: baseline 1.20, follow-up 12.50, change 11.33; Control: baseline, 0.59, follow-up 0.00, change -0.59Other movement academic: Group 1: baseline 2.17, follow-up 3.60, change 1.43; Group 2: baseline 0.50, follow-up 1.17, change 0.67; Group 3: baseline 1.43, follow-up 0.80, change -0.63; Control: baseline 1.18, follow-up 5.45, change 4.28Non-teacher directed transition: Group 1: baseline 20.77, follow-up 18.47, change −2.27; Group 2: baseline 31.53, follow-up 27.50, change -4.00; Group 3: baseline 22.67, follow-up 16.37, change −6.30; Control: baseline 16.16, follow-up 9.36, change −6.79 |
||
| Evenhuis, 2018 | ||
| Study characteristics | Design: nonrandomized trial | |
| Setting: Elementary schools | ||
| Population: Netherlands | ||
| n (number of participants) | Baseline: Intervention: 10 (schools); Control: 10 (schools) | Follow-up: Intervention: 10 (schools); Control: 10 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: The intervention schools received support to implement the “Guidelines for Healthier Canteens”; i.e. an advisory meeting and report, communication materials, newsletters, an online community and a factsheet with student’s wishes/needs - Canteen advisors also measured the extent to which canteens met the Guidelines for Healthier Canteens, using the online tool “the Canteen Scan” (audit and feedback) - School canteen advisors provided tailored advice in an advisory meeting (educational outreach visits) - Schools received communication materials, newsletter with information and had access to a closed Facebook community (educational materials). |
|
| Comparator description | Control schools only received the guidelines. | |
| Implementation outcomes | Outcome: Changes in school canteen: product availability on display, vending machines and product accessibility | |
| Measure: Changes in the school canteen were assessed using the “Canteen Scan,” an online tool to measure product availability on displays and vending machines, and product accessibility | ||
| Results: Availability of healthier products on display: (mean) Intervention: baseline 45.80 (27.12), follow-up 77.29 (13.41)*, p = .007; Control: baseline 50.40 (23.00), follow-up 60.10 (15.67), p value not reportedAccessibility criteria: Intervention: baseline 44.00 (20.66), follow-up 60.00 (21.60), p = .03;Control: baseline 43.00 (20.58), follow-up 50.00 (14.91), p value not reported |
||
| Farmer, 2017 | ||
| Study characteristics | Design: Cluster-RCT | |
| Setting: Elementary schools | ||
| Population: Otago and Auckland, New Zealand | ||
| n (number of participants) | Baseline: Intervention: 8 (schools); Control: 8 (schools) | Follow-up: Intervention: 8 (schools); Control: 8 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: The researchers, playworker and school community worked together to develop a playground action plan that met the needs of each school community. Following baseline evaluations of their play space, each intervention school was provided with a list of tailored suggestions for improvements. This was specific to each school but could include the addition of more interactive play equipment, and alterations to school rules and policies that may limit risk-taking during play, with all alterations meeting playground safety standards. The research team met with each school community to finalise the plan. - Provided with funds to assist with altering school play spaces (incentives). - The researchers, playworker and school community worked together to develop a playground action plan that met the needs of each school community (local consensus approach). - School was provided with a list of tailored suggestions for improvements. This was specific to each school but could include the addition of more interactive play equipment, and alterations to school rules and policies that may limit risk-taking during play with all alterations meeting playground safety standards (tailored interventions). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Physical activity policies within their school (break time, using physical activity as a punishment, promotion of community activities, adequacy and availability of facilities during school/after hours, enjoyment and promotion of PA regardless of skill level, amount and quality of physical education, and safety. | |
| Measure: principals completed an 18-item questionnaire assessing physical activity policies within their school. Principals indicated whether the policies were fully in place (score of 3), partially in place (2), under development (1), or not in place (0). | ||
| Results: School policy regarding physical activity: Follow-up: intervention 76.2% (10.4), control 76.4% (10.6), p = .568Provision of play opportunities: mean difference: 4.50 (95% confidence interval: 1.82–7.18, p = .005 |
||
| Nathan, unpublished | ||
| Study characteristics: | Design: Cluster-RCT | |
| Setting: Elementary schools | ||
| Population: Hunter region of New South Wales, Australia | ||
| n (number of participants): | Baseline: Treatment 1: 3 (schools); Treatment 2: 3 (schools); Treatment 3: 3 (schools); Control: 3 (schools) | Follow-up: Treatment 1: 3 (schools); Treatment 2: 3 (schools); Treatment 3: 3 (schools); Control: 3 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: Three key opportunities were targeted to improve physical activity. PE teachers were supported to program PE by developing a sequential plan for each school class. Sport teachers were supported to program sufficient time for sport and maximize student activity. Teachers were supported to integrate short bouts of activity into class routines, such as energizers or active lessons. - Teachers were provided with examples of school and classroom plans that show teachers how to implement 150 min of organized activities consistent with the policy across the school week (educational materials). - Support officers met with all teachers once as a group in each school for 1–2 h to introduce the in-school champion and their role in implementing the intervention and as a point of support in the school; to provide instruction on the development of how to implement 150 min of organized activities consistent with the policy across the school week (educational outreach visits). - Support officers provided technical assistance to schools throughout the study period to support policy implementation (centralized technical assistance). - Support officers met with principals and school executive to communicate the importance and benefits of scheduled PA. Principals and the executive were asked to demonstrate support for implementing the policy (mandate change). - Each school nominated at least 2 in-school champions who were existing teachers at the school (identify and prepare champions). - Support officers provided in-school champions with support remotely, that is,via telephone or e-mail twice per term to support implementing the intervention (other). |
|
| Comparator description | Treatment 1: PA support; Treatment 2: Lunchbox support; Treatment 3: Both PA support and lunchbox support; Control: Usual practice | |
| Implementation outcomes | Outcome: Mean minutes of teachers’ scheduled PA | |
| Measure: at the end of each day for one school week teachers completed a paper-based log book. This included the time they engaged in all teaching activities across all subjects each day including the duration PA was provided. | ||
| Results: Mean minutes of teachers’ scheduled PA: Follow-up: intervention 135.95 (59.46), control 99.04 (51.83), p = .04 | ||
| Taylor, 2018 | ||
| Study characteristics | Design: Cluster-RCT | |
| Setting: Elementary schools | ||
| Population: Northern California, USA | ||
| n (number of participants) | Baseline: Intervention: 1 (schools); Control: 1 (schools) | Follow-up: Intervention: 1 (schools); Control: 1 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Intervention description: Incorporates 5 program objectives: (1) increase nutrition knowledge and use of science processing skills among fourth-grade children; (2) promote availability, consumption, and enjoyment of fruits and vegetables in the school environment; (3) improve dietary patterns and encourage physical activity; (4) foster positive changes in the school environment; and (5) facilitate development of an infrastructure to sustain the program. - The school district was provided $3000 to increase procurement of regionally grown produce for use in the National School Lunch Program (incentives). - Program activities included 20 hr of classroom education using an inquiry-based, garden-enhanced nutrition curriculum (educational outreach visits). - Take-home activities, materials and family newsletters (educational materials). |
|
| Comparator description | Usual practice or waitlist control | |
| Implementation outcomes | Outcome: Fruit and vegetable availability | |
| Measure: Based on produce expenditures and variety for use in the schools. Procurement records were used to determine how many different types of fruits and vegetables were offered | ||
| Results: Fruit offered daily by schools: Baseline: 4.33 ± 0.82 control, 4.80 ± 1.10 intervention, p = .44; Follow-up: 4.17 ± 0.75 control, 4.17 ± 0.98, p = 1.00Vegetables offered daily by schools: Baseline:2.67 ± 0.52 control, 5.40 ± 1.95 intervention, p = .03; Follow-up: 3.00 ± 0.89 control, 8.33 ± 0.82 intervention, p < .001 |
||
| Waters, 2017 | ||
| Study characteristics | Design: Cluster-RCT | |
| Setting: Elementary schools | ||
| Population: Northern California, USA | ||
| n (number of participants) | Baseline: Intervention: 12 (schools); Control: 12 (schools) | Follow-up: Intervention: 12 (schools); Control: 10 (schools) |
| Intervention description(implementation strategy categorized by EPOC) | Schools were supported to develop fun “n healthy programs according to the fixed requirement of a whole school combined focus on increasing fruit, vegetable and water consumption, increasing physical activity and encouraging self-esteem in children. - The school community determined the exact content of the program strategies (tailored interventions and local consensus approach) - Community Development Workers acted as knowledge brokers, providing information and guiding schools’ customized development of intervention program strategies and their efforts to resource them (educational outreach visits and educational materials). |
|
| Comparator description | Usual practice | |
| Implementation outcomes | Outcome: Proportion of schools with written physical activity, healthy eating and canteen policies | |
| Measure: School principals were asked to report on whether their school had policies relating to physical activity and canteen | ||
| Results: Proportion of schools with physical activity policy: Control: baseline 7 (70%), follow-up 6 (60%); Intervention: baseline 8 (66.6%), follow-up 11 (91.7%)Proportion of schools with healthy eating policy: Control: follow-up 2 (20%); Intervention: follow-up 9 (75%)Proportion of schools with canteen policy: Control: baseline 4 (40%), follow-up 6 (60%); Intervention: baseline 2 (16.7%), follow-up 3 (25%) |
||
Funding: We would like to acknowledge the funding support provided by New South Wales Office Preventive Health. C.B. is supported by a cofunded industry scholarship between Hunter New England Population Health and the University of Newcastle; N.N. is supported by a Hunter New England Clinical Research Fellowship; S.Y. is funded by an Australian Research Council Discovery Early Career Researcher Award (DECRA) (DE170100382); R.S. is supported by a National Health and Medical Research Council Translating Research into Practice Fellowship (APP1150661); L.W. is a Hunter New England Clinical Research Fellow and is supported by Heart Foundation Future Leader Fellowship (Award No. 101175) and a National Health and Medical Research Council Career Development Fellowship (APP1128348).
Compliance with Ethical Standards
Conflicts of Interest: Several members of the review team are currently undertaking a series of randomized controlled trials within the school setting. L.W., N.N., R.S., S.L.Y., and R.H. are authors of one or more studies included in the review. For such studies, data were extracted by review authors who were not directly involved in these studies. Authors declare no other potential competing interests.
Authors’ Contributions: All review authors contributed to the conduct of the research. L.W. and C.B. led the development of the review. C.B. and F.S. contributed to the selection of studies. C.B., F.S., and S.Mc. contributed to data extraction and management. C.B. and S.Mc. contributed to the assessment of the risk of bias of included studies. C.B. led the drafting of the manuscript. All authors contributed to the interpretation of review findings and provided critical comment on drafts.
Ethical Approval: This article does not contain any studies with human participants performed by any of the authors. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: This study does not involve human participants and informed consent was, therefore, not required.
Transparency statement: This review aligns with the reporting guidelines specified within the 2009 PRISMA checklist for systematic reviews and utilized Cochrane methodology. The completed 2009 PRISMA checklist for systematic reviews has been provided in Supplementary File I.
References
- 1. Global Disease Collaborators. Health effects of dietary risks in 195 countries, 19902017: A systematic analysis for the Global Burden of Disease Study 2017. 2019;393(10184):1958–1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Burrows TL, Whatnall MC, Patterson AJ, Hutchesson MJ. Associations between dietary intake and academic achievement in college students: A systematic review. Healthcare (Basel). 2017;5(4):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. O’Neil A, Quirk SE, Housden S, et al. . Relationship between diet and mental health in children and adolescents: A systematic review. Am J Public Health. 2014;104(10):e31–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lubans D, Richards J, Hillman C, et al. . Physical activity for cognitive and mental health in youth: A systematic review of mechanisms. Pediatrics. 2016;138(3):e20161642. [DOI] [PubMed] [Google Scholar]
- 5. Singh A, Uijtdewilligen L, Twisk JW, van Mechelen W, Chinapaw MJ. Physical activity and performance at school: A systematic review of the literature including a methodological quality assessment. Arch Pediatr Adolesc Med. 2012;166(1):49–55. [DOI] [PubMed] [Google Scholar]
- 6. Donnelly JE, Hillman CH, Castelli D, et al. . Physical Activity, fitness, cognitive function, and academic achievement in children: A systematic review. Med Sci Sports Exerc. 2016;48(6):1197–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. OECD. The Heavy Burden of Obesity: The Economics of Prevention. Paris, France: OECD Publishing; 2019. [Google Scholar]
- 8. Swinburn BA, Sacks G, Hall KD, et al. . The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization. Population based approaches to childhood obesity prevention. 2012. Available at www.who.int/dietphysicalactivity/childhood/WHO_new_childhoodobesity_PREVENTION_27nov_HR_PRINT_OK.pdf. Accessibility verified May 12, 2020.
- 10. World Health Organization. Population-based approaches to childhood obesity prevention. 2012. Available at https://www.who.int/dietphysicalactivity/childhood/approaches/en/. Accessibility verified May 12, 2020.
- 11. World Health Organization. Report of the Commission on Ending Childhood Obesity. Implementation Plan: Executive Summary. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 12. Demetriou Y, Höner O. Physical activity interventions in the school setting: A systematic review. Psychol Sport Exerc. 2012;13(2):186–196. [Google Scholar]
- 13. Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: An update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev. 2009;10(1):110–141. [DOI] [PubMed] [Google Scholar]
- 14. Liu Z, Xu HM, Wen LM, et al. . A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int J Behav Nutr Phys Act. 2019;16(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Australian Government Department of Health and Ageing. National Healthy School Canteens Pocket Guide. 2013. Available at https://www1.health.gov.au/internet/main/publishing.nsf/Content/nhsc-pocket-guide. Accessibility verified May 12, 2020. [Google Scholar]
- 16. Public Health England. What works in schools and colleges to increase physical activity?2020. Available at https://assets.publishing.service.gov.uk/. Accessibility verified May 12, 2020.
- 17. Society of Health and Physical Educators. National Guidelines 2019. Available at https://www.shapeamerica.org/. Accessibility verified May 12, 2020.
- 18. Government of Canada. Healthy eating at school 2019. Available at https://food-guide.canada.ca/en/tips-for-healthy-eating/school/. Accessibility verified May 12, 2020.
- 19. NSW Government. Sport and Physical Activity Policy 2020. Available at https://policies.education.nsw.gov.au/policy-library/policies/sport-and-physical-activity-policy. Accessibility verified May 14, 2020.
- 20. Harrington DM, Belton S, Coppinger T, et al. . Results from Ireland’s 2014 Report Card on physical activity in children and youth. J Phys Act Health. 2014;11(suppl 1):S63–S68. [DOI] [PubMed] [Google Scholar]
- 21. Yoong SL, Nathan NK, Wyse RJ, et al. . Assessment of the school nutrition environment: A study in australian primary school canteens. Am J Prev Med. 2015;49(2):215–222. [DOI] [PubMed] [Google Scholar]
- 22. Chriqui JF, Resnick EA, Schneider L, Schermbeck R.. School District Wellness Policies: Evaluating Progress and Potential for Improving Children’s Health Five Years After the Federal Mandate. Chicago, IL: Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago; 2013. [Google Scholar]
- 23. Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: Current and future directions. Am J Public Health. 2012;102(7):1274–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brownson RC, Colditz GA, Proctor EK.. Dissemination and Implementation Research in Health: Translating Science to Practice. London: Oxford University Press; 2012. [Google Scholar]
- 25. Wolfenden L, Nathan NK, Sutherland R, et al. . Strategies for enhancing the implementation of school‐based policies or practices targeting risk factors for chronic disease. Cochrane Database Syst Rev. 2017;11(11):CD011677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bremer E, Graham JD, Veldhuizen S, Cairney J. A program evaluation of an in-school daily physical activity initiative for children and youth. BMC Public Health. 2018;18(1):1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Waters E, Gibbs L, Tadic M, et al. . Cluster randomised trial of a school-community child health promotion and obesity prevention intervention: Findings from the evaluation of fun ‘n healthy in Moreland! BMC Public Health. 2017;18(1):92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Egan CA. Two studies of partnership approaches to comprehensive school physical activity programming: A process evaluation and a case study. Diss Abstr Int Section A Humanit Soc Sci. 2018;78(11-A(E)):64–112. [Google Scholar]
- 29. Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schillinger D. An Introduction to Effectiveness, Dissemination and Implementation Research. UCSF Clinical and Translational Science Institute (CTSI) Resource Manuals and Guides to Community-Engaged Research. San Francisco, CA: University of California; 2010. [Google Scholar]
- 31. Australian Institute of Health Welfare. Australia’s Children. Canberra, Australia: AIHW; 2020. [Google Scholar]
- 32. Effective Practice and Organisation of Care. The EPOC Taxonomy of Health Systems Interventions. EPOC Resources for Review Authors. Oslo, Finland: Norwegian Knowledge Centre for the Health Services. 2016. Available at epoc.cochrane.org/epoc-taxonomy. Accessibility verified May 26, 2020. [Google Scholar]
- 33. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Chichester: The Cochrane Collaboration; 2011. [Google Scholar]
- 34. Bilandzic A, Fitzpatrick T, Rosella L, Henry D. Risk of bias in systematic reviews of non-randomized studies of adverse cardiovascular effects of thiazolidinediones and cyclooxygenase-2 inhibitors: Application of a new cochrane risk of bias tool. PLoS Med. 2016;13(4):e1001987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wolfenden L, Barnes C, Jones J, et al. . Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst Rev. 2020;2(2):CD011779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wolfenden L, Goldman S, Stacey FG, et al. . Strategies to improve the implementation of workplace‐based policies or practices targeting tobacco, alcohol, diet, physical activity and obesity. Cochrane Database Syst Rev. 2018;11(11):CD012439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nathan NK, Sutherland RL, Hope K, et al. . Implementation of a school physical activity policy improves student physical activity levels: Outcomes of a cluster-randomized controlled trial. J Phys Act Health. 2020;17(10):1009–1018. [DOI] [PubMed] [Google Scholar]
- 38. Cheung P, Franks P, Kramer M, et al. . Impact of a Georgia elementary school-based intervention on physical activity opportunities: A quasi-experimental study. J Sci Med Sport. 2019;22(2):191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Egan CA, Webster C, Weaver RG, et al. . Partnerships for Active Children in Elementary Schools (PACES): First year process evaluation. Eval Program Plann. 2018;67:61–69. [DOI] [PubMed] [Google Scholar]
- 40. Evenhuis IJ, Vyth EL, Jacobs S, Veldhuis L, Seidell JC, Renders CM. Does implementation of guidelines for healthier school canteens result in changes in canteens and healthier purchase behaviour of students? Obesity Facts. 2018;11(suppl 1):119–120. [Google Scholar]
- 41. Farmer VL, Williams SM, Mann JI, Schofield G, McPhee JC, Taylor RW. The effect of increasing risk and challenge in the school playground on physical activity and weight in children: A cluster randomised controlled trial (PLAY). Int J Obes (Lond). 2017;41(5):793–800. [DOI] [PubMed] [Google Scholar]
- 42. Taylor JC, Zidenberg-Cherr S, Linnell JD, Feenstra G, Scherr RE. Impact of a multicomponent, school-based nutrition intervention on students’ lunchtime fruit and vegetable availability and intake: A pilot study evaluating the Shaping Healthy Choices Program. J Hunger Environ Nutr. 2018;13(3):415–428. [Google Scholar]
- 43. Alaimo K, Carlson JJ, Pfeiffer KA, et al. . Project FIT: A school, community and social marketing intervention improves healthy eating among low-income elementary school children. J Community Health. 2015;40(4):815–826. [DOI] [PubMed] [Google Scholar]
- 44. Cunningham-Sabo L, Lohse B, Smith S, et al. . Fuel for Fun: A cluster-randomized controlled study of cooking skills, eating behaviors, and physical activity of 4th graders and their families. BMC Public Health. 2016;16:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Delk J, Harrell MB, Fakhouri THI, Muir KA, Perry CL. Implementation of a computerized tablet-survey in an adolescent large-scale, school-based study. J Sch Health. 2017;87(7):506–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Delk J, Springer AE, Kelder SH, Grayless M. Promoting teacher adoption of physical activity breaks in the classroom: findings of the Central Texas CATCH Middle School Project. J Sch Health. 2014;84(11):722–730. [DOI] [PubMed] [Google Scholar]
- 47. French SA, Story M, Fulkerson JA, Hannan P. An environmental intervention to promote lower-fat food choices in secondary schools: Outcomes of the TACOS Study. Am J Public Health. 2004;94(9):1507–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Heath EM, Coleman KJ. Evaluation of the institutionalization of the coordinated approach to child health (CATCH) in a U.S./Mexico border community. Health Educ Behav. 2002;29(4):444–460. [DOI] [PubMed] [Google Scholar]
- 49. Hoelscher DM, Springer AE, Ranjit N, et al. . Reductions in child obesity among disadvantaged school children with community involvement: The Travis County CATCH Trial. Obesity (Silver Spring). 2010;18(suppl 1):S36–S44. [DOI] [PubMed] [Google Scholar]
- 50. Lytle LA, Kubik MY, Perry C, Story M, Birnbaum AS, Murray DM. Influencing healthful food choices in school and home environments: Results from the TEENS study. Prev Med. 2006;43(1):8–13. [DOI] [PubMed] [Google Scholar]
- 51. Mobley CC, Stadler DD, Staten MA, et al. ; HEALTHY Study Group . Effect of nutrition changes on foods selected by students in a middle school-based diabetes prevention intervention program: The HEALTHY experience. J Sch Health. 2012;82(2):82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nathan N, Wolfenden L, Bell AC, et al. . Effectiveness of a multi-strategy intervention in increasing the implementation of vegetable and fruit breaks by Australian primary schools: A non-randomized controlled trial. BMC Public Health. 2012;12:651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Nathan N, Yoong SL, Sutherland R, et al. . Effectiveness of a multicomponent intervention to enhance implementation of a healthy canteen policy in Australian primary schools: A randomised controlled trial. Int J Behav Nutr Phys Act. 2016;13(1):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Naylor PJ, Macdonald HM, Reed KE, McKay HA. Action Schools! BC: A socioecological approach to modifying chronic disease risk factors in elementary school children. Prev Chronic Dis. 2006;3(2):A60. [PMC free article] [PubMed] [Google Scholar]
- 55. Perry CL, Bishop DB, Taylor GL, et al. . A randomized school trial of environmental strategies to encourage fruit and vegetable consumption among children. Health Educ Behav. 2004;31(1):65–76. [DOI] [PubMed] [Google Scholar]
- 56. Perry CL, Sellers DE, Johnson C, et al. . The Child and Adolescent Trial for Cardiovascular Health (CATCH): Intervention, implementation, and feasibility for elementary schools in the United States. Health Educ Behav. 1997;24(6):716–735. [DOI] [PubMed] [Google Scholar]
- 57. Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell MF. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, Play and Active Recreation for Kids. Am J Public Health. 1997;87(8):1328–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Story M, Mays RW, Bishop DB, et al. . 5-a-day Power Plus: process evaluation of a multicomponent elementary school program to increase fruit and vegetable consumption. Health Educ Behav. 2000;27(2):187–200. [DOI] [PubMed] [Google Scholar]
- 59. Simons-Morton BG, Parcel GS, O’Hara NM. Implementing organizational changes to promote healthful diet and physical activity at school. Health Educ Q. 1988;15(1):115–130. [DOI] [PubMed] [Google Scholar]
- 60. Sutherland RL, Nathan NK, Lubans DR, et al. . An RCT to facilitate implementation of school practices known to increase physical activity. Am J Prev Med. 2017;53(6):818–828. [DOI] [PubMed] [Google Scholar]
- 61. Whatley Blum JE, Davee AM, Devore RL, et al. . Implementation of low-fat, low-sugar, and portion-controlled nutrition guidelines in competitive food venues of Maine public high schools. J Sch Health. 2007;77(10):687–693. [DOI] [PubMed] [Google Scholar]
- 62. Wolfenden L, Nathan N, Janssen LM, et al. . Multi-strategic intervention to enhance implementation of healthy canteen policy: A randomised controlled trial. Implement Sci. 2017;12(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Yoong SL, Nathan N, Wolfenden L, et al. . CAFÉ: a multicomponent audit and feedback intervention to improve implementation of healthy food policy in primary school canteens: A randomised controlled trial. Int J Behav Nutr Phys Act. 2016;13(1):126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Young DR, Steckler A, Cohen S, et al. . Process evaluation results from a school- and community-linked intervention: The Trial of Activity for Adolescent Girls (TAAG). Health Educ Res. 2008;23(6):976–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Taylor SL, Noonan RJ, Knowles ZR, et al. . Evaluation of a pilot school-based physical activity clustered randomised controlled trial-active schools: skelmersdale. Int J Environ Res Public Health. 2018;15(5):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Saunders RP, Ward D, Felton GM, Dowda M, Pate RR. Examining the link between program implementation and behavior outcomes in the lifestyle education for activity program (LEAP). Eval Program Plann. 2006;29(4):352–364. [DOI] [PubMed] [Google Scholar]
- 67. Evenhuis IJ, Jacobs SM, Vyth EL, et al. . The effect of supportive implementation of healthier canteen guidelines on changes in Dutch school canteens and student purchase behaviour. Nutrients. 2020;12(8):2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Bell LL. Grandparents Raising Grandchildren in the 21st Century [PhD dissertation]. Ann Arbor, MI: Mississippi State University; 2018. [Google Scholar]
- 69. Love R, Adams J, van Sluijs EMF. Are school-based physical activity interventions effective and equitable? A systematic review and meta-analysis of cluster randomised controlled trials. Lancet. 2018;392:S53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. World Health Organisation. School and youth health 2020. Available at https://www.who.int/school_youth_health/gshi/hps/en/. Accessibility verified May 26, 2020.
- 71. National Health and Medical Research Council. Nutrient Reference Values Canberra2020. Available at https://www.nrv.gov.au/. Accessibility verified May 14, 2020.
- 72. Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: Where do we go from here? Science. 2003;299(5608):853–855. [DOI] [PubMed] [Google Scholar]
- 73. Braun HA, Kay CM, Cheung P, Weiss PS, Gazmararian JA. Impact of an elementary school-based intervention on physical activity time and aerobic capacity, Georgia, 2013–2014. Public Health Rep. 2017;132(2_suppl):24S–32S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: A systematic review of use over time. Am J Public Health. 2013;103(6):e38–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Glasgow RE, Huebschmann AG, Brownson RC. Expanding the CONSORT Figure: Increasing transparency in reporting on external validity. Am J Prev Med. 2018;55(3):422–430. [DOI] [PubMed] [Google Scholar]
- 76. Powell BJ, Waltz TJ, Chinman MJ, et al. . A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.