Abstract
Background
Patients presenting with the coronavirus-2019 disease (COVID-19) may have a high risk of cardiovascular adverse events, including death from cardiovascular causes. The long-term cardiovascular outcomes of these patients are entirely unknown. We aim to perform a registry of patients who have undergone a diagnostic nasopharyngeal swab for SARS-CoV-2 and to determine their long-term cardiovascular outcomes.
Study and design
This is a multicenter, observational, retrospective registry to be conducted at 17 centers in Spain and Italy (ClinicalTrials.gov number: NCT04359927). Consecutive patients older than 18 years, who underwent a real-time reverse transcriptase-polymerase chain reaction (RT-PCR) for SARS-CoV2 in the participating institutions, will be included since March 2020, to August 2020. Patients will be classified into two groups, according to the results of the RT-PCR: COVID-19 positive or negative. The primary outcome will be cardiovascular mortality at 1 year. The secondary outcomes will be acute myocardial infarction, stroke, heart failure hospitalization, pulmonary embolism, and serious cardiac arrhythmias, at 1 year. Outcomes will be compared between the two groups. Events will be adjudicated by an independent clinical event committee.
Conclusion
The results of this registry will contribute to a better understanding of the long-term cardiovascular implications of the COVID19.
Introduction
Since Coronavirus disease 2019 (COVID-19) was first reported in China in late December 2019, it has spread rapidly worldwide, and it has become a pandemic affecting more than 200 countries. The exponential increase in the number of COVID-19 patients has overwhelmed health-care systems in many countries across the world, with an unprecedented effect not only on public health, but also on social and economic activities.
COVID-19 is caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Currently, it is known that SARS-CoV-2 can produce a multi-system affectation, including cardiovascular system [1]. This virus enters the cells by binding of the viral spike (S) protein to angiotensin-converting enzyme 2 (ACE2) on the surface of the host cell. The ACE2 is highly expressed in pulmonary tissues, but also in adult human hearts and endothelial cells, indicating an intrinsic susceptibility of these organs to a direct invasion of SARS-CoV-2. Furthermore, SARS-CoV-2 probably produces a downregulation in the ACE2 activity, reducing the conversion of angiotensin II (Ang II) to Ang-(1–7). This may increase Ang II activity, which continues stimulating renin-angiotensin-aldosterone system (RAAS) with deleterious effects on heart and blood vessels [2–4].
An exacerbated inflammatory response with cytokine storm mediated through pathologic T cells and monocytes leading to myocarditis, is another possible mechanism postulated to explain cardiac injury due to COVID-19 [5, 6]. The pro-inflammatory environment and endothelial dysfunction can also trigger the development of coagulopathy. Hypercoagulability leads to coronary macro and microvascular thrombosis, and high incidence of thromboembolic events in venous territories [7–9].
We currently know that myocardial injury is related with worse in-hospital prognosis in COVID-19 patients [10–12]. A study of 26 patients recovered from COVID-19 evaluated with cardiac resonance showed myocardial edema, fibrosis, and impaired right ventricle function [13]. Available data suggests a probable implication on prognosis, but long-term implications of COVID-19 on cardiovascular events are completely unknown.
The Cardiovascular COVID-19 (CV COVID-19) registry will aim to a better understanding of the long-term cardiovascular implications in patients who had a SARS-CoV-2 infection.
Methods
Study design
It is a multicenter, observational, retrospective registry to be conducted at 17 centers in Spain and Italy. This study is an investigator-initiated registry, and the promoter is the Fundació Clínic per a la Recerca Biomédica. Table 1 shows the list of enrolling centers and their principal investigators. The detailed list of the study staff is in the S1 File.
Table 1. Centers and investigators.
| Centers | Investigators |
|---|---|
| Hospital Universitari Clínic de Barcelona | Dr. Luis Ortega-Paz |
| Hospital Universitari Sagrat Cor | Dr. Gabriela Bastidas |
| Hospital Universitari de Bellvitge | Dr. Josep Gómez-Lara |
| Hospital Marqués de Valdecilla | Dr. José María de la Torre |
| Hospital Universitario Juan Ramón Jiménez | Dr. Antonio Gómez-Menchero, Dr. José Francisco Díaz Fernández |
| Hospital Universitario La Princesa | Dr. Fernando Alfonso |
| Hospital Universitari Vall d’Hebron | Dr. Jordi Bañeras Rius |
| Hospital Clínico Universitario de Valladolid | Dr. Ignacio Jesús Amat-Santos |
| Hospital Universitario de León | Dr. Miguel Rodríguez-Santamarta |
| Hospital Universitario de Vigo | Dr. Victor Alfonso Jimenez-Díaz |
| Hospital Universitario Clínico San Carlos | Dr. Nieves Gonzalo |
| Istituto Clinico Sant’Ambrogio | Dr. Alfonso Ielasi |
| Azienda Ospedaliero-Universitaria di Ferrara | Dr. Gianluca Campo |
| Hospital de Tortosa Verge de la Cinta | Dr. Alberto Pernigotti |
| Ospedale Bolognini di Seriate | Dr. Antonio Silvestro |
| Hospital Universitari Arnau de Vilanova | Dr. Diego Fernández-Rodríguez |
| Hospital Universitari Joan XXIII | Dr. Claudia Scardino |
The Registry does not test clinical interventions, and individual patient care is entirely at the discretion of treating clinicians.
This study adhered to the principles outlined in the Declaration of Helsinki. Approval was given by the “Comité de Ética de la Investigación con medicamentos del Hospital Clínic de Barcelona” (Ethics Committee for Drug Research of the Hospital Clínic of Barcelona) with the registry HCB/2020/0457, on April 16, 2020. Given the registry’s anonymous characteristics and the health alarm situation generated by the COVID-19 pandemic, written informed consent was waived.
The study is registered at ClinicalTrials.gov (NCT number: NCT04359927).
Patient selection
Inclusion criteria are:
At least 18 years of age.
Patient who underwent a nasopharyngeal swab for real-time reverse transcriptase-polymerase chain reaction (RT-PCR) for SARS-CoV2 between March 2020 and August 2020.
Exclusion criteria are:
Those with terminal diseases and a life expectancy <1 year before the diagnosis will be excluded.
Patients will be classified into two groups: patients with confirmed COVID-19 (positive RT-PCRT for SARS-CoV-2) and patients without COVID-19 (negative RT-PCR for SARS-CoV2, and absence of absence of suspicious symptoms).
Data capture
Study data will be collected and managed using REDCap electronic data capture tools hosted at Hospital Clínic of Barcelona (redcap.clinic.cat). REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.
An anonymized and predefined electronic Case Report Form (eCRF) developed by the investigators will be filled by each participating center. The selected variables are oriented to the cardiovascular risk factors, conditions, medications, and outcomes (Table 2). Moreover, based on the current scientific literature, specific COVID-19 variable and treatment will be also collected. Charlson Comorbidity Index (CCI) will be used to assess patient’s comorbidities. CCI is a validated index for predicting life expectancy at ten years, depending on the age at which it is evaluated, and on the subject’s comorbidities [14]. The detailed eCRF format can be seen in the S2 File.
Table 2. Data to be obtained in the timeline of the study.
| Baseline characteristics | Acute phase | Long-term (until 1 year) |
|---|---|---|
| Demographic data • Age • Sex Risk factors and baseline comorbidities • Hypertension • Diabetes mellitus • Hypercholesterolemia • Smoking status • Kidney chronic disease • Previous ACS • Previous Stroke • Heart failure • Atrial fibrillation • Previous PE and DVT • Cancer • Organ transplant • Immunosupresion • Frailty Charlson Comorbidity Index Baseline medication • Anti-hypertensive drugs and cardiovascular medication • Chronic anticoagulation • Oral hypoglycemic agents • Insulin • Proton pump inhibitors • NSAIDs |
Symptoms Hospitalization • Length of stay Drugs: • Anti-hypertensive drugs and cardiovascular medication. • Anticoagulation • Antivirals • Immunosuppressive drugs • Vasopressors • ICU admission • Invasive mechanical ventilation Biomarkers • Hemoglobin* • Lymphocytes* • Platelets* • Creatinine** • HscTnI** • NT-proBNP** • D-dimer** • Fibrinogen* • Prothrombin time** In-hospital events: • All-cause death • Cardiovascular death • ACS • Stroke • DVT and PE • Cardiac arrhytmias • Bleeding • Red blood cell transfusion Discharge medication |
New SARS-CoV-2 infection Vaccination against SARS-CoV-2 Outcomes • All cause death • Cardiovascular death • ACS • Stroke • Heart failure hospitalization • PE • Cardiac arrhytmias |
ACS, acute coronary syndrome; DVT, deep venous thrombosis; Hs-cTnI, high sensitivity cardiac troponin I; NSAIDs, non-steroidal anti-inflammatory drugs; PE, pulmonary embolism.
*Lowest values during hospitalization.
*Highest values during hospitalization.
All the data will be obtained from electronic records (medical history). If deemed necessary, the investigator may check the patient vital status in the social national security database.
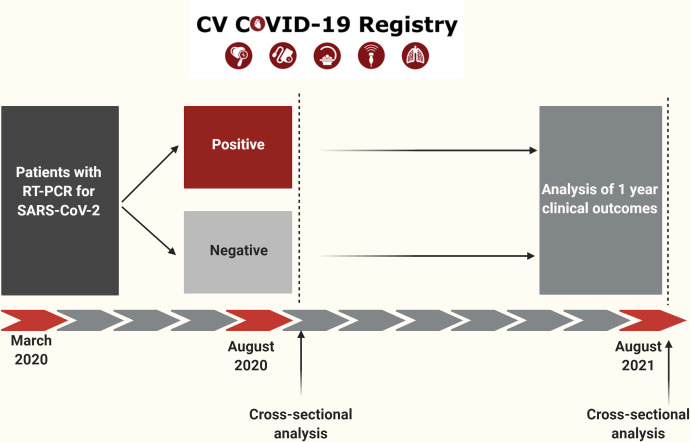
Clinical follow-up will be performed at 1-year. The flowchart and study timeline are detailed in Fig 1.
Fig 1. Timeline of the study.
Inclusion of the patients will be since March to August 2020. Analysis of the clinical outcomes will be performed in August 2021.
Monitoring
Independent study monitors (Effice, Madrid, Spain) verified the adequacy of the follow-up and events reported, conducting auditing in a random sample of 10% of all patients included. All events were adjudicated and classified by an independent event adjudication committee (S1 Table) blinded to the treatment groups by reviewing source documents (including angiograms) provided by each center (Barcicore Lab, Barcelona, Spain).
Outcomes and definitions
The primary outcome will be:
Cardiovascular mortality at 1-year follow-up, defined according to the Academic Research Consortium-2 [15].
The secondary outcomes will be:
Myocardial infarction: defined according to the Academic Research Consortium-2 [15].
Stroke: defined according to the Academic Research Consortium-2 [15].
Heart failure hospitalization must be documented in the diagnosis of the hospitalization discharge letter.
Pulmonary embolism must be documented with a computed tomography.
Cardiac arrhythmias must be documented in the diagnosis of the hospitalization discharge letter. Serious cardiac arrhythmias were defined as: bradycardia requiring intravenous medication or pacemaker, supraventricular tachycardia requiring intravenous medication or cardioversion, or ventricular tachycardia requiring intravenous medication or cardioversion.
Major bleeding was defined as a type 3 of the Bleeding Academic Research Consortium (BARC) or higher [16].
All the events will be independently adjudicated by a Clinical Events Committee. The Clinical Event Committee (CEC) consists of cardiologists not participating in the trial. The CEC members will be blinded to PCR COVID of the patient.
Statistical analysis plan
We did not estimate a precise sample size, due to lack of literature reports and we aim to get the maximum numbers of patients possible.
Continuous variables will be presented as mean ± standard deviation. Categorical variables will be reported as absolute number and percentage. Differences in proportions will be tested with Chi-square test or Fishers exact test and differences in continuous variables will be tested with a Student’s t-test. Kaplan-Meier method will be used to derive the event rates at follow-up and to plot time-to-event curves. Patients not eligible for 1-year follow-up will be considered at risk until the date of last contact, at which point they will be censored.
To determine the predictors of cardiovascular death, a Cox proportional hazards model will be used together with the Wald test to compare the results between the groups (patients with positive vs. negative RT-PCR for SARS-CoV-2).
All p-values will be two-sided and a value <0.05 will be considered statistically significant. All data will be processed using the Statistical Package for Social Sciences, version 22 (SPSS Inc., Chicago, IL, USA).
Discussion
In this multicenter, observational, retrospective registry, we aim of investigate the long-term cardiovascular implications of COVID-19. Currently is known that the presence of myocardial injury, vascular dysfunction and thrombosis in patients with COVID-19 have an important role in the short-term prognosis in these patients [9]. Previous experience with the severe acute respiratory syndrome coronavirus-1 (SARS-CoV-1) emerged in 2002, suggests that both the underlying disease and its treatment could be associated with a worse cardiovascular prognosis. In a study of 25 survivors of SARS-CoV-1, at 12 years of follow-up, altered lipid metabolism was found [17]. Similarly, viral diseases such as influenza A are associated with increased cardiovascular mortality after infection [18].
The focus of this registry will be on the cardiovascular outcomes, providing data not only about cardiac ischemic events but also arrhythmias, cerebrovascular events and heart failure. It should be highlighted that our findings will be applicable to any COVID19 patient, regardless of the severity of the disease, as we will be including a consecutive population of patients with COVID-19 infection. Confirmed cases will be evaluated and compared with those patients who did not have COVID-19 infection. This approach will offer a greater security at the moment of assessing study’s findings. This control group will help to minimize bias that would arise if only COVID-19 patients were independently analyzed. Cox regression will help to distinguish the independent predictors for mortality among the patients of the study. However, considering that a proportion of the SARS-CoV-2 infections can be asymptomatic, there can be a degree of bias if the control patients (non-COVID-19 group) become infected but exhibit an asymptomatic disease during follow-up. Nevertheless, potential patients fulfilling these characteristics can represent a minimal part of the sample size.
It is important to mention as strength of the study, that the events will be adjudicated by an independent committee blinded to the patients’ treatment allocation and trial results. This will guarantee a better evaluation of the study events.
Conclusion
The results of the CV COVID-19 registry will contribute to a better understanding of the short and long-term implications of this disease. It will provide information about cardiovascular mortality and cardiac events at one year of follow-up. Also, it will identify characteristics associated with higher incidence of complications, defining a profile of COVID-19 patients with worse prognosis.
Supporting information
(DOCX)
(DOCX)
(PDF)
(PDF)
Acknowledgments
The authors would like to thank to the CV COVID-19 registry investigators of each center of the study:
Hospital Clínic, Barcelona, Spain: Juan José Rodríguez-Arias, Margarita Calvo, Leticia Castrillo, Anthony Salazar, Marta Sabaté Tormos, and Francesco Spione.
Hospital Universitari Arnau de Vilanova, Lérida, Spain: Pastor Pueyo.
Complejo Hospitalario Universitario de Vigo, Vigo, Spain: Antonio Esmo, María Pena, Ubaldo Hernández, Moya Halley, Enrique Enzo, and Pablo Juan.
Hospital Vall’ de Hebron, Barcelona, Spain: Pablo Jordán, Montse Bach, and Eduard Rodenas.
Azienda Ospedaliero-Universitaria di Ferrara, Ferrara, Italy: Ottavio Zuchetti.
Hospital Universitario de León, León, Spain: Julio Echarte Morales, Samuel del Castillo García, and Carlos Minguito Carazo
Hospital Juan Ramón Jiménez, Huelva, Spain: José Francisco Díaz Fernández and Josefa García.
Hospital Clínico San Carlos, Madrid, Spain: Zaira Gómez and Teresa Romero.
Hospital Clínico Universitario de Valladolid, Valladolid, Spain: Alvaro Aparisi.
Hospital Marqués de Valdecilla, Santander, Spain: Manuel Lozano and Miguel Molina.
Hospital de Bellvitge, Barcelona, Spain: Loreto Oyarzabal.
They will be collaborating to collect all the necessary data to complete the present study.
Funding Statement
SB. Research grant (COV20/00040) from the Carlos III Institute, Madrid, Spain. https://www.isciii.es/Paginas/Inicio.aspx The funders had and will not have a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol. 2020;251(3):228–48. Epub 2020/05/18. doi: 10.1002/path.5471 ; PubMed Central PMCID: PMC7276767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. 2020;116(6):1097–100. Epub 2020/04/01. doi: 10.1093/cvr/cvaa078 ; PubMed Central PMCID: PMC7184507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39(7):618–25. Epub 2009/05/21. doi: 10.1111/j.1365-2362.2009.02153.x ; PubMed Central PMCID: PMC7163766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–8. Epub 2020/04/24. doi: 10.1016/S0140-6736(20)30937-5 ; PubMed Central PMCID: PMC7172722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou Y, Fu B, Zheng X, Wang D, Zhao C, Qi Y, et al. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. National Science Review. 2020;7(6):998–1002. doi: 10.1093/nsr/nwaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(6):355–62. Epub 2020/05/08. doi: 10.1038/s41577-020-0331-4 ; PubMed Central PMCID: PMC7201395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franchini M, Marano G, Cruciani M, Mengoli C, Pati I, Masiello F, et al. COVID-19-associated coagulopathy. Diagnosis (Berl). 2020;7(4):357–63. Epub 2020/07/20. doi: 10.1515/dx-2020-0078 . [DOI] [PubMed] [Google Scholar]
- 8.Luan YY, Liu Y, Liu XY, Yu BJ, Chen RL, Peng M, et al. Coronavirus disease 2019 (COVID-19) associated coagulopathy and its impact on outcomes in Shenzhen, China: A retrospective cohort study. Thromb Res. 2020;195:62–8. Epub 2020/07/14. doi: 10.1016/j.thromres.2020.07.015 ; PubMed Central PMCID: PMC7347306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ortega-Paz L, Capodanno D, Montalescot G, Angiolillo DJ. Coronavirus Disease 2019-Associated Thrombosis and Coagulopathy: Review of the Pathophysiological Characteristics and Implications for Antithrombotic Management. J Am Heart Assoc. 2021;10(3):e019650. Epub 2020/11/25. doi: 10.1161/JAHA.120.019650 ; PubMed Central PMCID: PMC7955431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL. Special Article—Acute myocardial injury in patients hospitalized with COVID-19 infection: A review. Prog Cardiovasc Dis. 2020;63(5):682–9. Epub 2020/06/09. doi: 10.1016/j.pcad.2020.05.013 ; PubMed Central PMCID: PMC7274977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–10. Epub 2020/03/27. doi: 10.1001/jamacardio.2020.0950 ; PubMed Central PMCID: PMC7097841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Toraih EA, Elshazli RM, Hussein MH, Elgaml A, Amin M, El-Mowafy M, et al. Association of cardiac biomarkers and comorbidities with increased mortality, severity, and cardiac injury in COVID-19 patients: A meta-regression and decision tree analysis. J Med Virol. 2020;92(11):2473–88. Epub 2020/06/13. doi: 10.1002/jmv.26166 ; PubMed Central PMCID: PMC7307124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, et al. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc Imaging. 2020;13(11):2330–9. Epub 2020/08/09. doi: 10.1016/j.jcmg.2020.05.004 ; PubMed Central PMCID: PMC7214335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51. Epub 1994/11/01. doi: 10.1016/0895-4356(94)90129-5 . [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, et al. Standardized End Point Definitions for Coronary Intervention Trials: The Academic Research Consortium-2 Consensus Document. Circulation. 2018;137(24):2635–50. Epub 2018/06/13. doi: 10.1161/CIRCULATIONAHA.117.029289 . [DOI] [PubMed] [Google Scholar]
- 16.Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47. Epub 2011/06/15. doi: 10.1161/CIRCULATIONAHA.110.009449 . [DOI] [PubMed] [Google Scholar]
- 17.Wu Q, Zhou L, Sun X, Yan Z, Hu C, Wu J, et al. Altered Lipid Metabolism in Recovered SARS Patients Twelve Years after Infection. Sci Rep. 2017;7(1):9110. Epub 2017/08/24. doi: 10.1038/s41598-017-09536-z ; PubMed Central PMCID: PMC5567209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal Influenza Infections and Cardiovascular Disease Mortality. JAMA Cardiol. 2016;1(3):274–81. Epub 2016/07/22. doi: 10.1001/jamacardio.2016.0433 ; PubMed Central PMCID: PMC5158013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(PDF)
(PDF)