Abstract
The burden of disability among survivors and the socio-economic impact of snakebite have not been adequately researched. We reviewed original research articles, case reports and small case series relating to chronic physical, mental and psycho-social disability and economic burden of snakebite. Both physical and psychological health problems seem common in snakebite survivors and can lead to disability and loss of productivity. Chronic physical health effects, musculoskeletal disability being the commonest, can be largely attributed to limited and delayed access to optimal treatment of acute envenoming. The economic burden is considerable, and includes health system costs, out-of-pocket expenditure and opportunity costs, with regional variations. Health systems should be more responsive to needs and circumstances of bite victims, and a more holistic approach should be developed in the treatment of snakebite which incorporates the management of chronic health effects.
Keywords: Snakebite, Socio-economic burden, Cost, Chronic health effects, Physical disability, Psychological effects
Graphical abstract
Highlights
-
•
Limited attention has been paid to chronic disability and the socio-economic impact of snakebite.
-
•
Physical and psychological health problems occur in snakebite survivors leading to disability and loss of productivity.
-
•
Chronic health effects can be largely attributed to limited and delayed access to optimal treatment of acute envenoming.
-
•
Economic burden includes health system costs, out-of-pocket expenditure and opportunity costs.
-
•
Health systems should be responsive to needs and circumstances of bite victims including care of chronic health effects.
1. Introduction
Snakebite envenoming causes significant morbidity and mortality in tropical and subtropical countries in Africa, Asia, Oceania and Latin America (Kasturiratne et al., 2008). Most of the morbidity and mortality occurs in young adults living and working in farming and other labour intensive occupations in impoverished rural areas. The combination of poor access to often sub-optimal health services, scarcity of effective and safe antivenom, and the burden placed on families and communities due to snakebite victims with disability, many of whom are young and economically productive, is very likely to result in a considerable medical, social and economic toll (Hansdak et al., 1998). Despite their importance, neither the burden of disability among survivors nor the socio-economic impact of snakebite have been adequately researched.
Most snakebite-related research is focussed on the epidemiology and clinical aspects of acute envenoming and mortality, which understandably take priority in countries struggling with inadequate resources to manage and save the lives of snakebite victims. Although recommendations have been made that assessments of snakebite burden should include chronic disability and related socio-economic costs, obtaining reliable data on these aspects is challenging. There are several reasons for this. Snakebite envenoming mainly occurs in the poorest regions of the world (Harrison et al., 2009) and the available data are usually based on incomplete hospital returns or central databases (Kasturiratne et al., 2008). Snakebites are often underreported because many victims may seek traditional treatments, either due to preference or inadequate or absent allopathic treatment facilities (Pugh et al., 1980; Snow et al., 1994; Rahman et al., 2010; Ediriweera et al., 2017). Furthermore, there is rarely, if ever, routine follow-up of snakebite victims who are discharged from hospital after the acute complications of envenoming have resolved and, with loss of further contact, the allopathic system fails to detect possible longer-term disabilities and their consequences.
In Asian, African and Latin American countries, there are many studies which report that health workers lack sufficient knowledge and confidence in snakebite management (Fung et al., 2009; Sapkota et al., 2020; Inthanomchanh et al., 2017; Gajbhive et al., 2019). The problem stems from deficiencies in the training of these professionals in their medical or nursing courses (Inthanomchanh et al., 2017; Kharusha et al., 2020). Chronic disability following snakebite is more likely to occur, both, where there is poor access to healthcare and in situations where management of the bite is inadequate. In such settings follow-up of victims is extremely unlikely to occur.
While improved medical management has the potential to reduce chronic physical disability, for example, reduce the rate of limb amputations or severe disfigurement, psychological disability following a snakebite may yet occur (Williams et al., 2011). Adverse physical effects of envenoming are related to the necrotoxic, neurotoxic and hematotoxic damage caused by venom components, but the mechanisms by which snake envenoming causes psychological disability has not been explored.
Although the allopathic system, in general, loses contact with snakebite victims after their discharge from hospital, some survivors can, and do, continue to seek help from traditional healers who are easy to access and offer them social and psychological support which takes into account the religious and cultural beliefs of local communities. Research on chronic disability following snakebite may, therefore, benefit from the inclusion of traditional healers (Stienstra et al., 2021).
In this paper we review the available published literature on chronic physical, mental and psycho-social disability and economic burden of snakebite.
2. Methods
2.1. The search strategy
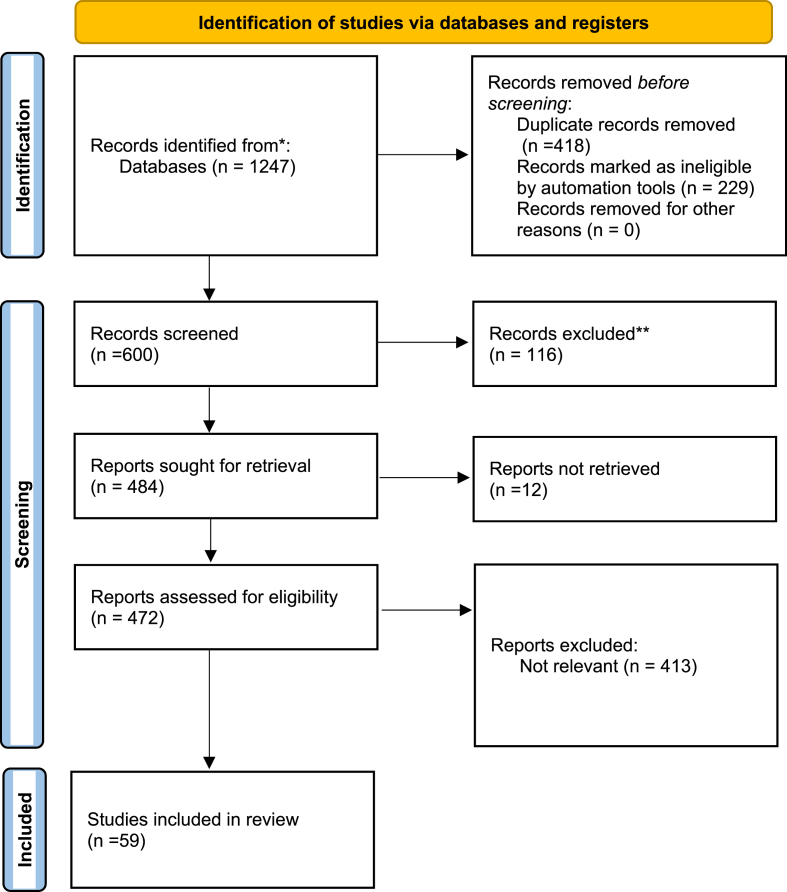
This review was conducted according to the PRISMA 2020 statement for reporting systematic reviews (Page et al., 2021). To identify original research papers published on chronic health effects of snakebite, we searched PubMed, Scopus and EBSCOhost databases using the terms “snake bite” OR “snakebite” AND “health effects” OR “morbidity” OR “disability” OR “sequelae” OR “consequences” AND “long term” OR “chronic” OR “delayed”. This search resulted in 1247 research papers. 829 remained after duplicates were merged. Of these, 229 were book or book sections. Remaining 600 journal articles and thesis were screened using the abstract and 41 and 75 were excluded due to being animal studies and reviews, respectively. The remaining 484 publications were screened for relevance and content. PubMed, EBSCOhost and Scopus databases and the specific journals websites were used to retrieve the full papers. 472 full papers and 12 abstracts were retrieved and reviewed. 59 papers contained data on chronic health effects of snakebite (Fig. 1). Health outcomes prevalent at the time of discharge from the hospital and reported as persistent at least 4 weeks after discharge and outcomes attributed to the index snakebite that occur after discharge from the hospital and persist for a minimum of 4 weeks from discharge were considered.
Fig. 1.
PRISMA 2020 flow diagram for reviewing the chronic health effects of snakebite.
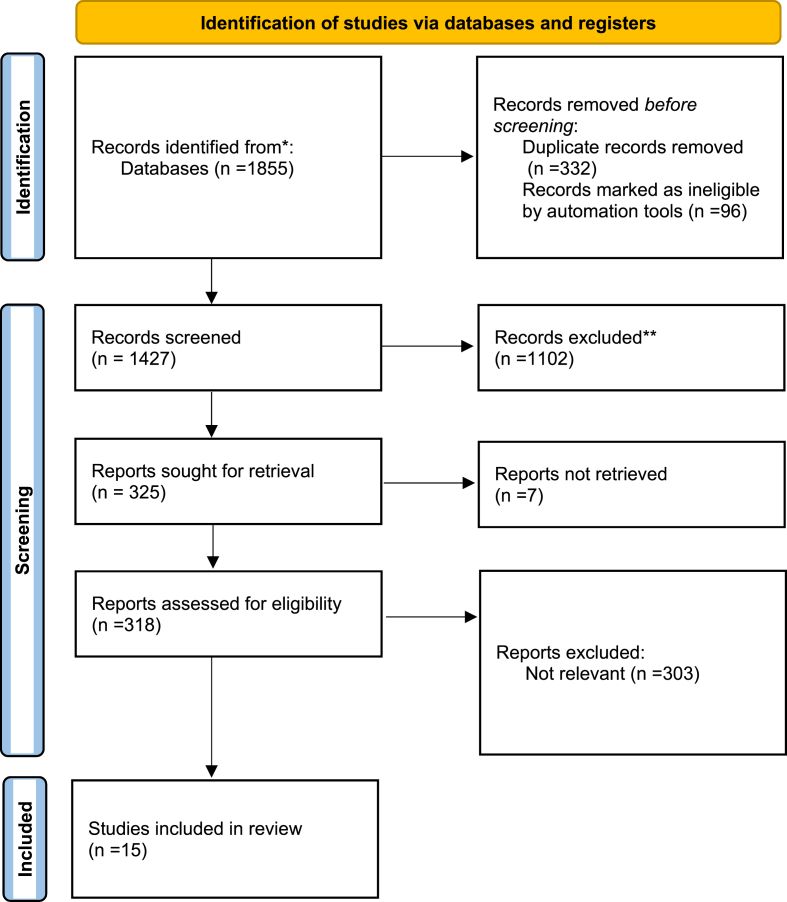
We conducted a separate search in PubMed, EBSCOhost and Scopus (limited to subject areas: Medicine and Economics, Econometrics and Finance) databases using the terms “snake bite” OR “snakebite” AND “economic” OR “cost” OR “expenditure” OR “burden”. This search resulted in 1855 scientific publications. 1523 remained after duplicates were merged. 96 book chapters and book sections were excluded. Remaining 1427 papers were evaluated for relevance through screening the abstract. This resulted in identifying 325 potentially relevant publications. 318 full papers and 7 abstracts were reviewed to identify 15 papers describing the out-of-pocket expenditure or the cost of snakebite for the health system at hospital, country or regional level (Fig. 2).
Fig. 2.
PRISMA 2020 flow diagram for reviewing the cost of snakebite.
3. Results
We reviewed 59 original research papers to identify information on chronic health effects of snakebite and 15 papers that dealt with its cost.
3.1. Chronic health effects of snakebite
Chronic or long-term health effects of snakebite has many definitions in the available literature. They include, any condition related to snakebite that required follow-up after discharge from hospital, conditions that last or appear more than six weeks following envenoming, or health problems that had occurred immediately or within 4 weeks of the bite and had persisted for more than 3 months (Williams et al., 2011; Jayawardana et al., 2018; Waiddyanatha et al., 2019; Brenes-Chacon et al., 2020).
Chronic physical health effects of snakebite can be broadly classified into dermatological, musculoskeletal, neurological, renal and endocrine conditions. Chronic psychological health effects include a broad group of mental health problems. These are summarized in (Table 1).
Table 1.
Chronic health effects of snake bites.
| No | Authors | Location | Long term health effects |
|
|---|---|---|---|---|
| Physical | Psychological | |||
| 1 | Caiaffa et al. (1994) | Southeast Brazil |
|
Not reported |
| 2 | Sharma et al. (2004) | South Eastern Nepal |
|
Not reported |
| 3 | Kidmas et al., 2004 | Jos, Nigeria |
|
Not reported |
| 4 | Bell et al. (2010) | Teaching Hospital, Kurunegala, Sri Lanka |
|
Not reported |
| 5 | Williams et al. (2011) | North Central Province, Sri Lanka |
|
|
| 6 | Khosrojerdi and Amini (2013) | Imam Reza Hospital, Iran | Not reported |
|
| 7 | Spano et al. (2014) | UCSF-Fresno Medical Education Program Medical Centre, Fresno Central California |
|
Not reported |
| 8 | Wijesinghe et al. (2015) | District General Hospital, Polonnaruwa, Sri Lanka | Not reported |
|
| 9 | Habib et al. (2015) | Northeastern Nigeria | Not reported |
|
| 10 | Jayawardana et al. (2016) |
|
|
Not reported |
| 11 | Naqvi (2016) | Sindh Institute of Urology and Transplantation, Karachi, Pakistan |
|
Not reported |
| 12 | Tsai et al., 2017 | Chia-Yi Chang Gung Memorial Hospital in Taiwan |
|
Not reported |
| 13 | Islam et al., 2017 | Rangamati Sadar Hospital, Rangamati, Bangladesh |
|
|
| 14 | Naik et al. (2018) | Chandigarh, India |
|
Not reported |
| 15 | Yerawar et al. (2020) | Nanded, India |
|
Not reported |
| 16 | Proby et al. (1990) | London, UK |
|
Not reported |
| 17 | Jayawardana et al. (2018) | Ampara, Sri Lanka |
|
|
| 18 | Arias-Rodríguez and Gutiérrez (2020) | South-eastern (Brunca region) Costa Rica |
|
|
| 19 |
Brenes-Chacon et al. (2020) |
National Children's Hospital in Costa Rica |
|
Not reported |
| 20 | Sachett et al. (2020a) | Brazil |
|
|
| 21 | Pucca et al. (2020) | Las Claritas Bolívar, Venezuela |
|
Not reported |
| 22 | Pulimaddi et al. (2017) | India |
|
Not reported |
| 23 | Priyamvada et al. (2019) | Puducherry, India |
|
Not reported |
| 24 | Alcoba et al. (2020) | Akonolinga health district, Centre Region, Cameroon |
|
|
| 25 | Kumar et al. (2018) | Malabar, North Kerala, India |
|
Not reported |
| 26 | Brenes et al. (2018) | National Children's Hospital, Costa Rica |
|
Not reported |
| 27 | Pérez-Gómez et al. (2019) | Western Brazilian Amazon |
|
Not reported |
| 28 | Sachett et al. (2020a) | Guajará (Amazonas state), Western Brazilian Amazon |
|
Not reported |
| 29 | Kim et al. (2021a) | Chungnam National University Hospital, Daejeon, Korea |
|
Not reported |
| 30 | van Oirschot et al. (2021) | Kajiado and Kilifi counties. Kenya |
|
Not reported |
| 31 | Kularatne (2002) | Anuradhapura, Sri Lanka |
|
|
| 32 | Corneille et al. (2006) | Texas, USA |
|
Not reported |
| 33 | Yates et al. (2010) | Meserani, Tanzania |
|
Not reported |
| 34 | Herath et al. (2012) | Kandy, Sri Lanka |
|
Not reported |
| 35 | Namal Rathnayaka et al., 2020 | Sri Lanka |
|
Not reported |
| 36 | Seneviratne and Dissanayake (2002) | Ratnapura and Polonnaruwa, Sri Lanka |
|
Not reported |
| 37 | Elbey et al. (2017) | Diyarbakır, Turkey |
|
Not reported |
| 38 | Weinstein et al. (2018) | Australia |
|
Not reported |
| 39 | Zeng et al. (2019) | Chongqing, P.R. China |
|
Not reported |
| 40 | Halilu et al. (2019) | Sub-Saharan Africa |
|
Not reported |
| 41 | Gerardo et al. (2019) | Southeastern United States |
|
Not reported |
| 42 | Banerjee et al. (2019) | India |
|
Not reported |
| 43 | Lizarazo et al. (2020) | Catatumbo, Colombia |
|
Not reported |
| 44 | Srirangan et al. (2020) | Kalubowila, Sri Lanka |
|
Not reported |
| 45 | Habib et al. (2021) | North-eastern Nigeria | Not reported |
|
| 46 | Kazemi et al. (2021) | Iran |
|
Not reported |
| 47 | Jelinek et al. (1998) | Nedlands, Western Australia |
|
Not reported |
| 48 | Chroni et al. (2005) | Rion-Patras, Greece |
|
Not reported |
| 49 | Sinha et al. (2009) | Kolkata, India |
|
Not reported |
| 50 | Golay et al. (2014) | West Bengal, India |
|
Not reported |
| 51 | Mahmood et al. (2018) | Mandalay Division, Myanmar |
|
Not reported |
| 52 | Lee and Yao (2010) | Arizona, USA |
|
Not reported |
| 53 | Bonasso et al. (2015) | West Virginia, USA |
|
Not reported |
| 54 | Gelman et al. (2021) | Texas, USA |
|
Not reported |
| 55 | Dhabhar et al. (2021) | India |
|
Not reported |
| 56 | Pérez-Gómez et al. (2019) | Western Brazilian Amazon |
|
Not reported |
| 57 | Abraham et al. (2020) | Kerala, India |
|
Not reported |
| 58 | KIm et al. (2021b)" | Republic of Korea |
|
Not reported |
| 59 | Gupta et al. (2021) | Delhi, India |
|
Not reported |
3.2. Chronic physical health effects
Skin blistering after snakebite envenoming often results in the development of necrotic lesions which are difficult to treat, especially in the context of poorly resourced health care facilities in areas where snakebite is common, where surgical expertise and antibiotics are in short supply and hospital conditions favour secondary infection. Chronic non-healing ulcers and persistent or recurrent blisters at the bite site, though rare, are the most commonly reported dermatological conditions (Jayawardana et al., 2016; Jayawardana et al., 2018). Hypertrophic scars, which may cause contractures leading to disfigurement and functional limitations even requiring reconstructive surgery, and hyper-pigmentation and discolouration of skin in the affected part of the body, have also been commonly reported. Excessive hair loss has also been reported rarely. Musculo-skeletal disabilities are the commonest chronic condition associated with snakebite. Weakness, functional limitation and deformities of the affected limbs due to muscle dystrophy are commonly reported (Caiaffa et al., 1994; Jayawardana et al., 2016; Rodríguez and Gutiérrez, 2019). Tissue necrosis leading to amputation of parts of the affected limb is the most severe and debilitating chronic condition associated with snakebite globally [Kidmas et al., 2004; Tsai et al., 2017]. There does not seem to be consistency in the use of surgical techniques emphasizing the need for standardization (Sachett et al., 2020b).
A migraine-like syndrome characterized by headache, blurred vision, nausea and dizziness has been described (Jayawardana et al., 2018). Other neurological conditions with long-lasting impact such as visual and hearing impairment, paresthesia at the bite site, and persistence of hemiparesis or hemiplegia due to cerebrovascular events at the time of acute envenoming have also been reported (Spano et al., 2014; Jayawardana et al., 2018). Chronic renal failure requiring haemodialysis has been reported in some victims of snakebite who had developed acute kidney injury following the bite (Naqvi, 2016; Pucca et al., 2020). Establishing causality is challenging as most of these reports provide no information regarding the victims’ renal function prior to envenoming, and therefore the problem is neglected. Hypopituitarism and resulting disturbances in related hormones has been reported in snakebite victims lasting for many years after the bite (Naik et al., 2018).
3.3. Delayed psychological effects
Delayed psychological effects following snakebite have been poorly investigated. Depressive symptoms and post-traumatic stress disorder are the most common psychological conditions reported following snakebite (Khosrojerdi and Amini, 2013; Williams et al., 2011). Non-specific somatic manifestations of psychological problems resulting from the experience of snakebite, which may be related to socio-cultural beliefs that promote a sick role are also described in the literature (Rodríguez and Gutiérrez, 2019; Alcoba et al., 2020).
3.4. Cost of snakebite
The estimations of the cost of snakebite in the literature are summarized in Table 2.
Table 2.
Cost of snakebite reported in global literature.
| Health system cost of snakebite | |||
|---|---|---|---|
| No | Author | Location | Cost |
| Lopoo et al. (1998) | USA |
|
|
| Hasan et al. (2012) | Bangladesh |
|
|
| Saz-Parkinson et al. (2012) | Spain |
|
|
| Narra et al. (2014) | 33 children's Hospitals in Pediatric Health Information System, USA |
|
|
| Kasturiratne et al. (2017) | Sri Lanka |
|
|
| Tochie (2017) | Cameroon |
|
|
| Okumu et al., 2019 | JOOTRH, Kisumu County, Western Kenya |
|
|
| Magalhães et al. (2020) | Brazilian Amazon |
|
|
| Benabdellah et al. (2020) | Children's University Hospital of Rabat, Morocco |
|
|
| Khan et al. (2020) | Saudi Arabia | Direct healthcare cost per snakebite patient by severity category
|
|
| Household cost of snakebite | |||
| No | Author | Location | Cost |
| Sharma et al. (2004) | South eastern Nepal |
|
|
| Vaiyapuri et al. (2013) | Tamil Nadu, India |
|
|
| Kasturiratne et al. (2017) | Sri Lanka |
|
|
| Magalhães et al. (2020) | Brazilian Amazon |
|
|
| Burden of snakebite | |||
| No | Author | Location | Cost |
| Habib et al. (2015) | Nigeria |
|
|
| Hamza et al. (2016) | West Africa | The cost/death averted for Guinea Bissau: US$1997 The cost/death averted for Liberia and Sierra Leone: US$6205 The cost/DALY averted for Benin Republic: US$$83 (95% Confidence Interval: US$36-$240) The cost/DALY averted for Sierra-Leone: US$281 ($159–457). |
|
| Kasturiratne et al. (2017) | Sri Lanka |
|
|
| Quintana-Castillo et al. (2020) |
|
||
| Magalhães et al. (2020) | Brazilian Amazon |
|
|
The available estimates cover health system costs and out-of-pocket expenditure of snakebite (Hasan et al., 2012), and the burden of snakebite (Habib et al., 2015). The cost per death averted has been estimated for 16 countries in West Africa (Hamza et al., 2016). Using data on mortality and amputations, the total burden of snakebite in West Africa has been estimated at 320,000 DALYs (95% CI: 248,000–403,000 DALYs) per year with Nigeria accounting for 43% of the burden (Habib et al., 2015).
In Cameroon, the relatively expensive prices of AVS ranging from US$20–75 are unaffordable for households of the most vulnerable communities (Tochie, 2017). Clinical protocols developed for standardization of antivenom use has been effective for reducing the cost of care, by reducing the number of vials used and the length of hospital stay, with no significant difference in complication rates (Ghosh et al., 2008; Weant et al., 2012). However, in many regions in Africa, including Cameroon, the antivenoms have not been tested for effectiveness, and the efficacy of the antivenoms used is questionable. This issue needs to be addressed as a priority (Potet et al., 2019).
Regional variations in the cost of care and the disease burden have been described within the most affected countries and across regions over the last 20 years (Kasturiratne et al., 2005; Habib et al., 2015; Curran-Sills and Kroeker, 2018).
4. Discussion
Snakebite is a debilitating condition both from a health and economic perspective (Habib and Brown, 2018). As the condition is most prevalent in the most vulnerable populations living in low-income countries and, in addition to development of adverse chronic health effects, the extra cost incurred by a snakebite may have a devastating economic impact on the victims and their families (Harrison et al., 2009). In this paper, we reviewed the available literature on the chronic health effects and costs of snakebite envenoming.
Chronic health effects of snakebite, though likely to be commoner than reports indicate, have received limited attention in the snakebite literature. The wide variation in the definition of “chronic health effects” in relation to their point of appearance and duration, indicates the lack of a systematic approach to defining and describing this very important aspect of snakebite (Williams et al., 2011; Jayawardana et al., 2018; Waiddyanatha et al., 2019; Brenes-Chacon et al., 2020). Screening and detection of chronic disability related to snakebite would require at least one out-patient follow-up visit after victims are discharged from hospital. The development of a set of patient-centred outcomes, based on the available evidence and expert consensus, would make the assessment for chronic disability and its management more systematic and meaningful.
The reported chronic physical health effects of snakebite can be largely attributed to delayed or lack of access to appropriate treatment, and inappropriate or sub-optimal treatment within health facilities due to limited resources or poor quality of care. Although “400,000 disabilities caused by snakebites each year worldwide” is often cited in the recent literature, how this number was arrived at or details regarding the severity, offending species and which regions are worst affected are sparse.
The most commonly reported is musculoskeletal disability. Persistent limb swelling, probably the result of lymphatic or vascular injury, has been reported, especially after viper bites; 8/800 snakebites in Sri Lanka (Jayawardana et al., 2016), 19% after Malayan pit viper bites in Thailand (Wongtongkam et al., 2005). While most dermatological and musculo-skeletal damage, especially those related to venom related tissue necrosis, may lead to disfigurement, surgical interventions such as fasciotomy and amputations to treat compartment syndrome and subsequent tissue necrosis have life-long consequences with severe disability and loss of productivity (Habib et al., 2015). Doppler Ultrasound is a useful tool to evaluate swelling and exclude compartment syndrome (Ho et al., 2021) and where available, may be a promising approach to avoid unnecessary fasciotomy. Another relatively simple intervention maybe physiotherapy, which is rarely done after snakebite, but will probably significantly improve the outcome and reduce the number and severity of chronic musculoskeletal disorders. At present there does not seem to be consistency in the use of surgical techniques, and standard protocols are urgently needed.
Psychological problems may occur even after “successful” treatment of snake envenoming with AVS, and although difficult to detect without adequate follow-up, together with associated non-specific somatic manifestations, can have considerable negative social and economic impacts, for example, from loss of employment (Williams et al., 2011). A small randomized trial of a brief psychological intervention, that can be provided by non-specialist doctors, appeared to reduce psychiatric symptoms and disability related to family and social life after snakebite envenoming, but not depression or post-traumatic stress disorder (Wijesinghe et al., 2015). More research is required to develop culturally-appropriate interventions for those affected, especially focusing on post-traumatic stress disorder and depression following snakebite.
There has been an increase in the number of studies reporting economic burden of snakebite over the last ten years (after 2010). Out of pocket expenditure and opportunity costs incurred by victims and their families have been reported in several studies (Vaiyapuri et al., 2013; Kasturiratne et al., 2017; Magalhães et al., 2020). Hospital based studies commonly report the cost of care for a single episode of snakebite. Although there are wide variations in the cost across the regions of the world, developing treatment protocols may help to reduce the cost of care as well as the rates of complications that may lead to chronic disability (Ghosh et al., 2008; Weant et al., 2012). National level studies on the economic burden of snakebite and studies on the cost-effectiveness of anti-venom treatment have highlighted the problem of limited availability of AVS and the financial burden placed on poorer economies where snakebite is common, due to the cost of AVS.
In conclusion, poor healthcare and limited access to anti-venom are the leading causes of morbidity and chronic disability due to snakebite envenoming. These can adversely impact the economy of poor communities. Health systems need to be more responsive to the needs and circumstances of the victims of snakebite, developing a more holistic approach that incorporates the management of the acute manifestations of envenoming, preventing mortality, together with management of chronic health effects, both physical and psychological. Chronic health effects of snakebite and the economic cost of snakebite are inter-related and are a part of a vicious poverty cycle that deserves the highest attention of snakebite researchers, administrators and policy makers.
Author contributions
AK: conceptualization, literature survey, writing the first draft, revision of the manuscript. DGL: conceptualization, revision of the manuscript. HJdeS: conceptualization, writing the first draft, revision of the manuscript. All three authors approved the final version of the manuscript.
Ethical Statement
“Chronic health effects and cost of snakebite”:
-
1)
This material is the authors' own original work, which has not been previously published elsewhere.
-
2)
The paper is not currently being considered for publication elsewhere.
-
3)
The paper reflects the authors' own research and analysis in a truthful and complete manner.
-
4)
The paper properly credits the meaningful contributions of co-authors and co-researchers.
-
5)
The results are appropriately placed in the context of prior and existing research.
-
6)
All sources used are properly disclosed (correct citation). Literally copying of text must be indicated as such by using quotation marks and giving proper reference.
-
7)
All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
The violation of the Ethical Statement rules may result in severe consequences.
To verify originality, your article may be checked by the originality detection software iThenticate. See also http://www.elsevier.com/editors/plagdetect.
I agree with the above statements and declare that this submission follows the policies of Toxicon as outlined in the Guide for Authors and in the Ethical Statement.
Declaration of competing interest
All three authors have no conflict of interests to declare.
Handling Editor: Raymond Norton
References
- Abraham S.V., Hakkeem B., Mathew D., Rafi A.M., Poomali A., Thomas J., Kassyap C.K. Hematotoxic snakebite victim with trauma: the role of guided transfusion, rotational thromboelastometry, and tranexamic acid. Wilderness Environ. Med. 2020;31(4):470–481. doi: 10.1016/j.wem.2020.08.003. [DOI] [PubMed] [Google Scholar]
- Alcoba G., Chabloz M., Eyong J., Wanda F., Ochoa C., Comte E., Nkwescheu A., Chappuis F. Snakebite epidemiology and health-seeking behavior in Akonolinga health district, Cameroon: cross-sectional study. PLoS Neglected Trop. Dis. 2020;14(6) doi: 10.1371/journal.pntd.0008334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias-Rodríguez J., Gutiérrez J.M. Circumstances and consequences of snakebite envenomings: a qualitative study in south-eastern Costa Rica. Toxins. 2020;12(1):45. doi: 10.3390/toxins12010045. 10.3390/toxins12010045. PMID: 31940786; PMCID: PMC7020421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee S., Pipliwal P.S., Joshi S., Goyal P., Sharma M., Sharma A. Cerebellar ataxia: a rare manifestation of snake envenomation. J. Indian Med. Assoc. 2019;117:28–29. 06. [Google Scholar]
- Bell D.J., Wijegunasinghe D., Samarakoon S., Palipana H., Gunasekera S., de Silva H.A., Lalloo D.G., Ranawaka U.K., de Silva H.J. Neurophysiological findings in patients 1 year after snake bite induced neurotoxicity in Sri Lanka. Trans. R. Soc. Trop. Med. Hyg. 2010;104(5):351–356. doi: 10.1016/j.trstmh.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Benabdellah F.Z., Soulaymani A., Mokhtari A. Economic evaluation of the direct cost resulting from childhood poisoning in Morocco: micro-costing analysis. Arch. Publ. Health. 2020;78:59. doi: 10.1186/s13690-020-00440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonasso P., Lucke-Wold B., Jacob G. Osteonecrosis of interphalangeal joint of thumb two months after rattlesnake bite. Hand Surg. 2015:330–332. doi: 10.1142/S021881041572017X. 10.1142/S021881041572017X. [DOI] [PubMed] [Google Scholar]
- Brenes H., Herrera M.L., Ávila-Aguero M.L. Chromoblastomycosis caused by phialophora verrucosa in a Costa Rican child with skin sequelae due to snake bite. Cureus. 2018;10(11) doi: 10.7759/cureus.3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes-Chacon H., Gutierrez J.M., Camacho-Badilla K. Long-term sequelae secondary to snakebite envenoming: a single centre retrospective study in a Costa Rican paediatric hospital. BMJ Paediatrics Open. 2020;4 doi: 10.1136/bmjpo-2020-000735. 2020. 10.1136/bmjpo-2020-000735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caiaffa W.T., Vlahov D., Antunes C.M., de Oliveira H.R., Diniz C.R. Snake bite and antivenom complications in Belo Horizonte, Brazil. Trans. R. Soc. Trop. Med. Hyg. 1994;88(1):81–85. doi: 10.1016/0035-9203(94)90511-8. [DOI] [PubMed] [Google Scholar]
- Chroni E., Papapetropoulos S., Argyriou A.A., Papapetropoulos T. A case of fatal progressive neuropathy. Delayed consequence of multiple bites of a non-venomous snake? Clin. Neurol. Neurosurg. 2005;108(1):45–47. doi: 10.1016/j.clineuro.2004.10.010. [DOI] [PubMed] [Google Scholar]
- Corneille M.G., Larson S., Stewart R.M., Dent D., Myers J.G., Lopez P.P., McFarland M.J., Cohn S.M. A large single-center experience with treatment of patients with crotalid envenomations: outcomes with and evolution of antivenin therapy. Am. J. Surg. 2006;192(6):848–852. doi: 10.1016/j.amjsurg.2006.08.056. [DOI] [PubMed] [Google Scholar]
- Curran-Sills G., Kroeker J. Venomous snakebites in Canada: a national review of patient epidemiology and antivenom usage. Wilderness Environ. Med. 2018;29(4):437–445. doi: 10.1016/j.wem.2018.06.005. [DOI] [PubMed] [Google Scholar]
- Dhabhar J., Mehta V., Desai N. Optic neuritis after a snakebite: a diagnostic dilemma. Ochsner J. 2021;21(1):90–92. doi: 10.31486/toj.19.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ediriweera D.S., Kasturiratne A., Pathmeswaran A., Gunawardena N.K., Jayamanne S.F., Lalloo D.G. Health seeking behavior following snakebites in Sri Lanka: results of an island wide community based survey. PLoS Neglected Trop. Dis. 2017;11 doi: 10.1371/journal.pntd.0006073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbey B., Baykal B., Yazgan Ü.C., Zengin Y. The prognostic value of the neutrophil/lymphocyte ratio in patients with snake bites for clinical outcomes and complications. Saudi J. Biol. Sci. 2017;24(2):362–366. doi: 10.1016/j.sjbs.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman D., Bates T., Nuelle J.A.V. Septic arthritis of the proximal interphalangeal joint after rattlesnake bite. J Hand Surg Am. S0363- 2021;5023(21) doi: 10.1016/j.jhsa.2021.04.004. 00209-4. [DOI] [PubMed] [Google Scholar]
- Gerardo C.J., Vissoci J.R.N., de Oliveira L.P., Anderson V.E., Quackenbush E., Lewis B., Rose S.R., Greene S., Toschlog E.A., Charlton N.P., Mullins M.E., Schwartz R., Denning D., Sharma K., Kleinschmidt K., Bush S.P., Brandehoff N.P., Lavonas E.J. The validity, reliability and minimal clinically important difference of the patient specific functional scale in snake envenomation. PloS One. 2019;14(3) doi: 10.1371/journal.pone.0213077. 10.1371/journal.pone.0213077. PMID: 30835744; PMCID: PMC6400437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh S., Maisnam I., Murmu B.K., Mitra P.K., Roy A., Simpson I.D. A locally developed snakebite management protocol significantly reduces overall anti snake venom utilization in West Bengal, India. Wilderness Environ. Med. 2008;(4):267–274. doi: 10.1580/08-WEME-OR-219.1. [DOI] [PubMed] [Google Scholar]
- Golay V., Roychowdhary A., Dasgupta S., Pandey R. Hypopituitarism in patients with vasculotoxic snake bite envenomation related acute kidney injury: a prospective study on the prevalence and outcomes of this complication. Pituitary. 2014;17(2):125–131. doi: 10.1007/s11102-013-0477-1. [DOI] [PubMed] [Google Scholar]
- Gupta A., Smilie C., Bhaskar V., Batra P. Unusually prolonged neuromuscular weakness caused by krait (Bungarus caeruleus) bite: two case reports. Toxicon. 2021;193:1–3. doi: 10.1016/j.toxicon.2021.01.011. [DOI] [PubMed] [Google Scholar]
- Habib A.G., Brown N.I. The snakebite problem and antivenom crisis from a health-economic perspective. Toxicon. 2018;150:115–123. doi: 10.1016/j.toxicon.2018.05.009. 10.1016/j.toxicon.2018.05.009. [DOI] [PubMed] [Google Scholar]
- Habib A.G., Kuznik A., Hamza M., Abdullahi M.I., Chedi B.A., Chippaux J.-P. Snakebite is under appreciated: appraisal of burden from West Africa. PLoS Neglected Trop. Dis. 2015;9(9) doi: 10.1371/journal.pntd.0004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habib Z.G., Salihu A.S., Hamza M., Yakasai A.M., Iliyasu G., Yola I.M., Gudaji M.I., Abubakar S.B., Habib A.G. Posttraumatic stress disorder and psycho-social impairment following snakebite in Northeastern Nigeria. Int. J. Psychiatr. Med. 2021;56(2):97–115. doi: 10.1177/0091217420913400. 10.1177/0091217420913400. Epub 2020 Mar 26. PMID: 32216497. [DOI] [PubMed] [Google Scholar]
- Halilu S., Iliyasu G., Hamza M., Chippaux J.P., Kuznik A., Habib A.G. Snakebite burden in Sub-Saharan Africa: estimates from 41 countries. Toxicon. 2019;159:1–4. doi: 10.1016/j.toxicon.2018.12.002. Epub 2018 Dec 27. PMID: 30594637. [DOI] [PubMed] [Google Scholar]
- Hamza M., Idris M.A., Maiyaki M.B., LamordeM, Chippaux J.-P., Warrell D.A. Cost-effectiveness of antivenoms for snakebite envenoming in 16 countries in West Africa. PLoSNegl Trop Dis. 2016;10(3) doi: 10.1371/journal.pntd.0004568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansdak S.G., Lallar K.S., Pokharel P., Shyangwa P., Karki P., Koirala S. A clinico-epidemiological study of snake bite in Nepal. Trop. Doct. 1998;28:223–226. doi: 10.1177/004947559802800412. [DOI] [PubMed] [Google Scholar]
- Harrison R.A., Hargreaves A., Wagstaff S.C., Faragher B., Lalloo D.G. Snake envenoming: a disease of poverty. PLoS Neglected Trop. Dis. 2009;3:e569. doi: 10.1371/journal.pntd.0000569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan S.M.K., Basher A., Molla A.A., Sultana N.K., Faiz M.A. The impact of snake bite on household economy in Bangladesh. Trop. Doct. 2012;42(1):41–43. doi: 10.1258/td.2011.110137. [DOI] [PubMed] [Google Scholar]
- Herath N., Wazil A., Kularatne S., Ratnatunga N., Weerakoon K., Badurdeen S., Rajakrishna P., Nanayakkara N., Dharmagunawardane D. Thrombotic microangiopathy and acute kidney injury in hump-nosed viper (Hypnale species) envenoming: a descriptive study in Sri Lanka. Toxicon. 2012;60(1):61–65. doi: 10.1016/j.toxicon.2012.03.015. [DOI] [PubMed] [Google Scholar]
- Ho Cheng-Hsuan, Ahmad Khaldun, Ismail Shing-Hwa Liu, Tzeng Yuan-Sheng, Li Ling-Yuan, Pai Feng-Cheng, Hong Chia-Wei, Mao Yan-Chiao, Chiang Liao-Chun, Chin-Sheng Lin, Shih-Hung Tsai. The role of a point-of-care ultrasound protocol in facilitating clinical decisions for snakebite envenomation in Taiwan: a pilot study. Clin. Toxicol. 2021 doi: 10.1080/15563650.2021.1881535. [DOI] [PubMed] [Google Scholar]
- Jayawardana S., Gnanathasan A., Arambepola C., Chang T. Chronic musculoskeletal disabilities following snake envenoming in Sri Lanka: a population-based study. PLoS Neglected Trop. Dis. 2016;10(11) doi: 10.1371/journal.pntd.0005103. 10.1371/journal.pntd.0005103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayawardana S., Arambepola C., Chang T., Gnanathasan A. Long-term health complications following snake envenoming. J. Multidiscip. Healthc. 2018;11:279–285. doi: 10.2147/JMDH.S126648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelinek G.A., Rogers I.R., Corkeron M.A., O'Donnell A. Severe multi-system failure following delayed presentation with tiger snake envenomation. Anaesth. Intensive Care. 1998;26(5):584–585. doi: 10.1177/0310057X9802600519. 10.1177/0310057X9802600519. PMID: 9807618. [DOI] [PubMed] [Google Scholar]
- Kasturiratne A., Pathmeswaran A., Fonseka M.M., Lalloo D.G., Brooker S., de Silva H.J. Estimates of disease burden due to land-snake bite in Sri Lankan hospitals. Southeast Asian J. Trop. Med. Publ. Health. 2005;36(3):733–740. PMID: 16124448. [PubMed] [Google Scholar]
- Kasturiratne A., Wickremasinghe A.R., de Silva N., Gunawardena N.K., Pathmeswaran A., Premaratna R., Savioli L., Lalloo D.G., de Silva H.J. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5:e218. doi: 10.1371/journal.pmed.0050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasturiratne A., Pathmeswaran A., Wickremasinghe A.R., Jayamanne S.F., Dawson A., Isbister G.K., de Silva H.J., Lalloo D.G. The socio-economic burden of snakebite in Sri Lanka. PLoS Neglected Trop. Dis. 2017;11(7) doi: 10.1371/journal.pntd.0005647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemi S.M., Al-Sabi A., Long C., Shoulkamy M.I., Abd El-Aziz T.M. Case report: recent case reports of levant blunt-nosed viper Macrovipera lebetina obtusa snakebites in Iran. Am. J. Trop. Med. Hyg. 2021;104(5):1870–1876. doi: 10.4269/ajtmh.20-1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A., Al-Kathiri W.H., Balkhi B., Samrkandi O., Al-Khalifa M.S., Asiri Y. The burden of bites and stings management: experience of an academic hospital in the Kingdom of Saudi Arabia. Saudi Pharmaceut. J. 2020;28(8):1049–1054. doi: 10.1016/j.jsps.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khosrojerdi H., Amini M. Acute and delayed stress symptoms following snakebite. Asia Pac J Med Toxicol. 2013;2:140–144. [Google Scholar]
- Kim K.J., Min J.H., Yoo I., Kim S.W., Lee J., Ryu S., You Y.H., Park J.S., Jeong W.J., Cho Y.C., Oh S.K., Yn In, Ahn H.J., Kang C.S., Kyung H., Lee B.K., Lee D.H., Lee D.H. Negative pressure wound therapy for skin necrosis prevention after snakebite in the emergency department: a retrospective cohort study. Medicine (Baltim.) 2021;100(3) doi: 10.1097/MD.0000000000024290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim T.Y., Roh Y.I., Cha K.C., Hwang S.O., Jung W.J. Delayed splenic rupture: a rare complication of snakebites. Wilderness Environ. Med. 2021;32(1):78–82. doi: 10.1016/j.wem.2020.10.004. [DOI] [PubMed] [Google Scholar]
- Kularatne S.A. Common krait (Bungarus caeruleus) bite in Anuradhapura, Sri Lanka: a prospective clinical study, 1996-98. Postgrad. Med. 2002;78(919):276–280. doi: 10.1136/pmj.78.919.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar K.S., Narayanan S., Udayabhaskaran V., Thulaseedharan N.K. Clinical and epidemiologic profile and predictors of outcome of poisonous snake bites - an analysis of 1,500 cases from a tertiary care center in Malabar, North Kerala, India. Int. J. Gen. Med. 2018;11:209–216. doi: 10.2147/IJGM.S136153. 10.2147/IJGM.S136153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee L., Yao J. Stenosing flexor tenosynovitis following a rattlesnake bite. Orthopedics. 2010;33(7):515. doi: 10.3928/01477447-20100526-20. 10.3928/01477447-20100526-20. PMID: 20608624. [DOI] [PubMed] [Google Scholar]
- Lizarazo J., Patiño R., Lizarazo D., Osorio G. Fatal brain hemorrhage after Bothrops asper bite in the Catatumbo region of Colombia. Biomedica. 2020;40(4):609–615. doi: 10.7705/biomedica.5181. English, Spanish. doi: 10.7705/biomedica.5181. PMID: 33275340; PMCID: PMC7808782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopoo J.B., Bealer J.F., Mantor P.C., Tuggle D.W. Treating the snakebitten child in North America: a study of pit viper bites. J. Pediatr. Surg. 1998;33(11):1593–1595. doi: 10.1016/s0022-3468(98)90587-5. [DOI] [PubMed] [Google Scholar]
- Magalhães S.F.V., Peixoto H.M., de Almeida Gonçalves Sachett J., Oliveira S.S., Alves E.C., Dos Santos Ibiapina H.N., Monteiro W.M., de Oliveira M.R.F. Snakebite envenomation in the Brazilian Amazon: a cost-of-illness study. Trans. R. Soc. Trop. Med. Hyg. 2020;114(9):635–642. doi: 10.1093/trstmh/traa005. [DOI] [PubMed] [Google Scholar]
- Mahmood M.A., Halliday D., Cumming R., Thwin K.T., Kyaw M.M.Z., White J., Alfred S., Warrell D., Bacon D., Naing W., Thein M.M., Chit N.N., Serhal S., Peh C.A. Snakebite incidence in two townships in Mandalay Division, Myanmar. PLoS Neglected Trop. Dis. 2018;12(7) doi: 10.1371/journal.pntd.0006643. 10.1371/journal.pntd.0006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik B.N., Bhalla A., Sharma N., Mokta J., Singh S., Gupta P., Rai A., Subbiah S., Bhansali A., Dutta P. Pituitary dysfunction in survivors of Russell's viper snake bite envenomation: a prospective study. Neurol. India. 2018;66(5):1351–1358. doi: 10.4103/0028-3886.241378. [DOI] [PubMed] [Google Scholar]
- Naqvi R. Snake-bite-induced acute kidney injury. J Coll Physicians Surg Pak. 2016;26(6):517–520. [PubMed] [Google Scholar]
- Narra A., Lie E., Hall M., Macy M., Alpern E., Shah S.S., Osterhoudt K.C., Fieldston E. Resource utilization of pediatric patients exposed to venom. Hosp. Pediatr. 2014;4(5):276–282. doi: 10.1542/hpeds.2014-0010. 10.1542/hpeds.2014-0010. PMID: 25318109. [DOI] [PubMed] [Google Scholar]
- Okumu M.O., Patel M.N., Bhogayata F.R., Ochola F.O., Olweny I.A., Onono J.O., Gikunju J.K. Management and cost of snakebite injuries at a teaching and referral hospital in Western Kenya. 2019;8:1588. doi: 10.12688/f1000research.20268.1. F1000Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Gómez A.S., Monteiro W.M., João G.A.P., Sousa J.D.B., Safe I.P., Damian M.M., Sachett J.A.G., Silva I.M.D. Hemorrhagic stroke following viper bites and delayed antivenom administration: three case reports from the Western Brazilian Amazon. Rev. Soc. Bras. Med. Trop. 2019 doi: 10.1590/0037-8682-0115-2019. 2019 Jul 18;52. e20190115. PMID: 31340373. [DOI] [PubMed] [Google Scholar]
- Potet J., Smith J., McIver L. Reviewing evidence of the clinical effectiveness of commercially available antivenoms in sub-Saharan Africa identifies the need for a multi-centre, multi-antivenom clinical trial. PLoS Neglected Trop. Dis. 2019;13(6) doi: 10.1371/journal.pntd.0007551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priyamvada P.S., Jaswanth C., Zachariah B., Haridasan S., Parameswaran S., Swaminathan R.P. Prognosis and long-term outcomes of acute kidney injury due to snake envenomation. Clin Kidney J. 2019;13(4):564–570. doi: 10.1093/ckj/sfz055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proby C, Tha-AungThet-Win Hla-Mon, Burrin JM, Joplin GF. Immediate and long-term effects on hormone levels following bites by the Burmese Russell’s viper. Q. J. Med. 1990;75(276):399–411. [PubMed] [Google Scholar]
- Pucca M.B., Franco M.V.S., Medeiros J.M., Oliveira I.S., Ahmadi S., Cerni F.A., Zottich U., Bassoli B.K., Monteiro W.M., Laustsen A.H. Chronic kidney failure following lancehead bite envenoming: a clinical report from the Amazon region. J. Venom. Anim. Toxins Incl. Trop. Dis. 2020;26 doi: 10.1590/1678-9199-JVATITD-2020-0083. PMID: 33424950; PMCID: PMC7754649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugh R.N., Theaskston R.D., Reid H.A. Malumfashi Endemic Diseases Research Project, XIII. Epidemiology of human encounters with the spitting cobra, Naja nigricollis, in the Malumfashi area of northern Nigeria. Ann. Trop. Med. Parasitol. 1980;74:523–530. [PubMed] [Google Scholar]
- Pulimaddi R., Parveda A.R., Brahmanpally B., Kalakanda P.M., Ramakrishna K., Chinnapaka V.R.D. Incidence & prognosis of acute kidney injury in individuals of snakebite in a tertiary care hospital in India. Indian J. Med. Res. 2017;146(6):754–758. doi: 10.4103/ijmr.IJMR_1581_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintana-Castillo J.C., Estrada-Gómez S., Cardona-Arias J.A. Economic evaluations of interventions for snakebites: a systematic review. Clinicoecon Outcomes Res. 2020;12:547–554. doi: 10.2147/CEOR.S259426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachett J.A.G., Mota da Silva A., Dantas A.W.C.B., Dantas T.R., Colombini M., Moura da Silva A.M., Monteiro W.M., Bernarde P.S. Cerebrovascular accidents related to snakebites in the amazon-two case reports. Wilderness Environ. Med. 2020;31(3):337–343. doi: 10.1016/j.wem.2020.04.009. [DOI] [PubMed] [Google Scholar]
- Sachett J.A.G., Val F.F., Alcântara J.A., Cubas-Vega N., Montenegro C.S., da Silva I.M., de Souza T.G., Santana M.F., Ferreira L.C.L., Monteiro W.M. Bothrops atrox snakebite: how a bad decision may lead to a chronic disability: a case report. Wilderness Environ. Med. 2020;31(3):317–323. doi: 10.1016/j.wem.2020.03.001. [DOI] [PubMed] [Google Scholar]
- Saz-Parkinson Z., del Pino Luengo M., López-Cuadrado T., Andújar D., Carmona-Alférez R., Flores R.M., Amate J.M. Approach to the epidemiology of venomous bites in Spain. Toxicon. 2012;60(4):706–711. doi: 10.1016/j.toxicon.2012.03.021. [DOI] [PubMed] [Google Scholar]
- Seneviratne U, Dissanayake S. Neurological manifestations of snake bite in Sri Lanka. J. Postgrad. Med. 2002;48(4):275–279. [PubMed] [Google Scholar]
- Sharma S.K., Chappuis F., Jha N., Bovier P.A., Loutan L., Koirala S. Impact of snake bites and determinants of fatal outcomes in southeastern Nepal. Am. J. Trop. Med. Hyg. 2004;71(2):234–238. doi: 10.4269/ajtmh.2004.71.234. [DOI] [PubMed] [Google Scholar]
- Sinha R., Nandi M., Tullus K., Marks S.D., Taraphder A. Ten-year follow-up of children after acute renal failure from a developing country. Nephrol. Dial. Transplant. 2009;24(3):829–833. doi: 10.1093/ndt/gfn539. [DOI] [PubMed] [Google Scholar]
- Snow R.W., Bronzan R., Roques T., Nyamawi C., Murphy S., Marsh K. The prevalence and morbidity of snake bite and treatment-seeking behaviour among a rural Kenyan population. Ann. Trop. Med. Parasitol. 1994;88:665–671. doi: 10.1080/00034983.1994.11812919. [DOI] [PubMed] [Google Scholar]
- Spano S.J., Vohra R., Macias F. Long-term complications of rattlesnake bites: a telephone survey from Central California. Wilderness Environ. Med. 2014;25(2):210–213. doi: 10.1016/j.wem.2013.11.004. [DOI] [PubMed] [Google Scholar]
- Srirangan A., Pushpakumara J., Wanigasuriya K. A life-threatening complication due to pulmonary haemorrhage following hump-nosed viper bite. BMC Pulm. Med. 2020;20(1):35. doi: 10.1186/s12890-020-1070-9. PMID: 32033543; PMCID: PMC7006151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stienstra Y., Steinhorst J., Aglanu L.M., Ravensbergen S.J., Dari C.D., Abass K.M., Mireku S.O., Ken J.A.P., Enuameh Y.A.K., Blessmann J., Harrison R.A., Amuasi J.H. ‘The medicine is not for sale’: practices of traditional healers in snakebite envenoming in Ghana. PLoS Neglected Trop. Dis. 2021 doi: 10.1371/journal.pntd.0009298. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tochie The neglected burden of snakebites in Cameroon: a review of the epidemiology, management and public health challenges. BMC Res. Notes. 2017;10:405. doi: 10.1186/s13104-017-2718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaiyapuri S., Vaiyapuri R., Ashokan R., Ramasamy K., Nattamaisundar K. Snakebite and its socio-economic impact on the rural population of Tamil nadu, India. PloS One. 2013;8(11) doi: 10.1371/journal.pone.0080090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oirschot J., Ooms G.I., Okemo D.J., Waldmann B., Reed T. An exploratory focus group study on experiences with snakebites: health-seeking behaviour and challenges in rural communities of Kenya. Trans. R. Soc. Trop. Med. Hyg. 2021;115(6):613–618. doi: 10.1093/trstmh/trab059. [DOI] [PubMed] [Google Scholar]
- Waiddyanatha S., Silva A., Siribaddana S., Isbister G.K. Long-term effects of snake envenoming. Toxins. 2019;11(4):193. doi: 10.3390/toxins11040193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weant K.A., Bowers R.C., Reed J., Braun K.A., Dodd D.M., Baker S.N. Safety and cost-effectiveness of a clinical protocol implemented to standardize the use of Crotalidae polyvalent immune Fab antivenom at an academic medical center. Pharmacotherapy. 2012 May;32(5):433–440. doi: 10.1002/j.1875-9114.2012.01026.x. Epub 2012 Mar 30. [DOI] [PubMed] [Google Scholar]
- Weinstein S.A., Mirtschin P.J., Tristram H., Lawton L., White J. Local morbidity from red-bellied black snake (Pseudechis porphyriacus, Elapidae) envenoming: two cases and a brief review of management. Toxicon. 2018;142:34–41. doi: 10.1016/j.toxicon.2017.12.047. 10.1016/j.toxicon.2017.12.047. Epub 2017 Dec 19. [DOI] [PubMed] [Google Scholar]
- Wijesinghe C.A., Williams S.S., Kasturiratne A., Dolawaththa N., Wimalaratne P., Wijewickrema B., Jayamanne S.F., Isbister G.K., Dawson A.H., Lalloo D.G., de Silva H.J. A randomized controlled trial of a brief intervention for delayed psychological effects in snakebite victims. PLoS Neglected Trop. Dis. 2015;9 doi: 10.1371/journal.pntd.0003989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams S.S., Wijesinghe C.A., Jayamanne S.F., Buckley N., Dawson A., Lalloo D.G., de Silva H.J. Delayed psychological morbidity associated with snakebite envenoming. PLoS Neglected Trop. Dis. 2011;5(8):e1255. doi: 10.1371/journal.pntd.0001255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wongtongkam N., Wilde H., Sitthi-Amorn C., Ratanabanangkoon K. A study of 225 Malayan pit viper bites in Thailand. Mil. Med. 2005;170(4):342–348. doi: 10.7205/milmed.170.4.342. [DOI] [PubMed] [Google Scholar]
- Yates V.M., Lebas E., Orpiay R., Bale B.J. Management of snakebites by the staff of a rural clinic: the impact of providing free antivenom in a nurse-led clinic in Meserani, Tanzania. Ann. Trop. Med. Parasitol. 2010;104(5):439–448. doi: 10.1179/136485910X12743554760306. 10.1179/136485910X12743554760306. PMID: 20819312. [DOI] [PubMed] [Google Scholar]
- Yerawar C., Punde D., Pandit A., Deokar P. Russell's viper bite & the empty sella syndrome. QJM. hcaa197. 2020 doi: 10.1093/qjmed/hcaa197. [DOI] [PubMed] [Google Scholar]
- Zeng F., Chen C., Chen X., Zhang L., Liu M. Small incisions combined with negative-pressure wound therapy for treatment of protobothrops mucrosquamatus bite envenomation: a new treatment strategy. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2019;25:4495–4502. doi: 10.12659/MSM.913579. PMID: 31204383; PMCID: PMC6592139. [DOI] [PMC free article] [PubMed] [Google Scholar]