Abstract
Dislocations of the elbow require recognition of the injury pattern followed by adequate treatment to allow early mobilisation. Not every injury requires surgery but if surgery is undertaken all structures providing stability should be addressed, including fractures, medial and lateral ligament insertion and the radial head. The current concepts of biomechanical modelling are addressed and surgical implications discussed.
Keywords: Elbow trauma, Joint dislocation, Elbow instability, Elbow clinical assessment, Elbow trauma imaging, Elbow surgery
1. Introduction
Elbow dislocations present with a variety of injury patterns which require expert recognition to define the best treatment pathway. These injuries are not uncommon and in children the elbow joint is the most frequently dislocated joint. In adults only the shoulder joint is more frequently dislocated.
Notably, the incidence of all elbow dislocations has been recorded at 5.21 per 100,000 person-years, with greater incidence in males (53% in males, with a 1.02 male – female incidence ratio, p < 0.001).1 Of all elbow dislocations 18–45% are likely to be terrible triad injuries,2 constituting a combination of elbow dislocation, radial head fracture and coronoid process fracture. These are more common in adults as children have flexible and strong ligaments whilst the bones are still immature. Consequently, children are more likely to incur a fracture of the distal humerus or an avulsion fracture at the ligament attachment but not commonly a dislocation.3,4
The mechanism of injury may vary, ranging from falling onto an outstretched hand or direct high energy impact. The combination of direction of the injury forces, energy of injury and patient characteristics, particularly bone age, will determine the injury pattern.
Elbow dislocations can be classified as simple, i.e., a stand-alone dislocation, mostly posterior, at the joint with peri-articular avulsions less than 2 mm,5 or complex, in combination with an associated fracture of the radius, humerus or ulna at the ipsilateral elbow joint.6 Multiple complex dislocation patterns can be identified, ranging from a posterior dislocation with a fracture of the radial head (Posterior radial head fracture dislocation, PRHFD), and the terrible triad injury (TTI),2 to the Varus posteromedial rotational instability injury (VPMRI), the latter potentially leading to chronic subluxation. Fractures of the proximal ulna not involving the trochlear notch are often associated with a dislocation of the proximal radio-ulnar joint and are known as Monteggia fracture dislocations. Olecranon fractures may be associated with anterior olecranon fracture dislocation (AOFD) or posterior olecranon fracture dislocation (POFD).
Treatment of simple and complex fracture dislocations of the elbow follows the principles of achieving a stable reduction with the aim to commence mobilisation as soon as possible. Stiffness is the most common untoward outcome rather than instability. Surgical intervention must be judiciously considered for the restoration of joint congruity and stabilisation of ligament injuries and avulsion fractures. Traditional treatment was mainly nonoperative7 but even with prolonged immobilisation ligament stability could not be guaranteed.8 Modern treatment advocates re-establishing the congruency and stability of the joint to allow early mobilisation, by surgical repair if necessary, as this would prevent joint stiffness, instability and arthrosis of the elbow.9,10
This review will address the anatomical background of simple and complex dislocations, including the role of stabilisers, present an overview of classification systems and provide a review of treatment principles as discussed in the literature.
1.1. Stabilisers of the elbow
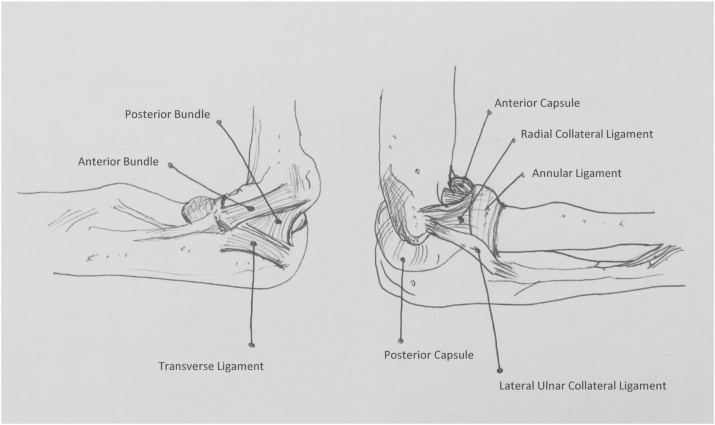
The elbow joint is a tricompartmental hinge joint. Bony and soft tissue components contribute to the stability of the elbow (Fig. 1). They can be broadly classified into:
Bony components
Ligaments
Muscles
Fig. 1.
Anatomy of elbow stabilisers (after Karbach and Elfar65).
1.1.1. Bony components
The ulno-humeral joint, by virtue of its shape, is the primary stabiliser of the elbow joint. The radial head is an important secondary stabiliser to resist valgus stress; and will become the main stabiliser against valgus forces if the medical collateral ligament (MCL) is incompetent. An intact coronoid process11 is necessary to counter posteriorly directed forces and plays an important role in stabilising the elbow.12,13 B Morrey has aptly described the coronoid process as the ‘most important piece of real estate in the elbow’ (personal communication).
1.1.2. Ligaments
The medio-lateral and rotatory stability to the elbow is provided by the medial and lateral ligament complex. The anterior band of the MCL14 and lateral ulnar collateral ligaments (LUCL) are the most important ligaments15 that provide postero-medial and postero-lateral rotatory stability to the elbow.16,17
1.1.3. Muscles
All muscles crossing the elbow and the anterior capsule contribute to the stability of elbow.18,19
Of all the structures, the following are the main primary stabiliser of the elbow:
Ulno-humeral joint
Anterior band of MCL
Lateral ulnar collateral ligament (LUCL)
1.2. Mechanism of injury and injury pattern
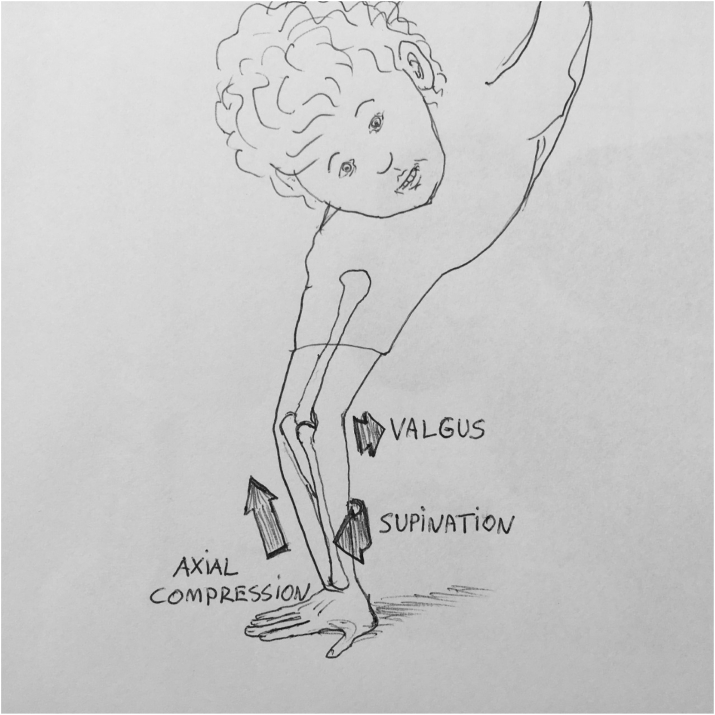
The two main rotatory mechanisms of injury are posterolateral and posteromedial. During a posterolateral rotatory force, the elbow dislocates posteriorly, radial head and coronoid process impact and may fracture, followed by the rupture of the anterior band of the MCL. This might occur falling onto an outstretched hand with the elbow in extension and forearm in supination20,21 thus the valgus force resulting in a terrible triad injury22,23(Fig. 2).
Fig. 2.
Illustration of mechanism resulting in a terrible triad injury.
The posterior radial head fracture dislocation involves falling onto the extended arm where there is hyperextension and posterolateral rotation, causing a radial head fracture.24,25
Conversely, a varus posteromedial rotatory load combined with an axial force will first lead to a fracture of the anteromedial facet followed by a fracture of the olecranon possibly with an additional fragment at the base of the coronoid and/or a lateral collateral ligament (LCL) injury.26 Both, the LCL and MCL usually avulse from the origin of their epicondyles.
The anterior olecranon fracture dislocation is thought to be caused by a direct high energy blow to the dorsal aspect of the forearm with the elbow in mid-flexion27 however the mechanism is not as well described.
1.3. Pathoanatomy and classification: dislocation, radial head fracture and coronoid fracture
There is no unifying classification for fracture dislocation of the elbow and authors have addressed separate elements to guide management. Specifically, the coronoid, radial head/neck and olecranon fractures are assessed for classification of the pathology.21 More recently recognition and description of instability as a continuum has come into the foreground.
1.3.1. Coronoid fractures
1.3.1.1. Regan-Morrey Classification
The size of the coronoid fragment has been recognised as important fracture to predict instability and been utilised in the Regan-Morrey Classification.28,29
Type 1: Avulsion fracture of the coronoid process tip
Type 2: fracture fragment is less than 50% of the coronoid process
Type 3: fracture fragment is more than 50% of the coronoid process
Also:
A: No associated elbow dislocation
B: Associated Elbow dislocation
1.3.2. O'Driscoll Stages of Instability
This classification originates from an understanding of the stages of instability and involves the anatomical location and fracture size, thus helping to derive further details entailing the mechanism of injury.30, 31, 32 This classification is based on anatomical location of the fracture: tip, anteromedial facet and base (which are subdivided further).32
1.3.2.1. Type 1 - tip fracture
Involves the coronoid tip with fragments smaller then 2 mm, most commonly seen in terrible triad injuries33 and also in isolation with subluxations.34 It is important to note the tip fractures does not extend past the sublime tubercle, hence the MCLC insertion to the sublime tubercle tends to remain intact with these injuries.35,36
1.3.2.2. Type 2 - anteromedial facet fracture
Sub-type 1: No coronoid tip involvement, fracture extends medially to the tip and anterior to the sublime tubercle.
Sub-type 2: Subtype 1 with the involvement of the tip.
Sub-type 3: Anteromedial rim of the coronoid process and the sublime tubercle ± tip involvement.
The type 2 injury is usually associated with varus posteromedial rotatory fracture subluxations,21 and anteromedial fractures are less common with triad injuries23 (Fig. 3a, b, 3c).
Fig. 3.
3a, 3b, 3c: Coronoid fracture Type 2 (anteromedial facet) treated with open reduction and internal fixation.
1.3.2.3. Type 3 - basal coronoid (large fractures)
Fracture through the body and basal part of the coronoid process with a minimum of 50% of the coronoid process height.
Sub-type 1: Involving only the coronoid process.
Sub-type 2: Involving both a coronoid body fracture and fracture of the olecranon.
1.4. Radial head fracture
The radial head fracture configuration may help to determine stability of the elbow and can also be classified into specific types to determine an effective treatment plan. The Mason classification was initially devised37 and succeeded by Johnson modifications, which has also been updated by Morrey and later Hotchkiss.38
1.4.1. Mason-Johnson classification
Type 1: Non-displaced fracture at head, neck, intra articular, or marginal lip (or those displaced up to less than 2 mm with no mechanical block).
Type 2: Displaced partial articular fracture with or without comminution (displacement more than 2 mm and considered repairable, possible mechanical block to motion and loss of congruency of joint surface therefore needing surgical intervention).
Type 3: Comminuted fracture of the radial head or neck involving the entire radial head (considered not repairable when radiographically/intraoperatively analysed, requiring excision or replacement).
Type 4: Radial head fracture with dislocation of the elbow joint.
Note: Type 4 might apply to all configurations of radial head fractures.
1.5. Olecranon fractures
Olecranon fractures are present in AOFD and POFD and have implication on the stability of the elbow. They can be classified by multiple methods including the Colton,39 Mayo40 and AO (Arbeitsgemeinschaft Osteosynthese)41 classifications.
1.6. Dislocations
1.6.1. Simple dislocations of the elbow
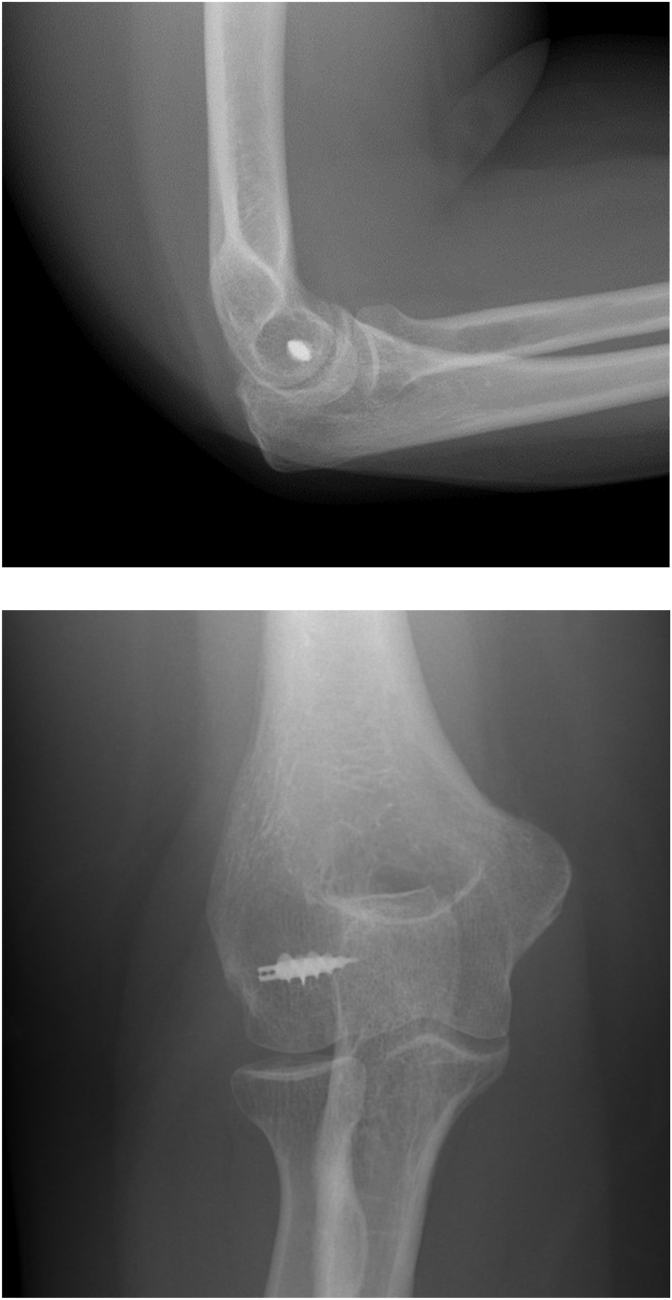
Simple dislocations of the elbow constitute injuries without major fracture component (Fig. 4) and most of them are stable after manipulation and reduction (98%). In a small percentage of injuries there may be a persistent subtle subluxation due to associated ligamentous injury. Further imaging utilising magnetic resonance imaging (MRI) may be useful.42 The threshold to perform a formal EUA under general anaesthesia should be low and these injuries may require surgical fixation.43,44
Fig. 4.
Simple posterior dislocation of the elbow without fracture.
1.6.1.1. Valgus hyper extension
Valgus hyper extension causes a posterolateral dislocation, which is considered the most frequent direction for dislocation.12 There is circular disruption of soft tissue structures, first being the LCLC, then the anterior and posterior capsule then MCLC, followed by the common flexor origin.5
1.6.1.2. Varus internal rotation
Posteromedial dislocations are 10% of all dislocations caused by varus and posteromedial rotation, leading to significant damage of the medial structures in the first instance (Fig. 5).
Fig. 5.
Simple medial dislocation of elbow with high risk of persistent instability.
1.6.1.3. Stages of simple elbow dislocation10
Stage 1
Disruption of LUCL with partial or complete disruption of remainder of LCLC, resulting in posterolateral subluxation.
Stage 2
Additional disruption of the anterior capsule, resulting in yet incomplete posterolateral elbow dislocation.
- Stage 3
-
a)Disruption of all soft tissues lateral to medial except the anterior bundle of the MCL, which forms a pivot around which the elbow dislocates in posterolateral rotational direction.
-
b)Complete disruption of all medial collateral ligament structures.
-
a)
The staging is based on the concept by O'Driscoll10 that the same mechanism of injury may lead with a different magnitude of force to an increasing circumferential rupture of soft tissues. Injuries at Stage 2 and 3 usually require surgical repair even in the absence of any bony injury (Fig. 6a and b) and can be diagnosed on careful analysis of the radiographs. It is important to understand that all simple elbow dislocations are not the same. The more energy is imparted during the injury, the more ‘aggressive’ the management may need to be, and the more guarded is the prognosis.
Fig. 6.
6 a, 6b: Ligament reconstruction following simple dislocation with complete ligament disruption (Stage 3).
1.6.2. Complex fracture-dislocations
Complex dislocations involve dislocations with one or more associated fractures. Treatment usually requires surgical reconstruction of bony and ligamentous stability. Recognition of the injury pattern is critical to diagnose and manage this injury.
1.7. Stability model and relevance for treatment
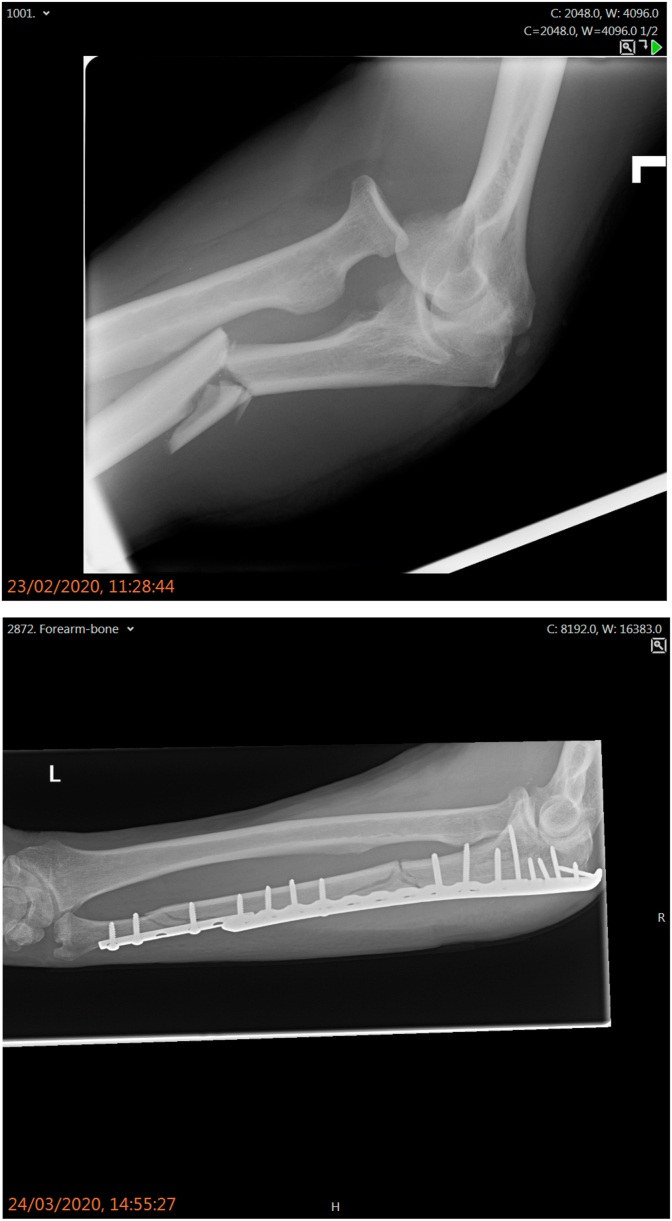
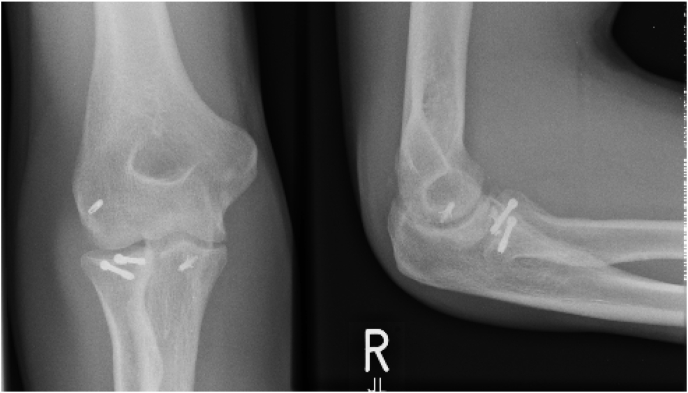
The conventional patterns of instability and fracture dislocation may fall under the following groups: Terrible triad,20,21 Posterior radial head fracture dislocation, Monteggia fracture-dislocation45 (Fig. 7a and b), Anteromedial coronoid fracture and Trans-olecranon fracture-dislocations.
Fig. 7.
7a, 7b: Monteggia fracture-dislocation treated with open reduction and internal fixation.
These groups are useful for identifying the mechanism of injury and possible treatment plans of the individual pathologies, furthermore the concept is important to make valid assumptions regarding the stability status of the joint.
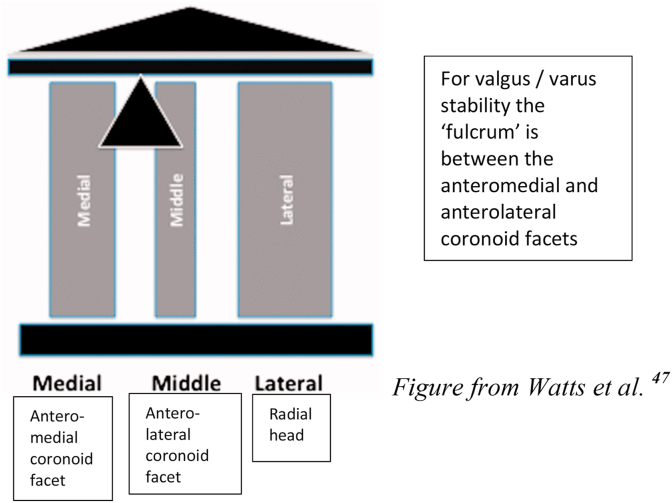
Recently the three-column model has been proposed by Watts et al. from Wrightington,5 which differs from the previously discussed ring concept.46 The model consists of a lateral, middle and medial column with the structures involved listed below:
| Lateral Column: Radial head + Capitellum + LCLC |
| Middle Column: Anterolateral facet of coronoid process + lateral trochlea |
| Medial Column: Anteromedial facet + medial trochlea + MCLC |
In this model varus and valgus stability is balanced around an axis between the medial and middle columns, with the lateral column being the primary resisting osseous structure against valgus stress. Varus forces are thought to be resisted primarily by the medial column.
As long as the lateral column is intact the middle column may be neglected in its contribution to valgus stability, however following disruption of the lateral column, the middle column (being a secondary valgus stabiliser) becomes important as a valgus restraint47, 48 (Fig. 8).
Fig. 8.
Illustration of ‘column theory’ – from Watts et al.47
1.8. Clinical assessments
1.8.1. Presentation
Clinical presentation of a dislocated elbow is usually unmistakable with pain, swelling, deformity and inability to flex or extend the elbow.49 However, a subluxed or unstable elbow following injury may present with subtle symptoms. Patients will complain of pain, clicking of the joint and inability to move through a full range of motion. Specifically, the patient may experience locking on extension.20
Overall, it is vital to derive a full history of the injury to develop an understanding of the mechanism of injury and if possible, to visualise the position of the elbow, along with the forces involved in the scenario of the accident. Evaluation and recording of the neurovascular status, the condition of surrounding skin and the involvement of other joints (shoulder and wrist) are also important.50
1.9. Clinical examination
In simple dislocations, loss of relationship of the normal bony landmarks will be evident.5 Bruising on the medial or lateral side would indicate possible ligamentous injury.12 Any associated neurovascular deficit and open injuries should be noted.
Posterolateral instability associated with a terrible triad injury might lead to a positive drawer sign and positive pivot test, this should only be assessed under general anaesthesia.
1.10. Imaging
Plain radiographs of the elbow in anteroposterior and lateral position, are usually diagnostic and would show any additional fractures (Fig. 10a and b). Post-manipulation radiographs are mandatory to demonstrate satisfactory relocation and full congruency of the joint.5,21 The drop sign, if persistent, may alert to ongoing instability (Fig. 9).
Fig. 10.
10a, 10b, 10c: Radiographic assessment (10a, b) of terrible triad injury followed by CT (10c).
Fig. 9.
The ‘drop sign’ after closed reduction indicating instability.66
As a simple guidance, a line drawn through the radial head and neck should always pass through the centre of the capitellum in a normally aligned elbow in any view seen on x-ray.20 Suspected injury anywhere else in the ipsilateral upper limb (10–20%)21 should be excluded by appropriate radiographs.
CT scan, especially 3D views (Fig. 10), is extremely helpful to evaluate any associated fracture.51
In an acute setting an MRI23 scan may be of limited use, unless required for further evaluation of a ‘simple dislocation’ with persistent instability (Fig. 11). In the case of longstanding symptoms an MRI may be invaluable to understand the structural status of the tendons and ligaments.12 To further investigate the soft tissue structures, ultrasound imaging can provide a dynamic examination of these structures but is of limited role in the acute setting.52
Fig. 11.
MRI following postero-lateral elbow dislocation with disruption of the LCLC.
1.11. Treatment
1.11.1. Non-surgical
Reduction of the dislocated elbow is usually performed with pain relief and under conscious sedation. Manipulation involves inline traction with leverage of the olecranon over the distal humerus. Stability is checked by supervised active range of motion by the patient. A posterior splint in 90° of flexion in a neutral position, or if unstable in protonation, for one to two weeks, will help the tissues to settle before commencing range of movement exercises.
Should there be an unstable dislocation which cannot be held reduced concentrically, further assessment and surgical intervention must be considered.
A nonoperative approach would be appropriate in following circumstances.20,53:
-
•
Small radial head fracture with no rotation block (pronation and supination being 60° block free), minimal radial fracture fragment displacement
-
•
Stable after reduction; on ROM from 45° flexion and beyond
-
•
Joint congruency
-
•
Small coronoid fracture that is reduced
-
•
Small fractures but no intra-articular fragments
The failure to recognise subtle instability may lead to persistent pain, stiffness and post-traumatic arthritis.53 Undisplaced or minimally displaced (<5 mm) fractures of the anteromedial facet (AMF) of the coronoid can be treated nonoperatively, provided the joint is concentric and stable to at least 30° of extension.51 In these patients, initial weekly radiograph is mandatory to exclude any re-displacement of joint or fracture fragments.
1.11.2. Surgical treatment
Surgical repair is required for the majority of terrible triad injuries15: the radial head by open reduction and internal fixation (ORIF) (Fig. 12) or replacement if irreparable (Fig. 13), the LCLC by reattaching to the lateral epicondyle by anchors or bony tunnel and secure fixation of the coronoid fracture by any of several different techniques. If there is stability throughout the range of motion after lateral (radial head and LCLC) column repair, ORIF may not be required for Regan-Morrey 1 and 2 coronoid fractures.54 The MCLC may need repair if there is persisting instability shown by a posterior sag test after lateral column and capsule/coronoid repair.
Fig. 12.
Open reduction and internal fixation of radial head fracture.
Fig. 13.
Prosthetic replacement of radial head after fracture.
The surgical approach would depend on the type of proposed procedure. The single universal posterior approach allows lateral and medial access, for fixation or replacement of the radial head as well as repair of the coronoid process.55 Separate approaches might carry less risk regarding haematoma formation and potential healing problems of the long posterior skin flaps15 but there is an increased chance of cutaneous nerve injury.
A trans-olecranon fracture dislocation will require surgical fixation of the olecranon by either tension-band wiring (for simple, non-comminuted transverse or short oblique fractures) or contoured plate (for comminuted or unstable fractures)51,56(Fig. 14).
Fig. 14.
Trans-olecranon fracture dislocation of elbow requiring plate fixation.
Anteromedial facet (AMF) fractures would normally require internal fixation (cannulated screws, tension band or buttress plate)57 as chronic instability, if developed, may be a difficult problem to treat.
Fluoroscopic examination of the elbow should be performed throughout the procedure for the assessment of fixation and residual instability.35
1.11.2.1. Post-surgical care
A removable posterior splint may be applied for comfort and soft tissue healing. Active/active assisted mobilisation of the elbow should be started as soon as possible (within 24–48 h) after stable reconstruction of the elbow.58 In patients where static fixators are used, these should ideally be removed after three weeks to avoid joint stiffness. Any hinged fixator should be limited to 30° of extension for four weeks followed by a hinged brace for another four weeks if needed.15 At the end of six-to-eight weeks the elbow brace should be removed, and unrestricted range of motion is advised.59
1.12. Complications
The more complex the injury, the higher will be the likelihood of complications. There is a significant (22%–40%) reoperation rate as a result of injury and post-surgery complications60, 61, 62in these injuries.
The following are the most common complications15:
-
•
Re-dislocation: as a result of soft tissue injury which give rise to this instability.
-
•
Post-traumatic stiffness: very common, in particular when early therapy/range of movement exercises are delayed.
-
•
Failure of internal fixation: a common complication when radial neck fixation is performed, with poor vascularity leading to non-union and osteonecrosis.
-
•
Malalignment: e.g., of the anteromedial coronoid process leading to varus subluxation and instability.63
-
•
Post-traumatic arthritis: as a result of cartilage damage and shearing forces due to persistent instability of the joint
-
•
Heterotopic ossification: common with delay to the initial surgery e.g., in the multiple injured patient, elbow injuries in association with burns, head injury, poor soft tissue handling during surgery.64
-
•
Neurovascular compromise: especially ulna nerve neuropathy in particular with malalignment or valgus instability.
-
•
Infection following prolonged surgery or open injuries.62
2. Conclusion
The elbow is normally an inherently stable joint and stability is maintained by the configuration of bone joint congruency and ligamentous support. Dislocations usually follow one of the two main injury patterns: rotatory posterolateral (most common) or posteromedial. The description of instability as a progressive sequence following a predictable pattern has helped to understand traumatic elbow dislocations better. The recent addition of the three-column concept has further added to the understanding and treatment rationale, in particular the role of the middle column after disruption of the lateral column.
A simple dislocation is normally managed by manipulation and reduction (98% of cases). A complex fracture dislocation, in majority of cases, requires surgical fixation of fractures and soft tissues including ligaments and capsule.
The patient should be given a guarded prognosis as return to full function depends on obtaining a stable joint and early mobilisation. Complications such as post-operative stiffness, heterotopic ossification, peripheral neurological impairment and post-traumatic arthritis are not uncommon. The aim of any treatment is to restore stability to allow early mobilisation and a safe rehabilitation program.
References
- 1.Stoneback J.W., Owens B.D., Sykes J., Athwal G.S., Pointer L., Wolf J.M. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am. 2012 Feb 1;94(3):240–245. doi: 10.2106/JBJS.J.01663. Available from: [DOI] [PubMed] [Google Scholar]
- 2.Hotchkiss R.N. fourth ed. vol. 1. J.B.Lippincott; Philadelphia: 1996. Fractures and dislocations of the elbow; pp. 929–1024. (Rockwood and Green's Fractures in Adults). [Google Scholar]
- 3.Lieber J., Zundel S.M., Luithle T., Fuchs J., Kirschner H.J. Acute traumatic posterior elbow dislocation in children. J Pediatr Orthop B. 2012 Sep;21(5):474–481. doi: 10.1097/BPB.0b013e328354b08c. Available from: [DOI] [PubMed] [Google Scholar]
- 4.Toros T., Ozaksar K. Controversy in the diagnosis of pediatric terrible triad elbow fracture dislocation. J Hand Surg Am. 2014 Oct;39(10):2121–2122. doi: 10.1016/j.jhsa.2014.06.138. `Available from: [DOI] [PubMed] [Google Scholar]
- 5.Singh J., Elvey M.H., Hamoodi Z., Watts A.C. Current perspectives on elbow dislocation and instability. Ann Joint. 2021 Jan;6:10. doi: 10.21037/aoj-19-186. Available from: [DOI] [Google Scholar]
- 6.Hildebrand K.A., Patterson S.D., King G.J. Acute elbow dislocations: simple and complex. Orthop Clin N Am. 1999 Jan;30(1):63–79. doi: 10.1016/s0030-5898(05)70061-4. Available from: [DOI] [PubMed] [Google Scholar]
- 7.Josefsson P.O., Gentz C.F., Johnell O., Wendeberg B. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. A prospective randomized study. J Bone Joint Surg Am. 1987 Apr;69(4):605–608. [PubMed] [Google Scholar]
- 8.Broberg M.A., Morrey B.F. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res. 1987 Mar;(216):109–119. [PubMed] [Google Scholar]
- 9.Pugh D.M., Wild L.M., Schemitsch E.H., King G.J., McKee M.D. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004 Jun;86(6):1122–1130. doi: 10.2106/00004623-200406000-00002. Available from: [DOI] [PubMed] [Google Scholar]
- 10.O'Driscoll S.W., Jupiter J.B., King G.J., Hotchkiss R.N., Morrey B.F. The unstable elbow. Instr Course Lect. 2001;50:89–102. [PubMed] [Google Scholar]
- 11.Xiao K., Zhang J., Li T., Dong Y.L., Weng X.S. Anatomy, definition, and treatment of the "terrible triad of the elbow" and contemplation of the rationality of this designation. Orthop Surg. 2015;7(1):13–18. doi: 10.1111/os.12149. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson P.M., Griffiths E., Watts A.C. Simple elbow dislocation. Shoulder Elbow. 2017 Jul;9(3):195–204. doi: 10.1177/1758573217694163. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reichel L.M., Milam G.S., Hillin C.D., Reitman C.A. Osteology of the coronoid process with clinical correlation to coronoid fractures in terrible triad injuries. J Shoulder Elbow Surg. 2013 Mar;22(3):323–328. doi: 10.1016/j.jse.2012.10.038. Available from: [DOI] [PubMed] [Google Scholar]
- 14.Regan W.D., Korinek S.L., Morrey B.F., An K.N. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. 1991 Oct;(271):170–179. [PubMed] [Google Scholar]
- 15.Jones A.D.R., Jordan R.W. Complex elbow dislocations and the "terrible triad" injury. Open Orthop J. 2017;11:1394–1404. doi: 10.2174/1874325001711011394. Published 2017 Nov 30. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edwards D.S., Arshad M.S., Luokkala T., Kedgley A.E., Watts A.C. The contribution of the posterolateral capsule to elbow joint stability: a cadaveric biomechanical investigation. J Shoulder Elbow Surg. 2018 Jul;27(7):1178–1184. doi: 10.1016/j.jse.2018.02.045. Available from: [DOI] [PubMed] [Google Scholar]
- 17.Tarassoli P., McCann P., Amirfeyz R. Complex instability of the elbow. Injury. 2017 Mar;48(3):568–577. doi: 10.1016/j.injury.2013.09.032. Available from: [DOI] [PubMed] [Google Scholar]
- 18.Safran M.R., Baillargeon D. Soft-tissue stabilizers of the elbow. J Shoulder Elbow Surg. 2005 Jan-Feb;14(1 Suppl S):179S–185S. doi: 10.1016/j.jse.2004.09.032. Available from: [DOI] [PubMed] [Google Scholar]
- 19.An K.N., Hui F.C., Morrey B.F., Linscheid R.L., Chao E.Y. Muscles across the elbow joint: a biomechanical analysis. J Biomech. 1981;14(10):659–669. doi: 10.1016/0021-9290(81)90048-8. Available from: [DOI] [PubMed] [Google Scholar]
- 20.Battista C., Cohen M. Terrible triad injury of elbow. ORTHO BULLETS. https://www.orthobullets.com/trauma/1021/terrible- triad-injury-of-elbow Available from:
- 21.Kani K.K., Chew F.S. Terrible triad injuries of the elbow. Emerg Radiol. 2019 Jun;26(3):341–347. doi: 10.1007/s10140-019-01676-1. Available from: [DOI] [PubMed] [Google Scholar]
- 22.Egol K.A., Immerman I., Paksima N., Tejwani N., Koval K.J. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis. 2007;65(4):263–270. [PubMed] [Google Scholar]
- 23.Beingessner D.M., Pollock J.W., King G.J.W. Elbow fractures and dislocations. In: Court-Brown C.M., Heckman J.D., McQueen M.M., editors. Rockwood and Green's Fractures in Adults. eighth ed. Lippincott Williams & Wilkins/Wolters Kluwer Health; Philadelphia: 2015. pp. 1180–1227. 2015. [Google Scholar]
- 24.Dines D.M., Lorich D., Helfet D. Thieme Medical Publishers; 2008. Solutions for Complex Upper Extremity Trauma. [Google Scholar]
- 25.Ring D., Jupiter J.B. Fracture-dislocation of the elbow. J Bone Joint Surg Am. 1998 Apr;80(4):566–580. [PubMed] [Google Scholar]
- 26.McLean J., Kempston M.P., Pike J.M., Goetz T.J., Daneshvar P. Varus posteromedial rotatory instability of the elbow. J Orthop Trauma. 2018 Dec;32(12):469–474. doi: 10.1097/BOT.0000000000001313. Available from: [DOI] [PubMed] [Google Scholar]
- 27.Mouhsine E., Akiki A., Castagna A. Transolecranon anterior fracture dislocation. J Shoulder Elbow Surg. 2007 May;16(3):352–357. doi: 10.1016/j.jse.2006.07.005. Available from: [DOI] [PubMed] [Google Scholar]
- 28.Regan W., Morrey Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989 Oct;71(9):1348–1354. [PubMed] [Google Scholar]
- 29.Doornberg J.N., Ring D. Coronoid fracture patterns. J Hand Surg Am. 2006 Jan;31(1):45–52. doi: 10.1016/j.jhsa.2005.08.014. Available from: [DOI] [PubMed] [Google Scholar]
- 30.O'Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991 Mar;73(3):440–446. [PubMed] [Google Scholar]
- 31.O'Driscoll SW, Morrey BF, Korinek S, An KN. Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop Relat Res. 1992Jul(280):186-197. [PubMed]
- 32.O'Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. 2003 Jan. [PubMed] [Google Scholar]
- 33.Mellema J.J., Doornberg J.N., Dyer G.S., Ring D. Distribution of coronoid fracture lines by specific patterns of traumatic elbow instability. J Hand Surg Am. 2014 Oct;39(10):2041–2046. doi: 10.1016/j.jhsa.2014.06.123. Available from: [DOI] [PubMed] [Google Scholar]
- 34.Sheehan S.E., Dyer G.S., Sodickson A.D., Patel K.I., Khurana B. Traumatic elbow injuries: what the orthopedic surgeon wants to know. Radiographics. 2013 May;33(3):869–888. doi: 10.1148/rg.333125176. Available from: [DOI] [PubMed] [Google Scholar]
- 35.Mathew P.K., Athwal G.S., King G.J. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009 Mar;17(3):137–151. doi: 10.5435/00124635-200903000-00003. Available from: [DOI] [PubMed] [Google Scholar]
- 36.Lindenhovius A., Karanicolas P.J., Bhandari M., van Dijk N. Ring D; Collaboration for Outcome Assessment in Surgical Trials. Interobserver reliability of coronoid fracture classification: two-dimensional versus three-dimensional computed tomography. J Hand Surg Am. 2009 Nov;34(9):1640–1646. doi: 10.1016/j.jhsa.2009.07.009. Available from: [DOI] [PubMed] [Google Scholar]
- 37.Mason M.L. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954 Sep;42(172):123–132. doi: 10.1002/bjs.18004217203. Available from: [DOI] [PubMed] [Google Scholar]
- 38.Hotchkiss R.N. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997 Jan;5(1):1–10. doi: 10.5435/00124635-199701000-00001. Available from: [DOI] [PubMed] [Google Scholar]
- 39.Colton C.L. Fractures of the olecranon in adults: classification and management. Injury. 1973 Nov;5(2):121–129. doi: 10.1016/s0020-1383(73)80088-9. Available from: [DOI] [PubMed] [Google Scholar]
- 40.Benetton C.A., Cesa G., El-Kouba Junior G., Ferreira A.P., Vissoci J.R., Pietrobon R. Agreement of olecranon fractures before and after the exposure to four classification systems. J Shoulder Elbow Surg. 2015 Mar;24(3):358–363. doi: 10.1016/j.jse.2014.10.025. Available from: [DOI] [PubMed] [Google Scholar]
- 41.Mueller M.E., Allgower M., Schneider R., Willenegger H. Springer Berlin; 1991. Manual of Internal Fixation: Techniques Recommended by the AO-ASIF Group; pp. 142–143. [Google Scholar]
- 42.Luokkala T., Temperley D., Basu S., Karjalainen T.V., Watts A.C. Analysis of magnetic resonance imaging-confirmed soft tissue injury pattern in simple elbow dislocations. J Shoulder Elbow Surg. 2019 Feb;28(2):341–348. doi: 10.1016/j.jse.2018.08.010. Available from: [DOI] [PubMed] [Google Scholar]
- 43.Van Riet R.P. Assessment and decision making in the unstable elbow: management of simple dislocations. Shoulder Elbow. 2017 Apr;9(2):136–143. doi: 10.1177/175857326686533. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Heo Y.M., Woong J., Lee J.B., Lee D.H., Park W.K., Kim S.J. Unstable simple elbow dislocation treated with the repair of lateral collateral ligament complex. Clin Orthop Surg. 2015 Jun;7(2):241–247. doi: 10.4055/cios.2015.7.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ring D. Monteggia fractures. Orthop Clin N Am. 2013 Jan;44(1):59–66. doi: 10.1016/j.ocl.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 46.Ring D., Jupiter J.B. Fracture-dislocation of the elbow. J Bone Joint Surg Am. 1998 Apr;80(4):566–580. [PubMed] [Google Scholar]
- 47.Watts A.C., Singh J., Elvey M., Hamoodi Z. Current concepts in elbow fracture dislocation. Shoulder Elbow. 2019 Nov doi: 10.1177/1758573219884010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hamoodi Z., Singh J., Elvey M.H., Watts A.C. Reliability and validity of the Wrightington classification of elbow fracture-dislocation. Bone Joint Lett J. 2020 Aug;102-B(8):1041–1047. doi: 10.1302/0301-620X.102B8.BJJ-2020-0013.R1. Available from: [DOI] [PubMed] [Google Scholar]
- 49.Frank R., Cohen M. Elbow dislocation. https://www.orthobullets.com/trauma/1018/elbow-dislocation Available from:
- 50.Frank R, Cohen M. Elbow Dislocation. Available from: https://www.orthobullets.com/trauma/1018/elbow-dislocation.
- 51.Chan K., King G.J., Faber K.J. Treatment of complex elbow fracture-dislocations. Curr Rev Musculoskelet Med. 2016;9(2):185–189. doi: 10.1007/s12178-016-9337-8. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Draghi F., Danesino G.M., de Gautard R., Bianchi S. Ultrasound of the elbow: examination techniques and US appearance of the normal and pathologic joint. J Ultrasound. 2007;10(2):76–84. doi: 10.1016/j.jus.2007.04.005. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Najd Mazhar F., Jafari D., Mirzaei A. Evaluation of functional outcome after nonsurgical management of terrible triad injuries of the elbow. J Shoulder Elbow Surg. 2017 Aug;26(8):1342–1347. doi: 10.1016/j.jse.2017.05.012. Available from: [DOI] [PubMed] [Google Scholar]
- 54.Papatheodorou L.K., Rubright J.H., Heim K.A., Weiser R.W., Sotereanos D.G. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res. 2014 Jul;472(7):2084–2091. doi: 10.1007/s11999-014-3471-7. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meena M.K., Singh K., Meena S., Kumbhare C., Chouhan D. Lateral approach versus combined lateral and anteromedial approach for surgical treatment of terrible triad of elbow: a meta-analysis. Bull Emerg Trauma. 2020 Jan;8(1):4–9. doi: 10.29252/beat-080102. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mortazavi S.M., Asadollahi S., Tahririan M.A. Functional outcome following treatment of transolecranon fracture-dislocation of the elbow. Injury. 2006 Mar;37(3):284–288. doi: 10.1016/j.injury.2005.10.028. Available from: [DOI] [PubMed] [Google Scholar]
- 57.Rhyou I.H., Kim K.C., Lee J.H., Kim S.Y. Strategic approach to O'Driscoll type 2 anteromedial coronoid facet fracture. J Shoulder Elbow Surg. 2014 Jul;23(7):924–932. doi: 10.1016/j.jse.2014.02.016. Available from: [DOI] [PubMed] [Google Scholar]
- 58.Liu G., Ma W., Li M., Feng J., Xu R., Pan Z. Operative treatment of terrible triad of the elbow with a modified Pugh standard protocol: retrospective analysis of a prospective cohort. Medicine (Baltim) 2018 Apr;97(16) doi: 10.1097/MD.0000000000010523. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Park S.M., Lee J.S., Jung J.Y., Kim J.Y., Song K.S. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O'Driscoll classification and ligament injury. J Shoulder Elbow Surg. 2015 Jan;24(1):74–82. doi: 10.1016/j.jse.2014.07.010. Available from: [DOI] [PubMed] [Google Scholar]
- 60.Chen H.W., Liu G.D., Wu L.J. Complications of treating terrible triad injury of the elbow: a systematic review. PloS One. 2014 May;9(5) doi: 10.1371/journal.pone.0097476. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Haller J.M., Hulet D.A., Hannay W., Cardon J., Tashjian R., Beingessner D. Patient outcomes after transolecranon fracture-dislocation. J Am Acad Orthop Surg. 2021 Feb;29(3):109–115. doi: 10.5435/JAAOS-D-20-00254. Available from: [DOI] [PubMed] [Google Scholar]
- 62.Lanzerath F., Hackl M., Wegmann K., Müller L.P., Leschinger T. The treatment of anteromedial coronoid facet fractures: a systematic review. J Shoulder Elbow Surg. 2020 Sep;S1058–2746(20):30770–30779. doi: 10.1016/j.jse.2020.09.008. Available from: [DOI] [PubMed] [Google Scholar]
- 63.Wang X., Chang S.M., Yu G.R. Anteromedial coronoid facet fractures. Eur J Orthop Surg Traumatol. 2013 Apr;23(3):251–255. doi: 10.1007/s00590-012-0990-3. Available from: [DOI] [PubMed] [Google Scholar]
- 64.Dodds S.D., Hanel D.P. 38.Heterotopic ossification of the elbow. In: Trumble T.E., editor. Wrist and Elbow Reconstruction & Arthroscopy. American society for surgery of the hand; 2006. pp. p425–p438. [Google Scholar]
- 65.Karbach L.E., Elfar J. Elbow instability: anatomy, biomechanics, diagnostic maneuvers, and testing. J Hand Surg Am. 2017;42(2):118–126. doi: 10.1016/j.jhsa.2016.11.025. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Coonrad R.W., Roush T.F., Major N.M., Basamania C.J. The drop sign, a radiographic warning of elbow instability. J Shoulder Elbow Surg. 2005;14(3):312–317. doi: 10.1016/j.jse.2004.09.002. [DOI] [PubMed] [Google Scholar]