Abstract
Background:
Advanced cancer (AC) patients experience serious physical and psychological problems with the disease progression. When approaching the end of life, these patients have to cope with not only the bodily illness, but also the spiritual crisis. Conventional psychological treatments reduce distress to a certain extent, but for patients with AC, especially when they face progressive illness and are approaching death, their psychological problems are complex, and no simple solutions are in sight. Therefore, we designed this study to evaluate the efficacy of the combined Naikan therapy (NT) and Morita therapy (MT) on psychological distress and posttraumatic growth in patients with AC.
Method:
One hundred thirty patients newly diagnosed with AC were allocated randomly into treatment (n = 65) and control (n = 65) groups. Patients in the treatment group received combined NT and MT for 7 consecutive weeks, while the control group received normal medical treatments without NT and MT. Patients were assessed before and after the therapies. The primary outcome measures include distress thermometer (DT) and posttraumatic growth, and the secondary outcome measure contains the list of distress problems.
Results:
At the post-treatment stage, the treatment group displayed a decreased score of psychological distress as compared to that in the control group, which accompanied by a higher post-traumatic growth total score and subscale scores in relationship to others, new possibilities, personal strength, spiritual changes, and appreciation of life. A significant decrease in fear, sleeping difficulty/insomnia, nervousness/anxiety, and loss of appetite was also observed in the treatment group.
Conclusion:
The results proved that the combined Naikan and Morita therapies decreased the psychological distress and improved the posttraumatic growth of the patients with AC.
Trial Registration:
ChiCTR1900026691.
Keywords: advanced cancer, distress, Morita therapy, naikan therapy, posttraumatic growth
1. Introduction
It has been reported that one-third of cancer patients encountered high levels of distress, and physical (84%) or emotional (56%) problems.[1] Advanced cancer (AC) patients experienced serious physical and psychological problems in the disease progression.[2] When approaching the end of life, these patients have to cope with not only the bodily illness, but also the spiritual crisis. Published literature demonstrated that male patients with early prostate cancer experienced deceased vitality and increased psychological distress within 12 months after the diagnosis. This trend was accelerated with the development of cancer.[3] Patients with stage IV cancer had a distress thermometer (DT) score of above 4 in compared to the patients with stage I∼III disease whose DT score was below 4.[4] Psychosocial distress is an unpleasant feeling extended from vulnerability, sadness, fear, and disabling problems in daily lives.[5] Most cancer patients undergo psychological distress and experience distressing thoughts, emotions, and worries, which could lead to other health problems. On the other hand, researchers found that individuals may exhibit positive changes also called posttraumatic growth when facing challenges or traumas,[6] which exhibit in many ways in terms of enhanced appreciation for life, improved interpersonal relationships, increased sense of personal strength, adjusted priorities, and existential and active spiritual life. Previous observation indicated that most cancer patients faced “significant adaptive challenge,” particularly after the diagnosis of cancer and at the end of treatment.[7] Even the dying process leads to the threat of mortality, AC patients also experienced posttraumatic growth if they received strong social support and prognostic awareness.[6,8] However, current literature about posttraumatic growth on cancer patients are mostly from early-stage cancer survivors. Ho et al[9] found that posttraumatic growth was negatively related to anxiety and depression levels. Liu et al[10] reported that breast cancer survivors developed posttraumatic growth at a low level after 3 months of diagnosis, which exhibited a weak negative association with psychological distress. Health care professionals tended to focus the treatments upon physical illness, but overlooked psychological problems in the AC patients, especially in overcrowded oncology wards where interventions are mainly performed for physical treatments.[11] Hedden et al[12] found that the participation of education sessions led to a significant reduction in the median DT score for male patients with newly diagnosed prostate cancer and their partners. Conventional psychological treatments can reduce distress to a certain extent, but for patients with AC, especially when they face progressive illness and approaching death, psychological problems are complex, and no simple solutions are in sight.
Naikan therapy (NT) was developed by Ishin Yoshimoto, a Japanese Jodo Shin Buddhist minister. Naikan is a Japanese word with the meaning of “inner-looking” or “introspection.”[13–15] Naikan believes that individuals are “I-centered” and thus a self-centered view guides life experiences. The key of Naikan method is to introduce a non-“I-centered” view into the people's life. Yoshimoto's own experience inspired him to explore the possibility of applying NT to everyone, not only in Buddhists. He simplified the method by eliminating the strict physical restrictions and constructing three questions for practitioners. Nowadays, NT has been adapted for use in prisons,[16] detention homes, schools and business training. As a kind of psychotherapy, Naikan method was reported to be an effective method for the treatment of mental disorder patients.[17,18] Morita therapy (MT), also named natural therapy, is a psychotherapy created by Dr Shoma Morita.[19] MT has been applied in the treatment of various mental health problems. It is a systematic psychological therapy based on Eastern philosophy.[20–22] The main purpose of MT is to help patients accept the view that unpleasant symptoms are the normal part of human emotions rather than negative things to be eliminated. Morita therapists help patients move away from preoccupation and struggle, which have been implied in interfering with the natural recovery process.[23] Previous publications[24,25] have elaborated the uniqueness and commonalities of NT and MT, proposed the theoretical basis underlying the combination of these two therapies, and further applied them in the clinical observation. The results showed that NT first evoked the patients’ positive emotions, and MT then improved behavioral initiative. The combined therapy demonstrated the advantage in integrating the emotional-behavioral complementarity. The combination of Naikan and Morita therapies is believed to be effective in promoting personality growth, enhancing trust level and tolerance, improving the capability of alexithymia, and relieving symptoms of anxiety. Therefore, the objective of this study is to explore the efficacy of the combined NT and MT on psychological distress and posttraumatic growth in patients with AC. We hypothesized that the combination of NT and MT would lower the levels of psychological distress and increase the levels of posttraumatic growth in the treatment group compared with the control group.
2. Methods/design
2.1. Study design
The study design has been constructed in consultation with clinical professionals. The trial was registered with the Chinese Clinical Trial Register (ChiCTR1900026691). This was a collaborative study between the Department of Comprehensive Therapy of Oncology, Jilin Province People's Hospital and Jilin University, China. Department of Comprehensive Therapy of Oncology in Jilin Province People's Hospital is a comprehensive department integrating medical treatment, teaching, and research. The hospital dedicates to chemotherapy, radiotherapy, cancer pain treatment, biological treatment, psychological intervention, and hospice care for patients with AC. More than 1000 patients with AC are hospitalized each year. The study subjects were approached by the staff and enrolled voluntarily.
One hundred thirty patients were randomly assigned to the control group (n = 65) for services as usual or to the treatment group (n = 65) for the same kind of services as usual as well as a combined psychological intervention for 7 consecutive weeks. Control group patients received services as usual, but without Naikan and Morita Therapies. Due to ethical and practical considerations, the control group received NT and MT (if desired) after this study.
2.2. Ethical
The trial protocol was conducted after the approval of the Institutional Review Board of Jilin Province People's Hospital, Changchun, China (Number: 2018RAN002). All participants were informed of the risks and benefits involved in this study, and signed the written consent forms.
2.3. Participants
Participants were recruited from inpatients at the Department of Comprehensive Therapy of Oncology, Jilin Province People's Hospital, China between May 2018 and July 2020.
Eligibility criteria included
-
(1)
Newly diagnosed AC patients who had received palliative radiation therapy for 6 weeks.
-
(2)
Able to understand and read Chinese, older than 20 years.
-
(3)
DT > 4, and with adequate stamina to complete the study. The adequate stamina was assessed according to the methodology reported in the paper: physician rated score of 80 on the Karnofsky performance scale.[26]
Exclusion criteria included
-
(1)
Had significant cognitive impairments assessed by the six-item Mini-Mental State Exam.[27]
-
(2)
Had physical limitations to participate.
2.4. Sample size
On the basis of effect sizes obtained from a meta-analysis that assessed the efficacy of psychological interventions for primary psychological distress,[28] the sample size was estimated at 120 patients with 60 patients per group using formula A total of 130 subjects were enrolled and analyzed to prevent the drop-out of patients. This meets the criteria for statistical analysis. A sample size of 130 in this study has 80% power to detect significant differences in score changes equal to or larger than 33% from baseline to post treatment between the treatment and the control groups (primary outcome).
2.5. Randomization
Random assignment of the patients was carried out by one of the authors (X.B.H) using a randomized block design with an average block size of 10. Ten patients who were hospitalized consecutively were classified into 1 block. In each block, 5 were randomly assigned to the treatment group and the other 5 were considered as the control group. There were 13 blocks in total. Sample demographic and clinical characteristics are presented in Table 1.
Table 1.
Patient demographic and clinical characteristics.
| Treatment | Control | |||
| Characteristic | No. (%) | No.% | χ2 | t |
| Sex | 0.14 | |||
| Male | 21 (32.30) | 23 (35.38) | ||
| Female | 44 (67.69) | 42 (64.62) | ||
| Age, yr | -0.05 | |||
| Mean | 58.04 | 58.19 | ||
| SD | 14.21 | 15.23 | ||
| Marital status | 0.14 | |||
| Currently married | 41 (63.07) | 43 (66.15) | ||
| Not currently married | 24 (36.92) | 22 (33.85) | ||
| Education | 0.03 | |||
| College degree or higher | 32 (49.23) | 31 (47.69) | ||
| Less than college degree | 33 (50.76) | 34 (52.31) | ||
| Primary cancer diagnosis | 0.5 | |||
| Breast | 25 (38.46) | 23 (35.38) | ||
| Lung | 11 (16.92) | 11 (16.92) | ||
| Colon or rectal | 19 (29.23) | 18 (27.69) | ||
| Renal | 10 (15.38) | 13 (20.00) | ||
| Stage | 0.15 | |||
| III | 45 (69.23) | 47 (72.31) | ||
| IV | 20 (30.77) | 18 (27.69) |
| Distress thermometer | Posttraumatic growth | |||||
| Characteristic of the treatment group | No. (%) | χ2 | P | No. (%) | χ2 | P |
| Sex | 0.42 | .837 | 0.174 | .677 | ||
| Male (17) | 14 (82.35) | 13 (76.47) | ||||
| Female (38) | 32 (84.21) | 27 (71.05) | ||||
| Age, years | 0.561 | .454 | 0.105 | .746 | ||
| <40 (3) | 2 (66.67) | 2 (66.67) | ||||
| 40∼50 (10) | 8 (80.00) | 7 (70.00) | ||||
| 50∼60 (30) | 26 (86.67) | 22 (73.33) | ||||
| >60 (12) | 10 (83.33) | 9 (75.00) | ||||
| Education | 0.638 | .425 | 0.248 | .619 | ||
| College degree or higher (30) | 24 (80.00) | 21 (70.00) | ||||
| Less than college degree (25) | 22 (88.00) | 19 (76.00) | ||||
| Type of cancer | 0.219 | .974 | 0.2 | .999 | ||
| Breast (23) | 19 (82.60) | 17 (73.91) | ||||
| Lung (10) | 8 (80.00) | 7 (70.00) | ||||
| Colon or rectal (15) | 13 (86.67) | 11 (73.33) | ||||
| Renal (7) | 6 (85.71) | 5 (71.43) | ||||
2.6. Blinding
This study was blinded to assessment personnel, radiation oncologists, radiation therapists, and front desk staff to reduce potential bias. Study sessions were carried out in a private room away from clinical staff. The outcome data were collected by assessment staff who were not cued to group assignment. Patients could not be blinded to their group given that this study was a behavioral intervention.
3. Intervention
The therapists have more than 10 years of clinical experience in counseling and treating cancer patients. We followed a model of training-to-criterion standard, which requests these therapists to demonstrate competence in the practical delivery of the Naikan/Morita program. The therapists were given 3 tests throughout the course of the training program. Before the start of the study, these therapists attended a series of discussion and information sharing sessions with the team of oncologists and nursing staff. Interventionists were given each patient's random assignment by one of the authors on the first study session in a sealed envelope. The sessions were conducted by the therapists assisted by nurses. The sessions were audio taped by 2 evaluators to monitor and ensure all the treatments were implemented correctly.
3.1. NT
A total of 20 sessions of NT, each of which lasted 2 hours, were conducted within 3 weeks by the therapists (n = 4) who had received NT training and have personally practiced NT.[29] One NT session consists of 15 minutes consultation with the patient, in which the outcome of the previous session was reviewed, and instructions and suggestions for the current session were given. The treatment was conducted in a selected room within the patients’ ward without any interference. Sitting in a quiet place at a relaxed posture or lying down if having serious psychological problems, the patient began to carefully introspect him/herself, and execute the introspection for 2 hours daily. Patients thought about 3 questions: What have I received from a particular person? What have I given to that person? What troubles and difficulties have I caused to that person? First, the patients were asked to examine the relationship with their parents through every period of their lives. Then, they were engaged to think about the relationship with people close to them. Interventionists continually aided the patients to shift from self-reflection toward a purpose-oriented lifestyle.
3.2. MT
MT was conducted by the trained therapists (n = 3) who are experienced in the delivery of complex psychological interventions. The MT is implemented in 3 periods: Relative bed rest period (1 week): one lecture was given to the patients about the key points of MT. Patients were on bed rest for more than 12 hours a day, keeping the mind in tranquility and learning distress tolerance. Patients were asked to write down their treatment experiences at the end of the week; Light work period (2 weeks): patients slept 7 to 8 hours every night. Light indoor activities were employed as main therapies, including listening to music, reading, calligraphy, painting, intellectual games, origami, gymnastics, cleaning, and so on. Patients were encouraged to overcome emotional vulnerability and divert attention to reality. Weekly summary reports were required in this period. Social adaptation training period (1 week): this period mainly focused on the training of social adaptation and interpersonal communication. Subgroup training was conducted on life adaptation, mutual communication, and self-analysis among patients. Patients were guided to develop future life and required to summarize the whole treatment experiences. Patients were prepared for discharge through the way of being allowed to return home on Friday and back to the hospital on Sunday.
Control group patients received standard medical care as scheduled, including drug education, balanced diet recommendations, health education about radiation therapy.
3.3. Adverse event
During the treatment sessions, the patients who exhibited doubt or emotion that could affect his participation would meet the oncology doctor for extra support and consultation.
3.4. Measurement
All recruited participants were required to complete a set of written questions, including the basic information, DT, distress problem list and the Posttraumatic Growth Inventory at pre-treatment and post-treatment (before discharge). The participants were not allowed to share their information with others. All answers and related information were analyzed by an independent investigator.
3.4.1. Primary outcome measures
DT: The scale of DT is from 0 (no distress) to 10 (extreme distress). Generally, a DT score of 4 was considered as a reasonable cut-off value. The patient having DT score of above 4 is identified as distressed patients and should be offered psychological consultation.[30–32]
Posttraumatic growth: Posttraumatic growth levels of the patients were evaluated by a Chinese version of the Posttraumatic Growth Inventory (PTGI).[9,33] The PTGI contains 5 subscales: new possibilities, relationship to others, appreciation of life, personal strength, and spiritual change. Six-point scales ranging from 0 to 5 were used and resulted in the total score ranging from 0 to 105. Scores between 60 and 66 are considered as the moderate level of Posttraumatic Growth, whereas the total scores above 66 as a high level of Posttraumatic Growth.
3.4.2. Secondary outcome measure
DT problem list: DT problem list includes 34 items in five categories: practical, family, emotional, spiritual, and physical. The participants were asked to select from a fixed yes/no format to indicate if they had any listed issues in the past week. The answers provided an overview of the problems affecting a patient's distress level.[34]
3.5. Statistical analysis
Medical statistician S. X. Liu participated in the data analysis of this study. Descriptive statistics were used to summarize the clinical characteristics of patients and the frequencies of the most common problems declared on the Problem Checklist. Comparisons of the clinical characteristics of the patients and the most common problems declared were conducted using t test and χ2 tests, respectively. Normally distributed outcome variables were evaluated using t test. Outcome variables in non-normal distribution were assessed using Wilcoxon test. Analysis of covariance (ANCOVA) mixed models were used to examine differences between the score after post-intervention and the baseline, and adjust the baseline value of each outcome variable. The intention-to-treat (ITT) principle was undertaken in 2 time-point measurements. All statistical tests were 2-tailed, and a P value < .05 was considered to be statistically significant. Statistical analyses were performed using IBM SPSS Statistics and SAS 9.2.
4. Results
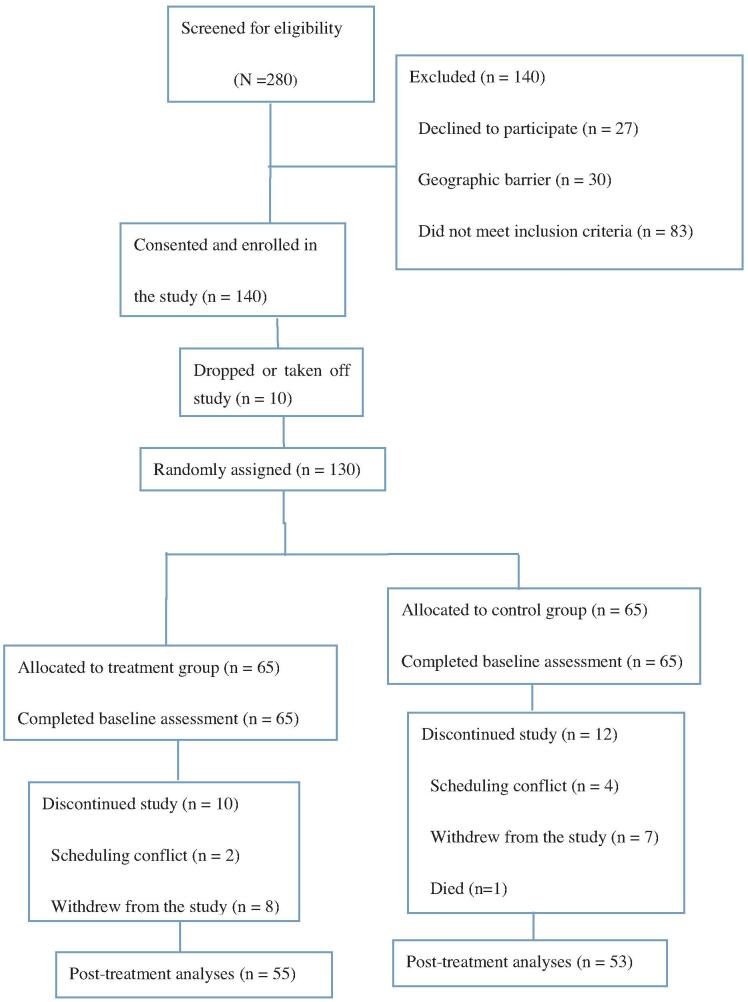
In this study, 280 eligible patients were approached and 140 patients consented to participate. The final sample size of 130 participated in the study after the dropout of 10 patients. Two participants in the treatment group did not attend any sessions due to scheduling conflicts; six participants withdrew because of the lack of interest and two individuals withdrew with unknown reason (Fig. 1). In the control group, 12 subjects had not finished the whole study (Fig. 1).
Figure 1.
CONSORT flow diagram.
There were no differences between control and treatment groups in the number of patients who lost the follow-up or did not attend study sessions. There was no statistically significant difference between patients with and without missing data regarding medical and baseline outcome results. Moreover, the 2 groups did not differ in demographic and clinical characteristics at pre-treatment (Table 1). We also compared the effects of the therapies among subjects based on sex, age, education status, and cancer type, and no differences were observed (Table 1).
4.1. DT
The score of psychological distress in the treatment group decreased significantly when compared to that in the control group with a statistically significant difference (P < .001) at the post-treatment stage (see Table 2 and Table S1, Supplemental Digital Content, which analyzed DT using ANCOVA). However, no differences (P > .05) were found in the psychological distress of participants between the treatment group and the control group at the pre-treatment stage.
Table 2.
Comparison of the score of the distress thermometer.
| The distress thermometer | The distress thermometer | ||||
| Pretreatment | treatment | control | Posttreatment | treatment | control |
| Median (IQR) | 4 (1) | 5 (2) | Median (IQR) | 2 (1) | 5 (2) |
| Mean (SD) | 4.62 (1.36) | 4.91 (1.38) | Mean (SD) | 2.42 (1.03) | 4.81 (1.43) |
| Wilcoxon test | P < .001 | ||||
| ANCOVA | P∗ < .001 | ||||
4.2. PTGI
The post-traumatic growth total score in the treatment group and the scores in the subscales, including relationship to others, new possibilities, personal strength, spiritual changes, and appreciation of life, were higher than those of the control group at the post-treatment stage with a statistical significance (P < .001), but no statistically significant difference (P > .05) at pre-treatment stage (see Table 3 and Table S2, Supplemental Digital Content, which evaluated posttraumatic growth using ANCOVA).
Table 3.
Comparison of the score of the posttraumatic growth.
| OVERALL | Pretreatment | treatment | control | Posttreatment | treatment | control |
| median (IQR) | 43 (7) | 41 (8) | median (IQR) | 74 (8) | 45 (7) | |
| Wilcoxon test | W = 1432 | P < .001 | ||||
| ANCOVA | P∗ < .001 | |||||
| Relating to other | Pretreatment | treatment | control | Posttreatment | treatment | control |
| median (IQR) | 16 (6) | 16 (6) | median (IQR) | 27 (4) | 17 (6) | |
| Wilcoxon test | W = 1468 | P < .001 | ||||
| ANCOVA | P∗ < .001 | |||||
| New possibilities | Pretreatment | treatment | control | Posttreatment | treatment | control |
| median (IQR) | 11 (4) | 11 (4) | median (IQR) | 18 (3) | 11 (4) | |
| Wilcoxon test | W = 1783.5 | P < .001 | ||||
| ANCOVA | P∗ < .001 | |||||
| Personal strength | Pretreatment | treatment | control | Posttreatment | treatment | control |
| median (IQR) | 6 (4) | 6 (4) | median (IQR) | 14 (5) | 7 (4) | |
| Wilcoxon test | W = 1711 | P < .001 | ||||
| ANCOVA | P∗ < .001 | |||||
| Spiritual changes | Pretreatment | treatment | control | Posttreatment | treatment | control |
| median (IQR) | 4 (1) | 4 (3) | median (IQR) | 6 (2) | 4 (2) | |
| Wilcoxon test | W = 1985 | P < .001 | ||||
| ANCOVA | P∗ < .001 | |||||
| Appreciation of life | Pretreatment | treatment | control | Posttreatment | treatment | control |
| median (IQR) | 6 (4) | 5 (3) | median (IQR) | 10 (4) | 6 (2) | |
| Wilcoxon test | W = 1581.5 | P < .001 | ||||
| ANCOVA | P∗ < .001 |
4.3. DT problem list
The comparison of the frequencies of the 10 most common problems endorsed is summarized in Table 4. The most common problems were classified into the following domains: emotional (2/10), physical (7/10), and practical (1/10). Chi-square test revealed that the treatment group showed significant decreases (P < .05) in fear, sleeping difficulty/insomnia, nervousness/anxiety and loss of appetite compared with the control group at the post-treatment stage. There were no significant differences between the 2 groups in reducing memory decline, fatigue, pain, insurance /financial problems, nausea/vomiting, and tingling hands/feet. No statistically significant difference (P > .05) was observed between the treatment group and the control group at the pre-treatment stage as well (Table 4).
Table 4.
Comparison of the frequencies of the 10 most common problems endorsed.
| Pre-treatment | Post-treatment | ||||||
| Treatment (65) | Control (65) | Treatment (55) | Control (53) | ||||
| Variable | No. (%) | No. (%) | χ2 | No. (%) | No. (%) | χ2 | P |
| Fears | 48 (73.85) | 46 (70.77) | 0.154 | 30 (54.55) | 40 (75.47) | 5.183 | .023 |
| Sleep/insomnia | 44 (67.69) | 45 (69.30) | 0.036 | 21 (38.18) | 39 (73.58) | 13.701 | .000 |
| Memory decline | 35 (53.85) | 33 (50.77) | 0.123 | 29 (52.73) | 28 (52.83) | 0.000 | .988 |
| Nervous, anxiety | 34 (52.31) | 35 (53.85) | 0.031 | 17 (30.91) | 27 (50.94) | 4.487 | .034 |
| Fatigue | 46 (70.77) | 41 (63.08) | 0.869 | 39 (70.91) | 42 (79.25) | 1.000 | .317 |
| Pain | 38 (58.46) | 37 (56.92) | 0.032 | 41 (74.55) | 36 (67.92) | 0.578 | .447 |
| Insurance/financial | 39 (60.00) | 41 (63.08) | 0.130 | 42 (76.36) | 38 (70.70) | 0.306 | .580 |
| Loss of appetite | 31 (47.69) | 33 (50.77) | 0.123 | 15 (27.27) | 30 (56.60) | 9.554 | .002 |
| Nausea/vomiting | 29 (44.62) | 26 (40.00) | 0.284 | 28 (50.91) | 25 (47.17) | 0.151 | .698 |
| Tingling hands/feet | 26 (40.00) | 25 (38.46) | 0.032 | 28 (50.91) | 24 (45.28) | 0.342 | .559 |
In this study, not all patients in the treatment group completely implemented their therapies. The participants were considered to adhere to the therapies if they completed the recommended treatment (20 NT sessions of 2 hours duration per session; 4 weeks of MT). Patients in the treatment group reported 91% adherence for NT, and 89% adherence for MT. Nevertheless, we are unable to evaluate the implementation fidelity of these therapies, as it is hard to define the effectiveness of cognitive and behavioral interventions only based on the treatment frequency and duration obtained from participants’ introspective reports and direct observation. No adverse events were reported.
5. Discussion
Clinical interventions have the potential to improve the quality of life in patients approaching the end of life. However, interventions for AC patients have been seldom developed, and those developed interventions have rarely focused on psychological distress and assessed these problems as primary outcomes. Because of this situation, we used a combined intervention, including NT and MT derived from the published literature on the respective effects of NT[16,29,35,36] and MT.[37–39] The present study showed the significant benefits of the combination of NT and MT in AC patients as compared with the control group, particularly in decreasing psychological distress. Our study also demonstrated that patients receiving the combination of NT and MT exhibited significant improvement when compared with those only receiving standard medical care. The patients in the control group did not show any improvement in overall distress levels at the post-treatment assessment. Thus, it is necessary to promote the combination of Naikan and Morita therapies as a palliative approach to improving the psychological state in end-of-life patients.
Four (fear, sleeping difficulty/insomnia, nervousness/anxiety, and loss of appetite) of the 10 most common problems endorsed decreased significantly in the treatment group compared with those in the control group. This could be due to a sense of relief from the reduced difficulties and symptom burden, or the feeling empowered by the improved functioning and quality of life.[40] The results are especially important for the patients with AC, as their stresses are usually aggravated over time due to painful symptoms, physical functioning deterioration and death awareness. This result suggests the importance of NT and MT in providing psychological relief in patients. AC patients are a unique group of people for the study of posttraumatic growth because the patients suffer a life-threatening disease and thus face high levels of stress after diagnosis. However, posttraumatic growth in people with AC has yet to be studied satisfactorily. Our results indicated a favorable effect of NT and MT on AC patients, which included a significantly improved level of posttraumatic growth. This improvement was mainly manifested in five aspects: enhancing relationships with others, discovering new possibilities, increasing the appreciation of life, recognizing their personal strengths, and promoting spiritual changes. NT and MT decreased the patients’ psychological distress and further promoted positive changes in the patients. Published research had indicated a positive living style correlated to posttraumatic growth.[6] NT and MT could promote patients’ positive life attitudes and change their mental states effectively. NT and MT appear to be effective in promoting a better emotional adjustment in newly diagnosed AC patients. This study provides evidence on the efficacy of the combined intervention on posttraumatic growth of patients with AC in the psychosocial adjustment.
To the best of our knowledge, this study is the first to explore the effects of combined NT and MT on the psychological distress and posttraumatic growth in AC patients during the course of palliative radiation therapy. We carried out the randomized controlled study to evaluate the influence of the psychological intervention on managing posttraumatic growth. The randomized clinical trial study completely disentangles the complexity of the factors that contributed to the before-and-after therapy results.[41] In order to assure the feasibility of the study and reduce the attrition at the same time, the intervention period for both groups was set to 7 weeks in the hospital.
There are 2 potential limitations to this study. First, due to the small sample size, the results should be considered preliminary. Second, the psychological states of patients before the AC diagnosis were not accessed, which is a factor that may be associated with the post-cancer treatments. Despite of the limitations in the present study, our results indicate that the combination of NT and MT is an efficacious intervention in reducing psychological distress and improving posttraumatic growth in patients with AC.
Author contributions
XB conceptualized the study, conducted patient interviews, performed qualitative analysis, wrote the original draft version, and edited subsequent versions. YQ contributed to patient interviews, data collection, and reviewed and edited draft version. JJ approved the conceptualization, supervised data collection, and analysis. YT supervised data collection and reviewed and edited draft version. SX conducted the statistical analysis and reviewed and edited draft versions. LJ contributed to the conception and design of the trial, analysis, and interpretation of data. FL approved the conceptualization, supervised data collection and analysis, and reviewed and edited draft and subsequent versions. All authors approved the final version.
Conceptualization: Xiang-Bei Han, Li-jing Zhao, Feng Li.
Data curation: Yan-Qiu Fang, Shu-Xiang Liu, Jun-jie Hou, Li-jing Zhao.
Formal analysis: Shu-Xiang Liu, Feng Li.
Supervision: Yan Tan, Feng Li.
Visualization: Jun-jie Hou, Feng Li.
Writing – original draft: Xiang-Bei Han, Jun-jie Hou, Li-jing Zhao.
Writing – review & editing: Xiang-Bei Han, Yan-Qiu Fang, Yan Tan, Li-jing Zhao, Feng Li.
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: AC = Advanced Cancer, DT = Distress Thermometer, MT = Morita Therapy, NT = Naikan Therapy, PTGI = Posttraumatic Growth Inventory.
How to cite this article: Han XB, Fang YQ, Liu SX, Tan Y, Hou JJ, Zhao LJ, Li F. Efficacy of combined naikan and morita therapies on psychological distress and posttraumatic growth in Chinese patients with advanced cancer: A randomized controlled trial. Medicine. 2021;100:30(e26701).
This work was supported by the Research Foundation of Jilin Provincial Science & Technology Development (20160622008JC).
The work is in compliance with ethical standards. All participants provided written informed consent after having been fully informed about the study aims.
The authors declare that they have no conflict of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
SD = standard deviation.
ANCOVA = analysis of covariance, IQR = interquartile range, SD = standard deviation.
ANCOVA = analysis of covariance, IQR = interquartile range, SD = standard deviation.
References
- [1].Hollingworth W, Metcalfe C, Mancero S, et al. Are needs assessments cost effective in reducing distress among patients with cancer? A randomized controlled trial using the Distress Thermometer and Problem List. J Clin Oncol 2013;31:3631–8. [DOI] [PubMed] [Google Scholar]
- [2].Rosenberg HJ, Rosenberg SD, Ernstoff MS, et al. Expressive disclosure and health outcomes in a prostate cancer population. Int J Psychiatry Med 2002;32:37–53. [DOI] [PubMed] [Google Scholar]
- [3].Couper JW, Love AW, Duchesne GM, et al. Predictors of psychosocial distress 12 months after diagnosis with early and advanced prostate cancer. MJA 2010;193:S58–61. [DOI] [PubMed] [Google Scholar]
- [4].Huang B, Chen H, Deng Y, et al. Diagnosis, disease stage, and distress of Chinese cancer patients. Ann Transl Med 2016;4:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].American Cancer Society & National Comprehensive Cancer Network. Distress Treatment guidelines for patients VersionII /July2005. Available at: http://www.nccn.org/patients_gls/_english/distres/contents.aps. Accessed January 12, 2017. [Google Scholar]
- [6].Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq 2004;15:01–18. [Google Scholar]
- [7].Morris BA, Shakespeare-Finch J, Scott JL. Posttraumatic growth after cancer:the importance of health-related benefits and new found compassion for others. Care Cancer 2012;20:749–56. [DOI] [PubMed] [Google Scholar]
- [8].Janoff-Bulman R. Posttraumatic growth: three explanatory models. Psychol Inq 2004;15:30–4. [Google Scholar]
- [9].Ho SM, Chan CL, Ho RT. Posttraumatic growth in Chinese cancer survivors. Psychooncology 2004;13:377–89. [DOI] [PubMed] [Google Scholar]
- [10].Liu JE, Wang HY, Wang ML, et al. Posttraumatic growth and psychological distress in Chinese early-stage breast cancer survivors: a longitudinal study. Psychooncology 2014;23:437–43. [DOI] [PubMed] [Google Scholar]
- [11].Madden J. Use of the Distress Thermometer as a means of effectively assessing emotional distress in patients with cancer. Oncol Nurs Forum 2006;33:484–5. [Google Scholar]
- [12].Hedden L, Wassersug R, Mahovlich S, et al. Evaluating an educational intervention to alleviate distress amongst men with newly diagnosed prostate cancer and their partners. BJU Int 2017;120:E21–9. [DOI] [PubMed] [Google Scholar]
- [13].Yoshimoto I. Naikan no Michi [The way of Naikan]. Nara, Japan: Naikan Kenshusho; 1981. [Google Scholar]
- [14].Yoshimoto I. Shinzen Shingo: Watashi no Naikan Taiken [Before and after faith: My Naikan experience]. Nara, Japan: Naikan Ken-shusho; 1985. [Google Scholar]
- [15].Yoshimoto I. Naikan ho [The Naikan method]. Tokyo, Japan: Shunjusha; 1997. [Google Scholar]
- [16].Ding X, Liu Z, Cao G, et al. The efficacy of Naikan therapy on male offenders: changes in perceived social support and externalized blame. Int J Offender Ther Comp Criminol 2018;62:3499–508. [DOI] [PubMed] [Google Scholar]
- [17].Reynolds D. The Quiet Therapies: Japanese Pathways to Personal Growth. Honolulu: The University Press of Hawaii; 1981. [Google Scholar]
- [18].Morita M, Kondō A, LeVine P. Morita Therapy and the True Nature of Anxiety-Based Disorders. Albany: State University of New York Press; 1998. [Google Scholar]
- [19].Kitanishi K, Mori A. Morita therapy: 1919 to 1995. Psychiatry Clin Neurosci 1995;49:245–54. [DOI] [PubMed] [Google Scholar]
- [20].Suzuki T, Suzuki R. The effectiveness of in-patient Morita therapy. PsychiatrQ 1981;53:201–13. [DOI] [PubMed] [Google Scholar]
- [21].Miura M, Usa S. A psychotherapy of neurosis: Morita therapy. Yonago Acta Med 1970;14:01–17. [PubMed] [Google Scholar]
- [22].Koru T. Morita therapy. Int J Psychiatry 1965;1:611–45. [PubMed] [Google Scholar]
- [23].Nakamura K, Kitanishi K, Maruyama S, et al. Guidelines for Practising Outpatient Morita Therapy. Tokyo: Japanese Society for Morita Therapy; 2010. [Google Scholar]
- [24].Zhang QF, Lu YZ. Application of combination of Naikan and Morita therapies in theory and practice of neuroses. Med J Chin People Health 2014;26:92–3. [Google Scholar]
- [25].Zhang QF, Yuan YT, Ren QT, Lu YZ. A randomized single-blind controlled trial of combination of Naikan and Morita therapy (NMT) in patients with generalized anxiety. Chin Mental Health J 2014;28:651–6. [Google Scholar]
- [26].Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer 1980;45:2220–4. [DOI] [PubMed] [Google Scholar]
- [27].Callahan CM, Unverzagt FW, Hui SL, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002;40:771–81. [DOI] [PubMed] [Google Scholar]
- [28].Wang CW, Chow AY, Chan CL. The effects of life review interventions on spiritual well-being, psychological distress, and quality of life in patients with terminal or advanced cancer: a systematic review and meta-analysis of randomized controlled trials. Palliat Med 2017;31:883–94. [DOI] [PubMed] [Google Scholar]
- [29].Zhang H, Li C, Zhao L, Zhan G. Single-blind, randomized controlled trial of effectiveness of Naikan therapy as an adjunctive treatment for schizophrenia over a one-year follow-up period. Shanghai Arch Psychiatry 2015;27:220–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Akizuki N, Akechi T, Nakanishi T, et al. Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer 2003;97:2605–13. [DOI] [PubMed] [Google Scholar]
- [31].Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychological distress in ambulatory cancer patients. Cancer 2005;103:1494–502. [DOI] [PubMed] [Google Scholar]
- [32].Giovanna F, Francesco B, Maria GM, et al. Impact of a psycho-oncological rehabilitation intervention on psychological distress: the experience of CeRiOn (Oncological Rehabilitation Centre) Florence 2007–2010. Support Care Cancer 2013;21:2381–6. [DOI] [PubMed] [Google Scholar]
- [33].Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 1996;9:455–71. [DOI] [PubMed] [Google Scholar]
- [34].Larouche S, Edgar L. The measure of distress: a practical thermometer for outpatient screening. Oncol Exchange 2004;3:34–9. [Google Scholar]
- [35].Sengoku M, Murata H, Kawahara T, et al. Does daily Naikan therapy maintain the efficacy of intensive Naikan therapy against depression? Psychiatry Clin Neurosci 2010;64:44–51. [DOI] [PubMed] [Google Scholar]
- [36].Ozawa-de Silva C. Mindfulness of the kindness of others: the contemplative practice of Naikan in cultural context. Transcult Psychiatry 2015;52:524–42. [DOI] [PubMed] [Google Scholar]
- [37].Sugg HV, Richards DA, Frost J. Morita therapy for depression and anxiety (Morita Trial): study protocol for a pilot randomised controlled trial. Trials 2016;17:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Gomibuchi T, Gomibuchi K, Akiyama T, et al. Obsession of hearing music: from the viewpoint of Morita theory. Psychiatry Clin Neurosci 2000;54:203–6. [DOI] [PubMed] [Google Scholar]
- [39].Sugg HVR, Richards DA, Frost J. Optimising the acceptability and feasibility of novel complex interventions: an iterative, person-based approach to developing the UK Morita therapy outpatient protocol. Pilot Feasibility Stud 2017;3:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Eades M, Murphy J, Carney S, et al. Effect of an interdisciplinary rehabilitation program on quality of life in patients with head and neck cancer: review of clinical experience. Head Neck 2013;35:343–9. [DOI] [PubMed] [Google Scholar]
- [41].Fors EA, Bertheussen GF, Thune I, et al. Psychosocial interventions as part of breast cancer rehabilitation programs? Results from a systematic review. Psychooncology 2011;20:909–18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.