Abstract
Aim:
This study aimed to assess the outcome of community-based nutritional counseling interventions on eating habits of rural-dwelling children.
Methods:
A group-randomized trial design was used in this study. A total of 108 rural-dwelling children from a community in the Enugu North agricultural zone, Enugu State, who participated in the study. The children were randomly assigned to 2 groups: the treatment group (n = 54) and the no-treatment control group (n = 54). The child eating behavior questionnaire was used for data collection. Parents of the participating children within each study group completed the child eating behavior questionnaire at 3 time points. The data collected were analyzed using an independent sample t test at a probability level of .05.
Result:
The outcome of the study showed that the children's eating habits in the treatment group improved positively following the community-based nutritional counseling intervention. The positive gain from exposure to the community-based nutritional counseling intervention program was sustained during follow-up for children in the treatment group compared with the no-treatment group.
Conclusion:
The community-based nutrition counseling intervention carried out among children in rural communities had a positive adjustment in children's eating habits. The intervention requires the constant collaboration of professional childhood educators, caregivers, home economists, school staff, healthcare specialists, families, and the children themselves. Furthermore, there is a need for future long-term evaluations of the effects of community-based nutritional counseling interventions on children's nutrition and eating habits.
Keywords: eating habits, malnutrition, nutritional counseling
1. Introduction
A proper eating habit, which is an index of a proper lifestyle, is considered the basis for good health status. Therefore, proper eating should be encouraged for the appropriate physical and mental development of everyone, including those within rural communities.[1] Although eating habit is a multidimensional phenomenon, it talks about what and how people eat, their choice of food items, and how they get their food.[2] Eating habit is influenced by 2 major factors, including biological factors that have to do with internal (genetic) influence, and psychosocial factors that deal with external or environmental influence.[3] To achieve a healthy body condition, one needs to regularly consume a balanced diet that meets the nutritional requirements of such a person. However, this has been lacking in most rural communities, especially in developing countries.
In developing countries, the prevalence of malnutrition due to poor eating habits remains high. Consequently, in 2013, 51 million children were at least moderately wasted at a global prevalence of nearly 8% globally, while 17 million had severe wasting at a global prevalence of almost 3% in Asia and Africa, with prevalence rates of 71% and 28%, respectively. More than a quarter of children below 5 years of age globally (nearly 161 million) were considered stunted, with Southern Asia and Africa having the highest prevalence rates of 56% and 36% respectively.[4] The Nigeria Demographic and Health Survey in 2013 reported that 37% of children in Nigeria were considered stunted, 21% were severely stunted, 18% were wasted, 9% were considered severely wasted, 29% were underweight, and 12% were seen as severely underweight with a higher prevalence in rural communities.[5] Previous studies have reported related findings.[6–9] This has attracted the attention of researchers in the relevant fields.
Researchers have employed different novel methods to improve eating behavior among a wide range of client populations. Several studies[10–12] have deemed mindfulness-based eating awareness training (MB-EAT) to be of medium effect size in improving eating habits among different populations, mostly undergraduates. Using a 2 × 2 factorial between-subjects design, van Koningsbruggen et al[13] compared the effects of dieting implementation intentions and a stop-signal treatment on poor eating behavior among 88 participants whose mean age was 21.17 and found both to be of small effect size in reducing poor eating behavior although the later was of smaller effect size. Attention bias modification intervention and food-specific inhibition training have also been tried to reduce unhealthy food intake among different client populations, with both yielding a medium effect size of.[14]
Notwithstanding the numerous efforts in trying to improve eating habits, the Joint FAO and WHO expert committee on food additives in 2017 noted that <50% of children and adolescents in rural communities globally meet the dietary recommendations for any food group.[15] Earlier attempts to correct eating habits have suffered a lack of active comparison clinical intervention or control groups that would make available foundations for initiating stronger assumptions, unknown variations among participants in various trials, use of a wide scope of interventions that differ in duration, deficient sample sizes and heterogeneity in control conditions, and even possible restrictions in statistical power. Therefore, the current study adopted a randomized control trial that sought to improve eating habits among children in rural households in selected communities in the Enugu North agricultural zone in South-Eastern Nigeria, using a community-based nutritional counseling intervention.
1.1. Hypothesis
In this study, it is hypothesized that the gain from exposure to the community-based nutritional counseling intervention program would improve eating habits among children in rural households, and such improvements will be maintained at follow-up for children in the intervention group as compared with those in the no-intervention group.
1.2. Objective
The current study aims to understand the effect of community-based nutritional counseling interventions on the eating habits of rural households.
2. Materials and methods
2.1. Ethical consideration
This study adhered to the ethical standards of research at the Faculty of Education, University of Nigeria, Nsukka. Moreover, the study followed the ethical principles of Helsinki, enshrined in the World Medical Association Declaration.[16] Participants were notified that they were at liberty to pull out of the study at will.
2.2. Study design
The study followed a group-randomized controlled design.
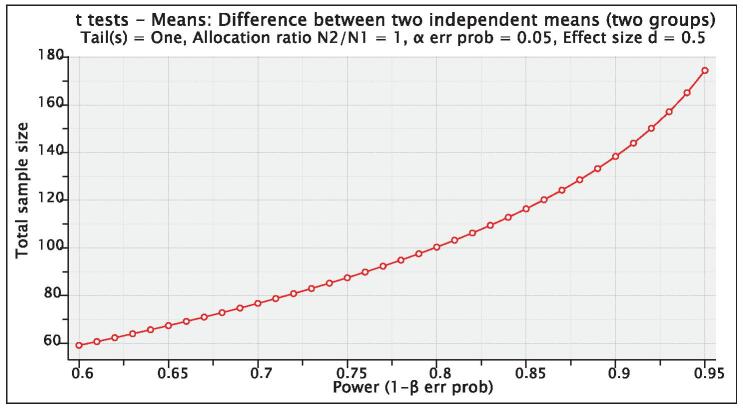
2.3. Sample size calculation
A sample size of 108 is shown to be adequate for a study of this kind with a chosen statistical power of 0.82 at an alpha level of 0.05 and a statistical effect size of 0.5 for 2 independent t tests analysis as determined using G∗Power 3.1.9.4 software (Uiversität Kiel, Germany).[17,18]
2.4. Study setting
The study was conducted in Enugu State in South-Eastern Nigeria. Enugu State is characterized by 2 major seasons in a year: the rainy season, with an average annual rainfall of 1600 to 2000 mm that takes off from April or May and the dry season. The temperature ranges from 21 to 35 °C while the vegetation is described as derived savannah. The soil type varies from sandy, sandy loam, loam, and clay loam to pure clay.
2.5. Participants
The study participants were pupils in upper basic classes from a community within the state. The researchers were able to access 320 pupils for eligibility. Only 108 pupils out of the 320 pupils whose parents completed the inclusion requirements finally participated in the study. The participants consisted of 64 (59.26%) female and 44 (40.74%) male pupils. Pupils’ demographic features such as sex, age, ethnicity (Igbo, House, Yoruba), mother's level of education (Certificate of basic education or less [up to age 15 years]; general/vocational secondary education [15–18 years]; University/Polytechnic degree [>18 years]), parents’ relationship status (both parents alive and living together, both parents alive but separated, one of the parents alive, neither of the parents alive) were collected (Table 1).
Table 1.
Demographic statistics.
| Pupils demographic features | Percentage % | Number |
| Gender | ||
| Male | 59.26% | 64 |
| Female | 40.74% | 44 |
| Age | ||
| 5–8 years | 67.59% | 73 |
| 9–12 years | 32.40% | 35 |
| Ethnicity | ||
| Igbo | 90.74% | 98 |
| Yoruba | 5.55% | 6 |
| House | 4.370% | 4 |
| Mother's level of education | ||
| No formal education | 52.77% | 57 |
| Certificate of basic education or less (up to age 15 years) | 26.85% | 29 |
| General/vocational secondary education (15–18 years) | 13.88% | 15 |
| University/Polytechnic degree (>18 years) | 7 | |
| Parents relationship status | ||
| Both parents alive and living together | 81.48% | 88 |
| Both parents alive but separated | 6.48% | 7 |
| One of the parents alive | 9.25% | 10 |
| Neither of the parents alive | 2.77% | 3 |
2.6. Outcome measure
2.6.1. Child eating behavior questionnaire (CEBQ)[21]
The CEBQ was designed to evaluate different aspects of children's appetites. The CEBQ was used at Times 1, 2, and 3 for data collection. The CEBQ has 35 items with 8 subscales: Satiety responsiveness (5 items), Emotional over-eating (4 items), Desire to drink (3 items), Food responsiveness (5 items), Enjoyment of food (4 items), Food fussiness (6), Emotional under-eating (4 items), Slowness in eating (4 items), rated on a 5-point Likert scale ranging from never (0) to always (4). The validity of the CEBQ in measuring eating styles in children has been shown to have a Cronbach α of 0·72 to 0·91, and test-retest reliability (r) of 0·52 to 0·87.[20,21] The internal consistency (Cronbach α) of the CEBQ based on this study sample was 0.82.
2.7. Inclusion/exclusion criteria
The inclusion criteria included pupils with poor eating habits according to the parent's response to the CEBQ, completing the informed consent in writing by parents of participating pupils, and being a member of the community where the research was carried out. The exclusion criteria were having no eating problems according to anecdotal records as indicated by their parents in the CEBQ, parents’ disapproval to allow their wards to participate even though they had a poor eating habit, not being a member of the community where the research was conducted, and are currently enrolled in an eating habit management intervention.
2.8. Intervention procedure
First, the researchers requested authorization of the management of the chosen school. Having ascertained this permission, the researchers through the school management invited parents to the school for a 2-hour orientation lecture during which parents were educated about eating disorders, and the dangers associated with poor eating habits in children. This was done for parents to see the need to allow their children to participate in the community-based nutritional counseling intervention already approved by the school. The meeting was attended by 320 parents of 320 children. After the lecture, informed consent forms were shared among the parents, out of which 108 parents of 108 children consented. Subsequently, 108 children were further assessed for other eligibility criteria. To determine eating disorders in children, the CEBQ was shared among the 108 parents who completed it with the help of the child's teacher to collect baseline data (Time 1). The intensity of the eating problem of the children was ascertained by summing up their eating habits, which were provided by their parents who observed their eating behavior at home. We set the eating disorder cut-off to 50%. After collecting the CEBQ from the parents, we found that 108 children fell above the eating disorder cut-off, representing a prevalence rate of 33.75%. The 108 children met all other eligibility criteria and, therefore, formed the study sample. The children were notified of their liberty to pull out of the study at will.
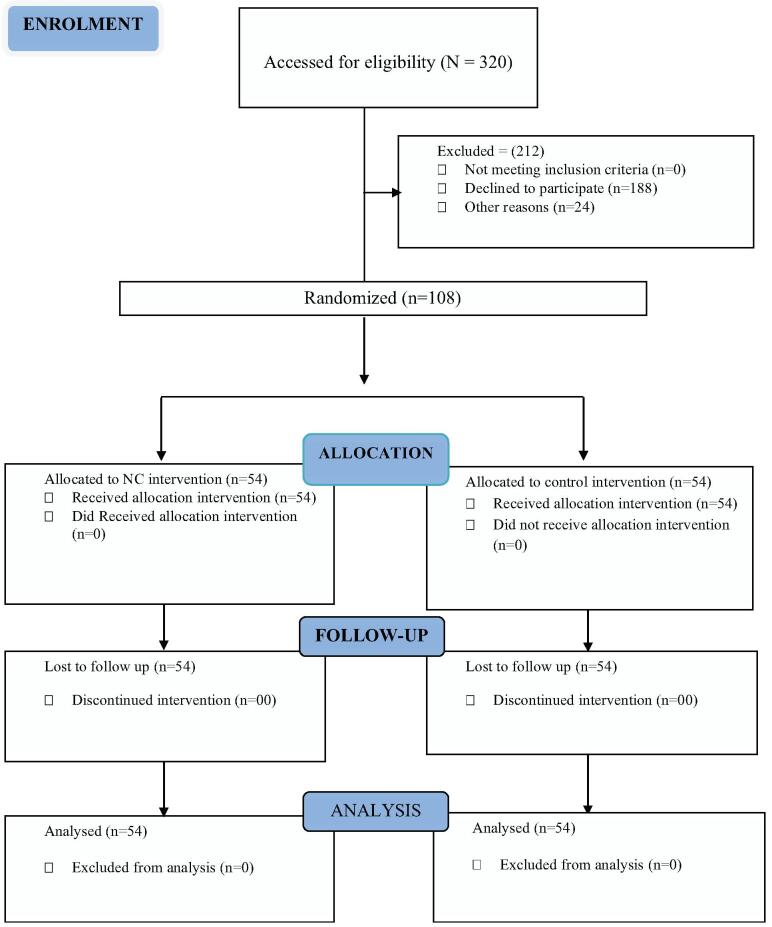
Simple randomization of participants (108 children) into 2 groups (intervention group [n = 54] and no-intervention group [n = 54]) was carried out using random allocation software[22] in order to avoid bias in allocation (see Fig. 1). The 10 weeks community-based nutrition counseling intervention was followed. At the end of the last session, the CEBQ was used to collect the post-test data. After 3 months, 4 follow-up sessions were conducted over 8 weeks (twice per week), after which data were collected using the CEBQ. The intervention was delivered at the community square using the nutritional counseling manual by 4 research assistants who were experts in counseling, childhood education, nutrition, and dietetics after receiving a 3 weeks orientation from the researchers concerning child education as well as the rudiments of the study. The nutritional counseling manual was developed by professors in counseling, childhood education, nutrition, and dietetics. The intervention lasted for 10 weeks, from September 2019 to December 2019. The intervention consisted of 20 nutrition counseling sessions held for 10 weeks and a 4-week follow-up. Each session lasted for 35 minutes and was closed with instructions about an exercise for the next session. The questions were also entertained. During the last treatment session, the CEBQ was given to the parents of participants to gather post-intervention data (Time 2). After 3 months, 4 follow-up sessions were conducted over 4 weeks (twice per week). At the last follow-up session, the CEBQ was also given to the parents of participants to gather follow-up data (Time 3). No dropouts were recorded. Additional sessions were offered to the pupils if they missed any session.
Figure 1.
Graphical presentation of sample size. This legend shows the results of the sample size determination based on a statistical power.
2.9. Intervention package
We developed and used a community-based nutrition counseling intervention to help children in rural communities with eating disorders. During the first session of the study, the pupils understood the objective and procedure of the intervention after the welcome note, which was done using the rapport building technique. In the second week of the intervention, a pretest assessment was performed to collect the pretest data. During the third week, the concept of nutritional counseling was treated using direct teaching and psycho-education techniques to acquaint the children with the concept. After this, the pupils understood the concept of nutritional counseling. In addition, through direct teaching skills and psycho-education techniques, the children were made to understand the concept of eating habits, which was the topic of the fourth week. The fifth week saw the children through a series of cognitive restructuring lessons to change the children's negative beliefs concerning some foods, especially fruits and vegetables. At the end of the lessons, the children were able to make independent decisions in choosing better foods that included more fruits and vegetables at the expense of more sugary and fad diets. The same objective was repeated in the sixth week. In this study, 18 eat-well cards were used to expose the children to different kinds of food combinations that could result in a more balanced diet. At the end of the week, the children were able to make better decisions concerning their diets by rightfully combining different foods using the cards to form different well-balanced diets. The topic of the seventh week was healthy eating. The exposure therapy technique was utilized to expose children to healthy eating situations. Practically, the children were shown pictures and videos of their highly cherished models. At the end of the session, the children were able to cope with their fears and phobias about some kind of food by choosing properly balanced diets in order to look like their models. Using the open dialog technique, the children were helped to understand the negative impacts of bad eating habits in the eighth week. In this way, the children were able to understand and identify the negative effects of bad eating habits and why bad habits should be avoided. In the ninth and tenth week, the children were helped to identify, dispute, and counter the beliefs that influenced their choice of poor diet. At the end of the session, pupils were able to counter their unhealthy beliefs that influenced their choice of poor diet by reenacting the fact that their role models do not eat such foods and hence look wonderful (Fig. 2).
Figure 2.
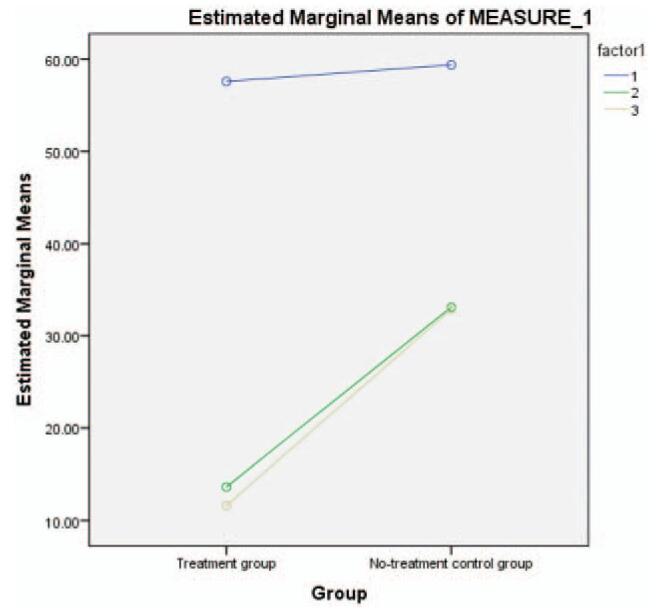
Graphical presentation. This legend shows the effect of intervention on children's eating habits.
2.10. Data analyses approach
A blinding technique was adopted by de-identifying some parts of the questionnaire to ensure that the data analyst was not biased. Repeated-measures analysis of variance (ANOVA) was used to show the effect of community-based nutritional counseling interventions on children's eating habits. Data normality and violations of the assumptions were tested. Normal distribution of data was performed while meeting the statistical assumptions. Missing data were also analyzed. All data were statistically analyzed using the IBM SPSS version 23. Results were considered significant at P ≤ .05.
Table 2 shows no significant results at the pre-treatment stage, F (1,101) = 0.670, P = .415, = 0.007, R2 = 0.003. The results further showed that children's eating habits in the treatment group improved positively following the nutritional counseling intervention, F (1,101) = 65.593, P = .000, = 0.455, R2 = 0.444. This result supported the hypothesis that nutritional counseling intervention could lead to a significant improvement in eating habits among children in rural communities in the treatment group.
Table 2.
Repeated-measures ANOVA showing the effect of community-based nutritional counseling intervention on children's eating habits.
| Time | Measures | Group | Mean (SD) | F | Sig. | R2 | 95% | |
| Pre-treatment | CEBQ | Treatment Control | 57.59 (1.20) 59.39 (2.44) | 0.670 | 0.415 | .007 | .003 | 54.11–61.06 56.59–62.19 |
| Post-treatment | CEBQ | Treatment Control | 13.63 (2.22) 33.11 (4.12) | 65.503 | .000 | .455 | .444 | 12.16–15.09 28.67–37.55 |
| Follow-up | CEBQ | Treatment Control | 11.61 (2.11) 32.86 (1.26) | 73.42 | .000 | .517 | .507 | 9.79–13.43 28.38–37.34 |
The results also showed that the positive gain from exposure to the nutritional counseling intervention program was sustained at follow-up for pupils in the treatment group compared with the no-treatment group, F (1,101) = 73.42, P = .000, = 0.517, R2 = 0.507. This result supported our hypothesis that the gain from exposure to the nutritional counseling intervention program would be maintained at follow-up for pupils in the treatment group compared with those in the no-treatment group (Fig. 3).
Figure 3.
Flow diagram. This legend shows the distribution of participants in the treatment and control groups.
3. Discussion
This study tested the hypothesis that nutritional counseling intervention could lead to a significant improvement in eating habits among children in rural communities in the treatment group, as indicated by scores on the CEBQ. Parallel with the results of[23,24] improvements in children's eating habits was recorded following the community-based nutritional counseling intervention carried out among children in rural communities in Enugu State, Nigeria. Evidence suggests that multicomponent interventions combining better availability of fruit and vegetables with a nutrition counseling curriculum presented by the teacher, as well as the involvement of parents to some level, can be helpful.[25] For children, especially those living in rural areas, there appears to be a great chance of success for a range of fruit and vegetable promotion activities if recommended for implementation, as an environmental and multicomponent intervention scheme by the government through multiple rural development projects. There is evidence that rural communities contribute immensely to the eating habits of children and adolescents; hence, it is advocated that the entire rural communities should be the focus of interventions aimed at improving children's eating habits.[26,27] While this notion abounds, a different notion suggests that positive deviation from the norms in eating habits of children due to nutritional counseling interventions may not be stable.[28] Poor eating habits are a major issue among most children in rural communities in Nigeria[29]; however, improvement in eating habits can be attained through community-based nutritional counseling interventions.
3.1. Limitations and suggestions for future study
In applying the findings of this experiment, one major limitation is the non-probabilistic sampling method used in this study. In particular, the recruitment of an adequate number of participants for factor analysis was a major concern. Even though we succeeded in doing this, the sample may not be deemed representative of Nigerian community-dwelling children with eating disorders. Again, notwithstanding the achievement of this study, it should be noted that only one instrument (CBEQ) was used repeatedly as an outcome measure that could result in a practice effect, a condition whereby participants master the instrument or become bored at completing the instrument.[30] Future studies should investigate the option of employing multiple measures concurrently or otherwise. Using the CEBQ in future studies might broaden our understanding of inherited behavioral phenotypes as well as direct health counseling initiatives.
There is a need to carry out community-based nutritional counseling interventions that would significantly improve the eating habits and well-being of children in rural communities. The interventions require the constant collaboration of health-promoting experts, families, nutritional experts, counselors, childhood educators, school staff, rural extension personnel, and the children themselves. Again, a potential long-term assessment of the effects of community-based nutritional counseling interventions on children's future nutrition and eating habits is needed. In particular, researchers are urged to conduct follow-up studies to examine the effectiveness of community-based nutritional counseling interventions for different study populations other than community-dwelling children. Again, it is recommended that community-based nutritional counseling should be approved and established in rural communities, given the effectiveness of community-based nutritional counseling interventions in reducing community-dwelling children's eating disorders. This may assure its use in championing children's health and well-being in Nigeria and beyond.
3.2. Implications of the study
In developing countries, poor rural areas are particularly important for health improvement initiatives. Poor eating habits and deficiencies in nutrition knowledge harmfully affect health, especially in underprivileged rural communities and increased healthcare costs. To foster good eating habits among rural communities in Nigeria, community development programs can work in partnership with nutritional counseling professionals to develop dietary frameworks to assist rural households, who are predominantly farmers, in developing better eating behaviors. Nutritional counseling professionals can help rural households get used to one of the most basic requirements of good health, a balanced diet.[31] Conversely, rural households could benefit from the prevention of illness and malnutrition when their eating practices and knowledge of food nutritive value are improved.
Nutritional educators through well-organized extension outreach programs can guide rural dwellers toward attaining nutrition-related goals by developing a nutrition plan that can promote healthy and proper eating practices. The researchers would like to encourage nutritional experts to get acquainted with adequate training in basic counseling, childhood practices, and cognitive-behavioral skills to facilitate nutritional counseling and education in rural areas. These techniques can be very useful in helping rural dwellers make successful changes in their dietary practices.[31] Finally, it appears that through the adoption of healthy diets facilitated by nutritional educators, many of the known nutritional health issues affecting individuals of all ages in rural communities in Nigeria and beyond might be avoided through community-based nutritional counseling intervention on eating habits among rural dwellers.
4. Conclusion
This study evaluated the effect of community-based nutritional counseling as an intervention for eating habits among children in rural communities. Poor eating habits may hinder the ability of children in rural communities to cope with physical illnesses. However, nutritional counseling interventions can help these children overcome poor eating habits. The outcomes of the research showed that children's eating habits in the treatment group improved positively following the community-based nutritional counseling intervention. The positive gain from exposure to the nutritional counseling intervention program was sustained at follow-up for children in the treatment group.
4.1. Uncited reference
[19].
Author contributions
Conceptualization: Ibiwari Caroline Dike, Elizabeth N. Ebizie, Chiamaka Adaobi Chukwuone, Eunice Ifenyinwa Ugwu, Grace Chinyere Nnadi.
Data curation: Elizabeth N. Ebizie, Ezeda Kalu Ogbonnaya, Scholastica Nkechinyere Udeagha, Justina Ndirika Chikwendu.
Formal analysis: Elizabeth N. Ebizie, Chiamaka Adaobi Chukwuone, Margret N. Ezeaku.
Funding acquisition: Ibiwari Caroline Dike, Ezeda Kalu Ogbonnaya, Scholastica Nkechinyere Udeagha, Margret N. Ezeaku, Nguvan Patience Gera.
Investigation: Chinwe Christiana Anowai, Eberechukwu Francisca Chigbu, Margret N. Ezeaku, Nguvan Patience Gera, Justina Ndirika Chikwendu.
Methodology: Eberechukwu Francisca Chigbu, Grace Chinyere Nnadi.
Project administration: Ibiwari Caroline Dike, Ezeda Kalu Ogbonnaya, Eunice Ifenyinwa Ugwu, Eberechukwu Francisca Chigbu, Grace Chinyere Nnadi, Nguvan Patience Gera, Justina Ndirika Chikwendu.
Resources: Ngozi Juliana Ejiofor, Chinwe Christiana Anowai, Eunice Ifenyinwa Ugwu, Grace Chinyere Nnadi.
Software: Elizabeth N. Ebizie, Ekomau Chinyere Ihuoma.
Supervision: Elizabeth N. Ebizie, Ngozi Juliana Ejiofor, Chinwe Christiana Anowai, Scholastica Nkechinyere Udeagha, Eberechukwu Francisca Chigbu, Ekomau Chinyere Ihuoma, Justina Ndirika Chikwendu.
Validation: Ibiwari Caroline Dike, Elizabeth N. Ebizie, Ngozi Juliana Ejiofor, Chinwe Christiana Anowai, Scholastica Nkechinyere Udeagha, Ekomau Chinyere Ihuoma.
Visualization: Elizabeth N. Ebizie, Ekomau Chinyere Ihuoma.
Writing – original draft: Ibiwari Caroline Dike, Margret N. Ezeaku.
Writing – review & editing: Ibiwari Caroline Dike, Ezeda Kalu Ogbonnaya.
Footnotes
Abbreviation: CEBQ = child eating behavior questionnaire.
How to cite this article: Dike IC, Ebizie EN, Chukwuone CA, Ejiofor NJ, Anowai CC, Ogbonnaya EK, Ugwu EI, Nkechinyere US, Chigbu EF, Ezeaku MN, Nnadi GC, Ihuoma EC, Gera NP, Chikwendu JN. Effect of community-based nutritional counseling intervention on children's eating habits. Medicine. 2021;100:30(e26563).
The authors have declared that no competing interests exist.
Data Statement: All relevant data are within the paper and its Supporting Information files.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Table showing demographic characteristics of participants.
= effect size, ANOVA = analysis of variance, CEBQ = child eating behavior questionnaire, Degree of freedom = 1101, M = mean, number for control group = 53, number for treatment group = 49, R2 = adjusted, SD = standard deviation.
References
- [1].Kollataj W, Sygit K, Sygit M, Karwat ID, Kollataj B. Eating habits of children and adolescents from rural regions depending on gender, education, and economic status of parents. Ann Agric Environ Med 2011;18:393–7. [PubMed] [Google Scholar]
- [2].Saronga NJ, Mosha IH, Kessy AT, et al. I eat two meals per day” impact of climate variability on eating habits among households in Rufiji district, Tanzania: a qualitative study. Agric Food Secur 2016;5:14.doi:10.1186/s40066-016-0064-6. [Google Scholar]
- [3].Cahyani AD, Ispurwanto W, Rumeser JA, Setyorini A. Eating Habit Among Workers in Jakarta. 2016;Indonesia: Bina Nusantara University, Published online. [Google Scholar]
- [4].Kramer CV, Allen S. Malnutrition in developing countries. Paediatr Child Health 2015;25:422–7. [Google Scholar]
- [5].Demographic NN. Health Survey 2008. Abuja National Population Commission and ICF Macro 2009. [Google Scholar]
- [6].Duru CB, Oluoha UR, Uwakwe KA, et al. Prevalence and sociodemographic determinants of malnutrition among under-five children in rural communities in Imo State, Nigeria. Am J Public Health Res 2015;3:199–206. [Google Scholar]
- [7].Prendergast AJ. Malnutrition and vaccination in developing countries. Philos Trans R Soc B Biol Sci 2015;370:20140141.doi:10.1098/rstb.2014.0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Endris N, Asefa H, Dube L. Prevalence of malnutrition and associated factors among children in rural Ethiopia. BioMed Res Int 2017;2017:6587853.doi:10.1155/2017/6587853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gladstone M, Mallewa M, Jalloh AA, et al. Assessment of neurodisability and malnutrition in children in Africa. Semin Pediatr Neurol 2014;21:50–7. [DOI] [PubMed] [Google Scholar]
- [10].Jordan CH, Wang W, Donatoni L, Meier BP. Mindful eating: trait and state mindfulness predict healthier eating behavior. Personal Individ Differ 2014;68:107–11. [Google Scholar]
- [11].Beshara M, Hutchinson AD, Wilson C. Does mindfulness matter? Everyday mindfulness, mindful eating and self-reported serving size of energy dense foods among a sample of South Australian adults. Appetite 2013;67:25–9. [DOI] [PubMed] [Google Scholar]
- [12].Kristeller J, Wolever RQ, Sheets V. Mindfulness-based eating awareness training (MB-EAT) for binge eating: a randomized clinical trial. Mindfulness 2014;5:282–97. [Google Scholar]
- [13].van Koningsbruggen GM, Veling H, Stroebe W, Aarts H. Comparing two psychological interventions in reducing impulsive processes of eating behaviour: effects on self-selected portion size. Br J Health Psychol 2014;19:767–82. [DOI] [PubMed] [Google Scholar]
- [14].Turton R, Bruidegom K, Cardi V, Hirsch CR, Treasure J. Novel methods to help develop healthier eating habits for eating and weight disorders: a systematic review and meta-analysis. Neurosci Biobehav Rev 2016;61:132–55. [DOI] [PubMed] [Google Scholar]
- [15].World Health Organization;, Joint FAO, Organization WH. Additives WEC on F. Evaluation of Certain Contaminants in Food: Eighty-Third Report of the Joint FAO/WHO Expert Committee on Food Additives. 2017. [Google Scholar]
- [16].Association WM. Declaration of Helsinki. Ethical principles for medical research involving human subjects. Jahrb Für Wiss Ethik 2009;14:233–8. [PubMed] [Google Scholar]
- [17].Faul F, Erdfelder E, Lang A-G, Buchner A. G∗ Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175–91. [DOI] [PubMed] [Google Scholar]
- [18].Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G∗ Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 2009;41:1149–60. [DOI] [PubMed] [Google Scholar]
- [19].Njokuocha RC. Evaluation of pollen and chemical composition of honey samples sourced from open markets in Anambra State, Nigeria to ascertain their authenticity. J Appl Life Sci Int 2019;22:01–12. Published online. [Google Scholar]
- [20].Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the children's eating behaviour questionnaire. J Child Psychol Psychiatry 2001;42:963–70. [DOI] [PubMed] [Google Scholar]
- [21].Viana V, Sinde S, Saxton JC. Children's eating behaviour questionnaire: associations with BMI in Portuguese children. Br J Nutr 2008;100:445–50. [DOI] [PubMed] [Google Scholar]
- [22].Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol 2004;4:01–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].O’Connor M, Touyz S, Beumont P. Nutritional management and dietary counseling in bulimia nervosa: some preliminary observations. Int J Eat Disord 1988;7:657–62. [Google Scholar]
- [24].Molenaar EA, van Ameijden EJ, Vergouwe Y, Grobbee DE, Numans ME. Effect of nutritional counselling and nutritional plus exercise counselling in overweight adults: a randomized trial in multidisciplinary primary care practice. Fam Pract 2010;27:143–50. [DOI] [PubMed] [Google Scholar]
- [25].Van Cauwenberghe E, Maes L, Spittaels H, et al. Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: systematic review of published and ‘grey’literature. Br J Nutr 2010;103:781–97. [DOI] [PubMed] [Google Scholar]
- [26].Cullen KW, Baranowski T, Owens E, Marsh T, Rittenberry L, De Moor C. Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children's dietary behavior. Health Educ Behav 2003;30:615–26. [DOI] [PubMed] [Google Scholar]
- [27].Patrick H, Nicklas TA. A review of family and social determinants of children's eating patterns and diet quality. J Am Coll Nutr 2005;24:83–92. [DOI] [PubMed] [Google Scholar]
- [28].Willaing I, Ladelund S, Jorgensen T, Simonsen T, Nielsen LM. Nutritional counselling in primary health care: a randomized comparison of an intervention by general practitioner or dietician. Eur J Cardiovasc Prev Rehabil 2004;11:513–20. [DOI] [PubMed] [Google Scholar]
- [29].Eze J, Oguonu T, Ojinnaka N, Ibe B. Physical growth and nutritional status assessment of school children in Enugu, Nigeria. Niger J Clin Pract 2017;20:64–70. [DOI] [PubMed] [Google Scholar]
- [30].Rana R, Singhal R, Singh V. Analysis of repeated measurement data in the clinical trials. J Ayurveda Integr Med 2013;4:77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Dylan B. Nutritional Counselling Career. 2016;Millburn, New Jersey, United States:Published online. [Google Scholar]