Abstract
Even though inside-out repair of meniscal tears is still the gold standard, the need for a posterior incision is a certain disadvantage of this approach. However, all-inside arthroscopic meniscal stacked suture repair can be performed for hypermobile lateral meniscus using all-inside devices and slotted canula. This technique is able not only to reduce surgical invasion but also preserve meniscal mobility, since sutures are placed on the peripheral area of the lateral meniscus. To successfully use the devices required for this procedure, surgeons must understand proper insertion techniques. The purpose of this Technical Note is to demonstrate this technique using FASTFIX 360.
Technique Video
The patient was a 66-year-old female who complained of a locking sensation in her right knee during knee flexion. A hypermobile lateral meniscus was suspected from physical findings and magnetic resonance imaging. After routine arthroscopic observation, the posterior portion of the lateral meniscus was easily pulled through the lateral condyle with a probe, despite the obvious tear observed from the anterolateral portal. Rasping was performed to refresh the peripheral rim of the lateral meniscus. Care should be taken during this procedure not to injure meniscal midbody and cartilage. A slotted cannula was inserted through the anteromedial portal with varus and internal rotation of the tibia, resulting in the figure-4 position. The slotted canula was then positioned above and below the peripheral lesion of the lateral meniscus to hold it. The built-in, adjustable depth penetration limiter of the FASTFIX 360 was set at 10 to 12 mm. The slotted cannula was not removed until the introduction of the first needle delivery to help position the tip of the needle at the ideal location on the meniscus, ensuring that the tip of the needle is pointing downwards. A vertical stacked suture using the FASTFIX 360 was placed through the loose meniscofemoral attachments and superior peripheral rim of the lateral meniscus to close the superior gap. Then, a second vertical stacked suture was placed through the loose meniscotibial attachments and inferior peripheral rim of the lateral meniscus to close the inferior gap. Double-stacked vertical sutures were placed approximately 5 mm from the peripheral rim so that meniscal mobility was preserved because the sutures were not placed inside the midbody of the lateral meniscus. Diagnostic probing was performed and lateral meniscus adjunct, and the popliteal fossa was pulled through the lateral condyle. Therefore, a third stacked suture was performed to tighten this lesion. In addition, the depth penetration limiter was then set at 10 to 12 mm, according to preoperative evaluation, so as not to interfere with the lateral collateral ligament. The slotted cannula was inserted into the popliteal fossa just lateral to the popliteus tendon. The delivery needle was then internally rotated to pass as close as possible to the popliteus tendon. Maintaining this position, the deployment slider was pushed forward to deploy the first implant. The delivery needle was then slightly pulled and externally rotated so that the tip of the delivery needle aims to the capsular side and the second implant was placed on the capsular side. The patient was immobilized for 4 weeks after surgery, and range of motion exercise and weight bearing, as tolerated, were allowed after immobilization. This patient recovered to the preoperative activity level 3 months after surgery, with no recurrence during the 2-year follow-up.
One of the causes of knee pain, hypermobile lateral meniscus (HLM), also results in a locking sensation during knee flexion. It is induced by disrupted popliteomeniscal fascicles1 and is commonly repaired with arthroscopic inside-out vertical stacked suturing. In this way, a skin incision is usually made behind the lateral collateral ligament (LCL) with the knee in a flexed position. The lateral head of the gastrocnemius muscle is then separated from the posterolateral capsule using a retractor to protect neurovascular bundles.2
Using an all-inside technique, however, can reduce surgical invasiveness from posterior incision and remove the need for an experienced assistant to catch the needle. Although the biomechanical fixation strength of previous-generation all-inside devices has been a concern, those that are currently in use have improved fixation strength and clinical results, and the procedure is now reported to be comparable with inside-out repair.3,4 However, all-inside devices bring with them neurovascular risk, increased incidence of technical error and device problems, greater cost, and theoretically, iatrogenic meniscus damage as a result of larger-diameter insertion needles.5
To minimize the surgical invasiveness of this procedure, we have developed an all-inside arthroscopic meniscal stacked suture repair for HLM. The purpose of this Technical Note is to guide surgeons through the appropriate use of this technique using FASTFIX 360 (Smith & Nephew Endoscopy, Andover, MA).
Indications
A history of repeated locking symptoms is an important indicator of possible HLM. The diagnosis of HLM is made by physical examination6 and magnetic resonance imaging, which can show disrupted popliteomeniscal fascicles. Surgery is indicated when patients with HLM complain of a frequent locking sensation and apprehension when valgus and deep flexion force are applied to the knee.
Surgical Technique (With Video Illustration)
This novel technique is carried out under regional or general anesthesia without a pneumatic tourniquet. The patient is placed in a supine position with the operative knee held in the leg drop position with 90° of flexion. Standard anterolateral and anteromedial portals are made and a routine arthroscopic evaluation is performed. Meniscus movement is observed from knee extension to flexion. The posterior portion of the lateral meniscus is easily pulled through the lateral condyle with a probe, regardless of the obvious tear observed from standard portals (Fig 1). To perform the all-inside arthroscopic meniscal stacked suture repair, the knee is flexed on the operating table with varus and internal rotation of the tibia, resulting in a figure-4 position, and adduction stress is applied to the medial femoral condyle for better visualization. Rasping is performed to refresh the peripheral rim of the lateral meniscus. Care should be taken during this procedure not to injure meniscal midbody and cartilage. Double-stacked vertical sutures (D-SVS) are used in the repair of the disrupted meniscotibial attachments approximately 5 mm from the peripheral rim so that mobility can be preserved in the lateral meniscus following surgery. A slotted cannula is inserted through the anteromedial portal and then positioned until it is above and below the peripheral lesion of the lateral meniscus so that the FASTFIX 360 can be easily inserted. The built-in, adjustable depth penetration limiter is set at 10 to 12 mm. The slotted cannula is not removed until the introduction of the first needle delivery to help position the tip of the needle at the ideal location on the meniscus, ensuring that the tip of the needle is pointing downwards. A delivery needle is introduced into the peripheral meniscal tissue about 5 mm from the capsular side. A slotted cannula is used as a stabilizer for the meniscus to ensure that the implants are placed accurately (Fig 2). When it is at the desired entry point, the tip of the slotted cannula is rotated, not only to protect neurovascular structures but also to obtain better visualization. While maintaining this position, the deployment slider is pushed forward to deploy the first implant. The delivery needle is then pulled slightly and rotated so that its tip aims to the capsular side, where the second implant is placed. The first stacked suture is placed through the loose meniscofemoral attachments and superior peripheral rim of the lateral meniscus to close the superior gap and fixed (Fig 3). The second stacked suture is placed through the loose meniscotibial attachments and inferior peripheral rim of the lateral meniscus to close the inferior gap and fixed (Fig 4). When the delivery needle inserted from the anteromedial portal is placed near the popliteus tendon with some risk of penetration, a central transpatellar tendon portal7 is made. Following D-SVS (Fig 5), diagnostic probing is performed and in case of lateral meniscus adjunct, the popliteal fossa can easily be pulled through the lateral condyle. A third stacked suture is performed to tighten this lesion. In addition, the depth penetration limiter is then set at 10 to 12 mm, according to preoperative evaluation, so as not to interfere with the LCL. The slotted cannula is inserted into the popliteal fossa just lateral to the popliteus tendon. The delivery needle is then internally rotated to pass as close as possible to the popliteus tendon. Maintaining this position, the deployment slider is pushed forward to deploy the first implant. The delivery needle is then slightly pulled and externally rotated so that the tip of the delivery needle aims to the capsular side and the second implant is placed on the capsular side (Fig 6 and Video 1).
Fig 1.
Arthroscopic image of hypermobile lateral meniscus of the right knee from the anterolateral portal. The knee is flexed on the operating table with varus and internal rotation of the tibia, resulting in the figure-four position, and adduction stress is applied to the medial femoral condyle. The posterior portion of lateral meniscus is easily pulled using a probe through the lateral condyle (black arrow).
Fig 2.
A slotted cannula was inserted through the anteromedial portal in the figure-4 position and was placed on the superior peripheral rim of the lateral meniscus to stabilize the meniscus for accurate placement of the implant for stacked suture using FASTFIX 360 (black arrow). Arthroscopic image from the anterolateral portal is shown.
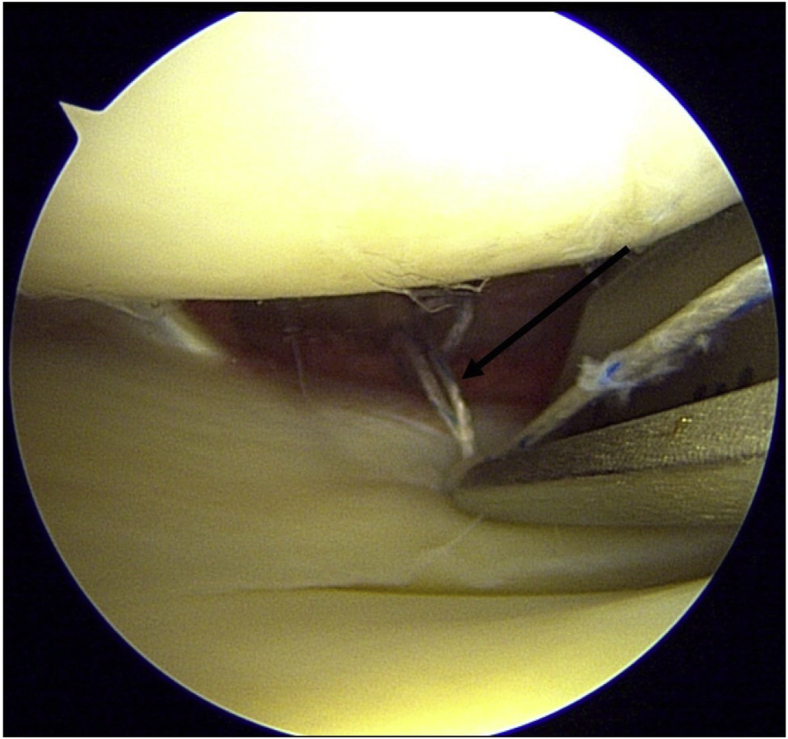
Fig 3.
A first vertical stacked suture is placed through the loose meniscofemoral attachments and superior peripheral rim of the lateral meniscus to close the superior gap (black arrow). A needle is inserted approximately 5 mm from the peripheral rim of the lateral meniscus so that mobility can be preserved following surgery. Arthroscopic image of the lateral meniscus of the right knee from the anterolateral portal in the figure-4 position is shown.
Fig 4.
A second stacked suture is placed through the loose meniscotibial attachments and inferior peripheral rim of the lateral meniscus to close the inferior gap (black arrow). Arthroscopic image of the lateral meniscus of the right knee from the anterolateral portal in the figure-4 position is shown.
Fig 5.
Arthroscopic image of lateral meniscus following double-stacked vertical sutures (black arrows). Meniscal mobility is preserved because the sutures are not placed inside the midbody of the lateral meniscus. Arthroscopic image of the lateral meniscus of the right knee from the anterolateral portal in the figure-4 position is shown.
Fig 6.
Diagnostic probing was performed after double-stacked vertical sutures, and in case of a lateral meniscus adjunct, the popliteal fossa is pulled through the lateral condyle, and an additional vertical stacked suturing at the popliteal fossa is performed to tighten this lesion in this patient. The depth penetration limiter is set at 10 to 12 mm so as to not interfere with the lateral collateral ligament (black arrow). Arthroscopic image of the lateral meniscus of the right knee from the anterolateral portal in the figure-4 position is shown.
Pearls and pitfalls and advantages and disadvantages of this technique are shown in Tables 1 and 2.
Table 1.
Pearls and Pitfalls of All-Inside Arthroscopic Meniscal Stacked Suture Repair
| Pearls |
| Holds the figure-4 position |
| Adduction stress for better visualization |
| Appropriate placement of the slotted canula |
| Avoids too-deep penetration of the delivery needle |
| Tightens the knot appropriately |
| Pitfalls |
| Inappropriate portals |
| Handling error due to insufficient synovectomy |
| Poor visualization due to intraarticular bleeding |
| Chondral damage when inserting the slotted canula |
| Neurovascular injury |
| Penetration of the LCL and popliteus tendon |
LCL, lateral collateral ligament.
Table 2.
Advantages and Disadvantages of All-Inside Arthroscopic Meniscal Stacked Suture Repair
| Advantages |
| No need for skin incision behind LCL |
| Reduced surgical invasiveness |
| No need for an experienced assistant |
| Disadvantages |
| Neurovascular risk |
| Technical error and device problems |
| Implant cost |
LCL, lateral collateral ligament.
Postoperative Rehabilitation
A brace to immobilize the affected limb is applied for 4 weeks. Range of motion exercise and open kinetic chain muscle training are permitted after immobilization, and the patients are permitted full weight bearing. Squatting and sports activities are permitted at 12 weeks after surgery.
Discussion
Inside-out repair of meniscal tears is still the gold standard in terms of biomechanical strength8; however, the need for a posterior incision is a disadvantage. In particular, when treating HLM, care should be taken not to interfere with the LCL, popliteus tendon, neurovascular bundles, and peroneal nerve. Using this all-inside arthroscopic meniscal stacked suture repair technique, we were able to treat HLM safely and less invasively without a posterior incision or the need for an experienced assistant to hold the needle. This is the greatest advantage of this procedure. Previous generations of all-inside devices often resulted in chondral damage because the suture was too rigidly prominent on the meniscal surface9 and caused pain due to penetration of the capsule.10 These 2 disadvantages were modified in this technique because D-SVS are performed approximately 5 mm from the peripheral rim of the lateral meniscus not only to preserve mobility in the lateral meniscus but also to prevent suture prominence on the meniscal surface; we set the depth penetration limiter at 10 to 12 mm to ensure that postoperative pain is not caused, which can occur if the capsule penetrates too deeply. On the contrary, there is a residual risk of interfering with the LCL, popliteus tendon, neurovascular bundles, and peroneal nerve in this technique; hence, accurate understanding of the anatomy around the posterolateral lesion of the knee is a prerequisite for performing this procedure safely. Biomechanically simple parallel vertical sutures have a pattern similar to crossed suture patterns for longitudinal meniscal tears.11 It is uncertain whether this is in line with HLM. Extensive lesions have been reported as a poor prognostic factor for all-inside meniscal repair using the FASTFIX 360.12 Therefore, further study is required to clarify the appropriate candidates for this procedure when treating patients with HLM.
Beyond the risks and limitations, however, this technique enables a reduction in surgical invasiveness and can preserve meniscal mobility since sutures are not placed inside the midbody of the lateral meniscus.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient was a 66-year-old female who complained of a locking sensation in her right knee during knee flexion. A hypermobile lateral meniscus was suspected from physical findings and magnetic resonance imaging. After routine arthroscopic observation, the posterior portion of the lateral meniscus was easily pulled through the lateral condyle with a probe, despite the obvious tear observed from the anterolateral portal. Rasping was performed to refresh the peripheral rim of the lateral meniscus. Care should be taken during this procedure not to injure meniscal midbody and cartilage. A slotted cannula was inserted through the anteromedial portal with varus and internal rotation of the tibia, resulting in the figure-4 position. The slotted canula was then positioned above and below the peripheral lesion of the lateral meniscus to hold it. The built-in, adjustable depth penetration limiter of the FASTFIX 360 was set at 10 to 12 mm. The slotted cannula was not removed until the introduction of the first needle delivery to help position the tip of the needle at the ideal location on the meniscus, ensuring that the tip of the needle is pointing downwards. A vertical stacked suture using the FASTFIX 360 was placed through the loose meniscofemoral attachments and superior peripheral rim of the lateral meniscus to close the superior gap. Then, a second vertical stacked suture was placed through the loose meniscotibial attachments and inferior peripheral rim of the lateral meniscus to close the inferior gap. Double-stacked vertical sutures were placed approximately 5 mm from the peripheral rim so that meniscal mobility was preserved because the sutures were not placed inside the midbody of the lateral meniscus. Diagnostic probing was performed and lateral meniscus adjunct, and the popliteal fossa was pulled through the lateral condyle. Therefore, a third stacked suture was performed to tighten this lesion. In addition, the depth penetration limiter was then set at 10 to 12 mm, according to preoperative evaluation, so as not to interfere with the lateral collateral ligament. The slotted cannula was inserted into the popliteal fossa just lateral to the popliteus tendon. The delivery needle was then internally rotated to pass as close as possible to the popliteus tendon. Maintaining this position, the deployment slider was pushed forward to deploy the first implant. The delivery needle was then slightly pulled and externally rotated so that the tip of the delivery needle aims to the capsular side and the second implant was placed on the capsular side. The patient was immobilized for 4 weeks after surgery, and range of motion exercise and weight bearing, as tolerated, were allowed after immobilization. This patient recovered to the preoperative activity level 3 months after surgery, with no recurrence during the 2-year follow-up.
References
- 1.Kimura M., Shirakura K., Hasegawa A., Kobayashi Y., Udagawa E. Anatomy and pathophysiology of the popliteal tendon area in the lateral meniscus: 1. Arthroscopic and anatomical investigation. Arthroscopy. 1992;8:419–423. doi: 10.1016/0749-8063(92)90001-r. [DOI] [PubMed] [Google Scholar]
- 2.Kamiya T., Suzuki T., Otsubo H., et al. Midterm outcomes after arthroscopic surgery for hypermobile lateral meniscus in adults: Restriction of paradoxical motion. J Orthop Sci. 2018;23:1000–1004. doi: 10.1016/j.jos.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Rosso C., Muller S., Buckland D.M., et al. All-inside meniscal repair devices compared with their matched inside-out vertical mattress suture repair: Introducing 10,000 and 100,000 loading cycles. Am J Sports Med. 2014;42:2226–2233. doi: 10.1177/0363546514538394. [DOI] [PubMed] [Google Scholar]
- 4.Fillingham Y.A., Riboh J.C., Erickson B.J., Bach B.R., Jr., Yanke A.B. Inside-out versus all-inside repair of isolated meniscal tears: An updated systematic review. Am J Sports Med. 2017;45:234–242. doi: 10.1177/0363546516632504. [DOI] [PubMed] [Google Scholar]
- 5.Miller M.D., Kline A.J., Gonzales J., Beach W.R. Pitfalls associated with FasT-Fix meniscal repair. Arthroscopy. 2002;18:939–943. doi: 10.1053/jars.2002.36146. [DOI] [PubMed] [Google Scholar]
- 6.LaPrade R.F., Konowalchuk B.K. Popliteomeniscal fascicle tears causing symptomatic lateral compartment knee pain: Diagnosis by the figure-4 test and treatment by open repair. Am. J. Sports Med. 2005;33:1231–1236. doi: 10.1177/0363546504274144. [DOI] [PubMed] [Google Scholar]
- 7.Perelli S, Erquicia JI, Morales Marin C, et al. Central transpatellar tendon portal is safe when used for anterior cruciate ligament reconstruction [published online September 8, 2020]. J. Knee Surg. https://doi.org/10.1055/s-0040-1716380. [DOI] [PubMed]
- 8.Passaro E., Jr., Howard T., Sawicki M. Gastrinomas in MEN-I. N Engl J Med. 1990;323:349–350. doi: 10.1056/NEJM199008023230518. [DOI] [PubMed] [Google Scholar]
- 9.Ross G., Grabill J., McDevitt E. Chondral injury after meniscal repair with bioabsorbable arrows. Arthroscopy. 2000;16:754–756. doi: 10.1053/jars.2000.4629. [DOI] [PubMed] [Google Scholar]
- 10.Goradia V.K. All-inside arthroscopic meniscal repair with meniscal cinch. Arthrosc Tech. 2013;2:e171–e174. doi: 10.1016/j.eats.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Milchteim C., Branch E.A., Maughon T., Hughey J., Anz A.W. Biomechanical comparison of parallel and crossed suture repair for longitudinal meniscus tears. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116640263. 2325967116640263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laurendon L., Neri T., Farizon F., Philippot R. Prognostic factors for all-inside meniscal repair. A 87-case series. Orthop Traumatol Surg Res. 2017;103:1017–1020. doi: 10.1016/j.otsr.2017.05.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient was a 66-year-old female who complained of a locking sensation in her right knee during knee flexion. A hypermobile lateral meniscus was suspected from physical findings and magnetic resonance imaging. After routine arthroscopic observation, the posterior portion of the lateral meniscus was easily pulled through the lateral condyle with a probe, despite the obvious tear observed from the anterolateral portal. Rasping was performed to refresh the peripheral rim of the lateral meniscus. Care should be taken during this procedure not to injure meniscal midbody and cartilage. A slotted cannula was inserted through the anteromedial portal with varus and internal rotation of the tibia, resulting in the figure-4 position. The slotted canula was then positioned above and below the peripheral lesion of the lateral meniscus to hold it. The built-in, adjustable depth penetration limiter of the FASTFIX 360 was set at 10 to 12 mm. The slotted cannula was not removed until the introduction of the first needle delivery to help position the tip of the needle at the ideal location on the meniscus, ensuring that the tip of the needle is pointing downwards. A vertical stacked suture using the FASTFIX 360 was placed through the loose meniscofemoral attachments and superior peripheral rim of the lateral meniscus to close the superior gap. Then, a second vertical stacked suture was placed through the loose meniscotibial attachments and inferior peripheral rim of the lateral meniscus to close the inferior gap. Double-stacked vertical sutures were placed approximately 5 mm from the peripheral rim so that meniscal mobility was preserved because the sutures were not placed inside the midbody of the lateral meniscus. Diagnostic probing was performed and lateral meniscus adjunct, and the popliteal fossa was pulled through the lateral condyle. Therefore, a third stacked suture was performed to tighten this lesion. In addition, the depth penetration limiter was then set at 10 to 12 mm, according to preoperative evaluation, so as not to interfere with the lateral collateral ligament. The slotted cannula was inserted into the popliteal fossa just lateral to the popliteus tendon. The delivery needle was then internally rotated to pass as close as possible to the popliteus tendon. Maintaining this position, the deployment slider was pushed forward to deploy the first implant. The delivery needle was then slightly pulled and externally rotated so that the tip of the delivery needle aims to the capsular side and the second implant was placed on the capsular side. The patient was immobilized for 4 weeks after surgery, and range of motion exercise and weight bearing, as tolerated, were allowed after immobilization. This patient recovered to the preoperative activity level 3 months after surgery, with no recurrence during the 2-year follow-up.
The patient was a 66-year-old female who complained of a locking sensation in her right knee during knee flexion. A hypermobile lateral meniscus was suspected from physical findings and magnetic resonance imaging. After routine arthroscopic observation, the posterior portion of the lateral meniscus was easily pulled through the lateral condyle with a probe, despite the obvious tear observed from the anterolateral portal. Rasping was performed to refresh the peripheral rim of the lateral meniscus. Care should be taken during this procedure not to injure meniscal midbody and cartilage. A slotted cannula was inserted through the anteromedial portal with varus and internal rotation of the tibia, resulting in the figure-4 position. The slotted canula was then positioned above and below the peripheral lesion of the lateral meniscus to hold it. The built-in, adjustable depth penetration limiter of the FASTFIX 360 was set at 10 to 12 mm. The slotted cannula was not removed until the introduction of the first needle delivery to help position the tip of the needle at the ideal location on the meniscus, ensuring that the tip of the needle is pointing downwards. A vertical stacked suture using the FASTFIX 360 was placed through the loose meniscofemoral attachments and superior peripheral rim of the lateral meniscus to close the superior gap. Then, a second vertical stacked suture was placed through the loose meniscotibial attachments and inferior peripheral rim of the lateral meniscus to close the inferior gap. Double-stacked vertical sutures were placed approximately 5 mm from the peripheral rim so that meniscal mobility was preserved because the sutures were not placed inside the midbody of the lateral meniscus. Diagnostic probing was performed and lateral meniscus adjunct, and the popliteal fossa was pulled through the lateral condyle. Therefore, a third stacked suture was performed to tighten this lesion. In addition, the depth penetration limiter was then set at 10 to 12 mm, according to preoperative evaluation, so as not to interfere with the lateral collateral ligament. The slotted cannula was inserted into the popliteal fossa just lateral to the popliteus tendon. The delivery needle was then internally rotated to pass as close as possible to the popliteus tendon. Maintaining this position, the deployment slider was pushed forward to deploy the first implant. The delivery needle was then slightly pulled and externally rotated so that the tip of the delivery needle aims to the capsular side and the second implant was placed on the capsular side. The patient was immobilized for 4 weeks after surgery, and range of motion exercise and weight bearing, as tolerated, were allowed after immobilization. This patient recovered to the preoperative activity level 3 months after surgery, with no recurrence during the 2-year follow-up.