Abstract
Perioperative pain control for hip arthroscopy procedures represents a significant challenge for both surgeons and anesthetists. In light of the opioid crisis, greater emphasis has been placed on multimodal pain control techniques. There is considerable debate regarding regional nerve blockade for hip arthroscopy. Although regional anesthesia has a significant role in perioperative pain management strategies, many of the most common techniques present their own risks and limitations. In particular, the less desirable effects of postoperative weakness in the lower extremity and difficulty with ambulation are commonly produced with standard regional blockades. We present a technique for performing a targeted, sensory nerve block that can be done efficiently and safely in the immediate preoperative period. This block can potentially lower the intraoperative and postoperative opioid requirements without the risks of muscle blockade and falls from other regional anesthesia modalities.
Technique Video
This video demonstrates the pericapsular nerve group (PENG) block done before surgery for regional anesthesia and postoperative pain control in a patient undergoing a right hip arthroscopy. The patient is in the supine position with the right hip exposed. The anesthetist is seated to the side of the patient, with the probe in his right hand the needle in his left. The block is performed with ultrasound guidance using a SonoSite X-Porte HFL50xp (15-6MHz) linear ultrasound probe. The ultrasound screen is placed on the opposite side of the patient for easy viewing. The video includes the labeled corresponding ultrasound video performed during the block.
As the understanding of the pathology of femoroacetabular impingement (FAI) has advanced, the number of hip arthroscopic procedures performed has increased 495% from 2004 to 2016, from 2.35 to 15.47 per 100,000 residents in New York State.1 At the same time, the opioid crisis has driven increased recognition of perioperative pain control and the evolution of various multimodal pain management strategies. Regarding arthroscopic procedures in the hip, most strategies incorporate perioperative oral medication regimens and the use of regional anesthesia for both intraoperative and postoperative pain control. A previously performed double-blinded, randomized controlled trial on the use of bupivacaine versus liposomal bupivacaine in a fascia iliaca block demonstrated no significant difference in the postoperative pain scores between the 2 groups. However, the liposomal group had a statistically higher amount of lateral thigh numbness at postoperative days 2 and 3. Four patients (5.4%) had a fall in the acute postoperative period.2 Another randomized controlled trial comparing the fascia iliaca block to local anesthetic infiltration after hip arthroscopy found that the locally administered group had better pain scores, decreased opioid consumption, and fewer side effects.3 On the basis of these results, there is concern among experts, that the fascia iliaca block may not be the optimal regional blockade for use in hip arthroscopy, thus prompting clinicians to search for a better regional anesthetic approach.
Initially described by Gardner in 1948,4 the sensory innervation of the anterior hip capsule is provided by the obturator nerve, accessory obturator nerve, and femoral nerve. A recent anatomic and histological study additionally found the anterior hip capsule to be the most heavily innervated portion of the hip capsule.5 Short et al.6 recently published an anatomic study confirming the classically described innervation pattern but also noted that the accessory obturator nerve and femoral nerve may play an even greater role in the anterior hip. They also describe the relevant anatomic landmarks for those articular branches. The femoral nerve and accessory obturator nerve were consistently located between the anterior inferior iliac spine and the iliopubic eminence, and the obturator nerve is found near the inferior, medial acetabulum.6
Building off this anatomic study, Girón-Arango et al.7 recently reported a novel pericapsular nerve group (PENG) block technique that was used before surgery in 5 patients with intracapsular hip fracture. Importantly, they found that all 5 patients had significantly reduced pain scores without any clinically evident quadriceps weakness.7 The purpose of this article is to describe our technique performing the PENG block in patients undergoing elective outpatient hip arthroscopy procedures.
Technique
The senior authors recently began performing the PENG block as routine preoperative regional blockade for the perioperative pain management of orthopaedic patients undergoing elective hip arthroscopy. Hip arthroscopy patients are administered the PENG block before surgery and subsequently undergo general anesthesia with an endotracheal tube for the procedure. Routine medications given perioperatively are acetaminophen 1 g intravenously (IV), ketorolac 30 mg IV, dexamethasone 0.1 mg/kg IV. Ketamine 0.25 mg/kg IV is also administered during surgery at the anesthetist’s discretion. At the end of the procedure, during emergence from anesthesia if required for superficial pain from port sites, small doses of opioids are titrated, or local anesthetic is infiltrated by the surgeon.
The block is performed by the anesthesia provider in the preoperative holding area with the patient in the supine position (Video 1). A positioning aid such as a pillow or blanket is placed below the ipsilateral knee to provide slight hip flexion and decrease tension of the iliopsoas muscles (Fig 1A). The bony landmark of the anterior superior iliac spine (ASIS) is easily palpated and marked as shown in Figure 1B. A SonoSite X-Porte HFL50xp (15-6 MHz; Fujifilm SonoSite, Inc., Tokyo, Japan) linear ultrasound probe is placed in a longitudinal plane over the ASIS (Fig 2) and then aligned with the pubic ramus by rotating the probe 45°. In this view the ASIS, iliopubic eminence, iliopsoas muscle, and tendon are observed, as shown in Figure 3. A 20-gauge, 80 mm needle is inserted from lateral to medial at an angle of approximately 45° to 60° depending on the size of the patient; in an in-plane approach to place the tip in the musculofascial plane between the psoas muscle anteriorly and the pubic ramus posteriorly. Once the ostium is contacted, the needle is rotated to ensure complete penetration through the fascia of the iliopsoas muscle. After negative aspiration, the local anesthetic solution is injected in 5 mL increments while observing for adequate lift and fluid spread in this plane for a total volume of 20 mL (Fig 4). In all cases a single injection of 0.5% ropivacaine with 4 mg dexamethasone is used.
Fig 1.
Pericapsular nerve group block patient positioning. (A) The patient is supine, with his right hip exposed for the block, his head is to the right of the image. Slight hip flexion is achieved from a folded blanket placed behind the knee. (B) The patient is supine with his head to the top of the image, the right ASIS is palpated then marked with a surgical marker to identify the ultrasound starting position. ASIS, anterior inferior iliac spine.
Fig 2.
Pericapsular nerve group block ultrasound probe starting position. (2A) The patient is supine with his head to the top of the image. The linear probe in placed longitudinally over the right ASIS. (2B) The ultrasound view of the right hip with the left side of the image corresponding to the superior pole of the probe with labeled ASIS. ASIS, anterior inferior iliac spine.
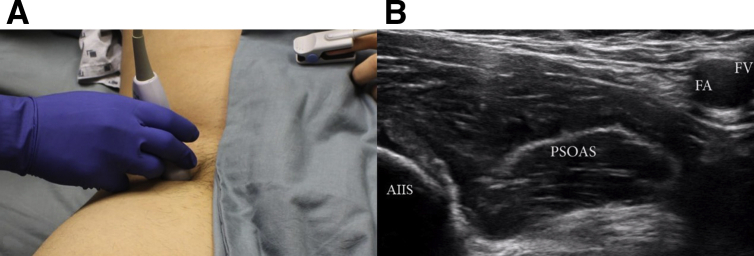
Fig 3.
Pericapsular nerve group block ultrasound probe injection position. (3A) The patient is supine with his head to the top of the image with the probe aligned with right pubic ramus. (3B) The ultrasound view of the right hip with the left of the image corresponds to the now-superolateral pole of the probe. Key anatomic structures are labeled: AIIS, anterior inferior iliac spine; FA, femoral artery; FV, femoral vein; Psoas, psoas tendon.
Fig 4.
Pericapsular nerve group block needle position and trajectory and post injection ultrasound image. (4A) The patient is supine with his head toward the bottom of the image, the probe is aligned with right pubic ramus, and the needle is inserted at a 50° angle from lateral to medial. (4B) The ultrasound view of the right hip, with the left side of the image corresponding to the superolateral pole of the probe. This image is following the 20 mL injection, demonstrating the increased fluid below the psoas tendon. AIIS, anterior inferior iliac spine; Psoas, psoas tendon.
All patients are discharged home the day of surgery and are educated on crutch use before surgery. Patients’ weightbearing status is either nonweightbearing or foot-flat weightbearing depending on the procedure and surgeons’ preference. All patients receive oxycodone IR 5-10 by mouth (PO) mg every 4 hours, acetaminophen 975 mg PO every 8 hours, celecoxib (Celebrex) 200 mg PO daily, aspirin EC 325 mg PO daily, ondansetron 4 mg PO every 4 hours, docusate sodium (Colace) 100 mg PO twice daily, senna 8.6 mg PO daily, and omeprazole (Prilosec) 20 mg PO daily. All patients receive education on the postoperative medications.
Pearls and Pitfalls
Table 1 summarizes the pearls and pitfalls of performing the PENG block. The starting point for this block is critical. If one enters the skin in a far lateral position, the needle often tracks to the AIIS, making it nearly impossible to reach the intended location for delivery. Conversely, starting too medially results in too steep of an angle of approach, making needle visualization more difficult. We have found the best results by using the linear probe to identify the AIIS and then move medially until it is just off the screen to ensure the best needle trajectory.
Table 1.
Pearls and Pitfalls of the PENG Block
| Pearls |
| Patient positioned with hip slightly flexed; takes tension off iliopsoas |
| Use linear US probe |
| Injection start point with needle just medial to AIIS |
| Twist needle once it contacts ostium; ensures you are through muscle |
| Tilt needle lateral just prior to injection; prevents occlusion by bone |
| Pitfalls |
| Avoid start point too far lateral (needle tracks to AIIS) |
| Avoid start point too medial (needle approach too steep for good visualization) |
AIIS, anterior inferior iliac spine; PENG, pericapsular nerve group; US, ultrasound.
Injection pressure with the PENG block are much higher than other blocks, due to the enclosed area for the medication with limited expansion compared to a more superficial location of most other nerve blocks. We try to accommodate for this by flexing the hip to take tension off the iliopsoas, thereby creating a larger potential space. As described above, this is easily done by placing a towel or sheet under the patient’s ipsilateral knee. Also, once the needle passes through the iliopsoas and contacts the ostium, twisting the needle ensures you are through the muscle and not injecting into the iliopsoas muscle. An additional technique trick is to tilt the needle laterally to make sure the needle tip is not occluded by the bone.
Discussion
Unlike most other arthroscopic procedures, the ideal postoperative pain control remains a significant challenge after hip arthroscopy. This is likely due to the complex innervation, significant amount of soft tissue surrounding the hip, as well as the significant amount of axial traction required to allow for instrumentation of the hip joint. In 2016, Yu, et al.8 reviewed multiple different options for anesthesia and analgesia for hip arthroscopy and concluded that the ideal anesthesia has yet to be determined. Although most arthroscopic procedures in the hip are performed with the patient under general anesthesia, spinal anesthesia is becoming more commonly used in lower extremity procedures. However, it may not offer sufficient muscular relaxation to perform adequate joint distraction; in addition, bilateral lower extremity weakness and potential postoperative urinary retention requiring catheterization9 may preclude spinal anesthesia from widespread use in hip arthroscopy.
In 2013, Nye et al.10 reported on the use of a posterior lumbar plexus blockade with indwelling catheter in 213 patients after hip arthroscopy. The nerve block was performed after surgery for continued pain. Two patients went on to develop local anesthetic systemic toxicity, and 1 patient was readmitted for bilateral weakness and numbness caused by epidural spread of the local anesthetic. A total of 20 patients reported some numbness, tingling, or burning in the operative leg. Although 14 were mild and resolved quickly, 6 had symptoms that lasted more than 6 months.10 Given this complication profile, as well as the need for a home indwelling catheter and its associated potential issues, we feel that a plexus block is not the most ideal regional anesthetic modality after hip arthroscopy.
Garner et al.3 performed an RCT comparing a fascia iliaca block with bupivacaine versus infiltration of the portal site with bupivacaine. The study was terminated early, after enrolling only 46 patients, due to significantly increased pain at 1-hour after surgery in the fascia iliaca block group. This increased pain led to higher consumption of opioids, with twice as many patients in the fascia iliaca block group requiring intravenous opioids compared to the local infiltration group. The authors did not find a statistically significant difference in pain scores at any other timepoint in the study.3 Interestingly, based on the anatomy of the hip and portal locations, if the local anesthetic was administered at the deepest point of the portal tracts, it is possible that a portion of the medication was delivered to a similar location as in a pericapsular nerve block.
Girón-Arango et al.7 reported their initial results using the PENG Block in five patients who sustained a hip fracture. They reported improved pain in all five patients, with an average pre block Numeric Rating Scale for pain score of 5.4 to a post block average score of 0.4. Notable, the authors also tested preservation of motor function by having all patients perform a straight leg raise to 15°. All patients were able to perform the leg raise and reported improved pain with leg raise when compared to baseline. Finally, the authors also reported no clinically apparent quadriceps weakness in any patients on physical examination.7
The goal of this Technique article was to demonstrate the feasibility of the PENG block for hip arthroscopy and to show a reproducible technique with recommendations on how to make the procedure as successful as possible. Weakness of this project include the lack of postoperative objective data such as postoperative opioid pill count, opioid analgesia requirements in the recovery room, and verified subjective pain scores. In the future prospective studies including a randomized trial comparing the PENG block to the fascia iliaca block or other reginal anesthesia is still necessary to truly determine the optimum anesthesia for hip arthroscopy. Given its early success in hip fracture patients, the PENG block may be the ideal regional anesthesia modality for hip arthroscopy. It is reproducible, easily performed in the preoperative setting, and appears to spare motor function while providing sensory pain relief. The addition of adjuvants such as epinephrine or dexamethasone or perhaps the use of longer-acting anesthetics may decrease postoperative narcotic demand even more.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates the pericapsular nerve group (PENG) block done before surgery for regional anesthesia and postoperative pain control in a patient undergoing a right hip arthroscopy. The patient is in the supine position with the right hip exposed. The anesthetist is seated to the side of the patient, with the probe in his right hand the needle in his left. The block is performed with ultrasound guidance using a SonoSite X-Porte HFL50xp (15-6MHz) linear ultrasound probe. The ultrasound screen is placed on the opposite side of the patient for easy viewing. The video includes the labeled corresponding ultrasound video performed during the block.
References
- 1.Schairer W.W., Nwachukwu B.U., Suryavanshi J.R., Yen Y.M., Kelly B.T., Fabricant P.D. A shift in hip arthroscopy use by patient age and surgeon volume: A New York State-based population analysis 2004 to 2016. Arthroscopy. 2019;35:2847–2854.e1. doi: 10.1016/j.arthro.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Purcell R.L., Brooks D.I., Steelman T.J. Fascia iliaca blockade with the addition of liposomal bupivacaine versus plain bupivacaine for perioperative pain management during hip arthroscopy: A double-blinded prospective randomized control trial. Arthroscopy. 2019;35:2608–2616. doi: 10.1016/j.arthro.2019.03.056. [DOI] [PubMed] [Google Scholar]
- 3.Garner M., Alshameeri Z., Sardesai A., Khanduja V. A prospective randomized controlled trial comparing the efficacy of fascia iliaca compartment block versus local anesthetic infiltration after hip arthroscopic surgery. Arthroscopy. 2017;33:125–132. doi: 10.1016/j.arthro.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Gardner E. The innervation of the hip joint. Anat Rec. 1948;101:353–371. doi: 10.1002/ar.1091010309. [DOI] [PubMed] [Google Scholar]
- 5.Gerhardt M., Johnson K., Atkinson R. Characterisation and classification of the neural anatomy in the human hip joint. Hip Int. 2012;22:75–81. doi: 10.5301/HIP.2012.9042. [DOI] [PubMed] [Google Scholar]
- 6.Short A.J., Barnett J.J.G., Gofeld M. Anatomic study of innervation of the anterior hip capsule: Implication for image-guided intervention. Reg Anesth Pain Med. 2018;43:186–192. doi: 10.1097/AAP.0000000000000701. [DOI] [PubMed] [Google Scholar]
- 7.Girón-Arango L., Peng P.W.H., Chin K.J., Brull R., Perlas A. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43:859–863. doi: 10.1097/AAP.0000000000000847. [DOI] [PubMed] [Google Scholar]
- 8.Yu H.C., Al-Shehri M., Johnston K.D., Endersby R., Baghirzada L. Anesthesia for hip arthroscopy: a narrative review. Can J Anaesth. 2016;63:1277–1290. doi: 10.1007/s12630-016-0718-7. [DOI] [PubMed] [Google Scholar]
- 9.Frisch N.B., Darrith B., Hansen D.C., Wells A., Sanders S., Berger R.A. Single-dose lidocaine spinal anesthesia in hip and knee arthroplasty. Arthroplast Today. 2018;4:236–239. doi: 10.1016/j.artd.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nye Z.B., Horn J.L., Crittenden W., Abrahams M.S., Aziz M.F. Ambulatory continuous posterior lumbar plexus blocks following hip arthroscopy: a review of 213 cases. J Clin Anesth. 2013;25:268–274. doi: 10.1016/j.jclinane.2012.11.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the pericapsular nerve group (PENG) block done before surgery for regional anesthesia and postoperative pain control in a patient undergoing a right hip arthroscopy. The patient is in the supine position with the right hip exposed. The anesthetist is seated to the side of the patient, with the probe in his right hand the needle in his left. The block is performed with ultrasound guidance using a SonoSite X-Porte HFL50xp (15-6MHz) linear ultrasound probe. The ultrasound screen is placed on the opposite side of the patient for easy viewing. The video includes the labeled corresponding ultrasound video performed during the block.
This video demonstrates the pericapsular nerve group (PENG) block done before surgery for regional anesthesia and postoperative pain control in a patient undergoing a right hip arthroscopy. The patient is in the supine position with the right hip exposed. The anesthetist is seated to the side of the patient, with the probe in his right hand the needle in his left. The block is performed with ultrasound guidance using a SonoSite X-Porte HFL50xp (15-6MHz) linear ultrasound probe. The ultrasound screen is placed on the opposite side of the patient for easy viewing. The video includes the labeled corresponding ultrasound video performed during the block.