Abstract
This study aimed to evaluate the effect of thiamine supplementation on left ventricular (LV) systolic function in patients of alcoholic cardiomyopathy(ACM) presenting with acute heart failure(HF). 11 newly diagnosed patients were included. They were treated with 3 days of intravenous(IV) therapy with thiamine followed by oral supplementation. LVEF was 30% at baseline which improved by 45% and 53% along with reduction in LV dimensions over 3 and 6 months respectively. The study suggests the benefit of thiamine supplementation on LVEF in ACM patients with HF.
Keywords: Alcoholic cardiomyopathy(ACM), Heart failure(HF), Left ventricular end diastolic, diameter(LVEDD), Left ventricular end systolic diameter(LVESD), Thiamine deficiency(TD)
1. Introduction
Alcoholic cardiomyopathy (ACM) is a chronic dilated heart disease with decreased left ventricular ejection fraction(LVEF). Studies have shown thiamine deficiency in patients of acute heart failure.1,2 We evaluated the changes in LVEF with thiamine supplementation in patients of ACM presenting with acute heart failure (HF).
2. Aims & objectives
To study the efficacy of thiamine supplementation along with standard medical therapy in ACM patients and reversibility of left ventricular systolic dysfunction.
3. Methods
3.1. Inclusion criteria
Patients presented with acute heart failure of New York Heart Association (NYHA) functional class 3 or 4 with a history of chronic heavy drinking of alcohol were included in the study.
3.2. Exclusion criteria
-
1.
Ischemic cardiomyopathy
-
2.
Left ventricular ejection fraction (LVEF) > 45%
-
3.
Recent thiamine or multivitamin supplementation
Patients with a first episode of acute heart failure with history of chronic heavy drinking of alcohol i.e, more than 5 years of duration with greater than 80 mg/day were included. Relevant history, electrocardiogram and chest radiograph were taken. Coronary angiogram was performed to rule out ischemic cardiomyopathy. A two dimensional echocardiographic examination was done before starting the treatment with thiamine. After completion of 3 days of intravenous treatment, all patients were given oral thiamine 200 mg/day for a maximum duration of 12 weeks. Patients were evaluated by serial echocardiography.
4. Results
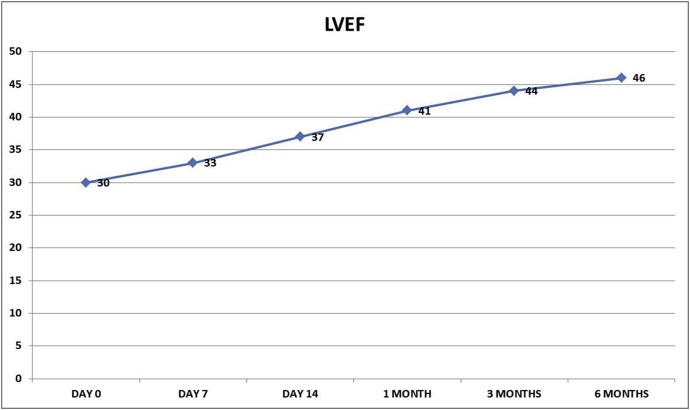
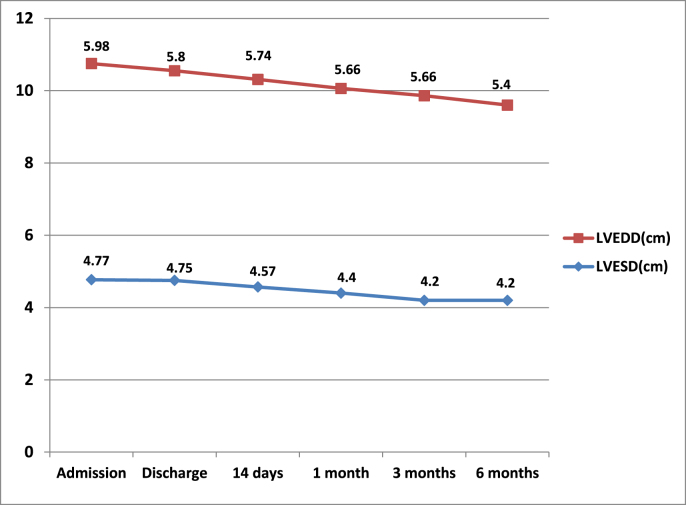
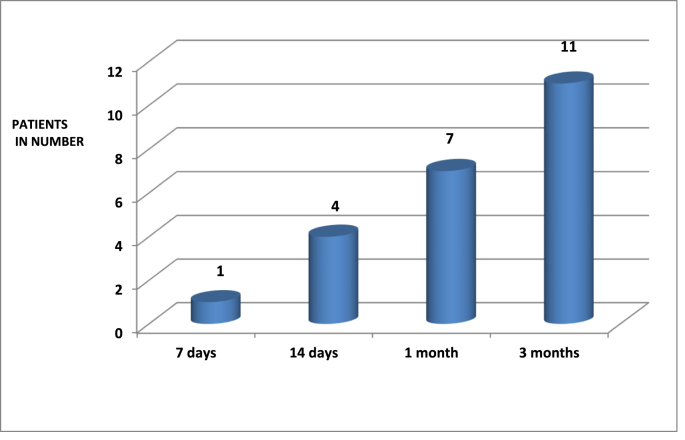
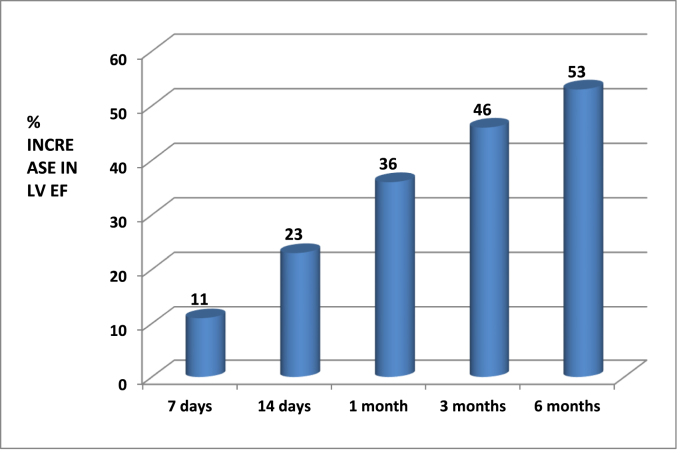
A total of eleven patients were studied. The baseline characteristics are shown in Table 1, Table 2. The average amount of alcohol consumed per day was 60–110 g/day over a mean duration of 14 years. Echocardiographic parameters were studied from admission to 6 months at regular intervals (Table 3). The mean LVEF was 30% at baseline improved to 46% at 6 months follow-up (Fig. 1). At admission LVEDD/LVESD were 5.98 ± 0.32cm/4.77 ± 0.62 cm which improved to 5.4 ± 0.33cm/4,2 ± 0.56 cm at 6 months(Fig. 2). Mitral regurgitation was moderate(2+) in severity at admission which improved to mild(1+) at 6 months. Left atrial size was 3.98 ± 0.49 cm which improved to 3.5 ± 0.3 cm. There was progressive improvement in right ventricular function as assessed by tricuspid annular plane systolic excursion(TAPSE) which was 1.7 ± 0.19 cm at admission to 2 ± 0.1 cm at 6 months and fall in pulmonary artery systolic pressures was 42 ± 8.8mmhg at admission to 31 ± 8.4mmhg at 4 weeks(Table 3). LVEF improved above 40% in 4(36%) at 14 days and in 7(64%) at 1 month and in all 11 patients (100%) by 3 months (Fig. 3) of thiamine supplementation. There was a 23% increase in LVEF at 14 days from that of baseline value and 45%, 53% increase was noted at 3 and 6 months respectively (Fig. 4).
Table 1.
Baseline characteristics of the study population.
| Baseline characteristics | Total (n = 11, male) |
|---|---|
| Breathlessness | 11(100%) |
| Orthopnea | 7(63.6%) |
| Paroxysmal nocturnal dyspnea | 10(90.9%) |
| Jaundice | 3(27%) |
| Pedal edema | 3(27%) |
| Oliguria | 4(36.4%) |
| Age in years(mean) | 44.2 ± 9.2 |
| Alcohol consumed(g/day) | 86.82 ± 10.78 |
| Alcohol consumption duration (yrs) | 14.1 ± 7.57 |
| H/O Hypertension | 6(54.5%) |
| H/O Diabetes | 2(18%) |
| ECG: LVH with strain Left atrial enlargement Right atrial enlargement |
6(54.5%) 7(63.6%) 3(27%) |
Table 2.
Mean values of laboratory parameters among study population.
| Laboratory parameters | Total (n = 11) |
|---|---|
| Hemoglobin(g/100 ml) | 14 ± 1.77 |
| Total leucocyte count(ml) | 9363 ± 250 |
| Platelet count(ml) | 2×105±0.45 |
| Total Bilirubin(mg/100 ml) | 1.4 ± 0.9 |
| SGOT(units/L) | 100 ± 19 |
| SGPT(units/L) | 80 ± 16 |
| ALP(units/L) | 84 ± 18 |
| Blood Urea(mg/100 ml) | 40 ± 1313 |
| Serum creatinine (mg/100 ml) | 1 ± 0.15 |
| CPK(units/L) | 124 ± 7.6 |
| LDH(units/L) | 208 ± 18 |
Table 3.
Echocardiographic parameters in the study population.
| Echocardiogra-phic Parameter | At admission | At Discharge (1 week) | At 14 days | At 1 Month | At 3 Months | At 6 Months |
|---|---|---|---|---|---|---|
| LVEDD(cm) | 5.98 ± 0.32 | 5.8 ± 0.34 | 5.74 ± 0.22 | 5.66 ± 0.25 | 5.5 ± 0.3 | 5.4 ± 0.33 |
| LVESD(cm) | 4.77 ± 0.62 | 4.75 ± 0.51 | 4.57 ± 0.69 | 4.4 ± 0.42 | 4.2 ± 0.55 | 4.2 ± 0.56 |
| LVEF(%) | 30 ± 4 | 33 ± 3.2 | 37 ± 2.77 | 41 ± 4.9 | 44 ± 5.2 | 46 ± 5.7 |
| MR(grade) | 2+ | 2+ | 1+ | 1+ | 1+ | 1+ |
| LA(cm) | 3.98 ± 0.49 | 3.9 ± 0.42 | 3.98 ± 0.4 | 3.64 ± 0.38 | 3.53 ± 0.34 | 3.5 ± 0.3 |
| AORTA(cm) | 2.72 ± 0.4 | 2.7 ± 0.34 | 2.6 ± 0.52 | 2.74 ± 0.31 | 2.8 ± 0.31 | 2.8 ± 0.3 |
| RVSP(mmHg) | 42 ± 8.8 | 39 ± 9.5 | 36 ± 9.6 | 33.6 ± 9.74 | 32.2 ± 9.15 | 31.6 ± 8.4 |
| TAPSE(cm) | 1.7 ± 0.19 | 1.8 ± 0.13 | 1.9 ± 0.14 | 2 ± 0.13 | 2 ± 0.1 | 2 ± 0.05 |
Fig. 1.
Graph showing trends in the improvement of LVEF(%) with thiamine supplementation.
Fig. 2.
Graph showing trends in the change in LV enddiastolic diameter(LVEDD) (cm) and LV endsystolic diameter(LVESD) (cm) on thiamine treatment.
Fig. 3.
Bar diagram showing percentage of patients showing improvement in. LVEF(>40%) on thiamine supplementation.
Fig. 4.
Bar diagram showing percentage of increase in LVEF after thiamine supplementation.
5. Discussion
Alcohol consumption 80 g/day for at least 5 years significantly increases the risk to develop ACM.3 The “total lifetime dose of ethanol” (TLDE) – the amount of ethanol consumed during lifetime expressed in kilograms per kilograms of body weight (kg/kg) correlates with left ventricle dysfunction, detectable in one third of chronic alcohol consumers.3 Alcohol consumption leads to thiamine deficiency by decreasing the transport of thiamine across the intestinal mucosa, impairing capacity of the liver to store thiamine and impairing the phosphorylation of thiamine to the more biological active thiamine diphosphate. Standardisation difficulties, pre-analytical sample preparation (requirement for washed red cells which are not widely available in most biobanks) and sample stability concerns making difficult to assess thiamine levels in patients with suspected thiamine deficiency(TD). TD in HF patients has been observed by Hanninen et al,4 Seligmann et al.,.5 In our study with thiamine addition there was improvement in LVEF in all patients from 30% (baseline) to 44%, 46% at 3 and 6 months respectively.
6. Limitations
-
1.
Small sample size
-
2.
Estimation of levels of serum thiamine was not done
7. Conclusion
This study suggests the role of thiamine supplementation along with standard medical therapy in improvement of LVEF in ACM patients with acute HF. However, to validate these findings, a placebo controlled study with a larger number of patients may be desirable.
Declaration of competing interest
NIL.
References
- 1.Leslie D., Gheorghiade M. Is there a role for thiamine supplementation in the management of heart failure? Am Heart J. 1996;131:1248–1250. doi: 10.1016/s0002-8703(96)90121-0. [DOI] [PubMed] [Google Scholar]
- 2.Piano M.R. Alcoholic cardiomyopathy: incidence, clinical characteristics, and pathophysiology. Chest. 2002;121:1638–1650. doi: 10.1378/chest.121.5.1638. [DOI] [PubMed] [Google Scholar]
- 3.Fernández-Solà J., Nicolás J.M., Paré J.C. Diastolic function impairment in alcoholics. Alcohol Clin Exp Res. 2000;24:1830–1835. [PubMed] [Google Scholar]
- 4.Hanninen S.A., Darling P.B., Sole M.J., Barr A., Keith M.E. The prevalence of thiamine deficiency in hospitalized patients with congestive heart failure. J Am Coll Cardiol. 2006;47:354–361. doi: 10.1016/j.jacc.2005.08.060. [DOI] [PubMed] [Google Scholar]
- 5.Seligmann H., Halkin H., Rauchfleisch S. Thiamine deficiency in patients with congestive heart failure receiving long-term furosemide therapy: a pilot study. Am J Med. 1991;91:151–155. doi: 10.1016/0002-9343(91)90007-k. [DOI] [PubMed] [Google Scholar]