Abstract
Hearing loss is associated with higher health care spending and use, but little is known about the unmet health care needs of people with hearing loss or difficulty. Analysis of 2016 Medicare Current Beneficiary Survey data for beneficiaries ages sixty-five and older reveals that those who reported a lot of trouble hearing in the past year were 49 percent more likely than those who reported no trouble hearing to indicate not having a usual source of care. Compared with those who reported no trouble hearing, those who reported some trouble hearing were more likely to indicate not having obtained medical care in the past year when they thought it was needed, as well as not filling a prescription, with the risk for both behaviors being greater among those reporting a lot of trouble hearing versus a little. Interventions that improve access to hearing services and aid communication may help older Medicare beneficiaries meet their health care needs.
Addressing access to affordable treatment for hearing loss among older adults, after decades of being overlooked, is gaining policy momentum. Notable progress includes the high and growing proportion of Medicare Advantage plans that cover treatment for hearing loss,1 as well as the passage of the Over-the-Counter Hearing Aid Act of 2017, which requires the Food and Drug Administration (FDA) to provide regulations for the over-the-counter sale of hearing aids for mild-to-moderate hearing loss.2
Although important, this progress has limitations. The almost two-thirds of Medicare beneficiaries not enrolled in Medicare Advantage plans do not have access to coverage for hearing treatment, and those who do are still paying the majority of their hearing treatment costs out of pocket.1 In addition, at the time of this writing, the FDA still had not released its guidance for over-the-counter hearing aids, which had a deadline of August 2020. As a result, regulated devices of this type are not yet available.2 With the majority of hearing loss untreated among Medicare beneficiaries,1 it is necessary to gauge the impact that hearing loss may be having on both health outcomes and the quality of care. In this article we examine one way in which it might influence both: as a possible determinant of whether the health care needs of older Medicare beneficiaries are being met.
Background
More than thirty-eight million3 US adults have hearing loss. Its prevalence increases with age, affecting nearly two-thirds of people age seventy or older.4 The number of adults with hearing loss will nearly double to more than seventy million by 2060.5 Nevertheless, a 2013 study found that fewer than 20 percent of adults ages fifty and older owned and used hearing aids.6 And although hearing loss has been independently associated with negative outcomes such as social isolation, loneliness,7 depression,8 and dementia,9 little is known about the association of hearing loss with unmet health needs.
More recent research has explored the impact of hearing loss on health care outcomes and suggests that people with hearing loss incur higher health care costs and experience higher rates of health care use than their peers without hearing loss.10 Specifically, people with hearing loss spent, on average, $22,434 more on health care, had a 17 percent higher risk for an emergency department visit, and had a 44 percent higher risk of experiencing a thirty-day readmission during a ten-year period.10 Further, people with hearing loss are more likely to report lower satisfaction with quality of care.11
The associations between hearing loss and negative health care outcomes noted above might be mediated by the effect of hearing loss on communication.12 Hearing loss creates a barrier to oral communication by limiting and distorting speech (akin to constantly listening to a bad phone signal) and contributes to fatigue and memory impairments.13,14 Barriers are exacerbated in difficult listening situations, such as against high background noise in hospitals15 or reliance on the use of unfamiliar language (for example, medical jargon).16 COVID-19 precautions such as universal masking and increased telehealth use have introduced new barriers in health communication faced by people with hearing loss.17 High-quality patient-provider communication is vital to patient-centered care and is associated with improved health outcomes, treatment understanding, satisfaction with care, and health literacy.18–21
Little is known about how well adults with hearing loss are able to meet their health care needs. The few relevant studies lack generalizability to the US older adult population and may underrepresent adults with hearing loss because of survey methods that limit their participation (for example, they are conducted by telephone).22,23 Importantly, unmet health care needs have negative consequences for receipt of preventive care, and previous research has found them to be associated with poorer health outcomes, increased rates of health care use, and higher costs.24–27
In this article we explore whether older Medicare beneficiaries who self-report difficulty hearing also describe themselves in a manner consistent with having unmet health care needs. Specifically, we examine the relationships between self-perceived hearing trouble and not having a usual source of care, not obtaining needed care, and not filling prescriptions.
Study Data And Methods
DATA SOURCE AND STUDY SAMPLE
This cross-sectional study used data from the Medicare Current Beneficiary Survey (MCBS) 2016 Cost and Use file. Medicare is the federal health insurance program for all US adults ages sixty-five and older, as well as adults younger than age sixty-five with qualifying disabilities and end-stage renal disease. The MCBS provides data on demographic, socioeconomic, health status, medical condition, and health care variables (utilization, access, and satisfaction ratings) for a nationally representative sample of the Medicare population.28 Participants are interviewed in person by a trained interviewer using computer-assisted personal interviewing software on a laptop computer. Participants may respond with the aid of a proxy when necessary (for example, when language problems, disability, or cognitive impairment are present).
In 2016 the full MCBS sample consisted of 14,778 community-dwelling Medicare beneficiaries. Of these, 12,850 completed the “satisfaction with care” and “use of care” modules that included the questions on having a usual source of care, obtaining care, and filling prescriptions. To generate the analytic sample, adults younger than age sixty-five on Medicare (n = 2,203) were excluded because of the complex nature of their health status relative to that of the rest of the Medicare population. In addition, participants with missing data (n = 225) were excluded from analyses. The final analytic sample included 10,422 participants, which represents a population of 44.4 million Medicare beneficiaries after survey weighting.
INDICATORS OF UNMET HEALTH CARE NEEDS
For the present study, the analyses focused on three outcome variables suggestive of unmet health care needs: not having a usual source of care, not obtaining needed medical care, and not filling a prescription. To assess the presence of a usual source of care, participants were asked: “Is there a particular doctor or other health professional, or a clinic you usually go to when you are sick or for advice about your health?” Participants could answer “yes” or “no.” To assess obtaining needed medical care, participants were asked: “During [the past year] did you have any health problem or condition about which you think you should have seen a doctor or other medical person, but did not?” Again, participants could answer “yes” or “no.” Participants were encouraged to “include all types of health problems ranging from minor to serious issues.” Participants who indicated that they had not obtained medical care when they thought they needed it were asked follow-up questions to disclose whether they attempted to see a doctor (“yes” or “no”) and the primary reason behind their inability to obtain care. Last, to assess filling prescriptions, participants were asked: “During [the past year], were any medicines prescribed for you that you did not get? Please include refills of earlier prescriptions as well as prescriptions that were written or phoned in by a doctor.” Participants could answer “yes” or “no.”
FUNCTIONAL HEARING DIFFICULTY
Functional hearing difficulty was identified on the basis of participants’ responses to the MCBS question, “Which statement best describes your hearing [with a hearing aid]?” The available answers were “no trouble,” “a little trouble,” and “a lot of trouble.” Functional hearing difficulty is a measure of self-perceived difficulty that reflects the respondent’s perceived hearing under daily circumstances; therefore, it takes the use of a hearing aid, if applicable, into account and represents the entire hearing process from peripheral signal encoding in the ear to central signal decoding in the brain.
COVARIATES
According to the Andersen-Aday29 behavioral model for health services use, predisposing characteristics, enabling resources, and perceived need factors were included as covariates in our analysis. Predisposing characteristics included demographic variables such as age (categorized in five-year strata), sex, and race/ethnicity. Enabling resources included educational attainment, income-to-poverty ratio, marital status, and enrollment in a Medicare Advantage plan. Medicare Advantage plans are Medicare plans offered by private companies that cover Medicare Parts A and B benefits and may include coverage for dental, vision, and hearing services and prescription drugs. Medicare Advantage plans also differ with respect to requirements for accessing services (for example, prior authorization).1 Perceived need factors included self-reported general health status compared with others of the same age, functional limitations defined by the number of activities of daily living the participant could not complete without help, self-reported depression based on ever being diagnosed by a doctor, and chronic comorbidities count (categorized as ever being diagnosed with zero, one to two, three to five, or six or more of the following conditions: cancer, chronic obstructive pulmonary disease or asthma, chronic heart disease, depression, mental or psychiatric disorder other than depression, acute myocardial infarction, hypertension, diabetes, stroke, arthritis, dementia, or Alzheimer disease).
STATISTICAL ANALYSIS
Descriptive analyses were used to explore proportional distributions of covariates and outcome variables by functional hearing difficulty. Multivariable logistic regression was used to model the association between functional hearing difficulty and unmet needs variables (not having a usual source of care, not obtaining needed medical care, and not filling prescriptions), with no trouble hearing as the reference group (“no trouble” versus “a little trouble” and “no trouble” versus “a lot of trouble”), while adjusting for confounding variables. The beta-coefficients (log-odds) were converted into odds ratios for ease of interpretation. Significance testing for all analyses was two-sided with a type I error of 0.05. Survey weights were applied according to Centers for Medicare and Medicaid Services recommendations for the MCBS to account for oversampling of subpopulations and cluster sampling design.30 The full model results are in the online appendix.31 The statistical software used was Stata, version 15.
LIMITATIONS
This study had several important limitations related to the nature of the MCBS Cost and Use data. The cross-sectional nature of the study prevented us from exploring temporal trends. It is also notable that survey participants may have relied on proxies to respond to the survey, suggesting that some of the responses may reflect the proxy’s perceptions. Moreover, the reliance of self-reported hearing may underestimate the actual overall prevalence of hearing loss.32 However, the current study was strengthened by using functional hearing ability (that is, with a hearing aid if applicable) as opposed to unassisted hearing ability. Functional hearing ability represents perceptions under daily circumstances, consistent with a disability framework approach. Nonetheless, there was the potential for bias, as both unmet health care needs and functional hearing loss were based on self-report, and any unmeasured characteristic that affects help-seeking behaviors may similarly affect how one self-reports trouble hearing. Moreover, self-report hearing versus clinically measured hearing represent different constructs and may be differentially associated with help-seeking behaviors. Because a functional approach to assessing hearing loss was taken, whether hearing aids influenced the current findings could not be determined. Notably, hearing aid use is so highly associated with protective socioeconomic variables for our study outcomes that it would be difficult to disentangle observed effects.
Finally, the MCBS file did not include information on the nature of the health care services or prescriptions that respondents did not obtain. Therefore, it was impossible to evaluate the severity of those conditions or to determine whether the forgone care (visit, medication, or both) could have involved hearing care.
Study Results
DESCRIPTION OF ANALYTIC SAMPLE
Exhibit 1 displays the characteristics of the weighted sample by functional hearing status. Among the weighted sample, 54.42 percent reported no trouble hearing, whereas 39.87 percent and 5.71 percent reported a little and a lot of trouble hearing, respectively. Medicare beneficiaries with either a little or a lot of hearing loss were proportionally older compared with those with no trouble hearing and tended to be non-Hispanic White males. Moreover, those with a lot of trouble hearing reported lower education levels and were less likely to be married relative to those with a little or no trouble hearing. Overall, Medicare beneficiaries who reported hearing trouble were more likely to report poorer general health, more functional limitations, and a higher count of chronic comorbidities.
EXHIBIT 1.
Demographic and socioeconomic characteristics of Medicare Current Beneficiary Survey (MCBS) respondents, by self-reported functional hearing difficulty, 2016
| Percent by level of functional hearing difficulty | ||||
|---|---|---|---|---|
| Characteristics | Percent of total sample (N = 10,422) | No trouble hearing (n = 5,264)a | A little trouble hearing (n = 4,406)b | A lot of trouble hearing (n = 752)c |
| No usual place of care | 5.72 | 5.90 | 5.26 | 7.19 |
| Not obtaining medical care | 8.93 | 7.09 | 10.67 | 14.33 |
| Not filling prescription | 5.88 | 5.10 | 6.77 | 7.03 |
| Age, years | ||||
| 65–69 | 34.59 | 38.61 | 31.09 | 20.64 |
| 70–74 | 25.37 | 26.67 | 24.34 | 20.93 |
| 75–79 | 17.23 | 17.28 | 17.32 | 15.75 |
| 80–84 | 11.68 | 9.78 | 13.93 | 14.47 |
| 85–89 | 7.12 | 5.31 | 8.55 | 14.41 |
| 90+ | 4.02 | 2.35 | 4.94 | 13.80 |
| Female | 55.03 | 61.11 | 48.63 | 41.82 |
| Race/ethnicity | ||||
| Non-Hispanic White | 78.21 | 73.86 | 83.56 | 82.35 |
| Non-Hispanic Black | 8.86 | 10.65 | 6.74 | 6.51 |
| Hispanic | 7.45 | 9.33 | 4.99 | 6.70 |
| Other | 5.48 | 6.15 | 4.71 | 4.44 |
| Educational attainment | ||||
| Less than high school | 15.74 | 15.79 | 14.13 | 26.49 |
| High school graduate | 25.45 | 25.10 | 25.37 | 29.39 |
| Vocational, some college, associate’s degree | 29.03 | 28.61 | 29.86 | 27.14 |
| Bachelor’s or higher degree | 29.78 | 30.50 | 30.63 | 16.97 |
| Income-to-poverty ratio | ||||
| <100% | 11.19 | 12.41 | 9.12 | 14.02 |
| 101–200% | 23.84 | 23.39 | 23.01 | 33.87 |
| >200% | 64.97 | 64.20 | 67.87 | 52.10 |
| Currently married | 57.35 | 56.57 | 59.29 | 51.28 |
| Medicare Advantage enrollee | 36.38 | 37.60 | 34.86 | 35.43 |
| General health | ||||
| Excellent | 19.54 | 22.22 | 17.47 | 8.61 |
| Very good | 32.93 | 34.02 | 32.60 | 24.83 |
| Good | 30.15 | 29.52 | 30.92 | 30.66 |
| Fair | 13.33 | 11.10 | 14.56 | 25.99 |
| Poor | 4.06 | 3.16 | 4.45 | 9.92 |
| Functional limitations | ||||
| None | 74.74 | 79.79 | 71.56 | 48.80 |
| 1 | 11.85 | 9.88 | 13.53 | 18.82 |
| 2+ | 13.41 | 10.32 | 14.91 | 32.39 |
| Chronic comorbidities count | ||||
| None | 10.20 | 12.13 | 8.36 | 4.71 |
| 1–2 | 42.91 | 46.64 | 40.12 | 26.89 |
| 3–5 | 38.19 | 33.94 | 42.49 | 48.67 |
| 6+ | 8.69 | 7.29 | 9.03 | 19.73 |
SOURCE Authors’ analysis of data from the MCBS, 2016.
NOTE Survey weights were applied according to MCBS instructions.
54.42% of weighted sample.
39.87% of weighted sample.
5.71% of weighted sample.
USUAL SOURCE OF CARE
Exhibit 2 displays the adjusted odds of survey participants who reported not having a usual source of medical care. Compared with participants with no trouble hearing, those with a little trouble hearing had similar odds (odds ratio: 1.038; 95% confidence interval: 0.814, 1.322) of not having a usual source of care, whereas those with a lot of perceived trouble hearing had 49 percent increased odds (OR: 1.489; 95% CI: 1.034, 2.143) of not having a usual source of care. The full results of the model are in appendix exhibit A.31 Among other factors, being female, having higher education, having higher income, being married, and being enrolled in Medicare Advantage were associated with reduced odds of not having a usual source of care.
EXHIBIT 2.
Odds of reporting three outcome variables suggesting unmet health care needs among Medicare beneficiaries, by self-reported functional hearing difficulty, 2016
| Odds ratios for outcome variables | |||
|---|---|---|---|
| Level of functional hearing difficulty | No usual source of care | Not obtaining needed medical care | Not filling a prescription |
| No trouble hearing | Ref | Ref | Ref |
| A little trouble hearing | 1.038 | 1.595**** | 1.440*** |
| A lot of trouble hearing | 1.489** | 1.854**** | 1.556** |
SOURCE Authors’ analysis of data from the Medicare Current Beneficiary Survey (MCBS), 2016.
NOTES Survey weights were applied according to MCBS instructions. Logistic regression models were adjusted for age, sex, race/ethnicity, educational attainment, income-to-poverty ratio, marital status, Medicare Advantage plan, general health, functional limitations, and comorbidity count.
p < 0.05
p < 0.01
p < 0.001
OBTAINING NEEDED MEDICAL CARE
Compared with beneficiaries with no trouble hearing, those with either a little trouble (OR: 1.595; 95% CI: 1.322, 1.924) or a lot of trouble (OR: 1.854; 95% CI: 1.446, 2.376) hearing had 60 percent and 85 percent higher odds of not obtaining medical care when needed, respectively (exhibit 2). The full results of the model are in appendix exhibit B.31 Among those who did not obtain medical care, only 38.09 percent reported that they had attempted to see a doctor. Descriptive analyses revealed that 41.87 percent of those with no trouble hearing attempted to see a doctor, compared with 34.24 percent of those with a little trouble and 40.33 percent of those with a lot of trouble hearing.
Exhibit 3 displays the reasons given for not obtaining medical care by hearing trouble status. The most commonly cited reason for not obtaining care was that participants “did not think the problem was serious” (31.25 percent of those with a lot of trouble hearing, 39.96 percent of those with a little trouble hearing, and 35.10 percent of those with no trouble hearing). Notably, a higher proportion of those with a lot of trouble hearing reported that they “thought the doctor couldn’t do much about the problem” (19.11 percent) compared with those with either a little trouble hearing (11.23 percent) or no trouble hearing (13.09 percent). A higher proportion of those with no trouble hearing (12.57 percent) reported that they “thought it would cost too much” compared with those with either a little trouble hearing (7.83 percent) or a lot of trouble hearing (7.41 percent).
EXHIBIT 3. Main reasons indicated by Medicare beneficiaries who reported not obtaining needed medical care in the past year, by self-reported functional hearing difficulty, 2016.
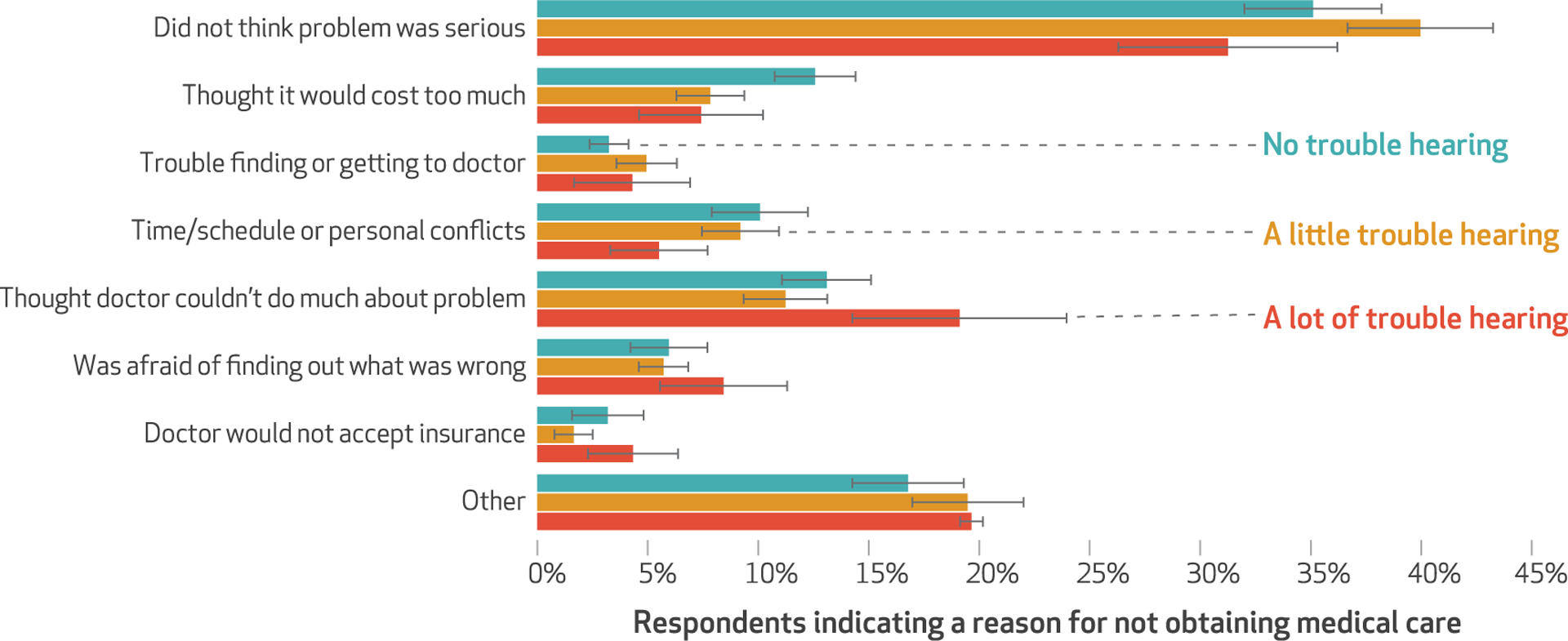
source Authors’ analysis of data from the Medicare Current Beneficiary Survey (MCBS), 2016. notes Survey weights were applied according to MCBS instructions. Error bars represent standard errors.
FILLING PRESCRIPTIONS
Medicare beneficiaries with a little trouble hearing were 44.0 percent more likely (OR: 1.440; 95% CI: 1.102, 1.882) to not fill their prescriptions relative to those with no trouble hearing, and those with a lot of trouble hearing were 55.6 percent more likely (OR, 1.556; 95% CI: 1.044, 2.318) to not fill their prescriptions relative to those with no trouble hearing (exhibit 2). The full results of the model are in appendix exhibit B.31
Discussion
This work builds on previous research by characterizing the association of functional hearing difficulty and not having a usual source of care, not obtaining needed medical care, and not filling prescriptions in a nationally representative sample of older Medicare beneficiaries. There was a consistent dose-response relationship across models whereby those who reported a lot of trouble hearing had higher odds of unmet needs compared with those who reported a little trouble hearing. Taken together, these findings suggest that among Medicare beneficiaries age sixty-five or older, those with perceived hearing difficulty were more likely to have unmet health care needs than those without hearing difficulty. This work highlights an often overlooked, potentially modifiable risk factor for unmet health needs and adds to the understanding of the association between hearing and health care services.
LINKING HEARING LOSS AND DIFFICULTY TO UNMET NEEDS
A usual source of care is a marker of higher-quality interaction with the health care system and is associated with better health outcomes and health care use patterns, including the use of preventive care services.24–26 In this study we found that hearing difficulty was associated with decreased odds of having a usual source of care. Previous studies in this area have focused on socioeconomic and demographic factors or lumped hearing loss in with other disabilities.26,33 The observed association between functional hearing difficulty and the lack of a usual source of care may help explain previous work suggesting a higher risk for emergency department visits and higher health care spending among adults with hearing loss.10 Without a usual source of care, such adults may be less likely to take preventive measures to treat problems early, resulting in high-cost emergency department visits.
In a 2016 study of Finnish adults,23 those with self-reported difficulties hearing conversations had 70 percent higher odds of having perceived unmet health needs specifically defined as desiring but not receiving care for a chronic illness. In the same study the clinical measurement of hearing loss by pure-tone audiometry, which is the clinical standard of measuring hearing loss by finding an person’s lowest threshold at which they respond to a tone, was not associated with unmet needs. Similarly, in an analysis of data from the Wisconsin Longitudinal Study,22 people with self-reported functional hearing trouble had 85 percent higher odds of reporting difficulties accessing health care. The observed coefficients in previous studies are similar to those we found among Medicare beneficiaries with a lot of trouble hearing in the current study.
The current study expands on previous work by including an ordinal scale of functional hearing difficulty (that is, including those with a little and a lot of trouble hearing) that offers a view into a dose-response impact of greater hearing trouble, as well as using a nationally representative sample that is generalizable to older Medicare beneficiaries. Moreover, this work adds a descriptive exploration of reasons given by participants for not obtaining needed health care that suggests that those with a lot of trouble hearing may have diminished faith in the capabilities of health care providers as a reason for not obtaining care, as opposed to an access issue such as cost.
Our work is also novel in characterizing the association of filling prescriptions and hearing difficulty among Medicare beneficiaries. Hearing data, although available, have not been included in previous analyses of correlates of filling prescriptions in the MCBS population.34 Our observed association may be related to patient-provider communication barriers, as previous work has reported that reasons for patients not filling their prescriptions include having unanswered concerns about medications after the prescriptions were written.35 Importantly, not filling prescriptions may serve as a proxy for lack of adherence to treatment that could mediate the association of hearing loss and poor health care use outcomes observed in previous studies, such as thirty-day readmissions.10
HEARING LOSS AND THE HEALTH CARE DYNAMIC
Observed associations between level of hearing difficulty and outcomes that suggest unmet health care needs in the current study might be explained by barriers in access to providers and pharmacies. Notably, using the telephone to schedule appointments or discuss medications may be difficult for adults with hearing loss. In addition, prior research indicates that previous dissatisfaction11 with care may result in adults with hearing loss being less likely to retain their usual source of care or to engage with their providers in the future when medical care is needed. It is plausible that continued communication problems with providers as a result of hearing loss contribute to confusion, frustration, and poor treatment understanding, which could result in poorer overall health outcomes and reduced confidence in health care providers. This could culminate in changes in help-seeking behavior. Medicare beneficiaries with hearing loss often cite communication with providers as a reason for accompaniment to medical appointments.36 In addition, it is possible that hearing loss’s association with psychosocial outcomes such as social isolation7 and depression8 may mediate these associations by modifying willingness to interact with society in general.
FUTURE RESEARCH
Future research could use gold-standard clinical measures of hearing loss and longitudinal data to further explore the nature of this relationship and perform mediation analyses to explain pathways linking hearing loss and unmet health needs among older Medicare beneficiaries. Such work could quantify the interactions and additive effect of hearing loss with other known risk factors for unmet health needs. Future work should assess the use of different hearing interventions (for example, hearing aids or hospital-based accommodations) in observational and randomized controlled trial settings to assess whether addressing hearing loss improves these outcomes.
Implications For Policy And Practice
Our findings have implications for health care planning and delivery, as well as for present and future policy. The positive, dose-dependent association we observed between hearing difficulty and unmet health care needs may place older Medicare beneficiaries with hearing loss at risk for poorer outcomes and higher health expenditures.10,24,26 Insurers and health systems may wish to test whether new incentives or interventions to improve access to hearing care and the health care experience among older adults with hearing loss represent areas for cost savings.
In identifying potential interventions, an important consideration is that unlike other factors associated with unmet health care needs, hearing loss is modifiable with low-risk interventions. Hence, numerous strategies with the potential to modify the observed associations between hearing and unmet medical needs should be tried in the older Medicare population. Among these are systematic approaches to the identification of hearing loss, communication training for providers, support and training programs for caregivers, provision of amplifiers in health care settings, use of captioning and web-based support services, and environmental modifications to reduce noise.12,17
Moreover, rethinking service delivery models to provide better access to hearing care could lead to increased hearing aid use and improved interactions between providers and patients with hearing loss. However, policy efforts to increase access to affordable hearing treatment through the Over-the-Counter Hearing Aid Act of 2017 have stalled, as the FDA missed the statutory deadline in August 2020 to announce the regulations for the over-the-counter sale of hearing aids to treat mild-to-moderate hearing loss.2 In the absence of these regulations, older adults are left with three options: prescribed hearing aids (the average cost of a pair was $4,700 in 2016);37 less expensive and nonprescription, but unregulated, personal sound amplification products of varying effectiveness;38 and doing without. Policy makers should consider ways to expedite the FDA’s guidance to ensure that progress continues on the accessibility of affordable, effective, and safe options for hearing treatment.
In the absence of more affordable and safe solutions, the expansion of coverage options available in Medicare Advantage plans has offered financial protection from the high costs of hearing care.1 Medicare Advantage plans, which are paid a capitated amount to cover Medicare Parts A and B services, are incentivized to ensure that health care needs are met in a timely manner to avoid costly avoidable hospitalizations. In the context of this study’s findings that older adults with hearing difficulty are at higher odds of not obtaining medical care, Medicare Advantage plans should consider ways to ensure that those with perceived hearing trouble are accessing hearing treatment with the available benefits. Studies suggest that the hearing benefits in Medicare Advantage plans are relatively limited, with beneficiaries still paying 79 percent of the costs of hearing care out of pocket, on average.1 This coverage might not be sufficient to improve access to hearing treatment. Studying the impact of different Medicare Advantage plans represents a future area for policy researchers.
Conclusion
This study reports on the increased odds of experiencing unmet health care needs for those with a little and a lot of perceived hearing trouble. Unmet health care needs may reflect attributes of individual preferences, available resources, and structural barriers. Creating an age-friendly health care system requires greater recognition and engagement from practitioners and policy makers on the importance of hearing loss to the health care system, how it contributes to unmet needs for health care, and the progress required to address it.
Supplementary Material
Acknowledgments
Aspects of this research were presented as part of a seminar at the 2020 Gerontological Society of America Annual Scientific Meeting (virtual), November 4–7, 2020. This research was supported by a grant to Nicholas Reed from the National Institute on Aging (Grant No. K23AG065443). Reed also reports being a scientific advisory board member with no financial interest for Shoebox Inc. and Good Machine Studio. Frank Lin reports receiving personal fees from Boehringer-Ingelheim; Autifony, Inc.; Frequency Therapeutics; and Caption Call outside the submitted work and being the director of a research center funded in part by a philanthropic gift from Cochlear Ltd. to the Johns Hopkins Bloomberg School of Public Health, as well as a board member of the nonprofit Access HEARS. Lauren Ferrante was supported by a Paul B. Beeson Emerging Leaders Career Development Award in Aging (K76 AG057023) and the Yale Claude D. Pepper Older Americans Independence Center (P30 AG021342), National Institute on Aging, during the conduct of the study. Sharon Inouye is supported by Grant Nos. R24AG054259 and P01AG031720 from the National Institute on Aging and holds the Milton and Shirley F. Levy Family Chair at Hebrew SeniorLife/Harvard Medical School. Amber Willink reports receiving funding support from the Commonwealth Fund as well as funding from the Cochlear Center for Hearing and Public Health at the Johns Hopkins Bloomberg School of Public Health. Willink also reports receiving a speaker honorarium from the American Speech-Language-Hearing Association (2019) and consulting honorarium from BioMedical Insights (2020).
Contributor Information
Nicholas S. Reed, Department of Epidemiology and in the Cochlear Center for Hearing and Public Health, both at the Johns Hopkins Bloomberg School of Public Health, in Baltimore, Maryland..
Lama Assi, Cochlear Center for Hearing and Public Health, Johns Hopkins Bloomberg School of Public Health..
Wakako Horiuchi, John A. Burns School of Medicine, University of Hawaii, in Honolulu, Hawaii..
Julie E. Hoover-Fong, McKusick-Nathans Institute of Genetic Medicine, Department of Genetic Medicine, and the director of the Kathryn and Alan C. Greenberg Center for Skeletal Dysplasias, both at Johns Hopkins School of Medicine, in Baltimore, Maryland..
Frank R. Lin, Department of Otolaryngology–Head and Neck Surgery, Johns Hopkins School of Medicine, and director of the Cochlear Center for Hearing and Public Health, Johns Hopkins Bloomberg School of Public Health..
Lauren E. Ferrante, Section of Pulmonary, Critical Care, and Sleep Medicine, Department of Internal Medicine, Yale School of Medicine, in New Haven, Connecticut..
Sharon K. Inouye, Department of Medicine, Beth Israel Deaconess Medical Center and Harvard Medical School, and the director of the Aging Brain Center in the Hinda and Arthur Marcus Institute for Aging Research, Hebrew SeniorLife, both in Boston, Massachusetts..
Edgar R. Miller, III, Department of Medicine, Johns Hopkins School of Medicine..
Emily F. Boss, Department of Otolaryngology–Head and Neck Surgery, Johns Hopkins School of Medicine..
Esther S. Oh, Department of Medicine, Johns Hopkins School of Medicine..
Amber Willink, Menzies Centre for Health Policy and Economics, University of Sydney, in New South Wales, Australia..
NOTES
- 1.Willink A, Reed NS, Swenor B, Leinbach L, DuGoff EH, Davis K. Dental, vision, and hearing services: access, spending, and coverage for Medicare beneficiaries. Health Aff (Millwood). 2020;39(2):297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franck KH, Rathi VK. Regulation of over-the-counter hearing aids—deafening silence from the FDA. N Engl J Med. 2020;383(21): 1997–2000. [DOI] [PubMed] [Google Scholar]
- 3.Goman AM, Lin FR. Prevalence of hearing loss by severity in the United States. Am J Public Health. 2016; 106(10):1820–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med. 2011;171(20):1851–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goman AM, Reed NS, Lin FR. Addressing estimated hearing loss in adults in 2060. JAMA Otolaryngol Head Neck Surg. 2017;143(7):733–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chien W, Lin FR. Prevalence of hearing aid use among older adults in the United States. Arch Intern Med. 2012;172(3):292–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shukla A, Harper M, Pedersen E, Goman A, Suen JJ, Price C, et al. Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngol Head Neck Surg. 2020;162(5):622–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brewster KK, Ciarleglio A, Brown PJ, Chen C, Kim HO, Roose SP, et al. Age-related hearing loss and its association with depression in later life. Am J Geriatr Psychiatry. 2018;26(7):788–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol. 2011;68(2): 214–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reed NS, Altan A, Deal JA, Yeh C, Kravetz AD, Wallhagen M, et al. Trends in health care costs and utilization associated with untreated hearing loss over 10 years. JAMA Otolaryngol Head Neck Surg. 2019;145(1):27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reed NS, Boss EF, Lin FR, Oh ES, Willink A. Satisfaction with quality of health care among Medicare beneficiaries with functional hearing loss. Med Care. 2021;59(1):22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shukla A, Nieman CL, Price C, Harper M, Lin FR, Reed NS. Impact of hearing loss on patient-provider communication among hospitalized patients: a systematic review. Am J Med Qual. 2019;34(3):284–92. [DOI] [PubMed] [Google Scholar]
- 13.Hornsby BWY, Naylor G, Bess FH. A taxonomy of fatigue concepts and their relation to hearing loss. Ear Hear. 2016;37 Suppl 1(Suppl 1): 136S–44S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wingfield A, Tun PA, McCoy SL. Hearing loss in older adulthood: what it is and how it interacts with cognitive performance. Curr Dir Psychol Sci. 2005;14(3):144–8. [Google Scholar]
- 15.Busch-Vishniac IJ, West JE, Barnhill C, Hunter T, Orellana D, Chivukula R. Noise levels in Johns Hopkins Hospital. J Acoust Soc Am. 2005; 118(6):3629–45. [DOI] [PubMed] [Google Scholar]
- 16.Cudmore V, Henn P, O’Tuathaigh CMP, Smith S. Age-related hearing loss and communication breakdown in the clinical setting. JAMA Otolaryngol Head Neck Surg. 2017; 143(10):1054–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reed NS, Ferrante LE, Oh ES. Addressing hearing loss to improve communication during the COVID-19 pandemic. J Am Geriatr Soc. 2020;68(9):1924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8): 826–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hironaka LK, Paasche-Orlow MK. The implications of health literacy on patient-provider communication. Arch Dis Child. 2008;93(5):428–32. [DOI] [PubMed] [Google Scholar]
- 20.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. [DOI] [PubMed] [Google Scholar]
- 21.Levy H, Janke A. Health literacy and access to care. J Health Commun. 2016;21 Suppl 1(Suppl):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pandhi N, Schumacher JR, Barnett S, Smith MA. Hearing loss and older adults’ perceptions of access to care. J Community Health. 2011;36(5): 748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mikkola TM, Polku H, Sainio P, Koponen P, Koskinen S, Viljanen A. Hearing loss and use of health services: a population-based cross-sectional study among Finnish older adults. BMC Geriatr. 2016;16(1):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ettner SL. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health. 1996; 86(12):1748–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spatz ES, Ross JS, Desai MM, Canavan ME, Krumholz HM. Beyond insurance coverage: usual source of care in the treatment of hypertension and hypercholesterolemia. Data from the 2003–2006 National Health and Nutrition Examination Survey. Am Heart J. 2010;160(1):115–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93(5):786–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hargreaves DS, Elliott MN, Viner RM, Richmond TK, Schuster MA. Unmet health care need in US adolescents and adult health outcomes. Pediatrics. 2015;136(3):513–20. [DOI] [PubMed] [Google Scholar]
- 28.Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Financ Rev. 1994;15(4):153–63. [PMC free article] [PubMed] [Google Scholar]
- 29.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3): 208–20. [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Medicare and Medicaid Services, Office of Enterprise Data and Analytics. Medicare Current Beneficiary Survey 2016: methodology report [Internet]. Baltimore (MD): CMS; 2018. Nov 16 [cited 2021 Mar 30]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/Downloads/MCBS2016MethodReport508.pdf [Google Scholar]
- 31.To access the appendix, click on the Details tab of the article online.
- 32.Goman AM, Reed NS, Lin FR, Willink A. Variations in prevalence and number of older adults with self-reported hearing trouble by audiometric hearing loss and socio-demographic characteristics. JAMA Otolaryngol Head Neck Surg. 2020; 146(2):201–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nothelle SK, Boyd C, Sheehan O, Wolff JL. Factors associated with loss of usual source of care among older adults. Ann Fam Med. 2018;16(6): 538–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kennedy J, Tuleu I, Mackay K. Unfilled prescriptions of Medicare beneficiaries: prevalence, reasons, and types of medicines prescribed. J Manag Care Pharm. 2008;14(6): 553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Serv Res. 2012;12:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reed NS, Assi L, Pedersen E, Alshabasy Y, Deemer A, Deal JA, et al. Accompaniment to healthcare visits: the impact of sensory impairment. BMC Health Serv Res. 2020;20(1):990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Academies of Sciences, Engineering, and Medicine. Hearing health care for adults: priorities for improving access and affordability. Washington (DC): National Academies Press; 2016. [PubMed] [Google Scholar]
- 38.Reed NS, Betz J, Kendig N, Korczak M, Lin FR. Personal sound amplification products vs a conventional hearing aid for speech understanding in noise. JAMA. 2017;318(1): 89–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


