Abstract
Introduction
As a result of high transmission and mortality rates, the Covid-19 pandemic has led to a worldwide health crisis, isolation, and widespread fear, therefore negatively influencing people’s quality of life (QOL). The goal of the present study was to examine the psychometric properties (validity and reliability) of the Persian version of the COVID-19-Impact on Quality of Life (COV19-QoL) scale.
Methods
After translating the scale using the forward–backward method, face and content validly was qualitatively assessed. Then the scale was distributed to 488 individuals from the general population via online platforms. Construct validity was assessed using exploratory (EFA) and confirmatory (CFA) factor analysis. In addition, internal consistency was examined using Cronbach’s alpha coefficient and McDonald’s omega, relative stability was assessed using interclass correlation coefficient (ICC), and absolute stability was calculated through examination of standard error of measurement.
Results
The EFA revealed one factor that explained 55.96% of the total variance of the scale. Internal consistencies of 0.823 and 0.882 were found using Cronbach’s alpha coefficient and McDonald’s omega, respectively. In addition, an ICC of 0.837 (with a two-week interval) was found. Covid-19 had a greater impact on the QOL of healthy participants than that of those with underling conditions (p = 0.004), and also on the QOL of single participants than that of married ones (p = 0.032).
Conclusion
The Persian version of the COV19-QoL is a valid and reliable instrument that can be used to examine the impact of Covid-19 on QOL.
Keywords: Psychometric properties, QOL, Covid-19
Introduction
On December 2019, the outbreak of an unknown pneumonia was reported in Wuhan, China (1). Shortly after, the new coronavirus (SARS-CoV-2) was confirmed as the cause of the pandemic in China and many other parts of the world (2). On January 30, 2020, the world health organization (WHO) declared the pandemic a public health emergency (3). On March 24, 2020, the number of COVID-19 confirmed cases and deaths were 372,755 and 16,231, respectively; by April 18, 2020, these increased to 2,160,207 and 146,088, respectively (4).
The fast prevalence of COVID-19 and the high death rates has led to widespread anxiety (5), fear and panic (6), psychological distress (7), depression (8), Post-traumatic stress symptoms (9), insomnia (10) and even stigma and xenophobia towards suspected cases (11). Many of these fears are related to getting the virus, losing loved ones, lack of medical treatment, and issues related to staying at home, unemployment, and job loss that lead to psychological disorders, and in some cases suicide (12, 13). A study conducted in India found a significant association between hours spent on watching news on COVID-19 and level of distress and anxiety experienced (14). In addition, false information about COVID-19, travel ban, and quarantine all can affect people’s psychological health (15). Therefore, governments should focus on disseminating unbiased COVID-19 knowledge, teaching the correct methods of restraint, providing basic services and goods, and adequate financial support (16).
The pandemic has led to closure of schools and jobs, financial vulnerability, and loss of many jobs (17), and has created many problems for people around the world. The results of various studies have shown that lockdown and social distancing have led to psychological distress in people (especially women, the elderly and people with many children) and had adverse effects on economic well-being and quality of life (18, 19). Some precautionary measures, such as compulsory face mask policies, depended on communities' previous experience with epidemics. For instance, due to the previous experience of the Chinese people in the SARS epidemic in 2003, the use of masks in the Chinese people was more than in Poland, while the use of masks in Poland was considered stigma (20).
Different aspects of daily life and people’s quality of life (QOL) have been affected by the rapid spread of the virus. QOL is a subjective, multidimensional, and personal concept that is defined as one’s perception of their life, values, objectives, standards, and interests, and refers to one’s attitude towards the difference between what is and what ought to be (21, 22). As a result of unprecedented death rates, unemployment, and isolation, life has become harder for many people during the pandemic (23). It is clear that from now on the world has to live with this virus; therefore, QOL and other psychological and demographic issues related to it should be examined, so that proper measures can be taken. Some studies have examined QOL using general instruments, such as the SF-36 (24, 25) and the SF-12 (26). Some other studies have used instruments measuring psychological problems and social support that do not seem to properly assess QOL (2, 27). Therefore, it seems necessary to have a scale specifically assessing QOL. The COVID-19–Impact on Quality of Life (COV19-QoL) scale is a standard and specific scale for assessing QOL during the COVID-19 pandemic that was developed by Repišti et al. It has good validity and reliability, and assesses the main dimensions of QOL in the general population (28). The goal of the present study is to examine the psychometric properties (validity and reliability) of the Persian version of the COV19-QoL.
Methods
Study design and environment
This is a methodological, cross-sectional study aimed at examining the psychometric properties (validity and reliability) of the COV19-QoL in the Iranian general population in 2020. The scale was distributed to the participants via online platforms.
Sample size and participants
The minimum sample size required to perform exploratory factor analysis is 3 to 10 samples per item. There is debate on the proper sample size for EFA. Some researchers suggest that 5–10 participants are needed per item. However, sample sizes of 150–300 and even 300–500 participants have also been suggested (29). In conducting a confirmatory factors analysis (CFA), sample size should not be lower than 200 (30). In the present study, the sample included 488 participants who were randomly divided into two groups, a 288-memebr group for the EFA and a 200-memebr group for the CFA.
Procedure
Participants were recruited in the study using anonymous online survey and snowball sampling method. Brief information about the study and a webpage link to the study, were shared via WhatsApp and Telegram. The online survey was administered by Porsline (which is equivalent to Google form). Distributing the questionnaire link through various channels on social networks in Iran is a type of advertising and requires payment. Therefore, the link was distributed in several free scientific channels and participants were asked to share this link with others. After agreeing to complete the survey, participants completed demographic information and COV19-QoL questionnaire. Answering all the questionnaire items were required and the respondents could only submit the form if they answered all the questions.
Instruments
The COV19-QoL assesses the respondent’s QOL in the past week during the COVID-19 pandemic. It has 6 items rated on a 5-point Likert-type scale ranging from 1 (totally agree) to 5 (totally disagree). Total score is the sum of item scores, and higher scores indicate a more severe impact of COVID-19 on QOL (28). The COV19-QoL was administered to 1346 participants from Croatian general population (non-clinical sample) and 201 patients with severe mental illness recruited from Bosnia and Herzegovina, Montenegro, North Macedonia and Serbia (clinical sample). Item #1 assesses the respondent’s feelings about the effects of COVID-19 on their overall QOL. Items #2 and #3 assess the respondent’s perception of possible deterioration in their mental and physical health. Items #4 and #5 assess anxiety and depression related to physical health and risk of being contaminated. The last item assesses the respondent’s perception of personal safety (28).
Translation process
First of all, the approval of the developer of the scale was obtained to translate it into Persian. Then, the scale was translated using the forward and backward method, so that it was first translated from English to Persian, and then back-translated into English by two other translators. The final version of the scale was developed by the research team (31). In order to increase the accuracy of the study, the cooperation of the original developer of the scale was sought.
Face and content validity
Face and content validity were assessed qualitatively. Cognitive interviews were used to assess face validity. In addition, 10 experts reviewed the items, and determined ambiguous items. Content validity shows the degree an instrument covers the concepts of interest (32). In order to assess content validity, 5 experts (two nurses, a health promotion expert, a psychiatrist, and a sociologist) were asked to assess the content of the Persian version of the scale. The ceiling and floor effects were also examined. When more than 15% of respondents obtain the lowest or highest possible scores, floor or ceiling effect is present, respectively (33), and the presence of these effects indicates that extreme items may be missing in the upper or lower end of the scale; this shows inadequate content validity (34).
Data analysis
The data was analyzed using PASW v18 and LISREL v8.8, as follows:
Construct validity
An EFA using Maximum likelihood and Promax rotation was used to assess underlying (or latent) relationships between the variables. Sampling adequacy was examined using Kaiser–Meyer–Olkin (KMO) coefficient. KMO values ranging from 0.7 to 0.8 and from 0.8 to 0.9 are considered good and great, respectively. High KMO values (more than 0.7) usually show that factor analysis is appropriate for the data (35). The Bartlett’s test of sphericity was used to examine the significance of the correlation matrix between the variables. A cut-off point of 0.30 was considered for factor loadings. The CFA was performed to examine whether the data conform to the theoretical model. It was conducted based on the results of the EFA using maximum likelihood estimation method and covariance indices. Goodness-of-fit was assessed using goodness-of-fit index (GFI), relative chi-square (χ2/df), normed fit index (NFI), comparative fit index (CFI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA) (36). The following values were considered acceptable for the aforementioned indices: χ2/df ≤ 2, GFI, CFI, and NFI > 0.95, RMSEA < 0.06, and SRMR < 0.08 (37, 38). Independent t-test and one-way analysis of variance (ANOVA) were used to compare the mean scores of quality of life in the two groups and more than the two groups, respectively.
Reliability
Internal consistency was assessed using Cronbach’s alpha coefficient and McDonald's omega, and relative stability was examined using interclass correlation coefficient (ICC) with two-way mixed effects, and 95% confidence interval; ICC values higher than 0.75 are regarded acceptable (39). Absolute stability was calculated by assessing standard error of measurement (SEM).
SEM was calculated using the following formula: SEM = SDbaseline × √(1 − ICC), and MDC was calculated by the following formula: MDC = 1.96 × √(2) × SEM. MDC is defined as the minimal amount of change that is not likely to be a result of measurement error (40). According to the classical test theory, error is the difference between a true score and an observed score (41, 42). Therefore, when measuring an individual, the true score may not be known as a result of variation in measurement. The threshold provided by the MDC data allows researchers to be confident that above a certain point, changes in scores are not just due to measurement error (43).
Ethical considerations
The present study is based on a research project approved by the research committee at Shahrekord University of Medical Sciences (IR.SKUMS.REC.1399.202). Before starting the study, the objectives were explained to the participants. In addition, the participants were not required to write down their real names on the questionnaires. Moreover, they were reassured that their personal information remained confidential.
Results
The sample included 488 individuals with a mean age of 28.90 ± 11.51 years. The majority of participants were female (75.6%), single (54.3%) and with college education (66.2%). Table 1 presents the average quality of life score by demographic characteristics. The impact of COVID-19 was higher on healthy participants than those with underlying conditions (16.81 ± 5.67 vs. 14.75 ± 5.68, p = 0.004), and also on single participants than those who were married (16.97 ± 5.51 vs. 15.86 ± 5.90, p = 0.032). In addition, there was no association between QOL and age, gender and education. The mean score of each item by demographic variables is presented in Table 2. The mean score of all items was higher in men than women, in single people more than married people and in healthy people more than people with comorbidities. Gender group showed a significant difference only for item I2, with males having higher scores. Marital status revealed a significant difference only for I3 and I6 items; conversely, educational status showed a significant difference for all items except for I2 and I6. Educational status of the population did not reveal any significant difference in the mean item score for any items. Total score on the COV19-QoL is calculated by summing the scores of the six items, and higher scores indicate better QOL. The mean QOL score was 16.46 ± 5.71.
Table 1.
Mean score of quality of life by demographic variables
| Variable | n | % | Mean (SD) | Statistical test | Results |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 119 | 24.4 | 17.13 (6.08) | Independent T test |
p = 0.145 t = 1.461 |
| Female | 369 | 75.6 | 16.25 (5.58) | ||
| Marital status | |||||
| Married | 265 | 54.3 | 15.86 (5.90) | Independent T test |
0.032 t = 2.148 |
| Single | 223 | 45.7 | 16.97 (5.51) | ||
| Comorbidity | |||||
| Yes | 81 | 16.6 | 14.75 (5.68) | Independent T test |
p = 0.030 t = 2.981 |
| No | 407 | 83.4 | 16.81 (5.67) | ||
| Educational Level | |||||
| Elementary | 42 | 8.6 | 15.90 (7.45) | One-way analysis of variance |
0.213 F = 1.461 |
| High school/ Diploma | 123 | 25.2 | 16.93 (5.66) | ||
| University degree | 323 | 66.2 | 16.36 (5.48) | ||
Table 2.
Item wise mean score comparison based on demographic variables
| Variable | I1 | I2 | I3 | I4 | I5 | I6 |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 2.44 (1.23) | 2.95 (1.29) | 3.07 (1.21) | 2.62 (1.14) | 2.95 (1.36) | 3.07 (1.30) |
| Female | 2.38 (1.13) | 2.64 (1.14) | 3.05 (1.20) | 2.49 (1.10) | 2.70 (1.20) | 2.97 (1.26) |
| p value† | 0.637 | 0.013* | 0.866 | 0.284 | 0.293 | 0.434 |
| Marital | ||||||
| Single | 2.45 (1.12) | 2.81 (1.15) | 3.16 (1.15) | 2.56 (1.10) | 2.84 (1.28) | 3.13 (1.26) |
| Married | 2.34 (1.20) | 2.60 (1.23) | 2.92 (1.25) | 2.48 (1.11) | 2.66 (1.20) | 2.83 (1.27) |
| p value† | 0.289 | 0.058 | 0.029* | 0.442 | 0.119 | 0.010* |
| Comorbidity | ||||||
| No | 2.45 (1.16) | 2.75 (1.17) | 3.15 (1.19) | 2.57 (1.09) | 2.83 (1.23) | 3.02 (1.27) |
| Yes | 2.12 (1.09) | 2.53 (1.29) | 2.59 (1.15) | 2.25 (1.17) | 2.41 (1.25) | 2.82 (1.30) |
| p value† | 0.018* | 0.116 | 0.001* | 0.018* | 0.006* | 0.193 |
| Educational status | ||||||
| Elementary | 2.40 (1.36) | 2.57 (1.36) | 2.69 (1.37) | 2.66 (1.35) | 2.66 (1.42) | 2.90 (1.55) |
| High school/ Diploma | 2.50 (1.14) | 2.73 (1.16) | 3.09 (1.21) | 2.69 (1.12) | 2.88 (1.24) | 3.00 (1.25) |
| University degree | 2.36 (1.14) | 2.73 (1.18) | 3.09 (1.17) | 2.44 (1.06) | 2.73 (1.22) | 3.00 (1.24) |
| P value†† | 0.516 | 0.696 | 0.117 | 0.065 | 0.437 | 0.889 |
*p < 0.05
†Based on independent samples t test
††Based on one-way ANOVA
Due to the simplicity of the items and the accurate translation, which was done under the supervision of the original designer, none of the items changed in face and content validity. In addition, both the ceiling and floor effects were found to be 0 and 2%, respectively, indicating good content validity of the scale.
Construct validity
Exploratory factor analysis (EFA)
A KMO value of 0.894 was found, and Bartlett’s test of sphericity was significant (X2 = 1400.651, df = 15, p = 0.001). The analysis revealed one factor that explained 55.967% of the total variance. (Table 3).
Table 3.
Exploratory factor analysis of the Persian version of the COV19-QoL
| Due to the COVID-19 pandemic | Factor loading | Mean (SD) | h2 |
|---|---|---|---|
| 1. …I think I have a lower quality of life than before | 0.691 | 2.40 (1.16) | 0.477 |
| 2. …I believe my mental health has declined | 0.814 | 2.72 (1.19) | 0.662 |
| 3. …I think my physical health may decline | 0.708 | 3.05 (1.20) | 0.502 |
| 4. …I am more tense than before | 0.754 | 2.52 (1.11) | 0.569 |
| 5. …I am more depressed than before | 0.814 | 2.76 (1.24) | 0.663 |
| 6. …I feel that my safety is in danger | 0.697 | 2.99 (1.27) | 0.486 |
| % variance | 55.967 | ||
| Eigen value | 3.789 | ||
| Internal consistency | Omega = 0.882; Alpha = 0.823 | ||
M: Mean; SD: Standard deviation
Confirmatory factor analysis
In the CFA, the model had a good fit. The examined goodness fit indices were as follows: normal fit index (NFI) = 0.98, root mean square error of approximation (RMSEA) = 0.052, goodness-of-fit index (GFI) = 0.0.97, standardized root mean square residual (SRMR) = 0.030, comparative fit index (CFI) = 0.963, and incremental fit index (IFI) = 0.99. The results of the CFA are presented in Fig. 1.
Fig. 1.
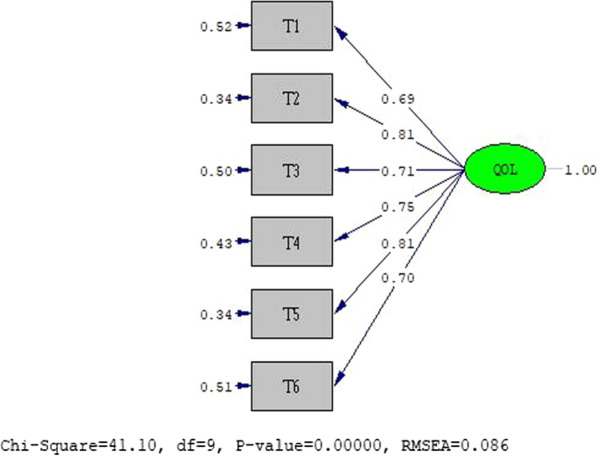
The final model
Reliability
Internal consistency of the scale was found to be 0.823 and 0.882 using Cronbach’s alpha coefficient and McDonald’s omega, respectively. In addition, relative stability of the scale with a two-week interval was found to be 0.837 (95% confidence interval: 0.686–0.935). Examination of absolute stability revealed a SEM of 1.8 and a MDC of 3.5.
Discussion
Validity and reliability are important indicators of instruments. The former indicates the accuracy of an instrument and the latter shows its stability (44). The present study was aimed at assessing the validity and reliability of the Persian version of the COV19-QoL. This tool has been designed to assess the effects of COVID-19 on QOL of people from the general population. The fast spread of COVID-19 has led to significant stress and anxiety among populations, and due to isolation, closure of schools, and loss of jobs, people may experience high levels of distress and their QOL of may be negatively influenced; therefore, assessing the effects of pandemic on QOL has an important role in taking necessary measures to combat these problems.
Under the supervision of the original tool designer, the translation process was carried out so the final Iranian version accurately represents the original one. Due to the small number of items and carefully guided translation, nothing changed in its face validity and content. Ceiling and floor effects were found to be 0% and 2% respectively, indicating that items showing the maximum and minimum intensity of the phenomenon are included in the scale, and that it has good content validity (33).
The COV19-QoL is a unidimensional instrument assessing QOL during the COVID-19 pandemic. According to the results of EFA, the variance explained for each item was higher than 0.4, and all factor loadings were higher than 0.6; these results were consistent with those found for the original version of the scale (28). In the original version of the scale, the highest factor loadings in the clinical (0.861) and non-clinical (878) samples were for item #4 (I am more tense than before). In the Persian version, the highest factor loadings were for items #5 (I am more depressed than before) and #2 (I think my mental health has declined) that both had a factor loading of 0.814. This difference can be attributed to cultural differences between the populations under study and different effects of COVID-19 on their QOL.
Internal consistency of the original version of the scale, based on Cronbach’s alpha coefficient, was found to be 0.856 and 0.885 in clinical and non-clinical samples, respectively (28). In addition, internal consistency of the Persian version of the scale was found to be 0.882 and 0.823 using Cronbach’s alpha coefficient and McDonald's omega. In contrast to the original version, absolute stability of the Persian version using SEM and MDS was found to be 1.8 and 3.5, respectively. SEM = 3.5 shows that if there is 3.5 points change in the total score after the intervention, we can be 95% confident that a true change has been occurred in QOL. The COV19-QoL had acceptable stability and internal consistency. Although a low Cronbach’s alpha coefficient was expected due to low number of items, an alpha of 0.8 was found that was great.
The results showed that the COV19-QoL scores were higher in healthy individuals than those with underlying conditions, and also in single than married participants. Healthy individuals may be more concerned about their health than those with underlying conditions. In other words, people with underlying conditions are more able to adjust to the COVID-19 pandemic, because they have experienced other conditions. In the original version, the quality of life of healthy people (non-clinical samples) was more affected compared to patients (clinical sample) and the mean score of all items of COV-19QoL in healthy people was higher than patients (28).
In addition, single individuals may experience more problems during the pandemic due to receiving less social support. A review study by Sanyaolu et al. showed that people with underlying conditions, such as diabetes and high blood pressure were more likely to die from COVID-19 than healthy individuals (45). Samlani et al. examined the QOL of their participants during the COVID-19 pandemic using the SF-12. The results of this study showed that there was a higher decrease in the QOL of participants compared to the quality of their physical life (26). In a study among cancer patients, Greco et al. found a higher decrease in the psychological aspect of QOL than its physical aspect during the COVID-19 pandemic (25).
Two main advantages of the present study were identified. They include (1) the use of CFA which was not conducted in the original study on the scale validity and (2) the calculation of two coefficients to examine the reliability of the scale. The main limitation of the study, as in most correlational studies, was the snowball (that is, non-probabilistic) sampling which does not guarantee that the findings and conclusions can be generalized without reasonable caution. Another limitation of this study was the lack of convergent validity.
Conclusion
The COV19-QoL is a valid and reliable instrument to assess the effects of COVID-19 on the quality of life of the general population. Therefore, it can be used in future studies.
Acknowledgements
The researchers would like to express their gratitude to the Deputy of Research of the Shahrekord University of Medical Sciences for acceptance, and approval of this research project. We also thank all the participants in this study.
Abbreviations
- CFA
Confirmatory factor analysis
- CFI
Comparative fit index
- COV19-QoL
COVID-19-impact on Quality of Life
- EFA
Exploratory factor analysis
- GFI
Goodness-of-fit index
- ICC
Interclass correlation coefficient
- KMO
Kaiser–Meyer–Olkin
- MDC
Minimal detectable change
- NFI
Normed fit index
- PASW
Predictive Analytics SoftWare
- QoL
Quality of life
- RMSEA
Root mean square error of approximation (RMSEA)
- SEM
Standard error of measurement
- SRMR
Standardized root mean square residual
- WHO
World Health Organization
Authors' contributions
RGG: data collection and manuscript preparation; AHD: manuscript preparation and study conceptualization; BM: study design; MR and SR: final revision and grammar editing; AE: statistical analysis. All authors read and approved the final manuscript.
Funding
This study was funded by the Shahrekord University of Medical sciences. The funding body had no role in the design of the study, data collection, and interpretation of result or in writing of the manuscript.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study has been approved by the Research Ethics Committee of Shahrekord University of Medical sciences. Written informed consent was received from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ali Hasanpour Dehkordi, Email: alihassanpourdehkordi@gmail.com.
Marzieh Aslani, Email: aslamnm63@yahoo.com.
Abbas Ebadi, Email: Ebadi1347@yahoo.com.
Selman Repišti, Email: selman9r@yahoo.com.
Borhan Moradveisi, Email: b.moradvaesi@yahoo.com.
Reza Ghanei Gheshlagh, Email: Rezaghanei30@gmail.com.
References
- 1.Wuhan Municipal Health Commission. Wuhan Municipal Health Commission’s Briefing on the Pneumonia Epidemic Situation. Available online: http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989 (Accessed on 31 December 2019).
- 2.Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross-sectional study. Int J Environ Res Public Health. 2020;17(7):2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization, 2020. The Coronavirus Disease (COVID-19) Outbreak.
- 4.https://www.who.int/ (Access March 30th 2020).
- 5.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. New Engl J Med. 2020;382:727. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease (COVID-19) in some regions of China. Psychol Health Med. 2019;2020:1–10. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- 7.Ahorsu DK, Lin C-Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020. [DOI] [PMC free article] [PubMed]
- 8.Rehman U, Shahnawaz MG, Khan NH, Kharshiing KD, Khursheed M, Gupta K, et al. Depression, anxiety and stress among Indians in times of Covid-19 lockdown. Community Ment Health J. 2020;57:1–7. doi: 10.1007/s10597-020-00664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. IJERPH. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. 2020;277:379–91. [DOI] [PMC free article] [PubMed]
- 11.Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mamun MA, Griffiths MD. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian J Psychiatry. 2020;51:102073. doi: 10.1016/j.ajp.2020.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Islam SD-U, Bodrud-Doza M, Khan RM, Haque MA, Mamun MA. Exploring COVID-19 stress and its factors in Bangladesh: a perception-based study. Heliyon. 2020;6(7):e04399. doi: 10.1016/j.heliyon.2020.e04399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suicide leading cause for over 300 lockdown deaths in India s, study. (2020). The Economic Times. Retrieved May 5 f, https://economictimes.indiatimes.com/news/politics-and-natio, n/suicide-leading-cause-for-over-300-lockdown-deaths-in-india, saysstudy/articleshow/75519279.cms.
- 15.Sharma PGS, Kushwaha P, Shekhawat K. Impact of Mass Media on Quality of Life during COVID-19 pandemic among Indian Population. Int J Sci Healthcare Res. 2020;5(3):260–267. [Google Scholar]
- 16.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. 2020;87:40–8. [DOI] [PMC free article] [PubMed]
- 18.Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. 2020;29:2047. doi: 10.1111/jocn.15296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Le XTT, Dang KA, Toweh J, Nguyen QN, Le HT, Toan DTT, et al. Evaluating the psychological impacts related to COVID-19 of Vietnamese people under the first Nationwide partial lockdown in Vietnam. 2020;11:824. [DOI] [PMC free article] [PubMed]
- 20.Tran BX, Nguyen HT, Le HT, Latkin CA, Pham HQ, Vu LG, et al. Impact of COVID-19 on economic well-being and quality of life of the Vietnamese during the national social distancing. 2020;11. [DOI] [PMC free article] [PubMed]
- 21.Wang C, Chudzicka-Czupała A, Grabowski D, Pan R, Adamus K, Wan X, et al. The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. 2020;11:901. [DOI] [PMC free article] [PubMed]
- 22.Ihsan N, Aziz B. A multidimensional analysis of quality of life: Pakistan’s context. Soc Indic Res. 2019;142(1):201–227. doi: 10.1007/s11205-018-1903-6. [DOI] [Google Scholar]
- 23.Farajzadeh M, Gheshlagh RG, Sayehmiri K. Health related quality of life in Iranian elderly citizens: a systematic review and meta-analysis. Int J Community Nurs Midwifery. 2017;5(2):100–111. [PMC free article] [PubMed] [Google Scholar]
- 24.Ciążyńska M, Pabianek M, Szczepaniak K, Ułańska M, Skibińska M, Owczarek W, et al. Quality of life of cancer patients during coronavirus disease (COVID‐19) pandemic. Psycho-oncology. 2020. [DOI] [PMC free article] [PubMed]
- 25.Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TT, Pham KM, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: The potential benefit of health literacy. J Clin Med. 2020;9(4):965. doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greco F, Altieri VM, Esperto F, Mirone V, Scarpa RM. Impact of COVID-19 Pandemic on Health-Related Quality of Life in Uro-oncologic Patients: What Should We Wait For? Clinical Genitourinary Cancer. 2020. [DOI] [PMC free article] [PubMed]
- 27.Samlani Z, Lemfadli Y, Errami AA, Oubaha S, Krati K. The impact of the COVID-19 pandemic on quality of life and well-being in Morocco. 2020.
- 28.Frey MK, Ellis AE, Zeligs K, Chapman-Davis E, Thomas C, Christos PJ, et al. Impact of the coronavirus disease 2019 pandemic on the quality of life for women with ovarian cancer. Am J Obstet Gynecol. 2020;223(5):721–725. doi: 10.1016/j.ajog.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Repišti S, Jovanović N, Kuzman MR, Medved S, Jerotić S, Ribić E, et al. How to measure the impact of the COVID-19 pandemic on quality of life: COV19-QoL–the development, reliability and validity of a new scale. Global Psychiatry. 2020;1 (ahead-of-print).
- 30.Plichta SB, Kelvin EA, Munro BH. Munro's statistical methods for health care research: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2012.
- 31.Mundfrom DJ, Shaw Sg, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Test. 2005;5:159–168. doi: 10.1207/s15327574ijt0502_4. [DOI] [Google Scholar]
- 32.World Health Organisation. Process of translation and adaptation of instruments. Geneva: WHO. Available from: https://www.who.int/substance_abuse/research_tools/translation/en/. Accessed March 31, 2020.
- 33.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 34.Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 35.Kievit AJ, Kuijer PPF, Kievit RA, Sierevelt IN, Blankevoort L, Frings-Dresen MH. A reliable, valid and responsive questionnaire to score the impact of knee complaints on work following total knee arthroplasty: the WORQ. J Arthroplasty. 2014;29(6):1169–1175. doi: 10.1016/j.arth.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 36.Kline RB. Principles and practice of structural equation modeling: Guilford Publications; 2015.
- 37.Bollen KA, Noble MD. Structural equation models and the quantification of behavior. Proc Natl Acad Sci. 2011;108(Supplement 3):15639–15646. doi: 10.1073/pnas.1010661108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tabachnick BG, Fidell LS, Ullman JB. Using multivariate statistics. Pearson, Boston, 2007.
- 39.Lt Hu, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model: Multidiscip J. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 40.Ebadi A, Ausili D, Albatineh AN, Salarvand S, Ghashlagh RG. Psychometric evaluation of the Farsi version of the self-care of diabetes inventory in iranian patients with diabetes. Diabetes Metab Syndrome Obes: Targets Therapy. 2019;12:2775. doi: 10.2147/DMSO.S235436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haley SM, Fragala-Pinkham MA. Interpreting change scores of tests and measures used in physical therapy. Phys Ther. 2006;86(5):735–743. doi: 10.1093/ptj/86.5.735. [DOI] [PubMed] [Google Scholar]
- 42.Dimitrov DM, Rumrill PD., Jr Pretest-posttest designs and measurement of change. Work. 2003;20(2):159–165. [PubMed] [Google Scholar]
- 43.DeVon HA, Block ME, Moyle-Wright P, Ernst DM, Hayden SJ, Lazzara DJ, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–164. doi: 10.1111/j.1547-5069.2007.00161.x. [DOI] [PubMed] [Google Scholar]
- 44.Fike DS, Denton JM, Esparza S, Palombaro K. Calculation of minimal detectable change of construct subscales of a cultural competence instrument. J Phys Therapy Educ. 2016;30(1):25–30. doi: 10.1097/00001416-201630010-00004. [DOI] [Google Scholar]
- 45.Hajiesmaello M, Kariman N, Sharif Nia H, Ozgoli G, Hajian S, Bazzazian S, et al. The translation and psychometric assessment of the perception of empowerment in midwifery scale: the Persian version. BMC Health Serv Res. 2020;20:1–9. doi: 10.1186/s12913-019-4778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, et al. Comorbidity and its impact on patients with COVID-19. SN Comprehen Clin Med. 2020;2:1–8. doi: 10.1007/s42399-019-00207-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


